Abstract
This study examines the long-term effects of child death on bereaved parents' health-related quality of life (HRQoL). Using data from the Wisconsin Longitudinal Study, we compared 233 bereaved couples and 229 comparison couples (mean age = 65.11 years) and examined the life course effects of child death on parents' HRQoL. Variations in bereavement effects were examined by gender and for different causes of death. Bereaved parents had significantly worse HRQoL than comparison group parents, and there was no evidence of gender differences for this effect. With respect to the cause of a child's death, bereaved parents whose child died in violent circumstances had particularly low levels of HRQoL. Multilevel models indicated that marital closeness mitigated the negative effects of bereavement.
Keywords: Couple data, Death, Health, Marital closeness, Multilevel models
Long-term Effects of Child Death on Parents' Health-Related Quality of Life: A Dyadic Analysis of Married Couples
The death of a child disrupts parents' health and well-being both during the acute phase of bereavement and for extended periods over the course of their lives. Studies have found that, compared to other parents, bereaved parents experience more emotional distress (Dyregrov, Nordanger, & Dyregrov, 2003; Lohan & Murphy, 2005-2006; Wijngaards-de Meij et al., 2005), more hostility (Moriarty, Carroll, & Cotroneo, 1996), more frequent psychiatric hospitalizations (Li, Laursen, Precht, Olsen, & Mortensen, 2005), a higher rate of certain types of cancers (Levav et al., 2000), and higher mortality (Li, Precht, Mortenson, & Olsen, 2003) than non-bereaved parents. Some studies have found that bereavement also causes considerable stress on the parents' marital relationship and has been associated with high rates of divorce (Lehman, Wortman, & Williams, 1987; Najman et al., 1993). However, other evidence suggests that marital disruption might be no more likely for these couples than for other parents (Murphy, Johnson, Wu, Fan, & Lohan, 2003; Oliver, 1999). Also, some parents have reported that experiencing grief together as a couple strengthened their marital bond (Schwab, 1998).
To date, there has been relatively little research on parental bereavement that specifically examines the role of marital quality in recovery from grief. Furthermore, most research that has examined marital quality focuses on the occurrence of divorce, examines impacts over a relatively short period of time, and neglects the potential role of marital support in coping with bereavement. The purpose of the present investigation was to examine the long-term adaptation of couples who experienced the death of a child and to examine marital quality as a source of support in coping with bereavement.
This investigation builds upon an earlier report (Rogers, Floyd, Seltzer, Greenberg, & Hong, 2008) in which we investigated the long term outcomes of parental bereavement for men and women who participated in the third wave (1992/94) of the Wisconsin Longitudinal Study (WLS; Hauser & Roan, 2006). The investigation was unusual in examining bereavement in an unselected sample of fathers and mothers who participated in a population-based study of adult development from high school to old age. Thus, the self-selection bias that occurs in many bereavement studies that recruit participants from clinical settings was avoided. The Rogers et al. investigation also evaluated long-term outcomes by examining functioning when the parents were in their early 50's, an average of 18 years after the child's death. The findings uncovered evidence of “lasting grief” for these parents who, in midlife, were more likely to have experienced a depressive episode, had lower levels of psychological well-being, more health problems, and a greater likelihood of divorce than a control group who were matched for background characteristics. However, marital quality was not measured at the 1992/94 wave of the WLS, and data were obtained only from one member of each married couple. The present investigation follows the same cohort 12 years later (2004/06), when data from both husbands and wives were available, and focuses on the sub-sample who maintained intact marriages. Thus, instead of focusing on divorce as an outcome, this analysis examines marital closeness as a potential source of support in later life.
The stress of bereavement on couples' relationships can be conceptualized as emanating from differences between mothers and fathers in their parenting experiences and the impacts of these experiences on their well being (e.g., McBride, Schoppe, & Rane, 2002), as well as gender differences in both socialization and social norms regarding the expression of emotions in grief (e.g., Murphy et al., 1998). As compared to mothers, fathers generally are less accessible and have less direct contact with children, and they assume less responsibility for managing the children's home and social environment (Parke, Dennis, Flyr, Morris, Leidy, & Schofield, 2005). Thus, because of greater role loss for mothers, the death of a child would be expected to have more negative effects on mothers than on fathers. Accordingly, studies have shown that bereaved mothers, as compared to fathers, experience more depression (Wijngaards-de Meij et al., 2005), greater global distress (Lohan & Murphy, 2005-2006; Moriarty et al., 1996), higher levels of grief (Sidmore, 1999-2000), more PTSD (Murphy et al., 2003), greater increase in mortality (Li et al., 2003), and have a greater odds of psychiatric hospitalization following the death of a child (Li et al., 2005). Women and men might also express grief and cope with bereavement differently, with men more likely than women to suppress negative emotions and withdraw as a means of coping (Cook, 1984). These coping differences, or discordant grief more generally, might be seen as unsupportive by spouses, leading to distress for the individuals and stress in the marital relationship (Buchi et al., 2009; Moriarty et al.).
However, research findings have not consistently identified gender differences specific to bereavement reactions. Notably, in midlife, the bereaved parents in the Rogers et al. (2008) investigation showed gender differences on a variety of measures of functioning, including higher odds of having depressive episode for women. However, this gender difference also occurred in the comparison sample of non-bereaved parents, and thus there were no unique impacts of bereavement for men and women (Rogers et al.). So, gender differences reported in earlier bereavement studies might reflect male-female differences in psychological functioning that are independent of bereavement. Alternatively, gender differences might occur in immediate or short term grief responses but could be less apparent in the long term adjustment as measured in midlife. By focusing on intact couples, and by including a comparison group of couples who did not experience child death, in the current investigation we were able to examine mothers and fathers who experienced the same loss at the same point in time. Thus, this study can provide a clearer picture of potential gender differences in bereavement than was possible in past research.
Perceived emotional support has been found to both directly and indirectly protect mental and physical health from the effects of stressful life events (Thoits, 1995). Shapiro (2001) suggested that family relationships can buffer the negative effects of bereavement. However, research on the effects of family relationships on bereavement has been inconclusive. For example, among bereaved parents, perceived effectiveness of emotional support was reported to be associated with a decrease of PTSD over time (Murphy et al., 2003) as well as an increase in self-esteem and lower levels of depression (Sherkat & Reed, 1992), but perceived effectiveness of emotional support was not associated with levels of mental distress (Murphy, Chung, & Johnson, 2002). In a longitudinal study of widowhood (Stroebe, Zech, Stroebe, & Abakoumkin, 2005), emotional support from family and friends was associated with lower levels of depression in general, but did not necessarily buffer stress or facilitate recovery associated with bereavement.
However, marital support may play a more significant role in parental bereavement than other forms of family support. For example, a recent longitudinal follow-up of couples who experienced infant death found that the ability of spouses to share emotions and experience grief in a concordant way predicted greater post-traumatic growth (Buchi et al., 2009). Given that most marriages remain intact after the death of a child (Schwab, 1998), the ability to maintain marital closeness over time might be a key to well-being for most parents.
The impact of bereavement on marital and individual functioning might differ depending on the circumstances surrounding the child's death. In particular, violent deaths have been found to more negatively affect bereaved parents' health outcomes than other causes of death. For example, Keesee, Currier, and Meineyer (2008) found that bereaved parents whose children died as a result of violent deaths (i.e., accident, suicide, and homicide) experienced more grief than parents whose children died as a result of illnesses, medical causes, or during infancy (i.e., cancer, heart attack, and miscarriage or stillbirth). In a national sample of bereaved parents in Norway, Dyregrov et al. (2003) found that bereaved parents whose children died as a result of suicide or accidents indicated greater subjective distress than parents whose children died of Sudden Infant Death Syndrome (SIDS).Wijngaards-de Meij et al. (2005) followed bereaved parents up to 20 months after the child's death and found that parents whose children died by traumatic death (accidents and suicide) reported the most complicated grief, parents whose children died as a result of illness experienced less intense grief, and bereaved parents whose children died in infancy had the lowest degree of grief.
Other family circumstances also need to be taken into consideration. Socioeconomic status likely affects both the cause of death (due to differential exposure to risk) and grief responses (due to differential access to counseling and health resources after the death). The presence of other children in the family can provide bereaved parents with a continued sense of purpose in life and function as a protective factor for the harmful effects of bereavement (e.g., Wijngaards-de Meij et al., 2005). Importantly, in the Rogers et al. (2008) study, having other living children in the household at the time of the death predicted less marital disruption for the bereaved parents.
The present investigation was guided by the integrative risk factor framework, which emphasizes the importance of a systematic examination of the associations of stressors, intra/interpersonal risk/protective factors, and appraisal and coping processes, in order to enhance the scholarly understanding of individual variations in adjustment to bereavement (Stroebe, Folkman, Hansson, & Schut, 2006). Proponents of the framework posit that the nature of the stressor (i.e., bereavement, cause of death) influences health and well-being outcomes in part through moderating factors such as inter/intra-personal risk/protective factors that can either mitigate or exacerbate the effects of stress. Based on the assumptions of the integrative risk factor framework, this study hypothesized that the circumstances of bereavement (i.e., the cause of child's death) would influence bereaved couples' health outcomes with moderations by interpersonal (i.e., marital closeness) and individual factors (i.e., gender, level of education).
Specifically, in this study, the dependent variable was health-related quality of life (HRQoL) of couples as measured by the Health Utilities Index Mark 3 (HUI-3). This measure assesses multiple dimensions of mental and physical health (e.g., emotion, cognition, pain). HRQoL has been widely used to evaluate population health quality as well as outcomes of clinical interventions (Feeny et al., 2002; Fryback et al., 2007; Kaplan et al., 2008; Robert et al., 2009; Tempier & Pawliuk, 2007). Multilevel models were estimated to test the effects of both shared and individual factors within a couple on the health outcomes of bereaved parents over time. In addition, the study included a matched comparison group consisting of parent couples who did not experience the death of a child in order to identify bereavement-specific predictors of health outcomes.
We investigated the following hypotheses:
Parents who experienced the death of a child would have worse HRQoL compared to parents who did not experience the death of a child.
Bereaved mothers would have worse HRQoL than bereaved fathers, but this gender effect would not be in the comparison group.
Bereaved parents who indicated greater marital closeness would report a better HRQoL than bereaved parents who reported less marital closeness.
HRQoL of bereaved parents would vary based on the cause of the child's death. Bereaved parents whose child died from violent causes would report even worse HRQoL than other bereaved parents.
Method
Data and Sample
The Wisconsin Longitudinal Study (WLS) is a long-term study of a random sample of 10,317 women and men who graduated from Wisconsin high schools in 1957 and 8,778 of their siblings (Hauser & Roan, 2006). The high school graduates were surveyed in 1957, 1975, 1992, 2004, and their randomly selected siblings were surveyed in 1977, 1994, and 2006. Most of the respondents were White, reflective of Wisconsin's population in the mid-20th century. The most recent point of data collection is referred to in this paper as the 2004/2006 survey, encompassing both the original sample and their siblings, who averaged approximately 65 years of age at that time. In the present study, the original sample members and their siblings are treated as one group of respondents from which the bereaved sample and the comparison group were selected.
The present analysis focuses on respondents who were married at the time of the 2004/2006 survey, and capitalizes on the availability of data from a separate abbreviated interview conducted with respondents' spouses following the 2004/2006 survey. The present study, therefore, is limited to the measures that were common to the interviews with both spouses.
The analytic sample for this study included two groups. One group consisted of couples who experienced the death of a child, while the other group consisted of couples whose children were all alive at the time of the 2004/2006 survey. A total of 932 WLS respondents experienced the death of a child before the 2004/2006 survey, of whom 706 (75.8%) were married at the time of survey. Of the 706 spouses, 452 wives or husbands (64.0%) completed the phone interview. The other spouses (36.0%) declined to participate in the interview or had substantial missing data. The main respondents whose spouses completed the phone interview were younger, more educated, and reported better HRQoL than their counterparts whose spouses did not complete the interview. There were no significant differences between the two groups in terms of household income, number of children, years since the child's death, parents' ages at child death, marital closeness, and history of depressive episodes. Further, 151 out of 452 were eliminated from the final analytic sample for this study for a variety of reasons: the deceased child was not the biological child of both parents (n = 115), the couple had more than one child who had died (n = 27), the child's cause of death was not known (n = 4), and both the WLS main respondent and his/her sibling experienced the death of their own child (n = 5); excluding one couple per sibling pair prevented the problem of non-independence in the data consisting of both WLS main respondents and their siblings. This resulted in a sample of 301 brereaved couples who met study criteria.
We selected a comparison group based on the following criteria: (a) the respondent was married at the time of the 2004/2006 survey and his or her spouse also participated in the survey, (b) the couple had at least one biological child from the current marriage, and (c) the couple did not have any deceased children or children with a developmental disability or mental health condition. Fully 2,139 WLS couples met these criteria.
We then used stratified random sampling to select a matched comparison group from these 2,139 couples. Gender, age, and education were used as stratification variables. We used the distributions of the bereaved group on these variables to identify strata, then we randomly selected, from within each stratum of the comparison pool, the same proportion of comparison group couples as bereaved parents in that stratum. In this way, the comparison group had equal representation with the target bereaved parents group across all strata. As a result, 301 couples constituted the comparison group pool.
The two samples were further reduced in size due to missing data. Specifically, in the bereaved sample, 65 couples were excluded because of missing data regarding whether the parent ever experienced a depressive episode; these data were missing because the depression module in WLS was administered to only an 80% random sample of the all respondents. Three couples were excluded from the bereaved sample due to missing data on marital closeness. Thus, the final bereaved sample consisted of 233 married couples for whom complete data were available and who had one deceased child with a known cause of death.
Similarly, 70 couples in the comparison group were excluded due to the 80% sampling of the depression module in WLS survey. Two other couples were excluded from the comparison group because of missing data on marital closeness. Thus, the final comparison sample consisted of 229 married couples. There were no significant differences between the bereaved and comparison couples with respect to parental age, education, household income, or number of living children.
Dependent Variable
Health Related Quality of Life (HRQoL) was measured by the Health Utilities Index Mark 3 (HUI-3). This is a multidimensional self-report measure of overall health status (Boyle, Furlong, Feeny, Torrance, & Hatcher, 1995; Feeny et al., 2002; Horsman, Furlong, Feeny, & Torrance, 2003). The measure evaluates eight attributes: vision, hearing, speech, ambulation, dexterity, emotion, cognition, and pain (Horsman et al.). Each attribute is assessed by five or six levels of health status or functionality. For example, vision is evaluated from level 1, “able to see well enough to read ordinary newsprint and recognize a friend on the other side of the street” to level 6, “unable to see at all.” Emotion is assessed from level 1, “happy and interested in life” to level 5, “so unhappy that life is not worthwhile”. Corresponding weights are assigned to each level of each attribute by a standardized scoring system, resulting in a multi-attribute summary HUI-3 score (see Feeny et al.), ranging from 0 to 1 where “0” means poorest health status and “1” means perfect health. Specifically, weights for each of the eight attributes in the HUI-3 scoring system were determined by surveying representative sample's ratings for selected sets of unique health states and then estimating the mean ratings of the respondents via econometric approaches. Once the weights were assessed, a scoring function reflecting the population valuation of the health states was created (Feeny et al., Roberts et al., 2009). The test-retest reliability and predictive as well as construct validity of the HUI-3 have been supported in many studies (Boyle et al., 1995; Feeny et al.; Feeny, Huguet, McFarland, & Kaplan, 2009; Maddigan, Feeny, Majumdar, Farris, & Johnson, 2006).
Independent variables
Parent bereavement status was coded as a dichotomous variable (1 = bereaved; 0 = comparison).
Cause of child death
We used parents' report as the primary source to identify the cause of child death. If the parents' report on the cause of death was missing or unclear, the information from National Death Index (NDI) was used. If both sources of information were not available (N = 4), the case was dropped from this analysis, as noted above. Each child's death was categorized into one of three causes: infant death, illness, or violent death. In a prior analysis, we examined the concordance between parent report and the NDI, and found high levels of agreement (78% exact matches, Rogers et al., 2008).
All deaths that occurred before the child reached his or her first birthday were categorized as infant deaths (N = 57). The infant death category included deaths due to infant respiratory distress syndrome, RH incompatibility, labor and delivery complications, SIDS, and congenital symptoms and malformations (including birth defects), and included other illness or accidents that occurred before the child's first birthday. Deaths that occurred after the child was one year of age were categorized as either due to violence (N = 86) or illness (N = 90). The violent death category included suicide, homicide, motor vehicle accidents, poisoning, drowning, fire, accidental gunshot wounds, and falls. The illness category included acute and chronic illnesses such as cancer, pneumonia, and heart attack.
Within the sample of bereaved couples, there were some significant differences related to the cause of the child's death. Understandably, the three groups differed with respect to parents' age at the time of the child death (F (df = 2, n = 233) = 104.10, p < .001 for mothers, (F (df = 2, n = 233) = 105.75, p < .001 for fathers), with parents whose child died in infancy the youngest at the time of the child's death. Accordingly, the duration of time since their child's death was longest in the infant death category (38.4 years) (F (df = 2, n = 233) = 118.86, p < .001). In addition, the number of living children was different among the three cause of death groups (F (df = 2, n = 233) = 4.70, p < .05), with parents whose child died in infancy having had more children who were living at the time of the 2004/06 follow-up. There were no differences, however, in child age, time since the death, or number of living children for the illness and violent death groups.
Marital closeness was evaluated with a single-item rating of how close the respondent currently feels to his or her spouse (1 = not at all close, 2 = not very close, 3 = somewhat close, 4 = very close). Past research has shown that the single-item marital closeness measure is a predictor of health and well-being outcomes such as life satisfaction, positive affect, negative affect, and happiness (Sandhya, 2009; Winsor, Ryan, & Smith, 2009).
Control variables
Several variables that have been reported to be associated with the health of older adults also were included as controls. Higher income has been consistently linked to better health outcomes (e.g., Marmot & Wilkinson, 2005). In this study, household income was log transformed to correct for skewness in these data. In the general population, a larger number of children in a family is associated with negative effects on parents' health and well-being (e.g., Weng, Bastian, Taylor, Moser, & Ostbye, 2004). Therefore, in this study we controlled for number of living children. Since older age and lower levels of education are associated with poorer health (Marmot & Wilkinson), current age and years of education were also controlled in all analyses. Also, to control for the possibility that HRQoL was affected by depression, a variable was included in the analysis reflecting whether the respondent ever had a time in life lasting two weeks or more when nearly every day he or she felt sad, blue, depressed, or lost interest in work, hobbies, or things he or she liked to do for fun (1 = yes; 0 = no).
Data Analysis
To account for the shared bereavement experience among couples, multilevel models were estimated using Hierarchical Linear Modeling (HLM; Raudenbush & Bryk, 2002), which has several advantages for the present study. HLM partitions the variance into multiple levels and thereby makes it possible to evaluate variation attributable to individuals and couples separately. Thus, HLM fits the purpose of this study by managing the dependency in spouses' data while allowing us to compare and contrast predictive associations for women and men. In addition, HLM allows us to examine hypotheses about cross-level effects including interactions between individual-level (i.e., gender, marital closeness) and couple-level (i.e., bereavement status, cause of child death) variables.
We first estimated multilevel models to examine the differences in HRQoL of the bereaved parents in contrast to the comparison parents, controlling for demographic variables at both the individual (gender, age, education) and couple (household income, number of living children) levels. After estimating the main effect of bereavement status in Model 1, we entered in Model 2 variables assessing whether the respondent had ever experienced a depressive episode and current marital closeness. In Model 3, Bereavement status × Parent gender and Bereavement status × Marital closeness interactions were added to the model. These interactions, respectively, evaluated whether bereaved mothers and fathers differed in HRQoL relative to comparison group mothers and fathers, and whether greater marital closeness reduced the negative effects of bereavement. We took these steps in order to first examine the main effect of child's death on parents' HRQoL (including only demographic control variables), then to add both marital closeness and the control variable for previous depression to observe their effects in the second step of the analysis, and finally, in the last step of analysis, to examine differences in the effects of child's death on individuals' HRQoL contingent on parents' gender and marital closeness. Next, we repeated the analyses to examine whether the effects differed depending on the cause of the child's death. We did so by replacing bereavement status with a set of coded vectors indicating the three specific cause of death categories, which contrasted each cause of death with the comparison group parents who had not experienced a child death. The comparison group couples constituted the omitted category in the set of dummy coded vectors for the groups.
Results
Table 1 presents descriptive statistics for the bereaved and comparison samples, as well as for each cause of death subsample. Although there were no significant group differences on demographic characteristics, as described earlier, the bereaved mothers reported a significantly greater likelihood of having experienced a depressive episode than comparison mothers (χ2 (df = 1, n = 462) = 20.38, p < .001). Fully 40% of bereaved mothers reported having experienced a depressive episode at some point in their life, as compared with 21% of comparison group mothers. There was no significant difference in the likelihood of experiencing a depressive episode between bereaved fathers and comparison group fathers. Among bereaved mothers, significantly fewer mothers whose child died in infancy reported ever having experienced a depressive episode (22%) than bereaved mothers who lost child due to illness (43%) or violent death (49%; χ2 (df = 2, n = 233) = 10.20, p < .01). Additionally, given the wide range of child age at death, we examined the potential significance of the child age at death. However, this factor was not significantly correlated with the HRQoL of the bereaved parents (r = -.039, ns).
Table 1. Descriptive Statistics for Bereaved and Comparison Parents.
| Bereaved | Comparison | |||||
|---|---|---|---|---|---|---|
| Infant Death | Illness | Violent death | Total Bereaved | |||
| Couple level | ||||||
| Number of couples | 57 | 90 | 86 | 233 | 229 | |
| Household income | 75722 (120538) | 62831 (51606) | 64253 (66235) | 66510 (78512) | 58909 (64912) | |
| N of living children | 3.3 (1.8) | 2.5 (1.2) | 2.8 (1.6) | 2.8 (1.5) | 2.9 (1.3) | |
| Years since death | 38.4 (5.4) | 15.6 (12.6) | 15.4 (8.4) | 21.1 (13.8) | --- | |
| Individual level | ||||||
| Number of parents | 114 | 180 | 172 | 466 | 458 | |
| Parent Current age | M | 64.0 (2.9) | 64.1 (4.6) | 64.1 (3.4) | 64.1 (3.8) | 63.4 (4.3) |
| F | 66.5 (3.9) | 67.0 (5.5) | 66.2 (3.6) | 66.6 (4.5) | 66.3 (4.8) | |
| Parent education | M | 13.3 (1.8) | 13.2 (2.2) | 12.3 (1.9) | 13.2 (2.0) | 13.3 (1.9) |
| F | 13.8 (2.8) | 13.8 (3.0) | 13.4 (2.3) | 13.7 (2.7) | 13.8 (2.7) | |
| Parent age at child death | M | 25.7 (4.5) | 48.6 (14.0) | 48.7 (8.9) | 43.0 (14.4) | --- |
| F | 28.1 (5.6) | 51.5 (13.4) | 50.8 (9.2) | 45.6 (14.4) | ||
| Marital closeness | M | 3.82 (.38) | 3.84 (.36) | 3.76 (.46) | 3.81 (.41) | 3.82 (.46) |
| F | 3.86 (.35) | 3.82 (.38) | 3.81 (.39) | 3.83 (.38) | 3.82 (.46) | |
| Depressive episode | M | 22.8% | 43.3% | 48.8% | 40.3% | 21.0% |
| F | 19.3% | 18.9% | 32.6% | 24.0% | 16.6% | |
| Health related quality of life | M | .79 (.22) | .82 (.22) | .79 (.21) | .80 (.22) | .84 (.19) |
| F | .78 (.25) | .82 (.20) | .75 (.25) | .78 (.23) | .82 (.20) | |
Note. Means are presented with SD in parentheses. M = Mothers, F = Fathers.
HRQoL Group Differences and Protective Effects of Marital Closeness
Table 2 presents the results of multilevel models examining the effects of child death on the parents' HRQoL. A significant effect of bereavement status in Model 1 shows that, with demographic factors controlled, bereaved parents had significantly worse HRQoL than comparison group parents, providing support for Hypothesis 1. In Model 2, both marital closeness and having experienced a depressive episode were significant predictors of HRQoL; marital closeness was a positive predictor, while having experienced a depressive episode predicted a poorer HRQoL. Nevertheless, it is notable that, with these variables added to the model, bereavement status still significantly predicted poorer HRQoL, again supportive of Hypothesis 1.
Table 2. Estimates from Multilevel Models of Predicting Health-related Quality of Life (HRQoL) of Bereaved Parents vs. Comparison Parents.
(N = 462 Couples; 233 Bereaved Couples + 229 Comparison Couples)
| HRQoL | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||
| b | SE | b | SE | b | SE | |
| Intercept | 0.82*** | 0.01 | 0.83*** | 0.01 | 0.83*** | 0.01 |
| Couple level variables | ||||||
| Household income (Logged) | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Number of living children | -0.01 | 0.01 | -0.01 | 0.01 | -0.01 | 0.01 |
| Bereavement status a | -0.04** | 0.02 | -0.03* | 0.02 | -0.04 | 0.02 |
| Individual level variables | ||||||
| Gender b | 0.03* | 0.02 | 0.04* | 0.02 | 0.04 | 0.02 |
| Age | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Education (Years) | 0.01 | 0.01 | 0.01* | 0.01 | 0.01* | 0.01 |
| Ever depressed c | -0.06*** | 0.02 | -0.06*** | 0.02 | ||
| Marital closeness | 0.06* | 0.03 | -0.00 | 0.03 | ||
| Cross level interactions | ||||||
| Bereavement × Parent gender | 0.01 | 0.02 | ||||
| Bereavement × Marital closeness | 0.13* | 0.05 | ||||
| Between-couple intercept(level 2) | .01 (d.f. = 458) | .01 (d.f. = 458) | .01 (d.f. = 458) | |||
| χ2 = 677.81*** | χ2 = 668.23*** | χ2 = 675.25*** | ||||
| Within-couple (level 1) | 0.04 | 0.03 | 0.19 | |||
Note. Bereavement status: 0 = No, 1 = Yes.
Gender: 0 = Fathers, 1 = Mothers.
Ever depressed: 0 = No, 1 = Yes;
p < .05.
p < .01.
p < .001. (two-tailed)
Regarding Hypothesis 2, which predicted gender differences within the bereaved sample alone, Model 1 revealed a significant main effect of parent gender, with mothers having a better HRQoL than fathers. However, in Model 3, the non-significant Bereavement × Parent gender interaction indicated that the mother-father discrepancy was not significantly different among bereaved parents and the comparison parents. This pattern was not consistent with Hypothesis 2, and instead indicated that the gender-related health differences were consistent across the groups.
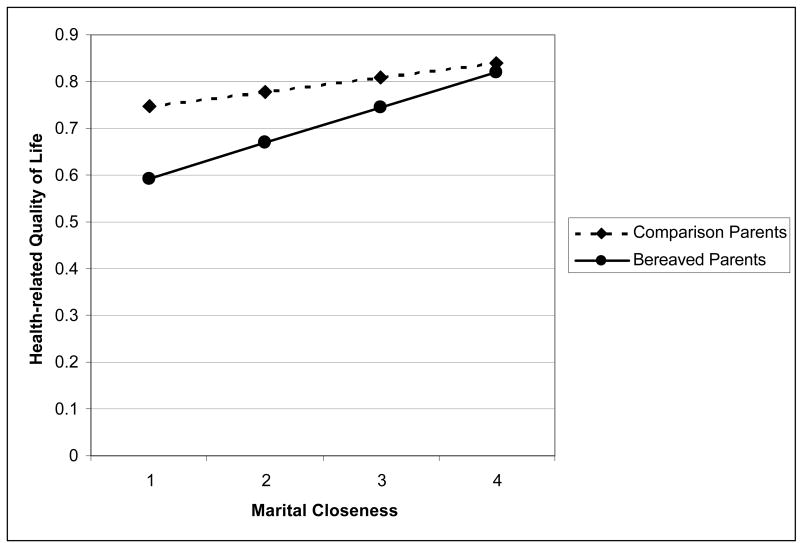
Regarding Hypothesis 3, the results for Model 3 did reveal a significant Bereavement × Marital closeness interaction effect, as expected. Figure 1 illustrates that bereaved parents who indicated greater marital closeness reported a better HRQoL score compared to bereaved parents who had lower levels of marital closeness, supportive of Hypothesis 3. In contrast, HRQoL did not vary according to marital closeness among comparison group parents.
Figure 1.
Parents' Marital Closeness predicting Health-related Quality of Life: Bereaved Parents vs. Comparison parents
Effects of Cause of Child Death
Table 3 presents the results of multilevel models examining the effects of the three causes of death (i.e., infant death, illness, violent death) on parents' HRQoL. Specifically, this analysis compared each cause of death category with the comparison group with respect to HRQoL.
Table 3. Estimates from Multilevel Models Predicting Health-related Quality of Life (HRQoL) for Variations in Bereaved Parents due to Multiple Causes of Child Death and Comparison Parents.
(N = 462 Couples; 233 Bereaved Couples + 229 Comparison Couples)
| HRQoL | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||
| b | SE | b | SE | b | SE | |
| Intercept | 0.82*** | 0.01 | 0.83*** | 0.01 | 0.83*** | 0.01 |
| Couple level variables | ||||||
| Household income (Logged) | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Number of living children | -0.01 | 0.01 | -0.01 | 0.01 | -0.01 | 0.01 |
| Bereaved: Infant death | -0.04 | 0.02 | -0.04 | 0.02 | -0.04 | 0.02 |
| Bereaved: Illness | -0.02 | 0.02 | -0.01 | 0.02 | -0.01 | 0.02 |
| Bereaved: Violent death | -0.07** | 0.02 | -0.05* | 0.02 | -0.05* | 0.02 |
| Comparison (omitted) | --- | --- | --- | |||
| Individual level variables | ||||||
| Gender a | 0.03* | 0.02 | 0.04* | 0.02 | 0.04** | 0.02 |
| Age | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Education (Years) | 0.01 | 0.01 | 0.01* | 0.01 | 0.01* | 0.01 |
| Ever depressed b | --- | -0.06** | 0.02 | -0.06*** | 0.02 | |
| Marital closeness | --- | 0.05* | 0.02 | -0.00 | 0.03 | |
| Cross-level interactions | ||||||
| Marital closeness × Infant death | 0.31** | 0.10 | ||||
| Marital closeness × Death due to illness | 0.10 | 0.06 | ||||
| Marital closeness × Violent death | 0.06 | 0.07 | ||||
| Between-couple intercept (level 2) | .01 (d.f. = 456) | .01 (d.f. = 456) | .01 (d.f. = 456) | |||
| χ2 = 673.07*** | χ2 = 664.86*** | χ2 = 679.66*** | ||||
| Within-couple (level 1) | 0.04 | 0.19 | 0.03 | |||
Note. Gender: 0 = Fathers, 1 = Mothers.
Ever depressed: 0 = No, 1 = Yes.
p < .05.
p < .01.
p < .001. (two-tailed)
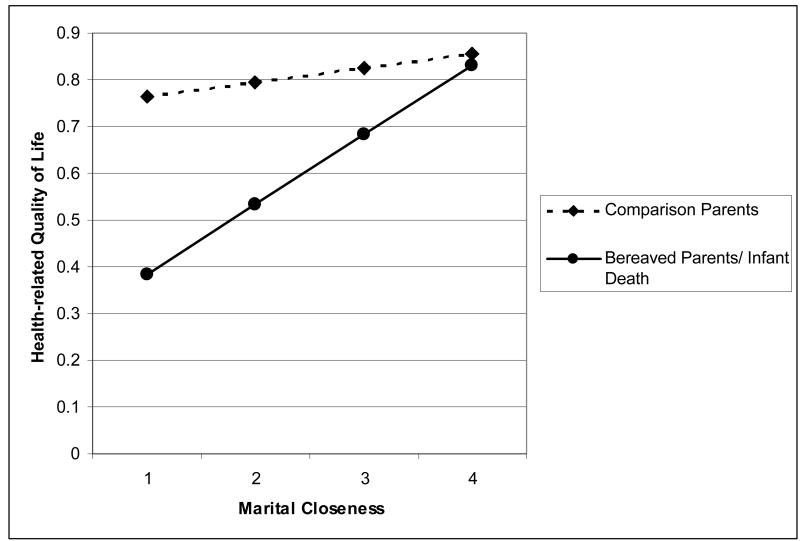
Model 1 shows that, after controlling for demographic factors, parents who lost children by violent death had significantly worse HRQoL than comparison group parents. Also, consistent with Hypothesis 4, this was the only cause of death group to differ significantly from the comparison group. Also, in Model 2, violent death remained a significant predictor of poorer HRQoL, even after controlling for the two significant effects of marital closeness and having experienced a depressive episode. However, in Model 3, the interaction of violent death with marital closeness was not significant. Thus, in contrast to the hypothesis, marital closeness did not moderate the negative effects of violent child death on the parents' HRQoL for this subgroup. Nevertheless, there was a significant interaction of marital closeness and infant death on parents' HRQoL. Figure 2 illustrates that parents who experienced an infant death reported better HRQoL when they also reported high levels of marital closeness, but experienced sharply lower HRQoL when they reported lower levels of marital closeness. In contrast, for the comparison group, the gradient in HRQoL scores was less dependent on marital closeness.
Figure 2.
Parents' Marital Closeness predicting Health-related Quality of Life: Bereaved Parents who lost a child through Infant Death vs. Comparison parents
Discussion
The present results extend previous findings about the effects of bereavement on parents by examining how the death of a child earlier during the life course relates to well-being for bereaved parents as they approach old age. Consistent with hypotheses, older bereaved couples had significantly poorer HRQoL than comparison couples when they were in their 60s, even though their experience of child death occurred, on average, two decades earlier. The age of the child or the amount of time since the child's death did not significantly predict health outcomes. With respect to the cause of a child's death, bereaved parents whose child died in violent circumstances had particularly low levels of HRQoL. This result is in agreement with previous studies examining the detrimental effects of child's death due to violent causes (Dyregrov et al., 2003; Keesee et al., 2008; Rachuba, Stanton & Howard, 1995; Wijngaards-de Meij et al., 2005). Also, there is evidence that having an opportunity to say good-bye before the death of a loved one is related to better adaptation after bereavement, compared to not having this opportunity (Wijngaards-de Meij et al., 2008), and possibly better health outcomes in later life.
Our findings also support the critical role of marital closeness as a source of support for spouses. As expected, marital closeness was a significant predictor of better health for bereaved couples. This effect is consistent with studies that have shown that social support after a death is associated with lower levels of depression among bereaved people (Norris & Murrell, 1990; Shapiro, 2001). Further analysis into variations due to the cause of a child's death revealed that the marital closeness effect was in evidence among those who experienced infant death, but not among those whose child died from illness or violence. It might be that the death of a child in infancy activates effective coping as a couple because, at this early stage of the family life cycle, the ability of couples to set a new course together as a family unit may be critical to long term adjustment. Indeed, either having additional children to replace the loss (Najman et al., 1993), or having other children to care for (Rogers et al., 2008), may place emphasis on marital and family roles at this stage. However, violent deaths and deaths due to illnesses tended to occur later, when parents were no longer in the early stage of active parenting and, thus, marital quality may be less relevant to working through bereavement. Furthermore, the shock and disruption that occurs when a child dies from violent circumstances might disrupt marital closeness as well, thus making it even less available as a coping resource for grieving parents.
It is noteworthy that there were similar gender differences in bereaved couples' HRQoL as in the comparison group. Although some previous studies have reported that a child's death was more detrimental to mothers' health than to fathers' health (e.g., Li et al., 2003), the results from the current dyadic data did not provide evidence of gender differences in long-term impacts of child death on bereaved couples. Since the current sample came from the same pool as our earlier investigation, the lack of gender differences in bereavement reactions in both studies might reflect circumstances that characterize the sample for this particular longitudinal study; notably the focus on midlife and later-life functioning, and the relatively long duration since the death (and, thus, extended time for recovery). Clearly, there is a need for more prospective longitudinal research to better understand how the recovery process unfolds for men and women, and how initial or early gender differences in bereavement might diminish over time.
Some limitations of this study must be noted. The WLS sample consists of mostly non-Hispanic, Whites who obtained at least a high school education. Thus, although it was representative of the American population in the mid-20th century, it does not represent the current U.S. population. Additionally, although the WLS is a longitudinal study of over 40 years, the present analysis used a cross-sectional approach because spouse data were available only for the most recent wave of the survey (2004/2006). Thus, some inevitable problems for interpreting causality remain. For example, the direction of effects in the association between marital closeness and HRQoL can be interpreted in two ways, i.e., that marital closeness leads to better HRQoL, or that those with better HRQoL have a closer marriage at this stage of life. However, this reversed causal direction would not explain why the effects differed for the bereaved and non-bereaved spouses. Nevertheless, more precise causal modeling with predictors and criteria measured together across time might help to better address the question of causal direction.
The mechanism by which marital closeness moderates the effect of bereavement with respect to health in older couples also warrants additional research. Because in the present study, marital closeness was measured when these parents were in their 60s and the child death occurred up to decades earlier, it cannot be concluded from these data that marital closeness had a buffering effect. Rather, spousal support may have a concurrent moderating effect on HRQoL during the early years of old age. In a longitudinal study examining the effects of social support on widows' adjustment, Stroebe et al. (2005) showed that better functioning depended on the support being currently active, but that support prior to the death alone did not prevent increases in depression following the event. Sustaining social support during the long post-bereavement period may be critical in order to mitigate stress after the loss of a child. Since a spouse is the most constantly accessible source of support for bereaved couples, ongoing spousal support may be critical to adjustment and health long after the loss of a child. That is, instead of buffering against the occurrence of negative reactions in a preventive way, the present findings are consistent with a process in which marital closeness is a key to recovery from grief and, possibly, the retention of gains over time. In future research, we need to investigate the mechanisms by which couples can maintain or develop marital closeness and prevent relationship breakdown in the aftermath of this stressful family event.
Implications for Practice
It is noteworthy the bereaved parents are not a homogeneous group. Depending on their resources and characteristics, as well as on the circumstances of the death, some bereaved parents might be at higher risk than others. Previous research (Schut, Stroebe, van den Bout, & Teheggen, 2001) found that intervention programs targeting specific vulnerable groups (e.g., those who experienced traumatic loss) were beneficial, whereas interventions targeting bereaved persons in general were less helpful. Murphy and colleagues (1998) also found that bereaved mothers who were more distressed at the beginning of the intervention benefited more from the intervention program, compared to less distressed bereaved mothers, suggesting the importance of identifying various risk levels of bereaved parents. The present study adds to the list of risk factors the presence of limited marital closeness. Assessments of individual and family functioning following the death of a child should attend to the quality of the parents' marriage as an important coping resource. Interventions designed to specifically address marital problems with the goal of improving marital closeness might be in order for at least some couples. Previous studies of interventions for bereaved mothers showed that emotional support from professionals alleviated bereaved mothers' psychological symptoms, but that the positive effects of the intervention lasted only half a year (Forrest, Standish, & Baum, 1982). Thus, services or programs that emphasize emotional support from a spouse in post-loss adjustment might be helpful to help couples sustain positive adjustment over the long term.
The present results also emphasize the importance of attending to lasting negative consequences of parental bereavement. As we noted earlier (Rogers et al., 2008), symptoms of lasting grief that are maintained many years after the death might be subtle and not clearly detectable by friends, family, or the bereaved parents themselves. The current findings suggest that the effects might take a toll in the form of long term health consequences. Thus, professionals should be sensitized to potential lingering stress and emergent health problems for bereaved parents.
In conclusion, the overall results from this study provide evidence of lasting negative consequences of child death on bereaved parents' HRQoL. The findings emphasize the importance of receiving emotional support from a spouse for good health outcomes among bereaved couples, particularly for bereaved couples in the early stages of the family life cycle who experience infant death, and they raise awareness of the need for ongoing interventions to help parents cope with the consequences of lasting grief.
Acknowledgments
Support for this research was provided by the National Institute on Aging for Project 3 of P01 AG021079, R.M. Hauser, PI; M.M. Seltzer, PI of Project 3.
Contributor Information
Jieun Song, Waisman Center, University of Wisconsin, Madison, 1500 Highland Ave. Room 557, Madison, WI 53705-2280, song@waisman.wisc.edu
Frank J. Floyd, Department of Psychology, Georgia State University, P.O. Box 5010, Atlanta, GA 30302-5010, ffloyd@gsu.edu
Marsha Mailick Seltzer, Waisman Center and School of Social Work, University of Wisconsin, Madison, 1500 Highland Ave., Madison, WI 53705-2280, mseltzer@waisman.wisc.edu
Jan S. Greenberg, School of Social Work and Waisman Center, University of Wisconsin, Madison, 1350 University Ave, Madison, WI 53706, greenberg@waisman.wisc.edu
Jinkuk Hong, Waisman Center, University of Wisconsin, Madison, 1500 Highland Ave., Madison, WI 53705-2280, jhong@waisman.wisc.edu
References
- Boyle MH, Furlong W, Feeny D, Torrance GW, Hatcher J. Reliability of the Health Utilities Index—Mark III used in the 1991 cycle 6 Canadian General Social Survey Health Questionnaire. Quality of Life Research. 1995;4:249–257. doi: 10.1007/BF02260864. [DOI] [PubMed] [Google Scholar]
- Buchi S, Morgeli H, Schnyder U, Jenewein J, Glaser A, Fauchere JC, et al. Shared or discordant grief in couples 2-6 years after the death of their premature baby: Effects of suffering and posttraumatic growth. Psychosomatics. 2009;50(2):123–130. doi: 10.1176/appi.psy.50.2.123. [DOI] [PubMed] [Google Scholar]
- Cook JA. Influence of gender on the problems of parents of fatally ill children. Journal of Psychosocial Oncology. 1984;2(1):71–91. [Google Scholar]
- Dyregrov K, Nordanger D, Dyregrov A. Predictors of psychosocial distress after suicide, SIDS, and accidents. Death Studies. 2003;27:143–165. doi: 10.1080/07481180302892. [DOI] [PubMed] [Google Scholar]
- Feeny D, Furlong W, Boyle M, Torrance GW. Multiattribute health-status classification systems: Health Utilities Index. Pharmacoeconomics. 1995;7(6):490–502. doi: 10.2165/00019053-199507060-00004. [DOI] [PubMed] [Google Scholar]
- Feeny D, Furlong W, Torrance GW, Goldsmith CH, Zhu Z, DePauw S, et al. Multiattribute and single-attribute utility functions for the Health Utilities Index Mark 3 System. Medical Care. 2002;40(2):113–128. doi: 10.1097/00005650-200202000-00006. [DOI] [PubMed] [Google Scholar]
- Feeny D, Huguet N, McFarland BH, Kaplan MS. The construct validity of the Health Utilities Index Mark 3 in assessing mental health in population health surveys. Quality of Life Research. 2009;18(4):519–526. doi: 10.1007/s11136-009-9457-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest GC, Standish E, Baum JD. Support after perinatal death: A study of support and counseling after perinatal bereavement. British Medical Journal. 1982;285(6353):1475–1479. doi: 10.1136/bmj.285.6353.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fryback DG, Dunham NC, Palta M, Hanmer J, Buechner J, Cherepanov D, et al. US norms for six generic health-related quality-of-life indexes from the national health measurement study. Medical Care. 2007;45(12):1162–1170. doi: 10.1097/MLR.0b013e31814848f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser RM, Roan CL. The class of 1957 in their mid-60s: A first look. University of Wisconsin-Madison, Center for Demography and Ecology; 2006. Working Paper No 2006-03. [Google Scholar]
- Horsman J, Furlong W, Feeny D, Torrance G. The health utilities index (HUI): Concepts, measurement properties and application. Health and Quality of Life Outcomes. 2003;1:54. doi: 10.1186/1477-7525-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan MS, Huguet N, Orpana H, Feeny D, McFarland BH, Ross N. Prevalence and factors associated with thriving in older adulthood: A 10-year population-based study. Journal of Gerontology: Medical Sciences. 2008;63:M1097–M1104. doi: 10.1093/gerona/63.10.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keesee NJ, Currier JM, Meymeyer RA. Predictors of grief following the death of one's child: The contribution of finding meaning. Journal of Clinical Psychology. 2008;64(10):1145–1163. doi: 10.1002/jclp.20502. [DOI] [PubMed] [Google Scholar]
- Lehman DR, Wortman CB, Williams AF. Long-term effects of losing a spouse or child in a motor-vehicle crash. Journal of Personality and Social Psychology. 1987;52(1):218–231. doi: 10.1037//0022-3514.52.1.218. [DOI] [PubMed] [Google Scholar]
- Levav I, Kohn R, Iscovich J, Abramson JH, Tsai WY, Vigdorovich D. Cancer incidence and survival following bereavement. American Journal of Public Health. 2000;90:1601–1607. doi: 10.2105/ajph.90.10.1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Laursen TM, Precht DH, Olsen J, Mortensen PB. Hospitalization for mental illness among parents after the death of a child. New England Journal of Medicine. 2005;352:1190–1196. doi: 10.1056/NEJMoa033160. [DOI] [PubMed] [Google Scholar]
- Li J, Precht DH, Mortenson PB, Olson J. Mortality in parents after death of a child in Denmark: A nationwide follow-up study. Lancet. 2003;361:363–367. doi: 10.1016/S0140-6736(03)12387-2. [DOI] [PubMed] [Google Scholar]
- Lohan JA, Murphy SA. Mental distress and family functioning among married parents bereaved by a child's sudden death. Omega: Journal of Death and Dying. 2005-2006;52(4):295–305. [Google Scholar]
- Lohan JA, Murphy SA. Bereaved mothers' marital status and family functioning after a child's sudden, violent death: A preliminary study. Journal of Loss and Trauma. 2007;12:333–347. [Google Scholar]
- Maddigan SL, Feeny DH, Majumdar SR, Farris KB, Johnson JA. Health Utilities Index Mark 3 demonstrated construct validity in a population-based sample with type 2 diabetes. Journal of Clinical Epidemiology. 2006;59(5):472–477. doi: 10.1016/j.jclinepi.2005.09.010. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Wilkinson RG. Social determinants of health. New York: Oxford Press; 2005. [Google Scholar]
- McBride BA, Schoppe SJ, Rane TR. Child characteristics, parenting stress, and parental involvement. Journal of Marriage and the Family. 2002;64:998–1011. [Google Scholar]
- Moriarty HJ, Carroll R, Cotroneo M. Differences in bereavement reactions within couples following death of a child. Research in Nursing & Health. 1996;19:461–469. doi: 10.1002/(SICI)1098-240X(199612)19:6<461::AID-NUR2>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- Murphy SA, Johnson C, Cain KC, Gupta AD, Dimond M, Lohan J. Broad-spectrum group treatment for parents bereaved by the violent deaths of their 12- to 28-year old children: A randomized controlled trial. Death Studies. 1998;22:209–235. doi: 10.1080/074811898201560. [DOI] [PubMed] [Google Scholar]
- Murphy SA, Chung IJ, Johnson LC. Patterns of mental distress following the violent death of a child and predictors of change over time. Research in Nursing & Health. 2002;25:425–437. doi: 10.1002/nur.10060. [DOI] [PubMed] [Google Scholar]
- Murphy SA, Johnson LC, Wu L, Fan JJ, Lohan J. Bereaved parents' outcomes 4 to 60 months after their children's deaths by accident, suicide, or homicide: A comparative study demonstrating differences. Death Studies. 2003;27(1):39–61. doi: 10.1080/07481180302871. [DOI] [PubMed] [Google Scholar]
- Najman JM, Vance JC, Boyle F, Embleton G, Foster B, Therle J. The impact of a child death on marital adjustment. Social Science and Medicine. 1993;37:1005–1010. doi: 10.1016/0277-9536(93)90435-7. [DOI] [PubMed] [Google Scholar]
- Norris F, Murrell S. Social support, life events, and stress as modifiers of adjustment to bereavement by older adults. Psychology and Aging. 1990;5:429–436. doi: 10.1037//0882-7974.5.3.429. [DOI] [PubMed] [Google Scholar]
- Oliver LE. Effects of a child's death on the marital relationships: A review. Omega: Journal of Death and Dying. 1999;39:197–227. [Google Scholar]
- Parke RD, Dennis J, Flyr ML, Morris KL, Leidy MS, Schofield TJ. Fathers: Cultural and ecological perspectives. In: Luster T, Okagaki L, editors. Parenting: An ecological perspective. 2nd. Mahwah, NJ: Lawrence Erlbaum Associates; 2005. pp. 103–144. [Google Scholar]
- Rachuba L, Stanton B, Howard D. Violent crime in the United States. An epidemiologic profile. Archives of Pediatric Adolescent Medicine. 1995;149:953–960. doi: 10.1001/archpedi.1995.02170220019002. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Robert SA, Cherepanov D, Palta M, Dunham NC, Feeny D, Fryback G. Socioeconomic status and age variations in health-related quality of life: Results from the National Health Measurement Study. Journal of Gerontology: Social Sciences. 2009;64(3):378–389. doi: 10.1093/geronb/gbp012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers CH, Floyd FJ, Seltzer MM, Greenberg J, Hong J. Long-term effects of the death of a child on parents' adjustment in midlife. Journal of Family Psychology. 2008;22(2):203–211. doi: 10.1037/0893-3200.22.2.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandhya S. The social context of marital happiness in urban Indian couples: Interplay of intimacy and conflict. Journal of Marital and Family Therapy. 2009;35(1):74–96. doi: 10.1111/j.1752-0606.2008.00103.x. [DOI] [PubMed] [Google Scholar]
- Schut H, Stroebe MS, van den Bout J, Teheggen M. The efficacy of bereavement interventions: Determining who benefits. In: Stroebe M, Hansson RO, Stroebe W, Schut H, editors. Handbook of bereavement research: Consequences, coping, and care. Washington D.C.: American Psychological Association; 2001. pp. 705–737. [Google Scholar]
- Schwab R. A child's death and divorce: Dispelling myth. Death Studies. 1998;22:445–468. [Google Scholar]
- Shapiro ER. Grief in interpersonal perspective: Theories and their implication. In: Stroebe MS, Stroebe W, Hansson RO, editors. Handbook of bereavement: Theory, research and intervention. New York: Cambridge University Press; 2001. pp. 301–327. [Google Scholar]
- Sherkat DE, Reed MD. The effects of religion and social support on self-esteem and depression among the suddenly bereaved. Social Indicators Research. 1992;26(3):259–275. [Google Scholar]
- Sidmore KV. Parental bereavement: levels of grief as affected by gender issues. Omega: Journal of Death and Dying. 1999-2000;40(2):351–374. [Google Scholar]
- Stroebe M, Folkman S, Hansson R, Schut H. The prediction of bereavement outcomes: Development of an integrative risk factor framework. Social Science and Medicine. 2006;63:2440–2451. doi: 10.1016/j.socscimed.2006.06.012. [DOI] [PubMed] [Google Scholar]
- Stroebe W, Zech E, Stroebe MS, Abakoumkin G. Does social support help in bereavement? Journal of Social and Clinical Psychology. 2005;24(7):1030–1050. [Google Scholar]
- Tempier R, Pawliuk N. Measuring patient quality of life: Is the health utility index useful? Psychiatric Quarterly. 2007;78(1):53–62. doi: 10.1007/s11126-006-9026-7. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Stress, coping, and social support processes: Where are we, what next [Special Issue] Journal of Health of Social Behavior. 1995:53–79. [PubMed] [Google Scholar]
- Weng HLH, Bastian LA, Taylor DH, Moser BK, Ostbye T. Number of children associated with obesity in middle-aged women and men: Results from the Health and Retirement Study. Journal of Women's Health. 2004;13(1):85–91. doi: 10.1089/154099904322836492. [DOI] [PubMed] [Google Scholar]
- Wijngaards-de Meij L, Stroebe M, Schut H, Stroebe W, van den Bout J, van der Heijden P, et al. Couples at risk following the death of their child: Predictors of grief versus depression. Journal of Consulting and Clinical Psychology. 2005;73(4):617–623. doi: 10.1037/0022-006X.73.4.617. [DOI] [PubMed] [Google Scholar]
- Wijngaards-de Meij L, Stroebe M, Stroebe W, Schut H, Van den Bout J, Van der Heijden PGM, et al. The impact of circumstances surrounding the death of a child on parents' grief. Death Studies. 2008;32:237–252. doi: 10.1080/07481180701881263. [DOI] [PubMed] [Google Scholar]
- Winsor TD, Ryan LH, Smith J. Individual well-being in middle and older adulthood: Do spousal beliefs matter? Journal of Gerontology: Psychological Sciences. 2009;64B(5):586–596. doi: 10.1093/geronb/gbp058. [DOI] [PMC free article] [PubMed] [Google Scholar]