Abstract
Reports have shown that interspecies differences in the metabolism and pharmacokinetics of naltrexone are a rule rather than exception. However, there is paucity of information on the disposition of naltrexone in selectively bred rat lines that reliably exhibit high and low voluntary alcohol consumption, and are often used to study alcohol-drinking behavior. We have characterized the pharmacokinetic profiles of naltrexone in selectively bred rat lines: high-alcohol-drinking (HAD-1) and low-alcohol-drinking (LAD-1) rats as well as the native Wistar strain. This study was carried out to establish a baseline pharmacokinetic profile of naltrexone in these rats prior to evaluating its pharmacokinetic profile in polymeric controlled-release formulations in our laboratory. The hypothesis is that alcohol-preferring and non-alcohol-preferring lines of rats should differ in the disposition of intravenously administered naltrexone. Naltrexone administration and blood collection were via the jugular vein. In a parallel experiment, naltrexone was administered via the jugular vein, but urine was collected using the Nalgene metabolic cage system. Data were analyzed by a noncompart-mental approach. Results show a high clearance that is close to or higher than hepatic blood flow in all groups (Wistar > LAD-1 > HAD-1, but with a statistically significant difference only between Wistar and HAD-1). Volume of distribution ( ~2.5-3 l/kg) and the half-life ( ~1 h) were similar. Urinary elimination of naltrexone was small, but also showed differences between the rats: HAD-1 > LAD-1 > Wistar, but with a statistically significant difference only between HAD-1 and Wistar rats. This study has therefore established the baseline disposition characteristics of naltrexone in these strains of rats.
Keywords: Naltrexone, Low-alcohol-drinking rat, High-alcohol-drinking rat, Pharmacokinetics profile
Introduction
Alcohol has been identified as a major societal problem: approximately 7.5% of the US population (about 14 million Americans) abuse and/or are dependent on alcohol. It accounts for about 5% of all deaths in the US, and it costs society about USD 116 billion per year [1]. In spite of the magnitude of its impact on society, there are few treatment options for alcohol dependence and abuse. Treatment methods for alcoholism include detoxifi cation, nonpharmacological (psychosocial) treatment methods and pharmacotherapy, which vary considerably in effectiveness [2]. Only 3 medications are approved for the treatment of alcoholism: disulfiram (Antabuse), naltrexone (REVIA ®) and calcium acetylhomotaurinate (acamprosate calcium or Campral ®).
Naltrexone represents a treatment option developed following the encouraging preclinical data indicating that alcohol drinking is modulated by opioid receptor activity, and that excessive alcohol drinking could be reduced with opioid antagonists. Naltrexone has been evaluated and approved for the adjunctive treatment of alcoholism [1] in conjunction with psychosocial intervention [3-5]. However, its oral use is associated with a high early drop-out rate, and its effectiveness appears to be highly dependent on compliance with the dosing regimen [6, 7]. Furthermore, some investigators have suggested the possibility of a polymorphic response to naltrexone in patients [8, 9], which has been attributed to the existence of allelic variants of μ-opioid receptor gene [4]. It is unclear, however, if the effect of the allelic variants of the μ-opioid receptor gene will be on the pharmacodynamic response to naltrexone (different sensitivity) or the pharmacokinetics of naltrexone (different exposures). Also, when orally administered, naltrexone is highly extracted, resulting in low systemic exposure [10, 11]. There are, therefore, significant challenges to successfully using naltrexone in the treatment of alcoholism.
While genotyping has been suggested as a way to address the issue of the polymorphic response to naltrexone, there are no good options currently available to overcome compliance and high-extraction issues. The use of a new formulation with a controlled-release property to reduce frequency of administration could help address the compliance issue, and, if administered by a route that avoids first-pass loss, could significantly improve systemic exposure. The long-term objective of this project, therefore, is to develop new controlled-release formulations (some with a sustained in vivo plasma availability of naltrexone of >3 months, and some capable of brain-targeted delivery of naltrexone) that could improve the clinical utility of naltrexone. Efforts have been made to develop a naltrexone controlled-release formulation capable of sustaining the release of naltrexone for 1 month [12, 13].
We have already embarked on the investigation of colloidal polymeric controlled-delivery systems for naltrexone. We reported previously on the design of naltrexone-loaded hydrolyzable cross-linked nanospheres suitable for targeted drug delivery [14] for the treatment of alcoholism and opiate addiction. We have extended the work to microspheres: drug delivery devices capable of sustaining the availability of naltrexone for up to 3 months.
As a prelude to evaluating some of these formulations in selectively bred rat lines that reliably exhibit high and low voluntary alcohol consumption, high-alcohol-drinking (HAD-1) and low-alcohol-drinking (LAD-1) rats [15, 16], we characterized the pharmacokinetic profiles of naltrexone in these rats to establish baseline profiles. The rationale for this is that significant interspecies differences in the metabolism and pharmacokinetics of naltrexone have been reported [11, 17-20]. Thus, the understanding of the behavior of these formulations in these rat strains requires appropriate baseline characteristics of naltrexone disposition in these animals. Selectively bred lines of rats are often used to study alcohol-drinking behavior, and a lot of progress has been made in understanding human alcoholism based on animal research using various models including LAD-1 and HAD-1 lines of rats. However, there is paucity of information on the disposition of naltrexone in the selectively bred lines of rats exhibiting different capacity for alcohol consumption. The HAD-1 rats have been selectively bred on the basis of their preference for 10% (v/v) ethanol solution with water and food concurrently available. Moreover, it has been reported that HAD-1 rats display an alcohol-induced enhancement in locomotor activity, which is not observed in their companion LAD-1 selected line [21]. Aside from the differences in the responsiveness of HAD-1 and LAD-1 rats to alcohol, which have been attributed to genetic differences in reward-related neural circuitry [15], they have exhibited differences to other palatable conventional reinforcers. HAD-1 exhibited a greater preference for 0.1% (w/v) saccharin solution [22] and sucrose solution [22, 23]. Studies on the differences in the phenotypic characteristics of the neurotransmitter systems of the rats selected for high and low alcohol preference revealed consistent differences in the mesolimbic dopamine reward system, serotonin, GABA (γ-aminobutyric acid), endogenous opioid and neuropeptide Y systems [15]. Although complex genetic factors as well as environmental variables contribute to alcohol-drinking behavior, the differences in voluntary alcohol consumption and other behavioral characteristics in selectively bred rats are believed to be largely due to innate differences attributable to genetic factors. Extensive discussions on selectively bred rat models of alcoholism can be found in the work of Li and colleagues [15, 16].
A control group of the native strain from where these rat lines were developed (outbred Wistar rats with no his-tory of alcohol consumption) was also included in this study, to assess profiles in the alcohol-drinking rats. The hypothesis is that HAD-1 rats, LAD-1 rats (both developed through selective breeding) and Wistar rats with no history of alcohol drinking will differ in the disposition of intravenously administered naltrexone. Given the reported possibility of a polymorphic response to naltrexone in patients [8, 9], and the fact that allelic variation at μ-opioid receptor gene has been associated with a differential response to μ-receptor antagonist [4], one could speculate that HAD-1 rats would require higher levels of naltrexone to show a similar response to LAD-1 rats. However, HAD-1 rats would be expected to have lower clearance than LAD-1 rats to achieve this higher exposure. Thus, the speculated differences in the disposition of naltrexone in these rats, if established, would suggest the need to vary the dosing levels of naltrexone in genetically predisposed alcoholics. Further, the idea of a ‘one size fits all’ approach in the dosing of naltrexone would need to be revised and changed.
Methods
Materials
Naltrexone hydrochloride was obtained from Mallinckrodt (St. Louis, Mo., USA). Naloxone hydrochloride and 6β-naltrexol hydrochloride were provided by National Institute on Drug Abuse/National Institutes of Health (NIH). High-performance-liquid chromatography (HPLC) -grade acetonitrile (99.9%) and analytical-grade ammonium dihydrogenphosphate, perchloric acid (70%), L -cysteine and EDTA-Na 2 were obtained from Aldrich (Milwaukee, Wisc., USA). Monobasic anhydrous potassium phosphate (KH2 PO4) was purchased from Sigma (St. Louis, Mo., USA). Analytical-grade chloroform, 2-propanol and sodium chloride were all obtained from Fisher Scientific (Fair Lawn, N.J., USA). HPLC-grade phosphoric acid (85 wt.%) was from Aldrich.
Experimental Design
The experimental design used was a randomized complete block design, with type of rat as the treatment. Six blocks were used (6 rats for each treatment).
Animals
Male Wistar rats (weight: 275–300 g) were purchased from Ace Animals (Boyertown, Pa., USA). The 7-week-old male HAD-1 (weight: 237–280 g) and LAD-1 (weight: 230–260 g) rats used in this study were from Indiana University Medical Center. The rats were housed in individual acrylic cages in a temperature-controlled room (constant temperature: 22 ± 1 ° C in a 12-hour light/12-hour dark cycle) at the Veterinary Services Department, Howard University Medical School. They were provided with food and water ad libitum. The rats had at least a 1-week acclimatization period in the animal room before the beginning of experiments. Each type of rat comprised 12 rats that were divided into 2 groups (n = 6 per group) for 2 studies carried out in parallel as follows: 6 for the plasma pharmacokinetic study and 6 for the urinary excretion study. The experimental procedures were approved by the Institutional Animal Care and Use Committee of Howard University (protocol number IACUC-PNAH-02-06), and were conducted according to NIH guidelines.
Sample Collection
Rats were anesthetized with isoflurane and cannulated in the right jugular vein with a polyethylene catheter (PE 60, Silastic medical-grade tubing, Dow Corning, Midland, Mich., USA; 0.51 mm i.d. × 0.94 mm o.d.). The catheter was exteriorized to the dorsal side of the neck, and the exposed area was closed using a surgical suture. The catheter was kept patent with saline containing 100 μg/ml (17 USP units/ml) heparin. After recovery from the anesthesia, each rat was then housed (1 per cage) within a temperature-controlled environment with a 12-hour light/12-hour dark cycle overnight, with free access to food and water.
On the day of the study, about 300 μl of whole blood was withdrawn into an Eppendorf tube from the right jugular vein as a blank control [24]. The Eppendorf tube contained 30 μl of 0.5 M EDTA-Na2 dissolved in phosphate-buffered saline (pH 7.4), as an anticoagulant. Naltrexone hydrochloride dissolved in saline (2.22 mg/kg) was injected into the same vein, and then flushed with 0.5 ml saline. Blood was withdrawn at the scheduled time (2, 5, 10, 20, 40 min, and 1, 1.5, 2, 4, 7, 10, 24, 48 h) and centrifuged immediately at 5,800 g for 10 min to obtain the plasma. The plasma sample was stored at (−20°C) prior to analysis, which was within 2 weeks.
For the urine group, the rats were kept in a Nalgene metabolic cage system (Fisher, Pittsburgh, Pa., USA) immediately after the naltrexone hydrochloride injection (2.22 mg/kg). Urine was collected as follows: 0–12, 12–24 and 24–48 h (the cage for urine collection was rinsed with 20 ml of water; the washings were combined with urine samples). The exact volume of urine output and the pH were measured. After centrifugation, an aliquot of the collected urine was stored in the freezer (−20°C) prior to analysis.
Extraction of Naltrexone from Plasma and Urine Samples
Naltrexone was extracted from plasma and urine by a modification of the methods of O'Connor et al. [24]. Briefly, a 180-μl aliquot of the plasma or diluted urine (12.5~25-fold) sample was added to 20-μl of 1.0 M perchloric acid containing 0.1 M L-cysteine and 0.1 M EDTA-Na2 in an Eppendorf tube. For the assay of conjugated naltrexone, urine samples (containing 20-μl of 1.0 M perchloric acid) were hydrolyzed by incubation at 37 ° C for 24 h to liberate free naltrexone from the conjugates. The difference between the results from hydrolyzed and unhydrolyzed samples was taken as ‘conjugated naltrexone’ or ‘conjugated 6β-naltrexol’. After addition of a 20- μl naloxone working solution (5 μg/ml) as an internal standard, 200 μl of 0.1-M ammonium dihydrogenphosphate solution (pH 8.6) was added. The tube was capped and briefly vortexed. The mixture was extracted by shaking with 1 ml of chloroform:2-propanol (9: 1, v/v) solvent for 30 min at 40 ° C. The mixture was separated into 2 phases by centrifugation (11,000 g for 10 min) at room temperature, and the organic phase was transferred carefully to a clean Eppendorf tube. The contents of the tube were evaporated to dryness under a stream of nitrogen using a N-EVAP ™ 111 Nitrogen Evaporator (Organomation Associates, Mass., USA) with an OA-SYS ™ heating system at 40 °C of a water bath (about 10–15 min). The residue was dissolved in the mobile phase (60 μl), and 20 μl was injected into the HPLC for analysis.
Preparation of Standard Solutions
Stock solutions (1 mg/ml) of naltrexone and naloxone (as an internal standard) were separately dissolved in the mobile phase. Working solutions of naltrexone at 0.1, 0.25, 0.5, 1, 2.5 and 5 μg/ ml and naloxone at 5 μg/ml (internal standard) were made from the stock solutions. The standard samples were prepared by spiking blank plasma or urine (180 ul) with the naltrexone working solutions to give final concentrations of 10, 25, 50, 100, 250 or 500 ng/ml of naltrexone. These samples were then extracted as described above. The standards were used to assess the linearity, precision, accuracy and recovery of naltrexone. The calibration standards were freshly prepared with each analysis. The preparation of the standard solutions for urine was the same as carried out for plasma, except that the urine samples were diluted as follows: 1/(12.5-25).
Instrumentation
Chromatographic analysis was performed on an HP series 1100 HPLC system equipped with a G1311A Quatpump, G1322A degasser, G1316A column compartment and G1315A diode-array detector. A model G1328A syringe loading injector fitted with a fixed 20- μl loop was used to inject the samples. Separation was achieved on a Zorbax 300 SB-C18 column (4.6 × 250 mm i.d., 5 μm), coupled with a guard column packed with the same material (4.6 × 12.5 mm, i.d., 5 μm; Agilent, Santa Clara, Calif., USA). The column temperature was maintained at 37 °C. For plasma analysis, the mobile phase comprised 88% (20 mM KH2PO4 buffer, pH 3.1, adjusted with phosphoric acid) and 12% acetonitrile; however, for urine analysis 84% (20 mM KH2PO4 buffer, pH 3.1), and 16% methanol mixture was used as the mobile phase, following preliminary studies, to avoid interference peaks from control urine. A flow rate of 0.8 ml/min and a UV wavelength of 202 nm were used.
Assay Validation
The HPLC assay method was validated for 3 days in terms of linearity, recovery, precision and accuracy. Linearity for calibration standards in 6 replicates were assessed by subjecting the spiked concentrations 10–1,000 ng/ml (for naltrexone), and the respective peak area ratios to a least-square regression analysis. For determination of the accuracy and precision, standards at low (10 ng/ml), medium (100 ng/ml) and high (500 ng/ml) concentrations were analyzed in 2 replicates for 3 different days (n = 2 × 3 × 3 = 18). Inter- and intra-batch precisions, in terms of the percentage of relative standard deviation (RSD), were obtained by subjecting the data to 1-way analysis of variance. Intra- and inter-batch accuracy was determined by calculating deviation from the theoretical concentration.
Pharmacokinetic Study and Statistical Analysis
Plasma concentration-time data of unchanged naltrexone were analyzed by noncompartmental methods using WinNonlin 4.0.1 (Pharsight, Mountain View, Calif., USA). Analyses of variance with F tests of significance were carried out on the pharmacokinetic parameters, and the pairwise comparison test was used to locate specific differences. The level of significance was set at 0.05. Statistical analyses were carried out using Minitab Release 14 (Minitab, State College, Pa., USA).
Results
Chromatography
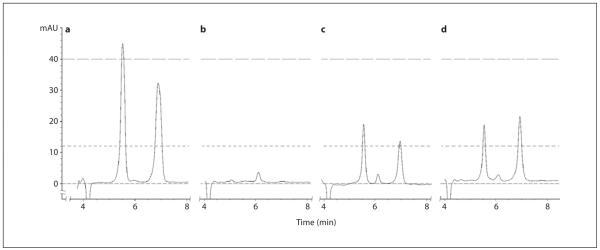
The analytical method produced well-resolved peaks of naltrexone and naloxone from each other and other endogenous components of plasma and urine (fig. 1). This condition enabled the quantification of naltrexone by this method. The retention times were 6.9 min for naltrexone and 5.5 min for naloxone.
Fig. 1.
Typical chromatograms of: a Analytical standard containing 500 ng/ml naltrexone and 500 ng/ml naloxone. b Drug-free rat plasma. c Rat plasma containing 500 ng/ml naltrexone and 500 ng/ml naloxone. d Rat plasma sample taken at 5 min after 2.22 mg/kg intravenous injection of naltrexone hydrochloride.
Absolute recoveries of naltrexone in 6 replicates in 1 day were 72.8, 105.4 and 91.4%, respectively, for concentrations of 10, 100 and 500 ng/ml. The coefficient of variation (CV) ranged from 2.1 to 15.9% (table 1). The recovery of naloxone (internal standard) from the extracted plasma at the concentration of 500 ng/ml used in this experiment was found to be 87.4 ± 3.4% (n = 18).
Table 1.
Recoveries of naltrexone from rat plasma (n = 6)
| Theoretical concentration, ng/ml | Recovery, % | CV, % |
|---|---|---|
| 10 | 72.8 | 15.9 |
| 100 | 105.4 | 3.4 |
| 500 | 91.4 | 2.1 |
The intra- and inter-run precision and accuracy are presented in table 2. The RSD for naltrexone were within ± 17.19% at the 3 concentration levels. The observed intra- and inter-assay accuracies were lowest at 10 ng/ ml.
Table 2.
Precision and accuracy for a HPLC assay of naltrexone from rat plasma (n = 6)
| Theoretical con- centration, ng/ml |
Precision, % RSD |
Accuracy, % |
||
|---|---|---|---|---|
| intra-batch | inter-batch | intra-batch | inter-batch | |
| 10 | 12.02 | 17.19 | 90.6 | 86.48 |
| 100 | 7.75 | 4.11 | 92.94 | 96.66 |
| 500 | 2.37 | 0.14 | 97.90 | 99.88 |
Pharmacokinetics
Plasma
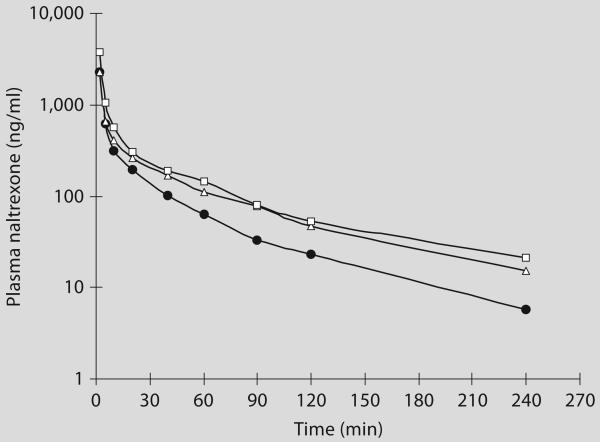
Naltrexone was quantified in plasma samples from all the rats only up to about 4 h. Subsequently, the levels were below the limit of quantification of the assay (4 ng/ml). The plasma concentrations of naltrexone declined in a multiphasic manner with a distinctly more rapid initial (distribution) phase and a later slower (elimination) phase. The profiles were similar for the 3 different types of rats (fig. 2). Table 3 shows the average plasma naltrexone concentrations.
Fig. 2.
Average (n = 6) plasma concentration-time profiles of naltrexone after single intravenous bolus injections of 2.22 mg/kg of naltrexone hydrochloride in the Wistar (●), LAD-1 (△) and HAD-1 (□) rats.
Table 3.
Plasma concentration-time relationship of naltrexone after a single intravenous bolus injection of 2.22 mg/kg of naltrexone hydrochloride (average ± SD; n = 6) in the Wistar, LAD-1 and HAD-1 rats
| Time, min | Plasma naltrexone, ng/ml |
||
|---|---|---|---|
| Wistar | LAD-1 | HAD-1 | |
| 2 | 2,262±312 | 2,291±414 | 3,743±1,081 |
| 5 | 616±145 | 653±306 | 1,040±308 |
| 10 | 312±125 | 407±199 | 561±152 |
| 20 | 193±57 | 258±103 | 302±41 |
| 40 | 100±39 | 169±87 | 189±56 |
| 60 | 63±22 | 112±49 | 143±38 |
| 90 | 33±11 | 77±0 | 80±28 |
| 120 | 23±10 | 47±20 | 53±28 |
| 240 | 6±2 | 15±10 | 21±16 |
A comparison of the estimated pharmacokinetic parameters revealed that most of the parameters were comparable between the different types of rats. However, some parameters [clearance, exposure (area under the curve; AUC) and the dose-normalized AUC] were statistically significantly different between the rat types (table 4a). Table 4b shows a typical analysis of variance. There was a significant difference in clearance, AUC and dose normalized-AUC parameters between HAD-1 and Wistar rats, but not between LAD-1 and Wistar rats on the one hand and HAD-1 and LAD-1 rats on the other hand (table 4c).
Table 4.
Comparison of pharmacokinetic parameters following intravenous bolus administration of naltrexone in Wistar, LAD-1 and HAD-1 rats by analysis of variance
a Comparison of pharmacokinetic parameters
| Parameters | LAD-1 rat | HAD-1 rat | Wistar rat | ANOVA result, p |
|---|---|---|---|---|
| C0, ng/ml | 5,828±2,105.5 | 9,303±2,105.5 | 5,632±1,935.2 | 0.320a |
| Half-life, min | 63.5±23.4 | 70.9±33.7 | 58.9±11 | 0.724a |
| AUC, min × ng/ml | 35,547±9,290.6 | 49,368±14,085.1 | 26,099±4,493.5 | 0.013b |
| AUC_D, min × kg × ng/ml/mg | 16,157.8±4,223 | 22,440.1±6,402.3 | 11,863.2±2,042.5 | 0.013b |
| Cl, ml/min/kg | 65±14.8 | 48±14.1 | 86±13.9 | 0.007b |
| Vss, ml/kg | 3,043.5±871.9 | 2,439.6±1,271.2 | 2,651.8±644.2 | 0.594a |
| AUMC, min × min × ng/ml | 1,829,172.426± 1,000,206.778 |
1,536,266.505± 607,546.849 |
656,693.955± 216,576.746 |
0.079c |
| MRT, min | 49±16.5 | 51.8±26.8 | 31.1±6.6 | 0.098c |
C0 = Extrapolated concentration at zero time; AUC = area under the blood level-time curve; AUC_D = dose-normalized AUC; Cl = clearance; Vss = volume of distribution at steady state; AUMC = area under the first moment curve; MRT = mean residence time.
Not significant;
highly significant;
not significant – borderline.
b A typical analysis of variance table for the pharmacokinetic parameters (randomized complete block experimental design involving 3 types of rats with 6 replications)
| Factor | Type | Levels | Values |
|---|---|---|---|
| Replications | fixed | 6 | I, II, III, IV, V, VI |
| Rats | fixed | 3 | WISTAR, HAD-1, LAD-1 |
| Analysis of variance for clearance (response variable: clearance) | ||||||
|---|---|---|---|---|---|---|
| Source | DF | SS | MS | FC | P | FT |
| Replications | 5 | 480.9 | 96.2 | 0.37 | 0.858 (not significant) | 3.33 (0.05, 5, 10) |
| Rat | 2 | 4,469.5 | 2,234.7 | 8.59 | 0.007 (significant) | 4.10 (0.05, 2, 10) |
| Error | 10 | 2,600.3 | 260.0 | |||
| Total | 17 | 7,550.8 | ||||
| Tukey simultaneous tests (response variable: clearance): all pairwise comparisons among types of rat | ||||
|---|---|---|---|---|
| Difference of means |
SE of difference |
Adjusted T value |
p value | |
| Rat (Wistar subtracted from) | ||||
| HAD-1 | −38.60 | 9.310 | −4.146 | 0.0051 (significant) |
| LAD-1 | −18.86 | 9.310 | −2.026 | 0.1563 (not significant) |
| Rat (HAD-1 subtracted from) | ||||
| LAD-1 | 19.73 | 9.310 | 2.119 | 0.1354 (not significant) |
c Tukey simultaneous tests: all pairwise comparisons among types of rat for statistically significant pharmacokinetic parameters
| Parameter | Pairwise comparison of means | p value |
|---|---|---|
| AUC, min × ng/ml | HAD-1 vs. LAD-1 | 0.1204 (not significant) |
| HAD-1 vs. Wistar | 0.0105 (highly significant) | |
| LAD-1 vs. Wistar | 0.3315 (not significant) | |
|
| ||
| AUC_D, min × kg × ng/ml/mg | HAD-1 vs. LAD-1 | 0.1204 (not significant) |
| HAD-1 vs. Wistar | 0.0105 (highly significant) | |
| LAD-1 vs. Wistar | 0.3315 (not significant) | |
|
| ||
| Cl, ml/min/kg | HAD-1 vs. LAD-1 | 0.2174 (not significant) |
| HAD-1 vs. Wistar | 0.0051 (highly significant) | |
| LAD-1 vs. Wistar | 0.1079 (not significant) | |
When a significant difference was found, Tukey simultaneous tests were employed. AUC = Area under the blood level-time curve; AUC_D= dose-normalized AUC; Cl = clearance.
Urine
In a parallel experiment, urine samples from Wistar, LAD-1 and HAD-1 rats, after a similar dose (2.2 mg/kg) of naltrexone hydrochloride, were analyzed to assess urinary recovery of naltrexone and its metabolite 6-β-naltrexol. Both free and conjugated forms of the compounds were quantified.
6β-Naltrexol was not detected in the urine samples from any of the 3 types of rat; hence, the assay validation procedure was not described. The administered dose was recovered mostly in the form of free naltrexone in all 3 types of rat ( table 5 ). Some were also found in the conjugated form, but less than the free form. The majority of the excretion occurred within the first 12 h of collection, with little additional recovery up to 48 h.
Table 5.
Urinary free- and conjugated-naltrexone levels after 2.22 mg/kg intravenous bolus administration of naltrexone hydrochloride in Wistar, LAD-1 and HAD-1 rats
| Groups | Time, h | Free naltrexone |
Conjugated naltrexone |
Total cumulative naltrexone, % (significant) |
||
|---|---|---|---|---|---|---|
| excretion, μg | cumulative, % (significant) |
excretion, μg | cumulative, % (not significant) |
|||
| Wistar | 12 | 13.80±0.56 | 2.09 | 4.66±3.15 | 0.71 | 2.80±0.77 |
| 24 | 0±0 | 2.09 | 1.13±0.75 | 0.88 | 2.97±0.73 | |
| 48 | 0±0 | 2.09 | 1.08±0.51 | 1.05 | 3.14±0.79 | |
| LAD-1 | 12 | 12.42±0.25 | 2.75 | 8.69±3.82 | 1.93 | 4.68±2.01 |
| 24 | 0.27±0.34 | 2.81 | 0.04±0.09 | 1.94 | 4.75±2.04 | |
| 48 | 0.26±0.46 | 2.87 | 0±0 | 1.94 | 4.81±1.97 | |
| HAD-1 | 12 | 19.46±0.51 | 4.06 | 7.67±5.17 | 1.48 | 5.53±1.21 |
| 24 | 0±0 | 4.06 | 1.68±1.06 | 1.60 | 5.66±1.16 | |
| 48 | 0.24±0.54 | 4.34 | 0.73±0.91 | 1.46 | 5.80±1.22 | |
Total cumulative % naltrexone excreted is significant with HAD-1 > Wistar, but no significant differences between Wistar and LAD-1 rats and also between HAD-1 and LAD-1 at 5% level of significance.
Free cumulative % naltrexone excreted is significant with HAD-1 > Wistar, but no significant difference between Wistar and LAD-1 rats and also between HAD-1 and LAD-1 at 5% level of significance.
Total cumulative % conjugated naltrexone excreted is not significant (i.e. no significant difference between Wistar, LAD-1 and HAD-1 rats at 5% level of significance).
Analysis of variance with the F test of significance was carried out on the free naltrexone, conjugated naltrexone and total naltrexone excreted, and the pairwise comparison test (Tukey simultaneous test) was used to locate specific differences in cases where a statistically significant difference was found.
Statistically significant differences among the selectively bred LAD-1 and HAD-1 and the unselected Wi-star rats were found in total and free naltrexone, but not in conjugated naltrexone ( table 5 ). The pairwise comparison test shows that the difference between the mean cumulative percentage of total naltrexone excreted in the urine might be due to differences between Wistar and HAD-1 rats, but not between Wistar and LAD-1 rats or LAD-1 and HAD-1 rats. Also, the pairwise comparison test shows that the difference between the mean cumulative percentage of free naltrexone excreted in the urine is different for Wistar and HAD-1 rats, but not different for Wistar and LAD-1 rats or LAD-1 and HAD-1 rats.
Discussion
Naltrexone Plasma Concentration-Time Data
There is a lot of interspecies variability in the reported pharmacokinetics of naltrexone in the literature. In fact, this interspecies variability led to the decision to study the disposition of naltrexone in unselected Wistar rats and the selectively bred LAD-1 and HAD-1 rat lines. This study will provide background information for the pharmacokinetics of naltrexone in our laboratory for these strains of rats, which will be used as a reference for subsequent work in the effort to assess the disposition of naltrexone controlled-release dosage forms. Moreover, various compartmental models have been used to analyze the data on the disposition of naltrexone in different animal species [11, 18, 25-28], which could have contributed significantly to the reported variability in its pharmacokinetics. We employed a noncompartmental approach for pharmacokinetic data analysis in this work to avoid any such contribution to variability.
Naltrexone demonstrated a profile characterized by high clearance that is close to or higher than hepatic blood flow in the rat. This result suggests the possibility of other routes of elimination than the hepatic contributing to the elimination of naltrexone. Recovery of free naltrexone in urine suggests that urinary elimination, though minor, could be one of these extra-hepatic routes of elimination. Naltrexone also displayed a large volume of distribution (~2.5−3 l/kg) indicating the possibility of extensive distribution into tissues. The half-life was about 1 h.
There was a significant difference in the clearance of naltrexone between the different types of rats. The trend was HAD-1 < LAD-1 < Wistar, but the difference was only statistically significant between HAD and Wistar rat types. Similar trends of statistical significance were seen with AUC and dose-normalized AUC. This trend suggests that the level of alcohol drinking has an effect on the clearance of naltrexone from rats. The exact mechanism responsible for this is unclear, but the results suggest that the effect might be due to an effect on hepatic elimination of naltrexone. This result is consistent with observations that have been made showing that hepatic metabolic capacity is compromised in alcoholics, with a resultant reduction in the clearance of compounds eliminated through hepatic metabolism [29]. However, given that these rats have not been chronically exposed to alcohol (though one of the criteria proposed for an animal model of alcoholism is chronic ethanol consumption which should lead to the expression of metabolic and functional tolerance and chronic consumption of ethanol which should lead to dependence, as indicated by withdrawal symptoms after access to ethanol is terminated [15, 30] ), the possibility of a linkage between genes coding for alcohol drinking and those responsible for metabolizing enzymes may account for the difference in naltrexone disposition. Further, a combination of selective breeding with DNA microarray analysis has been found to show consistently significant differences in gene expression in the hippocampus between inbred alcohol-preferring and inbred non-alcohol-preferring rats [31]. Gene expression profiles have also been generated from 4 key regions involved in dependence: cingulated cortex, nucleus accumbens, amygdale and hippocampus. About 30–50 genes per region were identified whose expression is specifically altered in the alcohol-preferring (AA) rats compared with non-alcohol-preferring (ANA) and Wistar rats [31].
A difference was also observed in the urinary elimination of naltrexone, even though the overall urinary elimination was very low (<10% of dose). The observation was that more naltrexone was eliminated in HAD-1 rats than in Wistar rats, with no difference between LAD-1 and Wistar rats. The observation is contrary to the trend seen in clearance, where HAD-1 rats had lower clearance. However, given that hepatic elimination is believed to be the major route of elimination, the decrease in overall clearance in HAD-1 rats, presumably due to reduced hepatic elimination, could mean that more naltrexone is available for urinary excretion, and hence the higher uri-nary elimination observed in these rats. This is consistent with the higher exposure (AUC) seen in HAD-1 rats.
Urinary Naltrexone Excretion Data
6β-Naltrexol was not detected in the urine from any of the 3 types of rat investigated in this study, which is in agreement with earlier reports that 6β-naltrexol is not a major metabolite of naltrexone excreted in the urine of rat, dog and mouse [17, 32]. However, 6β-naltrexol is a major metabolite of naltrexone in humans [33, 34]. All these reports point to the acknowledged significant inter-species differences in the quantitative pattern of the metabolism of naltrexone.
The cumulative total percentage of naltrexone (free plus conjugated) excreted in the urine was very small: 3.1 ± 0.8% for Wistar rats, 4.8 ± 2.0% for LAD-1 rats and 5.8 ± 1.2% for HAD-1 rats. This result is similar to earlier report indicating that for rats dosed with 100 mg/kg p.o. daily for 365 days, less than 1% of the total administered daily dose appeared in the 24-hour urine collection as naltrexone (free and conjugated) [32]. Furthermore, a higher proportion of the dose has been shown to be excreted in feces than urine [35]. Consequently, the low amount of naltrexone found in the urine may be due to extensive biliary excretion of naltrexone in Wistar, LAD-1 and HAD-1 rats, which eventually found its way out of the body through the feces. This study did not involve assessment of fecal excretion.
Conclusion
This study has characterized the pharmacokinetic profile of naltrexone in Wistar, LAD-1 and HAD-1 rats after a single bolus intravenous dose of 2.2 mg/kg. The results show naltrexone with a very high clearance and a high volume of distribution in LAD-1, HAD-1 and Wistar rats. The level of alcohol consumption appears to have some effect on the clearance of naltrexone, with the clearance lower in HAD-1 rats than Wistar rats, and LAD-1 rats showing a similar trend though it did not reach the level of statistical significance. Urinary elimination of naltrexone was very small and 6β-naltrexol was not detected in urine. This result suggests that other metabolic pathways and/or elimination in the feces is a major route of elimination of naltrexone in the rat. This study has therefore produced baseline disposition characteristics of naltrexone in these strains of rats, which can now be used as reference against which results of studies with controlled-release formulations of naltrexone can be compared.
Acknowledgments
Funding for this study was provided by NIAAA/NIH grant No. 1 R21 AA13407-01. This work was carried out in a facility supported by NCRR/NIH grant No. 1 C06 RR 020608-01. We thank Dr. Zhang Ren-Su, who assisted us in the cannulation of the jugular vein of rats, and Prof. Robert Taylor for his suggestions.
References
- 1.Weiner RM, O'Brien CP. Naltrexone in the treatment of alcoholism. Annu Rev Med. 1997;48:477–487. doi: 10.1146/annurev.med.48.1.477. [DOI] [PubMed] [Google Scholar]
- 2.Fuller RK, Hiller-Sturmhofel S. Alcoholism treatment in the United States: an overview. Alcohol Res Health. 1999;23:69–77. [PMC free article] [PubMed] [Google Scholar]
- 3.O'Malley SS, Jaffe AJ, Chang G, Schottenfeld RS, Meyer RE, Rounsaville B. Naltrexone and coping skills therapy for alcohol dependence: a controlled study. Arch Gen Psychiatry. 1992;49:881–887. doi: 10.1001/archpsyc.1992.01820110045007. [DOI] [PubMed] [Google Scholar]
- 4.Oslin DW, Berrettini W, Kranzler HR, Pettinati H, Gelernter J, Volpicelli JR, O'Brien CP. A functional polymorphism of the μ-opioid receptor gene is associated with naltrexone response in alcohol dependent patients. Neuropsychopharmacology. 2003;28:1546–1552. doi: 10.1038/sj.npp.1300219. [DOI] [PubMed] [Google Scholar]
- 5.O'Brien CP. Research advances in the understanding and treatment of addiction. Am J Addiction. 2003;12:S36–S37. [PubMed] [Google Scholar]
- 6.Volpicelli JR, Rhines KC, Rhines JS. Naltrexone and alcohol dependence. Arch Gen Psychiatry. 1997;54:737–742. doi: 10.1001/archpsyc.1997.01830200071010. [DOI] [PubMed] [Google Scholar]
- 7.Chick J, Anton R, Checinski K, Croop R, Drummond DC, Farmer R. A multicenter, randomized, double-blind, placebo-controlled trial of naltrexone in the treatment of alcohol dependence or abuse. Alcohol Alcohol. 2000;35:587–593. doi: 10.1093/alcalc/35.6.587. [DOI] [PubMed] [Google Scholar]
- 8.Krystal JH, Cramer JA, Krol WF, Kirk GF, Rosenheck RA. Veterans Affairs naltrexone cooperative study G (2001): naltrexone in the treatment of alcohol dependence. New Engl J Med. 2001;345:1734–1739. doi: 10.1056/NEJMoa011127. [DOI] [PubMed] [Google Scholar]
- 9.Kranzler H, Modesto-Lowe V, Van Kirk J. Naltrexone versus nefazodone for treatment of alcohol dependence: a placebo-controlled trial. Neuropsychopharmacology. 2000;22:493–503. doi: 10.1016/S0893-133X(99)00135-9. [DOI] [PubMed] [Google Scholar]
- 10.Johnson DAW. Observations on the use of long-acting depot neuroleptic injections in the maintenance therapy of schizophrenia. J Clin Psychiatry. 1984;5:13–21. [PubMed] [Google Scholar]
- 11.Wall ME, Brine DR, Perez-Reyes M. Metabolism and disposition of naltrexone in man after oral and intravenous administration. Drug Meta Dispos. 1981;9:370–375. [PubMed] [Google Scholar]
- 12.Bartus RT, Emerich DF, Hotz J, Blaustein M, Dean RL, Perdomo B, Basile A. Viitrex®, an injectable, extended-release formulation of naltrexone, provides pharmacokinetic and pharmacodynamic evidence of efficacy for one month in rats. Neuropsychopharmacology. 2003;28:1973–1982. doi: 10.1038/sj.npp.1300274. [DOI] [PubMed] [Google Scholar]
- 13.Leonard B, editor. Helping Patients Who Drink Too Much: A Clinician's Guide. Diane; Derby: 2005. Medications for treating alcohol dependence; p. 16. [Google Scholar]
- 14.Yin W, Akala E, Taylor R. Design of naltrexone-loaded hydrolyzable crosslinked nano-particles. Int J Pharm. 2002;244:9–19. doi: 10.1016/s0378-5173(02)00297-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McBride WJ, Li TK. Animal models of alcoholism: neurobiology of high alcohol-drinking behavior on rodents. Crit Rev Neurobiol. 1998;12:339–369. doi: 10.1615/critrevneurobiol.v12.i4.40. [DOI] [PubMed] [Google Scholar]
- 16.Murphy JM, Stewart RB, Bell RL, Badia-Elder NE, Carr LG, McBride WJ, Lumeng L, Li TK. Phenotypic and genotypic characterization of the Indiana University rat lines selectively bred for high and low alcohol preference. Behav Genet. 2002;32:363–388. doi: 10.1023/a:1020266306135. [DOI] [PubMed] [Google Scholar]
- 17.Malspeis L, Bathala MS, Ludden TM, Bhat HB, Frank SG, Sokoloski TD, Morrisson BE, Reuning RH. Metabolic reduction of naltrexone. I. Synthesis, separation and characterization of naloxone and naltrexone reduction products and quantitative assay of urine and bile following administration of naltrexone, alpha-naltrexol, or beta-naltrexol. Res Commun Chem Pathol Pharmacol. 1975;12:43–65. [PubMed] [Google Scholar]
- 18.Reuning RH, Batra VK, Ludden TM, Hao MY, Morrison BE, McCarthy DA, Harrigan SE, Ashcraft SB, Sams RA, Bathala MS, Staubus AE, Malspeis L. Plasma naltrexone kinetics after intravenous bolus administration in dogs and monkeys. J Pharm Sci. 1979;68:411–416. doi: 10.1002/jps.2600680405. [DOI] [PubMed] [Google Scholar]
- 19.Garrett ER, el-Koussi A el-D. Pharmacokinetics of morphine and its surrogates V: Naltrexone and naltrexone conjugate pharmacokinetics in the dog as a function of dose. J Pharm Sci. 1985;74:50–56. doi: 10.1002/jps.2600740114. [DOI] [PubMed] [Google Scholar]
- 20.Reuning RH, Liao SHT, Staubus AE, Ashcraft SB, Down DA, Harrigan SE, Wiley JN, Wise DL. Pharmacokinetic quantitation of naltrexone controlled release from a copolymer delivery system. J Pharmacokinet Biopharm. 1983;11:369–387. doi: 10.1007/BF01058956. [DOI] [PubMed] [Google Scholar]
- 21.Rodd ZA, Bell RL, McKinze DL, Webster AA, Murphy JM, Lumeng L. Low-dose stimulatory effect of ethanol during adolescence in rat lines selectively bred for high alcohol preference. Alcohol Clin Exp Res. 2004;28:535–543. doi: 10.1097/01.alc.0000122107.08417.d0. [DOI] [PubMed] [Google Scholar]
- 22.Stewart RB, Murphy JM, Lumeng L, Li TK. Intake of saccharin solution in selectively-bred high and low alcohol drinking (HAD and LAD) lines of rats and in the F2 progeny of HAD and LAD rat crosses. Alcohol Clin Exp Res. 1998;22:A55. [Google Scholar]
- 23.Badia-Elder NE, Stewart RB, Powrozek TA, Murphy JM, Li TK. Effects of Neuropeptide Y (NPY) on ethanol intake and anxiety in high and low alcohol drinking (HAD1/ LAD1) rats. Alcohol Clin Exp Res. 2000;24:A82. doi: 10.1097/01.ALC.0000071929.17974.DA. [DOI] [PubMed] [Google Scholar]
- 24.O'Connor EF, Cheng SW, North WG. Simultaneous extraction and chromatographic analysis of morphine, dilaudid, naltrexone and naloxone in biological fluids by high-performance liquid chromatography with electrochemical detection. J Chromatogr. 1989;491:240–247. doi: 10.1016/s0378-4347(00)82839-x. [DOI] [PubMed] [Google Scholar]
- 25.Reuning RH, Ashcraft SB, Wiley JN, Morrison BE. Disposition and pharmacokinetics of naltrexone after intravenous and oral administration in rhesus monkeys. Drug Metab Dispos. 1989;17:583–589. [PubMed] [Google Scholar]
- 26.Valiveti S, Hammell DC, Paudel KS, Hamad MO, Crooks PA, Stinchcomb AL. In vivo evaluation of 3-O-alkyl ester transdermal prodrugs of naltrexone in hairless guinea pigs. J Control Rel. 2005;102:509–520. doi: 10.1016/j.jconrel.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 27.Berkowitz BA, Spector S, Lee CH. Mechanism of narcotic antagonist and narcotic antagonist analgesic action. In: Ford DH, Clouet DH, editors. Tissues Responses to Addictive Drugs. Spectrum Publications; Jamaica, NY: 1976. pp. 139–153. [Google Scholar]
- 28.Pace NL, Parrish RG, Lieberman MM, Wong KC, Blatnick RA. Pharmacokinetics of naloxone and naltrexone in the dog. J Pharmacol Exp Ther. 1979;208:254–256. [PubMed] [Google Scholar]
- 29.Lieber CS. Medical and nutritional complications of alcoholism: mechanism and management. Plenum Press; New York: 1992. pp. 165–183. [Google Scholar]
- 30.Rodd ZA, Bell RL, Sable HJK, Murphy JM, McBride WJ. Recent advances in animal models of alcohol craving and relapse. Pharmacol Biochem Behav. 2004;79:439–450. doi: 10.1016/j.pbb.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 31.Hoffman PL, Miles M, Edenberg HJ, Somer W, Tabakoff B, Wehner JM, Lewohi J. Gene expression in brain: a window on ethanol dependence, neuroadaptation, and preference. Alcohol Clin Exp Res. 2003;27:155–168. doi: 10.1097/01.ALC.0000060101.89334.11. [DOI] [PubMed] [Google Scholar]
- 32.Dayton HE, Inturrissi CE. Naltrexone bio-transformation and incidence of subjective side effects: a preliminary study. Drug Metab Dispos. 1976;4:474. [Google Scholar]
- 33.Crabtree BL. Review of naltrexone, a long-acting opiated antagonist. Clin Pharm. 1976;3:273–280. [PubMed] [Google Scholar]
- 34.Vereb K, Volavka J, Mule SJ, Resnick RB. Naltrexone: disposition, metabolism and effects after acute and chronic dosing. Clin Pharmacol Ther. 1976;20:315–328. doi: 10.1002/cpt1976203315. [DOI] [PubMed] [Google Scholar]
- 35.Ludden TM, Bathala MS, Malspeis L, Drum MA, Reuning RH. Elimination of radioactivity following administration of [15, 16 3H] naltrexone to rats and guinea pigs. Drug Met Dispos. 1978;6:321–328. [PubMed] [Google Scholar]