Abstract
In the months before and years since Medicare Part D’s implementation in January 2006, many have been concerned with beneficiaries’ ability to benefit from the complex program. We undertook a systematic review of published Medline and grey literature from January 1, 2005 -August 20, 2009 in order to evaluate Medicare beneficiaries’ knowledge about Part D and how this knowledge informed decisions regarding enrollment and plan choice. We included 30 articles that reported original results describing either seniors’ knowledge of the Part D benefit, decision to enroll, and/or selection of plans, that reported results from patient surveys addressing these issues, or that analyzed actual enrollment data or plan selection patterns. Of these 30 articles, 10 described beneficiaries’ knowledge, 12 described enrollment and plan choices and 8 concerned both knowledge and choice. Across studies and years, beneficiaries’ knowledge of the Part D program and benefit structure/design was poor, particularly with regards to the coverage gap and the low-income subsidy. Beneficiaries had great difficulty choosing the lowest cost Part D plans and were disinclined to switch plans to improve their benefits. Knowledge deficits, enrollment problems, and plan choice difficulties were most pronounced during Part D implementation in early 2006, but also persisted in subsequent years of the benefit. Beneficiaries’ knowledge and choices should be monitored on an ongoing basis to inform potential changes to the Part D program.
Keywords: Medicare Part D, systematic review, choice, knowledge
BACKGROUND
The implementation of Medicare Part D in January 2006 offered seniors improved access to prescription drug insurance. At least one-quarter of elderly Medicare beneficiaries had no previous drug insurance,1 and 22.5 million beneficiaries (53%) were enrolled in the benefit by June 2006.2 In the months prior to Part D’s inception, and in the months and years since, researchers, policymakers, and patient advocates have fiercely debated elderly beneficiaries’ ability to navigate and benefit from the unique features of the Medicare Part D program.3, 4 Many have complained that the benefit is too complex:3 the benefit is administered by numerous private insurers; seniors must choose among over 40 plans in each geographic area;5 each plan uses an array of drug formulary and cost sharing mechanisms6 which insurers may change at any time;7, 8 and the standard benefit includes a gap in coverage during which beneficiaries are responsible for 100% of drug costs (the coverage gap).9 Beneficiaries with incomes below certain thresholds can apply for a low-income subsidy (LIS) to help ease the cost-sharing burden, but this process can be cumbersome and confusing.10 The intricacies of the Part D benefit may present information challenges for even the savviest Medicare beneficiary.
In this systematic review, we evaluate data from 2005 to the present regarding beneficiaries’ knowledge about Part D both before and after the benefit began. We examine how beneficiaries used their knowledge to choose Part D plans and the extent to which beneficiaries’ plan choices were aligned with their health and financial interests. We also assess beneficiaries’ responses to sub-optimal plan choices when they have the opportunity to switch plans. We discuss our findings’ implications for the future of the Part D program.
METHODS
Literature Search and Selection
A systematic search of the medical literature was performed to identify studies addressing seniors’ knowledge of the Medicare Part D prescription drug benefit, their choice to enroll, and their selection of Part D plans. The initial searches were limited to articles published in Medline between January 1, 2005, one year before the Part D benefit was implemented, and August 20, 2009. Our search used three main subject heading domains: terms relating to Medicare Part D (for example, [Medicare AND drug benefit OR drug plan OR prescription], OR Part D, OR Medicare Modernization Act, OR MMA), terms relating to knowledge (for example know$, OR understand$, OR comprehen$) and terms related to decisions to enroll or plan selection (for example: choice, OR choose, OR enroll$, or participat$, OR decide, OR select$, OR access, OR, utiliz$). Articles containing at least one search term regarding Part D and at least one search term from one of the other two categories were included in the review.
We also searched the “grey literature” for original reports using the same criteria. Our search included the websites of the Kaiser Family Foundation, General Accounting Office, Families USA, Congressional Budget Office, Centers for Medicare and Medicaid Services (CMS), Congressional Testimony, AARP, the Commonwealth Fund, and Avalere Health. We reference mined articles included from our initial search and sought input from an expert at CMS (A.B.) who had accumulated relevant articles.
Articles were included if they reported original results describing either seniors’ knowledge of the Part D benefit, their decision to enroll, and/or selection of plans. Articles were included if they reported results from patient surveys explicitly addressing these issues or if actual enrollment data were analyzed and plan selection or enrollment patterns were reported. We excluded all studies in which plan choice was simulated or modeled based on data prior to 2006.
Extraction of Study-Level Variables and Results
Two reviewers [W.S. and U.S.] evaluated the titles and abstracts of search results to identify potentially relevant articles. Complete articles were assessed for inclusion by two reviewers [J.P. and U.S.]. Data was extracted from selected articles by three reviewers [J.P., W.S., U.S.] and differences were resolved by consensus. Variables assessed included the key research questions in each study, characteristics of the patient population (i.e., sample size, sociodemographic characteristics), setting, study design (analysis of enrollment data or patient survey), results, and conclusions drawn.
Data Synthesis
Articles were grouped into 2 main categories: seniors’ knowledge about Part D plans and their choice of plans. We created evidence tables reporting results from each of these searches, one focusing on knowledge and the other focusing on choice. Several studies reported data relevant to both research questions and the relevant data from those studies were included in both tables. Based on common themes identified across articles, we further grouped studies into those that described knowledge of 1) the Part D program, 2) Part D’s benefit structure, cost sharing, and formularies, and 3) the low-income subsidy as well as those that described choices regarding 1) enrollment in Part D, 2) in which Part D plan to enroll, 3) switching Part D plans.
RESULTS
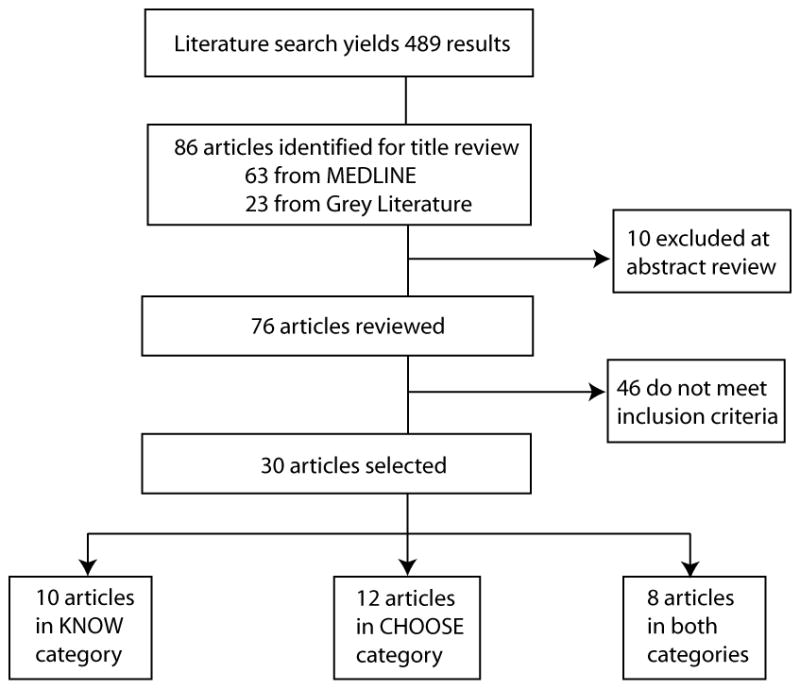
Of 489 potentially relevant abstracts and titles screened, 76 articles were evaluated in full, and 30 articles met all inclusion and exclusion criteria (Figure 1). These articles can be categorized as follows: 10 described beneficiaries’ knowledge of Part D,11–20 12 described beneficiaries’ Part D choices,18, 21–31 and 8 articles concerned both beneficiary knowledge and choice.32–39 Of the selected articles, 14 were from the peer-reviewed medical literature while the remaining were from the grey literature.
Figure 1.
Medicare beneficiaries’ knowledge about Part D (Table 1)
Table 1.
Medicare beneficiaries’ knowledge about Part D
| Reference | Research Question | # of Subjects | Design | Results | Conclusion |
|---|---|---|---|---|---|
| Goedken AM, Urmie JM, Farris KB, Doucette WR (2009) 13 | What are the characteristics of Medicare beneficiaries who intend to enroll in Part D? | 1200 English speaking U.S. residents aged 65+ enrolled in Medicare | Online cross- sectional survey administered in October 2005 |
|
Younger age, fair or poor health, lack of drug coverage, greater use of prescription drugs, and low income were predictors of Medicare beneficiaries’ intentions to enroll in Part D. |
| Skarupski KA, Mendes de Leon CF, Barnes LL, Evans DE (2009) 36 | Does knowledge of the Part D benefit differ among blacks and whites? | 2,694 community-dwelling adults aged 65+ in Chicago; 1,784 are black, 910 are white | Cross-sectional interviews between April 2006 and October 2007 |
|
Blacks in this community, in comparison to Whites, were more likely to express knowledge gaps or lack of awareness about the Part D program. These gaps may have hindered Part D enrollment. |
| Hsu J, Fung V, Price M et al. (2008) 15 | What do beneficiaries know about Part D benefits and costs? Are they aware of the coverage gap? | N=1040 of 1388 eligible, 74.9% response rate. Community-dwelling Kaiser- Permanente Northern California Medicare Advantage beneficiaries aged 65+ who were not eligible for Medicaid and did not receive a low-income subsidy | Mailed questionniare sent in January 2007, supplemented by telephone interview |
|
Beneficiaries in this Medicare Advantage plan have limited knowledge of Part D cost sharing, including limited knowledge of the coverage gap. The majority were unaware of Part D’s cost sharing structure unless they experienced it directly. |
| Summer L, Nemore P, Finberg J (2008) 18 | What are Part D counselors’ opinions regarding policy and procedural changes that could enhance Part D program performance? | 660 beneficiary contacts. 397/1707 (23%) on a list of individuals who assisted beneficiaries, 121 respond to forwarded email from another survey responder, 142 respond to GW Health Policy Institute request. Of the 660, 54% were beneficiary counselors, 8% were attorneys, 30% managed or directed organizations that assisted beneficiaries and the rest were health care providers and/or other interested parties | Electronic, cross- sectional survey in Fall 2006 |
|
Program complexity poses a challenge for the beneficiaries that these counselors assist, especially surrounding enrollment and low- income subsidy requirements. |
| Hargrave E, Piya B, Hoadley J, Summer L, Thompson J (2008) 32 | What have been the experiences of beneficiaries (and providers) in dealing with Part D? | 73 community-dwelling beneficiaries enrolled in a Part D plan and used at least 2 prescription drugs in Denver, CO, Richmond, VA, and Portland, ME. | 13 focus groups were conducted between July and October 2007. |
|
For the most part, beneficiaries were satisfied with Part D, despite knowledge gaps. Others were unwilling to switch plans because they did not want to undergo the complex processes of selecting and learning to use a new plan and/or were fearful of making a decision that placed them in a worse plan. |
| Cronk A, Humphries TL, Delate T, Clark D, Morris B (2008) 10 | What were the coping behaviors used by self- enrolled beneficiaries who reached the Part D coverage gap? How do these behaviors compare with those of Part D enrollees in a retiree drug subsidy plan who did not have a coverage gap but reached the gap threshold amount in 2006? | 1472 participants with >=$2250 in total drug spending by October 1, 2006: 740 in the KPCO Part D Medicare Advantage plan (MA-PD), 732 in the retiree drug subsidy plan (RDS). 42% competed the survey: 332 in the MA-PD plan, 290 in the RDS plan. | Retrospective review of electronic medical and pharmacy records from January 1 - September 30, 2006 to identify patients who met coverage gap threshold. Then, cross-sectional mailed survey administered in February and March 2007. |
|
Nearly a quarter of Medicare beneficiaries were unaware of the benefit thresholds for their plans. |
| Cummings JR, Rice T, Hanoch Y (2008) 11 | What are the characteristics of people who believe Medicare Part D is too complicated? What are the characteristics of people who endorse one of two policies to simplify the program? | 718 individuals 65 years and older were included in this group from a nationally representative telephone survey of 1,876 adults aged 18+ | Cross-sectional, nationally representative telephone survey |
|
Overall, most adults believe that the Part D program is too complex, that the number of plans should be reduced, and that seniors should have the option of purchasing drugs directly from a Medicare-operated plan. The authors assert that this conveys trust in government-run programs. |
| Hall JP, Kurth NK, Moore JM (2007) 14 | What was the impact of transition from Medicaid drug coverage to Medicare Part D on a sample of dually eligible adults younger than age 65 years with disabilities? | 328 (55%) individuals from a random sample of 600 employed Kansas community dual-eligibles participating in the Kansas Medicaid Buy-In Program. | Telephone survey/interviews between February and March 2006. |
|
Knowledge of enrollment requirements and plan switching ability was limited among these dual-eligibles. |
| De Natale (2007) 30 | What is beneficiaries’ access to and knowledge of Part D information? What are beneficiaries’ experiences in choosing plans? | 72 older adults (56 women and 16 men) with ages ranging from 65-90 from six senior centers in Santa Clara County, CA | Qualitative one- on-one, face-to- face interview study conducted from September – December 2006 |
|
Beneficiaries report that understanding the large influx of Part D information is daunting and that the coverage gap is of primary concern. Beneficiaries are reticent to make changes to their plan choices/assignments. |
| Keenan, TA (2007) 17 | What did beneficiaries know about the coverage gap and the LIS option? | 400 Part D beneficiaries aged 65+ | Cross-sectional telephone survey in October 2007 |
|
One in four Part D beneficiaries still are unaware of the coverage gap, a key feature of most Part D plans. Half are unaware of the LIS, and many who are aware believe that they would not qualify for such assistance. |
| Perry M, Dulio A, Cubanski J (2006) 35 | How knowledgeable are beneficiaries about Part D plans? What are their enrollment choices during the 2007 Part D enrollment period? | 35 Medicare beneficiaries with Part D plans. 27 are enrolled in Part D plans (8 non-duals in PDPs, 10 dual eligibles in PDPs, and 9 non-duals in MA-PDs), 5 have other creditable coverage, and 3 are not enrolled or have no creditable coverage. | In-person interviews completed October 2006 in 4 cities: Baltimore, Sacramento, Lincoln, and Miami |
|
Many beneficiaries lacked a basic understanding of their Part D coverage. They called for greater simplification of the program and plans offered to them, but for now they “make do” with what they have rather than shopping around, often due to fear that a new plan would be worse than the plan they currently had. |
| Winter J, Balza R, Caro F, Heiss F, Jun BH, Matzkin R, McFadden (2006) 19 | What were beneficiaries’ information and enrollment decisions for Part D before Part D open enrollment began in 2005? | Full sample is 4732, but most analyses report on 1808 individuals from sample of Medicare-eligible subjects surveyed before open enrollment began for Part D | Web-TV-based Retirement Perspectives Survey (RPS 2005) |
|
Many elderly consumers failed to understand the value of Part D as insurance against catastrophic prescription drug costs, and may as a consequence failed to enroll, or enrolled in expensive plans that emphasized low premiums or coverage of deductibles rather than catastrophic benefits. |
| Heiss F, McFadden D, Winter J (2006) 33 | What was the Part D enrollment process like for beneficiaries? | 2,137 seniors interviewed before open enrollment period (Nov 7–15, 2005) and then after open enrollment period ended (May 16 – June 2, 2006). Results presented for core of 1571 respondents age 65+ in May 2006 who were interviewed in both surveys and had no item nonresponse on key variables. | Web TV-based interview study, the Retirement Perspectives Survey (RPS). Respondents were asked about Part D knowledge and intentions in first interview, and about enrollment-process choices and opinions in second interview. |
|
More than half of respondents reported difficulty in understanding Part D’s structure, benefits, and formularies. Respondents were overwhelmed by the number of choices offered, but appreciated that they had choices. Respondents with more knowledge of the Part D benefit, prior drug coverage, and poorer health were more likely to enroll. |
| Keenan, TA (2006) 37 | What is beneficiary awareness and understanding of Part D? What is there enrollment status? When did beneficiaries enroll and with whom? | First survey in March 2006 mailed to 38,116 adults; 3602 of 5000 (72%) community elderly took a second survey in September 2006 | Cross-sectional mailed surveys |
|
Although 40% report limited understanding of their Part D plan, respondents gave Part D very high marks, and most would like to continue participation in the plans in which they are currently enrolled. Most believe that their current plan provides them good coverage and satisfactory access to medications. Most respondents who were eligible for LIS did not believe that they would qualify. |
| Dulio A, Perry M, Cubanski J (2006) 31 | What were Part D enrollees’ knowledge and experiences in the first 3 months of the benefit? | 21 Medicare beneficiaries; 6 in a stand-alone Part D plan, 6 in a Medicare Advantage plan (4 of whom were automatically enrolled), 5 with creditable coverage, and 4 with no drug coverage. These beneficiaries reside in Baltimore, MD; Lincoln, NE; Miami, FL; or Sacramento, CA | Face-to-face interviews conducted in March 2006 |
|
Three months into the benefit, beneficiaries expressed confusion about Part D and a desire for simplification of the program. |
| Kaiser Family Foundation (2005) 16 | What do dually-eligible beneficaries know about Part D in late 2005? | 4 dually-eligible adult beneficiaries, one each from Miami, FL; Baltimore, MD; Lincoln, NE; and Sacramento, CA | Face-to-face interview, between October 27 and November 16, 2005 |
|
In the months leading up to Part D’s implementation, these 4 dually- eligible beneficiaries expressed concern and a lack of knowledge as to how Part D would impact them. |
The Part D program
In each study, especially in the months surrounding Part D implementation, Medicare beneficiaries reported confusion about the Part D program. Among 784 beneficiaries surveyed in October-December 2005, 56% described having limited awareness of the upcoming changes to the Medicare program, and 53% did not know that all Medicare beneficiaries were eligible for Part D.36 Of 1500 respondents to 2 telephone interviews in November 2005 and May 2006, 34% said they poorly understood the Part D benefit.35 In a 2005 web-based survey, researchers found greater knowledge gaps among beneficiaries with a combination of low socio-economic status, bad health, and low cognition—54.3% of these beneficiaries had little or no knowledge about Part D plans.20 Differences in beneficiaries’ knowledge by race were also noted: in interviews with 2,694 community-dwelling elderly in the Chicago area in 2006–2007, researchers found that among non-enrollees, Blacks were more likely than Whites to report having been unaware of Part D (13.2% versus 2.4%) and that the program was too difficult to understand (12.9% versus 1.4%).38
Part D’s benefit structure
A majority admitted large gaps in their knowledge of and confusion about Part D’s benefit structure, particularly regarding the coverage gap. A 2007 mailed survey to beneficiaries of Kaiser Permanente Part D plans found that only 22% of high-spending respondents knew whether their plans had a coverage gap.11 In a separate 2007 survey, Hsu and colleagues found a larger percentage of beneficiaries (40%), knew about the coverage gap, but only 50% of those were able to state the monetary threshold to enter the coverage gap within $250.16 Even when beneficiaries were aware of the coverage gap, they frequently indicated that they did not understand how it worked or how to know whether they were at risk of entering the gap.34 Beneficiaries also reported confusion about the cost-sharing structures and formulary coverage of their plans, such as how their out-of-pocket costs were determined for each prescription purchase.13, 33
The low-income subsidy
At the time of Part D implementation and in later years, beneficiaries demonstrated a lack of awareness about the LIS and misperceptions about their eligibility and how to apply. Nearly one-third of community-dwelling elderly in a 2005 telephone survey thought that only dually-eligible beneficiaries could receive the LIS.36 In an electronic survey in Fall 2006, over 75% of professionals who counsel Medicare beneficiaries reported that beneficiaries were not aware of the LIS benefit, and 83% stated that beneficiaries often did not know how to apply or did not think they were eligible.19 One-half of community-dwelling elderly in a 2007 telephone survey had heard of the LIS, and only 10% thought that they would qualify for the assistance.18 Only 12% of LIS-eligible beneficiaries in a large mailed survey in 2007 thought they would qualify for the extra help.39
Medicare beneficiaries’ Part D choices (Table 2)
Table 2.
Medicare beneficiaries’ Part D choices
| Reference | Research Question | # of Subjects | Design | Results | Conclusion |
|---|---|---|---|---|---|
| Gruber, J (2009) 21 | Did Medicare beneficiaries choose the lowest cost stand-alone Part D plan available to them? | 55,000 individuals enrolled in a stand-alone PDP, had a Part D claim in 2006, were not employer-insured, dual eligible, or eligible for a low income subsidy or partial subsidy, were in the dataset for 2005 and 2006, and could be matched to a specific Part D plan | Estimates the cost of enrolling in each PDP available to each beneficiary. Two different models: 1) Backwards-looking model models plan choice using 2005 prescriptions; 2) Perfect foresight model models plan choice using 2006 prescriptions. |
|
In 2006, the majority of seniors did not make Part D plan choices that maximized their cost savings. |
| Neuman P, Cubanski J (2009)31 | What does Part D enrollment look like in 2009? | Plan enrollment data from the Centers for Medicare and Medicaid Services | Uses publicly available data released by CMS to determine beneficiaries’ prescription drug coverage in 2009 |
|
The majority of Medicare beneficiaries have drug coverage in 2009. Nearly 40% of beneficiaries are enrolled in stand-alone plans and 20% are enrolled in Medicare Advantage plans. |
| Patel R et al. (2009) 29 | How many beneficiaries are enrolled in the lowest cost plan available to them? | 155 Part D beneficiaries, 55% of whom were dual-eligible | Face-to-face intervention to help beneficiary select the Part D plan with the lowest cost |
|
Only 10% of beneficiaries were enrolled in the lowest cost Part D plan available to them. One quarter qualified for LIS but were not receiving it. |
| Skarupski KA, Mendes de Leon CF, Barnes LL, Evans DE (2009)36 | Does race affect who enrolled in Part D? | 2,694 community-dwelling adults aged 65+ in Chicago; 1,784 are black, 910 are white | Cross-sectional interviews between April 2006 and October 2007 |
|
While a higher percentage of blacks had enrolled in Part D than whites, the analysis suggests that racial differences in enrollment can be explained by other demographic and health characteristics. |
| Jackson EA, Axelsen KJ (2008)23 | Do dual-elgibile and other low-income subsidy beneficiaries make enrollment decisions based on formulary composition? | Users of top 168 drugs dispensed were persons above age 65 years as of October 2007; 20,958,188 persons in 2006; 22,127,705 persons in 2007; 23,485,757 in 2008. | Use publicly available data released by CMS to generate snapshots of formulary coverage and enrollment levels for years 2006 – 2008. Analysis tracked all Part D plans and tracked coverage of 152 of the most common brand name and generic drugs prescribed to seniors. |
|
A small percentage of beneficiaries switched plans from year to year, despite formulary changes by 39.3% of plans between 2006–2008. |
| Hargrave E, Piya B, Hoadley J, Summer L, Thompson J (2008)32 | What have beneficiaries (and providers) experienced in dealing with Part D? | 73 community-dwelling beneficiaries enrolled in a Part D plan and used at least 2 prescription drugs in Denver, CO, Richmond, VA, and Portland, ME. | 13 focus groups were conducted between July and October 2007. |
|
For the most part, beneficiaries were satisfied with Part D, despite knowledge gaps. Others were unwilling to switch plans because they did not want to undergo the complex processes of selecting and learning to use a new plan and/or were fearful of making a decision that placed them in a “worse” plan. |
| Keenan, TA (2008)24 | Did beneficiaries enroll in Part D? Why? Did they plan to switch plans for 2008? | 330 adults aged 65+ | Cross-sectional telephone survey in November 2008 |
|
40% of respondents had enrolled in a Part D plan, most often for financial reasons. 59% did not intend to switch their plan unless major changes occurred, and a majority felt they had made a good choice when choosing a plan. |
| McNerney T (2008)27 | Are Part D beneficiaries satisfied with their plans? Do they intend to switch plans for 2008? | 571 adults aged 65+ | Online cross-sectional survey conducted between November 29 and December 3, 2007 |
|
In 2007, the majority of Part D enrollees are satisfied with their plans. Only 19% were likely to switch plans. |
| Heiss F, McFadden D, Winter J (2007)22 | Did beneficiaries enroll in Part D? When did they enroll, and what plans did they choose? | Nationally representative sample of community-dwelling US elderly. 1573 respondents who were 65+ in May 2006, eligible for Part D, and interviewed in the Retirement Perspectives Study (RPS) in both 2005 and 2006. | Internet-based survey. Descriptive study of patients’ plan choices in 2006, their satisfaction with plans during 2006, and their subsequent plan-switching from 2006 – 2007. |
|
Seniors who were “active deciders” do not take full account of the future benefit and cost consequences of their Part D plan selection decisions, or the expected net benefits and risk properties of alternative plans. Rather, beneficiaries responded to the immediate incentives of their current health status and drug expenditures when picking plans. |
| Levy H, Weir D (2007)25 | Did elderly beneficiaries take up Part D benefits available to them? Did low-income beneficiaries enroll in low-income subsidies? | 10,175 Medicare-covered individuals ages 65 and older in 2006 enrolled in the Health and Retirement Study (HRS) who were also in the cohort in 2004 | HRS interview survey in 2004, 2006. |
|
Despite the complexity of the program, most Medicare beneficiaries seemed to have made enrollment decisions in which they had confidence. Those who enrolled in stand-alone Part D plans had the most choices to make, and 37% reported that the decision was “very” or “somewhat” difficult. Low-income subsidy applications were lower than expected, and many beneficiaries reported being unaware of the program. |
| Cubanski J, Neuman P (2007)20 | Which organizations and Part D plans attracted the most enrollees in 2006? What is the distribution of Part D enrollees by plan type and benefit design? | Plan-level Part D enrollment included 20.4 million enrollees in 2,811 Part D plans (1,446 PDPs and 1,365 MA-PD plans) | An analysis of Medicare Part D enrollment data exploring plan-level Part D enrollment. Also analyzed the distribution of Part D enrollees by plan type (PDP versus MA-PD) and benefit design. |
|
Beneficaries’ plan choices were influenced by name recognition or low premiums or both. Few enrollees chose plans with gap coverage in 2006. Those beneficiaries with minimal drug expenses might have opted to enroll in a low-premium plan likely to be without gap coverage to avoid the late enrollment premium penalty. It is also likely that some beneficiaries were unaware of the coverage gap when they enrolled in Part D or might not have understood the implications of choosing a plan with a gap. |
| Neuman P, Strollo MK, Guterman S, Rogers WH, Li A, Rodday AM, Safran DG (2007)28 | What proportion of seniors enrolled in Part D plans in 2006, and which subgroups were most likely to remain without coverage? What are the experiences of dual eligible Part D enrollees? How do the characteristics and experiences of Part D enrollees in stand-alone PDPs and MA-PD plans differ? | 16,072 noninstitutionalized seniors. Participants were respondents to 2003 national survey and a 1% sample of elderly beneficiaries provided by the CMS in June 2006 | Augmented longitudinal survey design. Survey was administered between 10/5 and 12/20/2006 using 5 stage survey protocol involving mail and telephone. Seniors received 1 of 3 possible surveys according to their CMS-designated enrollment status: 1) dual eligible, 2) Medicare Advantage, 3) all others. |
|
Only 10% of seniors still lacked drug coverage by end of 2006--most typically, those who were most difficult to reach (older, lower income, less education) or were in relatively good health. Many beneficiaries who were eligible for the LIS were not receiving it, and lack of awareness of the LIS program appeared to be a factor in the under-utilization of the benefit. Dual eligibles were more likely to switch plans in 2006 than were non-dual eligibles, in part most likely because they have this opportunity monthly and because of the random assignment nature of the auto-enrollment process. |
| De Natale (2007)30 | What were beneficiaries’ experiences in choosing Part D plans? | 72 older adults (56 women and 16 men) with ages ranging from 65–90 from six senior centers in Santa Clara County, CA | Qualitative one-on-one, face-to-face interview study conducted from September – December 2006 |
|
Beneficiaries are reticent to make changes to their plan choices/assignments, preferring to retain their current plan. |
| Keenan, TA (2007)18 | Why did beneficiaries enroll in Part D? Are they satisfied with their choices? Will they switch plans in 2008? | 400 Part D beneficiaries aged 65+ | Cross-sectional telephone survey in October 2007 |
|
Part D beneficiaries were motivated to enroll due to financial reasons and because they turned 65. Most beneficiaries planned to enroll again in 2008, and the majority planned to stick with the same plan in which they were currently enrolled. |
| McBride TD, Terry TL, Mueller KJ (2006)26 | What is Part D enrollment like in rural and urban areas? | 39% of all rural Medicare beneficiaries were enrolled in Part D coverage as of March 2006 (3,441,000/8,884,000); a small number (291,000) have drug coverage through MA plan (3.2%) while 21% (1,839,000) were enrollees in PDPs, and 15% (1,328,000) are dual-eligibles. | Cross-sectional, observational study/policy brief, data from CMS available March 2006 |
|
More rural beneficiaries are enrolled in the Medicare stand-alone Part D plans, which have equitable characteristics for urban and rural dwellers. Only 3% of rural beneficiaries are enrolled in Medicare Advantage Part D plans. The high enrollment in Part D in rural areas can be partially attributed to the high auto-enrollment of Medicaid dual-eligibles that live in rural areas. |
| Hibbard J, Greene J, Tusler M (2006)34 | What are beneficiaries’ intentions and experiences with regards to enrolling in a Part D plan? | 784 community-dwelling elderly individuals age 65+, not dually eligible (1600 originally sampled, response rate 49%) | Telephone survey administered between October 13-December 5, 2005 |
|
The complexity of the Part D benefit and the number of plan choices may be a barrier to enrollment. More than half of beneficiaries who had enrolled in a Part D plan did not compare the costs and benefits of different plans prior to selection, instead relying on prior experience with insurance plans or obtaining information from advertisements/plan representatives. |
| Perry M, Dulio A, Cubanski J (2006)35 | What were beneficiaries’ enrollment choices during the Part D 2007 enrollment period? | 35 Medicare beneficiaries with Part D plans. 27 are enrolled in Part D plans (8 non-duals in PDPs, 10 dual eligibles in PDPs, and 9 non-duals in MA-PDs), 5 have other creditable coverage, and 3 are not enrolled or have no creditable coverage. | In-person interviews completed October 2006 in 4 cities: Baltimore, Sacramento, Lincoln, and Miami |
|
Many expressed lacking a basic understanding of coverage. Most were not interested in switching plans in 2007. For now, they “make do” with the plan they have rather than shopping around, often due to the fear that a new plan will be worse than the plan they currently have. |
| Heiss F, McFadden D, Winter J (2006)33 | What plans did beneficiaries choose during enrollment in 2005–2006? | 2,137 seniors interviewed before open enrollment period (Nov 7–15, 2005) and then after open enrollment period ended (May 16 – June 2, 2006). Results presented for core of 1571 respondents age 65+ in May 2006 who were interviewed in both surveys and had no item nonresponse on key variables. | Web TV-based interview study, the Retirement Perspectives Survey (RPS). Respondents were asked about Part D knowledge and intentions in first interview, and about enrollment-process choices and opinions in second interview. |
|
Respondents with poorer health, prior drug coverage, and better knowledge of the Part D benefit were more likely to enroll in Part D by June 2006. |
| Keenan, TA (2006)37 | Did beneficiaries enroll in Part D? When did they enroll, and what plans did they choose? | First survey in March 2006 mailed to 38,116 adults; 3602 of 5000 (72%) community elderly took a second survey in September 2006 | Cross-sectional mailed surveys |
|
Respondents considered formulary coverage, premium amounts, and copayment amounts when selecting a Part D plan. A majority did not want to switch their plan. This was primarily because they believe that the plan provides them good coverage (although their knowledge is limited) and they are satisfied with the accessibility of medications under their current plan. |
| Keenan, TA (2006)37 | Did beneficiaries enroll in Part D? When did they enroll, and what plans did they choose? | First survey in March 2006 mailed to 38,116 adults; 3602 of 5000 (72%) community elderly took a second survey in September 200 | Cross-sectional mailed surveys |
|
Respondents considered formulary coverage, premium amounts, and copayment amounts when selecting a Part D plan. A majority did not want to switch their plan. This was primarily because they believe that the plan provides them good coverage (although their knowledge is limited) and they are satisfied with the accessibility of medications under their current plan. |
| Dulio A, Perry M, Cubanski J (2006)31 | How did beneficiaries decide whether to enroll in Part D? What plans did they choose? | 21 Medicare beneficiaries; 6 in a stand-alone Part D plan, 6 in a Medicare Advantage plan (4 of whom were automatically enrolled), 5 with creditable coverage, and 4 with no drug coverage. These beneficiaries reside in Baltimore, MD; Lincoln, NE; Miami, FL; or Sacramento, CA | Face-to-face interviews conducted in March 2006 |
|
Rather than methodological comparisons to find the plan that best suited their needs, beneficiaries’ enrollment choices were based on name recognition, prior experience with the company offering a plan, auto-enrollment, or feeling pressured to enroll. |
Beneficiaries’ enrollment choices
According to a 2006 national survey of 16,072 community-dwelling seniors, 61% of respondents who did not have drug coverage in 2005 enrolled in Part D plans in 2006.29 These findings are consistent with those of the Retirement Perspectives Study: 68.1% of respondents were enrolled in a Part D plan in 2006, 24.5% had other creditable coverage, and only 7.4% lacked any drug insurance.35 Of 22.5 million Part D enrollees as of July 1, 2006 nationwide, 16 million (71%) were enrolled in a stand-alone plan while 6.5 million (29%) were enrolled in a Medicare Advantage plan. As of February 1, 2009, 17.5 million (66%) Part D enrollees were enrolled in a stand-alone plan and 9.2 million (34%) were enrolled in a Medicare Advantage plan.31 Enrollment in stand-alone plans was higher in rural than in urban areas (21% versus 13%), reflecting the more limited presence of Medicare Advantage Part D plans in rural areas.27 Seniors listed the most important reasons they enrolled, which included: 1) enrolling seemed less costly than waiting, 2) high drug costs, 3) anticipated financial savings, and 4) turning 65.18, 25, 39 Of all Part D enrollees in one 2006 survey, 69% reported feeling “very confident” or “somewhat confident” about having made the right decision to enroll, and 86% of them planned to sign up for Part D again in 2007.26
Many plans, but poor plan choices
In many studies, Part D-eligible beneficiaries felt that there were “too many choices” when trying to select a plan and felt overwhelmed by the decision.19, 33, 35–37 Faced with the prospect of choosing a plan, 81% of 3,602 beneficiaries responding to a 2006 mailed survey reported that the specific drugs covered and the premium amounts a plan offered were important to them, while 80% cited the copayment amounts.39 Selecting a plan that covered all of their drugs was also important.33 However, in practice, beneficiaries made few plan comparisons to look for these attributes: in a telephone survey, only 41% of Part D plan self-enrollees reported comparing costs and benefits of different plans, and most compared an average of 4 plans.36
Instead of comparing plans, many beneficiaries chose plans with which they had a prior relationship or from which they had received information through a representative or advertisement.33, 36 In 2006 plan enrollment data, ten insurance companies accounted for 72% of Part D enrollment, and two plans accounted for 23% of Part D enrollment nationwide, the AARP MedicareRX and Standard plans.21 The researchers speculate that high enrollment in the AARP plan was likely due to brand recognition while enrollment in the Standard plan was likely based on its low premium costs.21
Regardless of their plan selection strategy, many beneficiaries did not choose the plan that saved them the most money. An economic analysis of 55,000 seniors’ plan choices revealed that only 6 – 9% chose the lowest cost plan available to them in 2006 and seniors would have saved between $360 – $520 had they chosen the lowest cost plan.22 A face-to-face intervention designed to help 155 Part D beneficiaries choose their optimal plan for the following year found that 90% of beneficiaries were not currently enrolled in their optimal plan and could realize cost savings by switching to a different Part D plan for the following year.30
Beneficiaries’ reluctance to switch plans
Despite beneficiaries’ poor plan choices, most expressed little desire to switch plans in order to improve their benefits.32 Reasons for not switching included beliefs that: 1) the plan they have is better than one they don’t know; 2) switching plans is a tedious, overwhelming process; 3) switching plans would actually cause problems; and 4) they cannot switch plans without assistance.34, 37 Even when assistance was available, such as in the open enrollment period intervention, only 55 of 123 (45%) of beneficiaries switched plans. 30 This reluctance to switch persisted throughout all study years. Among interviewees enrolled in a Part D plan in 2006, 62% did not consider switching; 18.4% considered switching but did not; and only 10.7% switched plans for 2007.23 Among 400 respondents to a telephone survey in 2007, 80% planned to keep the same plan in 2008,18 while another poll found that only 19% considered switching plans for 2008.28
DISCUSSION
In this systematic review, we examined studies concerning Medicare beneficiaries’ knowledge of and choices regarding Part D. Beneficiaries reported substantial gaps in their knowledge of the Part D program, including enrollment requirements and the coverage gap period. Part D knowledge differences across race, health status, and cognition group were documented. A conspicuously large group of beneficiaries eligible for a low-income subsidy (LIS) to defray out-of-pocket Part D costs were unaware of this option, did not think they were eligible, or did not know how to apply.
Regardless of their limited knowledge, beneficiaries enrolled in Part D in large numbers and generally expressed confidence in their decisions. However, confusion and lack of knowledge may have translated into poor Part D plan choices. In 2006, only 6–9% of beneficiaries chose the lowest cost plan available to them.22 Even though beneficiaries subsequently had the opportunity to improve upon their initial plan choices, a majority chose not to switch plans.
While the months just before and just after the Part D implementation on January 1, 2006 were marked by greater gaps in knowledge and greater difficulty with plan selection, there are some data from 2007 and 2008 to suggest that these problems persisted in later years. More data are needed from 2007-present to evaluate whether initial difficulties persisted, have been mitigated over time, or if new difficulties have arisen as the marketplace for plans, premiums, deductibles, coverage limits and offerings has shifted.31
Two gaps in understanding were particularly striking and persistent across studies and years: lack of knowledge about the coverage gap and lack of awareness of the low-income subsidy. If beneficiaries are unaware of coverage gap features, then they will make no effort to spend strategically prior to the gap or consider switching to lower cost drug alternatives and will fail to appreciate the advantage of choosing a plan that offers some gap coverage. In the years to come, if the coverage gap period remains part of the Part D benefit structure, improved education of beneficiaries is needed.
The LIS is intended to help those who are most financially vulnerable. At present, an estimated 2.5 million beneficiaries who are eligible for the LIS do not receive it.40 The Medicare Rights Center recommends providing LIS educational materials in multiple languages and at several reading levels to reach out to beneficiaries.41 Groups also advocate minimizing documentation requirements for and/or removing the asset testing process and removing the annual recertification process.42 Other initiatives are underway that may make identifying and targeting LIS-eligible beneficiaries easier. Section 113 of the “Medicare Improvements for Patients and Providers Act,” which takes effect in 2010, mandates improved cooperation between the Social Security Administration (SSA), which handles LIS enrollment, and Medicaid state offices, which administer subsidy programs to cover Medicare Part B premiums and co-payments.43 A recently proposed bill would allow the Internal Revenue Service to share financial records of potentially LIS-eligible citizens with the SSA.41
Despite beneficiaries’ well-reasoned enumeration of plan features that were important to them, they consistently failed to choose the Part D plan with the lowest cost,22, 30 had difficulty comparing plans, and often did not even compare plans at all. 21, 33, 36 Currently, the Medicare Prescription Drug Plan Finder,44 created by CMS, is the only source of comprehensive plan information. The Plan Finder requires that beneficiaries or their caregivers be comfortable with the Internet and able to sift through a vast amount of information and identify the attributes most important to them.45 Therefore, assistance from beneficiary counselors and/or enhancements to the Plan Finder would likely be helpful. In addition, given that older adults generally place most trust in their physician and pharmacists, it is important to provide these professionals with easy to use tools about comparative drug price data and plan features.46, 47
A related finding was beneficiaries’ reluctance to switch to a better plan when they were able to do so. This “inertia,” or preference to remain with the status quo, has been described in the economics literature among consumers choosing a health insurance plan48 and among employees electing to participate in 401(k) plans and allocating retirement savings.49, 50 In the Part D setting, interventions to assist beneficiaries in switching plans may help but cannot remove all barriers: while Patel et al’s intervention offered personnel with the know-how to assist beneficiaries in switching, only 45% of beneficiaries chose to do so. Some inertia may exist because of the relatively high levels of satisfaction Medicare beneficiaries report with the Part D program26 and/or beneficiary reluctance to switch out of plans picked based on brand name recognition or other personal preferences.21
In this systematic review, we assembled studies that examined beneficiaries’ knowledge of and choices with regards to Part D from 2005 to the present. We found that beneficiaries had significant gaps in knowledge, especially about the coverage gap period and the LIS. Even though beneficiaries were generally satisfied with their decisions to enroll in Part D plans, most beneficiaries chose a Part D plan that did not best meet their needs, and few expressed a desire to change their selections when given the opportunity to do so. These difficulties seemed to be most pronounced in the months surrounding the Part D implementation period in early 2006, but persist to some extent in subsequent years as well. As the Part D program continues, policymakers and Medicare advocates must monitor changes in beneficiaries’ knowledge and choices regarding Part D and determine whether improvements in educational outreach or other changes are necessary to enhance understanding and good decision making among Medicare beneficiaries.
Acknowledgments
National Institute on Aging T32 AG000158 (Ms. Polinski); National Institute of Mental Health R01 5U01MH079175-02 (Dr. Schneeweiss); National Heart Lung and Blood Institute K23 HL-090505 (Dr. Shrank)
Sponsor’s role: The sponsor had no role in the design or analysis of the study or in preparation of the manuscript.
Footnotes
Author contributions: Jennifer Polinski participated in study design, acquisition of data, analysis, and preparation of the manuscript. Aman Bhandari participated in study concept and design, acquisition of the data, and preparation of the manuscript. Uzaib Saya participated in acquisition of the data, analysis, and preparation of the manuscript. Sebastian Schneeweiss participated in the study concept and design, analysis, and preparation of the manuscript. William Shrank participated in study concept and design, acquisition of the data, analysis, and preparation of the manuscript.
Conflict of interest: Dr. Schneeweiss is a paid member of the Scientific Advisory Board of HealthCore and a consultant to HealthCore, WHISCON and RTI. Dr. Schneeweiss is Principal Investigator of the Brigham and Women’s Hospital DEcIDE Center on Comparative Effectiveness Research funded by AHRQ and of the Harvard-Brigham Drug Safety and Risk Management Research Center funded by FDA. Within the past 5 years, Dr. Schneeweiss was funded by an investigator-initiated grant from Pfizer which has ended. Dr. Shrank is the principal investigator for and has research funding from CVS/Caremark and Express Scripts. Dr. Schneeweiss is a co-investigator on and receives research funding from the CVS/Caremark grant. Opinions expressed here are only those of the authors and not necessarily those of the agencies or sponsors. These sponsors had no role in the design or analysis of the present study, nor did they participate in any way in the preparation of the paper.
References
- 1.Safran DG, Neuman P, Schoen C, et al. Prescription drug coverage and seniors: findings from a 2003 national survey. Health Aff. 2005;W5-152:W155–166. doi: 10.1377/hlthaff.w5.152. [DOI] [PubMed] [Google Scholar]
- 2.Kaiser Family Foundation. [Accessed October 7, 2008.];Prescription drug coverage among Medicare beneficiaries. 2006 Available at: http://www.kff.org/medicare/upload/7453.pdf.
- 3.Avorn J. Part “D” for “defective”--the Medicare drug-benefit chaos. N Engl J Med. 2006;354(13):1339–1341. doi: 10.1056/NEJMp068034. [DOI] [PubMed] [Google Scholar]
- 4.Dallek G. Washington Post. Dec 7, 2003. Thanks for the Medicare muddle; p. B1. [Google Scholar]
- 5.Kaiser Family Foundation. [Accessed October 7, 2008.];Medicare prescription drug plan information, by state, 2006. Available at: http://www.kff.org/medicare/upload/74261.pdf.
- 6.Hoadley J, Hargrave E, Cubanski J, Neumann P. [Accessed June 18, 2008.];The Medicare Drug Benefit: An In-Depth Examination of Formularies and Other Features of Medicare Drug Plans. Available at: http://www.kff.org/medicare/upload/7489.pdf.
- 7.Centers for Medicare and Medicaid Services. Medicare Program; Medicare Prescription Drug Benefit. Federal Register. 2005 Final Rule, 42 CFR 70, no. 18, 4460 . [Google Scholar]
- 8.Centers for Medicare and Medicaid Services. Drugs and Formulary Requirements. [Accessed September 29, 2009.];Medicare Prescription drug benefit manual: Chapter 6, Part D. 2007 Available at: http://www.healthplus.org/uploadedFiles/PDFs/Medicare/PDBMChap6FormularyReqrmts_03.09.07.pdf.
- 9.Altman DE. The new Medicare prescription-drug legislation. N Engl J Med. 2004;350(1):9–10. doi: 10.1056/NEJMp038224. [DOI] [PubMed] [Google Scholar]
- 10.Medicare Rights Center. [Accessed September 21, 2009.];Make low-income assistance more accessible. 2009 Available at: www.medicarerights.org/issues-actions/assistance.php.
- 11.Cronk A, Humphries TL, Delate T, Clark D, Morris B. Medication strategies used by Medicare beneficiaries who reach the Part D standard drug-benefit threshold. Am J Health-Syst Pharm. 2008;65(11):1062–1070. doi: 10.2146/ajhp070478. [DOI] [PubMed] [Google Scholar]
- 12.Cummings JR, Rice T, Hanoch Y. Who thinks that Part D is too complicated? Survey results on the Medicare Prescription Drug Benefit. Med Care Res Rev. 2009;66:97–115. doi: 10.1177/1077558708324340. [DOI] [PubMed] [Google Scholar]
- 13.Dulio A, Perry M, Cubanski J. [Accessed: August 10, 2009];Voices of beneficiaries: attitudes toward Medicare Part D open enrollment for 2008. Available at: http://www.kff.org/medicare/upload/7722.pdf.
- 14.Goedken AM, Urmie JM, Farris KB, Doucette WR. Effect of cost sharing on prescription drug use by Medicare beneficiaries prior to the Medicare Drug Benefit and potential adverse selection in the benefit. JAPhA. 2009;49(1):18–25. doi: 10.1331/JAPhA.2009.08001. [DOI] [PubMed] [Google Scholar]
- 15.Hall JP, Kurth NK, Moore JM. Transition to Medicare Part D: an early snapshot of barriers experienced by younger dual eligibles with disabilities. Am J Manag Care. 2007;13(1):14–18. [PubMed] [Google Scholar]
- 16.Hsu J, Fung V, Price M, et al. Medicare beneficiaries’ knowledge of Part D prescription drug program benefits and responses to drug costs. JAMA. 2008;299(16):1929–1936. doi: 10.1001/jama.299.16.1929. [DOI] [PubMed] [Google Scholar]
- 17.Kaiser Family Foundation. [Accessed August 10, 2009.];Profiles of Medicare beneficiaries with Medicaid drug coverage prior to the Medicare drug benefit. 2005 Available at: http://www.kff.org/medicaid/upload/Profiles-of-Medicare-Beneficiaries-With-Medicaid-Drug-Coverage-Prior-to-the-Medicare-Drug-Benefit-December-2005.pdf.
- 18.Keenan TA. [Accessed August 10, 2009.];Prescription drugs and Medicare Part D: a report on access, satisfaction, and cost. 2007 Available at: http://assets.aarp.org/rgcenter/health/rx_medicared.pdf.
- 19.Summer L, Nemore P, Finberg J. [Accessed August 10, 2009. .];Medicare Part D: how do vulnerable beneficiaries fare? 2008 Available at: http://www.commonwealthfund.org/usr_doc/Summer_McarePartDhowdovulnbeneficiariesfare_1127_ib.pdf?section=4039. [PubMed]
- 20.Winter J, Balza R, Caro F, et al. Medicare prescription drug coverage: consumer information and preferences. Proc Natl Acad Sci USA. 2006;103(20):7929–7934. doi: 10.1073/pnas.0601837103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cubanski J, Neuman P. Status report on Medicare Part D enrollment in 2006: analysis of plan-specific market share and coverage. Health Aff. 2007;26(1):w1–12. doi: 10.1377/hlthaff.26.1.w1. [DOI] [PubMed] [Google Scholar]
- 22.Gruber J. [Accessed August 10, 2009];Choosing a Medicare Part D plan: are Medicare beneficiaries choosing low-cost plans? 2009 Available at: http://www.kff.org/medicare/upload/7504.pdf.
- 23.Heiss F, McFadden D, Winter J. [Accessed August 10, 2009.];Mind the gap! Consumer perceptions and choices of Medicare Part D prescription drug plans. 2007 Available at: www.nber.org/papers/w13627.
- 24.Jackson EA, Axelsen KJ. Medicare Part D formulary coverage since program inception: are beneficiaries choosing wisely? Am J Manag Care. 2008;14(11 Suppl):SP29–35. [PubMed] [Google Scholar]
- 25.Keenan TA. [Accessed August 10, 2009.];Prescriptions for the future: medications, Medicare Part D and managing expenses in a difficult economy. 2007 Available at: http://assets.aarp.org/rgcenter/health/rx_future_08.pdf.
- 26.Levy H, Weir DR. [Accessed August 10, 2009.];Take-up of Medicare Part D and the SSA subsidy: early results from the health and retirement study. 2007 doi: 10.1093/geronb/gbp107. Available at: http://www.mrrc.isr.umich.edu/publications/papers/pdf/wp163.pdf. [DOI] [PMC free article] [PubMed]
- 27.McBride TD, Terry TT, Mueller KJ. Medicare Part D: early findings on enrollment and choices for rural beneficiaries. [Accessed August 10, 2009.];Rural Policy Brief. 2006 Available at: http://www.unmc.edu/ruprihealth/Pubs/Medicare_Part_D_brief.pdf. [PubMed]
- 28.McNerney T. [Accessed August 10, 2009.];A new WSJ.com/Harris Interactive study finds that a large majority of seniors are satisfied with Medicare drug plans. 2007 Available at: http://www.harrisinteractive.com/news/newsletters/wsjhealthnews/HI_WSJ_HealthCarePoll_2008_v07_i01.pdf.
- 29.Neuman P, Strollo MK, Guterman S, et al. Medicare prescription drug benefit progress report: findings from a 2006 national survey of seniors. Health Aff. 2007;26(5):w630–643. doi: 10.1377/hlthaff.26.5.w630. [DOI] [PubMed] [Google Scholar]
- 30.Patel RA, Lipton HL, Cutler TW, Smith A, Tsunoda SM, Stebbins MR. Cost minimization of Medicare Part D prescription drug plan expenditures. Am J Manag Care. 2009;15(8):545–553. [PubMed] [Google Scholar]
- 31.Neuman P, Cubanski J. Medicare Part D update--lessons learned and unfinished business. N Engl J Med. 2009;361(4):406–414. doi: 10.1056/NEJMhpr0809949. [DOI] [PubMed] [Google Scholar]
- 32.DeNatale ML. Understanding the Medicare Part D prescription program: partnerships for beneficiaries and health care professionals. Policy Polit Nurs Pract. 2007;8(3):170–181. doi: 10.1177/1527154407309048. [DOI] [PubMed] [Google Scholar]
- 33.Dulio A, Perry M, Cubanski J. [Accessed August 10, 2009.];Voices of beneficiaries: early experiences with the Medicare drug benefit. 2006 Available at: http://www.kff.org/medicare/upload/7504.pdf.
- 34.Hargrave E, Piya B, Hoadley J, Summer L, Thompson J. [Accessed August 10, 2009.];Experiences obtaining drugs under Part D: focus groups with beneficiaries, physicians, and pharmacists. 2008 Available at: http://www.medpac.gov/documents/May08_PartDFocusGroup_CONTRACTOR_JS.pdf.
- 35.Heiss F, McFadden D, Winter J. Who failed to enroll in Medicare Part D, and why? Early results. Health Aff. 2006;25(5):w344–354. doi: 10.1377/hlthaff.25.w344. [DOI] [PubMed] [Google Scholar]
- 36.Hibbard J, Greene J, Tusler M. [Accessed August 10, 2009.];An assessment of beneficiary knowledge of Medicare coverage options and the prescription drug benefit. 2006 Available at: http://assets.aarp.org/rgcenter/health/2006_12_medicare.pdf.
- 37.Perry M, Dulio A, Cubanski J. [Accessed August 10, 2009.];Voices of beneficiaries: Medicare Part D insights and observations one year later. 2006 Available at: http://www.kff.org/medicare/upload/7605.pdf.
- 38.Skarupski KA, Mendes de Leon CF, Barnes LL, Evans DA. Medicare Part D enrollment in a biracial community-based population of older adults. Gerontologist. 2009:1–11. doi: 10.1093/geront/gnp055. epub ahead of print, June 16, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Keenan TA. [Accessed August 10, 2009.];Experiences with Medicare Part D among enrollees and non-enrollees. 2006 Available at: http://assets.aarp.org/rgcenter/health/medicare_part_d.pdf.
- 40.Centers for Medicare and Medicaid Services. [Accessed October 1, 2009.];Enrollment information. 2009 February 1; 2009. Available at: www.cms.hhs.gov/PrescriptionDrugCovGenIn/
- 41.Medicare Rights Center. Letter of support for Sen. [Accessed October 1, 2009.];Bingaman’s bill. 2009 May 18; Available at: http://www.medicarerights.org/pdf/Letter-of-support-for-Sen-Bingaman-bill-May-2009.pdf.
- 42.Medicare Rights Center. [Accessed October 1, 2009.];Letter to House about Medicare Savings Programs and the Low Income Subsidy. 2009 May 28; Available at: http://www.medicarerights.org/pdf/MSP-LIS-letter-to-House-May-2009.pdf.
- 43.GovTrack.us. [Accessed October 1, 2009.];Text of H.R. 6331 [110th]: Medicare Improvements for Patients and Providers Act of 2008. Available at: http://www.govtrack.us/congress/billtext.xpd?bill=h110-6331&version=enr&nid=t0%3Aenr%3A242.
- 44.Centers for Medicare and Medicaid Services. [Accessed September 21, 2009.];Medicare Prescription Drug Plan Finder. 2009 Available at: http://www.medicare.gov/MPDPF/Public/Include/DataSection/Questions/SearchOptions.asp.
- 45.Minott J. [Accessed October 1, 2009.];Getting tools used: lessons learned from successful decision support tools unrelated to health care. 2009 Available at: http://www.hcfo.net/pdf/findings0709.pdf. [PubMed]
- 46.Donohue JM, Fischer MA, Huskamp HA, Weissman JS. Potential savings from an evidence-based consumer-oriented public education campaign on prescription drugs. Health Serv Res. 2008;43(5):1557–1575. doi: 10.1111/j.1475-6773.2008.00858.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Donohue JM, Huskamp HA, Wilson IA, Weissman JS. Whom do older adults trust most to provide information about prescription drugs? Am J Geriatr Pharmacother. 2009;7(2):105–116. doi: 10.1016/j.amjopharm.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Marquis MS, Holmer MR. Alternative models of choice under uncertainty and demand for health insurance. Rev Econ Stat. 1996;78(3):421–427. [Google Scholar]
- 49.Madrian BC, Shea DF. The power of suggestion: inertia in 401(k) participation and savings behavior. Quart J Econ. 2001;116(4):1149–1187. [Google Scholar]
- 50.Choi J, Laibson D, Madrian B, Metrick A. For better or for worse: default effects and 401(k) savings behavior. In: Wise D, editor. Perspectives in the economics of aging. Chicago, IL: University of Chicago Press; 2004. pp. 81–121. [Google Scholar]


