Indication
Dabigatran etexilate [1, 2] is registered for the prevention of thromboembolic events in patients who have received hip or knee surgery. The indication is limited, but might be extended in the future, for example to prevention of stroke and thromboembolic events in general. Recent studies have compared the effects of warfarin and dabigatran in patients with atrial fibrillation [3] and acute venous thromboembolism [4]. However these results are still under debate [5].
Mechanism
Dabigatran etexilate is the only direct thrombin inhibitor clinically available for oral administration. The active compound dabigatran is hardly absorbed from the gastrointestinal tract. However, the prodrug dabigatran etexilate had been identified as a substrate for the P-glycoprotein transporter.
Dabigatran is a potent, synthetic, reversible, non-peptide thrombin inhibitor. The inhibition of thrombin results in decreased formation of fibrin and reduces thrombin-stimulated platelet aggregation and thus prevents the formation of thrombi. Dabigatran inhibits both free and fibrin-bound forms of thrombin, as well as thrombin-induced platelet aggregation.
Dabigatran etexilate is administered orally once daily. The anticoagulant effect is predictable and depends on the dose. Monitoring by laboratory tests (analogous to INR) is not required in routine situations. No pharmacokinetic drug–drug interactions are currently known.
Adverse effects
The main toxic effect of the drug known so far is bleeding, in common with other anticoagulants. The frequency of severe bleeding compared with bleeding caused by warfarin is still an issue of discussion [5]. Gastrointestinal problems (nausea, vomiting and constipation) and vascular problems (oedema and deep vein thrombosis) have been described. Compared with warfarin, dabigatran etexilate is 10–30 times more expensive.
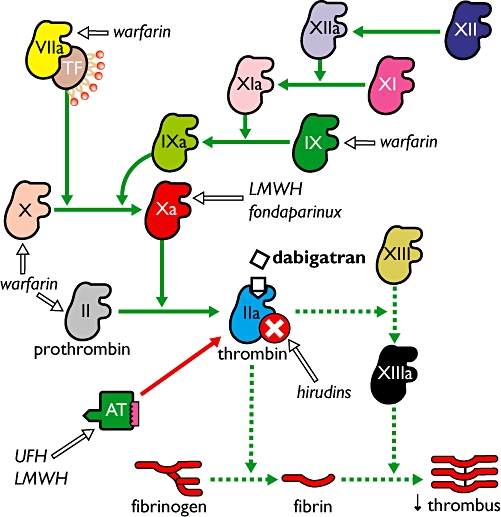
Dabigatran inhibits thrombin directly thereby preventing the formation of a thrombus. Other anticoagulants (warfarin, low molecular weight heparin (LMWH), unfractioned heparin (UFH), fondaparinux, and hirudins (parenterally administered direct thrombin inhibitors)) and their targets are also indicated in the graphic. TF, tissue factor; AT, anti-thrombin; the roman numbers represent the different clotting factors.
Literature
- 1. http://www.emea.europa.eu/humandocs/Humans/EPAR/pradaxa/pradaxa.htm.
- 2.Eriksson BI, Smith H, Yasothan U, Kirkpatrick P. Fresh from the pipeline: dabigatran etexilate. Nat Rev Drug Discov. 2008;7:557–8. doi: 10.1038/nrd2622. [DOI] [PubMed] [Google Scholar]
- 3.Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner JD, Wallentin L RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 4.Schulman S, Kearon C, Kakkar AK, Mismetti P, Schellong S, Eriksson H, Baanstra D, Schnee J, Goldhaber CZ for the RE-COVER Study Group. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361:2342–52. doi: 10.1056/NEJMoa0906598. [DOI] [PubMed] [Google Scholar]
- 5.Houston DS, Zarychanski R. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:2671–5. doi: 10.1056/NEJMc0909962. [DOI] [PubMed] [Google Scholar]


