Abstract
Background
Understanding the role of different classes of T cells during HIV infection is critical to determining which responses correlate with protective immunity. To date, it is unclear whether alterations in regulatory T cell (Treg) function are contributory to progression of HIV infection.
Methodology
FOXP3 expression was measured by both qRT-PCR and by flow cytometry in HIV-infected individuals and uninfected controls together with expression of CD25, GITR and CTLA-4. Cultured peripheral blood mononuclear cells were stimulated with anti-CD3 and cell proliferation was assessed by CFSE dilution.
Principal Findings
HIV infected individuals had significantly higher frequencies of CD4+FOXP3+ T cells (median of 8.11%; range 1.33%–26.27%) than healthy controls (median 3.72%; range 1.3–7.5%; P = 0.002), despite having lower absolute counts of CD4+FOXP3+ T cells. There was a significant positive correlation between the frequency of CD4+FOXP3+ T cells and viral load (rho = 0.593 P = 0.003) and a significant negative correlation with CD4 count (rho = −0.423 P = 0.044). 48% of our patients had CD4 counts below 200 cells/µl and these patients showed a marked elevation of FOXP3 percentage (median 10% range 4.07%–26.27%). Assessing the mechanism of increased FOXP3 frequency, we found that the high FOXP3 levels noted in HIV infected individuals dropped rapidly in unstimulated culture conditions but could be restimulated by T cell receptor stimulation. This suggests that the high FOXP3 expression in HIV infected patients is likely due to FOXP3 upregulation by individual CD4+ T cells following antigenic or other stimulation.
Conclusions/Significance
FOXP3 expression in the CD4+ T cell population is a marker of severity of HIV infection and a potential prognostic marker of disease progression.
Introduction
Many aspects of HIV pathogenesis are still poorly understood. Despite the CD4 T cell depletion and resulting immunosuppression which are hallmarks of the disease, HIV infected individuals display increased levels of immune activation as evidenced by elevated expression of markers of cell activation such as HLA-DR, CD38 and CD69 [1], [2]. The contributory role of preservation or destruction of regulatory T cells (Tregs), either in number or function, has not been established.
Naturally occurring Tregs are a subset of CD4+ T cells expressing the forkhead-winged-helix transcription factor, Forkhead box 3 or FOXP3 [3]. They are responsible for immunoregulation predominantly through cell-cell contact mediated suppression. It is plausible that preferential destruction or inactivation of Tregs by HIV could lead to excessive immune activation [4], [5]. Treg-mediated suppression of HIV specific responses in vitro has been shown to be more effective with cells isolated from relatively healthy HIV infected patients compared with later stage AIDS patients, suggesting that Tregs (total or HIV-specific) were depleted or dysfunctional later in HIV disease [6].
On the other hand, preferential preservation of Tregs over other subsets of T cells could lead to suppression of immune responses to viral infections, leading to a high viral load [7], [8]. Various authors have described increased Tregs as a proportion of CD4+ T cells in HIV positive patients, particularly in those with low CD4+ T cell counts (CD4 counts) [9], [10], [11]. In peripheral blood, Treg levels have been reported to remain elevated years after successful highly active antiretroviral therapy [9], [12], [13]. Certain authors [14] have suggested that with progression from HIV to AIDS the number of circulating CD4+CD25hi Treg as a proportion of CD4 T cells increases but their function (which was measured by FOXP3 mRNA expression) decreases.
Generation of T cells expressing FOXP3 or with suppressor activity has been reported to occur through incomplete activation of CD4+ T cells by immature, plasmacytoid or alternatively-activated dendritic cells [15], [16], [17], [18], [19], [20], [21] in HIV-infected individuals as well as in response to Vitamin D [22], all trans retinoic acid [23], [24], [25], [26] or indoleamine deoxygenase (IDO) modulation in antigen presenting cells [20], [27], [28], [29], [30], [31], [32]. One or more of these mechanisms may by responsible for alteration of FOXP3 expression in HIV infected individuals. The end result may be a disproportionate increase in cells with a suppressive or tolerant rather than a proinflammatory phenotype, resulting in an inability of the host to combat pathogens.
There are a number of reasons why different studies may have had contrasting findings. Principally, there is still no validated marker with which to identify human Tregs. The best available to date is forkhead box transcription factor P3, written “Foxp3” in animals and “FOXP3” in humans. FOXP3 is a key control element in the development and function of CD4+ T cells with suppressor function [33], [34], [35], [36].
Use of other markers to identify Tregs have varied from study to study and include CD25, Cytotoxic T lymphocyte associated protein 4 (CTLA-4 or CD152), glucocorticoid-induced tumour necrosis factor receptor (GITR), CD27, OX40 ([37], CD44 [38], CD62L [39], [40], CD39 [41] and decreased expression of CD127 [42], [43], [44]. Tregs are generally thought to be of memory phenotype expressing CD45RO [8], [45], [46], although there have been reports of naïve CD45RA Tregs [47], [48], [49]. None of these markers are exclusive to the Treg population and many are also expressed by activated CD4+ T cells.
While Tregs are easily defined in mice by concurrent expression of FOXP3 and high levels of CD25, in humans CD25 cannot be clearly delineated into low and hi expressing subsets due to a continuum of expression. In addition, CD25 expression does not always correlate with FOXP3 expression in humans, particularly in HIV infected individuals [31]. FOXP3 expression can be triggered in FOXP3− CD4+ T cells during activation or division which may correlate with, perhaps transient, suppressive potential [50], [51], [52], [53], [54], [55]. There is also however conflicting evidence suggesting that FOXP3 expression in humans may not be confined to cells with regulatory function [44], [56], [57], [58], [59].
We analysed FOXP3 expression, as well as other Treg markers, in South African patients with and without HIV infection. We found a significantly elevated percentage of FOXP3 expressing CD4+ T cells in HIV infected patients, particularly in those with lower CD4 counts. We explored the mechanism of FOXP3 upregulation by assessing the ability of cultured cells from HIV positive and negative patients to maintain FOXP3 expression in unstimulated conditions and following T cell receptor stimulation. While many previous studies have isolated CD4+CD25hi cells and mixed them with responder cells in a predetermined ratio such as 1∶1 or 1∶10, we avoided this approach as it does not reflect the situation in vivo at a physiological ratio of Tregs to responder cells. Additionally the isolation of Tregs by CD25hi sorting potentially leaves FOXP3-expressing Tregs behind in the responder population. We sought to investigate FOXP3 expression after T cell receptor stimulation while maintaining a physiological ratio of Tregs to responder cells. FOXP3 expression dropped rapidly in unstimulated cell culture but was restored by T cell receptor stimulation. This suggests that the high FOXP3 expression in HIV infected patients is likely due to FOXP3 upregulation by individual CD4+ T cells following antigenic or other stimulation.
Materials and Methods
Clinical Samples
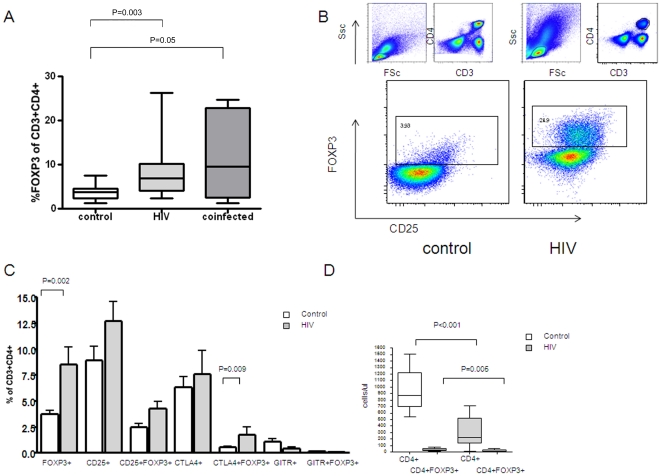
In this cross-sectional study, twenty-seven HIV infected patients were recruited from the antiretroviral clinics of the Charlotte Maxeke Johannesburg Academic hospital and health care centres in Alexandra township, Johannesburg. Ten of the patients had active Tuberculosis as diagnosed on the basis of symptoms and sputum microscopy. As the HIV-infected patients with and without active Tuberculosis did not differ from each other with regards to CD4 count or FOXP3 expression (Figure 1A), they were grouped together for further analysis. Patients had access to the national antiretroviral programme but had not yet commenced antiretroviral therapy or received more than four days of TB treatment at study enrolment.
Figure 1. FOXP3 expression at baseline in HIV infected patients.
Panel A: Subgroup analysis of the HIV and HIV/TB coinfected groups showed no difference in FOXP3 expression as a percentage of CD3+CD4+ T lymphocytes between the HIV and HIV/TB co-infected groups. Panel B: Representative plots of baseline FOXP3 expression in CD3+CD4+ lymphocytes plotted against CD25 for a control and an HIV positive sample. Panel C: Expression of FOXP3, CD25, CTLA-4 and GITR as a percentage of the CD3+CD4+ population. Panel D: Absolute numbers of total and FOXP3 expressing CD4+ T cells at baseline.
Twenty-two healthy controls were recruited from amongst health-care workers of the institutions named above as well as blood donors from the South African National Blood Transfusion Service. Controls and HIV infected subjects were similar with respect to gender and age. All subjects gave written informed consent for the study and ethics approval was granted by the University of the Witwatersrand Human Medical Ethics Committee (R14/49). The day of sample collection was regarded as Day 0.
HIV tests and haematological parameters
The HIV status of participants was confirmed using HIV rapid testing (Determine HIV-1/2, Abbott Laboratories, Abbot Park, Il 60064,USA). CD4 counting was performed using the PanLeucogating method [60]. Viral loads were performed using the COBAS Ampliprep/COBAS Taqman HIV-1 Test (Roche Diagnostics Division, Basel, Switzerland).
Isolation of Peripheral Blood Mononuclear cells
Peripheral blood mononuclear cells (PBMCs) were isolated within 3–5 hours of sample collection using Ficoll Hypaque in LeucoSep tubes. Cells were washed twice in Hanks Buffered Salt Solution with 0.1% gentamycin and counted using a capillary cytometer (Guava technologies, Hayward, CA). Cells (2×106 cells/ml) were then rested overnight at 37°C in a 5% CO2 atmosphere in RPMI 1640 medium with GlutaMAX and 25mM HEPES (Gibco, Scotland) supplemented with 20% fetal bovine serum (Gemini Bio-Products, USA) and 0.1% gentamycin (R20).
mRNA extraction and qRT-PCR
mRNA was extracted from one million PBMCs per sample using QIAamp RNA mini kit (QIAGEN, Germany). The mRNA was immediately converted to cDNA using the Applied Biosystems High-Capacity cDNA Archive Kit (Applied Biosystems, Foster City, CA) and the GeneAmp PCR System 9700 (Applied Biosystems, Foster City, CA). cDNA was frozen at −20°C until needed. Multiplexed real-time reverse transcriptase PCR was then performed using TaqMan Universal PCR Master Mix (Applied Biosystems, Foster City, CA.) on the 7500 Real Time PCR System (Applied Biosystems, Foster City, CA). FOXP3 expression was assessed using a fluorescently labelled probe (TaqMan Gene expression assays, probe Hs00203958_m1, Applied Biosystems, Foster City, CA) relative to expression of gapdh (Pre-Developed TaqMan Assay Reagents Control Kit, Applied Biosystems Foster City, CA). All PCR reactions were run in triplicate in the presence of a blank control tube.
Cell stimulations
PBMC were rested overnight in R20 medium at 2×106 cells/ml with analysis of unstimulated samples on day 1. For assessment of cell proliferation, an equal volume of 10µM CFSE (Molecular Probes, Netherlands) was added to the unstimulated PBMC suspension. Samples were vortexed and incubated at room temperature in the dark for 7 minutes. To quench the CFSE reaction, a double volume of ice cold FBS was added. Samples were again vortexed and incubated at room temperature in the dark for 1 minute. PBMC were washed twice with warm RPMI 1640 medium with GlutaMAX and 25mM HEPES (Gibco, Scotland) supplemented with 10% human serum AB (Gemini Bio-Products, USA) and 0.1% gentamycin (R10) to remove excess CFSE. 2×106 CFSE stained cells were seeded in a 24-well culture plate (Nunc, Denmark) in R10 medium to a final volume of 2ml. Stimulated samples were treated with 0.1 ug/ml stimulatory anti-CD3 mAb (12F6). Unstimulated samples were used as negative controls. Plates were incubated at 37°C, 5% CO2 for 4 days.
Intracellular cytokine staining
Harvested PBMC (both those rested overnight and those cultured for 4 days) were stained for intracellular FOXP3 and CTLA-4 expression and surface expression of CD25, GITR, CD3 and CD4 using the FOXP3 staining set (eBiosciences, UK) according to manufacturer's instructions. Mean FOXP3% is reported from triplicate measurements. Preliminary experiments with propidium iodide showed efficacy of cell permeabilisation to be above 98%.
Antibody-fluorochrome conjugates used included CD3 APC, CD3 PerCP, CD4 FITC, CD4 PerCP, CD8 FITC,CD25 APC (BD Biosciences, San Jose, CA), GITR APC, CTLA-4 FITC (R&D Systems, Minneapolis, USA) and FOXP3 PE (clone PCH101, eBiosciences, UK).
Flow cytometry
Flow cytometry was performed using FACSCalibur (BD Biosciences) and LSRII (BD Biosciences) flow cytometers with acquisition enabled by CellQuest Pro or FACSDiva software (BD Biosciences) respectively. Colour compensation was achieved using an appropriate single fluorochrome-labelled sample. Data was analysed using FlowJo 6.4.2 (TreeStar, USA). For CD25 quantitation, expression of CD25 on CD4− T cells was used as a reproducible reference point.
50 000 to 1 million events were collected per sample. There was no use of biexponential axes. Not all samples were available for analysis of all parameters, depending on CD4 count and numbers of PBMCs available for culture.
Statistical Analysis
Statistical analyses were performed using SPSS version 15 and GraphPad Prism version 4.0. Groups were compared by Mann Whitney analysis and correlations performed using the Spearman correlation coefficient. Significance was chosen at the 5% level. Group medians are reported.
Results
CD4 counts of HIV-infected subjects
HIV infected subjects had CD4 counts ranging from 0 to 712 cells/ul (median CD4 count 216 cells/ul) with 48% of patients <200 cells/ul group, 19% 200–350 cells/ul and 33% >350 cells/ul.
HIV infected subjects display higher percentages of CD4+ T cells that express FOXP3 despite lower absolute numbers
FOXP3 expression in CD4+ T cells has been reported to confer a regulatory phenotype and may be dysregulated in HIV infection. To explore whether FOXP3 expression by CD4+ T cells differs in HIV infected individuals compared with controls, we isolated PBMCs and performed intracellular cytokine staining after overnight rest. In the control group, 3.72% of CD3+CD4+ T cells were positive for FOXP3 (range from 1.3–7.5%), in keeping with that described in the literature [10], [56]. The HIV infected group showed significantly elevated FOXP3 expression when expressed as a percentage of total CD3+CD4+ cells (median of 8.11%, range 1.33–26.27%, P = 0.002, Figure 1B,C). Absolute numbers of FOXP3+ CD4+ T cells were lower in HIV positive patients than controls (12.6 cells/µl versus 30.47 cells/µl, P = 0.005, Figure 1C) because of the lower CD4+ T cell count. Similarly, there was lower FOXP3 mRNA levels in HIV positive patients versus controls (0.92 vs 1.35, P = 0.03, data not shown).
FOXP3 expression in CD8+T cells, while found at a much lower proportion than CD4+ T cells, has also been reported [9], [52], [56], [57], [61], [62], [63], [64] and may confer regulatory functions. It is unknown if there is an alteration in CD8+ T cell FOXP3 expression during HIV infection. We found FOXP3 expression at low levels in the CD8+ T cell population but no significant difference between the control and HIV infected groups (0.20% of CD3+CD4− versus 0.39% respectively). FOXP3 expression on the CD3+CD4− population could be upregulated by antiCD3 stimulation (data not shown). There was however no significant difference in stimulated FOXP3 expression of CD4+ T cells or CD8+ (CD3+CD4−) T cells between the HIV and control groups.
FOXP3 expression does not correlate with the activation marker CD25
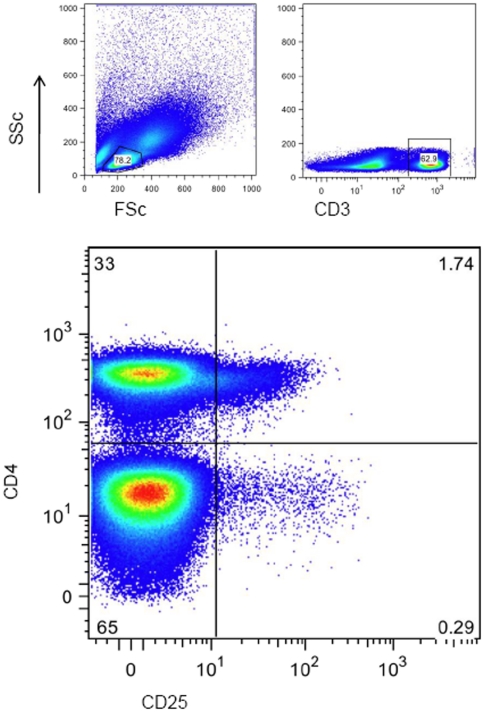
CD25 is often used as a marker of regulatory T cells but can also act as an activation marker. CD25 expression in humans appears as a continuum of expression rather than a discrete positive and negative population, therefore to ensure reproducible gating, CD25 was gated by selecting the total CD3+ population and plotting CD25 against CD4. FOXP3 expression on the CD4− population was used to set the positive gate. The resulting percentage obtained was used to calculate the CD25 expression as a percentage of the total CD3+CD4+ population (Figure 2).
Figure 2. Representative plot illustrating CD25 gating strategy.
Lymphocytes were gated according to forward and side scatter. CD3 positive lymphocytes were selected. CD25 expression on the x-axis was plotted against CD4 on the y-axis. A gate was set according to CD25 expression on the CD4− population. This gave a percentage of CD3+CD4+CD25+ lymphocytes as a percentage of CD3+ (figure in top-right quadrant). This percentage was then used to calculate the percentage of CD3+CD4+CD25+ lymphocytes as a percentage of the CD3+CD4+ population (CD4 population being top-left and right quadrants added together).
CD25 expression gated in this manner did not differ significantly between the HIV infected and control group. While FOXP3+T helper cells were visually CD25high as expected, FOXP3% showed no significant correlation with CD25 expression in either the control or HIV infected group. CD25 expression did not show a statistical correlation with either viral load or CD4 count.
Examining other postulated markers of regulatory T cells, CTLA4+FOXP3+ coexpression (as a percentage of CD3+CD4+ cells) was higher in the HIV group than the controls (0.78% versus 0.39%, P = 0.009, Figure 2A). There was no significant difference between the two groups in CD25+, CTLA-4+, GITR+ or GITR+FOXP3+ coexpression.
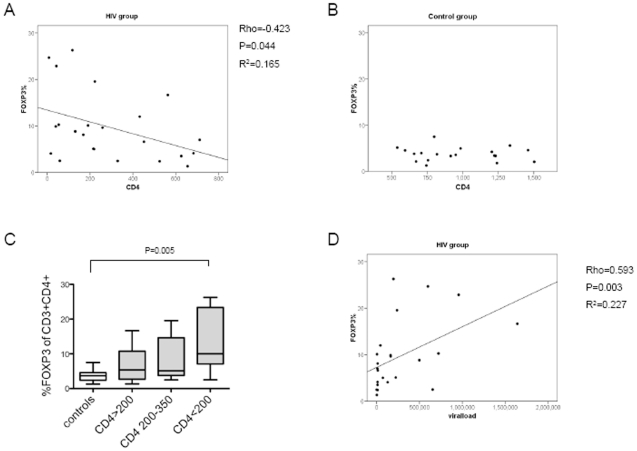
CD4+ T cell FOXP3 expression is negatively correlated with CD4+ T cell count and positively correlated with viral load
As FOXP3 expression may be affected by the degree of immunodeficiency, we analysed the relationship between the CD4+T cell count and the percentage of CD4+T cells expressing FOXP3. There was a negative correlation demonstrable between CD4 count and FOXP3 percentage in the HIV infected group (rho = −0.423 P = 0.044, Figure 3A) but no significant correlation in the control group (Figure 3B). Stratification based on CD4 count revealed that it was only the samples with CD4 count <200 cells/µl that showed a marked elevation in FOXP3 percentage (median 10%), while there was no elevation in FOXP3 percentage in samples with higher CD4 counts (5.09% in samples with CD4 counts of 200–350 cells/µl and 5.36% in samples >350 cells/µ) (Figure 3C).
Figure 3. Correlation of FOXP3 with CD4 count and viral load.
Panel A: CD4 count was negatively correlated with day 1 FOXP3 percentage in the HIV infected group. Panel B: The control group showed no correlation between CD4 count and FOXP3 percentage. Panel C: FOXP3 percentage stratified by CD4 count. Panel D: FOXP3 percentage was positively correlated with viral load.
As anticipated, there was a significant negative correlation between viral load and CD4 count (rho = −0.538 P = 0.005, data not shown). We further determined that FOXP3 percentage correlated positively with viral load (rho = 0.593 P = 0.003, Figure 3D).
High FOXP3 frequencies in HIV infected individuals are not due to increased FOXP3+ T cell lifespan nor increased T cell proliferation
In order to assess the mechanism by which the FOXP3 frequency of total CD4 T cells is elevated in HIV infected patients, we analysed FOXP3 expression in four-day cultures with and without stimulation through the T cell receptor with anti-CD3.
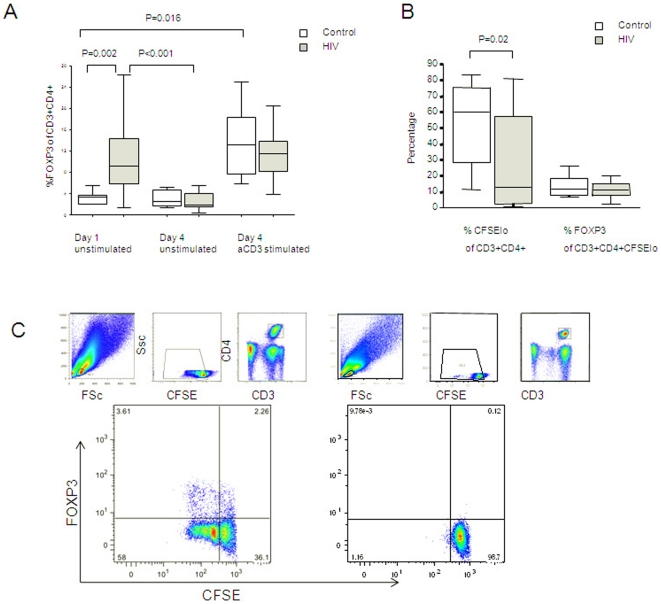
Unexpectedly, unstimulated FOXP3 expression, expressed as a percentage of CD3+CD4+ cells, was significantly lower on day 4 than on day 1 in the HIV infected group (1.95% versus 9.75%, P<0.001) whilst there was no significant drop in expression in the control group (2.56% versus 3.36%) (Figure 4A). This suggests that FOXP3+ cells were not maintaining high levels due to a longer lifespan than FOXP3− cells. After stimulation with anti-CD3, however, day 4 FOXP3 expression in the HIV infected group was comparable with baseline and with day 4 control group levels(Figure 4A), suggesting that mechanisms of FOXP3 upregulation after T cell receptor triggering are intact in HIV infected individuals.
Figure 4. FOXP3 expression after T cell receptor stimulation.
Panel A: FOXP3 expression as a percentage of T lymphocytes at baseline and after 4 days of cell culture, with and without T cell receptor stimulation with anti-CD3. Panel B: Proliferation of total CD4+ T cells and FOXP3+ expression in proliferated CD4+ T cells following T cell receptor stimulation with aCD3. Panel C: Representative plot of FOXP3+ expression in proliferated T cells (left-hand plot) following anti-CD3 stimulation compared with an unstimulated sample(right-hand plot). The small plots above show ancestry – lymphocytes were gated; followed by exclusion of events with high CFSE; followed by selection of CD3+CD4+ T cells. Proliferation is demonstrated by halving of CFSE fluorescence in cells that have divided (large plots below). In the anti-CD3 stimulated sample, FOXP3 expression is noted in cells which have proliferated (top-left quadrant) as well as those that have not proliferated (top-right quadrant).
To assess whether FOXP3 upregulation was due to increased CD4+T cell proliferation or increased expression in proliferated CD4+ T cells, we assessed FOXP3 expression following anti-CD3 stimulation of CFSE stained cells. Total CD4+ T cells proliferated less in the HIV infected group than in the control group (13.09% of CD3+CD4+ cells versus 60.08%, P = 0.02, Fig 4B). FOXP3 was upregulated in daughter cells (Figure 4C) but the percentage of proliferating cells expressing FOXP3 did not differ in the HIV infected and control groups (11.31% versus 11.78% Figure 4B).
Together, these findings suggest that high FOXP3 percentages in HIV infected patients is not due to longer lifespan, increased cell proliferation nor increased expression in proliferated cells. We conclude that the increased FOXP3 frequencies in HIV infected patients is likely due to upregulation of FOXP3 expression by individual CD4+ T cells, possibly following antigenic or other stimulation.
Discussion
We used intracellular cytokine staining to analyse FOXP3 expression and other postulated markers of regulatory T cells (CD25, CTLA4 and GITR) in HIV infected individuals. We found that HIV infected individuals showed a significantly higher percentage of CD4+ T cells that expressed FOXP3 compared with control individuals. The percentage of FOXP3 expressing CD4+ T cells correlated negatively with CD4 count and positively with viral load. Due to their lower absolute CD4 count, the absolute number of FOXP3 expressing cells, as well as FOXP3 mRNA expression, was found to be lower in HIV infected individuals than in controls.
The finding of higher FOXP3 levels in patients with lower CD4 counts and higher viral loads is in keeping with the findings of others [11], [37], [65]. The inverse relationship between CD4 count and FOXP3 expression has not been consistently described and is well illustrated in our sample group possibly due to the inclusion of HIV infected patients with very low CD4 counts.This relationship also explains why studies with patients with relatively high CD4 counts at enrolment may have failed to demonstrate elevations of FOXP3 expression in peripheral blood. If the data is stratified into patients according to CD4 count, it is only the patients with CD4 counts below 200 cells/µl who show a marked elevation in FOXP3 percentage of CD3+CD4+ T cells (median 10%) while there is no significant difference in FOXP3 percentage between the 200–350 cells/µl or >350 cells/µl group and the control group (Figure 3C).
We noted that FOXP3 positivity was not limited to the CD4+ T cell subset but was also observed on other CD4− T cells, albeit at much lower levels. Interestingly, FOXP3 upregulation after anti-CD3 stimulation, was noted on CD4− T cells as well as on CD4+ T cells (data not shown). FOXP3 expression in CD8+ T cells has been described [9], [52], [56], [57], [61], [62], [63], [64], as have other subsets of FOXP3− CD8+ cells with suppressor function [64], [66], [67], [68], [69]. In contrast to the CD4+FOXP3+ subset, we saw no significant difference in unstimulated or anti-CD3 stimulated percentages of CD4−FOXP3+ cells between the control and HIV infected groups.
HIV infected individuals are known to exhibit high levels of T cell activation and debate reigns as to whether FOXP3 is expressed by activated T cells that do not possess suppressive functions [52], [56], [58]. In this study, stimulated FOXP3 expression did correlate with in vitro proliferation of both CD4+ and CD8+ T cells to anti-CD3 stimulation but there was no correlation between expression of FOXP3 and the activation marker CD25. The correlation of FOXP3 with cell proliferation may suggest that FOXP3 acts as a marker of cell activation, however its discordance with CD25 expression indicates otherwise. The lack of statistical correlation between FOXP3 and CD25 expression, gated in a reproducible manner, lends weight to the argument that the elevated FOXP3 levels are not merely a marker of activated cells in HIV infection, in keeping with findings [70] describing dissociation between FOXP3 mRNA and CD25 expression in a SIV model. We took great care to gate CD25 using a reproducible gating strategy, namely using CD25 expression on CD4− T cells as the cutoff for CD25 positivity. This proved a more reliable strategy than setting an arbitrary threshold for CD25+ and CD25++. Future studies should, however, include reference beads to allow more accurate CD25 determination. In previous studies, FOXP3 has also been shown not to correlate with the activation markers CD69 [31] or CD38 [9] although there was a correlation with HLA-DR expression in CD4+ T cells in the latter study.
CTLA-4 and GITR did not coincide with FOXP3 expression ie cells did not co-express FOXP3 with CTLA4 or GITR (Figure 1c). This is in keeping with findings by Weiss et al. [8] of intracellular CTLA-4 positivity in only 30% of Tregs (identified by CD4+CD25hi expression) and Lim et al. [9] who found CTLA-4 or GITR expression in less than 10% of Tregs (CD4+CD25+CD127lo). A limitation of this study is that CD127 had not been included, which may have given additional discriminatory power of the Treg subset from activated cells. We therefore limited our functional analysis to FOXP3 expression.
The finding of increased percentages of CD4+ T cells expressing FOXP3 in HIV infected individuals suggests that an imbalance of regulatory to effector T cells could be responsible for susceptibility to opportunistic infection. Higher FOXP3 expression could be the result of one of four mechanisms: upregulated expression of FOXP3 in individual CD4+ T cells compared with HIV negative individuals, increased proliferation of cells expressing FOXP3+ cells, increased lifespan of FOXP3+ cells or increased cell death of FOXP3− CD4+ T cells.
To analyse the mechanism of increased expression of FOXP3 amongst CD4+ T cells from HIV infected individuals, we cultured PBMCs from HIV infected and uninfected individuals in the presence of a stimulating antibody against the T cell receptor (anti-CD3). We found FOXP3 to be markedly upregulated by antigenic stimulation with anti-CD3 stimulation.
We did not directly address the lifespan or susceptibility to cell death of FOXP3 expressing cells in this study, however we noted that during unstimulated culture conditions, the elevated FOXP3 levels in the HIV infected groups declined rapidly to control levels. This is in keeping with a previous study suggesting that Tregs (CD3+CD25hi) are highly susceptible to apoptosis in vitro due to low levels of the antiapoptotic molecule Bcl-2 [54] and suggests that they do not have a longer lifespan than FOXP3− cells.
In addition, FOXP3 expression in the HIV infected group could be rescued by anti-CD3 to levels comparable with and the stimulated control group. We explored whether this was due to increased CD4+ T cell proliferation or increased FOXP3 expression in cells which had proliferated. Using dual labelling with CFSE and FOXP3 we found that total CD4+ T cell proliferation was lower in the HIV group than in the control group, and the percentage of proliferated cells that expressed FOXP3 was similar in both groups. Thus the mechanism by which FOXP3 expression was upregulated in vitro in response to anti-CD3 stimulation is not likely to be due to CD4+ T cell proliferation. Together, these findings suggest that elevated FOXP3 percentages in HIV infected individuals is due to upregulation of FOXP3 expression in individual CD4+ T cells in HIV, likely due to antigenic or other stimulation. The downstream effect of FOXP3 upregulation was not directly addressed in this study. Transient FOXP3 upregulation after T cell receptor engagement may indicate that FOXP3 is an activation marker, however does not exclude the possible acquisition of suppressive potential after activation.
The debate over FOXP3 as activation marker versus marker of suppressive activity may eventually prove both sides right. The mechanisms of activation-induced cell death in healthy individuals is poorly understood, but every activated cell must eventually die or be suppressed, otherwise result in leukaemia. FOXP3 may indeed be both an “activation marker” and a marker of cells that have become unable to carryout effector functions.We have shown that FOXP3 expression was transient and could be lost and restimulated in HIV infected patients. Thus there did not seem to be an increase in number of natural Tregs with lineage-dependent FOXP3 expression in these patients, rather an increase in FOXP3 expression induced peripherally. This may be a result of cell activation, but the question remains as to why the increased numbers of activated T cells in HIV infected individuals fail to clear pathogens and are ineffectual in their actions. While not directly addressed by this study, it is plausible that continuous stimulation through the T cell receptor in HIV infected individuals may induce chronic rather than transient FOXP3 upregulation, resulting in dysfunctional effector T cells. A difference in function between FOXP3 and other activation markers may be an explanation for the discordance found in this study between FOXP3 expression and expression of the activation marker CD25.
It is recognised that CD4 count is not a perfect prognostic tool for monitoring of HIV infected individuals, with some patients appearing well even at low CD4 counts and some patients doing poorly even with relatively high counts (in our study one patient with a CD4 count of 2 appeared healthy). We suggest that FOXP3 expression in the CD4+ T cell subset may prove a more accurate prognostic tool to monitor disease progression and response to antiretroviral therapy. Longitudinal studies should be conducted to assess the use of FOXP3 frequency as a prognostic monitoring tool.
The inclusion in our HIV patient cohort of some HIV infected individuals with active Tuberculosis can be criticised, as there is evidence suggesting changes in Treg number or function result from Tuberculosis alone [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83] although these studies remain inconclusive. Roberts et al. [84] found no difference in the levels of CD4+CD25+ Tregs in active tuberculosis cases compared with latently infected controls in unstimulated peripheral blood mononuclear cell cultures. Many of these studies, as with studies of Tregs in HIV infection, have assessed FOXP3 mRNA expression rather than FOXP3 protein expression at the single cell level. Further, most quantitated Tregs based on CD25 expression without the use of a reference marker by which to set the CD25 gate. We conducted a subgroup analysis which showed no significant difference in levels of FOXP3 expression in HIV infected individuals with and without Tuberculosis (Figure 1A). Additionally, it can be hypothesized that any defect in Treg number or function may be of a similar nature in both HIV and Tuberculosis, given their propensity to occur simultaneously. Thus the co-infected group may illustrate more extreme changes not demonstrable in a small group of HIV infected patients alone.
In conclusion, we have shown that HIV infected individuals had significantly higher percentages of CD4+ T cells positive for FOXP3 than HIV uninfected individuals and that this is likely due to upregulation of FOXP3 expression by CD4+ T cells. FOXP3 expression as a percentage of CD4+ T cells correlated positively with viral load and negatively with CD4 count, with a marked elevation in FOXP3 percentage in patients with CD4 counts below 200 cells/µl. While correlation does not imply causation, this data support the hypothesis that FOXP3 plays a functional role in disease progression and may suppress responses to pathogens. The basis of the increased FOXP3 expression appears to be upregulation of FOXP3 expression by individual CD4+ T cells following T cell receptor stimulation. FOXP3 expression as a percentage of the CD4+ T cell population is a potential prognostic marker of disease progression.
Acknowledgments
We acknowledge the assistance of Greg Khoury, Stephina Nyoka, Phineas Mohube, Pauline Mokgotho, Sibongile Xaba, Netty Malatsi and Mandla Mlotshwa of the NICD HIV Immunology, Dr Guido Ferrari and Dr David Murdoch of Duke University, Dr Clement Penny and Prof Debbie Glencross of Wits University and George Makedonas of University of Pennsylvania. Volunteer recruitment was made possible by Prof Francois Venter, Prof Jeff Wing, Dr Dennis Rubel, Dr Shanil Naidoo, the staff of the Helen Joseph and New Johannesburg Hospital antiretroviral clinics, Alexandra 8th Ave and East Bank clinics and the South African National Blood Transfusion Service.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: Financial assistance was provided by Sarum St Michael Educational Charity, England (registered charity number 309456, ssmsarum@waitrose.com, no Web site), the University of Bath Alumni Fund, England (www.alumni.bath.ac.uk), Calne Rotary Club (www.calne.org.uk/community/groups/rotaryclub), the South African AIDS Vaccine Initiative (SAAVI), the Wellcome Trust (http://www.wellcome.ac.uk/Funding/index.htm), the National Institutes of Health and the Elizabeth Glazer Paediatric AIDS Foundation International Leadership Award. CTT is a Wellcome Trust International Senior Research Fellow (076352/Z/05/Z). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
References
- 1.Savarino A, Bottarel F, Malavasi F, Dianzani U. Role of CD38 in HIV-1 infection: an epiphenomenon of T-cell activation or an active player in virus/host interactions? AIDS. 2000;14:1079–1089. doi: 10.1097/00002030-200006160-00004. [DOI] [PubMed] [Google Scholar]
- 2.Sousa AE, Carneiro J, Meier-Schellersheim M, Grossman Z, Victorino RM. CD4 T cell depletion is linked directly to immune activation in the pathogenesis of HIV-1 and HIV-2 but only indirectly to the viral load. J Immunol. 2002;169:3400–3406. doi: 10.4049/jimmunol.169.6.3400. [DOI] [PubMed] [Google Scholar]
- 3.Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M. Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol. 1995;155:1151–1164. [PubMed] [Google Scholar]
- 4.Oswald-Richter K, Grill SM, Shariat N, Leelawong M, Sundrud MS, et al. HIV infection of naturally occurring and genetically reprogrammed human regulatory T-cells. PLoS Biol. 2004;2:E198. doi: 10.1371/journal.pbio.0020198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Apoil PA, Puissant B, Roubinet F, Abbal M, Massip P, et al. FOXP3 mRNA levels are decreased in peripheral blood CD4+ lymphocytes from HIV-positive patients. J Acquir Immune Defic Syndr. 2005;39:381–385. doi: 10.1097/01.qai.0000169662.30783.2d. [DOI] [PubMed] [Google Scholar]
- 6.Kinter AL, Hennessey M, Bell A, Kern S, Lin Y, et al. CD25(+)CD4(+) regulatory T cells from the peripheral blood of asymptomatic HIV-infected individuals regulate CD4(+) and CD8(+) HIV-specific T cell immune responses in vitro and are associated with favorable clinical markers of disease status. J Exp Med. 2004;200:331–343. doi: 10.1084/jem.20032069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aandahl EM, Michaelsson J, Moretto WJ, Hecht FM, Nixon DF. Human CD4+ CD25+ regulatory T cells control T-cell responses to human immunodeficiency virus and cytomegalovirus antigens. J Virol. 2004;78:2454–2459. doi: 10.1128/JVI.78.5.2454-2459.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weiss L, Donkova-Petrini V, Caccavelli L, Balbo M, Carbonneil C, et al. Human immunodeficiency virus-driven expansion of CD4+CD25+ regulatory T cells, which suppress HIV-specific CD4 T-cell responses in HIV-infected patients. Blood. 2004;104:3249–3256. doi: 10.1182/blood-2004-01-0365. [DOI] [PubMed] [Google Scholar]
- 9.Lim A, Tan D, Price P, Kamarulzaman A, Tan HY, et al. Proportions of circulating T cells with a regulatory cell phenotype increase with HIV-associated immune activation and remain high on antiretroviral therapy. AIDS. 2007;21:1525–1534. doi: 10.1097/QAD.0b013e32825eab8b. [DOI] [PubMed] [Google Scholar]
- 10.Montes M, Lewis DE, Sanchez C, de Castilla DL, Graviss EA, et al. Foxp3+ regulatory T cells in antiretroviral-naive HIV patients. AIDS. 2006;20:1669–1671. doi: 10.1097/01.aids.0000238415.98194.38. [DOI] [PubMed] [Google Scholar]
- 11.Rallon NI, Lopez M, Soriano V, Garcia-Samaniego J, Romero M, et al. Level, phenotype and activation status of CD4+FoxP3+ regulatory T cells in patients chronically infected with human immunodeficiency virus and/or hepatitis C virus. Clin Exp Immunol. 2009;155:35–43. doi: 10.1111/j.1365-2249.2008.03797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaardbo JC, Nielsen SD, Vedel SJ, Ersboll AK, Harritshoj L, et al. Regulatory T cells in human immunodeficiency virus-infected patients are elevated and independent of immunological and virological status, as well as initiation of highly active anti-retroviral therapy. Clin Exp Immunol. 2008;154:80–86. doi: 10.1111/j.1365-2249.2008.03725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kolte L, Gaardbo JC, Skogstrand K, Ryder LP, Ersboll AK, et al. Increased levels of regulatory T cells (Tregs) in human immunodeficiency virus-infected patients after 5 years of highly active anti-retroviral therapy may be due to increased thymic production of naive Tregs. Clin Exp Immunol. 2009;155:44–52. doi: 10.1111/j.1365-2249.2008.03803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsunemi S, Iwasaki T, Imado T, Higasa S, Kakishita E, et al. Relationship of CD4+CD25+ regulatory T cells to immune status in HIV-infected patients. AIDS. 2005;19:879–886. doi: 10.1097/01.aids.0000171401.23243.56. [DOI] [PubMed] [Google Scholar]
- 15.Kornbluth RS, Stone GW. Immunostimulatory combinations: designing the next generation of vaccine adjuvants. J Leukoc Biol. 2006;80:1084–1102. doi: 10.1189/jlb.0306147. [DOI] [PubMed] [Google Scholar]
- 16.Chougnet C, Gessani S. Role of gp120 in dendritic cell dysfunction in HIV infection. J Leukoc Biol. 2006;80:994–1000. doi: 10.1189/jlb.0306135. [DOI] [PubMed] [Google Scholar]
- 17.Granelli-Piperno A, Golebiowska A, Trumpfheller C, Siegal FP, Steinman RM. HIV-1-infected monocyte-derived dendritic cells do not undergo maturation but can elicit IL-10 production and T cell regulation. Proc Natl Acad Sci U S A. 2004;101:7669–7674. doi: 10.1073/pnas.0402431101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krathwohl MD, Schacker TW, Anderson JL. Abnormal presence of semimature dendritic cells that induce regulatory T cells in HIV-infected subjects. J Infect Dis. 2006;193:494–504. doi: 10.1086/499597. [DOI] [PubMed] [Google Scholar]
- 19.Lan YY, Wang Z, Raimondi G, Wu W, Colvin BL, et al. “Alternatively activated” dendritic cells preferentially secrete IL-10, expand Foxp3+CD4+ T cells, and induce long-term organ allograft survival in combination with CTLA4-Ig. J Immunol. 2006;177:5868–5877. doi: 10.4049/jimmunol.177.9.5868. [DOI] [PubMed] [Google Scholar]
- 20.Manches O, Munn D, Fallahi A, Lifson J, Chaperot L, et al. HIV-activated human plasmacytoid DCs induce Tregs through an indoleamine 2,3-dioxygenase-dependent mechanism. J Clin Invest. 2008;118:3431–3439. doi: 10.1172/JCI34823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang R, Lifson JD, Chougnet C. Failure of HIV-exposed CD4+ T cells to activate dendritic cells is reversed by restoration of CD40/CD154 interactions. Blood. 2006;107:1989–1995. doi: 10.1182/blood-2005-07-2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Penna G, Roncari A, Amuchastegui S, Daniel KC, Berti E, et al. Expression of the inhibitory receptor ILT3 on dendritic cells is dispensable for induction of CD4+Foxp3+ regulatory T cells by 1,25-dihydroxyvitamin D3. Blood. 2005;106:3490–3497. doi: 10.1182/blood-2005-05-2044. [DOI] [PubMed] [Google Scholar]
- 23.Benson MJ, Pino-Lagos K, Rosemblatt M, Noelle RJ. All-trans retinoic acid mediates enhanced T reg cell growth, differentiation, and gut homing in the face of high levels of co-stimulation. J Exp Med. 2007;204:1765–1774. doi: 10.1084/jem.20070719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coombes JL, Siddiqui KR, Arancibia-Carcamo CV, Hall J, Sun CM, et al. A functionally specialized population of mucosal CD103+ DCs induces Foxp3+ regulatory T cells via a TGF-beta and retinoic acid-dependent mechanism. J Exp Med. 2007;204:1757–1764. doi: 10.1084/jem.20070590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mucida D, Park Y, Kim G, Turovskaya O, Scott I, et al. Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science. 2007;317:256–260. doi: 10.1126/science.1145697. [DOI] [PubMed] [Google Scholar]
- 26.Sun CM, Hall JA, Blank RB, Bouladoux N, Oukka M, et al. Small intestine lamina propria dendritic cells promote de novo generation of Foxp3 T reg cells via retinoic acid. J Exp Med. 2007;204:1775–1785. doi: 10.1084/jem.20070602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen W, Liang X, Peterson AJ, Munn DH, Blazar BR. The indoleamine 2,3-dioxygenase pathway is essential for human plasmacytoid dendritic cell-induced adaptive T regulatory cell generation. J Immunol. 2008;181:5396–5404. doi: 10.4049/jimmunol.181.8.5396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fallarino F, Grohmann U, Hwang KW, Orabona C, Vacca C, et al. Modulation of tryptophan catabolism by regulatory T cells. Nat Immunol. 2003;4:1206–1212. doi: 10.1038/ni1003. [DOI] [PubMed] [Google Scholar]
- 29.Fallarino F, Grohmann U, You S, McGrath BC, Cavener DR, et al. Tryptophan catabolism generates autoimmune-preventive regulatory T cells. Transpl Immunol. 2006;17:58–60. doi: 10.1016/j.trim.2006.09.017. [DOI] [PubMed] [Google Scholar]
- 30.Goleva E, Cardona ID, Ou LS, Leung DY. Factors that regulate naturally occurring T regulatory cell-mediated suppression. J Allergy Clin Immunol. 2005;116:1094–1100. doi: 10.1016/j.jaci.2005.08.051. [DOI] [PubMed] [Google Scholar]
- 31.Nilsson J, Boasso A, Velilla PA, Zhang R, Vaccari M, et al. HIV-1-driven regulatory T-cell accumulation in lymphoid tissues is associated with disease progression in HIV/AIDS. Blood. 2006;108:3808–3817. doi: 10.1182/blood-2006-05-021576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sansom DM, Manzotti CN, Zheng Y. What's the difference between CD80 and CD86? Trends Immunol. 2003;24:314–319. doi: 10.1016/s1471-4906(03)00111-x. [DOI] [PubMed] [Google Scholar]
- 33.Bennett CL, Christie J, Ramsdell F, Brunkow ME, Ferguson PJ, et al. The immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome (IPEX) is caused by mutations of FOXP3. Nat Genet. 2001;27:20–21. doi: 10.1038/83713. [DOI] [PubMed] [Google Scholar]
- 34.Brunkow ME, Jeffery EW, Hjerrild KA, Paeper B, Clark LB, et al. Disruption of a new forkhead/winged-helix protein, scurfin, results in the fatal lymphoproliferative disorder of the scurfy mouse. Nat Genet. 2001;27:68–73. doi: 10.1038/83784. [DOI] [PubMed] [Google Scholar]
- 35.Wildin RS, Ramsdell F, Peake J, Faravelli F, Casanova JL, et al. X-linked neonatal diabetes mellitus, enteropathy and endocrinopathy syndrome is the human equivalent of mouse scurfy. Nat Genet. 2001;27:18–20. doi: 10.1038/83707. [DOI] [PubMed] [Google Scholar]
- 36.Ziegler SF. FOXP3: of mice and men. Annu Rev Immunol. 2006;24:209–226. doi: 10.1146/annurev.immunol.24.021605.090547. [DOI] [PubMed] [Google Scholar]
- 37.Fazekas de St Groth B, Landay AL. Regulatory T cells in HIV infection: pathogenic or protective participants in the immune response? AIDS. 2008;22:671–683. doi: 10.1097/QAD.0b013e3282f466da. [DOI] [PubMed] [Google Scholar]
- 38.Firan M, Dhillon S, Estess P, Siegelman MH. Suppressor activity and potency among regulatory T cells is discriminated by functionally active CD44. Blood. 2006;107:619–627. doi: 10.1182/blood-2005-06-2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eggena MP, Barugahare B, Jones N, Okello M, Mutalya S, et al. Depletion of regulatory T cells in HIV infection is associated with immune activation. J Immunol. 2005;174:4407–4414. doi: 10.4049/jimmunol.174.7.4407. [DOI] [PubMed] [Google Scholar]
- 40.Huehn J, Hamann A. Homing to suppress: address codes for Treg migration. Trends Immunol. 2005;26:632–636. doi: 10.1016/j.it.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 41.Seddiki N, Kelleher AD. Regulatory T cells in HIV infection: who's suppressing what? Curr HIV/AIDS Rep. 2008;5:20–26. doi: 10.1007/s11904-008-0004-6. [DOI] [PubMed] [Google Scholar]
- 42.Legrand FA, Nixon DF, Loo CP, Ono E, Chapman JM, et al. Strong HIV-1-specific T cell responses in HIV-1-exposed uninfected infants and neonates revealed after regulatory T cell removal. PLoS One. 2006;1:e102. doi: 10.1371/journal.pone.0000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu W, Putnam AL, Xu-Yu Z, Szot GL, Lee MR, et al. CD127 expression inversely correlates with FoxP3 and suppressive function of human CD4+ T reg cells. J Exp Med. 2006;203:1701–1711. doi: 10.1084/jem.20060772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Seddiki N, Santner-Nanan B, Martinson J, Zaunders J, Sasson S, et al. Expression of interleukin (IL)-2 and IL-7 receptors discriminates between human regulatory and activated T cells. J Exp Med. 2006;203:1693–1700. doi: 10.1084/jem.20060468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Levy Y. Cytokine-based modulation of immune function in HIV infection. Curr Opin HIV AIDS. 2006;1:69–73. doi: 10.1097/01.COH.0000194101.89944.a5. [DOI] [PubMed] [Google Scholar]
- 46.Sereti I, Imamichi H, Natarajan V, Imamichi T, Ramchandani MS, et al. In vivo expansion of CD4CD45RO-CD25 T cells expressing foxP3 in IL-2-treated HIV-infected patients. J Clin Invest. 2005;115:1839–1847. doi: 10.1172/JCI24307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fritzsching B, Oberle N, Pauly E, Geffers R, Buer J, et al. Naive regulatory T cells: a novel subpopulation defined by resistance toward CD95L-mediated cell death. Blood. 2006;108:3371–3378. doi: 10.1182/blood-2006-02-005660. [DOI] [PubMed] [Google Scholar]
- 48.Seddiki N, Santner-Nanan B, Tangye SG, Alexander SI, Solomon M, et al. Persistence of naive CD45RA+ regulatory T cells in adult life. Blood. 2006;107:2830–2838. doi: 10.1182/blood-2005-06-2403. [DOI] [PubMed] [Google Scholar]
- 49.Valmori D, Merlo A, Souleimanian NE, Hesdorffer CS, Ayyoub M. A peripheral circulating compartment of natural naive CD4 Tregs. J Clin Invest. 2005;115:1953–1962. doi: 10.1172/JCI23963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen W, Jin W, Hardegen N, Lei KJ, Li L, et al. Conversion of peripheral CD4+CD25- naive T cells to CD4+CD25+ regulatory T cells by TGF-beta induction of transcription factor Foxp3. J Exp Med. 2003;198:1875–1886. doi: 10.1084/jem.20030152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fu S, Zhang N, Yopp AC, Chen D, Mao M, et al. TGF-beta induces Foxp3 + T-regulatory cells from CD4+CD25 - precursors. Am J Transplant. 2004;4:1614–1627. doi: 10.1111/j.1600-6143.2004.00566.x. [DOI] [PubMed] [Google Scholar]
- 52.Pillai V, Ortega SB, Wang CK, Karandikar NJ. Transient regulatory T-cells: a state attained by all activated human T-cells. Clin Immunol. 2007;123:18–29. doi: 10.1016/j.clim.2006.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Walker MR, Kasprowicz DJ, Gersuk VH, Benard A, Van Landeghen M, et al. Induction of FoxP3 and acquisition of T regulatory activity by stimulated human CD4+CD25- T cells. J Clin Invest. 2003;112:1437–1443. doi: 10.1172/JCI19441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vukmanovic-Stejic M, Zhang Y, Cook JE, Fletcher JM, McQuaid A, et al. Human CD4+ CD25hi Foxp3+ regulatory T cells are derived by rapid turnover of memory populations in vivo. J Clin Invest. 2006;116:2423–2433. doi: 10.1172/JCI28941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Luth S, Huber S, Schramm C, Buch T, Zander S, et al. Ectopic expression of neural autoantigen in mouse liver suppresses experimental autoimmune neuroinflammation by inducing antigen-specific Tregs. J Clin Invest. 2008;118:3403–3410. doi: 10.1172/JCI32132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gavin MA, Torgerson TR, Houston E, DeRoos P, Ho WY, et al. Single-cell analysis of normal and FOXP3-mutant human T cells: FOXP3 expression without regulatory T cell development. Proc Natl Acad Sci U S A. 2006;103:6659–6664. doi: 10.1073/pnas.0509484103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Morgan ME, van Bilsen JH, Bakker AM, Heemskerk B, Schilham MW, et al. Expression of FOXP3 mRNA is not confined to CD4+CD25+ T regulatory cells in humans. Hum Immunol. 2005;66:13–20. doi: 10.1016/j.humimm.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 58.Tran DQ, Ramsey H, Shevach EM. Induction of FOXP3 expression in naive human CD4+FOXP3 T cells by T-cell receptor stimulation is transforming growth factor-beta dependent but does not confer a regulatory phenotype. Blood. 2007;110:2983–2990. doi: 10.1182/blood-2007-06-094656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang J, Ioan-Facsinay A, van der Voort EI, Huizinga TW, Toes RE. Transient expression of FOXP3 in human activated nonregulatory CD4+ T cells. Eur J Immunol. 2007;37:129–138. doi: 10.1002/eji.200636435. [DOI] [PubMed] [Google Scholar]
- 60.Glencross D, Scott LE, Jani IV, Barnett D, Janossy G. CD45-assisted PanLeucogating for accurate, cost-effective dual-platform CD4+ T-cell enumeration. Cytometry. 2002;50:69–77. doi: 10.1002/cyto.10068. [DOI] [PubMed] [Google Scholar]
- 61.Bisikirska B, Colgan J, Luban J, Bluestone JA, Herold KC. TCR stimulation with modified anti-CD3 mAb expands CD8+ T cell population and induces CD8+CD25+ Tregs. J Clin Invest. 2005;115:2904–2913. doi: 10.1172/JCI23961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hoji A, Coro A, Ng HL, Jamieson BD, Yang OO. Proliferation and foxp3 expression in virus-specific memory CD8+ T lymphocytes. AIDS Res Hum Retroviruses. 2008;24:1087–1095. doi: 10.1089/aid.2008.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mahic M, Henjum K, Yaqub S, Bjornbeth BA, Torgersen KM, et al. Generation of highly suppressive adaptive CD8(+)CD25(+)FOXP3(+) regulatory T cells by continuous antigen stimulation. Eur J Immunol. 2008;38:640–646. doi: 10.1002/eji.200737529. [DOI] [PubMed] [Google Scholar]
- 64.Sharabi A, Mozes E. The suppression of murine lupus by a tolerogenic peptide involves foxp3-expressing CD8 cells that are required for the optimal induction and function of foxp3-expressing CD4 cells. J Immunol. 2008;181:3243–3251. doi: 10.4049/jimmunol.181.5.3243. [DOI] [PubMed] [Google Scholar]
- 65.Zhang Z, Jiang Y, Zhang M, Shi W, Liu J, et al. Relationship of frequency of CD4+CD25+Foxp3+ regulatory T cells with disease progression in antiretroviral-naive HIV-1 infected Chinese. Jpn J Infect Dis. 2008;61:391–392. [PubMed] [Google Scholar]
- 66.Billerbeck E, Thimme R. CD8+ regulatory T cells in persistent human viral infections. Hum Immunol. 2008;69:771–775. doi: 10.1016/j.humimm.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 67.Jiang H, Wu Y, Liang B, Zheng Z, Tang G, et al. An affinity/avidity model of peripheral T cell regulation. J Clin Invest. 2005;115:302–312. doi: 10.1172/JCI23879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vogtenhuber C, O'Shaughnessy MJ, Vignali DA, Blazar BR. Outgrowth of CD4low/negCD25+ T cells with suppressor function in CD4+CD25+ T cell cultures upon polyclonal stimulation ex vivo. J Immunol. 2008;181:8767–8775. doi: 10.4049/jimmunol.181.12.8767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Koch SD, Uss E, van Lier RA, ten Berge IJ. Alloantigen-induced regulatory CD8+CD103+ T cells. Hum Immunol. 2008;69:737–744. doi: 10.1016/j.humimm.2008.08.281. [DOI] [PubMed] [Google Scholar]
- 70.Boasso A, Vaccari M, Hryniewicz A, Fuchs D, Nacsa J, et al. Regulatory T-cell markers, indoleamine 2,3-dioxygenase, and virus levels in spleen and gut during progressive simian immunodeficiency virus infection. J Virol. 2007;81:11593–11603. doi: 10.1128/JVI.00760-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Burl S, Hill PC, Jeffries DJ, Holland MJ, Fox A, et al. FOXP3 gene expression in a tuberculosis case contact study. Clin Exp Immunol. 2007;149:117–122. doi: 10.1111/j.1365-2249.2007.03399.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chen W, Perruche S, Li J. CD4+CD25+ T regulatory cells and TGF-beta in mucosal immune system: the good and the bad. Curr Med Chem. 2007;14:2245–2249. doi: 10.2174/092986707781696591. [DOI] [PubMed] [Google Scholar]
- 73.Gazzola L, Tincati C, Gori A, Saresella M, Marventano I, et al. FoxP3 mRNA expression in regulatory T cells from patients with tuberculosis. Am J Respir Crit Care Med. 2006;174:356; author reply 357. doi: 10.1164/ajrccm.174.3.356. [DOI] [PubMed] [Google Scholar]
- 74.Guyot-Revol V, Innes JA, Hackforth S, Hinks T, Lalvani A. Regulatory T cells are expanded in blood and disease sites in patients with tuberculosis. Am J Respir Crit Care Med. 2006;173:803–810. doi: 10.1164/rccm.200508-1294OC. [DOI] [PubMed] [Google Scholar]
- 75.Hougardy JM, Place S, Hildebrand M, Drowart A, Debrie AS, et al. Regulatory T cells depress immune responses to protective antigens in active tuberculosis. Am J Respir Crit Care Med. 2007;176:409–416. doi: 10.1164/rccm.200701-084OC. [DOI] [PubMed] [Google Scholar]
- 76.Hougardy JM, Verscheure V, Locht C, Mascart F. In vitro expansion of CD4+CD25highFOXP3+CD127low/- regulatory T cells from peripheral blood lymphocytes of healthy Mycobacterium tuberculosis-infected humans. Microbes Infect. 2007;9:1325–1332. doi: 10.1016/j.micinf.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 77.Jaron B, Maranghi E, Leclerc C, Majlessi L. Effect of attenuation of Treg during BCG immunization on anti-mycobacterial Th1 responses and protection against Mycobacterium tuberculosis. PLoS One. 2008;3:e2833. doi: 10.1371/journal.pone.0002833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kursar M, Koch M, Mittrucker HW, Nouailles G, Bonhagen K, et al. Cutting Edge: Regulatory T cells prevent efficient clearance of Mycobacterium tuberculosis. J Immunol. 2007;178:2661–2665. doi: 10.4049/jimmunol.178.5.2661. [DOI] [PubMed] [Google Scholar]
- 79.Li L, Lao SH, Wu CY. Increased frequency of CD4(+)CD25(high) Treg cells inhibit BCG-specific induction of IFN-gamma by CD4(+) T cells from TB patients. Tuberculosis (Edinb) 2007;87:526–534. doi: 10.1016/j.tube.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 80.Qin XJ, Shi HZ, Liang QL, Huang LY, Yang HB. CD4+CD25+ regulatory T lymphocytes in tuberculous pleural effusion. Chin Med J (Engl) 2008;121:581–586. [PubMed] [Google Scholar]
- 81.Ribeiro-Rodrigues R, Resende Co T, Rojas R, Toossi Z, Dietze R, et al. A role for CD4+CD25+ T cells in regulation of the immune response during human tuberculosis. Clin Exp Immunol. 2006;144:25–34. doi: 10.1111/j.1365-2249.2006.03027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Scott-Browne JP, Shafiani S, Tucker-Heard G, Ishida-Tsubota K, Fontenot JD, et al. Expansion and function of Foxp3-expressing T regulatory cells during tuberculosis. J Exp Med. 2007;204:2159–2169. doi: 10.1084/jem.20062105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wu B, Huang C, Kato-Maeda M, Hopewell PC, Daley CL, et al. Messenger RNA expression of IL-8, FOXP3, and IL-12beta differentiates latent tuberculosis infection from disease. J Immunol. 2007;178:3688–3694. doi: 10.4049/jimmunol.178.6.3688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Roberts T, Beyers N, Aguirre A, Walzl G. Immunosuppression during active tuberculosis is characterized by decreased interferon- gamma production and CD25 expression with elevated forkhead box P3, transforming growth factor- beta, and interleukin-4 mRNA levels. J Infect Dis. 2007;195:870–878. doi: 10.1086/511277. [DOI] [PubMed] [Google Scholar]