Abstract
In Karnataka, India only one-third of HIV-infected pregnant women received antiretroviral prophylaxis at delivery in 2007 through the state government’s prevention of parent-to-child HIV transmission (PPTCT) program. The current qualitative study explored the role of HIV-associated stigma as a barrier to accessing PPTCT services in the rural northern Karnataka district of Bagalkot using in depth interviews and focus group discussions with HIV-infected women who had participated in the PPTCT program, male and female family members, and HIV service providers. Participants discussed personal experiences, community perceptions of HIV, and decision-making related to accessing PPTCT services. They described stigma towards HIV-infected individuals from multiple sources: healthcare workers, community members, family and self. Stigma-related behaviors were based on fears of HIV transmission through personal contact and moral judgment. Experience and/or fears of discrimination led pregnant women to avoid using PPTCT interventions. Government, cultural and historical factors are described as the roots of much the stigma-related behavior in this setting. Based on these formative data, PPTCT program planners should consider further research and interventions aimed at diminishing institutional and interpersonal HIV-associated stigma experienced by pregnant women.
Introduction
It is estimated that 2.4 million adults were living with HIV in India in 2007, and that 80% of those individuals were unaware of their diagnosis (UNAIDS, 2008). The state of Karnataka is designated as one of the six high HIV prevalence states in India. Between 2003–2006, 2–2.25% of women presenting for antenatal care in Karnataka were HIV-infected (National AIDS Control Organization, 2007). According to the Karnataka State AIDS Prevention Society (KSAPS) in 2007, only 16% of an estimated 1.2 million pregnant women underwent HIV testing in the government’s PPTCT program, and one-third of mother-infant pairs received peripartum single dose nevirapine (SD NVP) ARV prophylaxis. (R. Washington, personal communication, June 18, 2009)
As in other settings, individuals with HIV in India suffer from stigma and discrimination that affect their access to health care, testing, disclosure, treatment adherence and prognosis (Bharat, Aggleton, & Tyrer, 2001; Mahendra et al, 2007; Steward et al, 2008). Pregnant women often suffer the burden of being HIV-infected, mothers of potentially infected infants, and caregivers of infected husbands or other family members (Bharat & Aggleton, 1999; Thomas, Nyamathi, & Swaminathan, 2008). HIV-infected women may be ostracized from their homes and communities after the death of their husbands (Bharat et al, 1999; Pallikadavath, Garda, Apte, Freedman, & Stones, 2005). This is in direct contrast to generally supportive behaviors for illness demonstrated by family and community members in many cultures (Ankrah, 1993; Bharat et al, 2001). This lack of supportive behavior has been characterized as stigma since family support is considered a fundamental value in Indian society (Green, Devi, & Paulraj, 2004).
Since many women are diagnosed with HIV during pregnancy, it is a critical time to intervene for PPTCT, VCT of male partners and enrollment of women into HIV-care and treatment programs. The purpose of this study is to explore how feared and experienced stigma acts as a barrier to accessing PPTCT-related services.
Conceptual framework
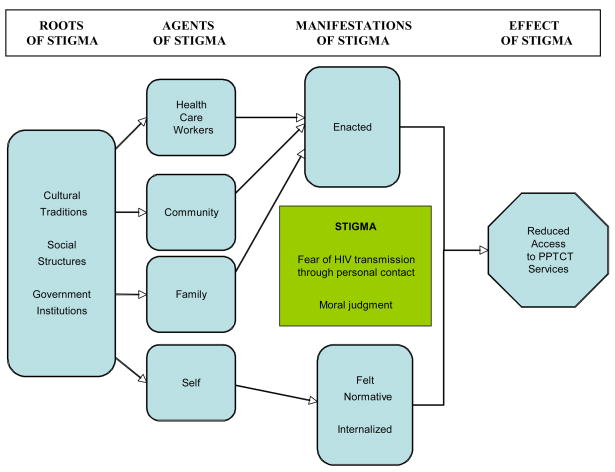
We used a theoretical framework developed by Steward et al. (2008) to understand the roots and effects of HIV-related stigma. Steward’s framework was designed to understand stigma in relation to HIV serostatus disclosure. The framework is based on qualitative research performed in Southern India, and thus is culturally appropriate for our setting. The authors described stigma as enacted (interpersonal experience of stigma), felt normative (awareness of/anticipation of stigma) and internalized or self stigma (acceptance of stigma as valid) (Steward et al., 2008). However, this framework does not clearly delineate role of social, cultural, and governmental institutions as justifications for stigma, which have been shown to be important factors in related analyses of prejudice and stereotyping (Jones, 2000). In this paper we examine the roles of enacted, felt normative and internalized stigma and consider the key actors expressing HIV/AIDS stigma experienced by HIV-infected pregnant women: health care workers, community, family, and self. The conceptual framework of the current study, incorporating all these elements, is presented in Figure 1.
Figure 1. Roots, agents and manifestations of HIV-related stigma and their subsequent effect on access to PPTCT services.
HIV-related stigma (fear of HIV transmission through personal contact and moral judgment) is rooted in cultural traditions, social structures and government institutions in India which influence the chief agents of stigma (health care workers, community members, family and self) described in this study. Ultimately, this stigma (enacted, felt normative, and internalized) serves as a barrier to PPTCT services in this study. Types of stigma are defined as enacted (interpersonal experience of stigma), felt normative (an individual’s awareness of /anticipation of stigma) and internalized (an individual’s acceptance of stigma as valid) based on the theoretical framework by Steward, et al. (2008).
Methods
Recruitment
This is a descriptive, qualitative study of barriers to PPTCT services for pregnant HIV-infected women in the Bagalkot district - one of four administrative district offices of KSAPS - in rural northern Karnataka. At the time of this study, VCT for antenatal patients was available at government hospitals in the six talukas (“subdistricts”) of Bagalkot district. HIV-infected women were then referred to Bagalkot District Hospital for cesarean delivery and SD NVP prophylaxis. Potential participants were identified by the PPTCT health care staff and staff of the nongovernmental organizations (NGOs), India Canada Collaborative HIV/AIDS Project (ICHAP) and Jeevan Jothi (the Bagalkot district network of HIV-infected men and women). We recruited three types of participants: 1) recently delivered (up to 24 months postpartum) women who had HIV infection during pregnancy; 2) partners and other family members who live in the same household as HIV-infected women who have been pregnant ; and 3) staff involved in PPTCT services in Bagalkot district. Audio-taped interviews were conducted by two female social workers trained in qualitative research methods in private rooms at either the Jeevan Jothi office or Bagalkot District Hospital after obtaining signed informed consent for individual in-depth interviews (IDIs) and verbal consent for focus group discussions (FGDs). Ethical approval for the study was obtained from the Committee on Human Research at the University of California San Francisco and ethical review board at St. John’s Medical College in Bangalore.
Interviews and Focus groups
Interview guides for IDIs and FGDs were adapted from previously developed tools for studying acceptance of PPTCT testing in South Africa (Varga C & Brooks H, 2008). This study tool was chosen due to similarities in the contexts, e.g. early stages of the PPTCT programs and the underlying societal discomfort with HIV/AIDS. The tool also incorporated a narrative research method, originally developed by the World Health Organization to study adolescent sexual and reproductive health behavior (Varga C & Brooks H, 2008) (World Health Organization, 1993). By using role-play, participants are able to explore and discuss these sensitive issues. Study instruments were modified based on six key informant discussions with Jeevan Jyothi members, Bagalkot physicians and PPTCT counselors and a focus group discussion with HIV-infected individuals from the community. The instruments were then pilot tested in the community with women living with HIV/AIDS.
The open-ended interview guides for both IDIs and FGDs covered themes such as knowledge, attitudes, and practices regarding HIV/AIDS and PPTCT and HIV-related stigma. During the IDI a narrative exercise was employed which related a story about a women named “Meena” (similar in age and background to the participant) who engages in PPTCT services and is diagnosed with HIV. The participants were asked to anticipate “Meena’s” decisions and perceptions regarding HIV testing, results disclosure, delivery, and infant care practices.
Analysis
An independent staff person transcribed the IDIs and FGDs from the audio-recordings verbatim. The transcriptions were translated from Kannada into English at St. John’s Research Institute (SJRI) by qualified translators. Every transcript and translated document was reviewed by the project coordinator at SJRI for accuracy and completeness of data. Two researchers independently analyzed the data manually by developing appropriate coding schemes using grounded theory techniques and collaboratively generated substantive and conceptual categories. Through an iterative process, researchers read the transcripts, generated codes based on the data, and refined the codes to better reflect the experiences expressed by the participants. After initial review, the primary focus of the analysis became stigma and its association with seeking HIV-related services among HIV-infected women obtaining maternal health services in Bagalkot.
Results
Between January and May 2006 fifteen HIV-infected women who had participated in Bagalkot district’s PPTCT program participated in IDIs. Fourteen of these interviews were analyzed; the recording of one interview not audible. Women were ages 19–30 years; all were married or widowed, and three participants were pregnant again. Most women were illiterate, and all were housewives or farm laborers. Most women lived in two room houses (range 1–4), only seven had an indoor water supply, and all except one practiced open-air defecation. (See Table 1)
Table 1.
Demographic information and socioeconomic background of HIV-infected postpartum women (N=14)
| Age | N (%) |
|---|---|
| 19–24 years | 8 (57.1) |
| 25–30 years | 6 (42.9) |
| Pregnancy status | |
| Currently pregnant | 3 (21.4) |
| Age of infant | |
| <0– 6 months | 3 (21.4) |
| 6–12 months | 4 (28.6) |
| 12–24 months | 7 (50.0) |
| Time of HIV diagnosis * | |
| During pregnancy | 11 (84.6) |
| Before pregnancy | 2 (15.4) |
| Marital status | |
| Living with husband | 8 (57.1) |
| Living with parents (separated) | 4 (28.6) |
| Widowed | 2 (14.3) |
| Education ** | |
| Illiterate/no school | 8 (66.7) |
| Up to 8th grade | 4 (33.3) |
| Access to media | |
| TV | 9 (64.3) |
| Radio | 5 (35.7) |
The timing of one participant’s diagnosis was unclear; denominator is 13.
Education level unknown from 2 participants; denominator is 12.
The three FGDs were conducted with one group of female (five participants), one group of male family members of HIV-infected women (six participants), and one group of HIV service providers (eight participants). The two focus groups with family members included some parents or spouses who have HIV infection. The HIV service providers included five VCT/PPTCT counselors, a PPTCT lab technician, and two administrators.
Initial analyses revealed that logistical barriers to accessing PPTCT services included lack of transportation, lack of staff, and lack of financial resources. Ultimately, women consistently expressed that stigma was an important barrier to accessing HIV-related care at the medical facility, community, and household levels. Actors engaging in enacted, felt normative, and internalized stigma described in this study are categorized as health care workers, community, family and self.
Health Care Workers
Several women described lack of facility and service delivery quality during HIV testing and antenatal/intrapartum care associated with PPTCT services. These included experiences of refusal for treatment, abusive behavior, moral judgment and lack of confidentiality by staff.
I thought that they [the government hospital] would take care of our delivery, but even when I was suffering from stomachache [labor pains], they did not care for me. Even though there were two nurses, they did not treat me, and they told us they are unable to admit for the delivery.. Then the doctor also told us to go to another hospital… (20 year old, 0–6 months postpartum)
During the delivery, there were two nurses and they did not even touch me during delivery even when I was suffering from pain… Even when I was bleeding they did not come to my help. They scolded my grandmother to wipe the blood, and they even did not touch my child.” (26 year old, 12–24 months postpartum)
Community
All study participants described conflict over desires to be open about their HIV infection versus fear of resultant stigma from the community. Stigma-related behaviors ranged from the denial of personal contact or hospitality to being physically removed from one’s own community. Participants literally described this fear of personal contact and treatment like an outcaste in the community by using the word “harijan” or “dalit” (“untouchable”1 in the context of the historical Indian caste system).
I do not think it is advisable for the people infected with HIV/AIDS to tell others about their [HIV] status because if they do so they will be treated as untouchables. They will not be allowed to mingle with other people … They will not be allowed to speak to others. The food they prepare will not be touched by anybody; nor will they [community] give them food. They will not be allowed to touch others, sit with others, etc. (19 year old, 12–24 months postpartum)
Family
Consistent with studies of how social networks are structured within Indian culture and society, a woman’s family—her parents, her husband and his family—were described as an integral component of a woman’s support system to ensure her physical, emotional, and financial wellbeing. However, due to lack of confidentiality practices, family members were frequently the first to be informed by providers of a woman’s HIV test results, thus making a women vulnerable immediately after testing. Moral judgment by family members (in addition to agents noted above) due to a belief that HIV infection was associated with immoral behavior led families to react negatively.
[HIV] spreads from husband to wife and vice versa. But at the in-law’s place, the daughter-in-law is accused of spreading the infection to the son. She might be thrown out of the house. They will not take care of the children or daughter-in-law… (HIV service provider: FGD)
Stigma and abandonment from the husband’s family often contrasted with support from the woman’s own parents. Though participants duly noted the significant emotional, physical, and financial burdens and resulting stigma taken on by parents, they consistently described having little doubt in the support that they would receive from their own mothers and fathers.
Self
IDI participants were all highly knowledgeable regarding HIV infection and transmission due to education via the NGO that recruited for this study. Though this education helped them recognize the injustice of externally derived stigma, their interviews revealed sources for felt normative (awareness of stigma) and potential internalized feelings of stigma (stigma was justifiable or inevitable) for themselves or other HIV-infected individuals in the community.
Though some participants shared and justified similar inaccurate fears as the community regarding HIV transmission via food or personal contact, self stigma was in many cases derived from moral judgment of one’s self for not fulfilling traditional gender roles of wife and mother. Two of the women were widows; four were separated from their husbands. Many had not resumed sexual relations with their husbands. Moral judgment about the woman’s character and fidelity has been described above.
In the role of mother, women judged themselves for being unable to properly care their own children. Participants feared HIV transmission during delivery and through personal contact with their children and wondered whether they would remain healthy enough to care for their children. They described balancing their desire to breastfeed in order to give their newborns the best option for infant feeding according to their own, family and community beliefs versus their fears of HIV transmission or disclosure of serostatus due to formula-feeding.
By breast-feeding the baby, you are sharing your love and affection with it. You are complete only when you become a mother and when you breast-feed the baby. (Female family member: FGD)
Discussion
To our knowledge, this is the first study of the role of stigma in the lives of HIV-infected pregnant women accessing PPTCT services in India. Stigma carried out by health care workers, the community, family and self was isolating; many women felt disclosure of HIV serostatus in order to obtain PPTCT services was not an option. Fear of discrimination and specific personal experience with abuse and denial of services led participants to report stigma as a barrier to HIV testing, accessing PPTCT-related care, and HIV serostatus disclosure at delivery despite understanding the prevention measures necessary for PPTCT. Externally-based stigma was based on both moral judgment and avoidance of personal contact, akin to historical treatment of the untouchable caste. This could then be internalized by participants to feel like they were, indeed, “untouchable” to family or children or to blame for failure to fulfill roles as wives and mothers. In a setting where the role of a woman in the family as a wife and mother is critical to the framework of Indian society, these findings are significant barriers to disclosure of HIV serostatus and subsequent HIV-related care during pregnancy and onwards.
A combination of the theoretical frameworks put forward by Steward et al (2008) and Jones (2000) described above applies well to our discussion regarding HIV-associated stigma and access to PPTCT services in India. Though it would be simple to categorize stigma by health care workers, from community members and within the family as “enacted” (interpersonal) stigma, and self stigma as “felt normative” or “internalized” stigma, it is important to understand their sources are likely deeply rooted in governmental, cultural, and historical institutions.
Government-based stigma was illustrated by the unprofessional behavior of health care workers who provided government-based PPTCT services. Prior research from Indian health care settings supports the study participants’ descriptions of abuse by health care staff (Bharat et al., 2001; Godbole & Mehendale, 2005) and lack of confidentiality of test results (Chandra, Deepthivarma, & Manjula, 2003; Rogers et al., 2006; Mahendra et al., 2007). Another government institution, the Indian Supreme Court, defended a hospital’s decision to disclose HIV serostatus without permission as a public health measure (Kumar, 1998). The moral judgment associated with HIV diagnosis was illustrated in the judge’s statement, “AIDS is a product of indisciplined sexual impulse.”
The cultural expectations that women should uphold the prestige and honor of the family by maintaining impeccable moral character (Bharat & Aggleton, 1999; Desai & Thakkar, 2001) led health care workers, community and family members to make moral judgments against HIV-infected pregnant women. Inability to function as a mother (by breast-feeding or personal contact with child) and wife (due to separation from husband or widowhood) may have also led to self stigma and disgrace, since being a mother and wife is of paramount importance for women in traditional Indian society (Desai & Thakkar, 2001; Sharma, 2008). Therefore, acknowledging potential infection by testing or disclosure during pregnancy or delivery may be prohibitive.
Lack of education regarding HIV transmission risk led to false fear of HIV transmission through personal contact and also lent itself to the comparison of people living with HIV to being “untouchable.” Indeed, negative attitudes and discriminatory behaviors against people living with HIV have led legal scholars, medical ethicists and media to describe HIV-infected individuals as a “new class of untouchables” (Burns, 1996; Krishnan, 2003; Pandya, 1997; Sharma, 2008). Although stigma related to fears of transmission secondary to personal contact occurs in virtually all countries and the special vulnerability of pregnant women to HIV/AIDS stigma and discrimination has been described in different settings around the world (Bond, Chase, & Aggleton, 2002; Thorsen, Sundby, & Martinson, 2008; Turan, Miller, Bukusi, Sande, & Cohen, 2008), India will have to combat an already existing framework of untouchability into which these attitudes and behaviors can be channeled.
This study had several limitations. Interview tools were translated into Kannada and then back translated into English. Though translation was checked by a native Kannada speaker and fluent English speaker, subtle intent or language may have been lost due to translation and in the analytic process. In addition, participants were selected from women currently engaged in HIV support services. Thus, we did not capture directly the experiences of HIV-infected women who do not access PPTCT services. These women, in fact, may be the ones who are suffering most from HIV-related stigma and discrimination.
Conclusions
Feared and experienced stigma by various agents that would normally provide support for HIV-infected pregnant women may create barriers to accessing PPTCT and maternity services in Bagalkot. Though the stigma enacted is similar to other settings in the world, it is combined with cultural and institutional issues unique to India. The findings of this formative research suggest that a multi-component approach is needed to reduce stigma and discrimination and increase access to essential PPTCT services. This approach should include acknowledging the institutional/cultural roots of the problem, examining HIV-related laws and policies, normalizing HIV testing, improving quality of PPTCT services, better training of health care providers in medical ethics and professionalism and community education strategies. Measures such as integration of PPTCT care with already existing antenatal services has already increased the numbers of pregnant women tested and accessing prophylaxis in the government-based PPTCT program in 2008. Women also cited local teachers, elders, health care professionals, NGOs and the media as potential sources of HIV-related information. Using these already available resources, interventions to decrease stigma and discrimination are possible and will be necessary to improve access to PPTCT services for HIV-infected pregnant women in India.
Footnotes
Based on early Hindu epics, a hierarchical social structure designated the lowest caste as “untouchable” or “dalit.” Caste was based on birth and holding occupations that were considered unclean (e.g. road sweepers, toilet cleaners). Physical contact with these individuals by higher caste members of society was forbidden. Due to religious and political reforms, attention to this unethical practice led to protections and anti-discrimination legislation in the 20th century.
References
- Ankrah EM. The impact of HIV/AIDS on the family and other significant relationships: the African clan revisited. AIDS Care. 1993;5:5–22. doi: 10.1080/09540129308258580. [DOI] [PubMed] [Google Scholar]
- Bharat S, Aggleton P. Facing the challenge: household responses to HIV/AIDS in Mumbai, India. AIDS Care. 1999;11:31–44. doi: 10.1080/09540129948180. [DOI] [PubMed] [Google Scholar]
- Bharat S, Aggleton P, Tyrer P. India: HIV and AIDS-related discrimination, stigmatization and denial. Geneva: UNAIDS; 2001. [Google Scholar]
- Bond V, Chase E, Aggleton P. Stigma, HIV/AIDS and prevention of mother-to-child transmission in Zambia. Evaluation and Program Planning. 2002;25(4):347–356. [Google Scholar]
- Burns JF. Virus begets wretched new class of untouchables. New York Times 1996 [Google Scholar]
- Chandra PS, Deepthivarma S, Manjula V. Disclosure of HIV infection in south India: patterns, reasons and reacitions. AIDS Care. 2003;15(207–215) doi: 10.1080/0954012031000068353. [DOI] [PubMed] [Google Scholar]
- Desai N, Thakkar U. Women in Indian Society. New Dehli: National Book Trust; 2001. [Google Scholar]
- Godbole S, Mehendale S. HIV/AIDS epidemic in India: risk factors, risk behaviour and strategies for prevention and control. Indian J Med Res. 2005;121:356–368. [PubMed] [Google Scholar]
- Green DA, Devi S, Paulraj LS. Care centre visits to married people living with HIV: An indicator for measuring AIDS-related stigma & discrimination. AIDS Care. 2004;19:910–915. doi: 10.1080/09540120701203253. [DOI] [PubMed] [Google Scholar]
- Jones CP. Levels of racisom: A theoretic framework and a gardener’s tale. Am J Public Health. 2000;90:1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan JK. The rights of the new untouchables: a constitutional analysis of HIV jurisprudence in India. Human Rights Quarterly. 2003;25:791–819. [Google Scholar]
- Kumar S. Medical confidentiality broken to stop marriage of man infected with HIV. Lancet. 1998;352:1764. doi: 10.1016/S0140-6736(05)79843-3. [DOI] [PubMed] [Google Scholar]
- Mahendra VS, Gilborn L, Bharat S, Mudoi R, Gupta I, George B, Samson L, Daly C, Pulerwitz J. Understanding and measuring AIDS-related stigma in health care settings: A developing country perspective. SAHARA J. 2007;4:616–625. doi: 10.1080/17290376.2007.9724883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National AIDS Control Organization. HIV Fact Sheets: Based on HIV Sentinel Surveillance data from 2003–2006. 2007 Retrieved July 28, 2009 from http://www.nacoonline.org/upload/NACO%20PDF/HIV_Fact_Sheets_2006.pdf.
- Pallikadavath S, Garda L, Apte H, Freedman J, Stones RW. HIV/AIDS in rural India: context and health care needs. J Biosoc Sci. 2005;37:641–655. doi: 10.1017/S0021932004006893. [DOI] [PubMed] [Google Scholar]
- Pandya SN. Patients testing positive for HIV: ethical dilemmas in India. Indian Jnl of Medical Ethics. 1997:5. [PubMed] [Google Scholar]
- Rogers A, Meundi A, Amma A, Rao A, Shetty P, Antony J, Sebastian D, Shetty P, Shetty AK. HIV-related knowledge, attitudes, perceived benefits, and risks of HIV testing among pregnant women in rural southern India. AIDS Patient Care STDs. 2006;20:803–811. doi: 10.1089/apc.2006.20.803. [DOI] [PubMed] [Google Scholar]
- Sharma N. The new untouchables. Tribune India: Dehradun Plus online edition. 2008 Retrieved on May 1, 2009 from http://www.tribuneindia.com/2008/20081202/dplus1.htm.
- Steward WT, Herek GM, Ramakrishna J, Bharat S, Chandy S, Wrubel J, Ekstrand ML. HIV-related stigma: Apdapting a theoretical framework for use in India. Social Science & Medicine. 2008;67:1225–1235. doi: 10.1016/j.socscimed.2008.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas B, Nyamathi A, Swaminathan S. Impact of HIV/AIDS on Mothers in Southern India: A qualitative study. Aids Behav. 2008 doi: 10.1007/s10461-008-9478-x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorsen VC, Sundby J, Martinson F. Potential initiators of HIV-related stigmatization: ethical and programmatic challenges for PMTCT programs. Dev World Bioeth. 2008;8(1):43–50. doi: 10.1111/j.1471-8847.2008.00227.x. [DOI] [PubMed] [Google Scholar]
- Turan JM, Miller S, Bukusi EA, Sande J, Cohen CR. HIV/AIDS and maternity care in Kenya: how fears of stigma and discrimination affect uptake and provision of labor and delivery services. AIDS Care. 2008;20(8):938–945. doi: 10.1080/09540120701767224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. India: July, 2008 Country Situation. 2008 Retrieved on Apr 29, 2009 from http://data.unaids.org/pub/FactSheet/2008/sa08_ind_en.pdf.
- Varga C, Brooks H. Factors influencing teen mothers’ enrollment and participation in prevention of mother-to-child HIV transmission services in Limpopo province, South Africa. Qualitative Health Research. 2008;18:786–802. doi: 10.1177/1049732308318449. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The Narrative Research Method: Studying Behaviour Patterns of Young People - By Young People, A Guide to its Use (WHO/ADH/93.4) Geneva: WHO Division of Family Health Technical Units; 1993. [Google Scholar]