Abstract
Purpose
Management of end stage rheumatoid wrist disease remains controversial. Total wrist fusion (TWF) provides reliable pain relief and stability and is the most commonly applied management strategy. Total wrist arthroplasty (TWA) is a motion-preserving alternative that is gaining popularity. The purpose of this study is to perform a cost–utility analysis comparing non-operative management, TWA and TWF for the rheumatoid wrist
Methods
A time trade-off utility survey was developed to investigate patient and physician preferences for the potential outcomes of TWA and TWF. The study sample consisted of rheumatoid patients (N=49) recruited as part of an ongoing prospective study as well as a national random sample of hand surgeons and rheumatologists (N=109). A decision tree was created using utility values derived from the survey, and the expected quality-adjusted-life-years (QALYs) for each procedure were determined. Using the societal perspective, costs were based on the Medicare fee schedules for the CPT codes associated with TWA and TWF and their potential complications. Costs per QALY were calculated and compared.
Results
Patients and physicians both showed a preference for operative management over non-operative management. Application of cost data indicated that the incremental cost per additional QALY gained for TWA over non-operative management was $2,281 and the incremental cost per QALY gained with TWA over TWF was $2,328 which is substantially less than the national standard of $50,000/QALY deemed acceptable for adoption.
Conclusions
In the absence of rigorous outcome data, cost-utility analysis is a useful tool to guide treatment decisions. TWA and TWF are both extremely cost-effective procedures. This study incorporated patient and physician utilities to demonstrate that TWA has only a small incremental cost over the traditional TWF procedure. Based on this economic model, TWA may be worthy of further consideration and cost should not be considered prohibitive.
Keywords: cost-utility analysis, wrist fusion, wrist arthroplasty
Introduction
The role of total wrist arthroplasty (TWA) in the management of rheumatoid wrist disease remains controversial. TWA was introduced over four decades ago as a motion-preserving alternative to total wrist fusion (TWF). Although prostheses have improved across the three generations of design, TWA has failed to achieve the same widespread application when compared with other total joint arthroplasty procedures. Proposed reasons for infrequent application include physician and patient concern about high complication and failure rates for TWA as well as the potentially higher cost for TWA compared to TWF.
A recent systematic review of the literature for TWA and TWF in rheumatoid arthritis highlights the lack of prospective data to compare the procedures.(1) In the absence of rigorous outcomes data, the decision to pursue TWA or TWF relies on patient and physician preferences for the expected outcome of each procedure. To further evaluate these preferences, we developed a decision analytic model of TWA and TWF compared to non-operative management of the rheumatoid wrist. Decision analysis is a technique for assessing the utility, or value, associated with potential treatment options, including surgical interventions.(2–5) The output of a decision analytic model is a calculation of the expected quality adjusted life years, or QALYs, gained with each treatment option.
QALYs take into account gains in both quality and quantity of life and allow side- by-side comparison of treatments as different as carpal tunnel release,(6) inguinal hernia repair,(7) and breast reconstruction.(8) Cost per QALY can therefore be applied in setting priorities in healthcare spending. Historically, a cost of $50,000 or less per QALY has been considered an acceptable amount. However, more recent estimates set this level much higher, approximately $100,000 per QALY.(9) The purpose of this study is to apply utility data from rheumatoid patients and a national random sample of hand surgeons and rheumatologists in a cost utility analysis of TWA and TWF compared to non-operative management for rheumatoid wrist disease.
Materials and Methods
Study Design
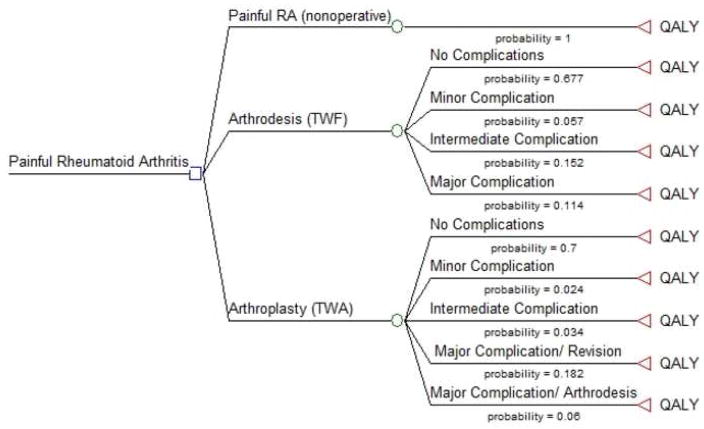
The basic decision analytic model is presented in Figure 1. This model addresses the three possible management options for the severely destroyed RA wrist: 1) non-operative management, 2) TWF, and 3) TWA. By convention, a decision node is shown as a square, a chance node is shown as a circle, and an outcome or terminal node is shown as a triangle. The model includes the potential complications associated with TWF and TWA leaving ten possible terminal outcomes. The probability of each outcome is derived from a systematic review of the literature with complications further stratified to include minor, intermediate and major categories.(1) Examples of minor complications include superficial wound infection treated with oral antibiotics and superficial wound breakdown treated with dressing changes. Examples of intermediate complications include a hematoma requiring evacuation and symptomatic hardware for TWF requiring removal. Major complications include conditions such as nonunion of a TWF and loosening of a wrist prosthesis requiring either prosthesis removal and replacement, or prosthesis removal and salvage arthrodesis using an iliac crest bone graft. Utility values used in the model are derived from patient and physician responses to our utility survey as described below.
Figure 1.
Basic decision tree model used for cost-utility analysis. The probability of each complication was derived from a prior systematic review of the literature.
Assumptions of the model include each patient proceeding through the decision tree with a single outcome. Patients can experience up to one complication and each complication fully resolves with appropriate treatment. Because no well-established long-term data are available on the longevity of currently available total wrist prostheses, we assume that prostheses are durable enough to last the duration of the patient’s life and explore the cost implications of varying patient lifespan in a sensitivity analysis. We also consider the cost implications of failed wrist prostheses requiring replacement or salvage arthrodesis. This model does not address all possible patient outcomes because the published literature does not include sufficient patient numbers or long-term follow-up to establish a more comprehensive outcome profile. However, this basic cost-utility model allows for assessment of baseline costs and the costs of complications currently reported in the literature. Determining the cost-utility of TWA compared to TWF and non-operative management provides an estimate of the anticipated costs and helps us to evaluate if one treatment is overwhelmingly more cost-effective.
Perspective
Perspective is the viewpoint used in a cost-effectiveness analysis. The Panel on Cost-Effectiveness in Health and Medicine recommends use of the societal perspective.(10) This perspective allows calculation of the costs experienced by society in general, rather than focusing on the costs experienced by the patient or physician. Cost calculations in our analysis reflect the societal perspective and are based on Medicare fee schedules as described below. Because cost structures vary amongst hospitals and healthcare systems, the use of the national standard of the Medicare fee structure gives generalizability to this model.
Utility Survey
Utility is defined as preference for a given state of health or disease relative to perfect health or death. By convention, a utility value of 1 represents perfect health whereas a utility value of 0 represents death.(11) Utility can be measured using direct or indirect methods. Indirect methods include validated general health questionnaires and disease-specific questionnaires administered to patients experiencing the health state under investigation. Patient responses are then converted to utility values using various scales or formulas. Direct assessment methods include tools such as visual analog scales, time trade-off (TTO), and standard gamble (SG) that directly assess preferences for specific health and disease states. TTO requires the respondent to determine the number of years in a compromised health state that he/she will be willing to trade for fewer years of life in a more favorable health state. Standard gamble asks the respondent to choose between living for a guaranteed number of years in a compromised health state and a gamble that would result in either perfect health or immediate death. In a TTO survey, the respondent compares years in one health state versus another (for example 15 years of life with blindness = 10 years of life with normal vision) whereas in a SG, the respondent decides the odds he/she is willing to risk for a more favorable health state (for example 15 years of life with blindness traded for a gamble in which the odds are 1/100,000 risk of immediate death and 99,999/100,000 chance for life with normal vision). In TTO the number of years varies and in SG the odds of the gamble varies. Initial pilot testing suggested TTO was easier for our respondents to understand than SG.
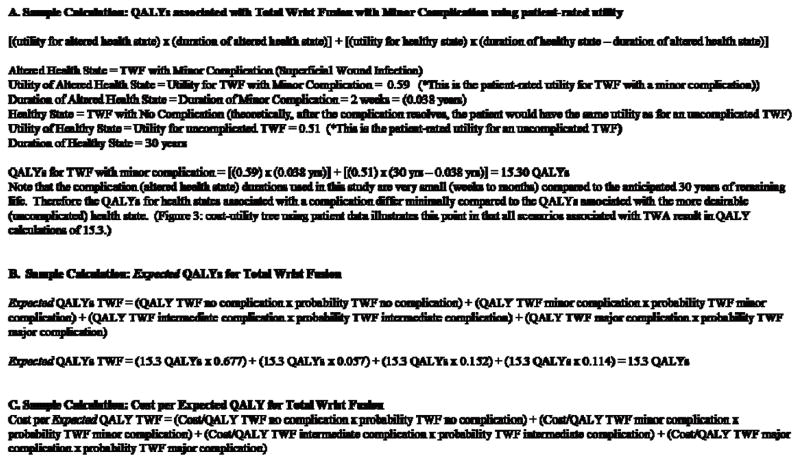
Our TTO survey included ten scenarios to address the ten potential outcomes of the model (Appendix 1). For example, the first scenario asks the responder to choose between living for 30 years with a painful, poorly-functioning RA wrist and living for X years with an essentially normal wrist. A third choice of “it’s too hard to choose” is always included as an option. The initial value for X is 30 years and therefore the logical choice is to live for 30 years with an essentially normal wrist instead of 30 years with a painful, poorly-functioning RA wrist. This scenario is instructive and orients the responder to the survey. The scenario choices then shift and the responder must decide between living for 30 years with a painful, poorly-functioning RA wrist and living for 15 years with an essentially normal wrist. Depending on the responder’s choices, X varies until the responder reaches a point of indifference at which he/she feels that the choices are equivalent. If the responder feels that living for 30 years with a painful RA wrist is equivalent to living for 20 years with an essentially normal wrist, then the utility for living with the RA wrist is 20 divided by 30, or 0.67. Similarly, if the responder feels that living for 30 years with an RA wrist is equivalent to living for 15 years with an essentially normal wrist, then the utility value for the RA wrist is 0.5. Utility values are weighted based on the probability and duration of the health state. A sample calculation is shown in Figure 2.
Figure 2.
Equation for QALYs using TWF with Minor Complication as the health state.
The utility survey was pilot tested on a group of attending and resident physicians as well as medical students and community members without medical training. Several rounds of major revisions were carried out followed by additional pilot testing and further minor revisions. Because we planned to administer the survey to hand surgeons, rheumatologists and RA patients, we designed two versions of the survey to allow for varying levels of understanding of the procedures and complications. Hand surgeons completed a version in which a complication such as hematoma or superficial infection was included with a very brief description. For patients and rheumatologists, the survey included more details about TWA and TWF, the nature of potential complications, and what the patient would likely experience in each scenario.
An internet-based survey engine was used for survey administration.(12) Each participant was assigned a log-in number and all responses remained anonymous. Upon completing the utility survey, physicians were asked a brief series of questions about practice patterns and patients were asked a brief series of health-related questions.
Patient Sample
Several studies have indicated that patients may rate the utility of their own health state differently than non-patients who are asked to imagine living in that same health state.(11) RA patients therefore provide an essential perspective in this study. Because we were interested in the preferences of patients with RA and severe upper extremity symptoms as well as patients with less severe RA, we surveyed patients followed for their RA in a hand surgery clinic and patients with RA followed in a general rheumatology clinic. A total of 50 consecutive patients were recruited, 25 from a hand surgery clinic and 25 from a rheumatology clinic. Patients were given a written description of the study and the study was also explained in person by a research assistant. Written consent was obtained and the patients received a one time cash incentive for participation.
Physician Sample
Although the Panel on Cost-Effectiveness recommends the use of utility values derived from community members or patients,(13) we felt that surveying physicians involved in the care of RA patients would provide a valuable additional perspective. A national random sample of hand surgeons (N=175) and rheumatologists (N=125) was recruited for participation. These physicians have long term experience with RA patients and the natural history of rheumatoid hand and wrist disease. Hand surgeons were randomly selected based on 2007 membership in the American Society for Surgery of the Hand. Rheumatologists were randomly selected based on membership in the American College of Rheumatology. Emeritus members, pediatric practitioners, retirees, research members, trainees, and members practicing outside of the United States were excluded because we were interested in assessing the opinions of physicians currently practicing in the United States. Specific utility results (without cost analysis), demographics, and practice patterns for the hand surgeon survey have been previously published.(14)
Costs
Surgeon Fee Schedule
Cost data were obtained based on Medicare Resource Based Relative Value Units (RBRVUs).(15) The RBRVU scale is an attempt by the Centers for Medicare and Medicaid Studies (CMS) to assign physician payments based on the resources necessary to provide care. Three components make up the RBRVU, including (1) physician work, (2) practice expenses, and (3) professional liability insurance costs. Costs are assigned based on the 2008 Current Procedural Terminology (CPT) code for a procedure. The cost is then multiplied by the 2008 conversion factor determined by CMS as well as a conversion factor to adjust for geographic differences in the cost of providing care. For this analysis we selected the appropriate geographic conversion factor for our region. Procedures can be carried out at inpatient hospitals, or at free standing surgical facilities. In this analysis we assume the procedures take place in a surgical facility and use the “facility” fee schedule in all cost calculations (Table 1).
Table 1.
Cost Estimates for Utility Scenarios
| Scenario | Surgical CPT1 Code | 2 Surgeon Fee | 3 ASC Fee | 4 Anesthesia Fee Schedule (* time estimate) | 5 Implant | 6 Cost |
|---|---|---|---|---|---|---|
| Well-controlled RA with painless, well-functioning wrist | Non-operative = $0 | |||||
| TWF, no complication | 25800 Arthrodesis wrist complete, without bone graft |
$690 | $3399 | $223–$385 (2–4 hours) |
$1230 | TWF= $5,704 |
| TWF, minor complication Superficial infection, oral antibiotic |
Complication $19 (14 day supply of cephalexin from a wholesale pharmacy) $5,704+$19= Total $5,723 |
|||||
| TWF, intermediate complication Symptomatic hardware requiring removal |
20680 Removal of implant; deep (eg buried wire, pin, screw, metal band, nail, rod, plate) |
$362 | $904 | $182–$223 (1.5–2 hours) |
Complication $1,488 $5,704+1,488= Total $7,192 |
|
| TWF, major complication Nonunion, revision with bone graft |
25810 Arthrodesis wrist, with iliac or other autograft, includes obtaining graft |
$792 | $3399 | $304–$506 (3–5 hours) |
$1,230 | Complication $5,927 $5,704+$5,927 Total $11,631 |
| TWA, no complication | 25446 Arthroplasty with prosthetic replacement; distal radius and partial or entire carpus (total wrist) |
$1082 | $5230 | $365–$527 (3–5 hours) |
$8992 | TWA=$15,831 |
| TWA, minor complication Delayed healing, dressing changes |
Complication $98 $15,831+$98 Total $15,929 |
|||||
| TWA, intermediate complication Hematoma |
25028 Incision and drainage forearm and/or wrist; deep abscess or hematoma | $470 | $910 | $142–$223 (1–2 hours) |
Complication $1,603 $15,831+$1,603 Total $17,434 |
|
| TWA, major complication Loosening of prosthesis Treated with revision TWA |
25449 Revision of arthroplasty, including removal of implant, wrist joint |
$950 | $1537 | $365–$527 (3–5 hours) |
$8992 | Complication $12,005 $15,831+$12,005 Total $27,836 |
| TWA, major complication Loosening of prosthesis Treated with TWF |
25250 Removal of wrist prosthesis; (separate procedure) 25810 Arthrodesis wrist, with iliac or other autograft, includes obtaining graft |
**$236 $792 |
**$625 $3399 |
$304–$466 (3–5 hours) |
$1230 | Complication $6,748 $15,831+$6,748 Total $22,579 |
2008 Current Procedural Terminology (CPT) code for surgical procedure
Medicare surgeon fee schedule (2008) based on CPT code, adjusted for geographic location
Medicare ambulatory surgery center fee schedule (2008) based on CPT code, adjusted for geographic location
Medicare anesthesia fee schedule (2008) based on CPT codes for anesthesia, adjusted for geographic location
01830 Anesthesia for open or surgical arthroscopic/endoscopic procedures on distal radius, distal ulna, wrist or hand joints, NOS
01832 Anesthesia for open or surgical arthroscopic/endoscopic procedures on distal radius, distal ulna, wrist, or hand joints, total wrist replacement
Note that the higher cost estimate was used in all cost calculations
Implant cost is the estimated cost of hardware implanted for a procedure. Values for TWA and TWF were obtained from an industry representative for our institution. TWA cost includes a total wrist prosthesis. TWF assumes an 8 hole fusion plate with four 2.7 mm screws and four 3.5 mm screws. The cost of the initial hardware is included for all operative scenarios. Additional implant cost is listed for scenarios describing a complication that requires additional hardware.
Cost indicates the cost for the scenario. A scenario describing a complication includes both the cost of the initial procedure (uncomplicated TWA or TWF) and the cost of treating the complication.
Reflects a 50% reduction in payment for second procedure
Anesthesia Fee Schedule
The Medicare anesthesia fee schedule is also determined by CMS. The formula used to calculate anesthesia fee schedule includes the base units associated with the appropriate anesthesia CPT code plus the time units that reflect the length of time the patient is under the anesthesiologist’s care. The sum of the base and time units is multiplied by a geographic conversion factor to determine the total cost. We considered a range of time estimates for each procedure and therefore a range of anesthesia costs. Relevant anesthesia codes and cost estimates for TWA and TWF are listed in Table 1. The lower anesthesia cost indicates the shorter operative time estimate and the higher cost the longer time estimate. For all cost analyses we used the higher estimated anesthesia cost.
Ambulatory Surgery Center Costs
We calculated cost based on the assumption that procedures would be carried out in an ambulatory surgery center (ASC). The 2008 Medicare fee schedule for ASCs includes a fee based on the surgical CPT code as well as a geographic conversion factor. ASC fees are shown in Table 1. The cost of implanted hardware is assumed to be separate and is described below.
Hardware Costs
Hardware costs for TWA and TWF were provided by an industry representative for our institution. A TWA prosthesis includes a radial component ($4624), a carpal component ($3360) and a carpal polyethylene component ($1008), for a total hardware cost of $8992. TWF includes an 8-hole fusion plate ($998), four 2.7 mm screws ($44 each), and four 3.5 mm screws ($14 each). Total hardware cost for TWF is $1230. We assume that a revision arthroplasty requires replacement of all TWA components and that a revision arthrodesis requires replacement of all TWF hardware.
Costs for Non-operative Management
Costs incurred by all patients regardless of treatment option do not alter the relationship between costs for the available treatment options. We assumed that all patients, including those who would select non-operative management, would be subject to the cost of an initial surgical consultation. We also assumed that all patients underwent an initial evaluation by a hand therapist and had received a trial of conservative management with medication, splinting and exercises. Surgical management of the rheumatoid wrist is unlikely to alter the patient’s need for systemic treatment of RA and therefore we assumed that the costs associated with anti-rheumatic medications were the same for all patients regardless of operative or non-operative management.
Lost Productivity
Lost productivity costs include employment income or productivity lost due to illness or treatment. Calculation of lost productivity is based on estimates of the average employment rate and income for the population experiencing the heath state under investigation. In reviewing the literature, we found many studies estimating the rate of employment for patients with RA.(16–19) These studies indicate that RA impairs a patient’s ability to participate in paid employment and leads to premature exit from the workforce.
Failure to participate in paid work likely reflects not only upper extremity dysfunction, but also more severe systemic RA symptoms that would not improve with wrist arthroplasty or arthrodesis. We were concerned that patients with severe rheumatoid hand and wrist disease who are candidates for TWF or TWA might have a much greater likelihood of disability and unemployment than the more general groups of RA patients described in the literature as well as the RA patients participating in our survey. We therefore reviewed our own survey data from a separate study (unpublished data) of RA patients presenting for evaluation for metacarpophalangeal joint arthroplasty. Only 20% of patients participated in paid employment at the time of initial evaluation. This is a lower rate of participation in paid employment than reported in the literature for RA patients.(16–19) Given the high rate of disability and unemployment among patients evaluated for metacarpophalangeal joint arthroplasty, we feel that patients undergoing TWA and TWF likely have similarly high rates of preoperative disability. Although detailed information on the rate of return to gainful employment as a result of TWA of TWF are lacking, our clinical experience suggests that RA patients who are unable to work preoperatively are unlikely to gain enough functional benefit to return to notable paid employment postoperatively. We therefore did not include productivity gains or losses in our general cost calculations.
Statistical Analysis
Survey data were analyzed using the STATA software package (STATA 10, STATA Corp., College Station, TX) to calculate mean utility values with 95% confidence intervals and to perform analyses for comparison of patient and physician responses to each survey question (Student’s t-test). The TreeAge software package (TreeAge Pro Suite, Version 2007; TreeAge Software, Inc., Williamstown, Mass) was used to apply the mean utility values obtained from our survey to calculate the QALYs associated with each procedure. Figure 2 shows a sample QALY calculation.
Sensitivity Analysis
Sensitivity analysis is a valuable part of a cost-utility analysis because it requires varying the assumptions of the cost-utility model to evaluate how the resulting outcome measures change. If the results are stable across varying assumptions, the model is considered to be robust. In this analysis, we chose to vary remaining years of life. Because QALY calculations include quantity of life, the number of remaining years of life can greatly influence the number of QALYs associated with each treatment option. We realize that assuming 30 remaining years of life in our survey is a generous estimate given that most patients undergo TWA or TWF in their mid 50’s. We therefore considered the implications of zero to 40 remaining years of life in a sensitivity analysis.
The published literature does not include sufficient data to determine the proportion of patients who may experience multiple complications or require multiple revisions. The literature also does not include adequate data to project the cost implication of a prosthesis that lasts for only a short period of time. In an attempt to capture these potential increased costs, we evaluated the effect of extremely high and extremely low complication rates on cost. We used the theoretical extremes of a 0% to 100% complication rate for TWA and TWF. Although this is not a direct calculation of the costs of multiple complications or revisions, it does provide a reference and we would expect that even with multiple complications, the expected cost of TWA or TWF would be unlikely to approach the cost of 100% of patients experiencing a major complication. For additional insight into the potential increased cost for multiple revisions, we calculated the anticipated cost for TWA with multiple revision arthroplasty procedures and eventual conversion to a total wrist fusion.
Results
Utility Survey
Based on inclusion and exclusion criteria, a total of 283 eligible hand surgeons and rheumatologists were contacted for participation. Seventeen physicians were excluded either due to incorrect contact information or because they indicated they had retired from clinical practice. Overall survey response rate for physicians was 39% (N=109) with 73 hand surgeons and 36 rheumatologists completing the entire survey. Of 50 recruited patients, 49 completed the survey (response rate 98%). One patient response was excluded due to the patient logging out of the survey prematurely.
Utility survey results for patients and physicians are shown in Table 2. Analysis of utilities for non-operative management, uncomplicated TWA and uncomplicated TWF shows that patients prefer TWA (p < 0.01), as did physicians (p < 0.001). Prior analysis of physician data showed no statistically significant difference between responses for hand surgeons and rheumatologists for all scenarios.(20) Mean utility values for physicians were compared to mean values for patients. Results for Scenario 1, living with a painful RA wrist, show that physicians rate the utility of this health state (mean utility 0.55) much higher than actual patients living with RA (mean utility 0.41). For all 10 scenarios, patients assigned a significantly lower utility than physicians for the health states described (p < 0.05).
Table 2.
Utility Survey Results
| Survey Scenario | Patient Mean Utility (95% CI) | Physician Mean Utility (95% CI) | p-value | |
|---|---|---|---|---|
| 1 | Non-operative treatment | 0.41 (0.33–0.49) | 0.55 (0.49–0.61) | p < 0.05 |
| 2 | TWF: no complication | 0.51 (0.43–0.60) | 0.80 (0.74–0.85) | p < 0.05 |
| 3 | TWF: minor complication | 0.59 (0.50–0.68) | 0.82 (0.77–0.87) | p < 0.05 |
| 4 | TWF: intermediate complication | 0.55 (0.46–0.64) | 0.84 (0.79–0.88) | p < 0.05 |
| 5 | TWF: major complication | 0.54 (0.45–0.63) | 0.81 (0.76–0.86) | p < 0.05 |
| 6 | TWA: no complication | 0.68 (0.60–0.77) | 0.85 (0.80–0.89) | p < 0.05 |
| 7 | TWA: minor complication | 0.64 (0.55–0.74) | 0.86 (0.81–0.91) | p < 0.05 |
| 8 | TWA: intermediate complication | 0.70 (0.61–0.79) | 0.87 (0.82–0.91) | p < 0.05 |
| 9 | TWA: major complication: revision arthroplasty | 0.63 (0.54–0.72) | 0.82 (0.77–0.87) | p < 0.05 |
| 10 | TWA: major complication: arthrodesis | 0.60 (0.51–0.70) | 0.81 (0.76–0.86) | p < 0.05 |
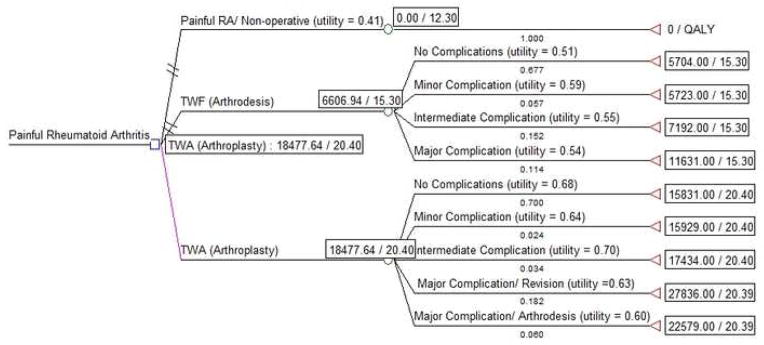
Using patient and physician utility values for each scenario along with complication rates for TWF and TWA obtained from the literature, we developed decision models to calculate the expected gain in QALYs for TWA and TWF based on an anticipated additional 30 years of life (Figures 3 and 4). Patient data showed TWF to be associated with an expected 15.3 QALYs, an incremental gain of 3.0 QALYs over non-operative management (12.3 QALYs). TWA was associated with an expected 20.4 QALYs, an incremental gain of 8.1 QALYs compared to non-operative management. The incremental gain in QALYs for TWA over TWF was 5.1 based on patient-rated utility.
Figure 3.
Cost-utility analysis using utility values derived from patient surveys. This analysis includes the higher cost estimates for each management strategy. The cost/utility ratios shown on the left indicate the overall cost-utility ratio for each procedure. These values are based on the weighted cost of each potential outcome (cost x probability). TWA is the most favorable treatment choice because it is associated with the lowest cost per QALY.
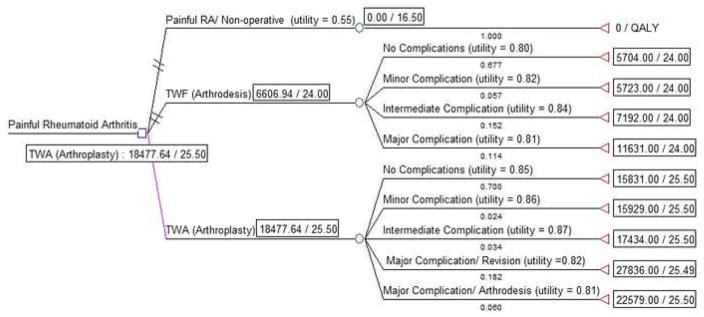
Figure 4.
Cost-utility analysis using utility values derived from physician surveys. Costs reflect the higher cost estimates for each management strategy. TWA is the most favorable treatment strategy.
Physician-rated utility was higher than patient-rated utility therefore calculations performed using physician data were associated with a higher number of expected QALYs. Non-operative management resulted in an expected 16.5 QALYs. TWF was associated with an expected 24.0 QALYs, an incremental gain of 7.5 QALYs compared to non-operative management. TWA was associated with 25.5 QALYs, an incremental gain of 9.0 QALYs over non-operative management. Using physician utility data, the incremental gain for TWA over TWF was 1.5 QALYs.
Cost per QALY
Cost calculations are shown in Table 3. The incremental cost-utility ratio (ICUR) is an estimate of the cost of each expected QALY gained with a management option relative to the cost of the alternative option to which it is being compared. In this analysis, we present the ICUR for TWA and TWF relative to non-operative management and for TWA relative to the standard of care, TWF. Patient-rated utility values were used for all ICUR calculations because patient-rated utility was lower than physician-rated utility resulting in fewer QALYs and a higher cost/QALY. We were interested in the most costly estimate as this determines of a procedure should be considered cost-effective. Using patient utility values, we found that TWA is associated with an approximate ICUR of $2281/QALY gained over non-operative management. TWF is associated with an approximate ICUR of $2202/QALY gained over non-operative management.
Table 3.
Comparison of Total Cost, Utilities, and Incremental Cost/Utility Ratio
| Treatment Option | 1 Total Cost | QALYs | Cost/QALY |
2 Incremental Cost-Utility Ratio (ICUR) compared to Non-Operative Management *calculated using patient utility values |
|---|---|---|---|---|
| Non-Operative | $0.00 | Patient 12.3 Physician 16.5 |
Patient $0/12.3 QALY Physician $0/16.5 QALY |
N/A |
| TWF (Arthrodesis) | $6,607 | Patient 15.3 Physician 24.0 |
Patient $6,607/15.3 QALY = $431.83/QALY Physician $6,607/24.0 QALY = $275.29/QALY |
$2,202/QALY |
| TWA (Arthroplasty) | $18,478 | Patient 20.4 Physician 25.5 |
Patient $18,478/20.4 QALY =$905.78/QALY Physician $18,478/25.5 QALY = $724.63/QALY |
$2,281/QALY 3 ICUR TWA compared to TWF = $2,327.64/QALY |
Total cost is the expected cost obtained from the decision analysis tree (Figures 3, 4). This cost reflects the cost of each possible outcome/complication for TWA and TWF as well as the probability of that outcome.
ICUR reflects the incremental cost for the additional QALYs gained with a more costly procedure. Here we evaluate the additional cost for TWA and TWF and the anticipated gain in QALYs compared to Non-operative Management.
Sample Calculation: ICUR for TWF compared to Non-Operative management (using patient-rated utility)
ICUR = (Cost TWF – Cost Non-Operative)/(QALY TWF – QALY Non-Operative)
ICUR = ($6,607 - $0)/(15.3 QALY – 12.3 QALY) = $6,607/3 QALY
ICUR = $2202.33 per additional QALY gained with TWF over Non-Operative Management
ICUR for TWA compared to TWF reflects the cost of each additional QALY gained with TWA over TWF.
In this decision model, TWA is associated with a greater expected gain in QALYs than TWF. Based on patient data, the incremental expected gain for TWA over TWF is 5.1 QALYs with an approximate ICUR of $2328/QALY gained with TWA over TWF.
Sensitivity Analysis
This cost-utility analysis addresses utility for living with wrist pain (non-operative management), TWA, or TWF for the remaining years of life. We performed a sensitivity analysis to investigate how changes in patient lifespan would affect cost estimates. Calculations reflect patient utility values and the higher procedural cost estimates in an effort to show the conditions that would produce the highest possible (most expensive) ICUR. As shown in Figure 5, the incremental cost per QALY for TWA compared to TWF and nonoperative management remains well under the historical $50,000 benchmark, even with only 2 remaining years of life.
Figure 5.
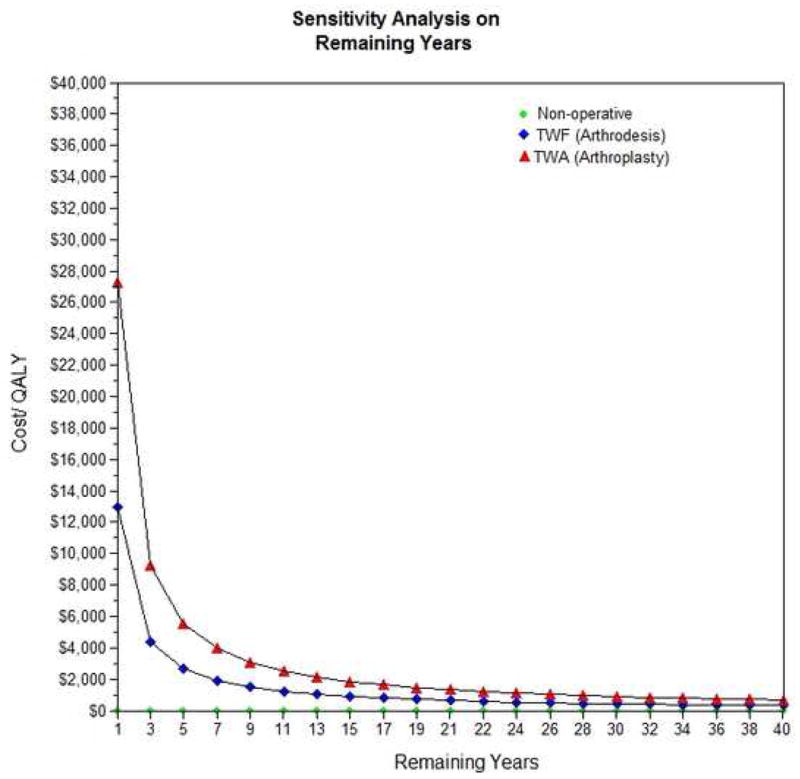
Sensitivity analysis varying healthy years of remaining life. This graph shows the incremental cost-utility ratio of TWA and TWF relative to non-operative management. The dotted vertical line at 30 years indicates the years of remaining life used in our model. Costs reflect the higher cost estimates and utility values were obtained from physician survey data.
The complication rates used in our models reflect the best estimates available because they are derived from a systematic literature search. To explore the implications of extremely high or low complication rates on cost estimates, we set the complication rate for TWF at 0% compared to a 100% major complication rate for TWA. Note that setting the complication rate affects both the cost and the utility calculations We ran these estimates through the decision analysis software program to determine how expensive TWA would be in the most expensive case scenario (all patients requiring revision arthroplasty). In this extreme theoretical scenario, TWA showed an ICUR of $3,441/QALY relative to nonoperative management and $4,348/QALY relative to TWF, still well below the $50,000 benchmark.
The expected lifespan of a total wrist prosthesis is unknown. We anticipate at least 1, and possibly as many as 3, revisions for a patient with an expected 30 to 40 year lifespan. Table 4 shows the expected cost for TWA and multiple revisions along with the additional cost if the patient requires conversion to a TWF. The cost for a TWA and 3 revision arthroplasties as well as eventual conversion to a TWF is $58,594. Our utility survey did not ask patients about multiple revision operations and therefore we cannot calculate an expected cost/QALY for patients requiring multiple revisions. Using the historical benchmark of $50,000/QALY, TWA would only need to be associated with a gain of 1.17 QALYs compared to TWF or non-operative management to be considered cost-effective. Therefore it is likely that TWA remains cost-effective even in the setting of multiple revisions over the patient’s lifespan.
Table 4.
Cost for TWA with Multiple Revisions
| Procedure(s) | Cost | Conversion to TWF with Bone Graft (Cost for TWF = $6,748) |
|---|---|---|
| TWA | $15,831 | $15,831 + $6,748 = $22,579 |
| TWA + 1 Revision TWA $15,831 + $12,005 | $27,836 | $27,836 + $6,748 = $34,584 |
| TWA + 2 Revision TWAs $15,831 + (2 x $12,005) | $39,841 | $39,841 + $6,748 = $46,589 |
| TWA + 3 Revision TWAs $15,831 + (3 x $12,005) | $51,846 | $51,846 + $6,748 = $58,594 |
Discussion
In this cost-utility analysis we found that RA patients feel that living with a painful, poorly-functioning RA wrist is an extremely unfavorable health state. A mean utility value of 0.41 indicates that patients feel that living for approximately 12 years with a normal wrist is equivalent to living for 30 years with a painful RA wrist. This finding is striking in that other authors have found utility values of 0.3 for blindness (21) and 0.4 for paraplegia (22). Although our results do not suggest that RA patients consider painful wrist disease equivalent to paraplegia, they are indicative of an extremely negative view of rheumatoid wrist disease. Clearly RA patients believe that severe wrist symptoms would have a devastating effect on their lives.
Physicians responding to our survey showed a mean utility value of 0.55 for the health state described as living with a painful, poorly-functioning RA wrist. Physician-rated utility for this health state (0.55) was significantly higher than patient-rated utility (0.41) (p < 0.05). The finding that patients assigned lower utility for the diseased wrist is of particular interest because patients living with a specific illness typically rate the utility of their health state higher than non-patients asked to imagine what it would be like to experience that same health state.(11) Physicians caring for RA patients may actually underestimate the negative effects of RA on their patients’ lives. A potential explanation of this finding is that RA patients have more experience living with chronic pain and therefore may view the scenario of living with pain (non-operative management) more negatively than physicians. Alternatively, physicians may have a less negative view of living with wrist pain (non-operative management) because of extensive experience with the drawbacks of surgical intervention. Physicians with long-term experience treating severe RA understand the capacity of a patient to adapt to severe wrist disease over time. This scenario is likely more concerning to a RA patient asked to consider what it would be like to live with severe wrist disease.
Several studies have evaluated the cost-effectiveness of large total joint arthroplasties. Using the historical benchmark of $50,000/QALY as a guideline, these procedures are considered to be an extremely good value. For example, total ankle arthroplasty is associated with a cost of approximately $18,000/QALY gained(23) and total hip arthroplasty is associated with a cost of approximately $4,600/QALY.(24) In this analysis of TWA and TWF, we have demonstrated an approximate incremental cost of $2,281/QALY for TWA compared to non-operative management and an approximate incremental cost of $2,328/QALY for TWA compared to TWF.
Postoperative hand therapy can increase cost estimates. In our institution, an 8 week course of supervised hand therapy 3 times per week would add approximately $3,600 to the cost of TWA and TWF. Because this cost is associated with both procedures, it does not affect the incremental cost-effectiveness of TWA compared to TWF. Even if patients undergoing TWA required an intense course of hand therapy (and patients undergoing TWF required no therapy), the addition of the $3,600 therapy cost to the overall cost of TWA would only increase the ICUR (TWA relative to TWF) to approximately $3,034/QALY.
TWF is a fairly straightforward procedure with predictable results. The successfully fused wrist is unlikely to require additional operative intervention. TWA is a complex and technically-demanding procedure that has historically been associated with high complication and revision rates. Although TWA has been a treatment option for the RA wrist for nearly four decades, the procedure is not frequently performed among hand surgeons (14). Three generations of total wrist prostheses have undergone clinical use and refinement, however, published reports of clinical outcomes for these prostheses are limited by small sample size, retrospective study design and inconsistent reporting of outcome measures making the actual clinical outcome uncertain.(1) Three prosthesis designs are currently FDA approved for use in the United States. Outcomes for these specific wrist prostheses have not been well-documented and no clinical information is available for two of the prosthesis designs (communication with industry representatives). The long-term complication and revision rates for current total wrist prostheses may be lower than the historical complication rates used for calculations in this analysis making TWA potentially more cost-effective than our estimates.
Cost-utility analyses require many estimated values to achieve a reasonable cost estimate. The resulting cost estimate reflects the limitations of these values. Our study is therefore limited by the uncertainty associated with utility values, lifespan and complication rates. Manipulation of lifespan and complication rates in sensitivity analyses indicates that even at the extremes, TWA remains a cost-effective procedure relative to TWF and nonoperative management. Utility values are subject to uncertainty because of potential difficulty understanding the survey, survey fatigue, and the perspective of those taking the survey. Utility values for the survey population may not reflect the utility that patients actually experiencing the health state would assign and also may not reflect the utility that a representative sample of the general population would assign to each scenario. Calculations based on much higher or lower utility values could substantially alter cost estimates.
This cost-utility analysis of TWA and TWF provides insight into the value that patients and physicians place on maintaining wrist movement. Based on survey results, RA patients would prefer TWA over TWF and non-operative management. We found that even with relatively high complication rates for TWA in the published literature, the procedure is extremely cost-effective in terms of cost per expected gain in QALYs.
Our initial evaluation of TWA and TWF in a systematic review of the literature indicated that the published outcomes for TWA show potentially higher complication and revision rates and no demonstrable functional benefit over TWF.(1) Under these circumstances, TWA would not be warranted unless patients demonstrated a greater utility for TWA than for TWF. This cost utility analysis indicates that RA patients place a great deal of emphasis on maintaining wrist motion. Calculation of cost per QALY gained with TWA show that in spite of fairly high complication and revision rates, TWA is a very cost-effective procedure. Additional research efforts to improve and refine TWA prosthesis design along with rigorous reporting of clinical outcomes will further define the appropriate application of TWA and TWF in the management of rheumatoid wrist disease.
Acknowledgments
This project was supported in part by the Integra Corporation. The first author is supported by the Robert Wood Johnson Clinical Scholars’ Program and the senior author (KCC) is supported by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01 AR047328), a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120), and an Exploratory/Developmental Research Grant Award (R21AR056988). We would like to thank Melissa Shauver for her assistance preparing this manuscript for publication.
Footnotes
Level of Evidence: Level 2, Economic and Decision Analyses
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cavaliere CM, Chung KC. Systematic Review of Total Wrist Arthroplasty Compared to Total Wrist Arthrodesis in Rheumatoid Arthritis. Plastic and Reconstructive Surgery. 2008;122:813–825. doi: 10.1097/PRS.0b013e318180ece3. [DOI] [PubMed] [Google Scholar]
- 2.Detsky AS, Naglie G, Krahn MD, Naimark D, Redelmeier DA. Primer on medical decision analysis: part 1- getting started. Medical Decision Making. 1997;17:123–125. doi: 10.1177/0272989X9701700201. [DOI] [PubMed] [Google Scholar]
- 3.Detsky AS, Naglie G, Krahn MD, Redelmeier DA, Naimark D. Primer on medical decision analysis: part 2- building a tree. Medical Decision Making. 1997;17:126–135. doi: 10.1177/0272989X9701700202. [DOI] [PubMed] [Google Scholar]
- 4.Kocher MS, Henley MB. It is money that matters: decision analysis and cost-effectiveness analysis. Clinical Orthopaedics and Related Research. 2003;413:106–116. doi: 10.1097/01.blo.0000079326.41006.4e. [DOI] [PubMed] [Google Scholar]
- 5.Torrance GW. Preferences for health outcomes and cost-utility analysis. The American Journal of Managed Care. 1997;3(Suppl):S8–S20. [PubMed] [Google Scholar]
- 6.Chung KC, Walters MR, Greenfield ML, Chernew ME. Endoscopic versus open carpal tunnel release: a cost-effectiveness analysis. Plastic and Reconstructive Surgery. 1998;102:1089–1099. doi: 10.1097/00006534-199809040-00026. [DOI] [PubMed] [Google Scholar]
- 7.Stylopoulos N, Gazelle GS, Rattner DW. A cost-utility analysis of treatment options for inguinal hernia in 1,513,008 adult patients. Surgical Endoscopy. 2003;17:180–189. doi: 10.1007/s00464-002-8849-z. [DOI] [PubMed] [Google Scholar]
- 8.Thoma A, Khuthaila D, Rockwell G, Veltri K. Cost-utility analysis comparing free and pedicled TRAM flap for breast reconstruction. Microsurgery. 2003;23:287–295. doi: 10.1002/micr.10138. [DOI] [PubMed] [Google Scholar]
- 9.Braithwaite RS, Meltzer DO, King JT, Leslie D, Roberts MS. What does the value of modern medicine say about the $50,000 per quality-adjusted life-year decision rule. Medical Care. 2008;46:349–356. doi: 10.1097/MLR.0b013e31815c31a7. [DOI] [PubMed] [Google Scholar]
- 10.Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC. The role of cost-effectiveness analysis in health and medicine. JAMA. 1996;276:1172–1177. [PubMed] [Google Scholar]
- 11.Gold MR, Patrick DL, Torrance GW, Fryback DG, Hadorn DC, Kamlet MS, et al. Identifying and Valuing Outcomes. In: Gold MR, Russell LB, Siegel JA, Weinstein MC, editors. Cost-Effectiveness in Health and Medicine. New York: Oxford University Press; 1996. pp. 82–134. [Google Scholar]
- 12.Zoomerang. 2008 http://www.zoomerang.com.
- 13.Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the panel on cost-effectiveness in health and medicine. JAMA. 1996;276:1253–1258. [PubMed] [Google Scholar]
- 14.Cavaliere CM, Chung KC. Total wrist arthroplasty and total wrist arthrodesis in rheumatoid arthritis: a decision analysis from the hand surgeons’ perspective. Journal of Hand Surgery. 2008;33A:1744–1755. doi: 10.1016/j.jhsa.2008.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Center for Medicare and Medicaid Services. Town Hall Practice Expense Data Files - Healthcare Common Procedure Coding System Level File. Department of Health and Human Service; 2006. [Google Scholar]
- 16.Burton W, Morrison A, Maclean R, Ruderman E. Systematic review of studies of productivity loss due to rheumatoid arthritis. Occupational Medicine. 2006;56:18–27. doi: 10.1093/occmed/kqi171. [DOI] [PubMed] [Google Scholar]
- 17.Reisine S, Fifield J, Walsh S, Dauser D. Work disability among two cohorts of women with recent-onset rheumatoid arthritis: a survival analysis. Arthritis & Rheumatism. 2007;57:372–380. doi: 10.1002/art.22620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shanahan EM, Smith M, Roberts-Thompson L, Esterman A, Ahern M. Influence of rheumatoid arthritis on work participation in Australia. Internal Medicine Journal. 2008;38:166–173. doi: 10.1111/j.1445-5994.2007.01432.x. [DOI] [PubMed] [Google Scholar]
- 19.Wolfe F, Allaire S, Michaud K. The prevalence and incidence of work disability in rheumatoid arthritis, and the effect of anti-tumor necrosis factor on work disability. Journal of Rheumatology. 2007;34:2211–2217. [PubMed] [Google Scholar]
- 20.Cavaliere CM, Oppenheimer AJ, Chung KC. Reconstructing the rheumatoid wrist: a utility analysis comparing total wrist fusion and total wrist arthroplasty from the perspectives of rheumatologists and hand surgeons. Hand. doi: 10.1007/s11552-009-9194-7. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown MM, Brown GC, Sharma S, Kistler J, Brown H. Utility values associated with blindness in an adult population. British Journal of Ophthalmology. 2001;85:327–331. doi: 10.1136/bjo.85.3.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gold MR, Franks P, McCoy KI, Fryback DG. Toward consistency in cost-utility analyses: using national measures to create condition-specific values. Medical Care. 1998;36:778–792. doi: 10.1097/00005650-199806000-00002. [DOI] [PubMed] [Google Scholar]
- 23.SooHoo NF, Sharifi H, Kominski G, Lieberman JR. Cost-effectiveness analysis of unicompartmental knee arthroplasty as an alternative to total knee arthroplasty for unicompartmental osteoarthritis. The Journal of Bone and Joint Surgery. 2006;88A:1975–1982. doi: 10.2106/JBJS.E.00597. [DOI] [PubMed] [Google Scholar]
- 24.Chang RW, Pellisier JM, Hazen GB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996;275:858–865. [PubMed] [Google Scholar]