Class III malocclusion is a consequence of maxillary deficiency and/or mandibular prognathism, often resulting in an anterior crossbite and a concave profile.1 Young patients with maxillary hypoplasia are usually treated with a facemask: heavy anterior traction is applied on the maxilla to stimulate its growth and to restrain or redirect mandibular growth. Forward and downward movement of the maxilla as well as favorable changes in the amount and direction of mandibular growth has been reported.2–5 However, these forces generally result in a posterior rotation of the mandible and an increased vertical dimension of the face.2,4,6 Moreover, dental compensations (proclination of the upper incisors and uprighting of the lower incisors) are observed as a consequence of the application of forces on the teeth,4,7 and facemask wear is usually limited to 14 hours per day at best.
Titanium miniplates used for anchorage now offer the possibility to apply pure bone-borne orthopedic forces between the maxilla and the mandible for 24 hours per day, avoiding any dentoalveolar compensations.
Summary of Cases and Diagnosis
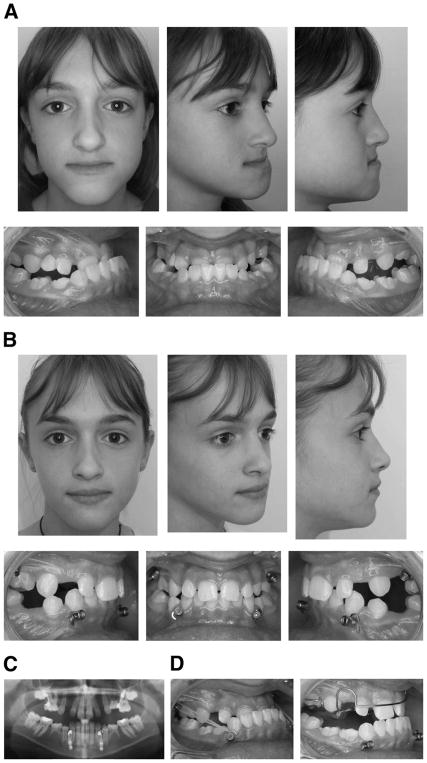
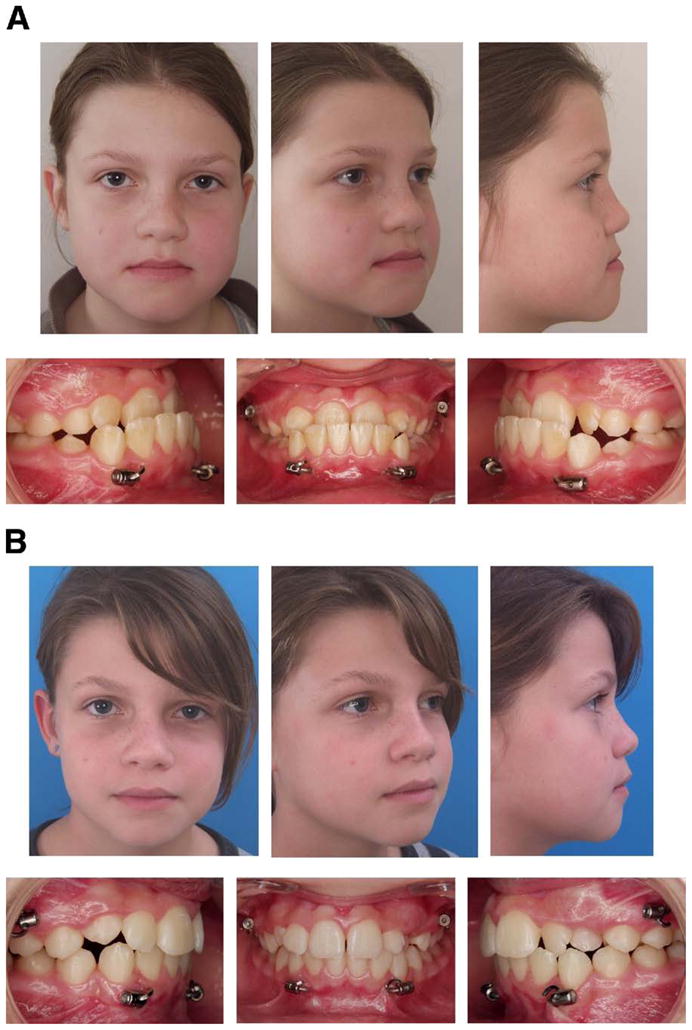
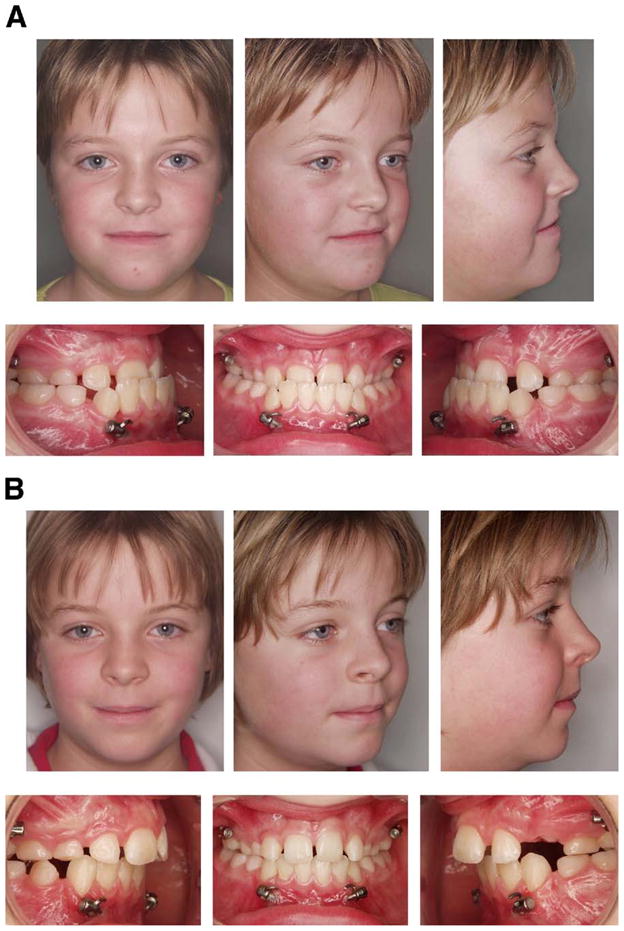
Three girls (aged 10 to 11 years) presenting with a severe skeletal Class III relationship with a maxillary deficiency and concave soft tissue profile were treated according to the same treatment plan (Figs 1A, 2A, 3A). Two of them had an anterior crossbite without anterior shift of the mandible (cases 2 and 3). One had an edge-to-edge incisor occlusion in centric relation, with a forward posture into maximum intercuspation (case 1).
FIGURE 1.
Patient 1. A, Pretreatment facial and intraoral photographs. B, Post-treatment facial and intraoral photographs.
FIGURE 2.
Patient 2. A, Pretreatment facial and intraoral photographs. B, Post-treatment facial and intraoral photographs.
FIGURE 3.
Patient 3. A, Pretreatment facial and intraoral photographs. B, Post-treatment facial and intraoral photographs. C, Panoramic radiograph after placement of miniplates. D, Treatment progress: placement of maxillomandibular elastics (left) and placement of bite plane (right).
Pretreatment cephalometric evaluation of the 3 cases showed a skeletal Class III relationship with hypoplasia of the maxilla combined with a normal or increased mandibular size and normal or slightly decreased vertical dimensions (Table 1). The patients’ upper incisors were proclined or retroclined, and the lower incisors were normal or proclined.
Table 1.
CEPHALOMETRIC VALUES
| Patient 1 |
Patient 2 |
Patient 3 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| T1 (10 yr 0 mo) | T2 (10 yr 9 mo) | T3 (11 yr 8 mo) | T1 (10 yr 2 mo) | T2 (11 yr 4 mo) | T3 (12 yr 5 mo) | T1 (11 yr 0 mo) | T2 (12 yr 7 mo) | T3 (15 yr 9 mo) | |
| SNA (°) | 85 | 92 | 90.5 | 81.5 | 86 | 85.5 | 72 | 79 | 82 |
| SNB (°) | 87 | 87 | 87 | 81.5 | 80 | 80 | 77 | 76.5 | 80 |
| ANB (°) | −2 | 5 | 3.5 | 0 | 6 | 5.5 | −5 | 2.5 | 2.5 |
| Wits (mm) | −5 | 2.5 | 1.5 | −6 | 4 | 3 | −11 | −1 | 1 |
| SN-PP (°) | 4 | 2.5 | 3.5 | 5.5 | 3 | 3 | 12 | 8.5 | 8.5 |
| GoGnSN (°) | 27 | 26.5 | 26 | 28 | 30 | 28 | 32 | 32 | 27 |
| G′-Sn-Pog′ (°) | −1 | 8 | 7.5 | 1 | 16 | 14 | −4 | 12 | 10 |
| Mx1-PP (°) | 116 | 120 | 122 | 101 | 106 | 109 | 115 | 114 | 114 |
| Md1-MP (°) | 93.5 | 100 | 99 | 95 | 101 | 102 | 89 | 94 | 98 |
| UL-E-line (mm) | 3.5 | −1 | −1 | 10 | 3 | 4.5 | 9.5 | 5 | 9 |
| LL-E-line (mm) | 0.5 | −2 | −1 | 5.5 | 2 | 3.5 | 3 | 3 | 8 |
Abbreviations: T1, beginning of treatment; T2, end of treatment; T3, follow-up; S, Sella; N, Nasion; A, Point A; B, Point B; Wits, distance between perpendicular projection of A and B on Downs occlusal plane; PP, Palatal Plane; Go, Gonion; Gn, Gnathion; G′, soft-tissue Glabella; Sn, subnasale; Pog′, soft-tissue Pogonion; Mx1, maxillary central incisor; Md1, mandibular central incisor; MP, mandibular Plane; UL, upper Lip, E-line, line from tip of the nose to Pog′; LL, lower Lip.
Treatment Objectives
The main treatment objective was to achieve a reduction of the facial concavity, maximize skeletal maxillary changes, and minimize dentoalveolar movement.
Treatment Plan
The 3 patients were treated exclusively by intermaxillary traction between miniplates placed in the maxilla and in the mandible, in combination with a bite plane to jump the crossbite (Fig 3D).
Treatment Alternatives
The skeletal deformity of these patients was judged too severe to consider treatment by dentoalveolar compensation alone, and the degree of maxillary hypoplasia and age of the patients were not favorable for facemask therapy. Orthognathic surgery after growth completion was offered to the patients. However, to avoid retaining such severe facial deformity until adulthood, each of the 3 patients and their parents preferred to try orthopedic traction from skeletal anchorage, even though they had been informed about the possible need for future orthognathic surgery.
Treatment Progress
Four orthodontic miniplates (Bollard; Tita-Link, Brussels, Belgium) were inserted into the infrazygomatic crests and between the canine and lateral incisor (cases 1 and 2) or between the canine and first premolar (case 3) in the mandible, on both the right and left sides (Fig 3C). Surgery was performed with patients under general anesthesia (cases 1 and 2) or local anesthesia (case 3). The miniplates were fixed to the bone with 2 or 3 titanium screws (2.3 mm in diameter and 5 mm in length) after predrilling with a 1.6-mm-diameter bur, as previously described.8 Three weeks after surgery, maxillomandibular elastics were attached between the upper and lower miniplates on each side, applying a force of 100 g per side (Fig 3D). The patients were asked to replace the elastics once a day and to wear them 24 hours per day. After 1 month (case 1) or 2 months (cases 2 and 3), a removable bite plane was placed to eliminate the occlusal interference in the incisor region (Fig 3D). At this time, the elastic force was increased to 200 g per side.
After 7 months (cases 1 and 2) or 12 months (case 3) of orthopedic traction, the bite plane was removed. The traction was maintained full time for a total period of 12 months (cases 1 and 2) or 16 months (case 3). No local infections were observed around any of the miniplates. They remained stable throughout treatment. During the follow-up period after the active treatment, the patients wore the elastics at night for retention.
Results
The anterior crossbite was corrected in each patient (Figs 1B, 2B, 3B). Their soft tissue profiles considerably improved, with anterior displacement of the whole midface (infraorbital ridge, nose, and upper lip), reducing the paranasal concavity. Almost no anterior displacement of the lower lip and chin was observed at the end of the traction, leading to an improvement of the relationship between the upper and lower lip. The tip of the nose moved slightly upward.
Lateral cephalograms were taken at the beginning of treatment, at the end of orthopedic treatment, and at follow-up 11 to 38 months later (Fig 4).
FIGURE 4.
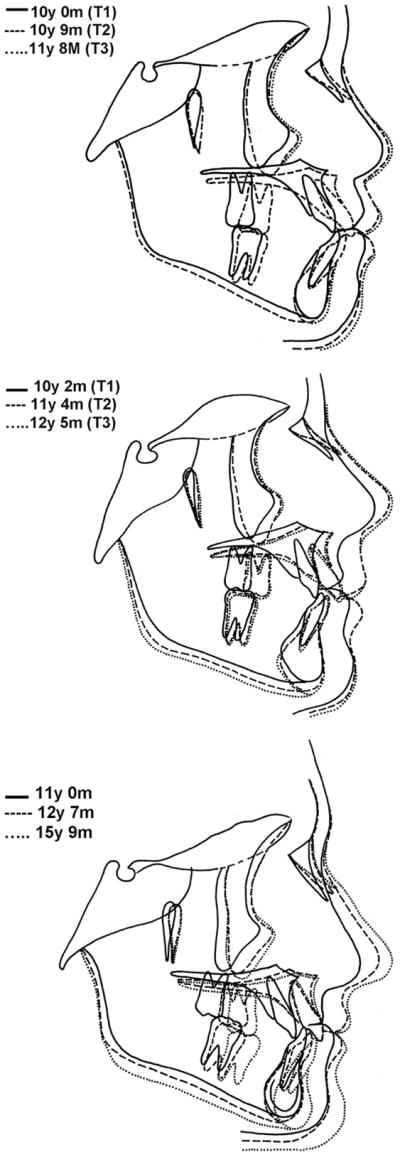
Superimposed cephalometric tracings of 3 patients. T1, beginning of treatment; T2, end of treatment; T3, follow-up.
Cephalometric evaluation between the beginning of treatment and end of treatment showed a marked increase of ANB, Wits, and facial convexity (G′-Sn-Pg′) values in all 3 cases (Table 1). No rotation of the mandible was observed in cases 1 and 3, whereas a slight clockwise rotation was seen in case 2; there was a slight counterclockwise rotation of the maxilla in all patients. No major changes occurred in the upper incisor inclination, whereas the lower incisors were proclined. During the follow-up period (from end of treatment to 11 to 38 months later), the Class III correction was maintained.
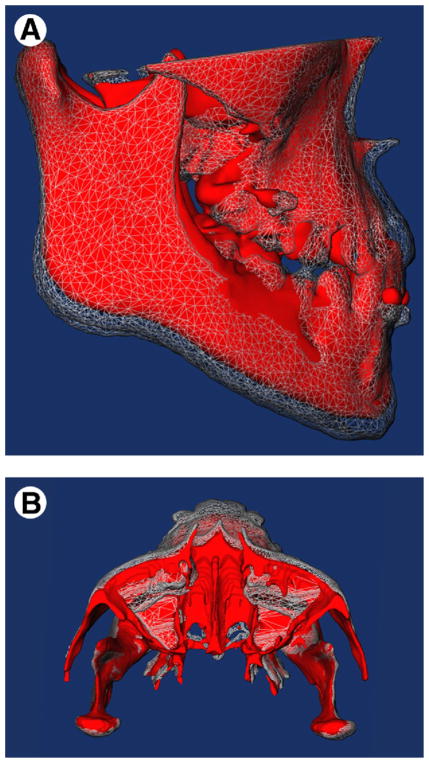
Figure 5 shows the cone-beam computed tomography scans from case 1 superimposed on the anterior cranial base. The post-treatment scan is a semitransparent overlay.9 The maxilla and the infraorbital border moved forward, whereas the horizontal growth of the mandible was restricted.
FIGURE 5.
A and B, Visualization of treatment changes as shown by 3-dimensional surface models from cone-beam computed tomography scans registered on anterior cranial base. Initial models are shown in red, and end-of-treatment models are shown as semitransparent mesh.
Discussion
For many decades, orthodontists have tried to modify facial growth by applying orthopedic forces to the teeth to be further transmitted to the skeletal base of the maxilla and mandible.2–4 However, dentoalveolar compensations rather than alterations of the facial growth were mostly responsible for the improvement seen in the dental arch relationships.4,7 To eliminate the dental side effects, titanium miniplates,10 shown to be well tolerated by patients,11 can now be used to apply the orthopedic forces. Liu et al12 reported sutural distraction osteogenesis to protract the midface in 4 young children using bone-borne traction hooks in combination with an extraoral face bow. The midface was pulled forward over a mean distance of 8 mm. Kircelli and Pektas13 reported a mean A-point advancement of 4.8 mm in 6 patients, using skeletal anchorage in conjunction with facemask therapy. Although those studies showed encouraging results, they still relied on facemask wear and, thus, patient compliance.
It is generally recommended that facemask therapy be started before the age of 8 years14,15 because the adaptability of the sutures and their response to anterior traction decrease with age.16,17 However, because miniplate placement surgery in young patients is complicated by the reduced height of the maxillary alveolar bone, and because the mandibular miniplates cannot be placed before canine eruption, orthopedic traction on miniplates usually cannot be started before the age of 10 years. Delaying the use of traction does have the advantage of keeping the post-orthopedic period of facial growth until adulthood shorter, reducing the risk for catch up of the skeletal Class III pattern. Forces of 100 g per side initially, and later, 200 g per side, were used, which are lower than the forces used for facemask therapy.2–4 There may be a more favorable maxillary growth response under moderate continuous traction rather than under heavy forces interrupted during the day. In our patients an important anterior displacement of the maxilla, associated with minimal mandibular growth, resulted in a clear reduction in facial concavity, which is in contrast to the worsening of the skeletal and dentoalveolar features expected for untreated Class III patients.1
Wearing maxillomandibular elastics is without doubt socially less constraining than wearing a face-mask. The cooperation needed from these 3 patients was limited to the replacement of the elastics once a day and the maintenance of good oral hygiene. By contrast, with facemask forces, these bone-borne forces could easily be maintained 24 hours per day. The direction of force application between the maxillary and mandibular miniplates was located below the center of resistance of the maxilla. Nevertheless, the resulting counterclockwise rotation of the palatal plane remained moderate (≤3.5°) (Table 1). Unlike with facemask therapy, the posterior rotation of the mandible was absent or very mild (2°) (Table 1). No dentoalveolar compensations were observed: whereas lower incisors tend upright with facemask therapy, they were protruded in these 3 cases (Table 1). This could be explained by increased tongue pressure on the lower incisors that was previously shielded by the upper incisors before correction of the anterior crossbite.
Improvement in facial esthetics before puberty has a positive impact on the psychosocial development of young children, whereas orthognathic surgery delayed until the end of growth requires the patient to accept his or her worsening facial disharmony until adulthood. Furthermore, surgical maxillary advancement often results in an unpleasing widening of the alar base,18–20 which was not observed in these 3 cases.
After this first series of Class III cases with orthopedic traction on miniplates, many questions remain unanswered, such as the ideal age and force for this type of orthopedic traction, the effect of the direction of force on the rotation of the palatal plane, or the possibilities of retention to prevent catch-up growth after treatment. A prospective clinical trial on a larger sample of patients has been started, to study the outcome of this type of orthopedic treatment of skeletal Class III cases; more research is needed to better understand the underlying biomechanics, the psychosocial benefits at an early age, and the possibility of decreased need for orthognathic surgery.
Pure bone-borne orthopedic forces applied with intermaxillary elastics on miniplates were shown to enhance midfacial growth in young maxillary-deficient patients.
References
- 1.Guyer EC, Ellis EE, III, McNamara JA, Jr, et al. Components of class III malocclusion in juveniles and adolescents. Angle Orthod. 1986;56:7. doi: 10.1043/0003-3219(1986)056<0007:COCIMI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Hata S, Itoh T, Nakagawa M, et al. Biomechanical effects of maxillary protraction on the craniofacial complex. Am J Orthod Dentofacial Orthop. 1987;91:305. doi: 10.1016/0889-5406(87)90171-5. [DOI] [PubMed] [Google Scholar]
- 3.Pangrazio-Kulbersh V, Berger J, Kersten G. Effects of protraction mechanics on the midface. Am J Orthod Dentofacial Orthop. 1998;114:484. doi: 10.1016/s0889-5406(98)70167-2. [DOI] [PubMed] [Google Scholar]
- 4.Chong YH, Ive JC, Artun J. Changes following the use of protraction headgear for early correction of class III malocclusion. Angle Orthod. 1996;66:351. doi: 10.1043/0003-3219(1996)066<0351:CFTUOP>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Westwood PV, McNamara JA, Jr, Baccetti T, et al. Long-term effects of class III treatment with rapid maxillary expansion and facemask therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2003;123:306. doi: 10.1067/mod.2003.44. [DOI] [PubMed] [Google Scholar]
- 6.Baik HS. Clinical results of the maxillary protraction in Korean children. Am J Orthod Dentofacial Orthop. 1995;108:583. doi: 10.1016/s0889-5406(95)70003-x. [DOI] [PubMed] [Google Scholar]
- 7.Kajiyama K, Murakami T, Suzuki A. Comparison of orthodontic and orthopedic effects of a modified maxillary protractor between deciduous and early mixed dentitions. Am J Orthod Dentofacial Orthop. 2004;126:23. doi: 10.1016/j.ajodo.2003.04.014. [DOI] [PubMed] [Google Scholar]
- 8.Cornelis MA, Scheffler NR, Mahy P, et al. Modified miniplates for temporary skeletal anchorage in orthodontics: Placement and removal surgeries. J Oral Maxillofac Surg. 2008;66:1439. doi: 10.1016/j.joms.2008.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cevidanes LH, Styner MA, Proffit WR. Image analysis and superimposition of 3-dimensional cone-beam computed tomography models. Am J Orthod Dentofacial Orthop. 2006;129:611. doi: 10.1016/j.ajodo.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Clerck H, Geerinckx V, Siciliano S. The zygoma anchorage system. J Clin Orthod. 2002;36:455. [PubMed] [Google Scholar]
- 11.Cornelis MA, Scheffler NR, Nyssen-Behets C, et al. Patients’ and orthodontists’ perceptions of miniplates used for temporary skeletal anchorage: A prospective study. Am J Orthod Dentofacial Orthop. 2008;133:18. doi: 10.1016/j.ajodo.2006.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu C, Hou M, Liang L, et al. Sutural distraction osteogenesis (SDO) versus osteotomy distraction osteogenesis (ODO) for midfacial advancement: A new technique and primary clinical report. J Craniofac Surg. 2005;16:537. doi: 10.1097/01.scs.0000159083.21931.c5. [DOI] [PubMed] [Google Scholar]
- 13.Kircelli BH, Pektas ZO. Midfacial protraction with skeletally anchored face mask therapy: A novel approach and preliminary results. Am J Orthod Dentofacial Orthop. 2008;133:440. doi: 10.1016/j.ajodo.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 14.Cha KS. Skeletal changes of maxillary protraction in patients exhibiting skeletal class III malocclusion: A comparison of three skeletal maturation groups. Angle Orthod. 2003;73:26. doi: 10.1043/0003-3219(2003)073<0026:SCOMPI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Merwin D, Ngan P, Hagg U, et al. Timing for effective application of anteriorly directed orthopedic force to the maxilla. Am J Orthod Dentofacial Orthop. 1997;112:292. doi: 10.1016/S0889-5406(97)70259-2. [DOI] [PubMed] [Google Scholar]
- 16.Persson M, Thilander B. Palatal suture closure in man from 15 to 35 years of age. Am J Orthod. 1977;72:42. doi: 10.1016/0002-9416(77)90123-3. [DOI] [PubMed] [Google Scholar]
- 17.Melsen B, Melsen F. The postnatal development of the palato-maxillary region studied on human autopsy material. Am J Orthod. 1982;82:329. doi: 10.1016/0002-9416(82)90467-5. [DOI] [PubMed] [Google Scholar]
- 18.Guymon M, Crosby DR, Wolford LM. The alar base cinch suture to control nasal width in maxillary osteotomies. Int J Adult Orthodon Orthognath Surg. 1988;3:89. [PubMed] [Google Scholar]
- 19.Rosen HM. Lip-nasal aesthetics following Le Fort I osteotomy. Plast Reconstr Surg. 1988;81:171. doi: 10.1097/00006534-198802000-00005. [DOI] [PubMed] [Google Scholar]
- 20.O’Ryan F, Schendel S. Nasal anatomy and maxillary surgery. II. Unfavorable nasolabial esthetics following the Le Fort I osteotomy. Int J Adult Orthodon Orthognath Surg. 1989;4:75. [PubMed] [Google Scholar]