SUMMARY
This study examines the relationship between contextual factors and attendance in a family-based HIV prevention program for low-income, urban, African-American women and their children. Participants’ motivations to become involved, their concerns about discussing sex-related issues with their children, recruiters’ perceptions of respondents’ understanding of the program, and environmental stressors were examined. Participants’ level of motivation and recruiters’ success in improving respondents’ understanding of the program were significant correlates of attendance. Stressors experienced by the family and concerns around talking with children about sex were not significantly associated with participation. Recommendations to enhance involvement in family-based HIV prevention programs are made.
Keywords: Attendance, HIV/AIDS prevention, African-American, families, women
INTRODUCTION
The HIV/AIDS epidemic is now entering its third decade. In the U.S., the number of AIDS cases has increased significantly among African-American females (Wortley & Fleming, 1997). In 1992, 14% of adults/adolescents with AIDS were female. By 1999 this number had risen to 20% (Centers for Disease Control and Prevention [CDC], 2002a). The CDC’s HIV/AIDS surveillance reports also indicate that a growing number of young adolescents (ages 13 to 19) have been contracting HIV (CDC, 2002b). In 2001, approximately one in four new cases of HIV infection were under 21 years of age (CDC, 2001). Ethnic minority adolescents are at highest risk for contracting STDs (DiLorenzo & Hein, 1993; Jemmott & Jemmott, 1992) compared to white adolescents. AIDS, genital herpes and gonorrhea disproportionately affect African-Americans (Adler, Boyce, Chesney, Cohen et al., 1994; CDC, 2003; Thomas & Bartelli, 2001). Adolescents have been contracting HIV at high rates (CDC, 2002a), and economically deprived young females have high rates of pregnancy (Children’s Defense Fund, 2000), further evidence of unprotected sex.
Given that there is currently no cure nor vaccine for AIDS, effective prevention strategies are critical. In particular, prevention programs that can reach high-risk populations, such as ethnic minority women and adolescents, need to be developed and disseminated. In response to this need, a cadre of prevention scientists have focused on developing programs that can reach minority females and adolescents of both genders (CDC, 2002c). Although these programs have been shown to be effective (see compendium created by Centers for Disease Control and Prevention, 2002c), they nonetheless remain focused on the individual, and are not designed to target simultaneously the prevention needs of mothers and their children.
The development and testing of family-based HIV prevention programs are warranted (Pequegnat&Szapocznik, 2000). Family relationship and family processes have been significantly associated with sexual behaviors in adolescence (Biglan, Matzler, Wirt, Ary et al., 1990; Black, Ricardo, Stanton et al., 1997; Romer, Black, Ricardo, Feigelman et al., 1994). Family-based HIV prevention approaches aim to strengthen the relationship between parents and youth, thus improving family communication, increasing HIV knowledge, and decreasing the sexual risk behaviors of all family members.
A family-based approach is a good model for African-American families, because it is consistent with the way African-American families and communities address psychosocial challenges (Boyd-Franklin, 1993), including conflicts between sexually active adolescents and their parents (Black et al., 1997). It is known that family relationships may influence adolescent health behavior (Walter, Vaughan&Cohall, 1993; Walter, Vaughan, Ragin, Cohall et al., 1994). For these reasons, and because a family may serve as a protective factor against high-risk sexual behavior, the present study highlights a family-based HIV prevention program for African-American families.
Ethnic and racial minorities’ involvement in prevention efforts is low, and little is known about the factors that influence minority families to become involved in HIV prevention programs (Escobar-Chavez, Tortolero, Masse, Watson & Fulton, 2002; National Institute of Mental Health, 1997). Understanding the influences on involvement in HIV prevention programs may help researchers and health practitioners design programs that will be better attended by the minority populations most at risk for HIV exposure. This study is thus designed to examine associations between contextual factors and attendance of low-income, African-American families in the Collaborative HIV Prevention and Adolescent Mental Health Project (CHAMP), an urban HIV prevention effort for African-American families. Recommendations are made below to enhance attendance in HIV prevention programs and to maximize the retention of participants.
High rates of transmissible disease among minority families point to several HIV-related risk factors, including health risk behaviors, poverty, poor health care, and insufficient access to health promotion programs. Studies on the use of HIV health-related services show that African-Americans have more problems accessing HIV services than do majority groups (Bonuck, Arno, Green, Fleishman et al., 1996; Kiefe & Hyman, 1996). Therefore, it is crucial to identify factors that might influence minority populations to use HIV prevention programs.
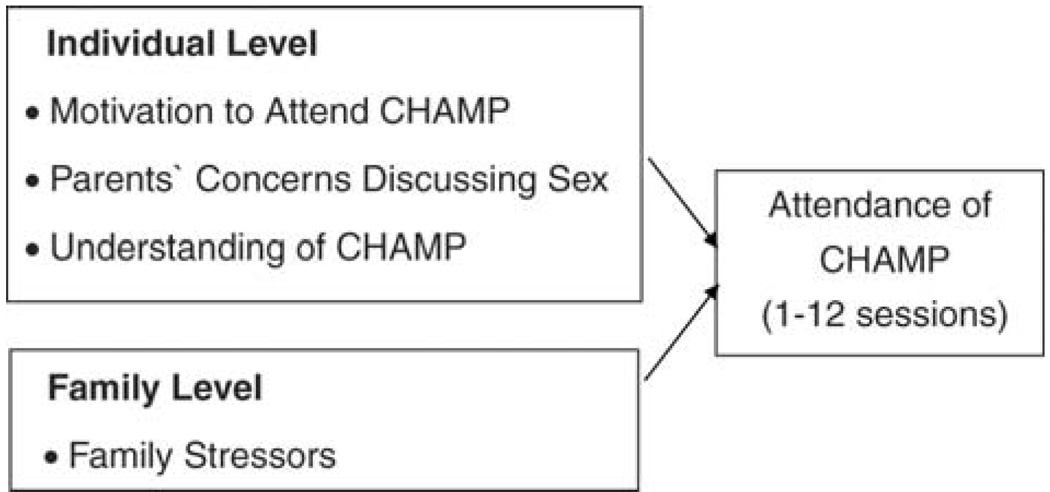
Lengthy interventions have been identified as necessary, particularly for urban families who experience significant stressors and have access to fewer resources (Wahler & Dumas, 1989; Webster-Stratton, 1985). The high-risk context in which many families reside necessitates the intensity of these interventions. Following an ecological perspective of myriad factors influencing attendance, the present study explores individual and family level factors that may influence involvement in CHAMP (Figure 1–for the full model, see McCormick et al., 2000).
FIGURE 1.
Potential Correlates of Attendance in CHAMP
This framework presents hypothetical relationships among factors that could influence participation in CHAMP. McCormick et al. (2000) propose multiple factors that could influence attendance in family-based prevention programs, such as CHAMP. These include factors at the individual level (e.g., motivation), family level (e.g., child care), program level (e.g., length, location), and community level (e.g., poverty). Following this framework, the present study examines motivation and impediments to involvement in CHAMP at the individual and family levels. At the individual level, motivation to participate, parents’ concerns about discussing sex-related issues with their children, and recruiters’ success in helping parents better understand the program are explored. At the family level, the presence of family stressors is tested in association with attendance in CHAMP. A review of these factors is presented below.
MOTIVATION AND UNDERSTANDING
Various factors have been shown to positively influence involvement in prevention programs, including recruitment and service delivery strategies (Prochaska, Redding&Evers, 1997), reminders from services providers (Larson, 1982), monetary incentives (Greenberg, Lifshay, Van Devanter, Gonzales & Celentano, 1998), and availability of social supports (Cohen, 1988; Epstein&Wing, 1987; Madison, McKay, Paikoff & Bell, 2000; Pinto & McKay, 2005). The program being tested here–CHAMP–is family-focused and has been developed with community input. This program provides: (1) individualized recruitment (e.g., home visits, phone calls) and one-on-one opportunities for learning about CHAMP; (2) monetary incentives; and (3) opportunities for development of social support. It is expected that these characteristics would enhance respondents’ understanding of the program, and motivate their attendance. Therefore, recruiters’ success in helping respondents understand CHAMP and motivation are expected to be positively associated with attendance of the program.
Individual level characteristics, such as age, race and education (Lacey, Tukes, Manfredi & Warnecke, 1991; Pettaway & Frank, 1999; Pinto, 2003), attitudes toward prevention services (Montaño, Kasprzyk&Taplin, 1997), cultural beliefs and values (Pinto & McKay, in press; Thomas & Bartelli, 2001), have been shown to influence involvement in HIV prevention programs. Although they are important, age, race, education and other demographic characteristics are not examined here. This study focuses exclusively on a sample of young African-American women, most of whom have similar educational, employment and income backgrounds.
CONCERNS ABOUT DISCUSSING SEX
It has been reported that the adults in a family can influence adolescents’ sexual attitudes and behaviors (Jemmott & Jemmott, 1992; Pick & Palos, 1995), and as a consequence help adolescents refrain from high-risk sexual behaviors. Since adolescents usually confront situations of sexual possibility before they become sexually active (McBride, Paikoff & Holbeck, 1999; Paikoff, 1995, 1997), CHAMP supports parents in helping their children avoid sexual possibilities at a young age by promoting family communication to address both sexual opportunities and abstinence. The program focuses on communication between adult caretakers and adolescents because communication between parents and children has been found to decrease adolescents’ high-risk behavior (Holtzman & Rubinson, 1995; Moore & Chase-Lansdale, 2001). Moreover, family communication about sex-related issues has been found to be associated with delays in initial sexual activity (Carabasi, Greene & Bernt, 1992; Holtzman & Rubinson, 1995; Hutchinson & Cooney, 1998; Jessor&Jessor, 1975; Romer et al., 1994; Pistella&Bonati, 1999).
Since communication between parents and their pubescent children about sexual development and sexual activity may help delay sexual activity and reduce risk behavior, CHAMP fosters parent-child interactions and communication about puberty, sex and HIV prevention. Therefore, it is expected that parents who hesitate to discuss sex-related topics with their children might be disinclined to attend a program that specifically encourages this type of communication. In order to clarify this assumption, the present study examines the association between parents’ concerns about discussing sex-related topics and their attendance at CHAMP.
FAMILY STRESSORS
A myriad of environmental stressors affect families, particularly minority families in urban areas. Tolan, Miller, and Thomas (1987) contend that environmental stressors on families are distributed across four key domains. Induced transition stressors include situations that change the patterns of family behavior (e.g., moving to a new house, discovery of learning problems). Developmental transition stressors refer to expected life changes that prompt reorganization of family structure (e.g., marriage, pregnancy). Circumscribed life events can be either short- or long-term, and include life events such as drug use, being robbed, and being arrested. Exposure to violence refers to both witnessing and experiencing criminal violent activities, including physical attack and death.
McCormick et al. (2000) underscore that multiple stressors–including time constraints, child care, and discouragement from other family members– may affect attendance in prevention programs. Many families that participated in CHAMP reported myriad stressors from each of the four domains in the year prior to their participation in the program. This raises the question of whether or not the presence of multiple stressors became a barrier to CHAMP attendance. Knowing that family stressors create difficulties in retaining participants in mental health services beyond the first session (Bui & Takeuchi, 1992; Cohen & Hesselbart, 1993; Kazdin, 1993) provides yet more support for exploring whether or not family stressors influence retention in HIV prevention programs. Therefore, the present study examines the association between the number of stressors experienced by participant families and their attendance in CHAMP.
Guided by the understanding that contextual factors at the individual and family levels influence attendance, it is expected that selected factors examined here are associated with attendance of African-American families in CHAMP. The program’s 12 weekly sessions, two hours each, are designed to help low-income African-American women and their adolescent children cope with daily struggles, and to incorporate health-promoting behaviors into their lives (Madison et al., 2000; McKay et al., 2000). CHAMP is delivered through multi-level group modalities (Tolan&McKay, 1996), which include 12 multi-family sessions (Paikoff & McKay, 1995).
Given CHAMP’s goal of promoting communication and support both within and between families, the idea of combining families into groups is a logical format for program delivery. In addition to family needs, children and parents within families have individual needs. For parents, these needs include support from other parents, frank discussion of strategies for supervision and monitoring, and chances to discuss information and communication strategies away from their children. For children, these needs include developing peer supports, developing social problem skills to assist them in recognizing risk situations, and negotiation skills to deal with such situations. Thus, a combination of multiple family sessions and parent/child sessions are used.
METHODS
Sample and Design
The current study employs a cross-sectional research design, and includes data from a sample that represents the first three cohorts of children and their adult caretakers (N = 227 families). We used baseline data derived from the Chicago HIV Prevention and Adolescent Mental Health Project (CHAMP), a family-based HIV prevention study involving low-income, African-American adults and their preadolescent children (McKay et al., 2000).
Families were chosen randomly starting with a pool of 550 adolescents in four Chicago inner-city public schools. Most of their families resided in public housing developments with high levels of poverty. Data examined in this study were drawn from pre-assessments completed by these adolescents’ adult caretakers, as well as from logs kept by program staff. The pre-assessment included instruments for collecting demographic data, social problem-solving methods, family stressors, and family processes. Respondents were paid $25 for completing the pre-test. Trained research staff assisted the participants by reading each item aloud.
Measures
CHAMP Attendance
The dependent variable for the current study is total attendance. It is operationalized as the number of sessions (one to 12) participants attended. Attendance was documented on sign-in sheets for each session. Respondents signed their names and indicated the attendance of their children.
CHAMP Impediments Scale
This is a 5-item rating scale (Gillman& McKay, 1996), completed by program recruiters for each family in the program. The scale aims to determine factors that might influence families not to attend some sessions of the program. The items in this scale are scored along a 4-point Likert-type scale ranging from “Not at all” to “Very much.” To assess the degree to which participants were motivated to attend CHAMP, program staff answered the single question, “Overall, how much did parents want to come to CHAMP?” To assess participants’ concerns about discussing sex-related issues with their children, the question, “How concerned was the parent about talking with her child about sex?” was used. To assess participants’ understanding of CHAMP, facilitators were asked “Do you feel that you helped the family to understand what the CHAMP family program is about?”
CHAMP staff were trained during weekly supervision sessions regarding data collection for this study. They were instructed to ask potential participants directly about items included on the Impediments Scale. In order to rate respondents’ motivation, recruiters also probed about their motivation to participate, their perceptions of participants’ understanding of the goals of CHAMP, and any barriers to involvement.
Family Stress Scale
This 21-item scale (Tolan et al., 1987) was used to identify environmental stressors faced by the families attending CHAMP. The scale was completed by adult participants. The scale identifies types of stressful events affecting urban families (see Guerra & Tolan, 1991). This measurement assesses whether participants have experienced stressful events within the four domains previously mentioned (e.g., “Spent a lot of time away from the family,” “Gotten divorced,” “Had a close relative or friend die”).
Single stressors usually do not remain isolated over time. Indeed, any combination of different stressors may appear in a family at different points of its development. Socioeconomically disadvantaged families are especially embedded in contexts of multiple stressors, which together may have an impact in several areas of family life (Dohrenwend, 2000; Dohrenwend, Askenasy, Krasnoff&Dohrenwend, 1978; Mellins & Ehrhardt, 1994; Pearlin, 1999). Guided by this theory of multiple stressors, a composite was created to represent the total number of stressors experienced by participating families.
Analytical Approach
As the theoretical model suggests, it was expected that several variables would influence attendance in the CHAMP program. A multiple linear regression model was used to examine simultaneously the relationship of several independent variables with attendance (Cohen & Cohen, 1983). Regression coefficients were used to estimate the magnitude of influence of the independent variables on attendance.
RESULTS
Two thirds of the youth involved in the CHAMP study were being reared by a female caregiver alone. Fifty percent of these single caregivers were the adolescents’ mothers; the remaining 50% comprised other female relatives, such as grandmothers or aunts. Of the children selected, 133 (59%) were females, and 94 (41%) were males. All participants were of African-American heritage. Ages ranged from nine to 15 years, with a mean age of 11.6 years (SD = 1.21). Generally, only one adult caregiver per child attended the CHAMP intervention.
The mean age of respondent adult caretakers was 33.8 years (SD = 7.4). More than half of all respondents (58.5%) had one to five children living with them; 35.1% had five or more; but 9.2% of all respondents had at least one child living outside of their home. Most respondents were not married (73.3%) at the time of interview; 66.5% were single, never married; and 11.2% were separated, divorced, or widowed.
Preliminary results indicate that of the 227 eligible families randomly chosen to receive the program, 201 (89%) were contacted by CHAMP facilitators. Twenty-six families could not be reached, primarily due to the demolition of four housing units in the target community, and relocation of families as part of revitalization efforts by the city. Of the 201 families reached, 149 (74%) attended at least one session of the program; 147 (73%) attended three or more sessions; and 127 families (63%) completed the full intervention (defined as nine to 12 sessions).
The means for the independent variables were: for parent motivation, 2.0 (SD = .9); for parents’ concerns about discussing sex with children, 2.5 (SD = 1.2); and for perceived parents’ understanding of the program, 3.1 (SD = .6). The mean number of environmental stressors within participant families was 12.4 (SD = 6.2) out of 21.
For each stressor presented, many respondents had personally experienced that stressor in their lives. For example, 61% of respondents had experienced the death of a family member. Whereas the total number of stressors was significantly related to attendance in bivariate analysis, both subscales and individual items did not yield significant correlations with attendance data, nor made significant contributions to the regression model below. Since environmental stressors are pervasive in this sample, the frequency of families reporting stressors most prevalent (stressors in at least 15% of the families) is reported in Table 1.
TABLE 1.
Families Reporting Stressors in the Past Year
| Stressor (N = 173) |
Families (%) |
|---|---|
| Had a family member die | 61 |
| Had another close relative die | 41 |
| Had a family member seriously ill or injured badly | 34 |
| Had someone in family been beaten or attacked | 27 |
| Had gotten in trouble at work, school, or with authorities | 25 |
| Had a new baby come into the family | 25 |
| Had been pregnant | 22 |
| Had spent a lot of time away from home | 20 |
| Had a major emotional problem | 20 |
| Had been arrested, or gone to court or jail | 20 |
| Had used drugs or drunk too much | 19 |
| Had seen someone beaten very badly, attacked or killed | 18 |
| Had been hit/shoved/kicked by partner during argument | 18 |
| Had moved to new home or apartment | 15 |
| Had been robbed or attacked | 15 |
Ordinary Least Square Regression analysis was used to test the relationship between total attendance and independent variables: motivation to attend; concerns around discussions of sex; family stressors; and perceived understanding of the program. The regression model explained 24% of the variance in total attendance at CHAMP, F (3, 169) = 21.3, p < .05. Participants’ levels of motivation (β= .97) and perceived understanding of the program (β= −1.5) were significant correlates to attendance. Individual stressors, total number of family stressors, as well as concerns about talking with their children about sex, did not contribute significantly to the model. See Table 2 for a summary of multivariate results.
TABLE 2.
Factors that Influence Attendance in CHAMP
| Variable | B | SE B | β | t |
|---|---|---|---|---|
| Motivation to participate | .58 | .87 | .97 | 3.0** |
| Concerns discussing sex | .29 | 1.6 | .52 | 1.2 |
| Family stressors | .22 | .43 | .03 | .34 |
| Perceived understanding of the program |
−.42 | −1.8 | −1.5 | −2.4* |
Notes: For overall model, F (3, 169), = 21.3, p < .05
R2 = .24
β = Standardized regression coefficients
p < .05
p < .01
DISCUSSION
A substantial body of knowledge on disease prevention and health promotion suggests that prevention efforts can be effective in many areas, including promotion of sexual health and prevention of sexually transmitted diseases (Muñoz, Mrazek & Haggert, 1996). Among these, many HIV prevention programs for adult women and their children have shown positive results, including the initiation and continuation of health protective behaviors, and decrease in HIV transmission (CDC, 2002c; Lauby, Smith, Stark, Person & Adams, 2000; Person & Cotton, 1996; Wingood & DiClemente, 2000).
A myriad of family-based programs have been developed to help prevent HIV/AIDS by aiding women and their children to: (1) build social support in their lives and increase their ability to cope with life’s problems (Cohen, Derish & Dorfman, 1994; McKay et al., 2000; Wingood & DiClemente, 2000); (2) endorse health-promoting attitudes and behaviors (Person & Cotton, 1996); and (3) develop ethnic and gender pride, sexual assertiveness, and social skills (DiClemente & Wingood, 1995). Overall, these programs help participants learn strategies for preventing HIV infection.
The current study uses data from CHAMP, a program for urban, African-American families, to identify factors that may influence African-American families’ attendance in HIV prevention programs. The results indicate that those potentialCHAMP participants, perceived by recruiters as motivated to participate, were indeed more likely to attend CHAMP sessions. The CHAMP program includes elements that have been shown to influence attendance when included in other prevention efforts. These elements include personalized recruitment and service delivery (Prochaska et al., 1997); monetary incentives (Greenberg et al., 1998); and availability of social supports within the program (Cohen, 1988; Madison et al., 2000).
Results also indicate that when recruiters perceive themselves as having difficulty helping potential participants understand CHAMP, those participants are likely to attend more sessions of the program. CHAMP staff members strive to help participants understand the content, the goals, and overall objectives of the program. Staff spend more time and provide more detailed explanations to participants who have difficulties understanding the program. This type of individualized attention not only improves participants’ understanding of CHAMP, but improves the attendance of those who may have had difficulty understanding CHAMP.
It is also true that participants with a better understanding of the program attend fewer sessions. Parents who clearly understand the goals and content of CHAMP know that the program encourages discussions about sexual issues and disease transmission. We contend that parents who have this knowledge and are uncomfortable about discussing sex may skip sessions focused on these topics, and thus attend fewer sessions overall.
Future research needs to explore whether recruiters put more effort into engaging those adult caretakers who seem to have less understanding about the program. Since understanding of the program was measured from the perspective of facilitators, it represents a limitation of this study, and future studies should also strive to collect data about motivation from participants. A comparison between facilitators and participants may better elucidate the relationship between participants’ understanding of a prevention program and their actual attendance.
The results also indicate that stressful events in the family were not significantly related to attendance. The Family Stress Scale–used to assess the influence of stressors on attendance–asks participants whether or not their families have experienced certain stressful events in the past year. Since individual stressors did not contribute separately to attendance, a composite was used to reflect the total number of stressful events most prevalent in this sample. It should be noted that at least 15% of the sample reported important stressors in their lives that even together did not significantly relate to attendance. We contend that families that experience more stressors may have better attendance in CHAMP because they may find both social acceptance and support which may help them address stressors. Nonetheless, future research needs to continue testing how specific stressful events may hinder attendance. By knowing participants’ specific sources of stress, practitioners can provide programs to help attenuate stress or make referrals to other programs that may help participants. In so doing, practitioners will be better able to recruit families for HIV prevention programs.
Parent concerns around discussions with their children about sex was not significantly related to attendance. It should be noted that this variable was measured by CHAMP facilitators, not participants. Again, the addition of parent reports would bolster future research studies. It is possible that recruiters may have either overestimated or underestimated participants’ concerns about sex-related discussions. A study that contrasts participants’ concerns with facilitators’ perceptions of the participants’ concerns may prove useful in better understanding correlates of attendance in HIV prevention programs.
Some authors suggest that myriad factors at many environmental levels may influence the involvement of families in prevention efforts. The current study examined only a small set of variables that may influence urban families’ attendance. The types and the small number of variables examined for association with attendance represent another limitation of this study. However, in viewing attendance of HIV prevention programs from an ecological perspective, this study demonstrates that variables shaped by both individual and environmental influences–such as motivation to participate and perceived understanding of the program–are associated with attendance of urban families in HIV prevention programs. It is recommended that future studies consider other contextual factors (e.g., community and service system influences) that may influence attendance of prevention efforts in general, and HIV prevention programs in particular.
Numerous factors have been hypothesized to motivate involvement in health prevention programs. CHAMP participants appear to be motivated to attend the program because CHAMP fosters community input in all phases of implementation, encourages participants to develop community-based activities related to other social problems, and has an attentive staff that helps participants understand the program (Pinto, 2003; Pinto & McKay, in press). Indeed, CHAMP facilitators and investigators have developed many strategies to address barriers to attendance in the program. Recruitment strategies used by CHAMP staff may prove helpful in enhancing involvement and retention of urban families in other HIV prevention efforts. Recruiters should use the following strategies to motivate potential participants:
Describe in clear and concise language the purposes and the length of the prevention program, and the specific topics that will be discussed.
Provide clear information about stipends, including whether such stipends may have an impact on participants’ receipt of public assistance.
Make personal contacts with participants in their homes or over the telephone.
Use parents who completed the program as facilitators and let their experience with the program be shared with potential participants.
Make the program available on weekends and evening hours.
Employ trained staff who are culturally competent, including local parents.
CONCLUSION
Few studies found in the literature address either the barriers or motivators encountered by minority families who might become involved in HIV prevention services. Researchers and health practitioners will be better equipped to help minority populations access HIV prevention services if they understand how these groups access and use these interventions.
This study demonstrates that participants who were perceived to be more motivated to participate were more likely to attend CHAMP. Researchers and practitioners developing HIV prevention programs need to use specific strategies that will enhance potential participants’ motivations to attend. The recommendations above may help health professionals engage minority populations–more specifically, African-American families–with strategies that reflect the factors that influence attendance of HIV prevention programs.
ACKNOWLEDGMENT
This study was supported by grants from NIMH (MH 63622) and the W. T. Grant Foundation. Dr. Pinto is currently a post-doctoral fellow supported by a training grant from NIMH (T32 MH19139, Behavioral Sciences Research in HIV Infection; Principal Investigator: Anke A. Ehrhardt, Ph.D.) at the HIV Center for Clinical and Behavioral Studies (P30 MH 43520; Center Director: Anke A. Ehrhardt, Ph.D.). The authors also thank CHAMP staff, CHAMP Collaborative Board and participant families.
Footnotes
Publisher's Disclaimer: Full terms and conditions of use: http://www.informaworld.com/terms-and-conditions-of-access.pdf
This article may be used for research, teaching and private study purposes. Any substantial or systematic reproduction, re-distribution, re-selling, loan or sub-licensing, systematic supply or distribution in any form to anyone is expressly forbidden.
The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The accuracy of any instructions, formulae and drug doses should be independently verified with primary sources. The publisher shall not be liable for any loss, actions, claims, proceedings, demand or costs or damages whatsoever or howsoever caused arising directly or indirectly in connection with or arising out of the use of this material.
REFERENCES
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman RL, Syme SL. Socioeconomic status and health: The challenge of the gradient. American Psychologist. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Biglan A, Matzler CW, Wirt R, Ary D, Noell J, Ochs LL, French C, Hood D. Social and behavioral factors associated with high-risk sexual behavior among adolescents. Journal of Behavioral Medicine. 1990;13:245–261. doi: 10.1007/BF00846833. [DOI] [PubMed] [Google Scholar]
- Black MM, Ricardo IB, Stanton B. Social and psychological factors associated with AIDS risk behaviors among low-income, urban, African American adolescents. Journal of Research on Adolescence. 1997;7(2):173–195. [Google Scholar]
- Bonuck KR, Arno PS, Green J, Fleishman J, Bennet CL, Fahs MC, Maffeo C. Self-perceived unmet needs of persons enrolled in HIV care. Journal of Community Health. 1996;21:183–198. doi: 10.1007/BF01557998. [DOI] [PubMed] [Google Scholar]
- Boyd-Franklin N. Black families. In: Walsh F, editor. Normal family process. New York: Guilford Press; 1993. [Google Scholar]
- Bui CT, Takeuchi DT. Ethnic minority adolescents and the use of community mental health care services. American Journal of Community Psychology. 1992;20:403–417. doi: 10.1007/BF00937752. [DOI] [PubMed] [Google Scholar]
- Carabasi JM, Greene WH, Bernt FM. Primary findings from the survey about AIDS for seventh and eighth graders (SASEG) AIDS Education and Prevention. 1992;4:240–250. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS Surveillance report. Atlanta, GA: Center for Disease Control and Prevention; 2001. [Google Scholar]
- Centers for Disease Control and Prevention. [Retrieved April 17, 2002];AIDS Surveillance report. 2002a 12 from http://www.cdc.gov/hiv/stats/hasr1301.pdf.
- Centers for Disease Control and Prevention. [Retrieved April 17, 2002];HIV/AIDS among US women: Minority and young women at continuing risk. 2002b from http://www.cdc.gov/hiv/pubs/facts/women.htm.
- Centers for Disease Control and Prevention. [Retrieved April 28, 2002];Compendium of HIV prevention interventions with evidence of effectiveness. 2002c from http://www.cdc/hiv/pubs/HIVcompendium/hivcompendium.htm.
- Centers for Disease Control and Prevention. [Retrieved March 01, 2003];African-Americans disproportionately affected by STS. 2003 from http://www.cdc.gov/ncstp/dstd/Press_Releases/AfAmericans.htm.
- Children’s Defense Fund. The state of America’s children. Boston: Beacon Press; 2000. [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. 2nd ed. New Jersey: Lawrence Erlbaum; 1983. [Google Scholar]
- Cohen JB, Derish PA, Dorfman L. AWARE: A community based research & peer intervention program for women. In: Van Vugt JP, editor. AIDS prevention and services: Community based research. Westport, CT: Bergin and Garvin; 1994. pp. 109–127. [Google Scholar]
- Cohen P, Hesselbart CS. Demographic factors in the use of children’s mental health service. American Journal of Public Health. 1993;83:49–52. doi: 10.2105/ajph.83.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. Social support interventions for smoking cessation. In: Gottlieb BH, editor. Marshaling social support: Formats, processes, and effects. Thousand Oaks, CA: Sage; 1988. [Google Scholar]
- DiClemente RJ, Wingood GM. A randomized controlled trial of an HIV sexual risk-reduction intervention for young African-American women. Journal of the American Medical Association. 1995;274:1271–1276. [PubMed] [Google Scholar]
- DiLorenzo T, Hein K. Adolescents: The leading edge of the next wave of the HIV epidemic. In: Wallender JL, Siegel LJ, editors. Adolescent health problems: Behavioral perspectives. New York: Guilford Press; 1993. pp. 117–140. [Google Scholar]
- Dohrenwend BS. The role of adversity and stress in psychopathology: Some evidence and its implication for theory and research. Journal of Health and Social Behavior. 2000;41:1–18. [PubMed] [Google Scholar]
- Dohrenwend BS, Askenasy AR, Krasnoff L, Dohrenwend BP. Exemplification of a method for scaling life events: The PERI Life Events Scale. Journal of Health and Social Behavior. 1978;19:205–229. [PubMed] [Google Scholar]
- Epstein LH, Wing RR. Behavioral treatment of childhood obesity. Psychological Bulletin. 1987;101:331–342. [PubMed] [Google Scholar]
- Escobar-Chaves SL, Tortolero SR, Masse LC, Watson KB, Fulton JE. Recruiting and retaining minority women: Findings from the Women on the Move study. Ethnicity & Disease. 2002;12:242–251. [PubMed] [Google Scholar]
- Gillman G, McKay MM. The CHAMP Impediments Scale. University of Illinois at Chicago; 1996. [Google Scholar]
- Greenberg J, Lifshay J, Van Devanter N, Gonzales V, Celentano D. Preventing HIV infection: The effects of community linkages, time, and money on recruiting and retaining women in intervention groups. Journal of Women’s Health. 1998;7:587–596. doi: 10.1089/jwh.1998.7.587. [DOI] [PubMed] [Google Scholar]
- Guerra NG, Tolan PH. Metropolitan area child study. University of Illinois at Chicago; 1991. [Google Scholar]
- Holtzman D, Rubinson R. Parent and peer communication effects on AIDS-related behavior among U.S. high school students. Family Planning Perspectives. 1995;27:235. [PubMed] [Google Scholar]
- Hutchinson MK, Cooney TM. Patterns of parent-teen sexual risk communication: Implications for intervention. Family Relations. 1998;47:185–194. [Google Scholar]
- Jemmott JB, Jemmott LS. Increasing condom-use intentions among sexually active Black adolescent women. Nursing Research. 1992;41:273–279. [PubMed] [Google Scholar]
- Jessor SL, Jessor R. Transition from virginity to nonvirginity among youth:Asocial-psychological study over time. Development Psychology. 1975;11:473–484. [Google Scholar]
- Kazdin A. Premature termination from treatment among children referred for antisocial behavior. Journal of Clinical Child Psychology. 1993;31:415–425. doi: 10.1111/j.1469-7610.1990.tb01578.x. [DOI] [PubMed] [Google Scholar]
- Kiefe CH, Hyman D. Do public clinics systems provide health care access for the urban poor? A cross-sectional survey. Community Health. 1996;21:61–70. doi: 10.1007/BF01682764. [DOI] [PubMed] [Google Scholar]
- Lacey L, Tukes S, Manfredi C, Warnecke RB. Use of lay health educators for smoking cessation in a hard-to-reach urban community. Journal of Community Health. 1991;16:269–282. doi: 10.1007/BF01320335. [DOI] [PubMed] [Google Scholar]
- Larson EG. Do postcard reminders improve influenza vaccination compliance? Medical Care. 1982;20:639–648. doi: 10.1097/00005650-198206000-00010. [DOI] [PubMed] [Google Scholar]
- Lauby JL, Smith PJ, Stark M, Person B, Adams J. A community-level HIV prevention intervention for inner-city women: Results of the women and infants demonstration projects. American Journal of Public Health. 2000;90:216–222. doi: 10.2105/ajph.90.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madison SM, McKay MM, Paikoff R, Bell CC. Basic research and community collaboration: Necessary ingredients for the development of a family-based HIV prevention program. AIDS Education and Prevention. 2000;12:281–298. [PubMed] [Google Scholar]
- McBride CK, Paikoff RL, Holmbeck GN. Family influences on the initiation of sexual activity among African-American adolescents. Presented at the Role of Families in Preventing and Adapting to HIV/AIDS Conference; Philadelphia, PA. 1999. Jul, [Google Scholar]
- McCormick A, McKay MM, Wilson M, McKinney L, Paikoff R, Bell B, Baptiste D, et al. Involving families in an urban HIV preventive intervention: How community collaboration addresses barriers to participation. AIDS Education and Prevention. 2000;12:299–307. [PubMed] [Google Scholar]
- McKay MM, Coleman D, Paikoff R, Baptiste D, Madison S, Scott R. Preventing HIV risk exposure in urban communities: The CHAMP family program. In: Pequegnat W, Szapocznik J, editors. Working with families in the era of HIV/AIDS. Thousand Oaks, CA: Sage; 2000. pp. 67–87. [Google Scholar]
- Mellins CA, Ehrhardt AA. Families affected by pediatric Acquired Immunodeficiency Syndrome: Sources of stress and coping. Journal of Developmental and Behavioral Pediatrics. 1994;15:54–60. [PubMed] [Google Scholar]
- Montaño DE, Kasprzyk D, Taplin SH. The theory of reasoned action the theory of planned behavior. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education: Theory, research, and practice. 2nd ed. San Francisco, CA: Jossey-Bass; 1997. pp. 85–112. [Google Scholar]
- Moore MR, Chase-Lansdale PL. Sexual intercourse and pregnancy among African American girls in high-poverty neighborhoods: The role of family and perceived community environment. Journal of Marriage and Family. 2001;63:1146–1157. [Google Scholar]
- Muñoz RF, Mrazek PJ, Haggert RJ. Institute of Medicine Report on Prevention of Mental Disorders: Summary and commentary. American Psychologist. 1996;51:1116–1122. doi: 10.1037//0003-066x.51.11.1116. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. Screening, recruiting and predicting retention of participants in a multisite HIV prevention trial. NIMH Multisite HIV Prevention Trial. AIDS. 1997;11 Suppl 2:S13–S19. [PubMed] [Google Scholar]
- Paikoff RL. Early heterosexual debut: Situations of sexual possibility during the transition to adolescence. American Journal of Orthopsychiatry. 1995;65:389–401. doi: 10.1037/h0079652. [DOI] [PubMed] [Google Scholar]
- Paikoff RL. Applying development psychology to an AIDS prevention model for urban African American youth. Journal of Negro Education. 1997;65:44–59. [Google Scholar]
- Paikoff RL, McKay M. The Chicago HIV Prevention adolescent mental health project (CHAMP) family-based intervention. National Institute of Mental Health Office on AIDS and William. T. Grant Foundation; 1995
- Pearlin LI. Stress and mental health: A conceptual overview. Stress and mental health: A conceptual overview. In: Horwitz AV, Scheid TL, editors. A handbook for the study of mental health: Social contexts, theories, and systems. Cambridge, MA: University Press; 1999. pp. 161–175. [Google Scholar]
- Pequegnat W, Szapocznik J. Working with families in the era of HIV/AIDS. Thousand Oaks, CA: Sage publications; 2000. [Google Scholar]
- Person B, Cotton D. A model of community mobilization for the prevention of HIV in women and infants. Prevention of HIV in women and infants demonstration projects. Public Health Reports. 1996;111 Suppl.:89–98. [PMC free article] [PubMed] [Google Scholar]
- Pettaway L, Frank D. Health promoting behaviors of urban African American female heads of household. ABNF Journal. 1999;10:14–19. [PubMed] [Google Scholar]
- Pick S, Palos PA. Impact of the family on the sex lives of adolescents. Adolescence. 1995;30:667–675. [PubMed] [Google Scholar]
- Pinto RM. Unpublished doctoral dissertation. New York: Columbia University School of Social Work; 2003. Factors that influence minority women’s participation in HIV prevention programs: An ecological perspective. [Google Scholar]
- Pinto RM, McKay MM. Do age and gender of social supports matter for low-income African-American women attending an HIV prevention program? Journal of HIV/AIDS & Social Services. 2005;3:5–25. [Google Scholar]
- Pinto RM, McKay MM. Lessons learned from African American women about participation in a family-based HIV prevention program. Families in Society: The Journal of Contemporary Human Services. in press. [Google Scholar]
- Pistella CLY, Bonati FA. Adolescent women’s recommendations for enhanced parent-adolescent communication about sexual behavior. Child and Adolescent Social Work Journal. 1999;16:305–315. [Google Scholar]
- Prochaska JO, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education: Theory, research, and practice. 2nd Ed. San Francisco, CA: Jossey-Bass; 1997. pp. 60–84. [Google Scholar]
- Romer D, Black M, Ricardo I, Feigelman S, Kaljee L, Galbraith J, Nesbit R, Homik R, Stanton B. Social influences on the sexual behavior of youth at risk of HIV exposure. American Journal of Public Health. 1994;84:977–985. doi: 10.2105/ajph.84.6.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas RK, Bartelli D. HIV services for a new generation. Marketing Health Services. 2001;21:24–29. [PubMed] [Google Scholar]
- Tolan PH, McKay MM. Preventing serious antisocial behavior in inner city children: An empirically based family prevention program. Family Relations. 1996;45:148–156. [Google Scholar]
- Tolan P, Miller L, Thomas P. Metropolitan Area Child Study Family Stress Questionnaire. Chicago: University of Illinois at Chicago; 1987. [Google Scholar]
- Wahler RG, Dumas JE. Attentional problems in dysfunctional mother-child interactions: An interbehavioral model. Psychological Bulletin. 1989;105:116–130. doi: 10.1037/0033-2909.105.1.116. [DOI] [PubMed] [Google Scholar]
- Walter HJ, Vaughan RD, Cohall AT. Comparison of three theoretical modules of substance use among urban minority high school students. Journal of the American Academy of Child Psychiatry. 1993;32:975–981. doi: 10.1097/00004583-199309000-00014. [DOI] [PubMed] [Google Scholar]
- Walter HJ, Vaughan RD, Ragin DF, Cohall AT, et al. Prevalence and correlates of AIDS-related behavioral intentions among urban minority high school students. AIDS Education and Prevention. 1994;6:339–350. [PubMed] [Google Scholar]
- Webster-Stratton C. Predictors of treatment outcome in parent training for conduct disordered children. Behavioral Therapy. 1985;16:223–243. [Google Scholar]
- Wingood GM, DiClemente RJ. The WILLOW program: Mobilizing social networks of women living with HIV to enhance coping and reduce sexual risk behaviors. In: Pequegnat W, Szapocznik J, editors. Working with families in the era of HIV/AIDS. Thousand Oaks, CA: Sage; 2000. pp. 281–298. [Google Scholar]
- Wortley PM, Fleming PL. AIDS in women in the United States. Journal of American Medical Association. 1997;278:911–916. [PubMed] [Google Scholar]