Abstract
Study Objectives:
To explore differences in craniofacial structures and obesity between Caucasian and Chinese patients with obstructive sleep apnea (OSA).
Design:
Inter-ethnic comparison study.
Setting:
Two sleep disorder clinics in Australia and Hong Kong.
Patients:
150 patients with OSA (74 Caucasian, 76 Chinese).
Interventions:
Anthropometry, cephalometry, and polysomnography were performed and compared. Subgroup analyses after matching for: (1) body mass index (BMI); (2) OSA severity.
Measurements and Results:
The mean age and BMI were similar between the ethnic groups. Chinese patients had more severe OSA (AHI 35.3 vs 25.2 events/h, P = 0.005). They also had more craniofacial bony restriction, including a shorter cranial base (63.6 ± 3.3 vs 77.5 ± 6.7 mm, P < 0.001), maxilla (50.7 ± 3.7 vs 58.8 ± 4.3 mm, P < 0.001) and mandible length (65.4 ± 4.2 vs 77.9 ± 9.4 mm, P < 0.001). These findings remained after correction for differences in body height. Similar results were shown in the BMI-matched analysis (n = 66). When matched for OSA severity (n = 52), Chinese patients had more craniofacial bony restriction, but Caucasian patients were more overweight (BMI 30.7 vs 28.4 kg/m2, P = 0.03) and had a larger neck circumference (40.8 vs 39.1 cm, P = 0.004); however, the ratios of BMI to the mandible or maxilla size were similar.
Conclusions:
Craniofacial factors and obesity contribute differentially to OSA in Caucasian and Chinese patients. For the same degree of OSA severity, Caucasians were more overweight, whereas Chinese exhibited more craniofacial bony restriction.
Citation:
Lee RWW; Vasudavan S; Hui DS; Prvan T; Petocz P; Darendeliler MA; Cistulli PA. Differences in craniofacial structures and obesity in Caucasian and Chinese patients with obstructive sleep apnea. SLEEP 2010;33(8):1075-1080.
Keywords: Obstructive sleep apnea, ethnicity, craniofacial, obesity
OBSTRUCTIVE SLEEP APNEA (OSA) IS A COMMON DISORDER IN WHICH RECURRENT SLEEP RELATED UPPER AIRWAY OBSTRUCTION CAUSES SLEEP fragmentation and intermittent hypoxemia. Ethnicity has been suggested as an important risk factor for OSA. However, defining the role of ethnicity is complex, as it incorporates genetic, environmental, and cultural factors that can, individually or in combination, influence the other recognized risk factors for OSA. Whilst earlier prevalence studies suggest that OSA may be more common in certain ethnic groups,1,2 recent data in Hong Kong Chinese,3 Indians4 and Koreans5 suggest that OSA prevalence in these ethnic groups are not dissimilar to the Caucasian populations.6
Obesity and craniofacial factors are well recognized in the pathogenesis of OSA. It is also becoming clear that the balance and interaction between these two risk factors is crucial in the development of OSA.7,8 It is likely that such interaction is strongly influenced by ethnicity. Cephalometric studies have suggested that craniofacial factors are important determinants of OSA risk in Asian cohorts.9–11 Similarly, studies evaluating the role of obesity suggest that whilst it is a consistent risk factor for OSA across ethnic groups, the risk attributable to obesity differs between racial groups.3,6 Despite suffering from a similar degree of OSA, patients from Asian groups are generally less overweight compared to their Caucasian counterparts, suggesting that ethnicity may differentially influence the attribution of these OSA risk factors. To date, studies that have explored these complex interactions remain limited, especially in a direct inter-ethnic comparison. Hence the aim of this study was to explore the differences in craniofacial structures and obesity between Caucasian and Chinese patients with OSA.
MATERIALS AND METHODS
Subjects
Patients in both ethnic groups were referred initially for the investigation of symptoms suggestive of OSA (snoring, daytime sleepiness, and/or witnessed apneas) in specialist sleep disorders clinics. The Caucasian subjects were OSA patients recruited from a tertiary referral sleep disorders center in Australia. This center has a longstanding strong clinical and research interest in oral appliance therapy, and offers this treatment as a first-line alternative to other treatment modalities for OSA. The patients were recruited on the basis of having had cephalometry performed as part of the routine clinical assessment for oral appliance therapy. The Chinese patients were recruited from a center in Hong Kong, and were part of a previous cephalometric study.12 Ethnicity was determined by self-report and was confirmed by the study investigators. All patients had OSA as determined by polysomnography (apnea-hypopnea Index [AHI] ≥ 5 /h).
Polysomnography
Diagnostic polysomnography (PSG) was performed in accordance with previous studies and recommendations.13,14 Sleep staging was determined using standardized definitions.15 Respiratory variables included chest wall and abdominal movement, diaphragm EMG, nasal airflow and pressure, and oxygen saturation by pulse oximetry. Definitions of all scored events were consistent at both study sites. Apnea was defined as a cessation of breathing during sleep ≥ 10 sec, with oxygen desaturation > 3% and/or associated with an arousal. Hypopnea was defined as ≥ 50% reduction in airflow, associated with an arousal and/or 3% reduction in blood oxygen saturation, lasting ≥ 10 sec. The AHI was calculated as the average number of episodes of apnea plus hypopnea per hour of sleep. Minimum oxygen saturation (MinSaO2) was also measured. Scoring was performed by experienced sleep technologists.
Cephalometric Examinations
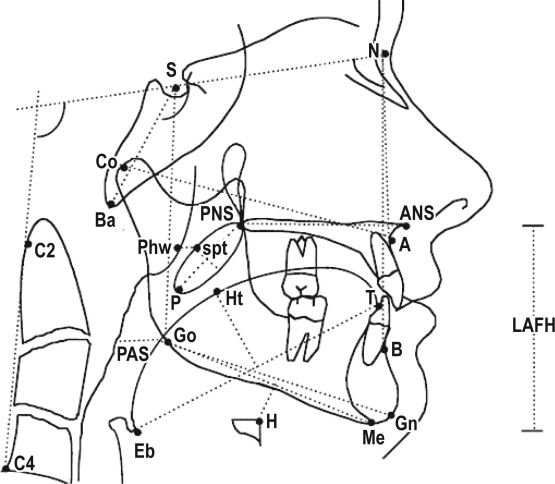
A lateral cephalometric radiograph was taken for each subject at both sites, according to previously described methods.16 Radiographs were taken at end-expiration, with the head in the natural position. This was achieved by asking the subjects to look into their own pupils reflected in a mirror located at eye level. Cephalometric analysis was performed in a standardized fashion to examine anatomical variables previously used for OSA investigation.13 The landmarks and measurements obtained are shown in Figure 1. All cephalograms were hand traced by a single investigator (SV). Where a bilateral landmark presented as 2 images, the average of the 2 was used, with a template of the bilateral structures employed to ensure accurate reproduction. The cephalograms were scanned and digitized using custom analysis software (Dolphin Imaging Program, Premium Version 10.0 CA, USA). The mean enlargement factor for the cephalograms was 11% for the Caucasian group and 13% for the Chinese group. While this did not affect the angular measurements, the linear measurements were transformed by the respective enlargement factors using the imaging software to allow direct comparison.
Figure 1.
Definitions of cephalometric landmarks and measurements
Anatomical Landmarks: ANS (Anterior nasal spine)—tip of the median sharp bony process of the palatine bone in the hard palate. A Point—deepest midline point on the maxillary alveolus between ANS and the maxillary alveolar crest. B Point—deepest midline point between the mandibular alveolar crest and the gnathion. Ba (Basion)—most inferior point on the anterior margin of the foramen magnum in the median plane. Go (Gonion)—most lateral external point at the junction of the horizontal and ascending rami of the mandible. Gn (Gnathion)—most antero-inferior point on the bony mandibular symphysis. H (Hyoidale)—most antero-superior point on the body of the hyoid bone. Me (Mentum)—lowest point on the bony outline of the mandibular symphysis. MP (Mandibular plane)—line joining Me and Go. N (Nasion)—most anterior point of the fronto-nasal suture. PNS (Posterior nasal spine)—tip of the posterior spine of the palatine bone of the hard palate. spt (soft palate tangent)—tangent point on a line parallel to the long axis of the soft palate at the maximum width. Phw (Posterior pharyngeal wall)—point on the posterior pharyngeal wall at the same horizontal level as spt. S (Sella)—the center of the sella turcica. Bony Dimensions: SN—anterior cranial base length. LAFH-—lower anterior face height (ANS-Me). AFH—anterior face height (N-Me). PFH—posterior face height (S-Go). Go-Me—mandibular length. ANS-PNS—maxillary length. Co-A—midface length. Overjet—horizontal distance between the upper and lower central incisors measured parallel to the occlusal plane. It is measured from the labioincisal edge of one upper central incisor to the labial surface of the corresponding lower central incisor with the upper and lower teeth in centric occlusion. Overbite—vertical distance between the incisal edge of the upper central incisor and the incisal edge of the lower central incisor. MP-H—perpendicular distance from the MP to H. Soft Tissue Dimensions: RPAS—width of nasopharynx (Phw-spt). PAS—distance between the posterior pharyngeal wall and the dorsal surface of the base of the tongue, measured on the line that intersects Go and B point. PNS-P—posterior nasal spine to the tip of the soft palate. Mx Soft Palate—maximal soft palate thickness. Tongue Length—length of the tongue. Tongue Height—maximal height of the tongue. Angular Measurements: BaSN—cranial base angulation in the mid-sagittal plane. SNA—angle from S to N to A Point. SNB—angle from S to N to B Point. ANB—angle from A Point to N to B Point. Y-Axis—facial axis (GnSN). Gonial Angle—angle formed by the posterior border of the mandible and the mandibular plane. CVT-SN—angulation of the cervical spine (C2-C4) with the cranial base (SN). SN-PP—angulation of the cranial base (SN) with the palatal plane. SN-OP—angulation of the cranial base (SN) with the occlusal plane. SN-MP—angulation of the cranial base (SN) with the mandibular plane. PP-MP—angulation of the palatal plane with the mandibular plane.
Measurement error was assessed in 20 randomly selected patients from both groups, whose radiographs were re-traced, re-digitized, and re-measured by the same examiner under the same conditions one month later. The coefficient of variation was calculated.
Anthropometric Measurements
The anthropometric measurements of obesity included neck circumference (cm), height (m) and weight (kg), enabling calculation of the body mass index (BMI) (kg/m2).
Statistical Analyses
Data were analyzed using a statistical package (SPSS for Windows Versions 14, Chicago IL, USA). Comparisons of the cephalometric, anthropometric, and polysomnographic data between 2 ethnic groups were performed using the unpaired t-tests. In addition, subgroup analyses with 2 separate matching procedures were performed from the recruited Caucasian and Chinese patients: (1) matched for BMI [ ± 1 kg/m2]; (2) matched for OSA severity (AHI [ ± 10 events/h] and MinSaO2 [± 10%]). These were performed by selecting pairs of patients, one from each ethnic group, with similar BMI or OSA severity, within the ranges described above. This allowed comparison of subgroups of Caucasian and Chinese patients that did not differ in overall BMI or OSA severity, while still maintaining a reasonable subgroup sample size after the matching. Allowing for the multiple comparisons, a P-value of less than 0.002 was considered significant for the cephalometric measurements (Bonferroni adjustment for 27 variables). For P-values between 0.002 and 0.005, these were considered marginally significant. Comparisons between bony and soft tissue dimensions were also made after correction of per meter of subject body height. Regression modeling was also performed on the entire sample of 150 patients. The natural logarithm of AHI [lnAHI] was used as the response variable, since the transformed values allowed the regression assumptions to be better satisfied. Variables examined included 27 cephalometric measurements, age, BMI, neck circumference, and ethnicity. Initial analysis involved constructing a multiple linear regression model using a stepwise approach to select potential explanatory variables for AHI. Subsequent exploratory analysis involved plotting lnAHI against each of the potential predictors, with ethnicity as a grouping variable, to identify significant two-way interactions between ethnicity and the cephalometric or obesity variables. Finally, linear models were constructed including ethnicity and its interactions in order to examine the differential impact of the 2 ethnic groups on OSA severity.
RESULTS
One hundred fifty patients with OSA (74 Caucasian, 76 Hong Kong Chinese) were recruited for this study. Baseline characteristics of the comparison groups are presented in Table 1. The two ethnic groups had similar mean age, gender proportions, neck circumference and BMI, but the Chinese patients had more severe OSA (mean AHI 35.3 ± 26.1 vs 25.2 ± 16.3 events/hr, P = 0.005; MinSaO2 75.5 ± 14.7 vs 85.3 ± 6.2%, P < 0.001). The Chinese patients also had more craniofacial bony restriction (Table 1). Specifically, they had a shorter cranial base [SN] (63.6 ± 3.3 vs 77.5 ± 6.7 mm, P < 0.001), midface length [Co-A] (82.7 ± 4.7 vs 96.2 ± 8.0 mm, P < 0.001), maxilla [ANS-PNS] (50.7 ± 3.7 vs 58.8 ± 4.3 mm, P < 0.001) and mandible [Go-Me] (65.4 ± 4.2 vs 77.9 ± 9.4 mm, P < 0.001). These cephalometric measurements remained shorter in the Chinese patients after correction for differences in body height. The hyoid position appeared lower relative to the mandibular plane [MP-H] in the Caucasian patients (22.4 ± 6.7 vs 19.0 ± 6.0 mm, P = 0.001), but this difference was no longer significant when corrected for body height. Other cephalometric skeletal differences are summarized in Table 1; these include a greater SNA, ANB, Y-Axis and SN-PP angle, and a smaller gonial angle in the Chinese patients. The Chinese patients had a relatively smaller airway space (PAS), and their soft palate and tongue size were also smaller (Table 1).
Table 1.
Baseline patient demographics and cephalometric characteristics
| Caucasian (n = 74) | Chinese (n = 76) | Mean difference | P value | ||||
|---|---|---|---|---|---|---|---|
| Age (years) | 48.5 ± 11.0 | 49.5 ± 11.0 | - | NS | |||
| Gender (% male) | 79.7 | 82.9 | - | NS | |||
| Neck circumference (cm) | 40.9 ± 3.4 | 40.1 ± 3.5 | 0.7 ± 0.6 | NS | |||
| Weight (kg) | 92.9 ± 17.0 | 80.1 ± 16.4 | 12.8 ± 2.7 | < 0.001 | |||
| Height (m) | 1.74 ± 0.08 | 1.64 ± 0.08 | 0.10 ± 0.01 | < 0.001 | |||
| BMI (kg/m2) | 30.8 ± 5.7 | 29.7 ± 5.2 | 1.0 ± 0.9 | NS | |||
| AHI (events/hour) | 25.2 ± 16.3 | 35.3 ± 26.1 | −10.1 ± 3.6 | 0.005 | |||
| MinSaO2(%) | 85.3 ± 6.2 | 75.5 ± 14.7 | 9.7 ± 1.9 | < 0.001 | |||
| Cephalometric bony dimensions (mm) | |||||||
| SN* | 77.5 ± 6.7 | 63.6 ± 3.3 | 13.9 ± 0.9 | < 0.001 | |||
| LAFH | 75.1 ± 8.8 | 70.8 ± 5.5 | 4.3 ± 1.2 | 0.001 | |||
| AFH | 131.7 ± 12.3 | 122.3 ± 7.1 | 9.4 ± 1.6 | < 0.001 | |||
| PFH | 87.3 ± 9.9 | 84.3 ± 6.5 | 3.0 ± 1.4 | NS | |||
| Go-Me* | 77.9 ± 9.4 | 65.4 ± 4.2 | 12.4 ± 1.2 | < 0.001 | |||
| ANS-PNS* | 58.8 ± 4.3 | 50.7 ± 3.7 | 8.2 ± 0.7 | < 0.001 | |||
| Co-A* | 96.2 ± 8.0 | 82.7 ± 4.7 | 13.4 ± 1.1 | < 0.001 | |||
| Overbite† | 2.6 ± 3.6 | 0.9 ± 2.8 | 1.7 ± 0.5 | 0.002 | |||
| Overjet | 4.2 ± 2.4 | 3.9 ± 2.4 | 0.3 ± 0.4 | NS | |||
| MP-H | 22.4 ± 6.7 | 19.0 ± 6.0 | 3.5 ± 1.0 | 0.001 | |||
| Cephalometric soft tissue dimensions (mm) | |||||||
| RPAS | 10.6 ± 4.0 | 8.8 ± 2.6 | 1.8 ± 0.5 | 0.002 | |||
| PAS† | 10.8 ± 4.5 | 8.2 ± 3.6 | 2.6 ± 0.7 | < 0.001 | |||
| PNS-P* | 40.0 ± 4.3 | 33.8 ± 4.8 | 6.2 ± 0.7 | < 0.001 | |||
| Mx Soft palate* | 11.4 ± 1.8 | 9.6 ± 1.5 | 1.8 ± 0.3 | < 0.001 | |||
| Tongue length* | 89.4 ± 7.6 | 67.3 ± 11.2 | 22.1 ± 1.6 | < 0.001 | |||
| Tongue height* | 40.0 ± 5.0 | 31.3 ± 4.3 | 8.7 ± 0.8 | < 0.001 | |||
| Cephalometric angular measurements (°) | |||||||
| BaSN | 126.7 ± 5.9 | 128.2 ± 6.1 | −1.5 ± 1.0 | NS | |||
| SNA | 82.3 ± 3.3 | 84.5 ± 4.6 | −2.2 ± 0.7 | 0.001 | |||
| SNB | 79.3 ± 3.6 | 79.5 ± 4.5 | −0.2 ± 0.7 | NS | |||
| ANB | 3.0 ± 3.3 | 5.1 ± 3.2 | −2.1 ± 0.5 | < 0.001 | |||
| Y-Axis | 67.1 ± 4.6 | 71.6 ± 4.8 | −4.4 ± 0.8 | < 0.001 | |||
| Gonial angle | 126.5 ± 6.0 | 120.6 ± 8.2 | 5.9 ± 1.2 | 0.002 | |||
| CVT-SN | 108.7 ± 7.8 | 111.6 ± 8.7 | −3.0 ± 1.3 | NS | |||
| SN-PP | 8.3 ± 3.8 | 10.2 ± 4.6 | −1.9 ± 0.7 | NS | |||
| SN-OP | 14.5 ± 9.5 | 18.3 ± 10.9 | −3.8 ± 1.7 | NS | |||
| SN-MP | 30.8 ± 7.0 | 30.6 ± 7.5 | 0.1 ± 1.2 | NS | |||
| PP-MP | 25.1 ± 6.7 | 24.0 ± 6.6 | 1.1 ± 1.1 | NS | |||
See Figure 1 for definitions of measurements. Data are presented as mean ± SD. Mean difference values are presented as mean ± SE.
BMI, Body mass index; AHI, apnea-hypopnea index; MinSaO2, minimum oxygen saturation; NS, non-significant. Measurements remained significantly shorter
(P < 0.001,
P < 0.01) in Chinese patients after the correction of per meter of body height.
In the BMI-matched subgroup analysis, 66 pairs of Caucasian and Chinese patients were compared. The mean BMI was 29.7 ± 4.7 kg/m2 in the Caucasians and 29.6 ± 4.6 kg/m2 in the Chinese patients. There were equal numbers of males in each group. Similar to the comparison with the entire patient cohort, the Chinese patients continued to have more severe OSA when matched for BMI (mean AHI 33.8 ± 24.5 vs 24.9 ± 15.8 events/h, P = 0.02; MinSaO2 76.2 ± 13.7 vs 85.3 ± 6.3%, P < 0.001). They also had more craniofacial bony restriction for the same degree of obesity (data not shown).
In the OSA severity-matched subgroup analysis, 52 pairs of Caucasian and Chinese patients were compared (Table 2). The mean AHI and MinSaO2 were similar between the 2 ethnic groups. When matched for OSA severity, the Caucasians were more overweight (BMI 30.7 ± 57 kg/m2 vs 28.4 ± 4.3 kg/m2, P = 0.03) and had larger neck circumference (40.8 ± 3.5 cm vs 39.1 ± 2.6 cm, P = 0.004). The Chinese patients had more craniofacial bony restriction (shorter cranial base, midface length, maxilla and mandible, etc.), a smaller airway space (PAS), and smaller soft palate and tongue size (Table 2). When comparing the ratio of the BMI to the height-adjusted mandible size (BMI: Go-Me/Height) or maxilla size (BMI: ANS-PNS/height), there was no difference between Caucasians and the OSA severity matched Chinese patients (Table 2).
Table 2.
Subgroup analysis after matching for OSA severity (AHI and MinSaO2)
| Caucasian (n = 52) | Chinese (n = 52) | P value | ||||
|---|---|---|---|---|---|---|
| AHI (events/hour) | 23.4 ± 14.4 | 23.5 ± 17.3 | - | |||
| MinSaO2 (%) | 84.5 ± 6.2 | 83.3 ± 6.7 | - | |||
| Age (years) | 47.8 ± 11.0 | 50.5 ± 11.1 | NS | |||
| Gender (% male) | 78.8% | 78.8% | NS | |||
| Neck circumference (cm) | 40.8 ± 3.5 | 39.1 ± 2.6 | 0.004 | |||
| Weight (kg) | 92.0 ± 16.8 | 75.0 ± 12.4 | < 0.001 | |||
| Height (m) | 1.73 ± 0.09 | 1.63 ± 0.08 | < 0.001 | |||
| BMI (kg/m2) | 30.7 ± 5.7 | 28.4 ± 4.3 | 0.03 | |||
| Cephalometric measurements§ | ||||||
| SN / height* | 44.2 ± 2.6 | 39.2 ± 2.6 | < 0.001 | |||
| Go-Me / height* | 44.4 ± 3.6 | 40.3 ± 3.0 | < 0.001 | |||
| ANS-PNS / height* | 33.6 ± 2.4 | 31.2 ± 2.5 | < 0.001 | |||
| Co-A / height* | 55.0 ± 3.7 | 51.2 ± 2.9 | < 0.001 | |||
| MPH / height* | 12.6 ± 2.7 | 11.2 ± 3.5 | NS | |||
| PAS / height* | 6.5 ± 2.6 | 4.5 ± 1.6 | < 0.001 | |||
| PNS-P / height* | 23.2 ± 2.7 | 20.2 ± 2.8 | < 0.001 | |||
| Mx soft palate / height* | 6.6 ± 1.0 | 5.8 ± 0.9 | < 0.001 | |||
| Tongue length / height* | 51.4 ± 4.2 | 40.2 ± 6.9 | < 0.001 | |||
| Tongue height / height* | 23.1 ± 2.7 | 19.1 ± 2.5 | < 0.001 | |||
| SNA† | 82.7 ± 3.2 | 85.3 ± 4.3 | 0.001 | |||
| ANB† | 3.1 ± 3.0 | 5.4 ± 2.7 | < 0.001 | |||
| Y-axis† | 66.8 ± 4.8 | 71.1 ± 4.8 | < 0.001 | |||
| Gonial angle† | 126.3 ± 5.7 | 120.9 ± 8.2 | < 0.001 | |||
| Ratios of obesity to mandibular and maxillary dimensions | ||||||
| BMI : Go-Me/height | 0.91 ± 0.17 | 0.91 ± 0.14 | NS | |||
| BMI : ANS-PNS/height | 0.69 ± 0.12 | 0.71 ± 0.11 | NS | |||
See Figure 1 for definitions of measurements. All data are presented as mean ± SD. NS – non-significant.
Cephalometric measurements that were significantly different are shown.
Dimensions adjusted for body height (mm/meter).
Angular measurements in degrees.
The explanatory model for OSA severity was developed using the entire cohort of 150 patients and it can be described by the following equations (developed from the one model, containing significant terms for interaction of ethnicity with BMI, SN-OP, and PNS-P):
Caucasian
lnAHI = 2.61 – 0.050*Co-A + 0.045*ANS-PNS + 0.028*PFH + 0.011*BMI – 0.0022*SN-OP – 0.0035*PNS-P.
Chinese
lnAHI = 0.50 – 0.050*Co-A + 0.045*ANS-PNS + 0.028*PFH + 0.041*BMI + 0.012*SN-OP + 0.024*PNS-P.
This model suggests that Co-A, ANS-PNS, PFH, and BMI were independent predictors for OSA severity in both Caucasian and Chinese. However, a one-unit increase in BMI resulted in a larger positive contribution to lnAHI for the Chinese patients (coefficient for BMI was 0.041 compared to 0.011 for Caucasians). The SN-OP and PNS-P also contributed positively to OSA severity in the Chinese, but not in the Caucasians. Overall, the model had an adjusted r2 of 0.39.
The coefficient of variation was < 5% for all the cephalometric variables on repeated measures in a subset of patients.
DISCUSSION
This study aimed to explore the differences in craniofacial structures and obesity as risk factors for OSA in Caucasian and Chinese patients. We found that craniofacial structures and obesity contributed differentially to OSA in these two ethnic groups. For the same degree of obesity, Chinese patients had more severe OSA and more craniofacial bony restriction. When OSA severity was similar, Caucasian patients were more overweight and had larger neck circumference, whereas the Chinese patients exhibited more craniofacial bony restriction.
Epidemiological evidence strongly supports obesity as being one of the most important risk factors for OSA across many ethnic groups.3,4,6 Despite similar disease prevalence, Chinese are less obese compared to communities from Australia and the United States.3,6,17–19 Our data demonstrated that on average Chinese patients with OSA had a BMI 2.3 kg/m2 (∼7.5%) lower than Caucasians with the same degree of OSA severity. When BMI was similar, however, Chinese patients had a mean AHI higher by 8.9 events/h in our cohorts and suffered from more severe oxygen desaturation. These findings are consistent with data from other inter-ethnic studies.19,20 Furthermore, our data also suggest that for every unit of BMI increment, it results in a greater increase in OSA severity in the Chinese. These results suggest that the impact of obesity on OSA is greater in the Chinese populations. However, epidemiological data indicate that the odds of having OSA for each standard deviation of BMI increment is in fact lower in Chinese patients compared to the Wisconsin cohort (odds ratio 2.42 versus 4.19).3,6 Therefore, at a population level, the risk of OSA attributable to obesity seems lower in Chinese patients, likely due to the lower prevalence of higher BMI levels. While in clinical OSA cohorts such as in this study, with higher prevalence of obesity and craniofacial bony restriction, the impact of BMI on OSA severity seems more pronounced in Chinese patients.
It has also been postulated that craniofacial factors, pharyngeal narrowing, and collapsibility assume greater pathogenic significance in Chinese subjects.3,21 In our study, Chinese patients clearly had evidence of craniofacial bony restriction that is more marked compared to Caucasians. Most importantly, this is taking into account differences in body height, unlike previous inter-ethnic comparison studies.10,19 The findings include maxillary and mandibular restriction, shorter midface and cranial base, in addition to a smaller airway space. Overall, while these findings have been reported in cephalometric studies within various ethnic groups,12,22–24 comparative studies between Caucasian and Chinese patients remain very limited. Our study further explored the impact of ethnicity on OSA severity with statistical modeling. Similar to many previous cephalometric studies in OSA,24–26 craniofacial structures and BMI were independent predictors of OSA severity in both ethnic groups. But in the Chinese patients, the soft palate length (PNS-P) and the angulation between the cranial base with the occlusal plane (SN-OP) had additional positive contribution to OSA severity. The former suggests that upper airway soft tissues may contribute to airway collapse more so in Chinese patients, especially in the presence of craniofacial bony restriction. The higher SN-OP could reflect a steeper cranial base, which is seen in Chinese patients with OSA.10
The balance between the relative size of the craniofacial bony compartment and the amount of upper airway soft tissue or degree of obesity is an important determinant of upper airway size and OSA risk.7,8,25 This concept is supported by our finding of the similar ratios of obesity to mandibular and maxillary dimensions in the OSA severity- matched Caucasian and Chinese patients. This anatomical balance model also explains the greater impact of obesity on OSA severity in Chinese patients who have on average smaller craniofacial bony enclosure.
Our study has a number of important limitations. Whilst the sample size for each ethnic group is modest, there is potential for selection bias as patients were recruited from two separate clinics. The difference in socioeconomic status, cultural, and environmental factors between Australians and Hong Kong Chinese may influence subject presentation or referral pattern for clinical assessment, and possibly their preponderance for certain OSA risk factors. Also, Caucasian patients were those who had cephalometry performed as part of a clinical assessment for oral appliance therapy. However, the matching procedures performed in our analyses should address the stated aims of this study while minimizing some of the potential selection bias. Furthermore, age and gender numbers were similar between the ethnic groups in both matching analyses. For OSA severity matching, while the ranges may seem wide, those pairs who were matched with AHI up to 10 events/h and MinSaO2 up to 10% difference tended to be those with more severe OSA. In these cases, OSA severity is practically well matched. The means and standard deviations of the AHI and MinSaO2 for the Caucasian and Chinese patients suggest that the overall matching was adequate. While there were no normal control groups available in this study, many previous intra-ethnic studies have already demonstrated differences compared to non-apneic controls.12,27,28 Future ethnic comparisons of larger clinical cohorts and control subjects in both genders would add further to the results of this study. Craniofacial assessment with a more convenient and higher throughput photographic analysis technique could have great potential for application in this endeavor.29,30 This study was to investigate anatomical differences between Caucasians and Chinese in OSA, and therefore other pathophysiological factors with possible ethnic influence (e.g., neuromuscular and ventilatory control) were not specifically examined. Examining detailed polysomnographic data, such as the ratio of apneas to hypopneas, could provide additional phenotypic differences between the two ethnic groups. The definition of ethnicity relies on the assumptions of the subjects and investigators, but this remains the most commonly used approach in epidemiological studies.
In summary, this study adds to the increasing evidence of the phenotypic differences between Caucasian and Chinese patients with OSA. We found that craniofacial structures and obesity contributed differentially to OSA in these two ethnic groups. Future work using more sophisticated analysis and imaging modalities will help to further define the interaction of these anatomical risk factors across ethnic groups and this may have implications in the diagnosis and management of OSA.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
We thank Associate Professor Gang Shen for his assistance. This research was sponsored in part by the Australian Society of Orthodontists Foundation for Research and Education.
REFERENCES
- 1.Kripke DF, AncoliIsrael S, Klauber MR, Wingard DL, Mason WJ, Mullaney DJ. Prevalence of sleep-disordered breathing in ages 40-64 years: A population-based survey. Sleep. 1997;20:65–76. doi: 10.1093/sleep/20.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Redline S, Tishler PV, Hans MG, Tosteson TD, Strohl KP, Spry K. Racial differences in sleep-disordered breathing in African-Americans and Caucasians. Am J Respir Crit Care Med. 1997;155:186–92. doi: 10.1164/ajrccm.155.1.9001310. [DOI] [PubMed] [Google Scholar]
- 3.Ip MS, Lam B, Lauder IJ, et al. A community study of sleep-disordered breathing in middle-aged Chinese men in Hong Kong. Chest. 2001;119:62–9. doi: 10.1378/chest.119.1.62. [DOI] [PubMed] [Google Scholar]
- 4.Udwadia ZF, Doshi AV, Lonkar SG, Singh CI. Prevalence of sleep-disordered breathing and sleep apnea in middle-aged urban Indian men. Am J Respir Crit Care Med. 2004;169:168–73. doi: 10.1164/rccm.200302-265OC. [DOI] [PubMed] [Google Scholar]
- 5.Kim J, In K, Kim J, et al. Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med. 2004;170:1108–13. doi: 10.1164/rccm.200404-519OC. [DOI] [PubMed] [Google Scholar]
- 6.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 7.Ferguson KA, Ono T, Lowe AA, Ryan CF, Fleetham JA. The relationship between obesity and craniofacial structure in obstructive sleep apnea. Chest. 1995;108:375–81. doi: 10.1378/chest.108.2.375. [DOI] [PubMed] [Google Scholar]
- 8.Watanabe T, Isono S, Tanaka A, Tanzawa H, Nishino T. Contribution of body habitus and craniofacial characteristics to segmental closing pressures of the passive pharynx in patients with sleep-disordered breathing. Am J Respir Crit Care Med. 2002;165:260–5. doi: 10.1164/ajrccm.165.2.2009032. [DOI] [PubMed] [Google Scholar]
- 9.Wong ML, Sandham A, Ang PK, Wong DC, Tan WC, Huggare J. Craniofacial morphology, head posture, and nasal respiratory resistance in obstructive sleep apnoea: an inter-ethnic comparison. Eur J Orthod. 2005;27:91–7. doi: 10.1093/ejo/cjh077. [DOI] [PubMed] [Google Scholar]
- 10.Liu Y, Lowe AA, Zeng X, Fu M, Fleetham JA. Cephalometric comparisons between Chinese and Caucasian patients with obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2000;117:479–85. doi: 10.1016/s0889-5406(00)70169-7. [DOI] [PubMed] [Google Scholar]
- 11.Lam B, Ooi CGC, Peh WCG, et al. Computed tomographic evaluation of the role of craniofacial and upper airway morphology in obstructive sleep apnea in Chinese. Respir Med. 2004;98:301–7. doi: 10.1016/j.rmed.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 12.Hui DSC, Ko FWS, Chu ASY, et al. Cephalometric assessment of craniofacial morphology in Chinese patients with obstructive sleep apnoea. Respir Med. 2003;97:640–6. doi: 10.1053/rmed.2003.1494. [DOI] [PubMed] [Google Scholar]
- 13.Mehta A, Qian J, Petocz P, Darendeliler MA, Cistulli PA. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Crit Care Med. 2001;163:1457–61. doi: 10.1164/ajrccm.163.6.2004213. [DOI] [PubMed] [Google Scholar]
- 14.Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 15.Rechtschaffen A, Kales A. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Los Angeles: Brain Information Service/Brain Research Institute; 1968. [Google Scholar]
- 16.Goldmann L. On-screen computerized cephalometric measurement. Sydney: Discipline of Orthodontics; 1996. [Google Scholar]
- 17.Bearpark H, Elliott L, Grunstein R, et al. Snoring and sleep apnea. A population study in Australian men. Am J Respir Crit Care Med. 1995;151:1459–65. doi: 10.1164/ajrccm.151.5.7735600. [DOI] [PubMed] [Google Scholar]
- 18.Lam B, Ip MSM, Tench E, Ryan CF. Craniofacial profile in Asian and white subjects with obstructive sleep apnoea. Thorax. 2005;60:504–10. doi: 10.1136/thx.2004.031591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li KK, Kushida C, Powell NB, Riley RW, Guilleminault C. Obstructive sleep apnea syndrome: a comparison between Far-East Asian and white men. Laryngoscope. 2000;110:1689–93. doi: 10.1097/00005537-200010000-00022. [DOI] [PubMed] [Google Scholar]
- 20.Ong KC, Clerk AA. Comparison of the severity of sleep-disordered breathing in Asian and Caucasian patients seen at a sleep disorders center. Respir Med. 1998;92:843–8. doi: 10.1016/s0954-6111(98)90386-9. [DOI] [PubMed] [Google Scholar]
- 21.Villaneuva ATC, Buchanan PR, Yee BJ, Grunstein RR. Ethnicity and obstructive sleep apnoea. Sleep Med Rev. 2005;9:419–36. doi: 10.1016/j.smrv.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 22.Miles PG, Vig PS, Weyant RJ, Forrest TD, Rockette HE., Jr Craniofacial structure and obstructive sleep apnea syndrome--a qualitative analysis and meta-analysis of the literature. Am J Orthod Dentofacial Orthop. 1996;109:163–72. doi: 10.1016/s0889-5406(96)70177-4. [DOI] [PubMed] [Google Scholar]
- 23.Sakakibara H, Tong M, Matsushita K, Hirata M, Konishi Y, Suetsugu S. Cephalometric abnormalities in non-obese and obese patients with obstructive sleep apnoea. Eur Respir J. 1999;13:403–10. doi: 10.1183/09031936.99.13240399. [DOI] [PubMed] [Google Scholar]
- 24.Hsu PP, Tan AKL, Chan YH, Lu PKS, Blair RL. Clinical predictors in obstructive sleep apnoea patients with calibrated cephalometric analysis--a new approach. Clin Otolaryngol. 2005;30:234–41. doi: 10.1111/j.1365-2273.2005.00983.x. [DOI] [PubMed] [Google Scholar]
- 25.Dempsey JA, Skatrud JB, Jacques AJ, et al. Anatomic determinants of sleep-disordered breathing across the spectrum of clinical and nonclinical male subjects. Chest. 2002;122:840–51. doi: 10.1378/chest.122.3.840. [DOI] [PubMed] [Google Scholar]
- 26.Lowe AA, Fleetham JA, Adachi S, Ryan CF. Cephalometric and computed tomographic predictors of obstructive sleep apnea severity. Am J Orthod Dentofacial Orthop. 1995;107:589–95. doi: 10.1016/s0889-5406(95)70101-x. [DOI] [PubMed] [Google Scholar]
- 27.Hoekema A, Hovinga B, Stegenga B, De Bont LGM. Craniofacial morphology and obstructive sleep apnoea: a cephalometric analysis. J Oral Rehabil. 2003;30:690–6. doi: 10.1046/j.1365-2842.2003.01130.x. [DOI] [PubMed] [Google Scholar]
- 28.Johal AMA, Patel SI, Battagel JM. The relationship between craniofacial anatomy and obstructive sleep apnoea: a case-controlled study. J Sleep Res. 2007;16:319–26. doi: 10.1111/j.1365-2869.2007.00599.x. [DOI] [PubMed] [Google Scholar]
- 29.Lee RWW, Chan ASL, Grunstein RR, Cistulli PA. Craniofacial phenotyping in obstructive sleep apnea – A novel quantitative photographic approach. Sleep. 2009;32:37–45. [PMC free article] [PubMed] [Google Scholar]
- 30.Lee RWW, Petocz P, Prvan T, Chan ASL, Grunstein RR, Cistulli PA. Prediction of obstructive sleep apnea with craniofacial photographic analysis. Sleep. 2009;32:46–52. [PMC free article] [PubMed] [Google Scholar]