Abstract
Objective
To examine adoption of telehealth in a rural public health district and to explain how the innovation became sustainable.
Study Setting
Longitudinal, qualitative study (1988–2008) of the largest public health district in Georgia.
Study Design
Case study design provided deep insights into the innovation's social dynamics. Punctuated equilibrium theory helped present and make sense of the process. We identified antecedent conditions and outcomes, and we distinguished between episodes and encounters based on the disruptive effects of events.
Data Collection
Twenty-five semistructured interviews with 19 decision makers and professionals, direct observations, published papers, grant proposals, technical specifications, and other written materials.
Principal Findings
Strong collaboration within the district, with local community, and with external partners energized the process. Well-functioning outreach clinics made telehealth desirable. Local champions cultivated participation and generative capability, and overcame barriers through opportunistic exploitation of technological and financial options. Telehealth usage fluctuated between medical and administrative operations in response to internal needs and contextual dynamics. External agencies provided initial funding and supported later expansion.
Conclusions
Extensive internal and external collaboration, and a combination of technology push and opportunistic exploitation, can enable sustainable rural telehealth innovation.
Keywords: Telehealth innovation, rural health, process model, punctuated equilibrium theory, case study, qualitative research
Two decades after Health Services Research published a special issue on the subject (Hersh and Van Hook 1989), rural health care delivery remains a topical research area. Availability and accessibility of rural health care services are still major concerns, and rural health care institutions remain vulnerable (Hicks 1990; Ricketts and Savitz 1994; Gamm et al. 2002; Ricketts 2005;). Specifically, these institutions face a long-standing problem of acquiring sufficient professional expertise: rural America has 20 percent of the population but <11 percent of the physicians, and this imbalance is worsening (Ricketts 2000, 2005; Rosenthal, Zaslavsky, and Newhouse 2005; Iezzoni, Killeen, and O'Day 2006).
Telehealth innovations can reduce the resource differential between urban and rural areas by enhancing access to medical services for underserved rural communities (Puskin 1992; Sanders, Salter, and Stachura 1996;). Telehealth can deliver medical services over distance, facilitate knowledge sharing, and distribute complex diagnostic processes and medical decision making across health care organizations (Bashshur and Armstrong 1976; Robinson, Savage, and Campbell 2003; Paul 2006; Cho and Mathiassen 2007;). Thus, telehealth can become an “alternative healthcare delivery system” (Bashshur, Reardon, and Shannon 2000). However, most telehealth innovations struggle to survive beyond the pilot stage, despite being medically and technically viable solutions (Sanders and Bashshur 1995; Wright 1999; Cradduck 2002;). The objective of this study is, therefore, to contribute to health services research by examining how rural public health institutions can sustainably adopt telehealth innovations.
LITERATURE REVIEW
Public health institutions provide population services such as disease prevention and health promotion, as well as personal services such as well-child checkups, prenatal care, and primary care (Slifkin, Silberman, and Reif 2001). These institutions have generally emphasized clinical services to Medicaid-eligible or other low-income populations (Goldberg 1998). In rural areas, residents are disproportionately poorer, fewer are of working age, and they have had less education (Ricketts 1999, 2000). Rural areas, therefore, have large indigent populations that depend on public health services (Lipson and Naierman 1996) or emergency rooms (Dohan 2002). However, policies such as managed care in Medicaid, and lack of infrastructure investments, have adversely affected public health institutions (Lipson and Naierman 1996; Ricketts 2000; Slifkin, Silberman, and Reif 2001;). As a result, these institutions are called upon to do more with substantially fewer resources (Wellever et al. 2006), a circumstance which can benefit from telehealth innovations (Sanders, Salter, and Stachura 1996). While many studies focus on policy-related changes to improve public health (Walker 1989; Goldberg 1998; Wellever et al. 2006;), few studies focus on local initiatives to innovate public health infrastructure.
Telehealth dates to the 1920s, when radio-linked, shore-based medical specialists were used for medical emergencies at sea (Winters 1921). Today, telehealth integrates multiple technologies to provide medical services without in-person physician-to-patient encounters (Bashshur and Lovett 1977). Although the focus initially was on medical care, the scope expanded to information exchanges in health care processes, including delivery of educational and collaborative services (Bennet, Rappaport, and Skinner 1978; Bashshur, Reardon, and Shannon 2000;). As a result, the broader term telehealth (rather than telemedicine) is increasingly used to describe the full array of technologies, networks, and health-related services provided through telecommunications.
Various studies have shown the benefits of telehealth to providers, clients, and society. For example, telehealth can substitute traditional encounters based on patients visiting physician offices or hospitals, provide specialist consultations in emergency rooms in remote or rural areas, and enable prehospital diagnosis for critical patients in transit (Chau and Hu 2004; Cho and Mathiassen 2007;). Medical home-based telehealth can facilitate remote monitoring, and follow-up, of patients requiring postacute or chronic care, and patients with limited mobility (Field and Grigsby 2002; Lau et al. 2002; LeRouge, Hevner, and Collins 2007;). Using data capture from home monitoring devices, Shea et al. (2006) showed the effectiveness of telehealth-based diabetes management. In another study, Izquierdo et al. (2003) showed that diabetes education via telemedicine was as effective as in-person education in improving glycemic control, and both methods were well accepted by patients. Telehealth can also facilitate staff training, real-time coordination, planning, reporting, and information sharing across medical and allied staff groups (Robinson, Savage, and Campbell 2003; Miscione 2007;).
However, telehealth innovations invariably struggle to sustain after initial sponsorship ends (Sanders and Bashshur 1995; Wright 1999; Stachura 2001; Cradduck 2002;). Sustainability is the long-term ability of a system to respond to external pressures, and to adapt to external constraints without detriment to its functioning (Whittaker et al. 2004). In economic terms, it refers to the ability to support projects when grants or start-up funds are no longer available (Rodgers, Anderson, and Manning 2003). Sustainability of telehealth is affected by existing structures and processes of the health care delivery system, policy frameworks, communication and technology costs, and physician and patient acceptance (Sanders, Salter, and Stachura 1996). A telehealth service is sustainable when it is “no longer considered a special case, but has been absorbed into routine healthcare delivery” (Cradduck 2002) and this requires its integration “among members of the relevant social system” (Rogers 2003), including managers, staff, and specialists at partnering institutions.
Previous studies have focused on adoption of telehealth at the individual level (Croteau and Vieru 2002; Gagnon et al. 2003; Chau and Hu 2004;), organizational level (Whitten and Allen 1995; Robinson, Savage, and Campbell 2003; Gagnon et al. 2005;), and organization population level (Cho, Mathiassen, and Gallivan 2008). However, none of these studies focuses on telehealth in rural institutions. On this backdrop, the current study investigates how a rural public health district integrated telehealth as a sustainable part of its operations.
RESEARCH DESIGN
The research is organized as a qualitative, longitudinal case study (Miles and Huberman 1994; Yin 2003;) of South East Health District (SEHD), the largest public health district in the state of Georgia. The use of qualitative methods in health services research is growing (Bowling 1997; Shortell 1999;), although the number of qualitative studies in top interdisciplinary journals in health services and management still lags far behind quantitative studies (Hoff and Witt 2000). Qualitative methods are particularly helpful in exploring emerging issues, and enhancing our understanding of the context of events as well as the events themselves (Miles and Huberman 1994; Sofaer 1999;). Case studies are useful when both the case and the context change over time, adding immeasurably to the number of variables under analysis (Yin 1999). In this study, we investigate why and how SEHD underwent many phases of telehealth technology selection, adoption, and integration during the period 1988–2008. Following Yin (1999) and Devers (1999), an in-depth, longitudinal case study is therefore an appropriate research design.
SEHD provides over 30 health services, including children's services, women's services, emergency preparedness training, chronic diseases prevention, and health promotion to 16 rural counties in Georgia. A staff of over 400 provides these services. We used purposive sampling (Kuzel 1992; Miles and Huberman 1994;, p. 27) to identify SEHD as offering substantive significance (Ragin 1999, p. 1141) and being well aligned with our research objectives. SEHD represents a rare example of rural telehealth innovation; it was the only one of five pilot programs in the Georgia Statewide Telemedicine Program (GSTP) that eventually became sustainable (the Georgia prisons telemedicine system also survived, but it remains fully state supported). Moreover, this innovation was driven mainly by local initiatives.
Drawing upon multiple data sources, we investigated the process through which the telehealth innovation became sustainable. Conceptualizing process as “a sequence of individual and collective events, actions, and activities unfolding over time in context” (Pettigrew 1997), we used the encounter-episode framework (Newman and Robey 1992) to develop a process model of telehealth innovation at SEHD. This framework draws on the theory of punctuated equilibrium, treating change as an “alternation between long periods when stable infrastructures permit only incremental adaptations, and brief periods of revolutionary upheaval” (Gersick 1991). Hence, events are classified as encounters or episodes that occur across time (Newman and Robey 1992). It should be noted that events are distinct from incidents because incidents actually occur, while events represent theoretical entities (Van de Ven and Poole 1990). Encounters are relatively brief events that punctuate a process and offer opportunities for establishing a new equilibrium. Encounters are thus opportunities for actors to challenge established practices triggered by both internal and external events. Episodes, in contrast, refer to sets of events that stand apart, representing relatively long periods of equilibrium, wherein the patterns set during an earlier encounter play out. Antecedent conditions are the relationships between the focal organization and its environment before the process began. Finally, outcomes represent the results of a sequence of encounters and episodes.
METHOD
Data Collection
We collected primary data between December 2007 and March 2008, beginning with a site visit to SEHD headquarters in Waycross. We interviewed the principal actors currently associated with the telehealth initiative: administrators, managers, nurses, and information technology (IT) specialists. Using snowball sampling (Lincoln and Guba 1985, p. 233; Miles and Huberman 1994, p. 28), we identified other key actors who had been involved in the initiative over the years. As a result, we interviewed the former health director, an influential community leader, the former telehealth program manager, the former external network consultant, as well as five physicians from the Medical College of Georgia (MCG) who provide specialty consultations at SEHD using telehealth. In all, we conducted 25 semistructured in-person and telephone interviews with 19 decision makers and professionals. Following Yin (1999), we collected evidence from multiple sources to enhance the quality of our data. We conducted direct, nonparticipant observations of how managers, nurses, nutritionists, and physicians used telehealth in their day-to-day operations. Finally, we reviewed secondary data sources such as grant proposals, technical specifications, published papers, annual reports, and other written materials. Basic descriptive information about these data sources is available as Appendix SA2.
Following Ragin (1999, p. 1139), we asked each respondent to reflect on their motives, feelings, and thought processes related to the telehealth innovation at SEHD. We prepared a protocol to structure the interview process and tailored it for specific interviewees. For example, the protocol for the IT specialist included information about networks, existing telecommunication capabilities, current and planned projects, security risks, and other technical challenges. The interviews typically lasted about 1 hour, were tape-recorded, and the researchers took separate notes.
Data Analysis
We transcribed the interviews, manually coded all key events, and classified them as encounters or episodes based on their disruptive effects and duration. We then used temporal bracketing as suggested by the encounter-episode framework to create a timeline of key events at SEHD. We also identified antecedent conditions as well as outcomes. Where necessary, we sought clarifications through follow-up interviews. To improve reliability, the analysis was peer-reviewed by three other researchers, presented to all key informants, and revised accordingly (Mays and Pope 1995). This analysis resulted in the process model in Figure 1, in which stars represent encounters and pentagonal boxes represent episodes.
Figure 1.
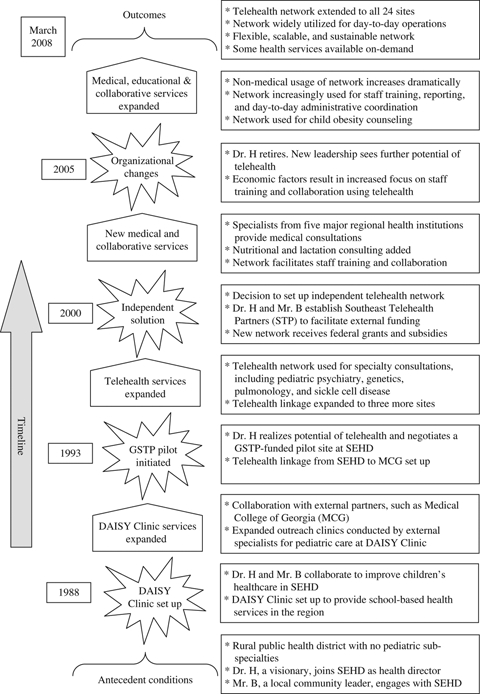
A Process Model of Telehealth Innovation at SEHD—After Newman and Robey (1992)
RESULTS
Antecedent Conditions
In 1974, when Dr. H became the public health director, SEHD had no pediatric subspecialists, and a poor and underinsured population discouraged specialists from visiting or opening practices in the region. Patients had to travel up to 4 hours to consult with specialists at tertiary centers (Karp et al. 2000). Dr. H soon met Mr. B, a local community leader, who had been instrumental in several projects for children. These two champions formed a lasting relationship, finding ways to improve public health care in the region, with Dr. H providing vision and leadership, and Mr. B providing key operational support. In late 1970s, Dr. H visited his brother, a physician in Alaska, and witnessed firsthand how remote communities benefitted from telehealth. As Mr. B told us, “this experience struck Dr. H, and we discussed its potential for rural Georgia.”
Encounter 1—Diversified Agencies Involved in Serving Youth (DAISY) Clinic Initiated (1988)
In 1988, Dr. H and Mr. B started the DAISY Clinic in Waycross and hired a pediatrician as its clinical director. Supported by the Robert Wood Johnson Foundation, the Clinic built upon existing collaboration between SEHD and MCG. It facilitated school-based health services, including programs relating to teen pregnancies, and drug and alcohol abuse, by stationing public health nurses in local schools (Keenan 1999).
Episode 1—Expanded Health Care Services (1988–1993)
Dr. H engaged external clinicians, primarily from MCG, to provide pediatric specialty care in the health district. These specialists regularly drove 185 miles from Augusta to Waycross to conduct in-person outreach clinics at SEHD. During this period, Mr. B recruited key operational support and local resources for expansion of services at DAISY and the outreach clinics. The clinics were successful in improving health care for underserved children but soon began to experience significant time delays in services, with waiting times over 3 months in some specialties. As a result, Dr. H and Mr. B started to think about telehealth, often referring to Dr. H's experience in Alaska.
Encounter 2—GSTP Initiated (1993)
In 1992, when Georgia Department of Administrative Services (DOAS) established the GSTP network, Dr. H and Mr. B negotiated for SEHD to become one of five pilot sites. Separate T-1 links connected each site to MCG in December 1993. DOAS managed the line and maintenance contracts. The monthly cost to each site was approximately U.S.$2,500, with a 50 percent subsidy for the first 3 years. It was anticipated that by the end of the subsidy period, reimbursement for telehealth services would offset those costs (Adams and Grigsby 1995).
Episode 2—Telehealth Services Expanded (1994–1999)
The SEHD component of the GSTP network expanded to connect three remote sites to SEHD headquarters at Waycross, and it was fully functional by 1995 (Adams and Grigsby 1995). The network facilitated telehealth-based consultations for pediatric immunology, pulmonology, neurology, sickle cell disease, and genetics (Karp et al. 2000). Within 2 years, SEHD became the most active site within the GSTP network. A factor that contributed to the success of telehealth initiative at SEHD was that specialists from MCG continued to conduct in-person outreach clinics at regular, albeit reduced, intervals. Thus, outreach clinics, used primarily for initial consultations where hands-on patient examination was critical, supplemented the videoconferencing consultations using the telehealth infrastructure. A total of 333 telehealth consultations were reported at SEHD between December 1995 and May 1997 (Karp et al. 2000). During this period, the network also facilitated training to local primary practitioners in pediatric genetics and pulmonology. A pediatric pulmonologist at MCG noted, “The local therapy has improved over the years. In the first five years (of telehealth implementation at SEHD), the number of ER visits by children (suffering from asthma attacks) reduced by over 30 percent.”
Encounter 3—Independent Solution Created (2000)
In 1999, the original subsidy for the GSTP project expired, and the design of the network made individual sites ineligible to receive telecommunications cost relief from the recently established federal Universal Services Fund (USF). According to Mr. B, this was the “tipping point.” The loss of state subsidy, coupled with federal ineligibility, made all GSTP sites financially unviable. Although the GSTP network was a clinical and technical success, the sites experienced doubling of their telecommunications costs. Further, under the GSTP network, the SEHD subnetwork was limited to only three sites, constraining its ability to expand linkage to all 24 offices within the district. Dr. H and Mr. B reconsidered their options, which included (a) continue with the GSTP network and bear the additional telecommunication costs, (b) discontinue telehealth-based health care delivery, or (c) build an independent telehealth network using other sources of funding.
Dr. H and Mr. B concluded that telehealth was the only affordable solution to help meet the health care needs of the distributed population within the health district, and creation of an independent network was the only viable alternative. To achieve this goal, in 1999 they set up an unincorporated, nonprofit association called the Southeast Telehealth Partners (STP). STP sought funding from the Human Resources and Services Administration's Office for the Advancement of Telehealth (OAT). A 3-year grant, approved in September 2000, allowed STP to initiate the new network. The independent structure and rural location of STP made it eligible for USF subsidy. STP negotiated directly with its regional telecommunication services provider, as required by USF, and reduced telecommunication costs by 75 percent. Once the network was fully functional, SEHD severed ties to the old GSTP network, but it maintained its relations to MCG by including it as a node in the new network.
Episode 3—Expansion of Network, and New Medical and Collaborative Services (2000–2005)
In 2000, Dr. H hired a program manager to oversee the operational activities of the STP network and engaged a consultant to help design, and set up, a secure and scalable network. By mid-2005, the network connected patients and staff at 16 of 24 sites in SEHD. Two new tertiary partners, Savannah Perinatology Associates and Coffee Regional Medical Center, joined the network to provide telehealth clinics for high-risk obstetrics and perinatal care. Specialists from these institutions used the STP network to provide level-II ultrasound evaluations to patients in SEHD. MCG specialists continued to provide remote consultations, now using the STP infrastructure.
In 2003, SEHD received a second round of 3-year funding from OAT for further network expansion. This provided resources to add a telehealth link to Grady Hospital in Atlanta for infectious disease collaboration and consultation, and another to Emory Hospital in Atlanta for HIV consultations. The expansion allowed extending HIV consultations to all five HIV Wellness Centers in the health district. SEHD also added three sites under the women, infant, and child (WIC) program to provide nutritional and lactation consulting. According to the STP program manager, the number of telemedical consultations increased from about 250 per year in 2000, to almost 1,000 per year by mid-2005. The network expansion also facilitated increase in nonmedical usage, with general staff training, management meetings, and administrative coordination representing almost 40 percent of network traffic.
Encounter 4—Organizational and Economic Changes (2005)
Dr. H retired in early 2005. The new SEHD director considered the telehealth network a strategic asset and hired additional staff, including a new program manager. In fall 2005, Hurricane Katrina caused a sudden increase in oil prices, leading to an almost doubling of travel reimbursements for SEHD staff, particularly the nutritionists and nurses who often travelled several hours to meet with patients at remote sites. Georgia's Department of Human Resources did not allocate any funds to cover this increase.
Episode 4—Medical, Educational, and Collaborative Services Expanded (2005–March 2008)
The SEHD director decided to expand the network further. As the program manager told us, “it became clear that expanding the STP network to all counties would enable staff to participate in training without the travel and costs associated with it.” In 2006, SEHD received a third round of 3-year funding from OAT, and the STP network expansion was complete by February 2007. The new configuration allowed patients at any of the 24 sites in the 16 counties to consult (using specialized equipment) with specialists from five major medical institutions in Georgia. An expanded WIC program provided nutritional counseling services, including child-obesity programs, to other health department offices within SEHD. The nursing staff and managers used the network increasingly for day-to-day administrative coordination, program updates, continuing medical education, and protocol sharing. The network also facilitated emergency preparedness training to the local community, such as for flu epidemic, bioterrorism, and emergency infection handling. SEHD regularly used the network to provide interpreter services to Hispanic patients. The network was widely utilized for coordination and communication during the wildfire control operations in Georgia and Northern Florida in summer 2007. As a result, these educational and collaborative services comprised almost 85 percent of network traffic.
Outcomes (March 2008)
The telehealth network at SEHD became sustainable, supported in part by federal funding, but increasingly paying for itself through new services and savings in travel expenses and time. The program manager estimated that telehealth had saved more than 56,000 miles of travel in 2006–2007. The network also reduced the turnaround time in recruitment and, according to estimates of the human resources manager, telehealth had contributed to a 25 percent reduction of nursing staff turnover during the past 3 years. The network connected a staff of over 400, including more than 100 nurses and 5 nutritionists. Videoconferencing sessions connected up to 16 sites simultaneously. In addition, specialists at five major regional medical institutions provided consultations using the network. A centralized staff of three network specialists and a manager supported the infrastructure while at the same time providing IT support for SEHD. A full-time scheduler managed the day-to-day linking of specific sites. A vendor in Ohio provided network support via remote access to the routers. Based on this configuration, SEHD continued to explore ways to realize the full potential of telehealth to provide additional medical, educational, and collaborative services. New services, such as on-demand lactation and nutritional consulting, are now available.
DISCUSSION
The process model (Figure 1) shows how interactions between key actors, institutional setting, and contextual dynamics shaped the telehealth innovation at SEHD. The model describes how the innovation became sustainable and how actors addressed key challenges. Table 1 offers detailed examples of this knowhow that we summarize into a number of lessons.
Table 1.
Path to Sustainable Telehealth Innovation at SEHD
| No. | Knowhow | Examples |
|---|---|---|
| 1 | Collaborate within institution | • The nursing staff shared information such as programs, schedules, and patient updates over the telehealth network |
| • The managers used the network to coordinate and collaborate with the staff located in 24 offices across 16 counties | ||
| 2 | Develop alliances within community | • SEHD collaborated with local public schools through DAISY Clinic to bring health care to schoolchildren |
| • Mr. B reached out to churches and local businesses to help provide personnel and financial support for telehealth initiatives at SEHD | ||
| 3 | Develop external partnerships | • SEHD collaborated with MCG and other regional health institutions to provide key medical specialists for outreach clinics and telehealth consultations |
| 4 | Identify critical services | • Dr. H and Mr. B identified existing outreach pediatric clinics for genetics and pulmonology as ideal launching pads for telehealth consultations. The existence of these well-functioning clinics created a pull for the telehealth initiative by both physicians and patients |
| 5 | Engage external specialists | • Specialists from MCG and other collaborating institutions supplemented their outreach clinics at SEHD with telehealth clinics. This arrangement allowed the specialists to see more patients with reduced travel and less time out of office |
| 6 | Develop shared vision | • Dr. H realized the potential of telehealth in providing specialty health care services to underserved communities |
| • Dr. H and Mr. B continuously pushed for telehealth innovation at SEHD | ||
| 7 | Cultivate participation | • Dr. H, Mr. B, and the managers at SEHD actively engaged physicians and nursing staff to overcome initial resistance to adoption of telehealth during GSTP pilot phase (1993–1999), and during the transition to the new STP network (2000–2001) |
| • They targeted potential early adopters to demonstrate the effectiveness of the telehealth innovation | ||
| 8 | Develop generative capability | • Dr. H and Mr. B fostered a generative capability among all employees by continuously encouraging new ideas. This resulted in an opportunistic pull to extend use of the telehealth infrastructure for nontraditional applications such as staff collaboration and training |
| 9 | Exploit funding opportunities | • SEHD exploited available funding from GSTP to build a pilot telehealth network |
| • Exploiting grants from OAT, SEHD created an independent entity STP to build a new telehealth network | ||
| 10 | Explore technological options | • In 1993, SEHD started with the GSTP pilot program and thus avoided the risk of a full-scale telehealth implementation |
| • In 2000, SEHD severed ties to the GSTP network and opted to implement an independent telehealth network that offered more design options, including greater scalability and flexibility. The independent network configuration allowed the IT support team to install new routers and expand telehealth services as usage increased and as new tertiary partners joined the initiative | ||
| • In 2000, SEHD engaged an external consultant who helped design and set up the independent telehealth network. | ||
| 11 | Improve medical services | • During 1993–1999, SEHD used the telehealth network primarily for specialty medical consultations, and to provide training to primary practitioners in subspecialty areas such as asthma, genetics, and pulmonology for pediatric patients |
| • SEHD expects the network traffic associated with medical specialty consultations to increase in the coming years as more tertiary partners join the telehealth network | ||
| 12 | Improve administrative processes | • After 2005, SEHD increasingly used the telehealth infrastructure for administrative processes, such as interviewing new employees, coordination, staff training, and program updates. This substantially reduced travel needs for the staff |
| 13 | Secure support from funding agencies | • In 1993, SEHD secured funding from GSTP to build a pilot telehealth network. |
| • In 2000, SEHD secured a 3-year grant from OAT, which helped it to create the STP network. The grant, renewed two more times, allowed SEHD to expand the network to all 24 sites, and to focus on providing additional medical, educational and collaborative services. This support from funding agencies was critical to success of the telehealth innovation |
DAISY, Diversified Agencies Involved in Serving Youth; GSTP, Georgia Statewide Telemedicine Program; IT, information technology; MCG, Medical College of Georgia; OAT, Office for the Advancement of Telehealth; SEHD, South East Health District; STP, Southeast Telehealth Partners.
Strong collaboration within the rural health institution, with the local community, and with external partners initiated the process and energized it as it evolved (1–3 in Table 1). The collaboration between Dr. H and Mr. B brought together local and external resources and set the stage for bringing specialty health services to SEHD. This collaboration created a continuous push for colleagues to become engaged in the DAISY Clinic, the GSTP pilot, and the independent STP network. According to Mr. B, “we realized early on that there must be a collaborative mindset. We learned to collaborate, not merely cooperate, and pushed this belief to our partnering communities.”
Establishing well-functioning, in-person outreach clinics within pediatric specialties made an early move toward adoption of telehealth desirable (4 and 5 in Table 1). A pediatric geneticist at MCG told us, “I started doing outreach clinics at SEHD in December 1984, and have continued ever since. Initially, I would drive nearly four hours from Augusta to Waycross every month. Since 1995, I hold a telehealth consultation every month for existing patients. I still conduct an outreach clinic every other month, but only for new patients.” The other specialists had similar experiences. Telehealth benefitted the patients and their families who did not have to travel to tertiary centers.
The champions and managers exhibited visionary leadership and adopted facilitating tactics to cultivate participation and generative capability (6–8 in Table 1). Mr. B explained how they got people engaged with telehealth, “the little kids showed the way in embracing technology. They loved the videoconferencing technology. They said, ‘Look, I am on TV!’ Their enthusiasm helped overcome the initial resistance of parents, physicians and nursing staff.” Dr. H elaborated, “We hired people who were interested in telehealth. Then we threw the ball into the air and had people jump at it. …. We encouraged them to use the system in new ways.”
The institution opportunistically exploited emerging technological options and available funding to overcome barriers (9 and 10 in Table 1). The SEHD telehealth initiative started as a GSTP pilot in 1993. When the supporting subsidy expired in 1999, the existing network became financially unviable. SEHD then created an independent network, as this allowed them access to federal grants and subsidies. This opportunistic exploitation of emerging options was also evident in selecting appropriate technology, and in engaging external consultants.
The use of the innovation fluctuated between supporting medical and administrative operations, in response to internal needs and contextual dynamics (11 and 12 in Table 1). Initially, medical consultations were the primary application of the telehealth infrastructure. However, nonmedical applications, such as general staff training and day-to-day coordination, began to grow during 2001–2005, contributing to almost 40 percent of network traffic. Facing financial pressures after fall 2005, SEHD encouraged educational and collaborative usage of the network, resulting in these services contributing to nearly 85 percent of network traffic. This increase did not suggest fewer medical specialty consultations; instead, it reflected new ways in which SEHD used telehealth.
Finally, the support of funding agencies was critical to providing seed capital for this rural telehealth initiative (13 in Table 1). SEHD benefitted from initial funding for telehealth network under the GSTP program. Later, when SEHD created an independent telehealth network, federal grants bridged the resource gap for network expansion. These grants facilitated delivery of telehealth services to the local community and complemented SEHD's own efforts to improve the sustainability of the telehealth initiative by saving costs and providing education and collaborative services through extensive use of the infrastructure.
CONCLUSION
Drawing on a longitudinal, qualitative data (1988–2008) from SEHD in Georgia, the objective of this study was to examine successful adoption of telehealth in a rural public health district. Punctuated equilibrium theory helped us analyze and present the rich data and explain how SEHD successfully integrated telehealth as an important and sustainable part of its operation. The findings suggest that SEHD managers skillfully combined leadership, collaboration, opportunistic use of technical and financial options, and usage based on local needs. Moreover, they communicated the innovation “among members of the relevant social system” (Rogers 2003), acting as change agents to demonstrate the value of the innovation for SEHD and its external partners.
As our study draws on a single case, any change in institutional setting, context, or antecedent conditions may produce different outcomes (Miles and Huberman 1994; Yin 2003;). To address this issue of limited generalizability, we followed Devers (1999) and provided detailed contextual information about the case. This may assist researchers and managers in assessing the transferability of our findings to other contexts (Lincoln and Guba 1985). In addition, our research design involved reconstructing sequences of events over a 20-year period, and this temporal reconstruction opens for multiple interpretations. In response to this challenge, we used Newman and Robey's (1992) framework to systematically distinguish between antecedent conditions, encounters, episodes, and outcomes to develop a comprehensive process model of key events at SEHD (Figure 1). Finally, our use of retrospective interviews may suffer from recall bias, particularly by emphasizing events that put some actors in a more favorable light. To minimize this effect, we interviewed multiple stakeholders about the same events, triangulated between different data sources, checked against “hard facts” (such as published documents), used multiple methods and investigators to interpret the data, and iteratively sought feedback on our interpretations from key stakeholders (Miles and Huberman 1994, p. 267; Yin 2003). This also helped us improve the confirmability and credibility of the study (Lincoln and Guba 1985; Devers 1999;).
The American Recovery and Reinvestment Act of 2009 provides funding to health care institutions to help them improve IT infrastructures, implement telehealth networks to serve patients in rural and remote areas, and to develop telehealth-enabled home health care (US Government 2009, p. 121). Our study provides valuable insights to rural health care organizations as they contemplate translating these funding opportunities into sustainable telehealth solutions. The key lessons from SEHD include (1) seeking initiating as well as follow-up grants to support telehealth; (2) creating independent entities with appropriate local telehealth knowhow; (3) tailoring telehealth innovations to emerging needs and available technology options; and (4) facilitating participation within the rural health institution, and collaboration with the local community and external partners, to make the innovation sustainable.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors acknowledge with appreciation the contributions of former and current nursing staff, managers, IT specialists, and administrators at the SEHD of Georgia. All of them have played important roles in developing a sustainable telehealth innovation and they have been most helpful in providing detailed data to support this research. In addition, we would like to thank the Georgia Research Alliance for providing funding in support of this research.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2. Primary and Secondary Data Sources.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Adams LN, Grigsby RK. The Georgia State Telemedicine Program: Initiation, Design, and Plans. Telemedicine Journal. 1995;1(3):227–35. doi: 10.1089/tmj.1.1995.1.227. [DOI] [PubMed] [Google Scholar]
- Bashshur R, Lovett J. Assessment of Telemedicine: Results of the Initial Experience. Aviation, Space, and Environmental Medicine. 1977;48(1):65–70. [PubMed] [Google Scholar]
- Bashshur RL, Armstrong PA. Telemedicine: A New Mode for the Delivery of Health Care. Inquiry. 1976;13(3):233–44. [PubMed] [Google Scholar]
- Bashshur RL, Reardon TG, Shannon GW. Telemedicine: A New Health Care Delivery System. Annual Reviews in Public Health. 2000;21(1):613–37. doi: 10.1146/annurev.publhealth.21.1.613. [DOI] [PubMed] [Google Scholar]
- Bennet AM, Rappaport WH, Skinner EL. Telehealth Handbook (PHS Publication No. 79–3210) Washington, DC: US Department of Health, Education, and Welfare; 1978. [Google Scholar]
- Bowling A. Research Methods in Health: Investigating Health and Health Services. Buckingham, England: Open University Press; 1997. [Google Scholar]
- Chau PYK, Hu PJ-H. Technology Implementation for Telemedicine Programs. Communications of the ACM. 2004;47(2):87–92. [Google Scholar]
- Cho S, Mathiassen L. The Role of Industry Infrastructure in Telehealth Innovations: A Multi-Level Analysis of a Telestroke Program. European Journal of Information Systems. 2007;16(6):738–50. [Google Scholar]
- Cho S, Mathiassen L, Gallivan M. 2008. From Adoption to Diffusion of a Telehealth Innovation. Proceedings of the 41st Hawaii International Conference on System Sciences, pp. 245–45. Hawaii.
- Cradduck TD. Sustainability-the Holy Grail of Telehealth? Journal of Telemedicine and Telecare. 2002;8(3):7–8. doi: 10.1258/13576330260440682. [DOI] [PubMed] [Google Scholar]
- Croteau AM, Vieru D. 2002. Telemedicine Adoption by Different Groups of Physicians. Proceedings of the 35th Hawaii International Conference on System Sciences, pp. 1985-93. Hawaii.
- Devers K. How Will We Know “Good” Qualitative Research When We See It? Beginning the Dialogue in Health Services Research. Health Services Research. 1999;34(5, part 2):1153–88. [PMC free article] [PubMed] [Google Scholar]
- Dohan D. Managing Indigent Care: A Case Study of a Safety-Net Emergency Department. Health Services Research. 2002;37(2):361–76. doi: 10.1111/1475-6773.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field MJ, Grigsby J. Telemedicine and Remote Patient Monitoring. The Journal of American Medical Association. 2002;288(4):423–5. doi: 10.1001/jama.288.4.423. [DOI] [PubMed] [Google Scholar]
- Gagnon MP, Godin G, Gagné C, Fortin JP, Lamothe L, Reinharz D, Cloutier A. An Adaptation of the Theory of Interpersonal Behaviour to the Study of Telemedicine Adoption by Physicians. International Journal of Medical Informatics. 2003;71(2–3):103–15. doi: 10.1016/s1386-5056(03)00094-7. [DOI] [PubMed] [Google Scholar]
- Gagnon MP, Lamothe L, Fortin JP, Cloutier A, Godin G, Gagné C, Reinharz D. Telehealth Adoption in Hospitals: An Organisational Perspective. Journal of Health, Organisation and Management. 2005;19(1):32–56. doi: 10.1108/14777260510592121. [DOI] [PubMed] [Google Scholar]
- Gamm L, Hutchison L, Bellamy G, Dabney BJ. Rural Healthy People 2010: Identifying Rural Health Priorities and Models for Practice. The Journal of Rural Health. 2002;18(1):9–14. doi: 10.1111/j.1748-0361.2002.tb00869.x. [DOI] [PubMed] [Google Scholar]
- Gersick CJG. Revolutionary Change Theories: A Multilevel Exploration of the Punctuated Equilibrium Paradigm. Academy of Management Review. 1991;16(1):10–36. [Google Scholar]
- Goldberg BW. Managed Care and Public Health Departments: Who Is Responsible for the Health of the Population? Annual Reviews in Public Health. 1998;19(1):527–37. doi: 10.1146/annurev.publhealth.19.1.527. [DOI] [PubMed] [Google Scholar]
- Hersh AS, Van Hook RT. A Research Agenda for Rural Health Services. Health Services Research. 1989;23(6):1053–64. [Google Scholar]
- Hicks LL. Availability and Accessibility of Rural Health Care. The Journal of Rural Health. 1990;6(4):485–505. doi: 10.1111/j.1748-0361.1990.tb00684.x. [DOI] [PubMed] [Google Scholar]
- Hoff TJ, Witt LC. Exploring the Use of Qualitative Methods in Published Health Services and Management Research. Medical Care Research and Review. 2000;57(2):139–60. doi: 10.1177/107755870005700201. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, Killeen MB, O'Day BL. Rural Residents with Disabilities Confront Substantial Barriers to Obtaining Primary Care. Health Services Research. 2006;41(4, part 1):1258–75. doi: 10.1111/j.1475-6773.2006.00534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izquierdo RE, Knudson PE, Meyer S, Kearns J, Ploutz-Snyder R, Weinstock RS. A Comparison of Diabetes Education Administered through Telemedicine versus in Person. Diabetes Care. 2003;26(4):1002–7. doi: 10.2337/diacare.26.4.1002. [DOI] [PubMed] [Google Scholar]
- Karp WB, Grigsby RK, Lcsw DSW, McSwiggan-Hardin M, Pursley-Crotteau S, Adams CLN, Bell W, Stachura ME, Kanto WP. Use of Telemedicine for Children with Special Health Care Needs. Pediatrics. 2000;105(4):843–7. doi: 10.1542/peds.105.4.843. [DOI] [PubMed] [Google Scholar]
- Keenan T. A Foundation Perspective on Community Access to Child Health Program. Pediatrics. 1999;103(6):1428–9. [PubMed] [Google Scholar]
- Kuzel AJ. Sampling in Qualitative Inquiry. In: Crabtree BF, Miller WL, editors. Doing Qualitative Research. Newbury Park, CA: Sage; 1992. pp. 31–44. [Google Scholar]
- Lau C, Churchill R, Kim J, Matsen F, Kim Y. Asynchronous Web-Based Patient-Centered Home Telemedicine System. IEEE Transactions on Biomedical Engineering. 2002;49(12):1452–62. doi: 10.1109/TBME.2002.805456. [DOI] [PubMed] [Google Scholar]
- LeRouge C, Hevner A, Collins R. It's More Than Just Use: An Exploration of Telemedicine Use Quality. Decision Support Systems. 2007;43:1287–304. [Google Scholar]
- Lincoln YS, Guba EG. Naturalistic Inquiry. Newbury Park, CA: Sage; 1985. [Google Scholar]
- Lipson DJ, Naierman N. Effects of Health System Changes on Safety-Net Providers. Health Affairs. 1996;15(2):33–48. doi: 10.1377/hlthaff.15.2.33. [DOI] [PubMed] [Google Scholar]
- Mays N, Pope C. Rigour and Qualitative Research. British Medical Journal. 1995;311(6997):109–12. doi: 10.1136/bmj.311.6997.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. Qualitative Data Analysis. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- Miscione G. Telemedicine in the Upper Amazon: Interplay with Local Health Care Practices. MIS Quarterly. 2007;31(2):403–25. [Google Scholar]
- Newman M, Robey D. A Social Process Model of User-Analyst Relationships. MIS Quarterly. 1992;16(2):249–66. [Google Scholar]
- Paul DL. Collaborative Activities in Virtual Settings: A Knowledge Management Perspective of Telemedicine. Journal of Management Information Systems. 2006;22(4):143–76. [Google Scholar]
- Pettigrew AM. What Is a Processual Analysis? Scandinavian Journal of Management. 1997;13(4):337–48. [Google Scholar]
- Puskin DS. Opportunities and Challenges for the Health Care System. Annals of the New York Academy of Sciences. 1992;670(1):67–75. doi: 10.1111/j.1749-6632.1992.tb26075.x. [DOI] [PubMed] [Google Scholar]
- Ragin C. The Distinctiveness of Case-Oriented Research. Health Services Research. 1999;34(5, part 2):1137–51. [PMC free article] [PubMed] [Google Scholar]
- Ricketts TC. Rural Health in the United States 1999. NewYork: Oxford University Press; 1999. [Google Scholar]
- Ricketts TC. The Changing Nature of Rural Health Care. Annual Review of Public Health. 2000;21(1):639–57. doi: 10.1146/annurev.publhealth.21.1.639. [DOI] [PubMed] [Google Scholar]
- Ricketts TC. Workforce Issues in Rural Areas: A Focus on Policy Equity. American Journal of Public Health. 2005;95(1):42–8. doi: 10.2105/AJPH.2004.047597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricketts TC, Savitz L. Access to Health Services. In: Ricketts TC, Savitz LA, Gesler WM, Osborne DN, editors. Geographic Methods for Health Services Research. Lanham, MD: University Press of America; 1994. pp. 91–119. [Google Scholar]
- Robinson DF, Savage GT, Campbell KS. Organizational Learning, Diffusion of Innovation, and International Collaboration in Telemedicine. Health Care Management Review. 2003;28(1):68–78. doi: 10.1097/00004010-200301000-00008. [DOI] [PubMed] [Google Scholar]
- Rodgers TL, Anderson EE, Manning T. 2003. Impact of Technology Sustainability on Healthcare Governance. Proceedings of the 36th Annual Hawaii International Conference on System Sciences, pp. 170–80. Hawaii.
- Rogers EM. Diffusion of Innovations. New York: Free Press; 2003. [Google Scholar]
- Rosenthal MB, Zaslavsky A, Newhouse JP. The Geographic Distribution of Physicians Revisited. Health Services Research. 2005;40(6, part 1):1931–52. doi: 10.1111/j.1475-6773.2005.00440.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders J, Salter P, Stachura M. The Unique Application of Telemedicine to the Managed Healthcare System. American Journal of Managed Care. 1996;2:551–4. [Google Scholar]
- Sanders JH, Bashshur RL. Challenges to the Implementation of Telemedicine. Telemedicine Journal. 1995;1(2):115–23. doi: 10.1089/tmj.1.1995.1.115. [DOI] [PubMed] [Google Scholar]
- Shea S, Weinstock RS, Starren J, Teresi J, Palmas W, Field L, Morin P, Goland R, Izquierdo RE, Wolff LT. A Randomized Trial Comparing Telemedicine Case Management with Usual Care in Older, Ethnically Diverse, Medically Underserved Patients with Diabetes Mellitus: 5 Year Results of the IDEA Tel Study. Journal of the American Medical Informatic Association. 2006;16(4):446–56. doi: 10.1197/jamia.M1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shortell SM. The Emergence of Qualitative Methods in Health Services Research. Health Services Research. 1999;34(5, part 2):1083–90. [PMC free article] [PubMed] [Google Scholar]
- Slifkin RT, Silberman P, Reif S. The Effect of Medicaid Managed Care on Rural Public Health Departments. The Journal of Rural Health. 2001;17(3):187–96. doi: 10.1111/j.1748-0361.2001.tb00956.x. [DOI] [PubMed] [Google Scholar]
- Sofaer S. Qualitative Methods: What Are They and Why Use Them. Health Services Research. 1999;34(5):1101–18. [PMC free article] [PubMed] [Google Scholar]
- Stachura ME. The Georgia State-Wide Telemedicine Network: Some Lessons Learned. Journal of Telemedicine and Telecare. 2001;7(suppl 2):62–3. doi: 10.1258/1357633011937164. [DOI] [PubMed] [Google Scholar]
- US Government. American Recovery and Reinvestment Act. Washington, DC: US Government Printing Office; 2009. [Google Scholar]
- Van de Ven AH, Poole MS. Methods for Studying Innovation Development in the Minnesota Innovation Research Program. Organization Science. 1990;1(3):313–35. [Google Scholar]
- Walker JB. “The Future of Public Health”: The Institute of Medicine's 1988 Report. Journal of Public Health Policy. 1989;10(1):19–31. [PubMed] [Google Scholar]
- Wellever A, Brennan J, Bryan D, Faubion J. Local Public Health at the Crossroads: The Structure of Health Departments in Rural Areas. Topeka, KS: Kansas Health Institute; 2006. [Google Scholar]
- Whittaker SL, Adkins S, Phillips R, Jones J, Horsley MA, Kelley G. Success Factors in the Long-Term Sustainability of a Telediabetes Programme. Journal of Telemedicine and Telecare. 2004;10(2):84–8. doi: 10.1258/135763304773391512. [DOI] [PubMed] [Google Scholar]
- Whitten PS, Allen A. Analysis of Telemedicine from an Organizational Perspective. Telemedicine Journal. 1995;1(3):203–13. doi: 10.1089/tmj.1.1995.1.203. [DOI] [PubMed] [Google Scholar]
- Winters SR. Diagnosis by Wireless. Scientific American. 1921;124:465. [Google Scholar]
- Wright D. The Sustainability of Telemedicine Projects. Journal of Telemedicine and Telecare. 1999;5(1):107–11. doi: 10.1258/1357633991932784. [DOI] [PubMed] [Google Scholar]
- Yin RK. Enhancing the Quality of Case Studies in Health Services Research. Health Services Research. 1999;34(5):1209–24. [PMC free article] [PubMed] [Google Scholar]
- Yin RK. Case Study Research: Design and Methods. Thousand Oaks, CA: Sage; 2003. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


