Abstract
Introduction
We studied the relationship between registered nurses' extended work duration with adverse events and errors, including needlestick injuries, work-related injuries, patient falls with injury, nosocomial infections, and medication errors.
Method
Using bivariate and multivariate logistic regression, this secondary analysis of 11,516 registered nurses examined nurse characteristics, work hours, and adverse events and errors.
Results
All of the adverse event and error variables were significantly related to working more than 40 hours in the average week. Medication errors and needlestick injuries had the strongest and most consistent relationships with the work hour and voluntary overtime variables.
Discussion
This study confirms prior findings that increased work hours raise the likelihood of adverse events and errors in healthcare, and further found the same relationship with voluntary overtime.
Impact on Industry
Legislation has focused on mandatory overtime; however, this study demonstrated that voluntary overtime could also negatively impact nurse and patient safety.
Keywords: Adverse events, Errors, Overtime, Registered nurses, Work hours
1. Problem
The issue of work hours in healthcare has attracted much attention. In 2003, the Accreditation Council for Graduate Medical Education instituted limits on resident duty hours as an approach to improve patient safety and quality of training (Rice & Leach, 2003). The standards include an 80-hour weekly limit on duty-hours averaged over four weeks, 10 hours of rest between duty periods, and a 24-hour limit on continuous duty with a possible 6 additional hours added for continuity of care and education, for a total of 30 hours of continuous duty. Currently 15 states have legislation or regulations prohibiting or restricting mandatory overtime for nurses. At the federal level, the American Nurses Association promoted the Safe Nursing and Patient Care Act of 2007 (HR 2122 and S 1842), which would have limited the amount of mandatory overtime worked by nurses employed by organizations receiving Medicare funding (American Nurses Association, 2008). Both bills went to committees during the 110th Congress, however, they were never brought to a vote in either chamber. All of these policy initiatives are based on the assumption that extended work hours negatively impact patients by contributing to worker fatigue. State legislation and proposed federal legislation restricting nurse work hours pertain only to mandated overtime, not to voluntary overtime hours nurses may choose to work.
The negative effects of fatigue have been demonstrated in occupations outside of healthcare, such as forestry and commercial motor vehicle (CMV) operation (Lilley, Feyer, Kirk, & Gander, 2002; Mitler, Milller, Lipsitz, Walsh, & Wylie, 1997). The Hours of Service of Drivers Final Rule (49 CFR Parts 385, 390, and 395) is a federal regulation that limits hours of driving between off-duty periods, consecutive hours of driving, and the number of work hours allowable over seven- to eight-day periods for drivers of property- and passenger-carrying CMVs (U.S. Department of Transportation, 2005). The basis for such regulations has been the belief that increased time awake and acute continuous sleep deprivation decrease both alertness and quality of task performance. Evidence from health healthcare settings also suggests that chronic partial sleep deprivation has a cumulative effect on alertness and performance, particularly under conditions of chronically long work hours without adequate off-duty time between shifts (Lockley, Landrigan, Barger, & Czeisler, 2006).
Overtime is time on the job beyond the hours scheduled for the individual shift and/or work week. Overtime is frequently used in healthcare settings to meet staffing needs due to employee shortages, patient influxes, or both. With a shortage of nurses and healthcare workers documented for well over a decade, overtime has been a major management tool for ensuring coverage of patient needs. Using New York State administrative data from 1995 to 2000, researchers showed that an average of 4.5% of total paid hours worked by registered nurses (RNs) were paid overtime (Berney, Needleman, & Kovner, 2005). From 1995 to 2002, paid overtime increased from an average of 3.9% to 5.9% of total hours and mean overtime rose from 0.23 to 0.39 hours per patient day (Berney & Needleman, 2005).
There are a number of recent studies in the literature examining the effects of physician work hours on safety. In a large controlled study, researchers in the Harvard Work Hours, Health, and Safety Group found that attentional failures occurred twice as often at night and 1.5 times more often during the day in physician trainee housestaff working under a traditional 30-hour duty schedule compared with those on a specially-designed 16-hour duty schedule (Lockley et al., 2004). In critical care, interns on the traditional schedule made 35.9 % more “serious” medical errors than those on the intervention schedule (Landrigan et al., 2004).
Despite talk of a need to regulate mandatory overtime for nurses, considerably fewer studies have been conducted to examine the association between the length of nurses’ shifts or work weeks and adverse events in patients. However, researchers have found, for example, that the odds of self-reported error are three times higher after shifts lasting 12.5 or more hours. Further, these authors report that working more than 40-hours a week significantly increased the risk of self-reported errors (Rogers, Hwang, Scott, Aiken & Dinges, 2004). Among critical care nurses, error reports almost doubled after 12.5 or more consecutive hours of work and working more than 40 hours per week had a significant effect on both errors and near misses (Scott, Rogers, Hwang, & Zhang, 2006).
However, not all studies have found negative effects of overtime. In New York State, overtime was significantly linked with elevated hospital-level mortality in medical and surgical patients in the opposite to expected direction: increasing use of overtime in a hospital was related to a decrease in mortality. In this study, models controlled for patient acuity, nurse staffing, and hospital characteristics. The authors hypothesized that this finding may partially reflect the potential benefits of hospitals using experienced permanent staff working overtime instead of temporary staff to fill staffing gaps (Berney & Needleman, 2006). Stone, Mooney-Kane, Larson, and colleagues (2007) had a similar paradoxical result in that increased overtime was significantly associated with decreased odds of experiencing a central-line blood stream infection after controlling for patient acuity, nurse staffing, and hospital characteristics. The authors, however, also found that higher overtime was significantly related to increased likelihood of catheter-associated urinary tract infections and decubitus ulcers.
In terms of negative influences of overtime on workers, research findings have connected overtime with work-related injuries across a variety of industries. Data from 1987 to 2000 revealed that every additional five hours worked per week (past 40 hours) was associated with an average increase of approximately 0.7 injuries per 100 worker-hours. In addition, the authors showed that working a job more than 60 hours per week was associated with a 23% higher injury hazard rate and working in a job with overtime was associated with a 61% higher injury hazard rate (Dembe, Erickson, Delbos,&Banks, 2005). In healthcare workers, a number of types of occupational injuries have been linked with overtime. Musculoskeletal disorders have been linked with hours of work per day and per week (Trinkoff, Le, Geiger-Brown, Lipscomb, & Lang, 2006). Working more than 12 hours per shift has been linked with needlestick risk in hospital workers (Trinkoff, Le, Geiger-Brown & Lipscomb, 2007). Clarke (2007) found that adjusted risks of needlestick injuries in hospital nurses increased by 16% for every additional 10 hours of work. The prevalence of needlestick injuries in Turkish nurses working more than 8 hours per day was significantly higher than in those who worked 8 hours or fewer per day (Ilhan, Durukan, Aras, Turkcuoglu, & Aygun, 2006). In the Harvard Work Hours, Health, and Safety Group study of medical interns, the rate of sharps injuries during an extended-hours schedule was significantly greater than the rate of sharps injuries during non-extended work schedules. Fatigue was more likely to be cited as a contributing factor for injuries in interns on extended-work schedules (Ayas et al., 2006).
Overall, there is strong evidence that fatigue associated with extended work schedules is related to adverse events and errors in patients and healthcare workers. Proposed and enacted legislation limiting mandatory overtime in nurses does not address the effects of voluntary paid overtime on adverse outcomes in patients and healthcare workers. To date, there is very little evidence specifically examining the role of voluntary paid overtime by nurses on adverse outcomes. This secondary analysis of a large group of hospital nurses seeks to explore links between work hours and both adverse events and errors experienced by patients and healthcare workers.
2. Method
This study involved secondary analysis of anonymous surveys from 1999, when a random 50% sample of RNs licensed in the state of Pennsylvania was mailed questionnaires and 52% of nurses contacted returned surveys. Nurses working in acute care general hospitals completed and returned 13,152 questionnaires (Aiken, Clarke, Sloane, Sochalski, & Silber, 2002). Nurses were asked to identify the hospital where they worked and to respond to the survey questions based on their experience at that hospital. The questionnaire addressed employment characteristics, work environment, job-related feelings, job characteristics, characteristics of the last shift worked, and demographic characteristics. Previous analyses of this dataset revealed the study sample of nurses to be comparable in most respects to the staff nurses in the National Sample Survey of Registered Nurses (NSSRN) conducted in 2000 (Aiken, Clarke, Cheung, Sloane, & Silber, 2003).
To help ensure that measures aggregated to the hospital level would be reliable, attention was restricted to respondents at hospitals from which at least 10 nurses returned questionnaires (Aiken et al., 2002). In addition, only those nurses who indicated that their job title was “staff nurse” were included in the analysis. This was done to assure that the data were provided by those with first-hand knowledge of adverse events in their clinical areas. Responses from nurses who indicated that they were responsible for more than 20 patients or less than one patient on their last shift were excluded to ensure that the nurses actually provided direct patient care, since responsibility for more than 20 patients suggests a supervisory rather than a direct care role (Clarke, 2007). The analytic sample here consisted of 11,516 RNs from 188 Pennsylvania hospitals.
2.1. Measures
2.1.1. Nurse Characteristics
Nurse characteristic variables were included in the analyses because of their potentially confounding influences on the reporting of both work hours and adverse events. Respondent characteristics used as control variables included sex, age, years of experience as an RN, permanent versus temporary employment, type or specialty of the unit the nurse worked on, country in which basic nursing education was received, highest nursing degree completed, whether the nurse was living with dependents, and whether the nurse was represented by a collective bargaining unit.
Two further nurse-level variables were used to adjust injury risk in the analyses of sharps injuries. Nurses were asked what tasks they performed on their last shift worked as a way to assess for clinical activities posing a risk for sharps injuries. Answering affirmatively that work on the last shift involved starting IVs and/or performing routine phlebotomy was considered to be a risk factor. The routine use of four types of safety-engineered sharps (blunted devices, needleless equipment, self-capping devices, and safety lock equipment) was assessed in the survey and used as a control variable in the analyses involving needlestick (sharps) injuries (Clarke, 2007).
One hospital-level characteristic, staffing, examined by a number of researchers as a predictor of adverse outcomes in patients and nurses, was included in analyses to rule out differences in workloads for RNs across hospitals as a potential explanation for findings. The measure used here was the mean patient load reported by all nurses deemed to be working in direct care from each hospital.
2.1.2. Work Hours and Overtime
Work hours were measured using the following question, “In the past year, how many hours per week did you work on average?” Specific types of overtime were assessed using the following question stem, “In the past year, about how many hours per week did you work the following types of overtime…” The response types were mandatory overtime, other paid overtime, and unpaid overtime. “Other paid overtime” can be understood as “voluntary paid overtime” because it is paid overtime that is not mandatory. Nurses were able to write the number of hours for any combination of overtime types. For example a nurse could have worked 2 hour of unpaid overtime, 2 hours of mandatory overtime, and 1 hour of voluntary paid overtime.
The “unpaid overtime” category does not distinguish between whether the unpaid overtime was mandated or voluntary and the “mandatory overtime” does not distinguish between whether the mandatory overtime was paid or unpaid. The analyses focused on the category of voluntary paid overtime because that category was the only one with a distinct meaning and did not overlap with the others. The overlap in the definitions of unpaid overtime and mandatory overtime meant that the hours in those categories could not be added together to yield consistently meaningful totals. From the example above, the nurse could have worked 5 hours of overtime if he or she thought the unpaid and mandatory categories were distinct. Or he or she could have worked 3 hours of overtime if the 2 hours of unpaid overtime were also counted as 2 mandated hours. Because the categories could not be used additively, the question, “In the past year, how many hours per week did you work on average?” was used in analyses to determine the effect of hours worked beyond a standard 40 hour work week.
2.1.3. Adverse Events and Errors
Adverse events in this study included needlestick and sharps injuries, work-related employee injuries, patient falls with injury, and nosocomial infections. A patient receiving the wrong medication or dose was considered an error without reference to whether or not harm was experienced. Adverse events and errors (AEs)were assessed with a series of items using the following stem: “Over the past year, how often would you say each of the following incidents has occurred involving you or your patients…” The possible responses were: never, rarely, occasionally, and frequently. Needlestick and sharp injuries were determined by asking nurses how many of these incidents occurred in the past year.
2.2. Analyses
Descriptive analyses of nurse characteristics and responses were conducted. Frequencies and percentages were calculated for categorical variables; means, standard deviations, and ranges were presented for continuous variables. Logistic regression was used in both bivariate and multivariate analyses to obtain odds ratios for nurse-reported occurrence of events in the previous year in relation to work hours. Huber-White robust standard errors were calculated to account for the correlations in the error terms created by the clustering of nurse respondents within hospitals (Huber, 1967; Rogers, 1993; White, 1980). Statistical significance was set at p<0.05. Stata versions 9.0 and 10.0 (College Station, TX) were used for all analyses.
The dependent variables, frequency of AEs, were dichotomized into occasionally/frequently with never/rarely as the reference category. This was done because the intervals between adverse event frequency choices were inexact (for instance, “never” to “rarely”) and for ease of interpretation. The independent variable education was dichotomized to contrast nurses holding a bachelor's or higher degree with those who did not (Aiken et al., 2003). Nurse experience was grouped into five-year increments following previous work with this dataset (Clarke, 2007). Nurse reports of the number of patients cared for on the last shift was aggregated and averaged at the hospital-level. This staffing measure has been validated in previous studies using this dataset (Aiken et al., 2002; Aiken et al., 2003).
Several work hour variables were created for the analysis. The first analyses conducted used a broad definition of overtime, that is, the hours worked beyond a standard 40-hour work week. To test for the effects of an extended-length work week, average total hours worked weekly was dichotomized at 40 hours [a “typical” full-time work week]. Additional analyses focused on the effect of voluntary overtime on nurse reports of AEs. The voluntary paid overtime variable was assessed as a predictor of outcomes both as a continuous variable (hours) and as a dichotomous variable of more than 4 hours of voluntary paid overtime versus fewer than four hours worked weekly. The cut point of 4 or more hours of overtime per week was chosen after examining the distribution of the voluntary paid overtime variable; it represents at least half of an 8-hour shift of voluntary overtime in the average week and implies that voluntary overtime was a regular feature of the nurse's work schedule.
Voluntary paid overtime represents the time that nurses chose to work above and beyond their normal work schedule, mandated hours, and/or unpaid hours. Therefore, the two voluntary paid overtime variables (continuous hours and more than 4 hours) included the voluntary paid overtime hours of any nurse who worked only voluntary overtime or voluntary overtime in addition to mandated and/or unpaid overtime. In the first voluntary overtime analyses, we did not exclude the voluntary paid overtime hours of nurses who also worked mandatory or unpaid overtime. Restricting analyses to the voluntary paid overtime hours of nurses who did not work any other type of overtime could limit generalizability. It would exclude the effects of voluntary paid overtime by nurses who chose to work additional hours beyond mandated or unpaid overtime. However, to validate the trends we identified, we performed additional analyses examining the responses of nurses who only worked voluntary paid overtime.
Multivariate analyses of the adverse event and error variables adjusted for the following nurse characteristics: sex, unit, age, years of experience as an RN grouped in 5 year increments, level of education at a baccalaureate degree or higher, hospital-level aggregated staffing measure, presence of dependents at home, permanent employment, representation by a collective bargaining unit, and basic nursing education obtained in the United States. These control variables all showed significant bivariate associations with nurse reports of AEs, work hours, or both. In addition to the nurse characteristics included in the previous analyses, the likelihood of reporting at least one needlestick injury in the last year was also assessed adjusting for clinical risk activities and the presence of sharps safety devices.
It is possible an increased risk of AEs could be merely due to greater opportunities to witness or experience errors or problems due to more hours on the job. In an attempt to rule out this possibility, the proportions of nurses reporting AEs were graphed against hours they worked per week and voluntary paid overtime. Odds ratios for AEs were then examined across 10-hour increments of hours worked per week and hours of voluntary overtime.
3. Results
3.1. Nurse Characteristics and Work Hours
Table 1 presents characteristics of the sample. The mean number of patients cared for by a nurse on his or her last shift aggregated to the hospital level was 5.5 (SD 1.1). The five largest specialties were medical-surgical (31.0%), critical care (19.6%), obstetrics (9.9%), perioperative (9.8%), and emergency department (7.0%). The other departments each represented fewer than 4.0% of respondents. The mean number of hours worked per week was 35.1. Of the 11,516 nurses in the study sample, 7,216 (63%) reported working at least one type of overtime. The distributions of the overtime types are described in Table 2. All of the overtime types had highly skewed distributions. Because of the skewed distributions, in multivariate analyses overtime hours were examined both as a continuous variable and as a dichotomous variable with a cut point of 4 hours.
Table 1.
Sample Characteristics.
| N=11,516 | |
|---|---|
| Percentage or Mean (SD) | |
| Female | 93.9% |
| Age (years) | 39.55 (9.59) |
| Dependents (vs. none) | 61.6% |
| Full-time (vs. part-time) Employment | 62.0% |
| Permanent (vs. Temporary) Employment | 95.2% |
| U.S. Educated | 98.9% |
| Represented by Collective Bargaining Unit | 21.5% |
| Education Level (Highest degree reported) | |
| Associate's | 34.8% |
| Diploma | 25.3% |
| Bachelor's or higher | 35.2% |
Table 2.
Distributions of the Types of Overtime Hours.
| N† | Mean | Standard Deviation | Skewness‡ | |
|---|---|---|---|---|
| Voluntary Paid | 5,532 | 2.64 | 6.25 | 6.66 |
| Mandatory | 1,938 | 0.96 | 3.56 | 9.26 |
| Unpaid | 1,489 | 0.49 | 2.44 | 16.02 |
Does not add to 7,216 because 1,487 nurses worked a combination of overtime categories.
Skewness is a measure of the symmetry of the distribution. The overtime types are highly positively skewed meaning that the majority of observations cluster around zero with a tail extending toward higher number of hours.
Nurses could report working more than one type of overtime in the average week. Of the 5,532 who worked voluntary paid overtime, 4,045 worked only voluntary paid overtime, and 1,487 worked mandatory and/or unpaid overtime, in addition to working voluntary paid overtime hours. Of all the nurse respondents, 9.6% indicated that they had sustained a needlestick or sharps injury in the last year. Nurse reports of occasional/frequent AEs were 15.1% for wrong medication or dose, 19.8% for patient falls with injury, 32.8% for work injuries, and 35.2% for nosocomial infections.
3.2. Adverse Events and Errors
Table 3 presents the associations between work hours and voluntary paid overtime with AEs revealed in the multivariate analyses. The reported frequency of all 5 types of AEs was s of AEs was significantly significantly higher— 14% to 28% higher — among nurses reporting an average work week longer than 40 hours. Voluntary paid overtime was linked with medication errors and needlesticks both as a linear trend (per hour per week) and with a cut point of regular voluntary paid overtime (4 hours or more in the average work week). Regular voluntary overtime was linked to a 30% and 20% increased risk of reporting that these problems occurred commonly over the previous year. The nature of the relationships between voluntary paid overtime and reports of patient falls, nosocomial infections, and work injuries was less consistent.
Table 3.
Adjusted Odd Ratios for Reports of Adverse Events in Relation to Work Hours.
| Worked Over 40 hours in the Average Week (vs. Worked 40 or Fewer Hours) OR (95% CI) |
Hours of Voluntary Paid Overtime Worked in the Average Week (Continuous Variable) OR (95% CI) |
Worked More than 4 hours of Voluntary Paid Overtime in the Average Week (vs. Worked 4 or Fewer Hours) OR (95% CI) |
|
|---|---|---|---|
| Occasional/Frequent Wrong Med. or Dose† |
1.28** (1.10, 1.49) |
1.02*** (1.01, 1.02) |
1.30** (1.11, 1.53) |
| Occasional/Frequent Falls with Injury† |
1.17* (1.02, 1.36) |
1.01* (1.00, 1.02) |
1.07 (0.91, 1.25) |
| Occasional/Frequent Nosocomial Infections† |
1.14* (1.02, 1.28) |
1.01* (1.00, 1.01) |
1.04 (0.91, 1.18) |
| Occasional/Frequent Work Injuries† |
1.25*** (1.11, 1.40) |
1.01 (1.00, 1.01) |
1.17* (1.03, 1.32) |
| Any Needlestick Injuries in the Last Year‡ |
1.28** (1.08, 1.52) |
1.01** (1.00, 1.02) |
1.20* (1.01, 1.42) |
p<0.05
p<0.01
p<0.001.
adjusted for nurse characteristics (sex, unit type, age, years of experience as an RN, education level, hospital-level staffing, temporary employment, dependents at home, union membership, and nursing education outside the U.S.).
adjusted for nurse characteristics (see above); risk factors for needlestick injury including starting IVs and routine phlebotomy performed on the last shift; and presence of sharps safety devices (see text).
For instance, after adjusting for nurse characteristics, all of the work hour variables remained significantly associated with reports of occasional/frequent wrong medication or dose administration. Those who worked more than 40 hours per week were 28% more likely to report that patients occasionally/frequently received the wrong medication or dose. For each additional hour of voluntary paid overtime worked each week, the likelihood that a nurse reported occasional/frequent wrong medication or dose administration increased by 2%. The mean amount of voluntary paid overtime in this study was almost 3 hours per week. Applying the multiplicative nature of odds ratios in logistic regression, the models suggest that a three-hour increase in voluntary paid overtime would result in an odds ratio of 1.023 or a 6.1% increased likelihood of reporting occasional/frequent wrong medication or dose administration errors as compared with a nurse working no overtime. Compared to those who reported working fewer than four hours of paid voluntary overtime in the average week, those who reported working more than four hours were 30% more likely to report occasional/frequent wrong medication or dose administration.
When patterns in the reports of AEs among nurses who worked only voluntary paid overtime were examined using the same modeling strategies and including the same control variables, many of the relationships with AEs remained statistically significant. In this subsample, the odds of reporting occasional/frequent wrong medication or dose administration increased by 1.2% (OR 1.012, p=0.012) for each additional hour of voluntary paid overtime. In other words, a three-hour increase in voluntary paid overtime would result in a 1.0123 or 3.6% increased likelihood of reporting occasional/frequent wrong medication or dose administration errors. Similarly in this subsample, a three-hour increase in voluntary paid overtime resulted in a 3% increase in the odds of reporting occasional/frequent work injuries (OR 1.010, p=0.013) and a 4.3% increase in the likelihood of reporting a needlestick injury in the past year (OR 1.014, p=0.002).
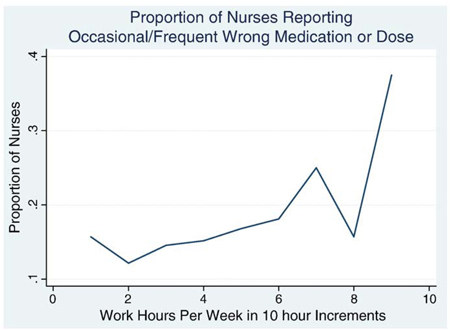
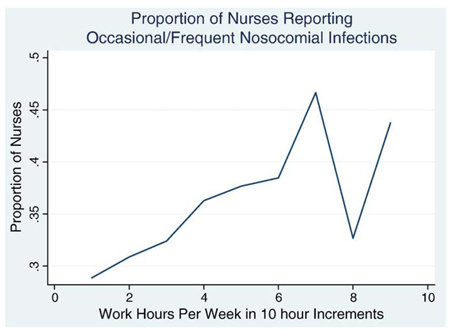
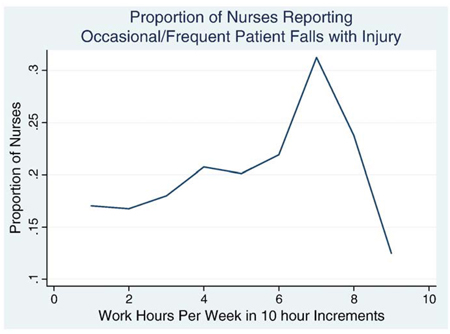
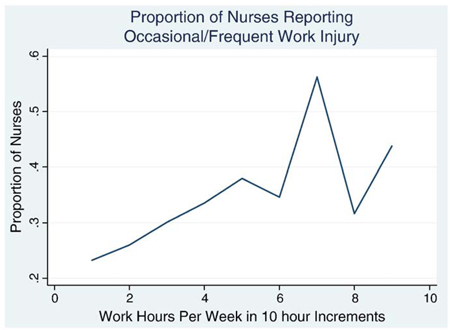
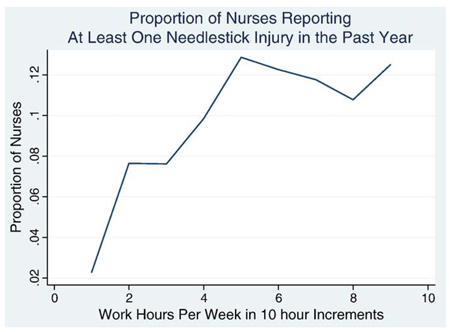
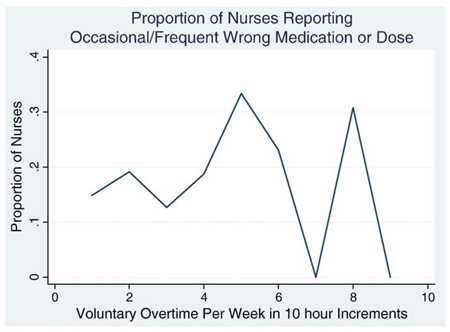
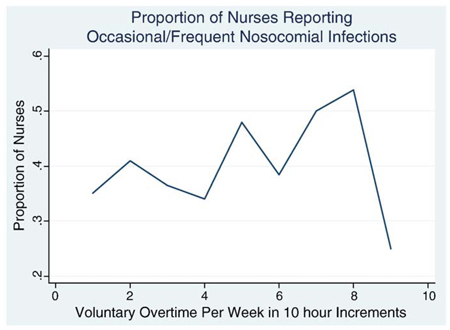
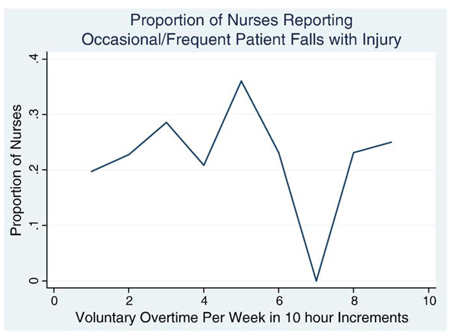
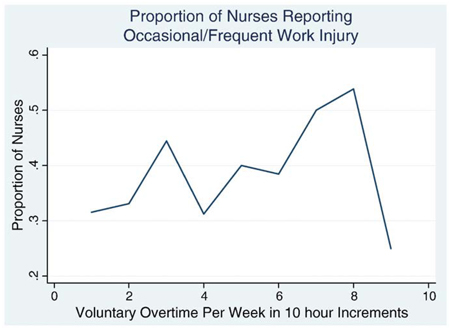
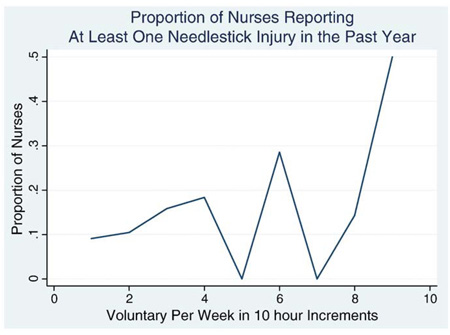
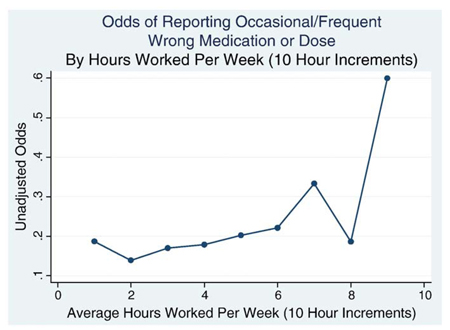
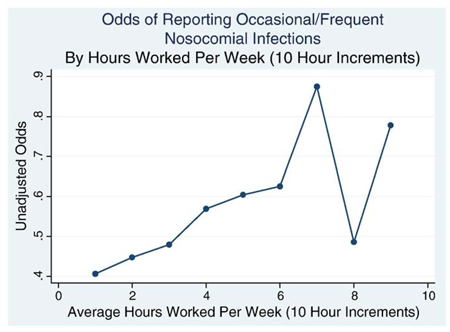
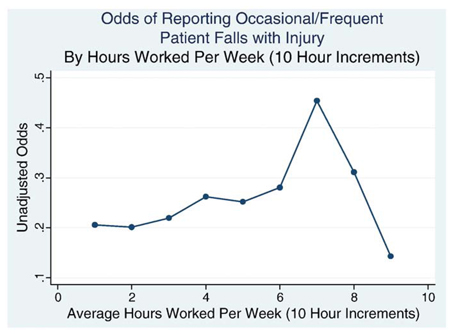
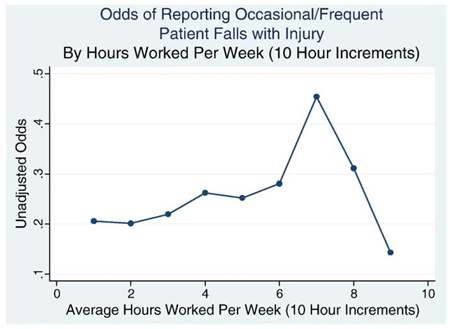
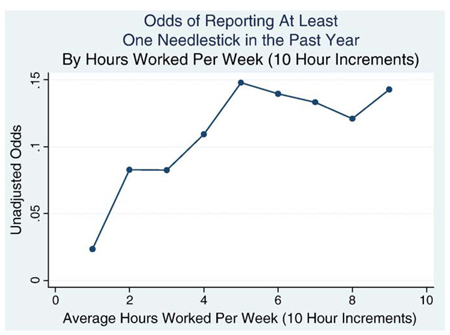
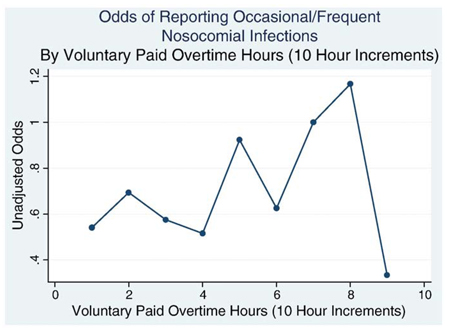
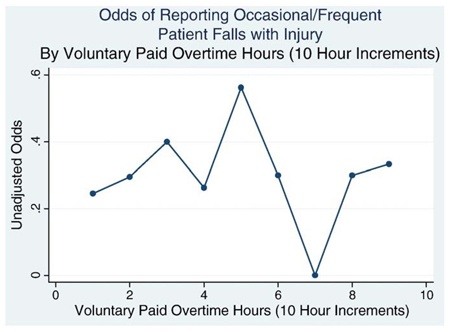
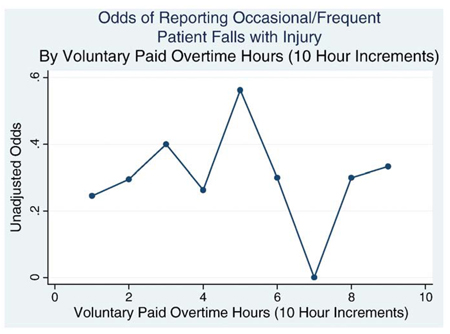
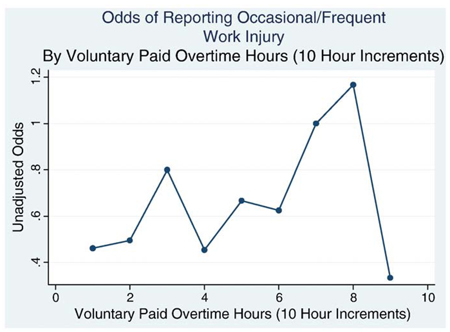
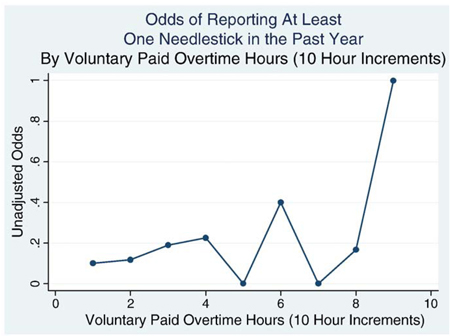
Finally, the proportions of nurses reporting AEs (Appendix A) and odds of reporting AEs (Appendix B) were graphed against hours worked per week and against voluntary paid overtime. Linear increases in adverse event reports as both total work week and voluntary paid overtime hours were observed. There was no evidence of a specific point of discontinuity. In other words, there was no specific time point at which AE reporting increased more than expected.
4. Discussion
The results suggest that nurses working more than 40 hours per week have an increased likelihood of observing or experiencing occasional or frequent (versus never or rare) AEs, particularly wrong medication and dose administration and needlestick injuries. In particular, voluntary paid overtime increases the risk of both of these AEs. In this study, overtime was assumed to be related to fatigue in nurses, such that the more hours nurses reported working, the more fatigued they might be. This indirect way of assessing fatigue is limited because the study did not assess the amount the respondents slept or other factors that might be related to fatigue such as emotional and physical stressors. Data suggestive of a relationship between medication errors and overtime has been reported previously (Dean, Scott, & Rogers, 2006; Jagsi et al., 2005; Rogers et al., 2004; Scott et al., 2006). The strong relationship between nurses reporting occasional/frequent medication errors may represent a decrease in vigilance associated with fatigue.
Although not as strong, relationships were found between work hours and nurse reports of occasional/frequent patient falls with injury and occasional/frequent nosocomial infections. Increased odds of nurses reporting occasional/frequent patient falls with injury were found to be related to working over 40 hours per week and with increasing hours of voluntary paid overtime. After controlling for nurse characteristics, working more than 40 hours per week and working increasing hours of voluntary paid overtime were significantly related to the likelihood of nurses reporting occasional or frequent nosocomial infections. This relationship may not have been as strong as that between medication errors and work hours because nosocomial infections may be difficult for staff nurses to identify, particularly if there is a lack of continuity of care. Patients are often transferred between units or stay in the same unit but have different nurses caring for them. In these situations, it may not be evident that a patient acquired an infection during the hospital stay. In addition, acquisition of a nosocomial infection is multifactorial and is related to both hospital and patient factors that were not examined in this study.
The relationship between working overtime, and in particular working voluntary paid overtime, with adverse outcomes was also seen in relation to reports of injuries among nurses. In this study, the term “work injury” could be broadly defined by the nurse survey participants to include not only needlestick and sharp instrument injuries, but also musculoskeletal injuries and injuries from assaults. The likelihood of nurses reporting occasional/frequent work injuries was significantly related to both working over 40 hours per week and working more than four hours of voluntary paid overtime per week, even after controlling for nurse characteristics. In addition, the relationships between voluntary paid overtime with work injuries and needlesticks were found even when the analyses were limited to nurses who only worked voluntary paid overtime. Because the term “work injuries” is broad, many contributing factors could be implicated. Certainly physical fatigue can increase the risk of physical injury. Irritability resulting from fatigue could decrease therapeutic communication skills nurses use when working with combative or agitated patients. In addition, a lack of concentration or vigilance could increase the risk of needlestick injuries. Heightened risk of reporting at least one needlestick in the prior year was associated with all of the voluntary paid overtime work hour variables.
While the effects observed here are generally consistent with the literature, several limitations of the approach taken in this study should be borne in mind and offer directions for future research. One limitation relates to the age of the data. Although the dataset is from 1999, one of its prime advantages is the large sample of nurses (n = 11,516) providing specific information about their work hours, both total hours per week and the number of weekly hours of voluntary paid overtime. In addition, the dataset also contains nurse-level reports of AEs, along with demographic and staffing data. However, since data collection, there have been a number of published studies focusing on the detrimental effects of work hours on adverse events and errors (Clarke, 2007; Dembe et al., 2005; Ilhan et al., 2006; Landrigan et al., 2004; Lockley et al., 2004; Rogers et al., 2004; Scott et al., 2006; Stone, Mooney-Kane, et al., 2007; Trinkoff, Geiger-Brown et al., 2006; Trinkoff, Le et al., 2006; Trinkoff et al., 2007). In addition, the American Nurses Association issued a statement in 2006 articulating its position that it is the RN's responsibility to evaluate his/her level of fatigue when accepting or rejecting overtime, including voluntary paid overtime assignments (American Nurses Association, 2006). This increase in awareness of the effect of fatigue on patient and nurse safety may prompt more nurses to voluntarily limit the total number of hours they work. Therefore, the effects found using data from 1999 may not be as strong today. Yet, it is also possible that with the recent economic downturn, nurses are feeling the need to work additional hours to compensate for the lost income of other family members.
Another limitation relates to difficulties in differentiating between a true effect of work week hours on adverse events and errors as opposed to the possibility that nurses who work more hours are more likely to observe both errors as a result of spending more time with patients and to sustain more work-related injuries because of increased time on the job and exposure to risky procedures. In this dataset, where relatively few nurses reported working the upper levels of overtime observed, we could not distinguish between a steady increase in exposures or opportunities for error or injury with increasing time on the job, a continuous upward influence of fatigue on errors and events, and the possibility that a threshold exists beyond which safety is particularly jeopardized by further work. The absence of a specific point at which AE reporting increased more than expected in the linear trend may have been due to the small number of nurses working at the upper intervals of hours per week and hours of overtime per week. There may have not been enough power to detect a significant increase in the proportion of nurses reporting AEs and needlestick injuries at the upper extremes of work hours. Future studies should not only increase the number of workers taking on large amounts of overtime, but should also match hours that a nurse worked prior to the occurrence of specific adverse events.
A third set of limitations relates to the definition of the work hours variables. This study examined overtime in terms of the hours in an average work week. However, both shift length and rotating shifts have been shown to be related to adverse events (Muecke, 2005; Rogers et al., 2004; Stone, Du, & Gershon, 2007; Scott et al., 2006). One advantage of using the work week as the base measurement is that it assesses the cumulative effects of fatigue that accrue over the course of several days. Because this study only examined nurses’ reports regarding their average work weeks, the effects of circadian rhythm disruption and acute sleep deprivation that occur with rotating shifts and extended shifts could not be explored. In this study, nurses were asked to report how many hours they worked in a week, on average, over the past year. This long time span guards against nurses responding based on a work week that might be exceptional or anomalous for them. However, without corroboration from other data sources, such survey data are vulnerable to recall and response bias.
We specifically examined associations between working more than 40 hours per week and working voluntary paid overtime on adverse events. Because of the construction of the survey question, there could have been overlap between mandatory overtime and unpaid overtime and we did not examine those two variables. Because the nature of mandatory overtime and unpaid overtime may be different from voluntary paid overtime, the study findings cannot be generalized to either of those overtime variables. In addition, the overtime measures reported in this study were self-reported and were not validated against other data sources.
The final category of limitations relates to the construction of the outcome variables. The work injury, patient falls with injury, wrong medication or dose, and nosocomial infection variables were categorized as never, rarely, occasionally, and frequently. The way these response categories were understood may have varied from respondent to respondent. Nonetheless, by grouping “never” with “rarely” and “occasionally” with “frequently,” we have arrived at an outcome variable with a relatively clear meaning that was reported by sizeable numbers of nurses. We are, however, in less of a position to make distinctions between the frequencies of events.
This study extends the literature in several ways. A variety of adverse events were studied, including needlestick injuries. These injuries have a clear definition and prior research suggests that self-reports of these injuries suffer less from memory issues and reporting bias (Aiken, Sloane, & Klocinski, 1997). In addition, the extensive demographic information provided on the survey allowed for analyses that controlled for many potential confounding variables. Overall, the results of this study corroborate previous findings that increased nurse work hours are related to adverse events in patients (Landrigan et al., 2004; Lockley et al., 2004; Rogers et al., 2004; Scott et al., 2006). Results here add to the emerging literature by suggesting that even hours of overtime that are voluntary appear to increase risk for adverse events in both nurses and patients.
5. Summary
A large body of literature has demonstrated that extended-work duration results in healthcare worker fatigue. Fatigue-related cognitive impairment, in turn, has been linked to adverse events and errors for patients and for healthcare workers. Analyses here suggest that working more than 40 hours per week and working voluntary paid overtime are both significantly related to adverse events and errors in patients and nurses. In this study of 11,516 Pennsylvania RNs, reports of falls, nosocomial infections, and work injuries were all associated with greater length of average work week; however, the likelihood of reporting occasional or frequent medication errors and at least one needlestick injury in the past year had the strongest and most consistent relationships with the work hour and voluntary paid overtime variables.
6. Impact on Industry
Overtime in healthcare is an important issue because it has implications for the safety of both patients and healthcare workers. Whereas resident physicians have limits on the total number of hours they work, such limits do not exist for nurses. Legislation related to nurses has thus far focused on banning or limiting mandatory overtime, without addressing voluntary overtime that can also have negative impacts on safety. This may be due, in part, to an assumption that a nurse who is fatigued will not voluntarily work beyond what is required. However, it can be difficult for individuals to recognize the effect of fatigue on their practice (Arnedt, Owens, Crouch, Stahl, & Carskadon, 2005). Limiting voluntary overtime is further complicated by the fact that for nurses who are paid hourly, there is a strong financial incentive to work additional hours, particularly if those hours are paid at premium rates. Further, nurses may not turn down voluntary overtime because of guilt or coercion from managers and peers. The results here suggest increased time at work may have negative consequences for patient safety and nurse occupational health. Researchers need to continue to critically examine the effects of overtime, including voluntary overtime, on patient and nurse safety. As evidence is generated, it will become increasingly important for professional organizations, healthcare facilities, and legislators to design evidence-based policies and practices to protect patients and nurses from the errors and adverse events that can result from long work hours while considering the realities of practice in clinical settings.
Acknowledgements
This study was supported by funding from the National Institute for Nursing Research, National Institutes of Health – Advanced Training in Nursing Outcomes Research (T32-NR-007104, Aiken, PI), Outcomes of Hospital Staffing (R01-NR-004513, Aiken, PI), and the Center for Nursing Outcomes Research (P30-NR-005043, Aiken, PI).
Biographies
Danielle Olds is a pre-doctoral fellow at the Center for Health Outcomes and Policy Research and a PhD student at the University of Pennsylvania School of Nursing. She has a master's degree in public health and a master's degree in Community Health Nursing from Case Western Reserve University. Her research interests are focused on organizational factors in nursing that contribute to adverse events in patients.
Dr. Sean P. Clarke currently holds the RBC Chair in Cardiovascular Nursing Research at the University of Toronto and the University Health Network. From 2001 to 2008 he served as Associate Director of the Center for Health Outcomes and Policy Research at the University of Pennsylvania School of Nursing. He holds graduate degrees in nursing from McGill University and completed postdoctoral training at the University of Pennsylvania. His research interests relate to the influence of organizational factors on safety and quality in health care settings.
Appendix A. Hours Worked Per Week
Fig. 1. Proportion of Nurses Reporting Occasional/Frequent Wrong Medication or Dose by Hours Worked per Week in 10 Hour Increments.
Fig. 2. Proportion of Nurses Reporting Occasional/Frequent Nosocomial Infections by Hours Worked per Week in 10 Hour Increments.
Fig. 3. Proportion of Nurses Reporting Occasional/Frequent Patient Falls with Injury by Hours Worked per Week in 10 Hour Increments.
Fig. 4. Proportion of Nurses Reporting Occasional/Frequent Work Injury by Hours Worked per Week in 10 Hour Increments.
Fig. 5. Proportion of Nurses Reporting at Least One Needlestick in the Past Year by Hours Worked per Week in 10 Hour Increments.
A.1. Voluntary Paid Overtime Hours
Fig. 6. Proportion of Nurses Reporting Occasional/Frequent Wrong Medication or Dose by Voluntary Paid Overtime Hours Worked per Week in 10 Hour Increments.
Fig. 7. Proportion of Nurses Reporting Occasional/Frequent Nosocomial Infections by Voluntary Paid Overtime Hours Worked per Week in 10 Hour Increments.
Fig. 8. Proportion of Nurses Reporting Occasional/Frequent Patient Falls with Injury by Voluntary Paid Overtime Hours Worked per Week in 10 Hour Increments.
Fig. 9. Proportion of Nurses Reporting Occasional/Frequent Work Injury by Voluntary Paid Overtime Hours Worked per Week in 10 Hour Increments.
Fig. 10. Proportion of Nurses Reporting at Least One Needlestick Injury in the Past Year by Voluntary Paid Overtime Hours Worked per Week in 10 Hour Increments.
Appendix B. Hours Worked Per Week
Fig. 1. Odds of Reporting Occasional/Frequent Wrong Medication or Dose By Hours Worked Per Week in 10 Hour Increments.
Fig. 2. Odds of Reporting Occasional/Frequent Nosocomial Infections By Hours Worked Per Week in 10 Hour Increments.
Fig. 3. Odds of Reporting Occasional/Frequent Patient Falls with Injury By Hours Worked Per Week in 10 Hour Increments.
Fig. 4. Odds of Reporting Occasional/Frequent Work Injury By Hours Worked Per Week in 10 Hour Increments.
Fig. 5. Odds of Reporting At Least One Needlestick Injury By Hours Worked Per Week in 10 Hour Increments.
B.1. Voluntary Paid Overtime
Fig. 6. Odds of Reporting Occasional/Frequent Wrong Medication or Dose By Voluntary Paid Overtime in 10 Hour Increments.
Fig. 7. Odds of Reporting Occasional/Frequent Nosocomial Infections By Voluntary Paid Overtime in 10 Hour Increments.
Fig. 8. Odds of Reporting Occasional/Frequent Patient Falls with Injury By Voluntary Paid Overtime in 10 Hour Increments.
Fig. 9. Odds of Reporting Occasional/Frequent Work Injury By Voluntary Paid Overtime in 10 Hour Increments.
Fig. 10. Odds of Reporting At Least One Needlestick Injury By Voluntary Paid Overtime in 10 Hour Increments.
References
- Aiken LH, Sloane DM, Klocinski JL. Hospital nurses’ occupational exposure to blood: Prospective, retrospective, and institutional reports. American Journal of Public Health. 1997;87(1):103–107. doi: 10.2105/ajph.87.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Cheung RB, Sloane DM, Silber JH. Educational levels of hospital nurses and surgical patient mortality. JAMA. 2003;290:617–1623. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Nurses Association. Position Statement. [Last updated: December 8, 2006. Last accessed: May 19, 2009];Assuring Patient Safety: Registered Nurses’ Responsibility in All Roles and Settings to Guard Against Working When Fatigued. 2006 Available at http://www.safestaffingsaveslives.org/WhatisSafeStaffing/MaketheCase/Fatigue.aspx. [PubMed]
- American Nurses Association. Mandatory Overtime. [Last updated: September 17, 2008. Last accessed: January 2, 2009];2008 Available at http://nursingworld.org/mainmenucategories/ANAPoliticalPower/State/StateLegislativeAgenda/Mandatoryovertime.aspx.
- Arnedt JT, Owens J, Crouch M, Stahl J, Carskadon MA. Neurobehavioral performance of residents after heavy night call vs. after alcohol ingestion. JAMA. 2005;294:1025–1033. doi: 10.1001/jama.294.9.1025. [DOI] [PubMed] [Google Scholar]
- Ayas NT, Barger LK, Cade BE, Hashimoto DM, Rosner B, Cronin JW, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA. 2006;296:1055–1062. doi: 10.1001/jama.296.9.1055. [DOI] [PubMed] [Google Scholar]
- Berney B, Needleman J. Trends in nurse overtime, 1995–2002. Policy, Politics, and Nursing Practice. 2005;6(3):183–190. doi: 10.1177/1527154405279334. [DOI] [PubMed] [Google Scholar]
- Berney B, Needleman J. Impact of nursing overtime on nurse-sensitive patient outcomes in New York hospitals, 1995–2000. Policy, Politics, and Nursing Practice. 2006;7(2):87–100. doi: 10.1177/1527154406291132. [DOI] [PubMed] [Google Scholar]
- Berney B, Needleman J, Kovner C. Factors influencing the use of Registered Nurse overtime in hospitals, 1995–2000. Journal of Nursing Scholarship. 2005;37(2):165–172. doi: 10.1111/j.1547-5069.2005.00032.x. [DOI] [PubMed] [Google Scholar]
- Clarke SP. Hospital work environments, nurse characteristics, and sharps injuries. American Journal of Infection Control. 2007;35:302–309. doi: 10.1016/j.ajic.2006.07.014. [DOI] [PubMed] [Google Scholar]
- Dean GE, Scott LD, Rogers AE. Infants at risk: When nurse fatigue jeopardizes quality care. Advances in Neonatal Care. 2006;6(3):120–126. doi: 10.1016/j.adnc.2006.02.001. [DOI] [PubMed] [Google Scholar]
- Dembe AE, Erickson JB, Delbos RG, Banks SM. The impact of overtime and long work hours on occupational injuries and illnesses: New evidence from the United States. Occupational and Environmental Medicine. 2005;62:588–597. doi: 10.1136/oem.2004.016667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber PJ. The behavior of maximum likelihood estimates under nonstandard conditions; Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability; Berkeley, CA: University of California Press; 1967. pp. 221–223. [Google Scholar]
- Ilhan MN, Durukan E, Aras E, Turkcuoglu S, Aygun R. Long working hours increase the risk of sharp and needlestick injury in nurses: the need for new policy implication. Journal of Advanced Nursing. 2006;56(5):563–568. doi: 10.1111/j.1365-2648.2006.04041.x. [DOI] [PubMed] [Google Scholar]
- Jagsi R, Kitch BT, Weinstein DF, Campbell EG, Hutter M, Weissman JS. Residents report on adverse events and their causes. Archives of Internal Medicine. 2005;165:2607–2613. doi: 10.1001/archinte.165.22.2607. [DOI] [PubMed] [Google Scholar]
- Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. New England Journal of Medicine. 2004;351:1838–1848. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- Lilley R, Feyer A, Kirk P, Gander P. A survey of forest workers in New Zealand. Do hours of work, rest and recovery play a role in accidents and injury? Journal of Safety Research. 2002;33:53–71. doi: 10.1016/s0022-4375(02)00003-8. [DOI] [PubMed] [Google Scholar]
- Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, et al. Effect of reducing interns’ weekly work hours on sleep and attentional failures. New England Journal of Medicine. 2004;351:1829–1837. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- Lockley SW, Landrigan CP, Barger LK, Czeisler CA. When policy meets physiology. The challenge of reducing resident work hours. Clinical Orthopaedics and Related Research. 2006;449:116–127. doi: 10.1097/01.blo.0000224057.32367.84. [DOI] [PubMed] [Google Scholar]
- Mitler MM, Milller JC, Lipsitz JJ, Walsh JK, Wylie CD. The sleep of long-haul truck drivers. New England Journal of Medicine. 1997;337:755–761. doi: 10.1056/NEJM199709113371106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muecke S. Effects of rotating night shifts: literature review. Journal of Advanced Nursing. 2005;50(4):433–439. doi: 10.1111/j.1365-2648.2005.03409.x. [DOI] [PubMed] [Google Scholar]
- Rice C, Leach D. Implementation of ACGME Common Duty Hour Standards. [Last updated: August 1, 2003. Accessed: July 8, 2008];2003 Available at http://www.acgme.org/acWebsite/dutyhours/dh_resdutyhr.pdf.
- Rogers WH. Regression standard errors in clustered samples. Stata Technical Bulletin. 1993;13:19–23. [Google Scholar]
- Rogers AE, Hwang WT, Scott LD, Aiken LH, Dinges DF. The working hours of hospital staff nurses and patient safety. Health Affairs. 2004;23(4):202–212. doi: 10.1377/hlthaff.23.4.202. [DOI] [PubMed] [Google Scholar]
- Scott LD, Rogers AE, Hwang WT, Zhang Y. Effects of critical care nurses’ work hours on vigilance and patients’ safety. American Journal of Critical Care. 2006;13(1):30–37. [PubMed] [Google Scholar]
- Stone PW, Du Y, Gershon RRM. Organizational climate and occupational health outcomes in hospital nurses. Journal of Occupational and Environmental Medicine. 2007;49(1):50–58. doi: 10.1097/01.jom.0000251622.05429.0c. [DOI] [PubMed] [Google Scholar]
- Stone PW, Mooney-Kane C, Larson EL, Horan T, Glance LG, Zwanzinger J, et al. Nurse working conditions and patient safety outcomes. Medical Care. 2007;45(6):571–578. doi: 10.1097/MLR.0b013e3180383667. [DOI] [PubMed] [Google Scholar]
- Trinkoff A, Geiger-Brown J, Brady B, Lipscomb J, Muntaner C. How long and how much are nurses now working? American Journal of Nursing. 2006;106(4):60–71. doi: 10.1097/00000446-200604000-00030. [DOI] [PubMed] [Google Scholar]
- Trinkoff AM, Le R, Geiger-Brown J, Lipscomb J, Lang G. Longitudinal relationship of work hours, mandatory overtime, and on-call to musculoskeletal problems in nurses. American Journal of Industrial Medicine. 2006;49:964–971. doi: 10.1002/ajim.20330. [DOI] [PubMed] [Google Scholar]
- Trinkoff A, Le R, Geiger-Brown J, Lipscomb J. Work schedule, needle use, and needlestick injuries among registered nurses. Infection Control and Hospital Epidemiology. 2007;28:156–164. doi: 10.1086/510785. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Transportation. Federal Motor Carrier Safety Administration, Final Rule Part 395.3, Hours of Service of Drivers. [Last Accessed: October 13, 2008];2005 Available at http://www.fmcsa.dot.gov/rules-regulations/administration/fmcsr/fmscrruletext.asp?rule_toc=764§ion395.5§ion_toc=121208.
- White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48(4):817–830. [Google Scholar]