Abstract
Context
Concerns about mental health recovery persist after the 2005 Gulf storms. We propose a recovery model and estimate costs and outcomes.
Objective
To estimate the costs and outcomes of enhanced mental health response to large-scale disasters, using the 2005 Gulf storms as a case study.
Design
Decision analysis using state-transition Markov models, for 6-month periods from 7-30 months post-disaster. Simulated movements between health states were based on probabilities drawn from the clinical literature and expert input.
Participants
Hypothetical cohort, based on the size and characteristics of the population affected by the Gulf storms.
Intervention
Enhanced mental health care consisting of evidence-based screening, assessment, treatment, and care coordination.
Main Outcome Measures
We report morbidity, in 6-month episodes of mid/moderate or severe mental health problems through 30 months post-disaster; units of service (e.g., office visits, prescriptions, hospital nights); intervention costs; human resources
Results
Full implementation would cost $1,133 per capita, or over $12.5 billion for the affected population; yield 94.8-96.1% recovered by 30 months; but exceed available provider capacity. Partial implementation would lower costs and recovery proportionately.
Conclusions
Evidence-based mental health response is feasible, but requires targeted resources, increased provider capacity and advance planning.
Introduction
Hurricanes Katrina and Rita, which struck the US Gulf coast in late summer 2005, constituted the largest natural disaster in US history. Out of pre-storm population of 11 million in the directly affected area, some 1.5 million (14%) were displaced from their homes; nearly 2000 deaths were directly attributed to the storms, along with countless injuries and unprecedented economic damage. (1-2)
Large-scale disasters like the Gulf storms cause substantial mental health problems across all age groups, including increased incidence of post-trauma stress disorder, depression and anxiety disorders, exacerbation of pre-existing mental disorders, and a variety of behavior problems. Morever, the mental health problems that commonly arise after a disaster are leading causes of disability in adults and youth; thus, such problems are both clinically important and, if unaddressed, may impede recovery efforts and compound the social and economic fallout of the disaster. (3-7)
Prior studies confirmed that the Gulf storms were followed by large increases in mental health problems in the affected population, which have dissipated only slowly. (8-10) Beyond the storms' unprecedented scale and scope, efforts to address the storms' mental health consequences were complicated by the fact that the affected population included a high proportion of historically underserved groups, such as low-income African Americans; by limited mental health system capacity and substantial unmet need, even prior to the storms; and by various limitations in short- and longer-term disaster response efforts. (11-12)
The Gulf storms highlight the opportunity to strengthen mental health recovery following a large-scale disaster, particularly beyond the immediate post-disaster period of humanitarian response. (10) In this paper, we use the example of the Gulf storms to propose a new comprehensive model for evidence-based mental health response to major disasters, quantify the potential costs and benefits of large-scale implementation of such a model, and consider its logistical and human resource requirements. We draw on existing scientific data on evidence-based mental health response to disasters and epidemiological findings after disasters, supplemented by expert input due to numerous gaps in the existing published literature. We focus on medium-term response, i.e., from 7 months post-disaster, when new mental disorders can be diagnosed, through 24 months, when more permanent delivery strategies might be considered (we report outcomes through 30 months). We did not attempt to address immediate post-disaster emergency relief, partly because relatively more plans/protocols exist for acute humanitarian response in this period (including crisis counseling), while far fewer strategies exist for the medium-term recovery period; and partly because immediate post-disaster response may be more specific to the details of a particular disaster.
Many government agencies and non-governmental institutions participate in short- and longer-term disaster response. For instance, the Substance Abuse and Mental Health Services Administration (SAMHSA) led federal efforts to disseminate mental health information and training in response to the Gulf storms; state health and mental health agencies were responsible for public sector health services, while private health and behavioral health plans, and providers, handled private sector services; and non-governmental relief organizations, particularly the American Red Cross, provided many kinds of volunteer response. (11) We do not attempt to analyze these institutions' actual response to the Gulf storms here. Rather, we propose a comprehensive framework for delivering evidence-based mental health treatments that would follow the initial crisis response and that take into account feasibility, capacity, and population needs following a disaster.
Methods
We developed an intervention model that could be implemented post-disaster to identify people with substantial mental health problems and provide them with evidence-based treatment, supplementing the local provider capacity via telehealth and other national resources. We used a multi-period decision analysis model to illustrate the potential costs and benefits of implementing the proposed interventions, at different levels of intensity/coverage, in the population affected by the Gulf storms.
Decision Analysis Framework
We specified a discrete-time Markov model, using six-month periods starting with 7-12 months post-disaster. In the model, appropriate treatment in a given period was determined by a person's clinical status at the start of the period, and outcomes were a function of a person's prior clinical status, treatment received, and response to treatment (or spontaneous recovery, for people who are sick but untreated in a given period). We modeled service use through 24 months post-disaster, and outcomes through 30 months as outcomes are affected by treatment in prior periods.
Inputs into the decision analysis model include the characteristics and geographic distribution of the affected population, incidence/prevalence of mental illness, evidence-based treatment models, the costs of such treatment, mental health system capacity in the affected areas, and options for expanding mental health treatment capacity to address surges in need and demand.
Population
Modeling is based on the pre-storm (1/7/05) population of 11 million residents across the 117 counties/parishes across Lousiana, Mississippi, Alabama and Texas that FEMA designated as eligible for individual relief following hurricanes Katrina and Rita. Data on the prestorm population came from the Area Resources File (ARF) and the US Census.
It seemed likely that intervention strategies would differ for urban vs. rural areas, because of health system differences; and within vs. outside storm-affected counties, because of differences in the population prevalence of disaster-related morbidity. In practice, we allocated the pre-storm population across three geographic areas for the post-storm period, based on data from the US Census as of January 1, 2006: urban affected areas (8.8 million), rural affected areas (2.0 million), and pre-hurricane residents of the affected areas that subsequently moved outside the affected areas (0.24 million). Because treatment recommendations vary by age, we considered three age strata: 5-14 (17% of the total), 15-19 (9%), and 20 and older (75%).
Morbidity
We used three categories of morbidity: none, mild-moderate (i.e., meeting criteria for a mental disorder, plus serious role impairment), and severe mental health problems (i.e., disorder, plus severe/multiple role impairment), in terms of needed treatment content and intensity, but not necessarily corresponding to specific disorders.
Our assumptions about incidence of mental health problems were based on available epidemiological data from prior disasters and on the storm-affected population (8, 9, 13-15), synthesized based on consensus within the research team. Specifically, after six months post-disaster, we assumed rates of mild-moderate storm-attributable problems of 25% among adults and 30% among children, and rates of severe problems of 5% among adults and 10% among children. (16-18) Morbidity in subsequent periods was determined by our assumptions about treatment and recovery. Additionally, we assumed some continued new incidence in previously healthy people over time, specifically 5% mild-moderate and 1% severe after 12 months, and 0.5% mild-moderate after 18 months, across age groups. (8, 17)
Recovery
We specified transition probabilities between each possible health state, as a function of whether the person received recommended treatment during the period. We assumed that treatment-outcome relationships were consisted with those reported in the literature, i.e., that individuals in this situation were not more treatment-resistant, as we are not aware of evidence to this effect. We assumed lower, but not zero, probabilities of improvement or recovery in the absence of treatment. For simplicity, we assumed that recovery from illness was an absorbing state, i.e., once recovered, people remained free of problems for the remainder of our study period. Parameter inputs are listed in Appendix Table 1.
Appendix Table 1. Parameter inputs.
| Parameter | Ages 20+ | Aged 5-19 | ||
|---|---|---|---|---|
| Disease incidencea | ||||
| 6-12mos. | Mild/moderate mental illness | 25% | 30% | |
| Severe mental illness | 5% | 10% | ||
| 13-18 mos. | Mild/moderate mental illness | 5% | 5% | |
| Severe mental illness | 1% | 1% | ||
| 19-24 mos. | Mild/moderate mental illness | 0.5% | 0.5% | |
| Severe mental illness | 0.0% | 0.0% | ||
| % of population screened for mental illnessb | ||||
| 6-12 mos. | 100% | 100.0% | ||
| 13-18 mos. | 4.2% | 3.6% | ||
| 19-24 mos. | 0.3% | 0.3% | ||
| % assessed I positive screenerb | 100% | 100% | ||
| % false positive screenersc | 26% | 26% | ||
| Clinical transitionsd | ||||
| Mild/moderate mental illness, not previously severe | 1st course of treatment | % recover | 70% | 80% |
| % remain mild/moderate | 25% | 15% | ||
| % shift to severe | 5% | 5% | ||
| 2nd course of treatment | % recover | 60% | 70% | |
| % remain mild/moderate | 30% | 20% | ||
| % shift to severe | 10% | 10% | ||
| 3rd course of treatment | % recover | 55% | 60% | |
| % remain mild/moderate | 35% | 30% | ||
| % shift to severe | 10% | 10% | ||
| No treatment | % recover | 30% | 45% | |
| % remain mild/moderate | 55% | 45% | ||
| % shift to severe | 15% | 10% | ||
| Severe mental illness | 1st course of treatment | % recover | 20% | 40% |
| % shift to mild/moderate | 30% | 25% | ||
| % remain severe | 50% | 35% | ||
| 2nd course of treatment | % recover | 10% | 30% | |
| % shift to mild/moderate | 40% | 30% | ||
| % remain severe | 50% | 40% | ||
| 3rd course of treatment | % recover | 10% | 25% | |
| % shift to mild/moderate | 40% | 35% | ||
| % remain severe | 50% | 40% | ||
| No treatment | % recover | 10% | 20% | |
| % shift to mild/moderate | 30% | 35% | ||
| % remain severe | 60% | 45% | ||
| Mild/moderate, previously severe mental illness | Treatment | % recover | 50% | 50% |
| % remain mild/moderate | 40% | 40% | ||
| % shift to severe | 10% | 10% | ||
| No treatment | % recover | 20% | 35% | |
| % remain mild/moderate | 60% | 50% | ||
| % shift to severe | 20% | 15% | ||
SOURCES:
These are model parameters.
Unit Costs
We developed estimates of the unit costs of screening, assessment, and treatment services using information from public sources, particularly the Medicaid fee schedule in the storm-affected states; and via personal communication with two national managed behavioral health organizations (MBHOs), and with several local hospitals within and outside the storm-affected areas. Overhead associated with health care services is typically incorporated into health care prices, and thus is included implicitly in our unit costs.
Two MBHOs reviewed our proposed model to consider feasibility; one MBHO determined that implementation would be within current capacity, while the other would have to add or train telephone therapists.
Intervention intensity
We specified the “intensity” of implementation, i.e., the probability that people would receive the recommended screening, assessment, and treatment. We made simplifying assumptions for model tractability. In particular, while we allowed for false positives in screening, we assumed zero false negatives in screening and assessment, and that treatment was conditional on positive screening/assessment (i.e., all who received treatment were sick). We assumed adults and children out of school would be screened one-on-one, but that there were economies of scale in screening schoolchildren; and that people were screened no more than once in the initial period, except for new incident illness. Finally, we assumed that each person received either the recommended treatment or no treatment in a given six-month period.
Interventions
We developed intervention strategies to identify people with substantial mental health consequences and provide them with evidence-based treatment. In terms of specific conditions, the disaster literature identified the most relevant as anxiety disorders, post-traumatic stress disorder (PTSD), and depressive disorders, but we also considered exacerbations of severe mental illness such as psychotic disorders. However, in keeping with our population focus – and for model tractability – we developed general treatment models, rather than attempting to develop treatment recommendations that would necessarily suit every individual patient; thus treatment profiles – and associated costs – should be viewed as population averages, which vary across individuals,
Post-disaster mental health treatment programs have focused on crisis interventions such as psychoeducation and Psychological First Aid during the immediate recovery period. (19) Cognitive Behavioral Therapy (CBT) has been found to be effective in treating PTSD in adults and youth. (18, 20) A recent Institute of Medicine report concludes that there is adequate evidence among adults for efficacy of exposure therapy, often based on CBT principles, for treatment of PTSD. (21) There is a large literature on effective treatments for depressive disorders, but little of it addresses the post-disaster context. A growing literature suggests that treatment programs for depression relying on distant delivery strategies, such as telephone counseling, are effective. (22) Such findings support the feasibility of our proposing innovative post-disaster delivery strategies that combine distant and local services delivery. Likewise, PTSD and depression have been effectively treated with CBT in youth with school-based interventions, which could be key resources for communities recovering from a disaster. (18-20, 23) Comprehensive programs to improve mental health care can improve outcomes for the poor and racial/ethnic minorities, (24, 25) the main underserved groups affected by hurricanes Katrina and Rita. To our knowledge, there has been no services delivery model that builds on this literature to support comprehensive mental health recovery after a disaster.
We specified one-time screening for common disorders post-disaster using as a prototype, one to 3 brief self-report screeners such as the MHI-5, K-6, or PHQ-9. We adjusted the mix of telephone and in-person screenings and the provider level according to age and geographic group. We assumed existing FEMA staff – who, in practice, visited individuals receiving assistance following the Gulf storms – could apply screeners in affected areas in months 7-12, when we assumed most screening would occur; however, our estimated costs of screening were largely independent of modality. We assumed that persons screening positive would require a clinical assessment of need by telephone or in person. We adjusted the mix of delivery mode (telephone or in-person) and provider type (masters, PhD, or MD) by age and geographic group.
We specified the provider type (masters, PhD, MD) and mix of services (inpatient, outpatient, psychotherapy and medication) based on level of need, history of response to treatment in prior periods, and age and geographic group. For adults and adolescents, we thought that psychotherapy could be provided in person or by telephone and adjusted that mix of modality by geographic area and need level for that period. For medication management, we assumed that providers were local and adjusted the mix of primary care and psychiatry by age and geographic group; we specified that telephone or local consultation by psychiatrists would be provided based on need, history of response in prior periods, and age and geographic group. We assumed that persons with severe mental illness faced a risk for hospitalization and required case management, which could be provided in person or by telephone, adjusting this modality mix by geographic group.
We assigned amount (such as duration, number of prescriptions) of services required, assuming that treatment for mild/moderate illness was equivalent to about 2/3 of the requirements for a course of cognitive behavioral therapy (8-10 sessions), and/or several months of medication management; and that severe illness faced a known risk of a short-term hospitalization and required both psychotherapy and medication, more visits, consultation and/or supervision, and case management. In general, we specified more volume of services and higher-level providers with more persistent need.
We focused our quantitative model on services that are provided to individuals. We address other types of resources that are applied at the program or population level in the discussion, particularly outreach/education campaigns, training programs for local and national providers, and management and coordination infrastructure.
Table 1 summarizes our recommended intervention model for adults in the “urban/affected” area. Information on other age groups and areas is available by request from the authors.
Table 1. Recommended intervention components (adult, urban/affected area).
| Type of Service | Unit cost* | Mild/moderate, 1st course | Mild/moderate, Refractory / previously severe | Severe, 1st course | Severe, Refractory | ||||
|---|---|---|---|---|---|---|---|---|---|
| # | % who receive | # | % who receive | # | % who receive | # | % who receive | ||
| Screening | 100% | 100% | |||||||
| In-person | $25 | 1 | 100% | 1 | 100% | ||||
| Telephone | $25 | 0 | -- | 0 | -- | ||||
| Assessment** | 100% | 100% | |||||||
| In-person I Mix of masters & nurse/MD in primary care | $100 | 1 | 65% | 1 | 65% | ||||
| Telephone I Masters Level | $75 | 1 | 35% | 1 | 35% | ||||
| Therapy*** | 70.0% | 85.0% | 100% | 100% | |||||
| In-person I Masters Level Provider (one-on-one) | $90 | 12 | 8.6% | 12 | 10.5% | 0 | -- | 0 | ---- |
| In-person I Masters Level Provider (group)* | $210 | 12 | 15.9% | 12 | 19.5% | 0 | -- | 0 | -- |
| In-person I PhD Level Provider (one-on-one) | $135 | 12 | 3.7% | 12 | 4.4% | 12 | 100% | 12 | 100% |
| In-person I PhD Level Provider (group)* | $245 | 12 | 6.8% | 12 | 8.1% | 0 | -- | 0 | -- |
| Telephone I Masters Level Provider | $47 | 12 | 24.5% | 12 | 30.0% | 0 | -- | 0 | -- |
| Telephone I PhD Level Provider | $67 | 12 | 10.5% | 12 | 12.5% | 0 | -- | 6 | - |
| Medication management*** | 50.0% | 85.0% | 100% | 100% | |||||
| In-person I MD Provider in primary care | $80 | 6 | 30.0% | 6 | 47.0% | 0 | -- | 0 | -- |
| In-person I NP Provider in primary care | $60 | 6 | 5.0% | 6 | 8.0% | 0 | -- | 0 | -- |
| In-person I Psychiatrist Provider | $96 | 6 | 15.0% | 6 | 30.0% | 6 | 100% | 6 | 100% |
| Telephone I Master's Level, meds reminders | $50 | 0 | -- | 0 | -- | 0 | -- | 0 | -- |
| Phone consults to PCP by psychiatrist*** | $70 | 2 | 5.3% | 2 | 80% | 0 | -- | 0 | -- |
| Inpatient care (hospital nights)*** | $900 | 0 | -- | 0 | -- | 5 | 20% | 5 | 40% |
| Rx (months)*** | $40 | 6 | 50.0% | 9 | 85.0% | 9 | 100% | 12 | 100% |
NOTES:
Group therapy session cost is divided across all participants; we assume 7 participants per group therapy session
Among those who screen positive
Among those who assess positive
Outcomes
We focused on the following outcomes of interest:
Morbidity, i.e., episodes of mild/moderate or severe morbidity, in each six-month interval up to 30 months
Units of Service, i.e., the volume each different type of service (e.g., psychotherapy or medication management visits, prescriptions, etc.) that would be required.
Intervention Costs, i.e., the estimated cost in dollars of implementing the model.
Human Resource Needs, i.e., the estimated volume of clinicians (measured in full-time equivalency (FTE)) that would be required to implement the model.
Analyses
We implemented Markov models by age and geographic group (nine analytic cells in all). We pooled results across the age and geographic groups. We estimated services and costs per 1000 persons (or per capita), and the total services and costs required and episodes averted for the complete population affected by the Gulf storms. We developed upper-limit estimates of pre-Katrina provider capacity in the affected counties from the Area Resources File.
We implemented our decision-analysis model several times, for different levels of intensity/coverage. Here we report results for the extremes of zero implementation, representing what would happen in the absence of any mental health intervention, and universal implementation, representing the maximum “achievable” outcomes implied by our recommended intervention.
We recognize that there is considerable uncertainty in many of the inputs to our model. While we implemented the model deterministically for tractability, we systematically varied the values of key parameters to gauge the sensitivity of the findings to changing assumptions.
Findings
Figure 1 illustrates the population distribution of mental health problems, given our assumptions. Figure 1a provides estimates of the time course of mild/moderate and severe mental health problems in the overall affected population under the assumption of zero treatment; this can be thought of as the “natural” course of illness, or upper bound of morbidity. Overall morbidity peaks around 33% (26% mild/moderate and 6% severe), and declines to about 15% (9% mild/moderate and 6% severe); prevalence of severe problems increases over the first year post-disaster, in part due to new incidence but also because rates of “spontaneous” recovery (i.e., without treatment) are assumed to be low, and some untreated cases worsen.
Figure 1. Estimated trends in mild/moderate and severe mental health problems.
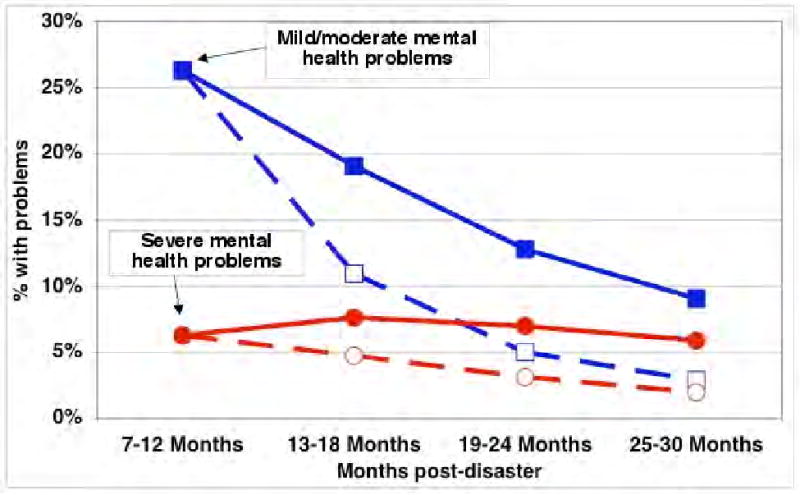
Solid lines: 0% treatment
Dashed lines: 100% implementation of recommended intervention model
Figure 1b provides comparable estimates under the assumption of 100% implementation of our recommended model. The area between the morbidity trajectories can be thought of as the maximum recovery achievable from active interventions; this is shown graphically in Figure 2 for mental health problems overall. Per 1000 population, the shaded green area in Figure 2 suggests a reduction of 327 six-month episodes of mental illness (221 mild/moderate and 106 severe) over our two-year analysis period. Put another way, full implementation would “eliminate” 34.9% of the episodes of illness that would arise under no treatment.
Figure 2. Maximum achievable recovery, 100% implementation vs. 0% treatment.
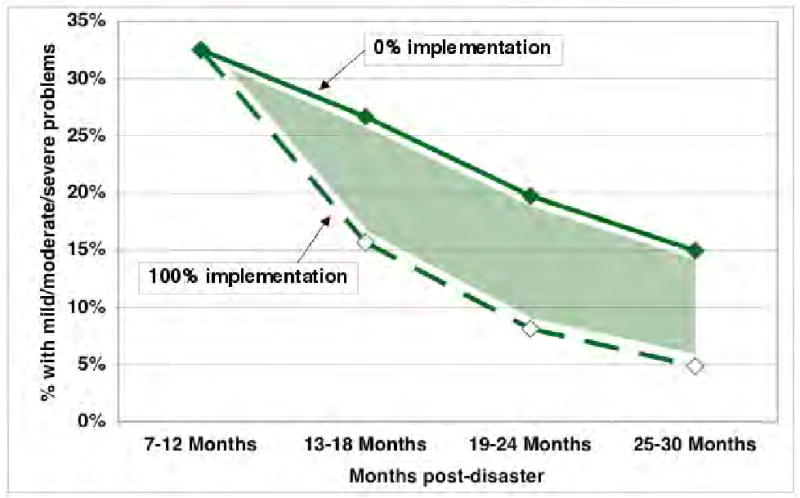
Table 2 lists the costs of implementing our model under 100% implementation (vs. 0% treatment), overall and by type of service and time period. Full (vs. zero) coverage of our intervention model would cost $1,133 per capita over 7-24 months post-disaster, which corresponds to $12.5 billion across the overall storm-affected population of 11 million people. This suggests an average cost of $3,460 per averted six-month episode of mental health problems. (Because a given episode of treatment changes transition probabilities across multiple outcomes, we cannot separately estimate costs of averting mild/moderate or severe episodes, respectively.)
Table 2. Costs per 1000 population, months 7-24 post-disaster (100% intervention implementation vs. 0% treatment).
| Intervention component | 7-12 months | 13-18 months | 19-24 months | TOTAL |
|---|---|---|---|---|
| Screening | $20,930 | $834 | $64 | $21,828 |
| Assessment | $50,534 | $5,883 | $1,144 | $57,561 |
| Therapy | $218,664 | $172,091 | $102,511 | $493,266 |
| Medication management* | $101,479 | $91,120 | $54,581 | $247,180 |
| Hospital nights | $36,998 | $50,046 | $39,282 | $126,326 |
| Prescription drugs | $56,611 | $78,297 | $51,768 | $186,676 |
| TOTAL | $485,217 | $398,270 | $249,350 | $1,132,837 |
NOTE: Includes office visits to primary care providers, nurse practitioners, and psychiatrists, plus provider-to-provider telephone consultation by psychiatrists to primary care providers, and telephone care management by masters-level providers.
Table 3 shows the number of different types of services that would be required 7-12 months post-disaster, under 100% model implementation for the full storm-affected population. Each of the 11 million people in the affected population would be screened, and 4.8 million would have a clinical assessment. Full treatment implementation would involve provision of 15 million masters-level and 8.5 million PhD-level therapy sessions, 6.6 million primary care visits, 5.4 million psychiatrist contacts, and 0.45 million nights of mental health-related hospital care during the 7-12 month period post-disaster. Results for 13-24 months are available from the authors.
Table 3.
Units of service for Gulf storm population, months 7-12 post-disaster (100% implementation of recommended intervention model)
| Intervention component | 7-12 months (millions of units) |
|---|---|
| Screening | 11.0 |
| Assessment | |
| In-person | 3.5 |
| Telephone | 1.3 |
| Therapy | |
| Masters-level in-person (1-on-1 and group) | 7.8 |
| Masters-level telephone | 7.2 |
| PhD-level in-person | 5.2 |
| PhD-level telephone | 3.3 |
| Medication management | |
| Primary care physician | 5.8 |
| Nurse practitioner | 0.8 |
| Psychiatrist | 4.6 |
| Psychiatrist consults to primary care provider | 0.8 |
| Hospital nights | 0.45 |
| Months of psychotropic prescriptions | 11.3 |
Measured in full-time equivalent (FTE) positions, we estimate that full implementation would require approximately 7500 FTEs of masters-level and 5000 PhD-level therapists for in-person outpatient psychotherapy, and 14,500 master-level and 8200 PhD-level FTEs overall (in-person and telephone) for outpatient care; 1,700 psychiatrist FTEs for outpatient medication management; and 2,500 hospital beds for inpatient psychiatric care (which would require additional psychiatrists, psychiatric nurses, and associated staff, beyond the estimated FTEs for outpatient care). By comparison, based on pre-storm data from the 2004 ARF, there were 14,245 social workers and 4,647 psychologists (proxies for masters- and PhD-level therapists, respectively), 1,443 psychiatrists, and 1,729 inpatient psychiatry beds across the storm-affected counties. The ARF estimates are an upper bound, as not all providers are in full-time practice, some time would be committed to established patients and the storms displaced providers and damaged hospitals. (11, 33)
In addition, successful population-level implementation would also require outreach efforts; provider training, particularly for care of children; and development of a management, communication, and accountability infrastructure. Based on general information on national campaigns such as NIMH's “Real Men, Real Depression” program, and local campaigns in New York after the terrorist attacks of 9/11, we estimate that such “overhead” costs would increase total program costs by perhaps 2-3%, with 5% as an upper limit (which would correspond to $625 million). While these elements are clearly essential for any large-scale intervention to be effective, detailed estimation of their costs is beyond the scope of this study.
Discussion
Based on the decision analysis framework described here, we estimated that universal provision of an evidence-based mental health intervention model to the population affected by a disaster such as the 2005 Gulf storms would cost on the order of $1,133 per capita across the affected population in months 7-24 post-disaster, with nearly half of this spending in months 7-12 due to an initial surge in need. In turn, we estimated that the services purchased by this money would reduce the number of six-month episodes of storm-attributable mental health problems by 35%, corresponding to a per capita average of two extra months spent free of mental illness for each person in the disaster-affected population.
Given the structure of our model, varying the overall level of implementation of the proposed interventions would reduce both costs and benefits in approximately equal proportion. Thus, for instance, 25% coverage (vs. zero) would cost $347 per capita over 7-24 months (30.6% of the cost of 100% vs. zero coverage), and avert 102 six-month episodes of illness (31.0% of 100% vs. zero). This correspond to a cost per averted episode of $3,416, vs. $3,460 for 100% vs. zero; this difference is because, under less than universal coverage, a smaller proportion of treatment episodes are provided to refractory patients. Similarly, if the base rate of treatment were 25%, moving to 100% yields a cost per averted episode of $3,549, or $3,535 to move to 70% coverage. Other permutations would likely shift this balance unfavorably, for instance if some people who initiate treatment discontinue early: they would consume services, and incur costs, when they start treatment, but then discontinue treatment before is (fully) therapeutic.
Formal estimation of cost-effectiveness was outside the scope of this study. Prior studies have mapped episodes of mental illness to quality-adjusted life years in order to provide a general framework for considering cost-effectiveness (27-28), in particular, using evidence from methodological studies that depression reduces the value of a quality-adjusted life year (QALY) by 0.2 to 0.4 (out of a maximum value of 1). (29-30) If we apply these scaling factors to episodes of mental illness in our model, our estimated cost per averted episode corresponds to an estimated cost per QALY of $17,301 to $34,603. Even the upper end of this range – to be conservative – is within the range of generally accepted medical practice, such as regular screening for colorectal, prostate, and breast cancers in average-risk patients, and blood pressure screening among normotensive people. (31-32)
Our intervention cost and outcome estimates are likely to be upper bounds, for several reasons. Our reference population was zero treatment (natural illness recovery) whereas “usual” care would include some delivered services. Yet this may not be so out of range as many affected people may choose not to receive mental health services even if offered, due to stigma, cultural acceptability of services, competing needs, and other factors. The Gulf storms, in particular, disproportionately affected racial/ethnic minority and low-income populations, which tend to have less access to and lower use and quality of mental health treatment. (12, 34)
This raises the issue of feasible implementation. Assuring the delivery of evidence-based mental health interventions can be challenging in the absence of a disaster. Moreover, there is evidence that demand – or at least clinical need – for mental health services exceeds the available supply in many parts of the country, even without surges in need following a disaster. (35) In the US public sector mental health providers are primarily oriented to persons with severe and persistent mental illness, such as schizophrenia; while private sector systems may be more familiar with disorders like depression that are common after disasters but have limited experience caring for disadvantaged or displaced populations – and often little mandate to do so. In addition, there is generally weak infrastructure for reliably delivering the types of psychotherapy such as CBT that are known to be effective in post-disaster situations.
Our findings suggest that population-level implementation would almost certainly exceed local provider capacity. While disaster preparedness may help motivate some expansion of local capacity, it is unlikely to be feasible or efficient for each geographic area to have adequate local reserve resources to meet post-disaster needs. Instead, response could draw on national reserve resources. Indeed, outside human and other resources played an important role in response to the Gulf storms; yet those resources were largely assembled after the storms had occurred and needs identified. Response to future disasters may be substantially enhanced if it could draw on a pre-established national “ready reserve” of providers trained in evidence-based treatments, along with a logistical infrastructure to deploy them effectively – in-person and via telehealth – and to coordinate their work.
We emphasize that “national” need not mean “public”. In practice, along with the Veterans Administration and the Department of Defense, the largest existing networks of mental health providers – in terms of both number of providers and geographic coverage – are those of private MBHOs, which may also have relevant managerial and logistical capabilities and experience. Disaster preparedness is now considered a public good, and national mental health preparedness will likely require some federal sponsorship for financing, as well as to establish the parameters for a national mental health response, develop the rules under which it would operate, activate/deploy the response infrastructure, and monitor outcomes.
Telehealth through available large managed care companies seems like a natural fit with the goal of achieving a nationally distributed network of “reserve” providers; and a growing body of research supports telephone psychotherapy as a viable delivery option. (22, 36-37) However, further research is needed to assess the effectiveness of telephonic mental health response in post-disaster settings, and to identify operational requirements such as referral mechanisms, clinical supervision, outcome monitoring, and billing/reimbursement for population-based care.
One particular local supply issue we identified was a likely shortage of inpatient beds and the associated clinical staff; addressing this shortage would require new structural resources such as psychiatric wards in field hospitals and/or evacuating patients to facilities outside the affected area that have extra capacity. Further research is also required to establish best practices for meeting these service delivery needs.
Policy changes are likely to be required to facilitate a 2-year response by providers from outside a disaster-affected area. In general, providers must be licensed in the state in which they are providing services, or be federally certified (e.g., employed by the Veterans Administration or the US Public Health Service), neither of which covers the majority of potential responders from outside a disaster-affected area; or the services can be classified as nonprofessional or educational, neither of which is generally germane here. In the case of the Gulf storms, some of the affected states waived licensure requirements some professions. In Louisiana, some waivers were maintained after the storms for provider groups that do not charge for services in the affected areas. However, these responses occurred somewhat ad hoc and mostly after the fact. Based on the experience following the Gulf storms, it may be appropriate to consider developing a standard national strategy to streamline licensing and malpractice issues, e.g., by allowing providers licensed anywhere in the US to practice in any FEMA-designated disaster area for a specified period of time, along with a viable mechanism to provide malpractice coverage to providers who participate in disaster response. Similarly, modification or extension of policies affecting medical licensing and malpractice are likely to be needed to facilitate telecare, both to cover cross-state provision of care and to enable reimbursement.
Other methods to consider for increasing supply rapidly may include rapid retooling of providers for other kinds of health or social services, and/or training and deployment of nonprofessional/lay providers; and developing a deeper local reserve of community leaders with relevant skills who could participate in response to local community emergencies. Some such innovations might additionally strengthen community mental health resources in non-disaster circumstances, a “dual use” that has been emphasized in other areas of preparedness.
Until the recent primary care authorization for New Orleans, potentially including support for behavioral health services, there was no specific federal allocation for mental health services in response to the Gulf storms. This raises the question of the priority that should be given to mental health response, given many competing recovery needs. The Gulf storms have dramatically illustrated the scope and persistence of mental distress, which cuts across age and cultural groups, and is likely to impede many aspects of both individual and community recovery, even as research has shown economic benefits from mental health interventions. (38)
We have focused on mental health recovery over months 7-24 post disaster, and additional strategies may be required to promote longer-term improvements subsequently. For example, while chronic disease management programs for depression improve outcomes, disseminating and sustaining these interventions outside of a disaster has been difficult, as key components are often not covered by insurance policies. Similarly, many schools were found to have adequate crisis response plans post-Katrina, but few had the resources to sustain provision of mental health services. (39) Yet even investing in short-term interventions may have long-term health benefits over many years for disadvantaged population groups. (40) Thus, we currently face the option of proactively developing a plan to intervene quickly following disasters – beyond current efforts, most notably crisis counseling – to promote mental health recovery for survivors; we wonder whether this would facilitate recovery in other life domains; and suggest that it is important to determine how to promote long-term recovery for individuals and communities.
More generally, we have taken a largely medical perspective on ameliorating mental health consequences of disasters. Comprehensive disaster response requires intervention across multiple domains, including short- and long-term efforts to ensure survivors' mental, physical, social and economic needs. While there are likely to be powerful synergies across these domains, we recognize that the optimal mix of interventions across them remains an open question. We necessarily leave this to future research.
A key related issue is when and for whom to activate this type of intervention program. In principle, the framework described here could be applied for disasters of varying scope and scale. In practice, the intervention details will vary by the scope, scale, nature and consequences of the disaster, e.g., depending on the extent of population displacement and on how the needs in an area exceed its available/remaining delivery system capacity.
Our analyses have important limitations. There are many knowledge gaps regarding “evidence-based” response to disasters and a recent report by the Institute of Medicine highlighted concerns about insufficient evidence of efficacy for most treatments for PTSD among adults. (21) Our models could not include data on individual differences in response to traumatic events, which are key predictors of outcome; so we present a population rather than individual perspective on services that promote recovery. There is some degree of uncertainty around each of the model's many inputs, and thus our overall findings. We focused on the context of the Gulf storms, and estimates for other disasters could require different assumptions and yield different results; but we designed the treatment and per-capita services model to be applicable across a wide range of contexts.
Given the recent evidence of high burden of disease and significant unmet need among the survivors of the Gulf Storms, and widespread discussion of disaster preparedness more generally, we hope that the response model proposed here may be a useful starting point for policy discussions, to improve services for people with persistent illness following the Gulf storms, as well as to plan a coordinated response strategy for future disasters.
Acknowledgments
The work was supported by the National Institutes of Mental Health (P50MH54623), RAND, the Robert Wood Johnson Foundation, and the South Central VA Mental Illness Research and Education Center.
Footnotes
Disclosures: The views expressed in this article do not necessarily represent the views of the National Institute of Mental Health, the National Institutes of Health, the Department of Health and Human Services, or the United States Government.
Contributor Information
Michael Schoenbaum, RAND Corporation (when work began), National Institute of Mental Health (current).
Brittany Butler, UCLA Semel Institute, Health Services Research Center (when work began), RAND Corporation (current).
Sheryl Kataoka, UCLA Semel Institute, Health Services Research Center.
Grayson Norquist, University of Mississippi, Department of Psychiatry.
Benjamin Springgate, UCLA, Robert Wood Johnson Foundation Clinical Scholars Program, Rapid Evaluation and Action for Community Health in New Orleans, Louisiana (REACH-NOLA).
Greer Sullivan, Little Rock VA & University of Arkansas, Department of Psychiatry (when work began), RAND Corporation (current).
Naihua Duan, UCLA Semel Institute, Health Services Research Center (when work began), Columbia University (current).
Ronald C. Kessler, Harvard Medical School, Department of Healthcare Policy.
Kenneth Wells, RAND Corporation and UCLA Semel Institute, Health Services Research Center.
References
- 1.US Census Bureau. Geography Branch, American Community Survey Office, US Census Bureau; 2006. [May 2008]. 2005 ACS Special Product for the Gulf Coast Area - FEMA Designated Individual and Public Assistance Area by State. available at http://www.census.gov/acs/www/Products/Profiles/gulfcoast/pdf/SpecKtabareaIPAbySTATE.pdf. [Google Scholar]
- 2.New Orleans Times-Picayune(2006) Deaths of Evacuees Push Tol to 1,577. [May 2008];2006 May 19; http://www.nola.com/news/t-p/frontpage/index.ssf?/base/news-5/1148020620117480.xml&coll=1.
- 3.Ahern M, Kovats RS, Wilkinson P, Few R, Matthies F. Global Health Impacts of Floods: Epidemiologic Evidence. Epidemiologic Reviews. 2005;27(1):36–46. doi: 10.1093/epirev/mxi004. [DOI] [PubMed] [Google Scholar]
- 4.Freedy JR, Saladin ME, Kilpatrick DG, Resnick HS, Saunders BE. Understanding acute psychological distress following natural disaster. Journal of Traumatic Stress. 1994;7(2):257–273. doi: 10.1007/BF02102947. [DOI] [PubMed] [Google Scholar]
- 5.Norris FH, Kaniasty K, Conrad ML, Inman GL, Murphy AD. Placing Age Differences in Cultural Context: A Comparison of the Effects of Age on PTSD After Disasters in the United States, Mexico, and Poland. Journal of Clinical Geropsychology. 2002;8(3):153–173. [Google Scholar]
- 6.Davis L, Siegel LJ. Posttraumatic Stress Disorder in Children and Adolescents: A Review and Analysis. Clinical Child and Family Psychology Review. 2000;3(3):135–154. doi: 10.1023/a:1009564724720. [DOI] [PubMed] [Google Scholar]
- 7.Nandi A, Galea S, Tracy M, et al. Job Loss, Unemployment, Work Stress, Job Satisfaction, and the Persistence of Posttraumatic Stress Disorder One Year After the September 11 Attacks. Journal of Occupational and Environmental Medicine. 2004;46(10):1057–1064. doi: 10.1097/01.jom.0000141663.22902.0a. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Galea S, Gruber MJ, Sampson NA, Ursano RJ, Wessely S. Trends in mental illness and suicidality after Hurricane Katrina. Mol Psychiatry. 2008 Jan 8; doi: 10.1038/sj.mp.4002119. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang PS, Gruber MJ, Powers RE, et al. Mental Health Service Use Among Hurricane Katrina Survivors in the Eight Months After the Disaster. Psychiatric Services. 2007;58(11):1403. doi: 10.1176/appi.ps.58.11.1403. and. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weisler RH, Barbee JG, Townsend MH. Mental Health and Recovery in the Gulf Coast After Hurricanes Katrina and Rita. JAMA. 2006;296(5):585. doi: 10.1001/jama.296.5.585. [DOI] [PubMed] [Google Scholar]
- 11.Lambrew JM, Shalala DE. Federal Health Policy Response to Hurricane Katrina: What It Was and What It Could Have Been. JAMA. 2006;296(11):1394. doi: 10.1001/jama.296.11.1394. [DOI] [PubMed] [Google Scholar]
- 12.Berggren RE, Curiel TJ. After the Storm--Health Care infrastructure in Post-Katrina New Orleans. New England Journal of Medicine. 2006 April 13;354(15):1549–1552. doi: 10.1056/NEJMp068039. [DOI] [PubMed] [Google Scholar]
- 13.Kessler RC, Galea S, Jones RT, Parker HA. Bulletin of the World Health Organization. 12. Vol. 84. 2006. Mental illness and suicidality after Hurricane Katrina; pp. 930–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galea S, Brewin CR, Gruber M, Jones RT, King DW, King LA, McNally RJ, Ursano RJ, Petukhova M, Kessler RC. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Archives of General Psychiatry. 2007;64(12):1427–1434. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Norris FH, Friedman MJ, Galea S, Watson PJ. Methods for Disaster Mental Health Research. Guilford Publications, Inc; Aug, 2006. [Google Scholar]
- 16.North CS, Kawasaki A, Spitznagel EL, Hong BA. The course of PTSD, major depression, substance abuse, and somatization after a natural disaster. J Nerv Ment Dis. 2004;192(12):823–829. doi: 10.1097/01.nmd.0000146911.52616.22. [DOI] [PubMed] [Google Scholar]
- 17.Norris FH, Murphy AD, Baker CK, Perilla JL. Postdisaster PTSD over four waves of a panel study of Mexico's 1999 flood. J Trauma Stress. 2004 Aug;17(4):283–292. doi: 10.1023/B:JOTS.0000038476.87634.9b. [DOI] [PubMed] [Google Scholar]
- 18.Shaw JA, Applegate B, Schorr C. Twenty-one-month follow-up study of school-age children exposed to Hurricane Andrew. J Am Acad Child Adolesc Psychiatry. 1996;35(3):359–364. doi: 10.1097/00004583-199603000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Psychological First Aid: Field Operations Guide. 2nd. National Child Traumatic Stress Network and National Center for PTSD; Jul, 2006. Available on: http://www.nctsn.org and http://www.ncptsd.va.gov. [Google Scholar]
- 20.Cohen JA. Principal Author, Journal of the American Academy of Child and Adolescent Psychiatry. 10, supplement. Vol. 37. American Academy of Child and Adolescent Psychiatry; 1998. Practice Parameters for the Diagnosis and Treatment of Posttraumatic Stress Disorder in Children and Adolescents; pp. 4S–26S. [DOI] [PubMed] [Google Scholar]
- 21.Institute of Medicine. Treatment of PTSD: Assessment of the Evidence. Washington, DC: The National Academies Press; oct 17, 2007. [Google Scholar]
- 22.Wang P, Simon G, Avorn J, et al. A randomized trial of telephone screening, outreach, and care management for depressed workers: Impact on clinical and work productivity outcomes. JAMA. 2007 Sep 26;298(12):1401–11. doi: 10.1001/jama.298.12.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Langley A, Jaycox L, Walker D, Cohen J, Mannarino A. Comparison of TF-CBT and CBITS for Youth Following the Gulf Hurricanes In Mental Health Services in Response to Hurricanes Katrina and Rita. Manuscript presented at the National Institute of Mental Health's Mental Health Services Research Conference; Washington, DC. July 2007. [Google Scholar]
- 24.Stein BD, Jaycox LH, Kataoka SH, Wong M, Tu W, Elliott MN, Fink A. A mental health intervention for schoolchildren exposed to violence: a randomized controlled trial. JAMA. 2003 Aug 6;290(5):603–11. doi: 10.1001/jama.290.5.603. [DOI] [PubMed] [Google Scholar]
- 25.Miranda J, Chung JY, Green BL, et al. Treating depression in predominantly low-income young minority women: A randomized controlled trial. JAMA. 2003 July 2;290(1):57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- 26.Graham JD, Corso PS, Morris JM, Segui-Gomez M, Weinstein MC. Evaluating the cost-effectiveness of clinical and public health measures. Annu Rev Public Health. 1998;19:125–52. doi: 10.1146/annurev.publhealth.19.1.125. [DOI] [PubMed] [Google Scholar]
- 27.Lave JR, Frank RG, Schulberg HC, Kamlet MS. Cost-effectiveness of treatments for major depression in primary care practice. Arch Gen Psychiatry. 1998;55(7):645–51. doi: 10.1001/archpsyc.55.7.645. [DOI] [PubMed] [Google Scholar]
- 28.Katon WJ, Schoenbaum M, Fan MY, Callahan CM, Williams J, Jr, Hunkeler E, Harpole L, Zhou XH, Langston C, Unützer J. Cost-effectiveness of improving primary care treatment of late-life depression. Arch Gen Psychiatry. 2005;62(12):1313–20. doi: 10.1001/archpsyc.62.12.1313. [DOI] [PubMed] [Google Scholar]
- 29.Wells K, Sherbourne C. Functioning and utility for current health of patients with depression or chronic medical conditions in managed, primary care practices. Arch Gen Psychiatry. 1999;56:897–904. doi: 10.1001/archpsyc.56.10.897. [DOI] [PubMed] [Google Scholar]
- 30.Fryback D, Dasbach E, Klein R, et al. The Beaver Dam Health Outcomes Study: initial catalog of health state quality factors. Med Decis Making. 1993;13:89–102. doi: 10.1177/0272989X9301300202. [DOI] [PubMed] [Google Scholar]
- 31.Tengs TO, Adams ME, Pliskin JS, et al. Five hundred life-saving interventions and their cost effectiveness. Risk Analysis. 1995;15:369–390. doi: 10.1111/j.1539-6924.1995.tb00330.x. [DOI] [PubMed] [Google Scholar]
- 32.Provenzale D. Cost-effectiveness of screening the average-risk population for colorectal cancer. Gastrointest Endosc Clin N Am. 2002 Jan;12(1):93–109. doi: 10.1016/s1052-5157(03)00061-8. [DOI] [PubMed] [Google Scholar]
- 33.Keeler EB. The value of remaining life is close to estimated values of life. J Health Econ. 2001;20:141–143. doi: 10.1016/s0167-6296(00)00070-9. [DOI] [PubMed] [Google Scholar]
- 34.U.S. Department of Health and Human Services, Office of The Surgeon General, SAMHSA. Mental Health: Culture, Race and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: USDHHS; 2001. [PubMed] [Google Scholar]
- 35.New Freedom Commission on Mental Health. Achieving the Promise: Transforming Mental Health Care in America Final Report. DHHS; Rockville, MD: 2003. Pub. No. SMA-03-3832. [Google Scholar]
- 36.Hunkeler EM, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Arch Fam Med. 2000 Aug;9(8):700–8. doi: 10.1001/archfami.9.8.700. [DOI] [PubMed] [Google Scholar]
- 37.Simon GE, et al. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004 Aug 25;292(8):935–42. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- 38.Lancet Global Mental Health Group. Chisholm D, Flisher AJ, Lund C, Patel V, Saxena S, Thornicroft G, Tomlinson M. Scale up services for mental disorders: a call for action. Lancet. 2007 Oct 6;370(9594):1241–52. doi: 10.1016/S0140-6736(07)61242-2. Review. [DOI] [PubMed] [Google Scholar]
- 39.Jaycox LH, Tanielian TL, Sharma P, Morse L, Clum G, Stein BD. Schools' mental health responses after Hurricanes Katrina and Rita. Psychiatr Serv. 2007 Oct;58(10):1339–43. doi: 10.1176/ps.2007.58.10.1339. [DOI] [PubMed] [Google Scholar]
- 40.Wells KB, Sherbourne CD, Miranda J, Tang L, Benjamin B, Duan N. The cumulative effects of quality improvement for depression on outcome disparities over 9 years: results from a randomized, controlled group-level trial. Med Care. 2007 Nov;45(11):1052–9. doi: 10.1097/MLR.0b013e31813797e5. [DOI] [PubMed] [Google Scholar]


