ABSTRACT
Purpose: To identify the educational needs of adults who undergo total hip and total knee replacement surgery.
Methods: A qualitative research design using a semi-standardized interviewing method was employed. A purposive sampling technique was used to recruit participants, who were eligible if they were scheduled to undergo total hip or total knee replacement or had undergone total hip or total knee replacement in the previous 3 to 6 months. A comparative contrast method of analysis was used.
Results: Of 22 potential participants who were approached, 15 participated. Five were booked for upcoming total hip or total knee replacement and 10 had undergone at least one total hip or total knee replacement in the previous 3 to 6 months. Several themes related to specific educational needs and factors affecting educational needs, including access, preoperative phase, surgery and medical recovery, rehabilitation process and functional recovery, fears, and expectations counterbalanced with responsibility, emerged from the interviews.
Conclusions: Educational needs of adults who undergo total hip and knee replacement surgery encompass a broad range of topics, confirming the importance of offering an all-inclusive information package regarding total hip and total knee replacement.
Key Words: educational needs, patient education, qualitative research, total hip arthroplasty, total knee arthroplasty
RÉSUMÉ
Objectif : Établir les besoins éducatifs des adultes qui subissent une chirurgie de remplacement total ou partiel de la hanche ou du genou.
Méthode : Recherche qualitative, pour laquelle on a eu recours à une méthode d'entrevue semi-standardisée. Une technique d'échantillonnage au jugé a été utilisée pour le recrutement des participants, qui étaient admissibles s'ils étaient appelés à subir une chirurgie de remplacement total ou partiel de la hanche ou du genou ou s'ils avaient subi une telle intervention au cours des derniers trois à six mois. Une méthode d'analyse comparative par contraste a été utilisée.
Résultats : Des 22 participants pressentis pour cette étude, 15 y ont finalement pris part. Cinq personnes devaient subir une chirurgie de remplacement total de la hanche ou du genou et dix avaient subi une chirurgie pour le remplacement total d'au moins un genou ou une hanche au cours des derniers trois à six mois. Plusieurs questions, portant notamment sur l'accès, les phases préopératoires, l'opération elle-même et le rétablissement, le processus de réadaptation et la récupération fonctionnelle, les peurs et les attentes en regard des responsabilités se sont dégagées des entrevues sur les besoins éducatifs précis et sur les facteurs qui affectent de tels besoins.
Conclusions : Les besoins éducatifs des adultes qui subissent une chirurgie de remplacement total ou partiel de la hanche ou du genou englobent un large éventail de sujets, ce qui vient souligner encore davantage l'importance d'offrir une trousse de renseignements complets en la matière.
Mots clés : arthroplastie totale de la hanche, arthroplastie totale du genou, besoins éducatifs, éducation des patients, recherche qualitative
INTRODUCTION
Total joint arthroplasty (TJA) of the hip and knee is a widely accepted, efficacious treatment for patients with advanced arthritis of the hip and knee who have unacceptable levels of pain and/or physical function.1–3 With an increasing burden of arthritis, there is a concomitant increase in the rate of TJA4 in Western countries such as the United States and Canada.5,6
There is evidence that patients undergoing TJA have better outcomes when timely information and education7–17 are delivered preoperatively, including decreased preoperative anxiety,9–15 decreased postoperative pain,10,15 better postoperative coping,16,17 and decreased length of hospital stay.7,8 Comparing the effects of preoperative and postoperative educational programs, prior research found that the preoperative group had higher knowledge levels, performed exercise more regularly, and had improved flexion of the knee joint postoperatively.12
While previous studies have provided evidence supporting the benefits of educating patients undergoing TJA, there is less evidence on the specific content of such education. Johansson et al. collected information from patients in Finland following total hip arthroplasty (THA), using the Canadian Patient Learning Needs Scale.18 The authors found that patients were most interested in information about complications and symptoms, followed by information about medications. In other research, potential candidates for TJA rated the importance of a predetermined list of questions.19 The results showed that patients had the most questions about the effects of surgery on their ability to care for themselves, the need for physical therapy, their mobility after surgery, and when they would walk normally again. Another study, which listed 29 predefined potential concerns, found that the top five concerns about TJA were cancellation of surgery, lack of pain relief, risk of losing the leg, risk of joint infection, and risk of dying. Patients undergoing THA were more concerned than patients undergoing total knee arthroplasty (TKA) about dislocation, return to work, and dressing.20 Other authors recommended addressing concerns such as pain management and bowel problems in preoperative education.21
While most of the previous research on educational needs used quantitative methods, such as surveys, to identify or rank information needs, our literature search found few studies that used a qualitative methodology to ascertain patients' perspectives on their educational needs prior to and following TJA. A qualitative research approach emphasizes meanings, experiences, views, and attitudes of participants; using a qualitative approach enables the researcher to gain a richer understanding of patients' perspectives on what information or education is required.22–25 We felt it was important to allow patients to express their views and needs in an open-ended forum in order to gain a comprehensive understanding of their perspectives, since the results of this study would inform a larger project aimed at developing a Web site (described elsewhere)26 for patients undergoing TJA. For this reason, a qualitative methodology was chosen for the study.
The purpose of our study was to identify specific educational needs of adults who undergo TJA.
METHODS
Semi-structured interviews were used to address the research question “What do patients undergoing TJA want to know?” The research protocol was approved by the Research Ethics Boards of the two participating hospitals, and informed consent was obtained from all participants.
Patient Recruitment
A purposive sampling technique was used, involving identification of participants who possess characteristics or live in circumstances relevant to the phenomenon under study and who are most likely to provide information relevant to the research question.23,27 Potential participants were identified by orthopaedic surgeons located at the two participating hospitals, one an academic hospital and the other a community hospital. Advertisements for the study were posted in the surgeons' offices; patients who expressed interest were then contacted by telephone by one of the two researchers, who explained the details of the study.
Inclusion/Exclusion Criteria
Participants were eligible for this study if they were
scheduled to undergo primary TJA or 3 to 6 months post primary TJA;
able to participate in an interview lasting approximately 1 hour; and
able to understand and converse in English.
Participants in both preoperative and rehabilitative phases were included in the study because it was considered important to gain perspectives from both of these groups, who may have different questions and information needs at different stages of the TJA process. For example, participants in the preoperative phase were asked to describe what information would be important for them as they approached their TJA, while participants in the rehabilitative phase were asked to reflect on what information they had received that was helpful to them and to consider what information (if any) they had not received that would have been helpful. Potential participants with cognitive impairments were excluded from the study; potential participants with other medical comorbidities were not excluded.
Procedure
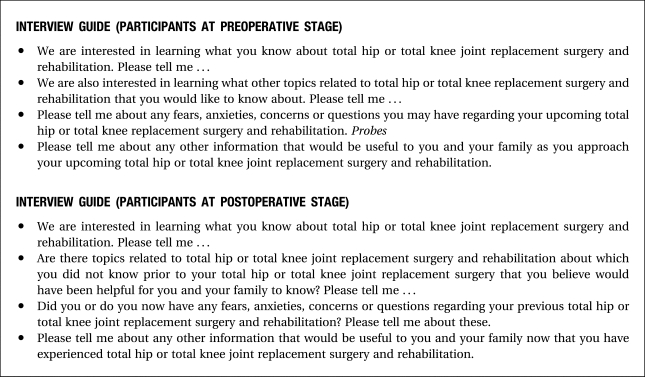
A semi-structured interview method following an interview guide (see Figure 1) was used to gather data. Questions ranged from general to more specific in nature; probes were used to encourage the elaboration of responses. The interviews were conducted by two investigators (LS and CM), both physiotherapists who had qualitative research experience. Prior to each interview, an informed consent process was undertaken, and all participants signed consent forms. The interviews were conducted at a time and location chosen by and convenient for each participant. The interviews were tape-recorded and were transcribed verbatim by a professional transcriptionist. Following each interview, the researchers recorded a summary of any conversations with the participant before and after the interviews that had not been tape-recorded. Data collection continued until saturation was reached (i.e., when no new data emerged from subsequent interviews);27 in this case, no new data emerged from the last three interviews.
Figure 1.
Interview guide
Each participant was assigned a unique identifier to ensure confidentiality. Names were omitted from transcriptions, and unique identifiers used instead. The data were entered into QSR NUD*IST® N5 (QSR International (Americas) Inc., Cambridge, MA), a software package used to help organize qualitative data.
Data Analysis
A comparative contrast method of analysis28 was used. The transcript of each interview was analyzed upon completion and prior to interviewing the next participant, to allow for identification of emergent themes and to identify any possible need to modify the interview guide. This “analyze as you go” method contributed to the rigour of the study by providing opportunities to discover whether the original questions turned up unexpected and interesting data and, if so, to pursue these data via further questions.27 Transcripts were analyzed line by line using a coding process that identified words and groups of words that addressed the research question. These words and groups of words were organized into themes. Each researcher undertook this exercise independently of the other; the two then met to compare and reconcile an understanding of emergent themes. The initial interview guide was modified to include new questions addressing new and developing themes. The analysis was conducted by the same researchers who conducted the interviews. All findings were discussed at meetings with the entire research team; this discussion allowed for further comparison and reconciliation of emergent themes and was used to minimize bias related to interpretation of results.
RESULTS
Participants
Of the 15 participants, 13 were female, 3 were awaiting a TKA, 2 were awaiting a THA, 3 were post-TKA, and 7 were post-THA. Participants ranged in age from 23 to 89 years.
Emergent Themes
Several themes emerged from the interviews. These themes are included under two broad categories: educational needs and factors affecting educational needs. Participants described how access to information about TJA would enable them to achieve an improved quality of life. Table 1 summarizes the emergent categories with their respective themes.
Table 1.
Emergent Categories and Related Themes
| Educational Needs |
Factors Affecting Educational Needs |
|---|---|
|
|
Educational Needs
The themes in the educational needs category address TJA-related topics about which participants were interested in learning.
Access
Participants specifically indicated a need for information related to how waiting lists are prioritized and whether one's position on the waiting list can change depending on circumstances. These concepts are illustrated by this comment from a participant who was awaiting TJA and experiencing progressively increasing pain:
Is it based on first come, first served, or is it based on priorities? If a priority really begins because [of] acute agony, can that be updated or changed or [do you] stay at the end of the list?
Participants spoke about their struggles to determine the appropriate timing for their TJA:
… to do the surgery, I think, the only question I had was, “When?” since the surgeon was going to decide what.
Stories of waiting as long as possible contrasted with other stories that advocated having the surgery sooner rather than later. Participants often reported deciding to proceed with surgery sooner rather than later after consultation with others who had been through the experience.
Knowing the team
Participants understood that several health care professionals would be involved in their care. Knowing these individuals, including having an understanding of their roles, was deemed very important. Having one member of the team, aside from the surgeon, whom they could consult at various phases of their TJA was also important. For example, one participant commented,
As I told you, knowing the team is … very important and knowing who I can contact other than the receptionist.
Arthritis
Participants also expressed a need for information about types of arthritis, causes, and management of symptoms. The following comments from two participants, relatively young and old and diagnosed with rheumatoid arthritis and osteoarthritis respectively, illustrate the desire for arthritis-related information:
I need more information about the disease … I like sometimes to have more information regarding my age because I'm not the only one—a lot of people are very young with rheumatoid arthritis, the information so far is related more to older people than to younger.
I would like to know what happened to [my joint], why does it go that way, … he says in one of my bones there's a fracture, I don't know why the fracture is … I had a Baker's cyst a year ago and nothing was done about it … they said your body will absorb the fluid in time … does that create this problem?
Preoperative phase
Participants expressed a need to know details of what happens during the preadmission visit, including how long it will take. Participants provided several details about important information that helped them prepare for surgery. They spoke of preparing themselves for the hospital stay and preparing their home environments for their return from the hospital. Specifically, participants were interested in knowing what medications, food, clothes, and toiletries they should bring to the hospital; what preparations need to be made to the home environment, including food and equipment; what exercises, if any, and blood tests need to be done prior to surgery; details about employability in the perioperative period; risks, benefits, and procedures related to blood donation and blood transfusion; and hospital length of stay and discharge destination following the acute-care stay.
Participants also expressed a need for education on pain management at various phases of the continuum, including while awaiting surgery, in the immediate postoperative period, and during the rehabilitation/recovery period. Interest in types of pain management other than medications was evident from the interviews.
Surgery and medical recovery
Participants expressed interest in details of the surgical procedure, including specifics of the prosthesis:
I happen to like to know exactly what is going to happen and what is going and what is staying … and what it is made of, all of those kinds of things.
A need for education on the advantages and disadvantages of bilateral TJA was identified, and participants were also interested in knowing any potential risks or complications associated with unilateral or bilateral TJA.
Education on options available for anaesthesia was identified as important:
… the anaesthetist, for me, is very important, to know what kind of an anaesthetic I am going to receive … how much, the amounts, for how long I'm going to be unconscious … what's going to be the side effect after the anaesthesia, those kinds of questions are very important for me to be resolved before surgery … because anaesthesiology is very important, it's your life in the hands of that person.
Participants spoke about their experiences with thromboses and expressed a desire for education on medications for anticoagulation, anti-embolic stockings, and prevention of thromboses.
Details of surgical wound care, including stitch/staple removal and bathing, were also identified as important:
How can I help the wound to close and be in good condition, I think this is very important to [avoid] infection?
Such education facilitated planning for the return home.
Rehabilitation process and functional recovery
Participants wanted education about positioning to provide comfort and prevent complications. For example, one participant wondered,
How long do I have to live with a pillow between the knees?
Details of therapy and exercises, including type, location, protocols, frequency, and duration, were important information for participants:
During those 3 months, my questions are what am I going to do … I understand I have to make exercises for rehabilitation, I would like to [know] if it's going to be here, if I have to go to the hospital every day or if I have to go somewhere else. Am I going to be directed where to go or [am I] going to have to find on my own—who is going to help me?
Specific details on ability to walk in the immediate postoperative period, as well as during the recovery period, were high priorities for participants, including what gait aids they may be required to use at different phases of their recovery. They were also interested in the practicalities of negotiating stairs. In addition, participants stated that information on precautions related to achieving positive outcomes, avoiding complications, and avoiding revision surgery; medications prior to dentistry; equipment; bathing, pedicures, and personal care; and transportation, driving, and transferring into vehicles would facilitate the rehabilitation process and functional recovery.
Follow-up
Participants were interested in details relating to the period required for recovery. Most frequently, they expressed a need for information about time frames. In reference to a booklet she had received, a participant who had undergone both knee and hip arthroplasties said,
I'm still referring to it but some of my rehab took a little longer than my expectations were. Because I was thinking knee … the rehab for the hip is quite different.
Participants were particularly interested in education about follow-up, as illustrated by the following comment:
… like after I come home, will I still see the doctor? Will I have to go back and see the doctor once in a while? … what [is] the follow-up? … and what he thinks, how he thinks it's coming along?
Educational needs related to employment were most prevalent among younger participants and related to various factors, including
estimated time to recover from surgery and rehabilitate;
rights that patients have in terms of their jobs' being protected and available for them to return to; and
whether certain jobs are even possible following TJA.
Factors Affecting Educational Needs
While participants were specific about the content of the education needed, they also explained why having such education was important.
Knowledge about TJA
Participants awaiting TJA admitted to a lack of knowledge about the surgery and rehabilitation process:
Well, I don't really know that much about [joint replacement], and I never asked [the doctor] anything really about what they were using or what the prosthesis was like, so I don't know, I should know … when I have the next one done I'll try to find out a little bit more about it.
Fears
Some fears expressed by participants related to overall outcome, while others related to specifics of the surgery and rehabilitation (see Table 2). Participants proposed that education related to their specific area of concern would help to alleviate some of their fears; they also acknowledged, however, that with TJA there would always be a degree of apprehension or fear.
Table 2.
Fears
| Related to Overall Outcome | Related to Specifics of the Surgery and Rehabilitation |
|---|---|
|
|
Family information needs
Participants noted that their families and other informal support systems require education on TJA. Participants said that such education would enable families to know how they could help, especially in the home environment:
… it will be good for my husband and my mother to learn more about how they can help me to cope after the surgery and what they can do.
Participants recognized that having help once they were discharged home was often necessary. The two main sources of help described were family or friends and professional caregivers. Absence of family was also noted as having a negative impact on the type and amount of help received. Access to education on what family and friends could do to help and how professional help could be accessed was considered important:
But I do live alone. So I have no help, I mean there's nobody living with me, so that makes a difference…. If I can get somebody to come in once or twice [to help me] take a bath or whatever.
Expectations counterbalanced with responsibility
Participants discussed expectations from two main perspectives: the actual process they would undergo for a TJA, including preparation, surgery, rehabilitation, and recovery; and the impact on their well-being or quality of life. Participants were most definite about expecting an improved quality of life after TJA and less certain about what to expect with the process and the continuum of care:
Well, I can't think of anything else pertaining to the operation … no, I don't know what to expect.
Participants also identified the importance of patients' accepting some responsibility for the success of their TJA. They said that it is important for those contemplating TJA to know that there is responsibility involved on the part of the patient, which was described as involving a positive attitude and expecting to have to “work” at the recovery process.
DISCUSSION
Through their narratives, participants in this study expressed the importance of accessing information on a multitude of topics related to TJA. The information needs identified by participants, at both preoperative and postoperative phases, indicate a desire for readily available information at all phases of the continuum of care, including preoperative, acute, and rehabilitative care. Interestingly, there was no difference in the information needs reported by the preoperative and postoperative groups.
Educational needs previously documented in the literature18–21 were also reported by participants in our study, including information on pain relief and ability to walk. In addition, however, our participants described a multitude of specific educational needs ranging from those related to practical aspects of activities of daily living, such as preparing food ahead of time, to those related to the health care system, such as access to physiotherapy and follow-up by the surgeon after TJA. The vast range of educational needs identified is in keeping with a society that is increasingly consumer driven and has a desire to be informed. The content identified is invaluable for clinicians, including physiotherapists, as they educate and care for patients undergoing TJA. A clinical checklist of educational topics for TJA patients, based on the findings of this study, is shown in Table 3.
Table 3.
Clinical Checklist of Educational Topics for Patients Undergoing TJA
General Educational Needs
|
Preadmission Visit
|
Preoperative Period
|
Surgery
|
Hospital Stay
|
Postoperative Period
|
Rehabilitation Period
|
Follow-Up
|
Other studies using qualitative29,30 and quantitative31,32 methods have determined that patients' expectations should be considered when identifying educational needs, because incongruence between patients' expectations of the outcome of TJA and their experience of recovery following TJA can be a source of distress. For example, it is important to include information on recovery time, noting that it varies among individuals and may range from weeks to months following TKA. The results of our study confirm that patients' expectations need to be considered and addressed through educational initiatives. Other factors identified by the participants, including level of knowledge, fears, family information needs, and amount of support at home, may also provide valuable insight for practitioners as they develop educational initiatives for patients. Participants noted that factors (including expectations) affecting educational needs may be very individualized, highlighting the importance of providing opportunities for patients to ask questions of health care professionals. This also means that it is important for health care professionals to consider patients' expectations when providing information and answering questions. The fact that participants acknowledged the importance of their role in accepting responsibility demonstrates a desire for empowerment. Patient empowerment, including support for self-management, can be facilitated by addressing patients' expectations and their education needs.
Participants' fears and concerns reflected those identified in other studies,18,20,21 particularly with respect to surgical outcomes and pain. However, participants in this study also identified specific fears related to dependence on others and lack of support, both in the hospital environment and upon discharge home. These findings highlight the importance of patient and family education regarding expectations for recovery and discharge planning.
Most of the emergent themes were consistent across the age range (23–89 years). However, some themes—such as longevity of the TJA, timing of surgery, and follow-up, including issues related to employment—were more prominent among those participants who were relatively young. Formal and informal supports at home, comorbidities, equipment, bathing and pedicure, and recovery period were themes more common among elderly participants.
LIMITATIONS
A limitation of this study was that most participants (13/15) were female. Research has shown that age-standardized rates by sex for hip and knee replacements in Canada are generally higher for women than for their male counterparts (75.8 per 100,000 for women vs. 68.3 per 100,000 for men). While women have higher rates of TJA overall, men have higher rates in some age groups, including people under age 54 for hip replacements and those over age 85 for knee replacements.33 Although the men and women in this study reported similar educational needs, a more equal distribution of male and female participants might have affected the emergent themes. A further limitation was that all participants resided in an urban setting, where services and information may be more readily available than in rural settings. TJA patients from rural settings may have different educational needs and may identify different perspectives on those educational needs that emerged from this study. In addition, this study included only participants who spoke English; non-English-speaking participants might have identified different information needs. Further qualitative and quantitative research is warranted to add to the body of knowledge on educational needs of patients with TJA, including studies using samples of patients in rural settings and those who do not speak English at all or are not fluent in English.
CONCLUSION
In an effort to promote successful outcomes and improved quality of life for patients following TJA, it is recommended that health care professionals provide a comprehensive range of educational information. Availability of information during all phases of the continuum of care, including the preoperative, acute, and rehabilitative phases, is important for patients, families, and caregivers. A clinical checklist of educational topics has been developed to provide practical guidance in settings for patients with TJA (see Table 3).
KEY MESSAGES
What Is Already Known on This Subject
There is evidence that patients with TJA have better outcomes when timely information and education are delivered preoperatively, including decreased preoperative anxiety, decreased postoperative pain, better postoperative coping, and decreased length of hospital stay. While previous studies have provided evidence for the benefits of educating patients undergoing TJA, most of these studies have used quantitative methodologies and have provided minimal evidence on the specific content of education.
What This Study Adds
Through a qualitative methodology, study participants expressed the importance of accessing information on a multitude of specific topics related to TJA. Specific educational needs ranged from those that addressed practical aspects of activities of daily living, such as preparing food ahead of time, to those related to the health care system, such as access to physiotherapy and follow-up by the surgeon after TJA. Based on the educational needs identified by participants in our study, a clinical checklist of educational topics was developed to provide practical guidance in settings for patients with TJA.
Soever LJ, MacKay C, Saryeddine T, Davis AM, Flannery JF, Jaglal SB, Levy C, Mahomed N. Educational needs of patients undergoing total joint arthroplasty. Physiother Can. 2010;62:206–214.
References
- 1.Chang RW, Pelliser JM, Hazen GB. A cost-effective analysis of total hip arthroplasty of osteoarthritis of the hip. J Am Med Assoc. 1996;275:858–65. doi: 10.1001/jama.275.11.858. [PubMed] [Google Scholar]
- 2.Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, et al. Health-related quality of life after knee replacement. J Bone Joint Surg Am. 1998;80:163–73. doi: 10.2106/00004623-199802000-00003. doi: 10.1016/j.joca.2007.02.019. [DOI] [PubMed] [Google Scholar]
- 3.Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. Health-related quality of life outcomes after total hip and knee arthroplasties in a community based population. J Rheumatol. 2000;27:1745–52. [PubMed] [Google Scholar]
- 4.Health Canada. Arthritis in Canada: an ongoing challenge. Ottawa: Health Canada; 2003. [Google Scholar]
- 5.Canadian Joint Replacement Registry [CJRR] 2005 Report: Total Joint Hip and Knee Replacements in Canada. Ottawa: Canadian Institute for Health Information; 2005. [Google Scholar]
- 6.Kurtz SM, Ong KL, Schmier J, Zhao K, Mowat F, Lau E. Primary and revision arthroplasty surgery caseloads in the United States from 1900 to 2004. J Arthroplasty. 2009;24:195–203. doi: 10.1016/j.arth.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 7.Crowe J, Henderson J. Pre-arthroplasty rehabilitation is effective in reducing hospital stay. Can J Occup Ther. 2003;70:88–96. doi: 10.1177/000841740307000204. [DOI] [PubMed] [Google Scholar]
- 8.Kelly MH, Ackerman M. Total joint arthroplasty: a comparison of past acute settings on patient functional outcomes. Orthop Nurs. 1999;18:75–84. [PubMed] [Google Scholar]
- 9.Daltroy LH, Morlino CI, Eaton HM, Poss R, Liang MH. Preoperative education for total hip and knee replacement patients. Arthritis Care Res. 1998;11:469–78. doi: 10.1002/art.1790110607. doi: 10.1002/art.1790110607. [DOI] [PubMed] [Google Scholar]
- 10.Sjoling M, Nordahl G, Olofsson N, Asplund K. The impact of preoperative information on state anxiety, postoperative pain and satisfaction with pain management. Patient Educ Couns. 2003;51:169–76. doi: 10.1016/s0738-3991(02)00191-x. doi: 10.1016/S0738-3991(02)00191-X. [DOI] [PubMed] [Google Scholar]
- 11.Spalding NJ. Reducing anxiety by pre-operative education: make the future familiar. Occup Ther Int. 2003;10:278–93. doi: 10.1002/oti.191. doi: 10.1002/oti.191. [DOI] [PubMed] [Google Scholar]
- 12.Lin PC, Lin LC, Lin JJ. Comparing the effectiveness of different educational programs for patients with total knee arthroplasty. Orthop Nurs. 1997;16:43–9. doi: 10.1097/00006416-199709000-00013. [PubMed] [Google Scholar]
- 13.Butler GS, Hurley CAM, Buchanan KL, Smith-VanHorne J. Prehospital education: effectiveness with total hip replacement surgery patients. Patient Educ Couns. 1996;29:189–97. doi: 10.1016/0738-3991(96)00883-x. doi: 10.1016/0738-3991(96)00883-X. [DOI] [PubMed] [Google Scholar]
- 14.Bondy LR, Sims N, Schroeder DR, Offord KP, Narr BJ. The effect of anesthetic patient education on preoperative patient anxiety. Region Anesth Pain Med. 1999;24:158–64. doi: 10.1016/s1098-7339(99)90078-0. doi: 10.1097/00115550-199924020-00011. [DOI] [PubMed] [Google Scholar]
- 15.Giraudet-Le Quintrec JS, Coste J, Vastel L, Pacault V, Jeanne L, Lamas JP, et al. Positive effect of patient education for hip surgery: a randomized trial. Clin Orthop Relat R. 2003;1:112–20. doi: 10.1097/01.blo.0000079268.91782.bc. [DOI] [PubMed] [Google Scholar]
- 16.Gammon J, Mulholland CW. Effect of preparatory information prior to elective total hip replacement on post-operative physical coping outcomes. Int J Nurs Stud. 1996;33:589–604. doi: 10.1016/s0020-7489(96)00019-3. doi: 10.1016/S0020-7489(96)00019-3. [DOI] [PubMed] [Google Scholar]
- 17.Gammon J, Mulholland CW. Effect of preparatory information prior to elective total hip replacement on psychological coping outcomes. J Adv Nurs. 1996;24:303–8. doi: 10.1046/j.1365-2648.1996.17911.x. doi: 10.1046/j.1365-2648.1996.17911.x. [DOI] [PubMed] [Google Scholar]
- 18.Johansson K, Hupli M, Salantera S. Patients' learning needs after hip arthroplasty. J Clin Nurs. 2002;11:634–9. doi: 10.1046/j.1365-2702.2002.00648.x. doi: 10.1046/j.1365-2702.2002.00648.x. [DOI] [PubMed] [Google Scholar]
- 19.Macario A, Schilling P, Rubio R, Bhalla A, Goodman S. What questions do patients undergoing lower extremity joint replacement surgery have? BMC Health Serv Res. 2003;3:11. doi: 10.1186/1472-6963-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moran M, Khan A, Sochart DH, Andrew G. Evaluation of patient concerns before total knee and hip arthroplasty. J Arthroplasty. 2003;18:442–5. doi: 10.1016/s0883-5403(03)00061-5. doi: 10.1016/S0883-5403(03)00061-5. [DOI] [PubMed] [Google Scholar]
- 21.Barksdale P, Backer J. Health-related stressors experienced by patients who underwent total knee replacement seven days after being discharged home. Orthop Nurs. 2005;24:336–42. doi: 10.1097/00006416-200509000-00009. doi: 10.1097/00006416-200509000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Denzin NK, Lincoln YS. Introduction entering the field of qualitative research. In: Denzin NK, Lincoln YS, editors. Handbook of qualitative research. Thousand Oaks, CA: Sage; 1994. pp. 1–17. [Google Scholar]
- 23.Wright JG, McKeever P. Qualitative research: its role in clinical research. Annales CRMCC. 2000;33(5):275–80. [Google Scholar]
- 24.Martin D, McKneally M. Qualitative research. In: Troidl H, Spitzer W, McKneally M, McPeek B, Mulder D, Wechsler A, et al., editors. Principles and practice of research: strategies for surgeon investigators. New York: Springer; 1998. pp. 235–41. [Google Scholar]
- 25.Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. Brit Med J. 1995;311:42–5. doi: 10.1136/bmj.311.6996.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saryeddine T, Levy C, Davis A, Flannery J, Jaglal S, Hurley L, et al. Patient education as a strategy for provider education and engagement: a case study using myJointReplacement.ca. Healthc Q. 2008;11:84–90. doi: 10.12927/hcq.2013.19502. [DOI] [PubMed] [Google Scholar]
- 27.Mays N, Pope C. Rigour and qualitative research. Brit Med J. 1995;311:109–17. doi: 10.1136/bmj.311.6997.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Strauss AL, Corbin JM. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park, CA: Sage; 1990. [Google Scholar]
- 29.Marcinkowski K, Wong VG, Dignam D. Getting back to the future: a grounded theory study of the patient perspective of total knee joint arthroplasty. Orthop Nurs. 2005;24:202–9. doi: 10.1097/00006416-200505000-00009. [DOI] [PubMed] [Google Scholar]
- 30.Showalter A, Burger S, Salyer J. Patients' and their spouses needs after total joint arthroplasty: a pilot study. Orthop Nurs. 2000;19:49–57. doi: 10.1097/00006416-200019010-00011. [DOI] [PubMed] [Google Scholar]
- 31.Mancuso CA, Sculco TP, Wickiewicz TL, Jones EC, Robbins L, Warren RF, et al. Patients' expectations of knee surgery. J Bone Joint Surg. 2001;83:1005–12. doi: 10.2106/00004623-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Mancuso CA, Sculco TP, Salvati EA. Patients with poor preoperative functional status have high expectations of total hip arthroplasty. J Arthroplasty. 2003;18:972–8. doi: 10.1016/s0883-5403(03)00276-6. doi: 10.1016/S0883-5403(03)00276-6. [DOI] [PubMed] [Google Scholar]
- 33.Canadian Institute for Health Information. Canadian Joint Replacement Registry (CJRR) 2007 annual report—hip and knee replacements in Canada. Ottawa: The Institute; 2008. [Google Scholar]