Abstract
Among patients with multiple sclerosis (MS), fatigue is the most commonly reported symptom, and one of the most debilitating. Despite its high prevalence and significant impact, fatigue is still poorly understood and often under-emphasized because of its complexity and subjective nature. In recent years, an abundance of literature from specialists in sleep medicine, neurology, psychiatry, psychology, physical medicine and rehabilitation, and radiology have shed light on the potential causes, impact, and treatment of MS-related fatigue. Though such a diversity of contributions clearly has advantages, few recent articles have attempted to synthesize this literature, and existing overviews have focused primarily on potential causes of fatigue rather than clinical evaluation or treatment. The aims of this review are to examine, in particular for sleep specialists, the most commonly proposed primary and secondary mechanisms of fatigue in MS, tools for assessment of fatigue in this setting, and available treatment approaches to a most common and challenging problem.
Citation:
Braley TJ; Chervin RD. Fatigue in multiple sclerosis: mechanisms, evaluation, and treatment. SLEEP 2010;33(8):1061-1067.
Keywords: Fatigue, multiple sclerosis, restless legs syndrome, insomnia, circadian rhythm
MULTIPLE SCLEROSIS (MS) IS AN INFLAMMATORY DISEASE OF THE CENTRAL NERVOUS SYSTEM THAT RESULTS IN MYELIN DESTRUCTION AND AXONAL degeneration in the brain and spinal cord. According to the National Multiple Sclerosis Society, the prevalence of this condition is estimated to be 400,000 in the United States and over 2.5 million worldwide. Several subtypes of MS exist. Eighty percent of patients present with a relapsing-remitting subtype, characterized by clearly defined episodes of neurological dysfunction (relapses) separated by periods of relative clinical stability (remissions). In the majority of untreated cases, relapsing-remitting MS evolves into a secondary-progressive phase during which the subject experiences a gradual, insidious deterioration, usually in the form of paraparesis, hemiparesis, or dementia. A primary-progressive subtype occurs in a smaller percentage of patients, characterized by a slow deterioration in neurologic function from onset, without distinct relapses.
Therapies available for management of the MS disease process can decrease the frequency of clinical relapses and new radiological lesion formation. However, none of these therapies reverse preexisting tissue damage or control chronic symptoms, such as fatigue, that are common to all subtypes of MS. Other treatments and management strategies that can alleviate these symptoms sometimes provide critical opportunities to improve quality of life and occupational productivity.
Fatigue is considered to be one of the main causes of impaired quality of life among MS patients, independent of depression or disability.1 Fatigue is also among the most common symptoms, reported by at least 75% of MS patients at some point in the disease course.2,3 For many, fatigue is considered to be the single most debilitating symptom, surpassing pain and even physical disability.4 Fatigue also imposes significant socioeconomic consequences, including loss of work hours and in some instances, loss of employment.5
Nonetheless, fatigue in MS remains poorly understood and often underemphasized for several reasons. First, fatigue is a subjective symptom without a unified definition. While common definitions include a sense of exhaustion, lack of energy, or tiredness,1 and “a subjective lack of physical and/or mental energy that is perceived by the individual or caregiver to interfere with usual or desired activity,”6 these terms may be interpreted differently depending on cultural or educational backgrounds.
Ambiguity also arises because no gold standard exists by which to measure fatigue. Although multiple questionnaires are available, most clinicians do not know which are best suited to MS patients. Furthermore, whereas questionnaires can be helpful to rate the level of fatigue, most do not include questions to qualify or define the fatigue.
Finally, fatigue in MS patients may be multifactorial. In addition to immunologic abnormalities, multiple sclerosis is associated with an increased prevalence of other conditions that contribute to fatigue, including depression and several sleep disorders. For example, although sleep disorders are recognized for contributions to excessive daytime sleepiness, many patients with sleep disorders such as obstructive sleep apnea consider their problems with fatigue, tiredness, or lack of energy to supersede their problems with sleepiness per se.7 Moreover, treatment of these disorders leads to robust improvement in patient-defined fatigue, tiredness, and lack of energy, as well as sleepiness.8 Separation of treatable from untreatable causes of fatigue can be challenging in MS, however, and the wide range of potential etiologies within this population makes MS a unique model for the study of fatigue.
Primary Mechanisms
The most commonly proposed primary mechanisms of fatigue in MS involve the immune system or sequelae from central nervous system damage. Specific causes are thought to include proinflammatory cytokines, endocrine influences, axonal loss, and altered patterns of cerebral activation.
Cytokine influences
Although the pathological mechanisms of MS are poorly understood, cytokines implicated in the disease are thought to be strong mediators of fatigue. Among these, interferon-γ and TNF-α are the most studied. Both are important inflammatory mediators in MS.9,10 Significantly increased TNF-α mRNA expression, TNF-α levels, and interferon-γ levels are found in fatigued MS patients compared to non-fatigued patients.11,12 Unfortunately, use of these observations to devise therapeutic targets is not straightforward. For instance, TNF-α antagonists that have been shown to reduce sleepiness in patients with obstructive sleep apnea13 may worsen MS.14 In addition, both cytokines are relatively nonspecific and may be elevated in a variety of inflammatory conditions.
Endocrine influences
The hypothalamic-pituitary-adrenal (HPA) axis and the hormone dehydroepiandrosterone (DHEA) have been studied in multiple autoimmune diseases in which fatigue is a common symptom. Both low cortisol15 and low DHEA levels16 have been implicated in chronic fatigue syndrome, and low DHEA levels are found in patients with lupus and rheumatoid arthritis.17 Recent attempts have been made to translate these findings to multiple sclerosis. An association between fatigue and dysregulation of ACTH levels has been proposed, but studies examining ACTH levels after dexamethasone-corticotropin stimulation (Dex-CRH) tests in fatigued MS patients have shown conflicting results.11,18 Lower levels of DHEA and its sulfated compound, DHEAS, have been demonstrated in MS patients with sustained fatigue than their non-fatigued counterparts.19 Although definitive conclusions cannot be drawn based solely on these studies, these results suggest a possible endocrine contribution to fatigue in MS. The fact that many MS patients report increased energy while taking corticosteroids as treatment for their neurologic symptoms further supports a possible hormonal influence. However, because of the chronic nature of fatigue and risks of long-term steroid use, steroids are not advocated as treatment for fatigue.
Axonal loss and altered cerebral activation
As conventional measures of T2 lesion volume and atrophy have fallen short in providing a basis for fatigue in MS,20 many investigators have relied on non-conventional neuroimaging techniques to shed further insight. The demonstration on positron emission tomography (PET) of decreased regional glucose metabolism in the frontal cortex and basal ganglia of fatigued MS patients has suggested that neuronal dysfunction in these regions may play a role.21 Magnetic resonance spectroscopy (MRS) studies have shown significant reductions in N-acetylaspartate/creatine (NAA/Cr) ratios in multiple brain regions among fatigued MS patients in comparison to non-fatigued MS patients, suggesting axonal loss as a contributing factor.22,23 MS-related fatigue also may arise at least in part from compensatory reorganization and increased brain recruitment, as functional MRI studies that have demonstrated increased volumes and patterns of activation in the cingulate gyri and left primary sensory cortex in fatigued MS patients compared to non-fatigued patients.24
Secondary Mechanisms
Fatigue in MS also can arise from associated conditions or accumulation of disease burden. Specific causes to consider include sleep disorders, depression, disability status, MS subtype, and iatrogenicity.
Sleep disorders
Sleep disorders and their potential contributions to fatigue in MS have gained increasing attention in the past several years. Specific sleep disorders or problems that may affect MS patients disproportionately include restless legs syndrome, periodic limb movement disorder, chronic insomnia, and circadian rhythm disturbances.
Restless legs syndrome:
Restless legs syndrome (RLS) affects about 10% of the general population.25–27 RLS is classified as either idiopathic or secondary to another medical cause known to increase vulnerability. The prevalence of RLS among MS patients is approximately 3-5 times that of the general population.28–31
The pathophysiologic basis for this association is still poorly understood. The frequency of RLS is proposed to rise with MS severity, as assessed by the Expanded Disability Status Score, irrespective of brain lesion load or location.28,30 Other authors suggest a correlation between spinal cord pathology and RLS. Dopaminergic diencephalospinal and reticulospinal pathways that project to the spinal cord, to inhibit sensory inputs and autonomic output, are susceptible to damage from a variety of pathologic processes, including MS.32,33 Dysfunction of these dopaminergic pathways could decrease sensory thresholds and increase susceptibility to RLS. This hypothesis is supported by a recent study utilizing spinal cord diffusion tensor imaging in MS patients with and without RLS: Fractional anisotropy, a measure of axonal integrity, is lower in MS patients with RLS than those without RLS.34
Sleep disordered breathing:
MS lesions that affect medullary respiratory centers can lead to sleep disordered breathing in the form of central sleep apnea (Ondine's curse). Studies regarding the prevalence of obstructive sleep apnea (OSA) among persons with MS have yielded conflicting results.35,36,37 Given the relatively high prevalence of OSA in the general population, further studies are necessary. Nonetheless, MS patients with medullary lesions should be assessed for central or obstructive sleep disordered breathing with a high index of suspicion, as medullary reticular formation damage can impair respiratory control.38
Chronic insomnia and circadian rhythm abnormalities:
The frequency of sleep disturbance is increased among patients with MS as compared to the general population.39 Risk for chronic insomnia may arise secondary to pain, spasticity, depression, anxiety, nocturia, medication effects, or primary sleep disorders such as RLS or periodic limb movement disorder.40–43 Potential causes such as these must be addressed, as insomnia and poor sleep quality in MS patients correlate significantly with quality of life.42
Some investigators have implicated disrupted sleep architecture and circadian disturbances as contributors to fatigue. In a recent study, Attarian and colleagues used actigraphy to assess the sleep of fatigued MS subjects. A modestly increased frequency of delayed sleep onset distinguished fatigued MS subjects from non-fatigued subjects and healthy controls. Fatigued MS subjects were also more likely to have disrupted sleep. The authors concluded that MS-related fatigue may arise, at least in part, from circadian rhythm disturbances.44 A relatively small sample size (including 15 fatigued MS subjects), and the inability of actigraphy to identify the cause of sleep disruption, were limitations of this study. However, the findings seem consistent with an important hypothesis—that disrupted nocturnal sleep may contribute to fatigue in MS.
Kaynak and colleagues asked 37 MS patients (27 who were fatigued and 10 who were not) and 13 healthy controls to undergo polysomnography and complete several subjective measures, including the Fatigue Severity Scale, Fatigue Impact Scale, Epworth Sleepiness Scale, Pittsburgh Sleep Quality Index, Beck Depression Inventory, and subjective reports of RLS symptoms and snoring.36 Polysomnographic data included sleep stage percentages and latencies, sleep efficiency and continuity indices, time in bed, wake time after sleep onset, and arousals that occurred spontaneously or in association with respiratory events or leg movements. The MS patients, regardless of level of fatigue, had a significantly higher frequency of RLS, higher Epworth Sleepiness Scale scores, and higher Pittsburgh Sleep Quality Index scores. The time in bed, wake time after sleep onset %, total arousal index, limb movement arousal index, and periodic limb movement arousal index were also elevated in MS patients as compared to healthy controls. The sleep efficiency index and sleep continuity index were decreased. Fatigued vs. non-fatigued MS patients on average had a significantly higher total arousal index. The Pittsburgh Sleep Quality Index results also suggested more disrupted sleep in fatigued MS patients. There were no group differences in sleep stage percentages, apnea/hypopnea indices, or minimum oxygen saturations. In the study by Kaynak et al., depression symptoms also correlated with fatigue.
Depression
Depression commonly accompanies MS, with a prevalence of up to 50%.45,46 Depression itself can manifest with fatigue and symptoms often mistaken for fatigue (loss of motivation, anhedonia), making this condition difficult to sort out from MS-associated fatigue. Contrary to previous studies, recent studies have identified a correlation between fatigue and depression in MS.47 Various rating scales including the Beck Depression Inventory and the Zung self-rating depression scale correlate with the Fatigue Severity Scale.48,49 The presence of fatigue must alert the clinician to the possibility of depression. Regardless of any contribution to fatigue, depression should be addressed and treated, as it has substantial impact on quality of life.
MS subtype and disability
MS subtype and disease severity can affect the risk of fatigue. The Expanded Disability Status Score correlates with fatigue scores,48,50,51 though less strongly, perhaps, after adjusting for depression.51,52 A review of The New York State Multiple Sclerosis Consortium Database showed that fatigue consistently correlated with Expanded Disability Status Score.47 Fatigue appears to be more severe in patients with progressive subtypes of MS,3,49 but this observation may in part be confounded by differences in disability levels.49
Iatrogenic mechanisms
Medications used to treat symptoms of MS have the potential to cause fatigue. Drowsiness, a common side of effect of several antispasmodics including cyclobenzaprine and the benzodiazepines, may be perceived or reported as fatigue. Pain medications or anxiolytics may have a similar effect. Clinicians should be aware of these side effects in patients presenting with fatigue, and efforts should be made to minimize use of these medications, if possible.
Immunomodulatory and immunosuppressive therapies also have the potential to cause or exacerbate fatigue. Fatigue is generally thought to occur more frequently with interferon-β relative to other immunomodulatory agents, although this has not been unequivocally demonstrated.50,53
Fatigue Rating Scales
Many fatigue rating scales are available, but not all correlate well with each other, and most are not specific to MS. Several of the original fatigue scales, including some of the most widely used, were created to quantify fatigue associated with other chronic medical conditions including chronic fatigue syndrome and systemic lupus erythematosus. Some scales primarily quantify fatigue, whereas others assess the impact of fatigue on various functions. A useful comprehensive review of the various general and disease specific scales is outlined by Dittner et al.54 Here, we review scales most commonly used for MS patients, including instruments designed specifically for MS.
The Chalder Fatigue Scale (The Fatigue Scale)
One of the most well-known fatigue scales, the Chalder Fatigue Scale was created for chronic fatigue syndrome patients. This 14-item instrument quantifies fatigue intensity in terms of physical and mental domains.55 Each item is quantified by a numeric value on a Likert scale, and a sum score is calculated. Higher totals indicate more fatigue. Advantages of this instrument include its ease of use and brevity: it can usually be completed within 2-3 minutes. Although it has demonstrated good internal consistency in patients with chronic fatigue syndrome, MS-specific assessments of validity and consistency for this instrument are lacking. Nonetheless, some investigators still regard The Fatigue Scale as a valuable instrument for clinical studies.56,57
Krupp's Fatigue Severity Scale (FSS)
Many studies of MS-related fatigue have used the Fatigue Severity Scale to identify fatigued patients. Initially designed to identify common features of fatigue in both MS and lupus patients, the Fatigue Severity Scale assesses the impact of fatigue on multiple outcomes, with a physical focus.58 Each of 9 responses is provided on a 7-point Likert scale. Prior studies have shown acceptable internal consistency and stability over time, and sensitivity to change afforded by clinical improvement. The Fatigue Severity Scale has been shown to differentiate between subgroups of patients with MS, chronic fatigue syndrome, and primary depression. Moreover, the scores correlate with other scales commonly used in MS, including the Modified Fatigue Impact Scale and Fatigue Descriptive Scale.48
The Modified Fatigue Impact Scale (MFIS)
The Modified Fatigue Impact Scale, proposed by the Multiple Sclerosis Council for Clinical Practice Guidelines, has gained recognition among MS specialists as a reliable tool. Originally derived from the 40-item Fatigue Impact Scale (FIS),59 the MFIS contains only 21 items and offers a more multidimensional assessment: physical (pMFIS, 9 items), cognitive (cMFIS, 10 items), and psychosocial functioning (psMFIS, 2 items). The total score is the sum of the 21 items. An abbreviated version that contains 5 items also exists. Besides its multidimensional features, other advantages of the MFIS include ease of use, good reproducibility, and strong correlation with FSS results (r = 0.68).51
A Diagnostic Approach to Fatigue
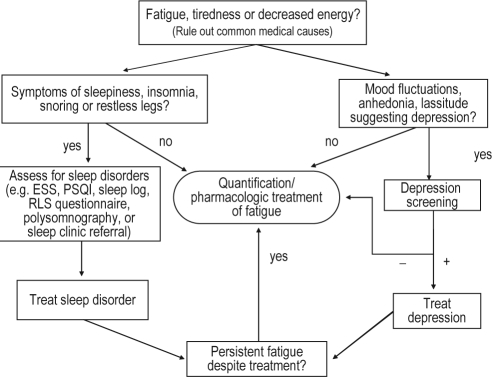
An open ended question, followed by a series of more focused inquiries will often prove to be a productive approach. This should be followed by screening for other confounding conditions such as sleep disorders or depression. A systematic approach to the assessment and treatment of fatigue in patients with MS is summarized in Figure 1.
Figure 1.
Systematic approach to treating reversible causes of fatigue. (abbreviations: ESS, Epworth Sleepiness Scale; PSQI, Pittsburgh Sleep Quality Index; RLS, restless legs syndrome)
Initial questioning
If the patient does not volunteer fatigue, one suggested approach is to ask the patient about his or her level of energy. Often patients will endorse terms such as “low energy,” “fatigue,” or “tiredness”; but they should be allowed to provide their own descriptions to avoid any misconceptions from the start. If significant fatigue, low energy, or tiredness is endorsed, quantification with one of the above fatigue scales may be helpful to clarify severity or establish a baseline from which future progression or response to intervention can be assessed.
Sleepiness assessment
Fatigue and sleepiness may be difficult to distinguish. If the problem is reported to be worse during sedentary, monotonous activities than during extended physical activity, sleepiness is more likely than fatigue. If the patient endorses what appears to be sleepiness, describes poor sleep quality, or reports the use of sleep as a recovery mechanism, screening for excessive daytime sleepiness is recommended. The Epworth Sleepiness Scale (ESS) is a validated 8-item questionnaire that uses a 4-point Likert scale to quantify the patient's likelihood of falling asleep (dozing) in 8 sedentary circumstances.60 This instrument is widely used in the outpatient setting to evaluate subjective sleepiness. A patient's perception of sleep quality can be quantified with instruments such as the Pittsburgh Sleep Quality Index (PSQI). The PQSI is a 19-item, self-rated, valid, and reliable measure of sleep quality and disturbances over the preceding month61; results may correlate with the perception of fatigue and disrupted sleep in MS patients.36 If excessive daytime sleepiness or poor sleep quality is endorsed, patients should be screened for potential sleep disorders, including obstructive sleep apnea, primary insomnia, narcolepsy, periodic limb movement disorder, and restless legs syndrome.
Depression screening
Multiple screening tools exist for evaluation of depression. Often, observation of the patient's demeanor or a few simple questions about mood will alert the clinician that depression may be present. Among the most common tools are the Beck Depression Inventory (BDI) and the Zung Self-Rating Depression scale. A positive screen should prompt consideration for treatment of depressive symptoms or referral to a mental health specialist.
Fatigue quantification
In clinical settings, use of a fatigue scale is not always necessary when a patient clearly endorses the symptom, its importance, and desire for treatment. However, even in such instances, a formal scale may be a useful tool to evaluate treatment response. If a fatigue scale is favored, the clinician's level of comfort, time requirements, reliability, reproducibility, and applicability to MS patients should also be considered when selecting the appropriate instrument. Taking all of these factors into consideration, the Fatigue Severity Scale or Modified Fatigue Impact Scale may be optimal.
Other medical conditions
Laboratory testing for common hematologic and metabolic conditions should be considered as part of the initial screening process. Iron studies, including ferritin levels, may be warranted if exercise intolerance or symptoms of restless legs syndrome are endorsed, as clinically significant iron deficiency may be missed with routine blood counts. Vitamin B12 and folate levels should be assessed in patients with a history of excessive alcohol use or suspected nutritional deficiencies. Thyroid studies should be considered if the patient presents with systemic symptoms suggestive of hyper- or hypothyroidism (weight fluctuation, skin changes, temperature intolerance). Clinicians should also have a low threshold for assessing 25-hydroxy vitamin D levels (the primary circulating form of vitamin D),62 as vitamin D deficiency is common in MS63 and is associated with fatigue in a variety of conditions,64 as well as skeletal muscle dysfunction.65,66
Pharmacologic Treatment
Treatment options for fatigue and MS are summarized in Table 1, along with indications, doses, side effects, and contraindications.
Table 1.
Commonly used pharmacologic treatments for MS-related fatigue.
| Drug | Brand Name | FDA Indications | Dosage | Common Side Effects | Contraindications and Precautions |
|---|---|---|---|---|---|
| Amantadine | Symmetrel® |
|
100 mg BID |
|
|
| Modafinil | Provigil® |
|
Start 200 mg every morning or at start of shift, may escalate to 400 mg |
|
|
| Armodafinil | Nuvigil® |
|
Start at 150 mg every morning or at start of shift, may escalate to 250 mg |
|
|
Amantadine
Amantadine (Symmetrel) is approved by the FDA for treatment of influenza. By an unknown mechanism that involves cholinergic and dopaminergic transmission, amantadine also has anti-parkinsonism properties and is FDA-approved for Parkinson disease. The drug is generally well tolerated and has a mild side-effect profile. It also remains the most extensively studied for MS-related fatigue. Although several placebo-controlled trials have shown modestly favorable results for subjective measures of fatigue,67 a Cochrane Database Review conducted by Taus et al. demonstrated that the small scale of these studies and potential for bias preclude formal prescribing recommendations or FDA approval.68
Pemoline
Pemoline is a central nervous system stimulant with dopaminergic effects. It has not been studied as extensively as amantadine. One crossover and one parallel-arm study with amantadine have yielded unimpressive results.69,70 In addition, pemoline has been associated with liver toxicity that has limited its use and made it an unattractive option for treating multiple sclerosis patients.
Modafinil
Modafinil (Provigil), and its (R)-enantiomer Armodafinil (Nuvigil), are wake-promoting agents approved by the FDA for narcolepsy, shift-work sleep disorder, and obstructive sleep apnea with residual excessive sleepiness despite optimal use of continuous positive airway pressure. At recommended doses, modafinil is generally safe and well tolerated, although increased risk of adverse psychiatric and cardiovascular effects have been reported. Modafinil has been studied in two controlled trials involving MS patients with fatigue; neither unequivocally demonstrated significant differences against placebo.71,72 Nonetheless, many MS specialists rely on modafinil when other agents have failed.
Non-Pharmacologic Treatments
In addition to pharmacologic treatments, many authors consider non-pharmacologic treatments to be important tools in the management of MS-related fatigue. A recent study of cognitive behavioral therapy (CBT) demonstrated sustained fatigue reduction over a six-month period. Incidentally, the active control arm of the trial, relaxation therapy (RT), was also shown to have benefit, to a lesser extent.56 Limitations of the study included use of a single therapist, potential underpowering, and exclusion of MS patients with EDSS scores > 6. Nonetheless, these findings highlight the potential role for a new approach to fatigue management, apparently with lasting benefit.
Aerobic exercise and rehabilitation regimens, energy conservation strategies, and cooling devices have also been studied as potential interventions.73–76 With the exception of cooling therapy,77 no large-scale randomized controlled studies have demonstrated their effectiveness in the MS population. Nonetheless, numerous smaller studies have shown trends in favor of these treatments as potential mediators of fatigue. Moreover, as exercise and cooling devices are associated with other health benefits in patients with MS, most clinicians advocate their use in tandem with pharmacologic treatments.
CONCLUSIONS
Sleep specialists, neurologists, and MS specialists alike will inevitably encounter MS patients with fatigue complaints at some point during their practice. While the treatment of MS-related fatigue is challenging, knowledge of treatable etiologies and use of a systematic approach can facilitate prompt diagnosis and management, offer the best chance to identify treatable causes, and ultimately have a profound positive impact for the patient.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Chervin is on the advisory board of Pavad. Dr. Braley is the principal investigator on several industry funded studies at the University of Michigan but receives no compensation for this work; she has participated in speaking engagements for Teva Pharmaceuticals, EMD Serono, Pfizer and Biogen-Idec.
ACKNOWLEDGMENTS
Dr. Braley's contribution was supported (in part) by a Sylvia Lawry Physician Fellowship from the National Multiple Sclerosis Society.
Abbreviations
- DI
Beck Depression Inventory
- Dex-CRH
Dexamethasone-corticotropin stimulation test
- DHEA
Dehydroepiandrosterone
- DHEA-S
Sulfated dehydroepiandrosterone
- ESS
Epworth Sleepiness Scale
- FIS
Fatigue Impact Scale
- FSS
Fatigue Severity Scale
- HPA
Hypothalamic-pituitary axis
- MFIS
Modified Fatigue Impact Scale
- cMFIS
cognitive subscale of MFIS
- pMFIS
physical subscale of MFIS
- psMFIS
psychosocial subscale of MFIS
- MRI
Magnetic resonance imaging
- MRS
Magnetic resonance spectroscopy
- MS
Multiple sclerosis
- NAA/Cr
N-acetyl acetate/creatine ratio
- PET
Positron emission tomography
- PSQI
Pittsburgh Sleep Quality Index
- RLS
Restless legs syndrome
- TNF-α
Tumor necrosis factor alpha
Footnotes
A commentary on this article appears in this issue on page 1005.
REFERENCES
- 1.Krupp LB, Alvarez LA, LaRocca NG, Scheinberg LC. Fatigue in multiple sclerosis. Arch Neurol. 1988;45:435–7. doi: 10.1001/archneur.1988.00520280085020. [DOI] [PubMed] [Google Scholar]
- 2.Krupp L. Fatigue is intrinsic to multiple sclerosis (MS) and is the most commonly reported symptom of the disease. Mult Scler. 2006;12:367–8. doi: 10.1191/135248506ms1373ed. [DOI] [PubMed] [Google Scholar]
- 3.Lerdal A, Celius EG, Krupp L, Dahl AA. A prospective study of patterns of fatigue in multiple sclerosis. Eur J Neurol. 2007;14:1338–43. doi: 10.1111/j.1468-1331.2007.01974.x. [DOI] [PubMed] [Google Scholar]
- 4.Janardhan V, Bakshi R. Quality of life in patients with multiple sclerosis: the impact of fatigue and depression. J Neurol Sci. 2002;205:51–8. doi: 10.1016/s0022-510x(02)00312-x. [DOI] [PubMed] [Google Scholar]
- 5.Smith MM, Arnett PA. Factors related to employment status changes in individuals with multiple sclerosis. Mult Scler. 2005;11:602–9. doi: 10.1191/1352458505ms1204oa. [DOI] [PubMed] [Google Scholar]
- 6.Fatigue Guidelines Development Panel of the Multiple Sclerosis Council for Clinical Practice Guidelines. Fatigue and Multiple Sclerosis. Evidence-Based Management Strategies for Fatigue in Multiple Sclerosis. Washington, DC: Paralyzed Veterans of America; 1998. [Google Scholar]
- 7.Chervin RD. Sleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apnea. Chest. 2000;118:372–9. doi: 10.1378/chest.118.2.372. [DOI] [PubMed] [Google Scholar]
- 8.Chotinaiwattarakul W, O'Brien L, Chervin R. Fatigue, tiredness, and lack of energy improve with treatment for OSA. J Clin Sleep Med. 2009;5:222–7. [PMC free article] [PubMed] [Google Scholar]
- 9.Sharief MK, Hentges R. Association between tumor necrosis factor-alpha and disease progression in patients with multiple sclerosis. N Engl J Med. 1991;325:467–72. doi: 10.1056/NEJM199108153250704. [DOI] [PubMed] [Google Scholar]
- 10.Hirsch RL, Panitch HS, Johnson KP. Lymphocytes from multiple sclerosis patients produce elevated levels of gamma interferon in vitro. J Clin Immunol. 1985;5:386–9. doi: 10.1007/BF00915335. [DOI] [PubMed] [Google Scholar]
- 11.Heesen C, Nawrath L, Reich C, Bauer N, Schulz KH, Gold SM. Fatigue in multiple sclerosis: an example of cytokine mediated sickness behaviour? J Neurol Neurosurg Psychiatry. 2006;77:34–9. doi: 10.1136/jnnp.2005.065805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flachenecker P, Bihler I, Weber F, Gottschalk M, Toyka KV, Rieckmann P. Cytokine mRNA expression in patients with multiple sclerosis and fatigue. Mult Scler. 2004;10:165–9. doi: 10.1191/1352458504ms991oa. [DOI] [PubMed] [Google Scholar]
- 13.Vgontzas AN, Zoumakis E, Lin HM, Bixler EO, Trakada G, Chrousos GP. Marked decrease in sleepiness in patients with sleep apnea by etanercept, a tumor necrosis factor-alpha antagonist. J Clin Endocrinol Metab. 2004;89:4409–13. doi: 10.1210/jc.2003-031929. [DOI] [PubMed] [Google Scholar]
- 14.The Lenercept Multiple Sclerosis Study Group and The University of British Columbia MS/MRI Analysis Group. TNF neutralization in MS: results of a randomized placebo-controlled multicenter study. Neurology. 1999;53:457–65. [PubMed] [Google Scholar]
- 15.Cleare AJ. The neuroendocrinology of chronic fatigue syndrome. Endocr Rev. 2003;24:236–52. doi: 10.1210/er.2002-0014. [DOI] [PubMed] [Google Scholar]
- 16.Maes M, Mihaylova I, De Ruyter M. Decreased dehydroepiandrosterone sulfate but normal insulin-like growth factor in chronic fatigue syndrome (CFS): relevance for the inflammatory response in CFS. Neuro Endocrinol Lett. 2005;26:487–92. [PubMed] [Google Scholar]
- 17.Chen CC, Parker CR., Jr Adrenal androgens and the immune system. Semin Reprod Med. 2004;22:369–77. doi: 10.1055/s-2004-861553. [DOI] [PubMed] [Google Scholar]
- 18.Gottschalk M, Kumpfel T, Flachenecker P, et al. Fatigue and regulation of the hypothalamo-pituitary-adrenal axis in multiple sclerosis. Arch Neurol. 2005;62:277–80. doi: 10.1001/archneur.62.2.277. [DOI] [PubMed] [Google Scholar]
- 19.Tellez N, Comabella M, Julia E, et al. Fatigue in progressive multiple sclerosis is associated with low levels of dehydroepiandrosterone. Mult Scler. 2006;12:487–94. doi: 10.1191/135248505ms1322oa. [DOI] [PubMed] [Google Scholar]
- 20.van der Werf SP, Jongen PJ, Lycklama a Nijeholt GJ, Barkhof F, Hommes OR, Bleijenberg G. Fatigue in multiple sclerosis: interrelations between fatigue complaints, cerebral MRI abnormalities and neurological disability. J Neurol Sci. 1998;160:164–70. doi: 10.1016/s0022-510x(98)00251-2. [DOI] [PubMed] [Google Scholar]
- 21.Roelcke U, Kappos L, Lechner-Scott J, et al. Reduced glucose metabolism in the frontal cortex and basal ganglia of multiple sclerosis patients with fatigue: a 18F-fluorodeoxyglucose positron emission tomography study. Neurology. 1997;48:1566–71. doi: 10.1212/wnl.48.6.1566. [DOI] [PubMed] [Google Scholar]
- 22.Tartaglia MC, Narayanan S, Francis SJ, et al. The relationship between diffuse axonal damage and fatigue in multiple sclerosis. Arch Neurol. 2004;61:201–7. doi: 10.1001/archneur.61.2.201. [DOI] [PubMed] [Google Scholar]
- 23.Tellez N, Alonso J, Rio J, et al. The basal ganglia: a substrate for fatigue in multiple sclerosis. Neuroradiology. 2008;50:17–23. doi: 10.1007/s00234-007-0304-3. [DOI] [PubMed] [Google Scholar]
- 24.Tartaglia MC, Narayanan S, Arnold DL. Mental fatigue alters the pattern and increases the volume of cerebral activation required for a motor task in multiple sclerosis patients with fatigue. Eur J Neurol. 2008;15:413–9. doi: 10.1111/j.1468-1331.2008.02090.x. [DOI] [PubMed] [Google Scholar]
- 25.Phillips B, Young T, Finn L, Asher K, Hening WA, Purvis C. Epidemiology of restless legs symptoms in adults. Arch Intern Med. 2000;160:2137–41. doi: 10.1001/archinte.160.14.2137. [DOI] [PubMed] [Google Scholar]
- 26.Lavigne GJ, Montplaisir JY. Restless legs syndrome and sleep bruxism: prevalence and association among Canadians. Sleep. 1994;17:739–43. [PubMed] [Google Scholar]
- 27.Rothdach AJ, Trenkwalder C, Haberstock J, Keil U, Berger K. Prevalence and risk factors of RLS in an elderly population: the MEMO study. Memory and Morbidity in Augsburg Elderly. Neurology. 2000;54:1064–8. doi: 10.1212/wnl.54.5.1064. [DOI] [PubMed] [Google Scholar]
- 28.Manconi M, Ferini-Strambi L, Filippi M, et al. Multicenter case-control study on restless legs syndrome in multiple sclerosis: the REMS study. Sleep. 2008;31:944–52. [PMC free article] [PubMed] [Google Scholar]
- 29.Auger C, Montplaisir J, Duquette P. Increased frequency of restless legs syndrome in a French-Canadian population with multiple sclerosis. Neurology. 2005;65:1652–3. doi: 10.1212/01.wnl.0000184519.47689.c4. [DOI] [PubMed] [Google Scholar]
- 30.Manconi M, Fabbrini M, Bonanni E, et al. High prevalence of restless legs syndrome in multiple sclerosis. Eur J Neurol. 2007;14:534–9. doi: 10.1111/j.1468-1331.2007.01740.x. [DOI] [PubMed] [Google Scholar]
- 31.Ajayi OF, Chang-McDowell T, Culpepper WJ, III, Royal W, Bever CT. High prevalence of sleep disorders in veterans with multiple sclerosis. Neurology. 2008;50:P06–141. [Google Scholar]
- 32.Clemens S, Rye D, Hochman S. Restless legs syndrome: revisiting the dopamine hypothesis from the spinal cord perspective. Neurology. 2006;67:125–30. doi: 10.1212/01.wnl.0000223316.53428.c9. [DOI] [PubMed] [Google Scholar]
- 33.Frauscher B, Loscher W, Hogl B, Poewe W, Kofler M. Auditory startle reaction is disinhibited in idiopathic restless legs syndrome. Sleep. 2007;30:489–93. doi: 10.1093/sleep/30.4.489. [DOI] [PubMed] [Google Scholar]
- 34.Manconi M, Rocca MA, Ferini-Strambi L, et al. Restless legs syndrome is a common finding in multiple sclerosis and correlates with cervical cord damage. Mult Scler. 2008;14:86–93. doi: 10.1177/1352458507080734. [DOI] [PubMed] [Google Scholar]
- 35.Wunderlin B. Fatigue in multiple sclerosis is not due to sleep apnoea. Eur J Neurol. 1997;4:72–78. doi: 10.1111/j.1468-1331.1997.tb00302.x. [DOI] [PubMed] [Google Scholar]
- 36.Kaynak H, Altintas A, Kaynak D, et al. Fatigue and sleep disturbance in multiple sclerosis. Eur J Neurol. 2006;13:1333–9. doi: 10.1111/j.1468-1331.2006.01499.x. [DOI] [PubMed] [Google Scholar]
- 37.Trojan DA, Da Costa D, Bar-Or A, et al. Sleep abnormalities in multiple sclerosis patients. Mult Scler. 2008;14:S160. [Google Scholar]
- 38.Auer RN, Rowlands CG, Perry SF, Remmers JE. Multiple sclerosis with medullary plaques and fatal sleep apnea (Ondine's curse) Clin Neuropathol. 1996;15:101–5. [PubMed] [Google Scholar]
- 39.Tachibana N, Howard RS, Hirsch NP, Miller DH, Moseley IF, Fish D. Sleep problems in multiple sclerosis. Eur Neurol. 1994;34:320–3. doi: 10.1159/000117070. [DOI] [PubMed] [Google Scholar]
- 40.Amarenco G, Kerdraon J, Denys P. [Bladder and sphincter disorders in multiple sclerosis. Clinical, urodynamic and neurophysiological study of 225 cases] Rev Neurol (Paris) 1995;151:722–30. [PubMed] [Google Scholar]
- 41.Rae-Grant AD, Eckert NJ, Bartz S, Reed JF. Sensory symptoms of multiple sclerosis: a hidden reservoir of morbidity. Mult Scler. 1999;5:179–83. doi: 10.1177/135245859900500307. [DOI] [PubMed] [Google Scholar]
- 42.Merlino G, Fratticci L, Lenchig C, et al. Prevalence of ‘poor sleep' among patients with multiple sclerosis: an independent predictor of mental and physical status. Sleep Med. 2009;10:26–34. doi: 10.1016/j.sleep.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 43.Chesson A, Jr, Hartse K, Anderson WM, et al. Practice parameters for the evaluation of chronic insomnia. An American Academy of Sleep Medicine report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep. 2000;23:237–41. [PubMed] [Google Scholar]
- 44.Attarian HP, Brown KM, Duntley SP, Carter JD, Cross AH. The relationship of sleep disturbances and fatigue in multiple sclerosis. Arch Neurol. 2004;61:525–8. doi: 10.1001/archneur.61.4.525. [DOI] [PubMed] [Google Scholar]
- 45.Figved N, Klevan G, Myhr KM, et al. Neuropsychiatric symptoms in patients with multiple sclerosis. Acta Psychiatr Scand. 2005;112:463–8. doi: 10.1111/j.1600-0447.2005.00624.x. [DOI] [PubMed] [Google Scholar]
- 46.Scott TF, Allen D, Price TR, McConnell H, Lang D. Characterization of major depression symptoms in multiple sclerosis patients. J Neuropsychiatry Clin Neurosci. 1996;8:318–23. doi: 10.1176/jnp.8.3.318. [DOI] [PubMed] [Google Scholar]
- 47.Patrick E, Christodoulou C, Krupp LB. Longitudinal correlates of fatigue in multiple sclerosis. Mult Scler. 2009;15:258–61. doi: 10.1177/1352458508097466. [DOI] [PubMed] [Google Scholar]
- 48.Flachenecker P, Kumpfel T, Kallmann B, et al. Fatigue in multiple sclerosis: a comparison of different rating scales and correlation to clinical parameters. Mult Scler. 2002;8:523–6. doi: 10.1191/1352458502ms839oa. [DOI] [PubMed] [Google Scholar]
- 49.Kroencke DC, Lynch SG, Denney DR. Fatigue in multiple sclerosis: relationship to depression, disability, and disease pattern. Mult Scler. 2000;6:131–6. doi: 10.1177/135245850000600213. [DOI] [PubMed] [Google Scholar]
- 50.Iriarte J, Subira ML, Castro P. Modalities of fatigue in multiple sclerosis: correlation with clinical and biological factors. Mult Scler. 2000;6:124–30. doi: 10.1177/135245850000600212. [DOI] [PubMed] [Google Scholar]
- 51.Tellez N, Rio J, Tintore M, Nos C, Galan I, Montalban X. Does the Modified Fatigue Impact Scale offer a more comprehensive assessment of fatigue in MS? Mult Scler. 2005;11:198–202. doi: 10.1191/1352458505ms1148oa. [DOI] [PubMed] [Google Scholar]
- 52.Bakshi R, Shaikh ZA, Miletich RS, et al. Fatigue in multiple sclerosis and its relationship to depression and neurologic disability. Mult Scler. 2000;6:181–5. doi: 10.1177/135245850000600308. [DOI] [PubMed] [Google Scholar]
- 53.Hadjimichael O, Vollmer T, Oleen-Burkey M. Fatigue characteristics in multiple sclerosis: the North American Research Committee on Multiple Sclerosis (NARCOMS) survey. Health Qual Life Outcomes. 2008;6:100. doi: 10.1186/1477-7525-6-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dittner AJ, Wessely SC, Brown RG. The assessment of fatigue: a practical guide for clinicians and researchers. J Psychosom Res. 2004;56:157–70. doi: 10.1016/S0022-3999(03)00371-4. [DOI] [PubMed] [Google Scholar]
- 55.Chalder T, Berelowitz G, Pawlikowska T, et al. Development of a fatigue scale. J Psychosom Res. 1993;37:147–53. doi: 10.1016/0022-3999(93)90081-p. [DOI] [PubMed] [Google Scholar]
- 56.van Kessel K, Moss-Morris R, Willoughby E, Chalder T, Johnson MH, Robinson E. A randomized controlled trial of cognitive behavior therapy for multiple sclerosis fatigue. Psychosom Med. 2008;70:205–13. doi: 10.1097/PSY.0b013e3181643065. [DOI] [PubMed] [Google Scholar]
- 57.Wade DT, Young CA, Chaudhuri KR, Davidson DL. A randomised placebo controlled exploratory study of vitamin B-12, lofepramine, and L-phenylalanine (the “Cari Loder regime”) in the treatment of multiple sclerosis. J Neurol Neurosurg Psychiatry. 2002;73:246–9. doi: 10.1136/jnnp.73.3.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–3. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 59.Fisk JD, Pontefract A, Ritvo PG, Archibald CJ, Murray TJ. The impact of fatigue on patients with multiple sclerosis. Can J Neurol Sci. 1994;21:9–14. [PubMed] [Google Scholar]
- 60.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 61.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 62.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 63.Nieves J, Cosman F, Herbert J, Shen V, Lindsay R. High prevalence of vitamin D deficiency and reduced bone mass in multiple sclerosis. Neurology. 1994;44:1687–92. doi: 10.1212/wnl.44.9.1687. [DOI] [PubMed] [Google Scholar]
- 64.Ruiz-Irastorza G, Egurbide MV, Olivares N, Martinez-Berriotxoa A, Aguirre C. Vitamin D deficiency in systemic lupus erythematosus: prevalence, predictors and clinical consequences. Rheumatology (Oxford) 2008;47:920–3. doi: 10.1093/rheumatology/ken121. [DOI] [PubMed] [Google Scholar]
- 65.Glerup H, Mikkelsen K, Poulsen L, et al. Hypovitaminosis D myopathy without biochemical signs of osteomalacic bone involvement. Calcif Tissue Int. 2000;66:419–24. doi: 10.1007/s002230010085. [DOI] [PubMed] [Google Scholar]
- 66.Boland R. Role of vitamin D in skeletal muscle function. Endocr Rev. 1986;7:434–48. doi: 10.1210/edrv-7-4-434. [DOI] [PubMed] [Google Scholar]
- 67.Cohen RA, Fisher M. Amantadine treatment of fatigue associated with multiple sclerosis. Arch Neurol. 1989;46:676–80. doi: 10.1001/archneur.1989.00520420096030. [DOI] [PubMed] [Google Scholar]
- 68.Taus C, Giuliani G, Pucci E, D'Amico R, Solari A. Cochrane Database Syst Rev. 2003. Amantadine for fatigue in multiple sclerosis; p. CD002818. [DOI] [PubMed] [Google Scholar]
- 69.Weinshenker BG, Penman M, Bass B, Ebers GC, Rice GP. A double-blind, randomized, crossover trial of pemoline in fatigue associated with multiple sclerosis. Neurology. 1992;42:1468–71. doi: 10.1212/wnl.42.8.1468. [DOI] [PubMed] [Google Scholar]
- 70.Krupp LB, Coyle PK, Doscher C, et al. Fatigue therapy in multiple sclerosis: results of a double-blind, randomized, parallel trial of amantadine, pemoline, and placebo. Neurology. 1995;45:1956–61. doi: 10.1212/wnl.45.11.1956. [DOI] [PubMed] [Google Scholar]
- 71.Rammohan KW, Rosenberg JH, Lynn DJ, Blumenfeld AM, Pollak CP, Nagaraja HN. Efficacy and safety of modafinil (Provigil) for the treatment of fatigue in multiple sclerosis: a two centre phase 2 study. J Neurol Neurosurg Psychiatry. 2002;72:179–83. doi: 10.1136/jnnp.72.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stankoff B, Waubant E, Confavreux C, et al. Modafinil for fatigue in MS: a randomized placebo-controlled double-blind study. Neurology. 2005;64:1139–43. doi: 10.1212/01.WNL.0000158272.27070.6A. [DOI] [PubMed] [Google Scholar]
- 73.Di Fabio RP, Soderberg J, Choi T, Hansen CR, Schapiro RT. Extended outpatient rehabilitation: its influence on symptom frequency, fatigue, and functional status for persons with progressive multiple sclerosis. Arch Phys Med Rehabil. 1998;79:141–6. doi: 10.1016/s0003-9993(98)90290-8. [DOI] [PubMed] [Google Scholar]
- 74.Mostert S, Kesselring J. Effects of a short-term exercise training program on aerobic fitness, fatigue, health perception and activity level of subjects with multiple sclerosis. Mult Scler. 2002;8:161–8. doi: 10.1191/1352458502ms779oa. [DOI] [PubMed] [Google Scholar]
- 75.Roehrs T, Karst G. Effects of an aquatics exercise program on quality of life measures for individuals with progressive multiple sclerosis. J Neurol Phys Ther. 2004;28:63–71. [Google Scholar]
- 76.Smith C, Hale L, Olson K, Schneiders AG. Disabil Rehabil. 2008. How does exercise influence fatigue in people with multiple sclerosis? pp. 1–8. [DOI] [PubMed] [Google Scholar]
- 77.Schwid SR, Petrie MD, Murray R, et al. A randomized controlled study of the acute and chronic effects of cooling therapy for MS. Neurology. 2003;60:1955–60. doi: 10.1212/01.wnl.0000070183.30517.2f. [DOI] [PubMed] [Google Scholar]