Abstract
Objective
To evaluate the effectiveness of the American Academy of Pediatrics Neonatal Resuscitation Program (NRP) in improving knowledge, skills, and self-efficacy of nurse midwives in low-risk delivery clinics in a developing country.
Study design
We used the content specifications of the NRP material applicable to college-educated nurse midwives working in low-risk clinics in Zambia to develop performance and self-efficacy evaluations focused on principles of resuscitation, initial steps, ventilation, and chest compressions. These evaluations were administered to 127 nurse midwives before and after NRP training and 6-months later.
Results
After training, written scores (knowledge evaluation) improved from 57% ± 14% to 80% ± 12% (mean ± SD; P < .0001); performance scores (skills evaluation) improved the most from 43% ± 21% to 88% ± 9% (P < .0001); self-efficacy scores improved from 74% ± 14% to 90% ± 10% (P < .0001). Written and performance scores decreased significantly 6 months after training, but self-efficacy scores remained high.
Conclusions
As conducted, the NRP training improved educational outcomes in college-educated practicing nurse midwives. Pre-training knowledge and skills scores were relatively low despite the advanced formal education and experience of the participants, whereas the self-efficacy scores were high. NRP training has the potential to substantially improve knowledge and skills of neonatal resuscitation.
Birth asphyxia is one of the most frequent causes of early deaths, accounting for approximately 23% of 4 million neonatal deaths worldwide.1 Neonatal resuscitation is a simple, inexpensive, readily available, and cost-effective intervention that can prevent many of the deaths and reduce disabilities in survivors from birth asphyxia.2,3 However, the World Health Organization has concluded that resuscitation is often not initiated or the methods used are inadequate or wrong.4 This is especially true in the developing world, which accounts for 98% of the 4 million neonatal deaths and could benefit dramatically from effective neonatal resuscitation training of birth attendants.
The Neonatal Resuscitation Program (NRP) is the official educational program of the American Academy of Pediatrics and the American Heart Association for educating and training health care providers in the knowledge and skills of neonatal resuscitation. During the decade after the introduction of NRP in 1987, deaths caused by birth asphyxia in the United States decreased by 42%,5,6 although this improvement cannot be ascribed to NRP alone. Although controlled non-randomized studies in China, India, and Africa suggest that training in resuscitation with the NRP or other programs may reduce neonatal mortality caused by birth asphyxia,2,3,7–9 studies do not show a consistent decrease in mortality and a meta-analysis is inconclusive on all-cause neonatal mortality.10 The NRP has been widely adopted for use throughout many highly developed and lesser-developed countries.
The NRP course improved healthcare providers’ knowledge, skills, and attitudes in developed countries10; however, there has been no rigorous evaluation of its educational impact and retention in developing countries. Furthermore, the evaluation of the educational impact of other resuscitation training in developing countries has been limited.11,12 Evaluation of the educational effectiveness of NRP training in low-resource environments is important because the impact may differ on the basis of differences in education, practices, and resources. The purpose of this study was to determine whether NRP training improves knowledge, skills, and self-efficacy of primary healthcare providers in low-risk delivery centers.
METHODS
Study Design
Qualified NRP instructors administered the NRP course to 127 college-educated (4 years) nurse midwives who were employed in 18 primary-level delivery clinics in Lusaka and Ndola, Zambia in 2005. The midwives had been in practice for 16 ± 9 years (range, 3–30 years; median, 14 years). The midwives were trained previously in neonatal resuscitation, but had not been trained with the NRP course. The midwives were encouraged to read the NRP textbook before the training. The course was conducted in English, with group meetings held at a high-delivery service referral hospital (University Hospital of Zambia) in 2 phases with the trainer-of-trainers model. The first phase, led by an experienced NRP regional trainer (W.C.), consisted of a 4-day course for 15 nurse midwives who became trainers. Subsequently, these 15 trainers trained an additional 112 nurse midwives in small groups with the same format.
The standard NRP course content and format used cognitive and psychomotor activities to allow individuals to complete the course through group meetings following the materials and guidelines published in 2000.13–15 Participants not only completed self-directed and self-assessment exercises with textbooks, but also participated in extensive hands-on practice scenarios and actual deliveries with the guidance of trained instructors. Each nurse midwife completed the written, performance, and self-efficacy evaluations before and after the NRP training, and a subgroup repeated the evaluations 6-months after completion of training. The institutional review boards of the University of Alabama at Birmingham, the University of Zambia, and the Research Triangle Institute approved the study.
NRP Evaluations
The NRP course has a written evaluation to test knowledge and a performance evaluation to test skills. To determine educational effectiveness of NRP training on knowledge in Zambia, the standard NRP written evaluation was used. The evaluation (scale) was split in subscales by grouping the related individual items. To evaluate performance, 2 physicians (W.C., L.W.), a nurse/educator (M. Collins), and an educator (B.M.) identified 29 content items from the standard NRP Megacode (NRP Textbook, 2000) pertinent to Lessons 1 to 4 that were determined to be essential and appropriate for the low-resource low-risk delivery centers in urban Zambia. Thus, the performance evaluations excluded intubation and medications. These items were compiled on a checklist that included specific and objective instructions for the participant and observer. An observer recorded the midwives’ skills as they performed procedures on a mannequin following the instructions. The same group of physicians and educator/nurse developed a 14-item self-efficacy evaluation and used a 5-point Likert scale (1-not very confident to 5-very confident). All 3 evaluation tools were pre-tested with local midwives and modified as needed by the group of physicians and educator/nurse. For the purposes of scoring the evaluations, each item within the written, performance, and self-efficacy evaluations were given equal value. The same evaluations were administered before and after NRP training and again 6 months after completion of training.
Analytic Methods
Each item on the written and performance evaluations in the lessons “Overview and Principles of Resuscitation,” “Initial Steps,” “Ventilation,” and “Chest Compressions” was scored as correct or incorrect. Although the written evaluation tested the concepts of intubation and medications, these contents were not included in the performance evaluation or in the analyses of the written evaluations. Scores for the scales and their subscales were computed as the percentage of items on the scale or subscale answered correctly. Items on the self-efficacy scale were scored from 1 to 5, and scale scores were calculated as the mean of the item responses.
We computed Cronbach’s alphas16 to assess the internal consistency of the 3 evaluations (scales) at each time point. In addition, we explored the relationship between the participants’ scores on the written and performance evaluations. We divided participants in 2 groups on the basis of their scores on the performance evaluation after the training: high performance (score ≥85), or low performance (score <85). t tests were used to compare mean written evaluation scores after the training for the 2 groups. When the written and performance evaluations were measuring similar constructs, we would expect participants in the high performance group to have significantly higher written evaluation scores.
To assess the impact of the training, we conducted 2 sets of analyses. First, we examined the change from before to after the training for all participants. The items on the scales were analyzed individually or in groups of subscales on the basis of content (eg, ventilation or chest compressions) to identify specific topics in which participants either performed well or had difficulty to target future training efforts or modify the evaluations. Paired t tests were used to test for changes in mean scores on the overall scale or subscale scores, and Mc-Nemar tests were used to compare responses with the individual items between pre-training and post-training.
The second set of analyses focused on retention of knowledge through the 6 months after the training. We used generalized linear models with generalized estimating equations estimation to test for changes in the evaluation (scale) scores from the pre-training to the 6-month follow-up. Generalized estimating equation models were selected because they account for the correlation between repeated measurements with time and permit the inclusion of participants with missing data. This approach allowed us to use data from all participants, even when they were not in the 6-month follow-up evaluation. In addition, we explored whether retention of knowledge and skills differed according to participants’ reported self-efficacy by testing a time by self-efficacy interaction in the models. A P value < .05 was considered to be statistically significant.
RESULTS
On the basis of Cronbach’s alpha, overall the 3 evaluation scales demonstrated good internal consistency (generally defined as alpha >0.70). The Cronbach’s alphas for the scales were: written evaluation (pre-training = 0.80, post-training = 0.84, 6 months = 0.87), performance evaluation (pre-training = 0.87, post-training = 0.60, 6 months = 0.87), and self-efficacy (pre-training = 0.90, post-training = 0.84, 6 months = 0.87). The alpha for the performance evaluation decreased from pre-training to post-training, suggesting that there may be less consistency in how participants performed across the items after the training.
The percentage of items on the written evaluation answered correctly increased from 57% ± 14% pre-training to 80% ± 12% post-training (P < .001; Table I). Similar levels of improvement were observed across the 4 subscales (Table I) and for almost all items on the subscales (Appendix 1; available at www.jpeds.com). Scores on the performance evaluation scale and subscales showed the largest improvements of all 3 scales. Overall, scores increased from 43% ± 21% before training to 88% ± 9% after training (P < .001; Table I). Scores improved in all 4 subscales and for almost all items on the subscales (Appendix 2; available at www.jpeds.com). There was a wide variation in performance. For example, although there was almost uniform provision of infant warming both before and after training (79% ± 41% to 90% ± 30%), techniques for depth of chest compressions improved from as low as 20% ± 40% to 92% ± 27% for correct depth of chest compressions.
Table I.
Percentage of items answered correctly on written and performance evaluations and mean self-efficacy ratings
| Scale | Pre-training mean (SD) | Post-training mean (SD) | Post-training–pre-training mean (SD) |
|---|---|---|---|
| Written evaluation | |||
| Overall | 57 (14) | 80 (12) | 23 (14) |
| Overview and principles of resuscitation | 61 (19) | 83 (13) | 22 (23) |
| Initial steps in resuscitation | 53 (19) | 77 (17) | 24 (23) |
| Ventilation | 54 (15) | 77 (17) | 23 (18) |
| Chest compressions | 61 (21) | 86 (14) | 26 (23) |
| Performance evaluation | |||
| Overall | 43 (21) | 88 (9) | 45 (21) |
| Initial steps | 60 (18) | 87 (11) | 26 (20) |
| Ventilation | 34 (88) | 88 (12) | 53 (28) |
| Chest compressions | 28 (33) | 93 (14) | 65 (35) |
| Self-efficacy | |||
| Overall | 3.7 (0.7) | 4.5 (0.5) | 0.8 (0.8) |
n = 127.
Differences from pre- to post-training were significant for all scales (P < .001).
Self-efficacy ratings range from 1 to 5 (rather than 0 to 100) and therefore are presented with 1 decimal point to provide detail that may be missed by rounding to whole numbers.
Appendix 1.
Percentage of correct responses to written evaluation items
| Item | Pre-test Mean (SD) | Post-test Mean (SD) | Post-test–pre-test Mean (SD) |
|---|---|---|---|
| Overall written evaluation | 57 (14) | 80 (12) | 23 (14) |
| A. Overview and principles of resuscitation | 61 (19) | 83 (13) | 22 (23) |
| 1. Evaluation of a newborn’s needs for resuscitation is based primarily on what signs? | 84 (37) | 96 (20) | 12 (41) |
| 2. What action should be taken if a newborn is not breathing after tactile stimulation? | 44 (50) | 80 (41) | 35 (64) |
| 3. Newborns who experience secondary apnea: | 61 (49) | 86 (35) | 25 (55) |
| 4. Approximately what percentage of newborns requires at least some assistance to initiate spontaneous and regular respiration? | 50 (50) | 81 (39) | 32 (53) |
| 5. In what order do cardiorespiratory changes occur after a normal delivery of a term newborn? | 48 (50) | 67 (47) | 19 (66) |
| 6. A newborn does not make a normal transition at birth. Which of the following conditions are you likely to find? | 57 (50) | 83 (37) | 26 (59) |
| 7. Which is not associated with secondary apnea? | 72 (45) | 83 (38) | 11 (51) |
| 8. What characteristic of primary apnea distinguishes it from secondary apnea? | 62 (49) | 80 (40) | 18 (59) |
| 9. Premature babies may present unique challenges during resuscitation because of: | 76 (43) | 81 (39) | 5 (58) |
| 10. At a minimum, how many skilled people whose primary responsibility is the management of the newborn should be present at every delivery? | 36 (48) | 83 (38) | 46 (63) |
| 11. When a newborn is apneic at birth: | 87 (34) | 94 (23) | 7 (43) |
| 12. The preferred sequence for neonatal resuscitation is to: | 43 (50) | 80 (40) | 38 (58) |
| 13. A newborn has been given positive-pressure ventilation for approximately 30 seconds. Her heart rate is 55 beats per minute. What should you do next? | 83 (38) | 89 (31) | 6 (45) |
| B. Initial steps in resuscitation | 53 (19) | 77 (17) | 24 (23) |
| 1. What is the major deciding factor concerning whether a meconium-stained newborn needs intubation and suctioning? | 35 (48) | 72 (45) | 37 (60) |
| 2. Which of the following is not an acceptable method of stimulating a newborn to breathe? | 85 (36) | 92 (27) | 7 (42) |
| 3. The most effective action in the resuscitation of an apneic newborn who has not responded to drying and rubbing of the back is: | 46 (50) | 72 (45) | 25 (66) |
| 4. When deciding which meconium-stained newborns need tracheal suctioning, the term “vigorous” is defined by what 3 characteristics? | 46 (50) | 74 (44) | 28 (64) |
| 5. The best initial intervention for a newborn who is breathing well and has an adequate heart rate, but who also has central cyanosis is to: | 63 (48) | 83 (38) | 19 (58) |
| 6. Which drawing shows the correct way to position a newborn’s head for suctioning? | 44 (50) | 80 (40) | 36 (59) |
| 7. After you have warmed, positioned, cleared the airway, dried, stimulated, and given oxygen as necessary, what do you evaluate next to determine if further resuscitative actions are needed? | 82 (39) | 96 (20) | 14 (41) |
| 8. After a normal delivery at term, a crying newborn’s mouth is suctioned and this action is repeated for “excessive secretions.” The heart rate decreases from 120 to 80 beats per minute. Of the following the most appropriate action would be to: | 25 (44) | 49 (50) | 24 (62) |
| 9. Which drawing shows the incorrect way of providing free-flow oxygen to a newborn who is cyanotic but breathing well? | 42 (50) | 70 (46) | 28 (55) |
| 10. Thick meconium is noted in the amniotic fluid of a term newborn. As the head is delivered, the newborn’s mouth, pharynx, and nose are suctioned. After the newborn is placed under a preheated radiant warmer, the newborn is observed to be pale, limp, and showing no respiratory effort. The initial action should be to: | 38 (49) | 65 (48) | 27 (66) |
| 11. You count a newborn’s heart beats for 6 seconds and count 9 beats. You would report the heart rate as: | 76 (43) | 94 (24) | 18 (44) |
| 12. Which of the following statements is true concerning clearing the airway when no meconium is present? | 46 (50) | 74 (44) | 29 (62) |
| 13. After evaluation and tactile stimulation, a newborn’s heart rate remains less than 100 beats per minute. The next most appropriate intervention would be to: | 59 (49) | 83 (38) | 24 (60) |
| C. Resuscitation bag and mask | 54 (15) | 77 (17) | 23 (18) |
| 1. Your flow-inflating resuscitation bag will not inflate. Which of the following is NOT a possible reason? | 56 (50) | 75 (44) | 19 (59) |
| 2. Which diagram reflects correct positioning of face masks for ventilating newborns? | 35 (48) | 75 (44) | 39 (61) |
| 3. Which of the following should be done with an orogastric tube? | 36 (48) | 71 (45) | 37 (63) |
| 4. The single BEST way to assess whether your positive-pressure ventilations are adequate is: | 70 (46) | 84 (37) | 14 (51) |
| 5. Which of the following is TRUE of a flow-inflating resuscitation bag? | 48 (50) | 60 (49) | 12 (70) |
| 6. A self-inflating bag equipped with an oxygen reservoir and attached to a 100% oxygen source will deliver what percentage of oxygen to the newborn? | 70 (46) | 92 (27) | 22 (54) |
| 7. Which of the following illustrates a properly inflated flow-inflating resuscitation bag? | 24 (43) | 59 (49) | 36 (60) |
| 8. Which of the following does NOT determine the amount of pressure delivered from a self-inflating resuscitation bag? | 18 (39) | 57 (50) | 39 (58) |
| 9. Which of the following is a desirable characteristic of a fag mask? | 62 (49) | 83 (38) | 21 (62) |
| 10. During the initial stages of positive-pressure ventilation, breaths should be delivered at a rate of ___ times per minute. | 56 (50) | 85 (36) | 30 (57) |
| 11. A newborn ahs been given positive-pressure ventilation, has a heart rate greater than 100 beats per minute, and is breathing spontaneously. You should: | 48 (50) | 69 (47) | 21 (55) |
| 12. If a newborn requires positive-pressure ventilation with a bag and mask for longer than several minutes: | 49 (50) | 70 (46) | 21 (61) |
| 13. As an estimate, the length of the orogastric catheter to be inserted should be equal to: | 73 (44) | 92 (27) | 19 (50) |
| 14. Which of the following is NOT a sign of improvement in a newborn being resuscitated? | 95 (21) | 97 (18) | 2 (24) |
| 15. The proper place for you to stand while using the resuscitation bag most effectively is: | 72 (45) | 85 (36) | 13 (55) |
| 16. Which of the following is NOT an advantage of a flow-inflating resuscitation bag? | 29 (46) | 65 (48) | 36 (54) |
| 17. Which of the following is (are) disadvantage(s) of a self-inflating resuscitation bag? | 62 (49) | 72 (45) | 11 (57) |
| 18. When using a self-inflating resuscitation bag for resuscitating newborns, it is important that the: | 61 (49) | 81 (39) | 22 (58) |
| 19. Which of the following need NOT be accomplished before assisting ventilation with a resuscitation bag? | 76 (43) | 96 (20) | 20 (47) |
| D. Chest compressions | 61 (21) | 86 (14) | 26 (23) |
| 1. After rapid delivery, a newborn is apneic, limp, and blue with a heart rate of 40. The amniotic fluid is clear. In what order should the following steps be performed if the newborn continues to fail to respond? | 81 (39) | 93 (25) | 12 (42) |
| 2. Chest compressions must always be accompanied by: | 81 (39) | 94 (23) | 13 (40) |
| 3. When coordinating positive-pressure ventilation with chest compressions, approximately how many of each are performed each minute: | 49 (50) | 86 (35) | 37 (56) |
| 4. Which of the following is an appropriate depth to depress the sternum while performing cardiac compressions on a newborn | 72 (45) | 95 (22) | 24 (50) |
| 5. The person performing the chest compressions should assist the person performing ventilation by | 58 (50) | 93 (26) | 36 (52) |
| 6. When performing chest compressions on a newborn, ventilations should be given at what rate | 52 (50) | 86 (35) | 35 (50) |
| 7. Which of the following is NOT a potential danger of administering chest compressions? | 72 (45) | 89 (31) | 18 (50) |
| 8. Once you have initiated well-coordinated chest compressions and ventilations, how soon should you stop to recheck the newborn’s heart rate? | 48 (50) | 74 (44) | 28 (65) |
| 9. A newborn initially required chest compressions, but a recheck reveals a heart rate of 70 beats per minute. What should you do? | 56 (50) | 84 (37) | 28 (58) |
| 10. Chest compressions consist of rhythmic compressions of the sternum that … | 37 (49) | 67 (47) | 32 (65) |
| 11. Immediately after delivery, a newborn is blue, floppy, and apneic. The newborn does not respond to stimulation, and the heart rate is 40 beats per minute. Which of the following is most likely to restore a spontaneous normal heart rate? | 82 (39) | 92 (28) | 10 (44) |
| 12. Which of the following increases the safety and efficacy of chest compressions? | 59 (49) | 91 (29) | 33 (54) |
| 13. Which is a TRUE statement about coordinated chest compressions and positive- pressure ventilation? | 52 (50) | 83 (37) | 33 (60) |
| 14. For the thumb technique and the 2-finger technique, you should: | 64 (48) | 93 (26) | 28 (54) |
n = 127.
Paired t tests were conducted to compare scales at pre- versus post-test and McNemar’s tests were used to compare items at pre- versus post-test.
Comparisons of scores with time were significant at P < .05 for all items and scales except the following: A9 (P < .35), A11 (P = .12), A13 (P = .209), B2 (P = .06), C5 (P = .06), and C14 (P = .27).
Appendix 2.
Percentage of items performed correctly on the performance evaluation
| Item | Pre-test Mean (SD) | Post-test Mean (SD) | Post-test–pre-test Mean (SD) |
|---|---|---|---|
| Overall performance evaluation | 43 (21) | 88 (9) | 45 (21) |
| A. Initial steps | 60 (18) | 87 (11) | 26 (20) |
| 1. Indicates use of (universal) standard precautions | 35 (48) | 78 (42) | 43 (58) |
| 2. Prepares for warming | 94 (24) | 98 (12) | 5 (28) |
| 3. Prepares for positioning or for clearing airway | 76 (43) | 93 (26) | 17 (48) |
| 4. Prepares for ventilation | 76 (43) | 98 (15) | 22 (47) |
| 5. Prepares medications | 47 (50) | 72 (45) | 25 (63) |
| 6. Determines need for the initial steps of resuscitation | 46 (50) | 76 (43) | 31 (61) |
| 7. Places baby on preheated radiant warmer or on mother with neck slightly extended | 79 (41) | 90 (30) | 11 (49) |
| 8. Clears mouth and nose | 80 (41) | 94 (23) | 15 (44) |
| 9. Dries the baby | 65 (48) | 98 (15) | 33 (49) |
| 10. Removes wet linen | 42 (50) | 84 (37) | 42 (51) |
| 11. Slaps foot, flicks heel, or rubs back briefly | 26 (44) | 72 (45) | 46 (60) |
| B. Ventilation | 34 (27) | 88 (12) | 53 (28) |
| 12. Chooses correct size mask or positions the bag | 46 (50) | 92 (27) | 46 (57) |
| 13. Checks the seal | 26 (44) | 86 (35) | 60 (51) |
| 14. Positions the head and applies the face mask | 46 (50) | 96 (20) | 50 (52) |
| 15. Checks for and removes secretions | 43 (50) | 92 (27) | 49 (59) |
| 16. Ventilates with mouth slightly open | 26 (44) | 79 (41) | 53 (59) |
| 17. Increases ventilation pressure | 20 (41) | 75 (44) | 54 (55) |
| 18. Ventilates 30 seconds at a rate of 40–60 times/min | 35 (58) | 87 (34) | 52 (59) |
| 19. Achieves visible rise and fall of the chest | 31 (47) | 90 (30) | 58 (54) |
| 20. Asks for help to administer chest compressions | 43 (50) | 94 (24) | 51 (52) |
| 21. Continues positive pressure ventilation | 57 (50) | 95 (21) | 39 (52) |
| 22. Checks the heart rate by palpation or stethoscope | 27 (44) | 85 (36) | 58 (53) |
| 23. Checks to ensure adequate chest movement | 25 (44) | 87 (34) | 61 (54) |
| 24. Coordinates ventilations and chest compressions appropriately | 20 (40) | 81 (39) | 61 (52) |
| C. Chest compressions | 28 (33) | 93 (14) | 65 (35) |
| 25. Locates appropriate position on lower one-third of baby’s sternum | 38 (49) | 95 (21) | 58 (53) |
| 26. Provides firm support for baby’s back | 31 (47) | 93 (26) | 61 (50) |
| 27. Uses fingertips or ring fingers or distal portion of both thumbs | 27 (44) | 94 (24) | 67 (50) |
| 28. Compresses sternum approximately one-third of the anterior-posterior diameter of the chest | 20 (40) | 92 (27) | 72 (48) |
| 29. Maintains cadence of “one- and two- and three- and breathe- and..”. | 25 (44) | 92 (27) | 67 (49) |
n = 127.
Paired t tests were conducted to compare scales at pre- versus post-test and McNemar’s tests were used to compare items at pre- versus post-test. Comparisons for all scales and items were significant at P < .05, except item A2 (P < .06).
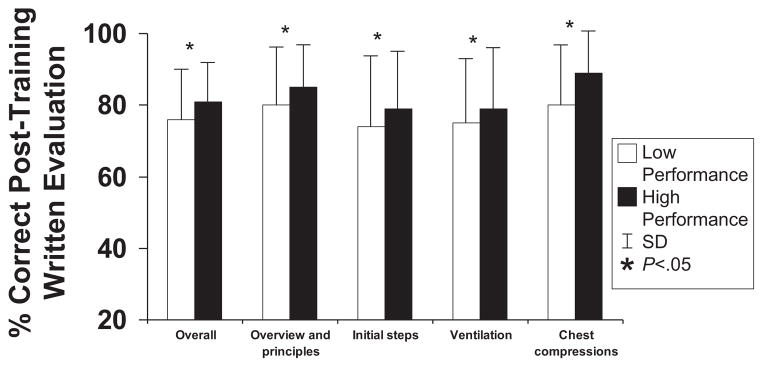
The comparisons of mean written evaluation scores by birth attendants with high and low scores on the performance evaluation at post-training are shown in the on line material (Appendix 3; available at www.jpeds.com). As might be expected, birth attendants in the high performance group had significantly higher scores (P < .05) on the written evaluation overall and all the subscales, except the Ventilation subscale.
Appendix 3.
Comparison of post-training written evaluation scores according to high vs. low scores on post-training performance evaluation. High performance is a score of 85 or higher on the performance evaluation at post-training. The comparisons of low vs. high score on performance evaluation were statistically significant (P < .05) for all scores of the written evaluation except for the bag and mask.
The pre-training score average for the self-efficacy test was the highest of any scale, but also increased from 3.7 ± 0.7 to 4.5 ± 0.5 on a scale of 1 to 5, or an average of 68% ± 17% to 87% ± 12% (both P < .001) of the total possible maximum score (Table I). Participants’ scores on the self-efficacy scale increased for each of the items (Appendix 4; available at www.jpeds.com) after the training. Self-efficacy scores for “Initial Steps” and “Ventilation” were highest before training and increased the least after training. The largest increases in self-efficacy were in the most advanced aspects of resuscitation (Intubation, Medications), although they were not the focus of the training (Figure 1).
Appendix 4.
Means (and SDs) of items on self-efficacy scale
| Item | Pre-test Mean (SD) | Post-test Mean (SD) | Post-test–Pre-test Mean (SD) |
|---|---|---|---|
| Overall self-efficacy score | 3.7 (0.7) | 4.5 (0.5) | 0.8 (0.8) |
| 1. I am able to recognize the need for resuscitation | 4.4 (0.8) | 4.9 (0.5) | 0.4 (0.9) |
| 2. I am able to initiate a resuscitation | 4.1 (0.9) | 4.8 (0.5) | 0.7 (1.0) |
| 3. I am able to successfully complete a resuscitation | 3.8 (0.9) | 4.7 (0.6) | 0.9 (1.1) |
| 4. I can suction the baby | 4.6 (0.7) | 4.9 (0.4) | 0.3 (0.8) |
| 5. I can provide bag and mask ventilation | 4.3 (0.8) | 4.8 (0.5) | 0.6 (0.9) |
| 6. I can recognize the need to intubate a baby | 3.3 (1.2) | 4.3 (1.0) | 1.0 (1.4) |
| 7. I can intubate a baby | 1.9 (1.2) | 2.6 (1.5) | 0.7 (1.5) |
| 8. I can recognize the need for chest compressions | 3.6 (1.0) | 4.7 (0.6) | 1.1 (1.2) |
| 9. I can give chest compressions | 3.6 (1.1) | 4.7 (0.6) | 1.1 (1.3) |
| 10. I can recognize the need for epinephrine | 2.7 (1.2) | 4.2 (1.0) | 1.5 (1.4) |
| 11. I can recognize shock | 3.7 (1.2) | 4.3 (0.8) | 0.6 (1.1) |
| 12. I can administer fluid | 3.1 (1.4) | 3.9 (1.4) | 0.7 (1.4) |
| 13. I can identify a baby who has been successfully resuscitated | 4.3 (0.8) | 4.8 (0.5) | 0.5 (1.0) |
| 14. I can recognize a baby that needs additional ongoing care | 4.3 (0.8) | 4.9 (0.5) | 0.5 (0.9) |
n = 127.
Scores range from 1 (not very confident) to 5 (very confident).
Paired t tests comparing scores from pre- to post-test were significant for all items (P < .001).
Figure 1.
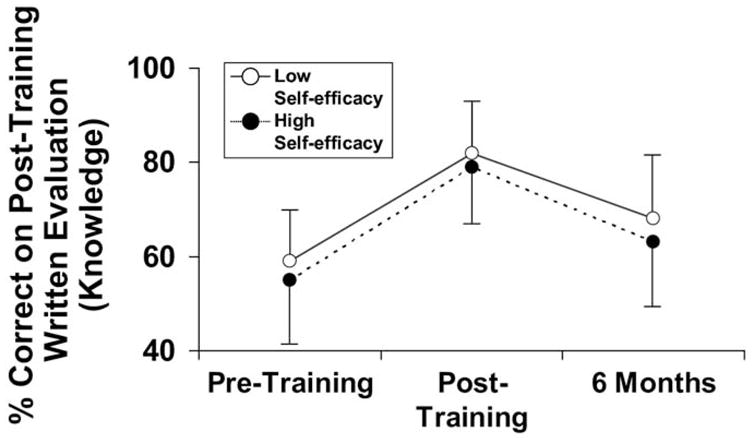
Model-adjusted mean written (knowledge) evaluation scores by self-efficacy. Self-efficacy scores did not affect the written evaluation scores. Time × self-efficacy interaction: χ2(2) = 1.01; P = .64.
The mean evaluation scores at each time point for the birth attendants who participated in the 6-month follow-up are shown on Table II. Scores on all 3 evaluations increased significantly from pre-training to post-training. Written and performance evaluation scores declined from post-training to 6-month follow-up, but remained significantly higher than pre-training scores.
Table II.
Percentage of items answered correctly on written and performance evaluations and mean self-efficacy ratings for birth attendants participating in the 6-month follow-up
| Item | Pre-training mean (SD) | Post-training mean (SD) | 6-month mean (SD) |
|---|---|---|---|
| Written evaluation | |||
| Overall*‡ | 59 (15) | 86 (10) | 62 (16) |
| Overview and principles of resuscitation*‡ | 58 (22) | 84 (13) | 62 (20) |
| Initial steps in resuscitation*‡ | 56 (21) | 87 (13) | 65 (24) |
| Ventilation*‡ | 60 (14) | 87 (12) | 58 (18) |
| Chest compressions*‡ | 65 (17) | 91 (10) | 68 (18) |
| Performance evaluation | |||
| Overall*†‡ | 55 (21) | 90 (8) | 80 (19) |
| Initial steps*† | 66 (20) | 88 (11) | 83 (15) |
| Ventilation*†‡ | 50 (25) | 89 (11) | 75 (25) |
| Chest compressions*†‡ | 43 (36) | 95 (10) | 82 (23) |
| Self-efficacy*† | |||
| Overall | 3.6 (0.7) | 4.3 (0.7) | 4.2 (0.5) |
n = 33.
Pre- verus post-test comparison significant (P < .05).
Pre-test vs. 6 month comparison significant (P < .05).
Post-test vs. 6 month comparison significant (P < .05).
With generalized linear models, we explored possible differences in changes in skills with time for birth attendants with high self-efficacy versus birth attendants with low self-efficacy (highest 50% versus lowest 50%). As suggested by non-significant time by self-efficacy interaction term (P = .6), the 2 groups had similar patterns of change in written evaluations with time (Figure 1).
A slightly different pattern emerges for the performance evaluation scores for which the interaction term is significant (P = .04; Figure 2). The high and low self-efficacy groups have similar levels of improvement in scores from pre- to post-training. However, the low self-efficacy group retained their skills (maintained the performance scores from 88% ± 10% to 86% ± 15%) from post-training to 6-month follow-up, whereas the high self-efficacy group experienced a decline in performance scores (from 88% ± 7% to 74% ± 21%) during the same period.
Figure 2.
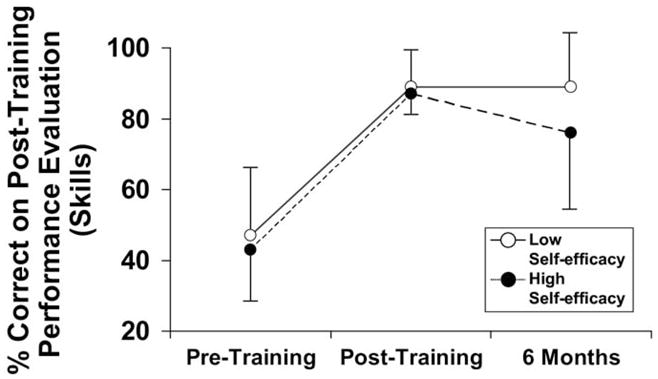
Model-adjusted mean performance (skills) evaluation scores by self-efficacy. The low self-efficacy participants retained their skills for post-training to 6-month evaluations, whereas participants scoring high on the self-efficacy scores evaluation had a decline in scores after post-training. Time × self-efficacy interaction: χ2(2) = 6.05; P = 0.04.
DISCUSSION
We report a comprehensive evaluation of the educational impact of NRP training in the developing world to address several domains of educational outcomes. All 3 evaluations had acceptable internal consistency and thus were valid evaluations of knowledge, skills, and self- efficacy of resuscitation. The improvements in scores between the pre-training period and post-training period demonstrated that the NRP training significantly increased scores on evaluations of knowledge, skills, and self-efficacy in midwives despite their earlier advanced formal education and many years of clinical experience. NRP training was more effective in increasing the scores on the performance evaluation than on the written evaluation, although scores of both evaluations were low pre-NRP training. In contrast to the low knowledge and skills scores pre-NRP training, self-efficacy scores were relatively high pre-NRP training; thus, the nurse midwives rated themselves more knowledgeable and skilled than reflected by their evaluations pre-NRP training.
Performance training was most effective; almost all (99%) the participants increased their performance scores by 20% or more. In contrast, only approximately 50% of the participants increased their knowledge or self-efficacy scores by at least 20%. The marked increase in performance scores may reflect the effectiveness of NRP training’s emphasis on psychomotor skills. The high self-efficacy scores pre-training despite the low knowledge and skills scores are concerning because clinicians may not believe they need the training. Furthermore, self-efficacy scores were not predictive of written or performance evaluation scores or their improvement with training. It is also concerning that birth attendants with high self-efficacy had a decline in performance scores 6 months post-training. However, in birth attendants with low self-efficacy, the performance scores remained high 6 months post-NRP training.
Although this study was well designed for a broad assessment of the effect of NRP training on a body of knowledge, skills, and self-efficacy attitudes, it has several important limitations. We used the standard NRP written evaluation materials although the midwives had limited opportunities for advanced resuscitation because they worked in low-risk delivery centers. The smaller increase in written versus performance scores may reflect a difficulty with written test skills although the midwives were college-educated. In evaluating performance, the unmasked observer who recorded the midwives’ skills was aware of whether the test was pre-training or post-training. However, because the performance evaluation had a checklist of skills and specific coding instructions, the potential for bias was limited. Although there was acceptable internal consistency of the evaluations, another limitation is that the performance and self-efficacy evaluations have not been thoroughly validated before implementation and, therefore, may need further testing to document their validity in assessing skills and self-efficacy. A potential confounder to the study was the wide range of the midwives’ years of practice; because of sample size limitations, subgroup analysis was not planned. However, the midwives shared the same foundation of a college education and some resuscitation training. Such variety in years of practice is difficult to avoid with any group of individuals and may suggest good generalizability because NRP training had such a consistent effect on all 3 areas tested.
Most studies of the effectiveness of NRP have been performed in developed countries.17–22 Typically, these studies were conducted in hospitals in which NRP was taught to residents and other healthcare providers with advanced levels of education. In this setting, NRP was effective in improving educational outcomes. A study to evaluate knowledge gained by pediatric residents during NRP showed comparable improvement by pediatric residents in both a developed and in a developing country.23 Two other studies have documented the educational effectiveness of resuscitation (but not NRP) training to primary healthcare providers in very low-resource countries.11,12 This study used carefully designed evaluation tools to determine whether NRP training would have the same beneficial impact in low-resource environments. Judging from the large effects on educational outcomes, it can be inferred that NRP training can effectively increase resuscitation knowledge, skills, and self-efficacy of midwives in developing countries.
Although NRP training may improve test scores acutely, several studies show that knowledge is lost as early as 3 to 5 months after training.11,17,19,24 Some studies advocate for boosters to improve knowledge and performance.19 Maintaining midwives’ knowledge and skills through retraining or reinforcement could be pivotal to maintaining the high levels of resuscitation skills in midwives required to improve infant mortality. Ultimately, the effect of NRP on patient’ outcomes depends on retention of the knowledge and skills learned and their correct application. Finally, it is necessary to evaluate the effect of resuscitation training on the quality of care, neonatal outcomes, and cost effectiveness.11,25,26 To date, there have been only limited studies to determine whether resuscitation training reduces neonatal mortality and other important adverse outcomes, and those results are inconclusive.10 Whether NRP training is sufficient to significantly reduce neonatal mortality in developing countries needs further evaluation.
In summary, this study shows low written and performance scores pre-NRP training despite earlier advanced formal education and long-term clinical practice, but relatively high self-efficacy scores in midwives in a developing country. NRP training increased scores in all 3 scales evaluated, but retention of knowledge and performance skills decreased significantly by 6 months post-training. Further research is needed to determine optimal timing for retraining in NRP in different clinical settings. NRP training has the potential to substantially improve knowledge and skills of neonatal resuscitation.
Acknowledgments
Supported by the NICHD Global Network for Women’s and Children’s Health Research (HD43475, HD404636) and the Bill and Melinda Gates Foundation.
Footnotes
The authors declare no conflicts of interest.
References
- 1.Lawn J, Cousens S, Zupan J. 4 million deaths. When? Where? Why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 2.Zhu XY, Fang HQ, Zeng SP, Li YM, Lin HL, Shi SZ. The impact of the Neonatal Resuscitation Program Guidelines (NRPG) on the neonatal mortality in a hospital in Zhuhai, China. Singapore Med J. 1997;38:485–7. [PubMed] [Google Scholar]
- 3.Deorari AK, Paul VK, Singh M, Vidyasagar D Medical Colleges Network. Impact of education and training on neonatal resuscitation practices in 14 teaching hospitals in India. Ann Trop Paediatr. 2001;21:29–33. [PubMed] [Google Scholar]
- 4.Safe Motherhood Unit. Basic newborn resuscitation: a practical guide. Geneva: World Health Organization; 1997. [Google Scholar]
- 5.Wegman ME. Annual summary of vital statistics—1990. Pediatrics. 1991;88:1081–92. [PubMed] [Google Scholar]
- 6.Guyer B, Hoyert DL, Martin JA, Ventura SJ, McDorman MF, Strobino DM. Annual summary of vital statistics—1998. Pediatrics. 1999;104:1229–46. doi: 10.1542/peds.104.6.1229. [DOI] [PubMed] [Google Scholar]
- 7.Anonymous Improved neonatal resuscitation by TBAs. Afr Health. 1995;17:27. [PubMed] [Google Scholar]
- 8.Bang AT, Bang RA, Baitule SB, Reddy HM, Deshmukh MD. Management of birth asphyxia in home deliveries in rural Gadchiroli: the effect of two types of birth attendants and of resuscitation with mouth-to-mouth, tube-mask or bag-mask. J Perinatol. 2005;25:S82–91. doi: 10.1038/sj.jp.7211275. [DOI] [PubMed] [Google Scholar]
- 9.O’Hare BA, Nakakeeto M, Southall DP. A pilot study to determine if nurses trained in basic neonatal resuscitation would impact the outcome of neonates delivered in Kampala, Uganda. J Trop Pediatr. 2006;52:376–9. doi: 10.1093/tropej/fml027. [DOI] [PubMed] [Google Scholar]
- 10.Dempsey EM, Barrington KJ, Ryan A. The effectiveness of neonatal resuscitation training programs. [Accessed September 17, 2008];Pediatr Res. Available at: http://www.abstracts2view.com/pas.
- 11.Singhal N, McMillan DD, Yee WH, Akierman AR, Yee YJ. Evaluation of the effectiveness of the standardized neonatal resuscitation program. J Perinatol. 2001;21:388–92. doi: 10.1038/sj.jp.7210551. [DOI] [PubMed] [Google Scholar]
- 12.Couper ID, Thurley JD, Hugo JF. The neonatal resuscitation training project in rural South Africa. Rural Remote Health. 2005;5:459–69. [PubMed] [Google Scholar]
- 13.Zaichkin J, Kattwinkel J, editors. Neonatal resuscitation instructor’s manual. 3. ELK Grove Village, IL: American Academy of Pediatrics, American Heart Association; 2000. [Google Scholar]
- 14.Kattwinkel J, editor. Neonatal resuscitation textbook. 4. Elk Grove Village, IL: American Academy of Pediatrics, American Heart Association; 2000. [Google Scholar]
- 15.Niermeyer S, Kattwinkel J, Van Reempts P, Nadkarni V, Phillips B, Zideman D, et al. International guidelines for neonatal resuscitation: an excerpt from the guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care: international consensus on science. [Accessed September 17, 2008]; doi: 10.1542/peds.106.3.e29. Available at: pediatrics.org/cgi/content/full/106/3/e29; neonatal resuscitation. [DOI] [PubMed]
- 16.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 17.Trevisanuto D, Ferrarese P, Cavicchioli P, Fasson A, Zanardo V, Zacchello F. Knowledge gained by pediatric residents after neonatal resuscitation program courses. Paediatr Anaesth. 2005;15:944–7. doi: 10.1111/j.1460-9592.2005.01589.x. [DOI] [PubMed] [Google Scholar]
- 18.Levitt C, Kaczorowski J, Outerbridge E, Jimenez V, Connolly B, Slapcoff B. Knowledge gained following Neonatal Resuscitation Program courses. Fam Med. 1996;28:403–6. [PubMed] [Google Scholar]
- 19.Kaczorowski J, Levitt C, Hammond M, Outerbridge E, Grad R, Rothman A, et al. Retention of neonatal resuscitation skills and knowledge: a randomized controlled trial. Fam Med. 1998;30:705–11. [PubMed] [Google Scholar]
- 20.Curran VR, Khalid A, O’Young S, Bessell C. Evaluation of the effect of a computerized training simulator (ANAKIN) on the retention of neonatal resuscitation skills. Teach Learn Med. 2004;16:157–64. doi: 10.1207/s15328015tlm1602_7. [DOI] [PubMed] [Google Scholar]
- 21.Dunn S, Nidal P, Watters NE, McGrath P, Alcock D. The provision and evaluation of a neonatal resuscitation program. J Cont Ed Nursing. 1992;23:118–26. doi: 10.3928/0022-0124-19920501-08. [DOI] [PubMed] [Google Scholar]
- 22.Ergenekon E, Koc E, Atalay Y, Soysal S. Neonatal resuscitation course experience in Turkey. Resuscitation. 2000;45:225–7. doi: 10.1016/s0300-9572(00)00179-9. [DOI] [PubMed] [Google Scholar]
- 23.Trevisanuto D, Ibrahim SA, Doglioni N, Salvadori S, Ferrarese P, Zanardo V. Neonatal resuscitation courses for pediatric residents: comparison between Khartoum (Sudan) and Padova (Italy) Paediatr Anaesth. 2007;17:28–31. doi: 10.1111/j.1460-9592.2006.02001.x. [DOI] [PubMed] [Google Scholar]
- 24.Trevisanuto D, Ferrarese P, Cavicchioli P, Fasson A, Zanardo V, Zacchello F. Knowledge gained by pediatric residents after neonatal resuscitation program courses. Paediatr Anaesth. 2005;15:944–7. doi: 10.1111/j.1460-9592.2005.01589.x. [DOI] [PubMed] [Google Scholar]