Abstract
Background
The efficacy of using diffuse near infrared spectroscopy (NIRS) in predicting wound healing in diabetic foot ulcers was demonstrated by conducting a pilot human study.
Method
Sixteen chronic diabetic wounds were followed and assessed for subsurface oxyhemoglobin concentration using the NIRS device. Weekly measurements were conducted until there was wound closure, limb amputation, or 20 completed visits without healing. Wound size and degree of wound contraction were measured by image analysis of digital photographs, and results were compared to NIRS results.
Results
In the 16 patients followed, seven wounds healed, six limbs were amputated, and three wounds remained opened after 20 visits. Initial values of subsurface hemoglobin concentration, in all wounds, were higher than in nonwound control sites. Healed wounds exhibited a consistent reduction of hemoglobin concentration several weeks prior to closure, and the absolute hemoglobin concentration approached the value at the control site. In wounds that did not heal or ended in amputations, the hemoglobin concentration remained elevated throughout the study. A negative slope for the rate of change of hemoglobin concentration was indicative of healing across all wounds.
Conclusions
Evaluation of diabetic foot ulcers using NIRS may provide an effective and more complete measurement of wound healing compared to current clinical approaches.
Keywords: chronic diabetic foot ulcers, diffuse photon density wave, frequency-domain near infrared spectroscopy, hemoglobin, wound healing
Introduction
Diabetic foot ulcers are a growing problem as the prevalence of diabetes increases worldwide. In diabetes patients, vascular disease and neuropathy in the lower limbs lead to the formation of chronic ulcers from what is often initially a minor trauma. It is estimated that 15% of diabetes patients will develop an ulcer of the feet or ankles some time during their disease course, and approximately 14% of diabetic ulcers lead to amputation.1 It is also estimated that diabetic foot ulcers are the underlying cause of 85% of all nontraumatic amputations.2 Mortality during the 5-year period following amputation ranges from 39 to 80%,2 and the health-related quality of life of patients with chronic neuropathic foot ulcers is poor and comparable with quality of life in patients with recurrent cancer.3
A wide variety of advanced treatments for diabetic foot ulcers, such as topical growth factors, bioengineered skin equivalents, negative pressure wound therapy, and hyperbaric oxygen therapy, are available commercially, and clinical studies of these products have shown some evidence of improved healing compared to standard of care.4 However, the effectiveness of each treatment is not the same in all patients. For example, evidence shows that growth factors and cell therapies improve healing in diabetic neuropathic foot ulcers compared to standard care; however, only roughly 30–50% of patients who received these treatments healed by 12–20 weeks of care.5 Clinicians often need to try several different treatment options before finding one that is effective for a particular wound. During the prolonged healing process of a chronic wound, rapid and accurate evaluation of the healing progress is critical so that unsuccessful treatments can be discontinued and alternate treatments be initiated as soon as possible.6,7 Hence, there is a need to develop noninvasive technologies that would enable improved diagnosis of chronic wounds and allow reduction of the currently high cost of treatment.
Diffuse photon density wave (DPDW) methodology of near infrared spectroscopy (NIRS) can be used to measure the absolute concentrations of oxyhemoglobin and deoxyhemoglobin in tissue at depths of up to several centimeters8 and therefore may provide clinicians with valuable information to supplement traditional wound assessment methodologies that consist primarily of wound surface assessment. Our laboratory has demonstrated previously that changes in wound optical properties in an animal model of acute wounds could be quantified using DPDW and that these changes corresponded to changes in wound vascularization and oxygenation.9,10 These animal studies led us to development of a model of the expected behavior of hemoglobin concentration during the course of healing. Results from independent animal studies demonstrate that optical absorption coefficients increase compared to established prewound baseline values and later return to the prewound baseline condition after healing is complete. The clinical success of any optical device would depend on the validity of this hypothesis in human studies. In a human study, patients present with existing open wounds. Therefore, we do not have baseline measurements in a human study. In this case, tissue changes due to wound healing will be manifested by changes in optical properties and hemoglobin concentrations, while the absence of any dynamic change would correspond to nonhealing wounds. This article reports on results of a pilot human study in which chronic diabetic foot ulcers were monitored over the course of several weeks using DPDW methodology of NIRS.
Methods
Details of the frequency domain near infrared instrument have been described previously.9,10 Briefly, one optical fiber was used to deliver intensity modulated light (70 MHz) to the tissue from three diode lasers (λ = 685, 780, and 830). Four optical fibers were used to deliver backscattered light from the tissue to the instrument. A Teflon probe was used to hold the fibers in place, with the four detector fibers at fixed distances (ρ = 4, 8, 12, and 16 mm) from the source fiber. Using diffusion approximation, optical absorption and reduced scattering coefficients (μa and μ’s) were calculated from the amplitude and phase shift of backscattered light at each detector position.10 Values of oxyhemoglobin concentration (HbO2) and deoxyhemo-globin concentration (Hhb) were calculated from the optical absorption coefficients at each wavelength.9 Total hemo-globin concentration (Tot Hb) was calculated as the sum of HbO2 and Hhb.
Sixteen patients with diabetic foot ulcers were enrolled in the study. All subjects were between the ages of 30 to 65. All patients had a previous documented history of diabetes mellitus for at least 6 months. Areas evaluated were strictly ankle and foot wounds secondary to complications from diabetes that presented with a minimum surface area of 1 cm2 . Patients were only enrolled in the study if the ankle–brachial index was >0.75, indicating adequate blood supply to the wounded limb. All wounds were debrided of necrotic tissue before entering into the study. Patients diagnosed with osteomyelitis had excision of the infected bone and treatment with antibiotics before enrollment. Each of the 16 patients underwent a standard wound care routine for their foot ulcers, which consisted of weekly or biweekly debridement, offloading when possible, and treatment with moist wound-healing protocols. When indicated, active wound-healing modalities such as hyperbaric oxygen, negative pressure wound healing, and active biosynthetic skin substitutes were used.
Optical measurements were performed prior to weekly or biweekly debridement. Serial measurements were obtained at every patient visit to the clinic from the time of enrollment until complete wound closure, amputation of the limb, or a maximum of 20 visits without closure or amputation. A wound was classified as “nonhealing” for the purposes of this study if it did not heal by the 20th visit or if the limb was amputated. Optical measurements of the wound tissue were conducted at various sites, depending on the geometry and location of each wound. Locations measured included the area directly on the wound (1), intact skin at the edge of the wound (2), nonwound tissue on the wounded limb at a distance of at least 2 cm from the wound (3), and nonwound tissue on the contralateral limb as symmetric to the wound location as possible (4). The control site chosen varied between a location on the wounded or contralateral limb, depending on access to the site due to other wounds or previous amputations. Tegaderm transparent sterile dressing (3M Health Care, St. Paul, MN) was used to cover the fiber optic probe during all measurements. The near infrared device was configured to complete one measurement in approximately 3 seconds, and at all measurement locations the probe was held in continuous contact with the wound or skin tissue until 8–10 successive measurements were obtained over a period of approximately 30 seconds. Patients were asked to avoid moving the limb during each measurement period.
During every visit, a digital photograph of the wound was obtained after near infrared data were collected. Cross-polarizing filters were used on the digital camera to reduce surface reflections. A paper ruler was used in each photograph to correct for variations in the distance between the camera and the wound. Wound surface area was calculated by tracing the wound boundary and using an image analysis program created with MATLAB computing software (MathWorks, Inc., Natick, MA).
Results
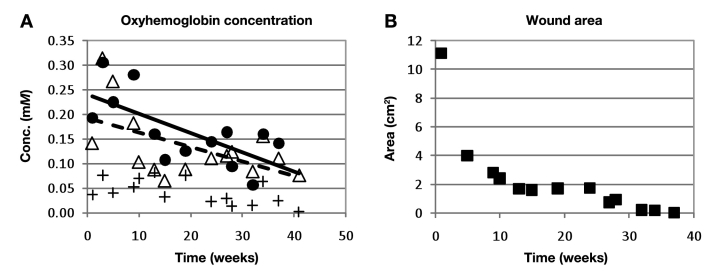
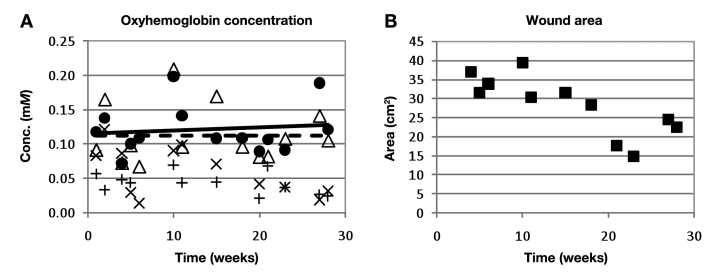
Of the 16 wounds studied, 7 wounds healed completely (to full closure) and 9 wounds remained unhealed or resulted in amputation. In both healing and nonhealing wounds, the HbO2 concentration and the Tot Hb concentration during the initial measurement session were higher at the wound center and wound edges than at the control sites. In the 7 wounds that healed, wound measurements of HbO2 and Tot Hb decreased gradually over time and converged with control site values of HbO2 and Tot Hb. An example of data obtained from a healing wound is given in Figure 1. In the 9 nonhealing wounds, HbO2 and Tot Hb at the wound sites remained elevated throughout the duration of the study and did not converge with control site values. An example of data obtained from a nonhealing wound is given in Figure 2.
Figure 1.
Example of data obtained from a healing wound that closed after 41 weeks. (A) Oxyhemoglobin concentration as measured by the near infrared device at the wound center (•), wound edge (Δ), and control site on the same limb as the wound (+). The solid line is the linear trend line associated with data obtained from the wound center (slope = –3.9 μM/week); the dashed line is the linear trend line associated with data obtained from the wound edge (slope = –2.9 μM/week). The slopes of both trend lines are negative, as is characteristic of the healing wounds in this study. (B) Wound sizes measured on each day.
Figure 2.
Example of data obtained from a nonhealing wound that resulted in amputation of the limb after 28 weeks of participation in the study. (A) Oxyhemoglobin concentration as measured by the near infrared device at the wound center (•), wound edge (Δ), control site on the same limb as the wound (+), and control site on the contralateral limb (×). The solid line is the linear trend line associated with data obtained from the wound center (slope = 0.4 μM/week); the dashed line is the linear trend line associated with data obtained from the wound edge (slope = 0.0 μM/week). The slopes of both trend lines are nearly zero or slightly positive, as is characteristic of the nonhealing wounds in this study. (B) Wound sizes measured on each day.
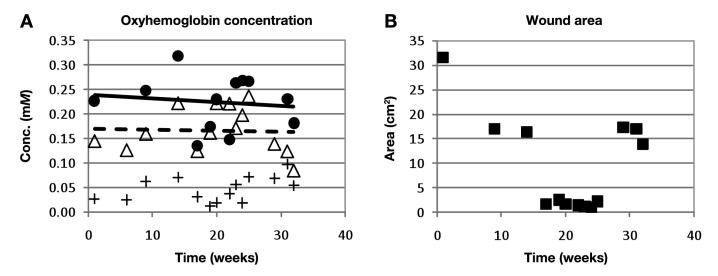
Figure 3 shows results from a wound that appeared to be healing by clinical standards (i.e., a rapid decrease in wound size). However, the rate of change in HbO2 was not converging with the control as is typical of nonhealing wounds. Although the wound size decreased sharply by week 18, it never closed and required major debridement after week 25. In this case, near infrared HbO2 measurements reflected the outcome of the wound more accurately and earlier than measurements of wound size.
Figure 3.
Example of data obtained from a wound that was classified as nonhealing by near infrared measurements despite a sharp decrease in wound size. Ultimately, the wound required major debridement and ultimately resulted in amputation. (A) Oxyhemoglobin concentration as measured by the near infrared device at the wound center (•), wound edge (Δ), and control site on the same limb as the wound (+). The solid line is the linear trend line associated with data obtained from the wound center (slope = –0.8 μM/week); the dashed line is the linear trend line associated with data obtained from the wound edge (slope = –0.2 μM/week). The slopes of both trend lines are nearly zero or slightly positive, as is characteristic of the nonhealing wounds in this study. (B) Wound sizes measured on each day. A major debridement was performed prior to week 29, causing the observed increase in wound size.
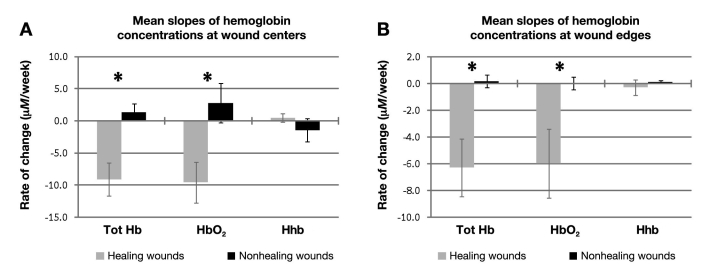
Rates of change in hemoglobin concentration over time were quantified by fitting a linear trend line to the measured values. The HbO2 and Tot Hb slopes for all healing wounds were negative, whereas the slopes of nonhealing wounds were nearly zero or slightly positive. The mean and standard errors of slopes obtained from healing and nonhealing wounds are compared in Figure 4. Healing and nonhealing groups were compared using two-tailed heteroscedastic t tests, and a significant difference was found between the HbO2 and the Tot Hb slopes of healed and nonhealing wounds (p < 0.05).
Figure 4.
Mean ± standard error of the temporal slopes of total, oxy-, and deoxyhemoglobin concentration for healing and nonhealing wounds measured at (A) centers of wounds and (B) edges of wounds. A significant difference was found between HbO2 and Tot Hb slopes of healed and nonhealing wounds (*p < 0.05, two-tailed heteroscedastic t tests).
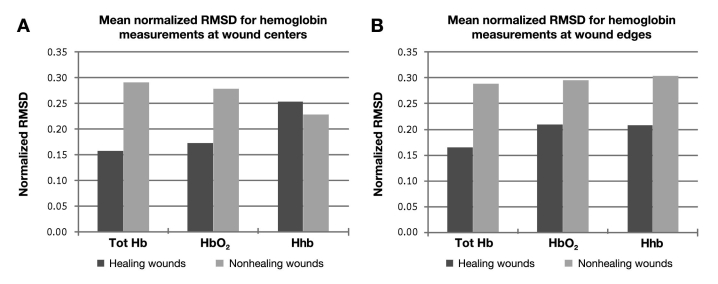
In addition to the rate of change of hemoglobin concentration, the week-to-week variability in optical data from a wound may provide an indicator of its healing potential. To quantify week-to-week variability in optical data from each wound, the root mean square deviation (RMSD) of measured data points from the hemoglobin trend line was calculated using the following equation:
| (1) |
where n is the number of measurements obtained from a wound, xi,meas are measured values, and xi,fit are values predicted by the linear trend line fitted to measured values. The RMSD values were normalized by dividing by the mean of the measured values obtained for each wound. Figure 5 shows that the mean normalized RMSD was greater in nonhealing wounds than in healing wounds for all hemoglobin concentrations (oxy-, deoxy-, and total hemoglobin).
Figure 5.
Normalized RMSD of trend lines fitted to hemoglobin concentration measured at (A) centers of wounds and (B) edges of wounds.
Discussion
Results suggest that healing diabetic foot ulcers can be distinguished from nonhealing ulcers by measuring changes in hemoglobin concentration noninvasively with DPDW methodology of NIRS. It may be possible to use the rate of change of HbO2 concentration to predict whether or not a wound will heal. Using all of the HbO2 slopes acquired from the center of wounds in this study, healing wounds can be separated from nonhealing wounds by selecting a threshold of –3 μM/week (i.e., all wounds with an HbO2 slope less than –3 μM/week were classified as healing wounds, whereas all wounds with an HbO2 slope greater than this threshold were classified as nonhealing wounds). In a clinical environment, it will be necessary to be able to predict healing before the end points of this study are reached. An accurate assessment of the capability of the HbO2 slopes over time to predict healing or nonhealing would need to be determined through a study of more patients with measurements taken at more time points. However, as a first approximation, the HbO2 slope for each wound was calculated by fitting data from the first 10 weeks of NIR measurements to a linear trend line. Table 1 shows the number and percentage of healing and nonhealing wounds from this study that would have been classified correctly for two different threshold levels. It is clear that more data are needed to allow one to determine the threshold value of the slope that will distinguish healing from nonhealing wounds. It is likely that the period of time needed to establish a predictive trend could be reduced if measurements were conducted more frequently. The average number of measurements obtained during each subject’s first 10 weeks in our study was 4.4. We chose to evaluate trends using 10 weeks of data because four to five measurements appear to be adequate to establish a statistically reliable trend line. If measurements were conducted every week in a future near infrared study, we believe that it would be possible to establish a predictive trend line in 5 weeks or less.
Table 1.
Prediction Capability of [HbO2] Slopes at the Center of Wounds for Two Different Thresholdsa
| Amount of data used in trend line calculations | Threshold (μM/week) | Healing wounds classified correctly | Nonhealing wounds classified correctly |
|---|---|---|---|
| All weeks | −3 | 6 of 6 (100%) | 8 of 8 (100%) |
| All weeks | −6 | 4 of 6 (67%) | 8 of 8 (100%) |
| First 10 weeks | −3 | 5 of 6 (83%) | 5 of 8 (63%) |
| First 10 weeks | −6 | 4 of 6 (67%) | 8 of 8 (100%) |
Data from only six of seven healing wounds and eight of nine nonhealing wounds are shown because the size and shape of one wound from each group prevented measurements at the wound center.
There are three interrelated and overlapping phases of wound healing: first an inflammatory phase; then a proliferative phase, which is characterized by increased cell growth and angiogenesis; and finally a remodeling phase in which collagen is deposited and organized to form scar tissue.11 During the late inflammatory/early proliferation stage of wound healing, angiogenesis increases the supply of oxygenated blood to the wound, resulting in increased levels of HbO2. In the late proliferation stage, angiogenesis stops and blood vessels begin to break down as a result of apoptosis.12 The decreasing levels of HbO2 concentration over time seen in healing wounds in this study may be correlated with a decrease in blood vessel density that occurs during the late proliferative stage of wound healing. Concentrations of deoxygenated hemoglobin reflect metabolic activity within the wound bed and would be expected to remain relatively constant, assuming that an adequate supply of oxygenated blood is being delivered to the wound. This could explain why the changes in Hhb in healing wounds were less pronounced than changes in HbO2.
It has been hypothesized that chronic nonhealing diabetic wounds may be “stuck” in various phases of the healing process.13 The nonhealing wounds observed in this study may have been “arrested” before reaching the end of the proliferative phase of healing, resulting in oxygenated hemoglobin concentrations that did not decrease like healing wounds. Furthermore, evidence shows that a prolonged inflammatory response in diabetes patients is an important factor in the etiology of diabetic foot ulcers.13,14 It has been hypothesized that repeated ischemia and reperfusion within the microvasculature of the foot may lead to cycles of inflammation in foot ulcers that impair the wound-healing process.15 The high degree of week-to-week variability in nonhealing wounds compared to healing wounds shown in Figure 5 supports this hypothesis and could be an indication of cyclical inflammation in these wounds.
Conclusions
Results indicate that temporal changes in the concentration of hemoglobin derived from diffuse near infrared measurements of the optical absorption coefficient in diabetic foot ulcers can be used to monitor the healing progress. The linear rate of change of hemoglobin concentration over time was used to differentiate healing from nonhealing wounds in a study of human diabetic foot ulcers, indicating that this method may be able to help wound care clinicians in the assessment of overall wound health when treating diabetic foot ulcers.
Abbreviations
- DPDW
diffuse photon density wave
- HbO2
oxyhemoglobin
- Hhb
deoxyhemoglobin
- NIRS
near infrared spectroscopy
- RMSD
root mean square deviation
- Tot Hb
total hemoglobin
References
- 1.Reiber GE, Lipsky BA, Gibbons GW. The burden of diabetic foot ulcers. Am J Surg. 1998;176(2A Suppl):5S–10S. doi: 10.1016/s0002-9610(98)00181-0. [DOI] [PubMed] [Google Scholar]
- 2.Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293(2):217–228. doi: 10.1001/jama.293.2.217. [DOI] [PubMed] [Google Scholar]
- 3.Nabuurs-Franssen MH, Huijberts MS, Nieuwenhuijzen Kruseman AC, Willems J, Schaper NC. Health-related quality of life of diabetic foot ulcer patients and their caregivers. Diabetologia. 2005;48(9):1906–1910. doi: 10.1007/s00125-005-1856-6. [DOI] [PubMed] [Google Scholar]
- 4.Sibbald RG, Orsted HL, Coutts PM, Keast DH. Best practice recommendations for preparing the wound bed: update 2006. Adv Skin Wound Care. 2007;20(7):390–405. doi: 10.1097/01.ASW.0000280200.65883.fd. [DOI] [PubMed] [Google Scholar]
- 5.Margolis DJ, Allen-Taylor L, Hoffstad O, Berlin JA. Diabetic neuropathic foot ulcers: the association of wound size, wound duration, and wound grade on healing. Diabetes Care. 2002;25(10):1835–1839. doi: 10.2337/diacare.25.10.1835. [DOI] [PubMed] [Google Scholar]
- 6.Goldman RJ, Salcido R. More than one way to measure a wound: an overview of tools and techniques. Adv Skin Wound Care. 2002;15(5):236–243. doi: 10.1097/00129334-200209000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Jessup RL. What is the best method for assessing the rate of wound healing? A comparison of 3 mathematical formulas. Adv Skin Wound Care. 2006;19(3):138–146. doi: 10.1097/00129334-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Mobley J, Vo-Dinh T. Biomedical photonics handbook. Boca Raton, FL: CRC Press; 2003. Optical properties of tissue. [Google Scholar]
- 9.Papazoglou ES, Weingarten MS, Zubkov L, Neidrauer M, Zhu L, Tyagi S, Pourrezaei K. Changes in optical properties of tissue during acute wound healing in an animal model. J Biomed Optics. 2008;13:044005. doi: 10.1117/1.2960952. [DOI] [PubMed] [Google Scholar]
- 10.Papazoglou ES, Weingarten MS, Zubkov L, Zhu L, Tyagi S, Pourrezaei K. Optical properties of wounds: diabetic versus healthy tissue. IEEE Trans Biomed Eng. 2006;53(6):1047–1055. doi: 10.1109/TBME.2006.873541. [DOI] [PubMed] [Google Scholar]
- 11.Witte MB, Barbul A. General principles of wound healing. Surg Clin North Am. 1997;77(3):509–528. doi: 10.1016/s0039-6109(05)70566-1. [DOI] [PubMed] [Google Scholar]
- 12.Singer AJ, Clark RA. Cutaneous wound healing. N Engl J Med. 1999;341(10):738–746. doi: 10.1056/NEJM199909023411006. [DOI] [PubMed] [Google Scholar]
- 13.Falanga V. Wound healing and its impairment in the diabetic foot. Lancet. 2005;366(9498):1736–1743. doi: 10.1016/S0140-6736(05)67700-8. [DOI] [PubMed] [Google Scholar]
- 14.Loots MA, Lamme EN, Zeegelaar J, Mekkes JR, Bos JD, Middelkoop E. Differences in cellular infiltrate and extracellular matrix of chronic diabetic and venous ulcers versus acute wounds. J Invest Dermatol. 1998;111(5):850–857. doi: 10.1046/j.1523-1747.1998.00381.x. [DOI] [PubMed] [Google Scholar]
- 15.Mustoe TA, O’Shaughnessy K, Kloeters O. Chronic wound pathogenesis and current treatment strategies: a unifying hypothesis. Plast Reconstr Surg. 2006;117(7 Suppl):35S–41S. doi: 10.1097/01.prs.0000225431.63010.1b. [DOI] [PubMed] [Google Scholar]