Abstract
Objective
To determine whether there would be racial and ethnic disparities in meeting eligibility criteria for medication therapy management (MTM) services implemented in 2006 for Medicare beneficiaries.
Data Sources/Study Setting
Secondary data analyses of the Medical Expenditure Panel Survey (2004–2005).
Study Design
Logistic regression and recycled predictions were used to test the disparities in meeting eligibility criteria across racial and ethnic groups. The eligibility thresholds used by health plans in 2006 and new thresholds recommended for 2010 were examined. Racial and ethnic disparities were examined by comparing non-Hispanic blacks (blacks) with non-Hispanic whites (whites) and comparing Hispanics with whites, respectively. Disparities were also examined among individuals with severe health problems.
Principal Findings
According to 2006 thresholds, the adjusted odds ratios for meeting eligibility criteria for blacks and Hispanics to whites were 0.36–0.60 (p<.05) and 0.13–0.46 (p<.05), respectively. Blacks and Hispanics would be 21–34 and 32–38 percent, respectively, less likely to be eligible than whites according to recycled predictions. Similar patterns were found using the 2010 eligibility thresholds and among individuals with severe health problems.
Conclusions
There would be racial and ethnic disparities in meeting MTM eligibility criteria. Future research is warranted to confirm the findings using data after MTM implementation.
Keywords: Disparity, MTM services, eligibility criteria, race, ethnicity
Effective January 1, 2006, the Centers for Medicare and Medicaid Services (CMS), Department of Health and Human Services (2005) required that health plans provide medication therapy management (MTM) services for Medicare beneficiaries as part of their outpatient prescription drug benefit, or Part D benefit. MTM services consist of a distinct group of services to optimize therapeutic outcomes (American Pharmacists Association and National Association of Chain Drug Stores Foundation 2005; Bluml 2005;). Its core components are the formulation of a medication treatment plan and the integration of medication management within the broader context of all health services provided to patients (American Pharmacists Association and National Association of Chain Drug Stores Foundation 2005). The value of MTM has been increasingly accepted because of its effectiveness in improving therapeutic outcomes in a cost-effective fashion, particularly among patients with chronic diseases (Cranor and Christensen 2003; Etemad and Hay 2003; Smith et al. 2006; Fera, Bluml, and Ellis 2009;). By more appropriately managing the patient's disease, there are improved health outcomes that lead to downstream medical cost reductions. For instance, in the American Pharmacists Association Foundation's Diabetes Ten City Challenge, community pharmacists at 10 geographic sites contracted with 29 employers to identify and resolve drug therapy problems and coach patients on diabetes self-management. As a result of these efforts, over an average period of 14.8 months, patients experienced significant clinical and economic benefits; the average glycosylated hemoglobin decreased from 7.5 to 7.1 percent (p=.002), average low-density lipoprotein cholesterol decreased from 98 to 94 mg/dl (p<.001), and annual health care costs per patient decreased by U.S.$1,079 (7.2 percent) from the projected costs (Fera, Bluml, and Ellis 2009).
According to the original 2003 guidelines, CMS requires MTM to be provided to targeted beneficiaries meeting three criteria (CMS, Department of Health and Human Services 2005): (1) having multiple chronic conditions, (2) using multiple covered drugs, and (3) being likely to incur over U.S.$4,000 (in 2006 dollars) in annual Part D drug costs.
The thresholds for MTM eligibility criteria have been evolving since the inception of the program. According to CMS, in 2006, the eligibility thresholds used by Part D plans based on number of chronic conditions ranged from 2 to 5; the thresholds based on number of Part D drugs ranged from 2 to 23 (CMS 2008). The upper limits of the eligibility thresholds are going to be reduced as required by CMS. According to the March 30, 2009, Call Letter from CMS, which provides information for the Part D plans to bid for contract in 2010, CMS stipulated that the plans cannot require more than eight Part D drugs, three chronic conditions, and a lowered cost threshold of U.S.$3,000 as the MTM eligibility thresholds (CMS 2009).
Individuals who meet the eligibility criteria have more complicated medication regimens than do others, and they are more likely to benefit from MTM services. Therefore, by restricting MTM to qualified individuals, CMS strives to move America's health care to a value-based system (Edgar 2006). However, racial and ethnic minorities may have a lower likelihood of meeting eligibility criteria for MTM. The reason is that MTM eligibility criteria 2 and 3 are predominantly based on drug utilization, while previous research has shown that blacks and Hispanics are apt to use fewer prescription drugs compared with their non-Hispanic white (whites) counterparts (Briesacher, Limcangco, and Gaskin 2003; Schore, Brown, and Lavin 2003; Wang et al. 2006, 2007a, b). Regarding eligibility criterion 1, existing literature has documented that minority groups have a higher incidence of developing certain diseases than do their majority counterparts (Institute of Medicine 2002; Byrd, Fletcher, and Menifield 2007;). Nonetheless, it is not clear whether minority groups are more or less likely than their majority counterparts to exceed a certain number of chronic conditions (Institute of Medicine 2002; Byrd, Fletcher, and Menifield 2007;).
Examining the disparity implications of MTM eligibility criteria can inform the policy- and decision-making process for the federal government and health insurance plans that manage Medicare beneficiaries' health care services. CMS designed the MTM eligibility criteria in a flexible manner to encourage their evolution (Edgar 2006), and examining the disparity implications of MTM eligibility criteria can provide for the evolution of MTM services an important consideration related to racial and ethnic disparities. Without examining the disparity implications of MTM eligibility criteria, equity concerns may continue to be ignored in the evolution of the MTM criteria. For example, some researchers already have suggested refining the MTM criteria by focusing only on the drug cost criterion of the MTM eligibility criteria (Daniel and Malone 2007). They made this suggestion because they found that there is a redundancy in the eligibility criteria. For example, approximately 97 percent of the older adults who exceeded the drug cost threshold for MTM (criterion 3) also had two or more chronic diseases (criterion 1) (Daniel and Malone 2007). While these suggestions can increase efficiency, equity concerns were further ignored.
Using historical data, this study was conducted to examine whether there would be racial and ethnic disparities in meeting MTM eligibility criteria among Medicare beneficiaries. There were three specific study objectives: (1) to test the hypothesis that non-Hispanic blacks (blacks) and Hispanics would have a lower likelihood of meeting MTM eligibility criteria than would whites according to the eligibility thresholds used by Part D plans in 2006, (2) to test the hypothesis that blacks and Hispanics would have a lower likelihood of meeting MTM eligibility criteria than would whites according to the new CMS eligibility thresholds for 2010, and (3) to test the hypothesis that blacks and Hispanics would have a lower likelihood of meeting MTM eligibility criteria than would whites among Medicare beneficiaries with severe health problems.
Methodology
Conceptual Framework
The MTM eligibility criteria are predominantly based on the utilization of pharmaceutical products and health services. Even the criterion based on the number of chronic conditions reflects health services utilization because medical conditions have to be diagnosed during physician visits. Therefore, this study used as its conceptual framework Andersen's Behavioral Model of Health Services Utilization. According to this model, the utilization of health services is determined by three groups of factors: predisposing factors, enabling factors, and need factors; the utilization of health services then leads to improved patient satisfaction and improved health outcomes (Andersen and Davidson 2001). Among the determinants of health services utilization, predisposing factors, including race, ethnicity, age, gender, and marital status, “predispose” individuals to the utilization of health services. Enabling factors, including income, health insurance, education, and region of residence, “enable” individuals to utilize health services. Need factors, such as health status perceived by health care providers or patients, reflect individuals' need for services.
Data Source
This study is a retrospective analysis of the Medicare beneficiaries in the Medical Expenditure Panel Survey (MEPS) (Agency for Healthcare Research and Quality 2009). MEPS is a federal survey cosponsored by the Agency for Healthcare Research and Quality and the National Center for Health Statistics with a purpose of producing national estimates of health expenditures, sources of payment, and insurance coverage in the United States. MEPS data have been collected annually since 1996 from nationally representative samples of noninstitutionalized U.S. civilians. The most recent complete data were from 2006 at the time of this analysis (Agency for Healthcare Research and Quality 2009).
This study used MEPS data from 2004 and 2005. Data from 2 years were combined to have adequate statistical power. Data from 2006 were not used because MTM and Medicare Part D were both implemented in 2006, resulting in a major change in coverage in 2006. This suggests that it is not appropriate to combine 2006 data with data from previous years. Furthermore, Medicare beneficiaries had until May 15, 2006 to enroll in Medicare Part D without incurring a penalty of higher monthly premiums (CMS, Department of Health and Human Services 2005). Therefore, data after May 15, 2006, or from even later years may be more reliable while plans and patients are more likely to have gone over the learning curve. Nonetheless, data from 2006 were analyzed in a sensitivity analysis.
From the MEPS data files, the following information was obtained for each survey respondent: (1) sociodemographic characteristics including race and ethnicity, health status, and use of medications and health services; (2) characteristics of each medical condition that a survey respondent reported; (3) each prescribed medicine event, including the drug name. Race and ethnicity were self-reported in MEPS.
Determining MTM Eligibility According to 2006 Thresholds
If one is to determine the disparity implications of the eligibility criteria, it is reasonable to examine the ranges of the thresholds represented by three data points: the upper limit, median, and lower limit. For example, the MTM eligibility thresholds in 2006 had the following patterns: the threshold based on the number of Part D drugs ranged from 2 to 23 (median=5); the threshold based on the number of chronic conditions ranged from 2 to 5 (median=3); and the threshold based on Part D drug costs was constant at U.S.$4,000 (CMS 2008). Because an individual had to meet all three criteria to be eligible for MTM, one needs to determine just the disparity implications of 3 × 3 × 1=9 different combinations of the thresholds.
We conducted both main analysis and sensitivity analyses. In the main analysis, we examined racial and ethnic disparities in meeting MTM eligibility criteria for the criteria represented by the median values of the 2006 thresholds used by Part D plans. All other eight combinations of the eligibility thresholds were included in the sensitivity analyses.
Determining eligibility based on the number of Part D drugs and the total Part D drug costs was based on drug use information directly available in MEPS. All prescription drugs were included rather than only “Part D drugs” because of the wide variety of Part D plans (CMS, Department of Health and Human Services 2005). When determining eligibility based on the number of chronic conditions, we based this on a raw count of medical conditions among a list of 25 chronic conditions. This list of medical conditions was developed by Daniel and Malone (2007) as applicable to Medicare beneficiaries. This list of medical conditions was based on clinical classification codes that were developed in MEPS by aggregating ICD-9 codes. Each of the clinical classification codes represents a clinical classification category; for example, code “5” is for HIV infection and “127” is for chronic obstructive pulmonary disease and bronchiectasis.
Disparity Implications of the Eligibility Thresholds
We included three major racial and ethnic groups: whites, non-Hispanic blacks (blacks), and Hispanics. By including these racial and ethnic groups, we could examine both racial and ethnic disparities. Racial disparities were examined by comparing whites with blacks, and ethnic disparities were examined by comparing whites with Hispanics. Other racial and ethnic groups were excluded from further analysis because the sample sizes of these groups were too small to provide sufficient statistical power to detect meaningful differences between them and other groups. Additionally, fewer than 0.001 percent of the individuals in our study sample reported more than one racial group. They were excluded from the analysis because their small sample sizes did not warrant the technical complexity of including them in the analyses.
For study objective 1, we tested the hypothesis that blacks and Hispanics would have a lower likelihood of meeting MTM eligibility criteria than would whites according to the eligibility thresholds used by Part D plans in 2006. We examined racial and ethnic disparities in meeting eligibility criteria for each unique combination of the 2006 eligibility criteria using bivariate analysis and multivariate analyses. For the bivariate analyses, we first used a survey-weighted χ2-test to determine the statistical differences in the likelihood of meeting eligibility criteria by racial and ethnic groups. Additionally, to explore how each eligibility criterion contributed to potential disparities, we used a similar method to examine the likelihood of exceeding the thresholds for each eligibility criterion. For the multivariate analyses, we used a survey-weighted logistic regression in the following model:
| (Model 1) |
where Y is the dependent variable of the model defined as whether one meets the eligibility criteria. “Race” is a vector of dummy variables for racial and ethnic groups, including blacks and Hispanics (whites is the reference group). “Sociodemo” includes all sociodemographic characteristics and “Health_Status” includes all health-related characteristics as determined by Andersen's Behavioral Model of Health Services Utilization (Andersen and Davidson 2001). We included predisposing factors measured by age, gender, and marital status (married or not); enabling factors measured by education (highest degree achieved), whether an individual had Medicaid, whether an individual had private insurance, income categories (poor, near poor, low income, middle income, and high income), whether an individual resided in a metropolitan statistical area, census region in which an individual resided (Northeast, Midwest, West, and South); and need factors measured by self-perceived health status (excellent, very good, good, fair, and poor) and whether an individual was eligible for Medicare because of disabilities (Andersen and Davidson 2001). ɛ is an error term. In the results from the logistic regression, an adjusted odds ratio for blacks to whites lower than 1, for example, would indicate that blacks would have a lower likelihood of being eligible for MTM than would whites.
For study objective 2, we tested the hypothesis that blacks and Hispanics would have a lower likelihood of meeting MTM eligibility than would whites according to the new CMS eligibility thresholds for 2010. For this study objective, survey-weighted χ2-tests and survey-weighted logistic regressions were used, similar to those for study objective 1. While upper limits for the new CMS eligibility thresholds for 2010 were reduced from the 2006 thresholds, we assumed that the lower limits of eligibility thresholds would stay the same in 2010 as in 2006 because the lower limits of two chronic conditions and two Part D drugs in 2006 already were rather low.
Study objective 3 tested the hypothesis that blacks and Hispanics would have a lower likelihood of meeting MTM eligibility criteria than would whites among Medicare beneficiaries with severe health problems. For this study objective, we used methods similar to those in study objective 1. Individuals with “severe health problems” were defined as Medicare beneficiaries belonging to two groups: those having reported fair or poor health (versus excellent, very good, and good health), and those having reported any limitations with daily activities such as activities of daily living. This definition is based on a previous study among Medicare beneficiaries (Riley 2000). A further sensitivity analysis was conducted that included individuals who reported fair or poor health (versus excellent, very good, or good health).
Finally, because odds ratios produced by logistic regressions are harder to interpret than probabilities are, we used the method of recycled predictions to determine the disparities in the probabilities of meeting MTM eligibility criteria. For example, when estimating the differences between whites and blacks, we first estimated the logistic regression models including only whites and blacks in the sample; we then estimated the predicted probabilities of meeting eligibility criteria under the assumption that all in the sample were whites and all other variables remained the same; we further estimated the predicted probabilities of meeting eligibility criteria assuming all in the sample were blacks and all other variables remained the same; finally, we compared the averages of these two predicted probabilities and produced a new estimate of the difference between blacks and whites. The differences between whites and Hispanics were estimated in a similar manner.
All data analyses above took into account the complex survey design of MEPS, including primary sampling units, strata, and personal weights. This study was approved by the Institutional Review Board. Data analyses were conducted using the survey data analysis procedures in SAS 9.2 (SAS Institute Inc., Cary, NC) and Stata (StataCorp LP, College Station, TX). The statistical significance level was set a priori at 0.05.
Results
Characteristics of the Population
The study sample included 8,454 (weighted to 80,725,686) Medicare beneficiaries in MEPS in 2004 and 2005. Within the study sample, 5,888 (weighted to 66,418,455 or 82.28 percent) were white, 1,330 (weighted to 8,419,373 or 10.43 percent) were black, and 1,236 (weighted to 5,887,858 or 7.29 percent) were Hispanic. The differences between whites and minorities were significant for all characteristics except gender (Table 1; p<.05): minorities were more likely to belong to the younger age groups than were whites; compared with whites, minorities were less likely to be married, less likely to have advanced degrees, more likely to have Medicaid, less likely to have private insurance, less likely to belong to higher income categories, less likely to have reported better health categories, and more likely to be eligible for Medicare because of disabilities. Minorities and whites also had different geographic distributions across census regions. Minorities were more likely to reside in metropolitan statistical areas than were whites.
Table 1.
Sociodemographic Characteristics of Individuals across Racial and Ethnic Groups in 2004–2005
| Non-Hispanic Whites (N=5,888; Weighted to 66,418,455) |
Non-Hispanic Blacks (N=1,330;Weighted to 8,419,373) |
Hispanics (N=1,236; Weighted to 5,887,858) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics* | Groups | Number | Weighted Number | Weighted (%) | Number | Weighted Number | Weighted (%) | Number | Weighted Number | Weighted (%) |
| Age (years) | <65 | 876 | 8,423,844 | 12.77 | 397 | 2,411,607 | 29.02 | 340 | 1,456,171 | 24.94 |
| 65–74 | 2,544 | 29,328,292 | 44.45 | 502 | 3,410,309 | 41.04 | 527 | 2,613,504 | 44.76 | |
| 75–84 | 1,870 | 21,536,346 | 32.64 | 305 | 1,877,177 | 22.59 | 292 | 1,476,351 | 25.29 | |
| ≥85 | 557 | 6,697,811 | 10.15 | 109 | 609,816 | 7.34 | 66 | 292,316 | 5.01 | |
| Gender | Female | 3,362 | 37,467,430 | 56.41 | 832 | 5,024,142 | 59.67 | 733 | 3,285,454 | 55.80 |
| Marital status | Married | 3,084 | 35,949,340 | 54.13 | 380 | 2,597,142 | 30.85 | 508 | 2,496,673 | 42.40 |
| Education | Lower than high school | 1,644 | 15,973,126 | 24.27 | 656 | 3,724,623 | 46.12 | 826 | 3,547,169 | 65.15 |
| High school | 2,838 | 32,993,550 | 50.14 | 461 | 3,186,628 | 39.46 | 212 | 1,355,315 | 24.89 | |
| Bachelor | 619 | 7,941,488 | 12.07 | 57 | 493,228 | 6.11 | 36 | 247,837 | 4.55 | |
| Master and higher | 419 | 5,118,924 | 7.78 | 46 | 336,386 | 4.17 | 13 | 99,382 | 1.83 | |
| Other degree | 313 | 3,776,696 | 5.74 | 49 | 334,778 | 4.15 | 27 | 194,579 | 3.57 | |
| Health insurance | With Medicaid | 836 | 6,976,373 | 10.50 | 560 | 3,116,208 | 37.01 | 678 | 2,676,460 | 45.46 |
| With private insurance | 3,227 | 38,923,017 | 58.60 | 362 | 2,630,470 | 31.24 | 215 | 1,470,970 | 24.98 | |
| Poverty status† | Negative or poor | 843 | 6,686,090 | 10.07 | 475 | 2,343,541 | 27.84 | 410 | 1,349,007 | 22.91 |
| Near poor | 414 | 3,937,555 | 5.93 | 138 | 850,070 | 10.10 | 166 | 775,061 | 13.16 | |
| Low income | 1,088 | 12,837,561 | 19.33 | 281 | 2,149,298 | 25.53 | 273 | 1,368,811 | 23.25 | |
| Middle income | 1,701 | 19,990,653 | 30.10 | 293 | 2,022,119 | 24.02 | 269 | 1,440,006 | 24.46 | |
| High income | 1,842 | 22,966,597 | 34.58 | 143 | 1,054,345 | 12.52 | 118 | 954,972 | 16.22 | |
| U.S. Census regions | Northeast | 1,058 | 13,308,870 | 20.74 | 173 | 1,487,089 | 18.30 | 142 | 834,819 | 14.51 |
| Midwest | 1,459 | 15,677,492 | 24.43 | 237 | 1,505,951 | 18.53 | 42 | 311,462 | 5.41 | |
| South | 2,164 | 22,923,803 | 35.72 | 775 | 4,486,665 | 55.21 | 481 | 2,226,922 | 38.70 | |
| West | 1,019 | 12,258,417 | 19.10 | 98 | 646,132 | 7.95 | 543 | 2,381,769 | 41.39 | |
| Metropolitan statistical areas | Yes | 4,083 | 48,523,522 | 75.62 | 1,075 | 7,024,273 | 86.44 | 1,068 | 5,298,706 | 92.07 |
| Self-perceived health status | Excellent | 745 | 9,380,038 | 14.84 | 119 | 727,434 | 9.04 | 112 | 584,454 | 10.26 |
| Very good | 1,514 | 17,901,580 | 28.33 | 217 | 1,479,155 | 18.38 | 214 | 1,130,286 | 19.85 | |
| Good | 1,795 | 20,115,815 | 31.83 | 408 | 2,718,803 | 33.78 | 380 | 1,841,917 | 32.34 | |
| Fair | 1,037 | 10,634,968 | 16.83 | 373 | 2,257,225 | 28.04 | 329 | 1,387,224 | 24.36 | |
| Poor | 517 | 5,167,052 | 8.18 | 151 | 866,653 | 10.77 | 161 | 751,127 | 13.19 | |
| Disability eligibility | Yes | 917 | 8,856,005 | 13.33 | 414 | 2,522,071 | 29.96 | 351 | 1,505,687 | 25.57 |
p<.05 between non-Hispanic whites and both minority groups (non-Hispanic blacks and Hispanics) for all variables except gender.
Categories of poverty status: negative income or poor, <100% of poverty line; near poor, 100–<125% of poverty line; low income, 125–<200%; middle income, 200–<400%; high income, 400% and greater.
Disparities in MTM Eligibility for 2006 Thresholds
According to bivariate analyses, the would-be proportion of blacks meeting MTM eligibility criteria was similar to that of whites, while the proportion of Hispanics was lower than that of whites (Table 2). For example, according to the main analysis, the proportions of eligible individuals would be 13.22 percent among whites, 13.19 percent among blacks, and 8.98 percent among Hispanics. The difference between whites and blacks was not significant, but the difference between whites and Hispanics was significant (Table 2). The sensitivity analyses had similar findings.
Table 2.
Numbers and Proportions of Individuals across Racial and Ethnic Groups Who Would Be Eligible for Medication Therapy Management Services According to 2006 Eligibility Criteria
| Analyses | Number of Part D Drugs | Number of Chronic Conditions | Groups | Number Eligible | Number Eligible Weighted | Proportion Eligible (%) |
|---|---|---|---|---|---|---|
| Main analysis | ≥5 | ≥3 | Whites | 867 | 8,779,481 | 13.22 |
| Blacks | 182 | 1,110,706 | 13.19 | |||
| Hispanics* | 120 | 528,912 | 8.98 | |||
| Sensitivity analysis 1 | ≥5 | ≥2 | Whites | 933 | 9,563,500 | 14.40 |
| Blacks | 189 | 1,150,347 | 13.66 | |||
| Hispanics* | 127 | 555,586 | 9.44 | |||
| Sensitivity analysis 2 | ≥5 | ≥5 | Whites | 610 | 6,026,502 | 9.07 |
| Blacks | 113 | 713,199 | 8.47 | |||
| Hispanics* | 79 | 357,726 | 6.08 | |||
| Sensitivity analysis 3 | ≥2 | ≥3 | Whites | 881 | 8,954,796 | 13.48 |
| Blacks | 184 | 1,115,810 | 13.25 | |||
| Hispanics* | 122 | 548,159 | 9.31 | |||
| Sensitivity analysis 4 | ≥2 | ≥2 | Whites | 955 | 9,822,706 | 14.79 |
| Blacks | 192 | 1,158,809 | 13.76 | |||
| Hispanics* | 132 | 592,735 | 10.07 | |||
| Sensitivity analysis 5 | ≥2 | ≥5 | Whites | 612 | 6,047,933 | 9.11 |
| Blacks | 113 | 713,199 | 8.47 | |||
| Hispanics* | 80 | 360,974 | 6.13 | |||
| Sensitivity analysis 6 | ≥23 | ≥3 | Whites | 81 | 855,214 | 1.29 |
| Blacks | 13 | 64,437 | 0.77 | |||
| Hispanics* | 6 | 19,081 | 0.32 | |||
| Sensitivity analysis 7 | ≥23 | ≥2 | Whites | 82 | 865,775 | 1.30 |
| Blacks | 13 | 64,437 | 0.77 | |||
| Hispanics* | 6 | 19,081 | 0.32 | |||
| Sensitivity analysis 8 | ≥23 | ≥5 | Whites | 75 | 814,490 | 1.23 |
| Blacks | 13 | 64,437 | 0.77 | |||
| Hispanics* | 6 | 19,081 | 0.32 |
Note. Whites, non-Hispanic whites; Blacks, non-Hispanic blacks; total Part D drugs costs >4,000 in 2006 dollars for all analyses.
p<.05 compared with whites.
We calculated the proportions of individuals that would exceed a certain eligibility threshold based on each eligibility criterion (results not shown). We found that, for most eligibility thresholds, the proportion of eligible blacks would be similar to that of whites, while the proportion of Hispanics would be lower than that of whites. This pattern held for both the criteria based on Part D drugs and the criterion based on the number of chronic conditions.
In the multivariate analysis, the adjusted odds ratios of meeting eligibility criteria for blacks and Hispanics to whites were produced using a survey-weighted logistic regression (Table 3). According to the main analysis (Table 3), the adjusted odds ratios for blacks and Hispanics to whites were 0.60 and 0.46. These data suggested that the odds for blacks and Hispanics to meet eligibility thresholds represented by the main analysis would be 40 and 54 percent lower than for whites, respectively. Using the method of recycled predictions, the proportions of blacks and Hispanics meeting eligibility thresholds were found to be 28 and 35 percent lower than for whites, respectively.
Table 3.
Racial and Ethnic Disparities in Meeting the 2006 Eligibility Criteria for Medication Therapy Management Services According to a Logistic Regression (Main Analysis)*
| Coefficient | Odd Ratio (OR) | Confidence Interval of OR | Standard Error | χ2 | p | |
|---|---|---|---|---|---|---|
| Intercept | −3.37 | — | — | 0.57 | 34.96 | <.0001 |
| Non-Hispanic whites | — | — | — | — | — | — |
| Non-Hispanic blacks | −0.52 | 0.60 | 0.45–0.79 | 0.14 | 13.01 | .00 |
| Hispanics | −0.78 | 0.46 | 0.32–0.66 | 0.19 | 17.66 | <.0001 |
| Age | 0.01 | 1.01 | 1.00–1.02 | 0.01 | 1.20 | .27 |
| Female | — | — | — | — | — | — |
| Male | −0.37 | 0.69 | 0.58–0.82 | 0.09 | 18.02 | <.0001 |
| Not married | — | — | — | — | — | — |
| Married | −0.18 | 0.84 | 0.68–1.03 | 0.10 | 2.84 | .09 |
| With Medicaid | 0.44 | 1.55 | 1.18–2.04 | 0.14 | 10.12 | .00 |
| With any private insurance | 0.08 | 1.08 | 0.89–1.31 | 0.10 | 0.64 | .42 |
| Negative income or poor† | — | — | — | — | — | — |
| Near poor | 0.04 | 1.05 | 0.77–1.42 | 0.16 | 0.08 | .78 |
| Low income | −0.11 | 0.89 | 0.70–1.14 | 0.12 | 0.83 | .36 |
| Middle income | −0.20 | 0.82 | 0.63–1.07 | 0.13 | 2.17 | .14 |
| High income | −0.04 | 0.96 | 0.71–1.28 | 0.15 | 0.09 | .77 |
| Lower than high school education | — | — | — | — | — | — |
| High school | −0.10 | 0.91 | 0.74–1.11 | 0.11 | 0.88 | .35 |
| Bachelor | −0.02 | 0.98 | 0.68–1.41 | 0.19 | 0.01 | .91 |
| Master and higher | 0.10 | 1.11 | 0.71–1.73 | 0.23 | 0.20 | .65 |
| Other degree | 0.12 | 1.13 | 0.81–1.59 | 0.17 | 0.51 | .47 |
| Census region “Northeast” | — | — | — | — | — | — |
| Census region “Midwest” | 0.32 | 1.37 | 0.96–1.96 | 0.18 | 3.04 | .08 |
| Census region “South” | −0.05 | 0.95 | 0.67–1.35 | 0.18 | 0.08 | .78 |
| Census region “West” | −0.34 | 0.71 | 0.48–1.04 | 0.20 | 3.08 | .08 |
| Non-metropolitan statistical area | — | — | — | — | — | — |
| Metropolitan statistical area | 0.16 | 1.18 | 0.93–1.50 | 0.12 | 1.77 | .18 |
| Self-perceived excellent health status | — | — | — | — | — | — |
| Self-perceived very good health status | 0.29 | 1.34 | 0.89–2.01 | 0.21 | 1.93 | .16 |
| Self-perceived good health status | 1.07 | 2.92 | 1.99–4.28 | 0.20 | 29.80 | <.0001 |
| Self-perceived fair health status | 1.68 | 5.38 | 3.65–7.92 | 0.20 | 72.42 | <.0001 |
| Self-perceived poor health status | 2.25 | 9.52 | 6.33–14.32 | 0.21 | 117.23 | <.0001 |
| Disability eligibility | 0.74 | 2.09 | 1.48–2.95 | 0.18 | 17.45 | <.0001 |
Wald's statistic: 504.08 (p<.0001).
Categories of poverty status: negative income or poor, <100% of poverty line; near poor, 100–<125% of poverty line; low income, 125–<200%; middle income, 200–<400%; high income, 400% and greater.
When the adjusted odds ratios for all analyses were taken into consideration (Figure 1), the following two general patterns can be seen: (1) the adjusted odds ratios stayed lower than one (range 0.36–0.60, p<.05), which suggested that the odds for blacks to meet the eligibility criteria would be 40–64 percent lower than for whites; (2) higher thresholds for the number of Part D drugs appeared to be associated with lower adjusted odds ratios and, thus, greater disparities. The proportions of blacks meeting eligibility thresholds were found to be 21–34 percent lower than for whites.
Figure 1.
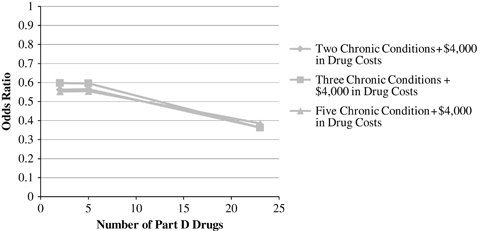
Adjusted Odds Ratios of Medication Therapy Management Eligibility Fulfillment for Non-Hispanic Blacks to Non-Hispanic Whites According to Eligibility Thresholds in 2006 (Each Line Represents a Different Threshold Based on the Number of Chronic Conditions)
The same general patterns can be seen for Hispanics (Figure 2): (1) the adjusted odds ratios were always lower than 1 (range 0.13–0.46, p<.05), which suggested that the odds for Hispanics to be eligible for MTM would be 54–87 percent lower than for whites; (2) higher thresholds for the number of Part D drugs appeared to be associated with lower adjusted odds ratios and, thus, greater disparities. Using recycled predictions, we found that the proportions of Hispanics meeting eligibility thresholds were 32–38 percent lower than for whites.
Figure 2.
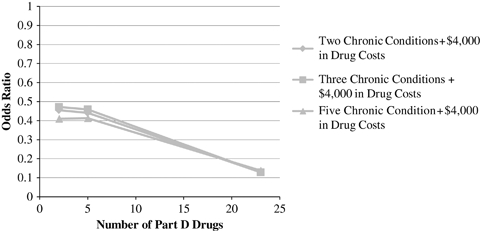
Adjusted Odds Ratios of Medication Therapy Management Eligibility Fulfillment for Hispanics to Non-Hispanic Whites According to Eligibility Thresholds in 2006 (Each Line Represents a Different Threshold Based on the Number of Chronic Conditions)
Disparities Associated with the 2010 CMS Eligibility Thresholds
This part of the analyses produced findings similar to those analyses for the 2006 eligibility thresholds. (1) According to the bivariate analysis, the proportion of blacks meeting MTM eligibility criteria would be similar to that among whites, while the proportion among Hispanics would be lower than that for whites (p<.05). (2) According to the multivariate analyses, all adjusted odds ratios for blacks and Hispanics were lower than 1 (ranges 0.65–0.71 and 0.48–0.59, respectively), which suggested that blacks and Hispanics would still have a lower likelihood of meeting eligibility criteria compared with whites (p<.05). (3) Higher thresholds based on the number of Part D drugs appeared to be associated with greater racial and ethnic disparities. Based on the method of recycled predictions, the proportions of blacks and Hispanics meeting eligibility criteria would be 22–32 percent and 34–39 percent lower, respectively, than that of whites.
We compared the 2006 thresholds and 2010 thresholds on disparity implications by comparing the confidence intervals for the odds ratios when the upper limits of the eligibility thresholds were examined. The confidence intervals for the odds ratios for blacks to whites overlapped for the two sets of thresholds (0.17–0.86 for 2006 criteria; and 0.50–0.91 for 2010 criteria). The confidence intervals for Hispanics to whites also overlapped (0.04–0.69 for 2006 criteria and 0.35–0.78 for the 2010 criteria, respectively). The confidence intervals based on the methods of recycled predictions overlapped in both comparisons.
Disparities among Medicare Beneficiaries with Severe Health Problems
This part of the analysis, which included 27 percent of the overall study sample, produced similar patterns as the above analyses. In particular, according to the 2006 criteria, the range of adjusted odds ratios for blacks to whites was 0.38–0.56 (p<.05); the range of adjusted odds ratios for Hispanics to whites was 0.09–0.45 (p<.05). According to the 2010 criteria, the range of the adjusted odds ratios for blacks to whites was 0.63–0.68 (p<.05); the range of adjusted odds ratios for Hispanics to whites was 0.59–0.66 (p<.05). Analyses based on the sensitivity analysis using an alternative definition of “severe health problems” had similar findings.
The analysis of 2006 data produced similar directions of disparities, but some disparities were not significant. This held for all three study objectives (results not shown).
Discussion
Using historical data from a federal survey, this study found that blacks and Hispanics both would have a lower likelihood of being eligible for MTM than would whites according to 2006 criteria and 2010 criteria. Using 2006 data after MTM implementation, similar disparity patterns were found, although some disparity findings were not significant because of inadequate statistical power. Because the MTM eligibility criteria are predominantly based on the use of prescription drugs and health services, these study findings are consistent with previous literature that reported that minorities use fewer prescription drugs and health services than do whites (Briesacher, Limcangco, and Gaskin 2003; Schore, Brown, and Lavin 2003; Wang et al. 2006, 2007a, b).
Andersen's Behavioral Model of Health Services Utilization seems to be a reasonable model to use for this study. For example, in the main analysis in Table 3, the significant variables included predisposing factors (non-Hispanic blacks, Hispanics, and male), enabling factors (with Medicaid), and need factors (self-perceived good, fair, and poor health status, disability eligibility). Previous literature has reported various causes for the lower utilization of health services and pharmaceutical products among minorities than among whites. These causes can again be summarized as predisposing, enabling, and need factors (e.g., Briesacher, Limcangco, and Gaskin 2003; Wang et al. 2006, 2007b, 2008). Regardless of the causes for the lower utilization among racial and ethnic minorities, because MTM eligibility criteria are predominantly based on utilizations, our study found that there would be a lower likelihood of meeting MTM eligibility criteria among racial and ethnic minorities than among whites. Andersen's Behavioral Model of Health Services Utilization then further reminds us that, because of the would-be lower likelihood of meeting eligibility criteria among minorities than among whites, minorities may have lower likelihood of enjoying improved patient satisfaction and improved health outcomes from the use of MTM services compared with whites. The findings of this study have wider implications than Medicare because health plans that offer MTM services also include state Medicaid programs and self-insured employers (Schommer et al. 2008). As the government agency that administers both Medicare and Medicaid, CMS has great influence on all other payers.
MTM is one example of value-based strategies, which are typically based on economic evaluations that do not usually incorporate the distributional effects or equity concerns of the strategies. Equity-efficiency dilemma has characterized the health care systems that formally include economic evaluation in their decision-making processes (Sassi, Le Grand, and Archard 2001). One example of these systems is the British National Health Service (NHS) (Sassi, Le Grand, and Archard 2001). It has been reported that policies to improve economic efficiency are often in direct conflict with the equity doctrine on which the NHS was founded (Sassi, Le Grand, and Archard 2001). There have been few studies on equity concerns of specific value-based strategies in the United States partly because value-based strategies are not common in the United States (Neumann 2005). With the ever-increasing burden of the health care budget, the United States may need to use more value-based strategies in the future.
A health care environment conducive to equal access is pivotal for eliminating health disparities, one of the two overarching goals of Healthy People 2010 (U.S. Department of Health and Human Services 2000). The U.S. government's commitment to eliminate racial and ethnic disparities is all the more justified because of the increasing proportion of the minority populations in the United States. According to the U.S. Census Bureau, 40 percent of the elderly population in the United States will be persons of color by 2050, while this proportion was only 20 percent in 2000 (U.S. Census Bureau 2008).
According to a widely cited framework for the causes of racial and ethnic disparities, if certain systems or policies cause racial and ethnic disparities, these systems and policies are classified as institutionalized causes for disparities (Jones 2000, 2001). Researchers previously have examined institutionalized causes for racial and ethnic disparities in health status. For example, Williams and Collins (2001) suggested that residential segregation determines access to education and employment opportunities and, in turn, creates conditions inimical to health in the physical and social environment.
In this study, we found that, among individuals with severe health problems, blacks and Hispanics still would have a lower likelihood of meeting MTM eligibility criteria than would whites, suggesting further urgency of changing the existing eligibility criteria for MTM. Regarding the previous literature related to the disparities for needy situations, Wang et al. (2006) found that blacks used fewer essential new medications than did whites. The researchers defined new medications as those in the market <5 years and essential drugs as those whose use can prevent worsening medical conditions, hospitalization, or mortality.
Our study findings were based on historical data, and the disparity implications of the MTM eligibility criteria were based on simulation. Therefore, future studies are warranted to confirm our findings using data after MTM implementation. Additionally, this study aimed to determine the would-be disparities in meeting eligibility criteria. Further research should examine whether the proportions of accepting the services differ across racial and ethnic groups when these services are actually offered to patients. This study examined only whether there would be disparities in meeting MTM eligibility criteria but did not determine effective measures to eliminate disparities. Strategies for eliminating disparities in meeting MTM eligibility criteria have national policy implications, so such strategies should be subject to more comprehensive tests.
The merits of this study come with several limitations. First of all, the target population for MEPS is noninstitutionalized civilians, so the study findings may not be generalizable to other populations such as individuals living in nursing homes. Additionally, MEPS data are mainly self-reported and have the potential for error during data collection, editing, and imputation. However, MEPS represents a significant improvement in the quality of pharmacy data over most other surveys, because it also collects information from pharmacy providers frequented by survey respondents, a step rarely taken in other surveys (Agency for Healthcare Research and Quality 2009). MEPS data are frequently used in important studies and federal reports (Agency for Healthcare Research and Quality 2005, 2007). When determining MTM eligibility, we have included all drugs rather than only Part D drugs; without a universal list of chronic conditions used by Part D plans, we used 25 medical conditions devised by Daniel and Malone (2007). All these strategies, although well thought through, may have caused some inaccuracy in the estimation of would-be disparities. Nonetheless, the internal validity of this study is boosted because the eligibility thresholds for the MTM criteria are clearly defined, and our findings on racial and ethnic disparities are rather robust. Additionally, this study had similar findings as a CMS report on the proportions of individuals eligible for MTM. According to the main analysis for 2006 thresholds, the proportions of eligible individuals represent approximately 10 percent for each racial and ethnic group. Although these are would-be proportions, they are consistent with the CMS report on the proportion of MTM enrollees among the Part D beneficiaries in 2006 (CMS 2008). This consistency attests to the reliability of our findings.
Conclusions
This study found that both blacks and Hispanics would have a lower likelihood of meeting MTM eligibility criteria than would whites based on the eligibility thresholds used by Part D plans in 2006 and the new CMS eligibility thresholds for 2010. These disparity patterns also were found among individuals with severe health problems. Therefore, it seems that there is significant urgency for changing the existing MTM eligibility criteria. Future studies are warranted to confirm the findings from this study using data after the MTM implementation, to examine the uptake rates of MTM services across racial and ethnic groups, and to determine effective strategies for eliminating racial and ethnic disparities in meeting MTM eligibility criteria.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: While we have not taken any public stands related to any disparity related to the eligibility requirements for MTM under Medicare Part D, Dr. Brown is an expert in pharmacist-provided MTM and has given several invited presentations related to the value of MTM services and the need for more pharmacists to provide MTM services. He also served as an MTM expert on an environmental scan of Part D MTM Programs study conducted by Abt Associates. The report included a section on the range of eligibility requirements of the various MTM Programs. Dr. Mullins receives consulting income, honoraria, and/or grant support from GlaxoSmithKline, Lilly, Novartis, Pfizer, and Sanofi-Aventis. This study is funded by a Research Starter Grant in Health Outcomes of the Pharmaceutical Research and Manufacturers of America Foundation to Dr. Wang. It was presented as a podium presentation at the American Public Health Association (APHA) Annual Meeting in November 2009 in Philadelphia, PA. An earlier version of this manuscript has won an Honorable Mention for Betty J. Cleckley Minority Issues Research Award from the Gerontological Health Section of APHA in 2009. The authors would like to thank David L. Armbruster, Ph.D., M.A., B.S., professor in library, and Megan F. Saalfrank, M.S., R.D., L.D.N., graduate research assistant, for their editorial assistance.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Agency for Healthcare Research and Quality. 2005. “National Healthcare Disparities Report” [accessed on April 30, 2009]. Available at http://www.ahrq.gov/qual/nhdr05/nhdr05.htm. [DOI] [PubMed]
- Agency for Healthcare Research and Quality. 2007. “National Healthcare Quality Report” [accessed on April 30, 2009]. Available at http://www.ahrq.gov/qual/nhqr05/nhqr05.htm. [DOI] [PubMed]
- Agency for Healthcare Research and Quality. 2009. “Medical Expenditure Panel Survey” [accessed on April 30, 2009]. Available at http://www.meps.ahrq.gov/mepsweb/ [DOI] [PubMed]
- American Pharmacists Association and National Association of Chain Drug Stores Foundation. Medication Therapy Management in Community Pharmacy Practice: Core Elements of an MTM Service (Version 1.0) Journal of the American Pharmacists Association. 2005;45(5):573–9. doi: 10.1331/1544345055001256. [DOI] [PubMed] [Google Scholar]
- Andersen RM, Davidson PL. Improving Access to Care in America: Individual and Contextual Indicators. In: Andersen T, Rice T, Kominski G, editors. Changing the U.S. Health Care System: Key Issues in Health Services, Policy and Management. San Francisco, CA: Jossey-Bass; 2001. pp. 3–30. [Google Scholar]
- Bluml BM. Definition of Medication Therapy Management: Development of Professionwide Consensus. Journal of the American Pharmacists Association. 2005;45(5):566–72. doi: 10.1331/1544345055001274. [DOI] [PubMed] [Google Scholar]
- Briesacher B, Limcangco R, Gaskin D. Racial and Ethnic Disparities in Prescription Coverage and Medication Use. Health Care Financing Review. 2003;25(2):63–76. [PMC free article] [PubMed] [Google Scholar]
- Byrd L, Fletcher A, Menifield C. Disparities in Health Care: Minority Elders at Risk. The Association of Black Nursing Faculty Journal. 2007;18(2):51–5. [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services (CMS), Department of Health and Human Services. Medicare Program; Medicare Prescription Drug Benefit. Final Rule. Federal Register. 2005;70(18):4193–585. [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services (CMS) 2008. “Medicare Part D Medication Therapy Management (MTM) Programs: 2008 Fact Sheet” [accessed on April 13, 2009]. Available at http://www.cms.hhs.gov/PrescriptionDrugCovContra/Downloads/MTMFactSheet.pdf.
- Centers for Medicare and Medicaid Services (CMS) 2009. “2010 Call Letter” [accessed on April 13, 2009]. Available at http://www.cms.hhs.gov/PrescriptionDrugCovContra/Downloads/2010CallLetter.pdf. [PubMed]
- Cranor CW, Christensen DB. The Asheville Project: Short-Term Outcomes of a Community Pharmacy Diabetes Care Program. Journal of the American Pharmacists Association. 2003;43(2):149–59. doi: 10.1331/108658003321480696. [DOI] [PubMed] [Google Scholar]
- Daniel GW, Malone DC. Characteristics of Older Adults Who Meet the Annual Prescription Drug Expenditure Threshold for Medicare Medication Therapy Management Programs. Journal of Managed Care Pharmacy. 2007;13(2):142–54. doi: 10.18553/jmcp.2007.13.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgar BS. Shifting the Focus from Cost to Value: A Government Perspective. Journal of Managed Care Pharmacy. 2006;12(6, suppl B):S11–5. doi: 10.18553/jmcp.2006.12.S6-B.S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etemad LR, Hay JW. Cost-Effectiveness Analysis of Pharmaceutical Care in a Medicare Drug Benefit Program. Value in Health. 2003;6(4):425–35. doi: 10.1046/j.1524-4733.2003.64255.x. [DOI] [PubMed] [Google Scholar]
- Fera T, Bluml BM, Ellis WM. Diabetes Ten City Challenge: Final Economic and Clinical Results. Journal of the American Pharmacists Association. 2009;49(3):383–91. doi: 10.1331/JAPhA.2009.09015. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. The Healthcare Environment and Its Relation to Disparities. In: Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. pp. 80–124. [PubMed] [Google Scholar]
- Jones CP. Levels of Racism: A Theoretic Framework and a Gardener's Tale. American Journal of Public Health. 2000;90(8):1212–5. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CP. Invited Commentary: ‘Race,’ Racism, and the Practice of Epidemiology. American Journal of Epidemiology. 2001;154(4):299–304. doi: 10.1093/aje/154.4.299. [DOI] [PubMed] [Google Scholar]
- Neumann PJ. Using Cost-Effectiveness Analysis to Improve Health Care. Opportunities and Barriers. New York: Oxford University Press; 2005. [Google Scholar]
- Riley G. Two-Year Changes in Health and Functional Status among Elderly Medicare Beneficiaries in HMOs and Fee-for-Service. Health Services Research. 2000;25(5, part 3):44–59. [PMC free article] [PubMed] [Google Scholar]
- Sassi F, Le Grand J, Archard L. Equity versus Efficiency: A Dilemma for the NHS. If the NHS Is Serious about Equity It Must Offer Guidance When Principles Conflict. British Medical Journal. 2001;323(7316):762–3. doi: 10.1136/bmj.323.7316.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schommer JC, Planas LG, Johnson KA, Doucette WR. Pharmacist-Provided Medication Therapy Management (Part 2): Payer Perspective in 2007. Journal of the American Pharmacists Association. 2008;48(4):478–86. doi: 10.1331/JAPhA.2008.08023. [DOI] [PubMed] [Google Scholar]
- Schore J, Brown R, Lavin B. Racial Disparities in Prescription Drug Use among Dually Eligible Beneficiaries. Health Care Financing Review. 2003;25(2):77–90. [PMC free article] [PubMed] [Google Scholar]
- Smith SR, Catellier DJ, Conlisk EA, Upchurch GA. Effect on Health Outcomes of a Community-Based Medication Therapy Management Program for Seniors with Limited Incomes. American Journal of Health-System Pharmacy. 2006;63(4):372–9. doi: 10.2146/ajhp050089. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. 2008. “U.S. Interim Projections by Age, Sex, Race, and Hispanic Origin: 2000–2050” [accessed on April 30, 2009]. Available at http://www.census.gov/population/www/projections/usinterimproj/
- U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2d Edition. Washington, DC: U.S. Government Printing Office; 2000. A Systematic Approach to Health Improvement; pp. 7–23. [Google Scholar]
- Wang J, Dong Z, Hong SH, Suda KJ. A Comparison of Direct Medical Costs across Racial and Ethnic Groups among Children with Cancer. Current Medical Research and Opinion. 2008;24(3):847–58. doi: 10.1185/030079908X273390. [DOI] [PubMed] [Google Scholar]
- Wang J, Noel JM, Zuckerman IH, Miller NA, Shaya FT, Mullins CD. Disparities in Access to Essential New Prescription Drugs between Non-Hispanic Whites, Non-Hispanic Blacks, and Hispanic Whites. Medical Care Research and Review. 2006;63(6):742–63. doi: 10.1177/1077558706293638. [DOI] [PubMed] [Google Scholar]
- Wang J, White-Means SI, Hufstader MA, Walker GD. The Economic Implications of the Racial and Ethnic Disparities in the Use of Selective Serotonin Reuptake Inhibitors. Current Medical Research and Opinion. 2007a;23(4):853–63. doi: 10.1185/030079907x182220. [DOI] [PubMed] [Google Scholar]
- Wang J, Zuckerman IH, Miller NA, Shaya FT, Noel JM, Mullins CD. Accessing New Prescription Drugs: Disparities among Non-Hispanic Whites, Non-Hispanic Blacks, and Hispanic Whites. Health Services Research. 2007b;42(4):1499–19. doi: 10.1111/j.1475-6773.2006.00682.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Collins C. Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. Public Health Report. 2001;116(5):404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


