Abstract
Aims/hypothesis
The glomerular endothelial layer is coated by the endothelial surface layer (ESL), which is suggested to play a role in regulation of the permselectivity of macromolecules. Production of heparanase, a degrading enzyme of the ESL, is induced by reactive oxygen species (ROS). We hypothesised that oxidative stress could cause deterioration of the glomerular ESL by induction of heparanase, resulting in increased glomerular permeability.
Methods
Male Zucker fatty (ZF) rats with albuminuria and Zucker lean (ZL) rats were used in this study. Some of the ZF rats were treated with the angiotensin II receptor blocker, irbesartan. We determined the amount of ESL by wheat germ agglutinin staining and heparan sulphate proteoglycan production by western blot analysis. Glomerular hyperfiltration of macromolecules was visualised using in vivo microscopy. We used 2′,7′-dichlorofluorescein diacetate-derived chemiluminescence staining to assess ROS production, and heparanase production and expression were determined by western blot analysis and quantitative real-time polymerase chain reaction respectively.
Results
By 18 weeks of age, ZF rats had developed albuminuria. The glomerular endothelial cell glycocalyx was significantly decreased in ZF compared with ZL rats. Glomerular filtration and the permeability of macromolecules were increased in ZF, but not in ZL rats. Glomerular ROS and heparanase production were significantly increased in ZF compared with ZL rats. These changes in ZF rats were reversed by irbesartan treatment.
Conclusions/interpretation
Increased oxidative stress induces glomerular ESL deterioration in part through increased heparanase levels, resulting in exacerbation of glomerular permselectivity and development of albuminuria.
Electronic supplementary material
The online version of this article (doi:10.1007/s00125-010-1810-0) contains supplementary material, which is available to authorised users.
Keywords: Endothelial cell, Endothelial surface layer, Glomerulus, Glycocalyx, Haemodynamics, Permeability, Reactive oxygen species, Vascular regulation, Zucker fatty rat
Introduction
Recent clinical studies have indicated that a decreased glomerular filtration rate and albuminuria are strong risk factors not only for end-stage renal disease, but also cardiovascular events including coronary heart disease, heart failure, stroke and peripheral arterial disease [1, 2]. An elevated urinary albumin excretion rate is associated with a two- to fourfold increase in cardiovascular and all-cause mortality rates [3]. These observations have led to the hypothesis that a common process underlies albuminuria and cardiovascular events. Any degree of albuminuria is thought to increase the risk of cardiovascular events in the general population with or without diabetes or hypertension [4, 5]. The risk of cardiovascular events increases with an increase in urine albumin:creatinine ratio, starting well below the microalbuminuria cut-off [4, 5]. The results of a clinical study have shown that endothelial dysfunction is correlated with albuminuria [6], suggesting that endothelial dysfunction may be a link between albuminuria and atherosclerotic cardiovascular disease. However, the detailed mechanisms linking microalbuminuria with end-organ damage remain unclear.
Microalbuminuria results from the increased passage of albumin through the glomerular filtration barrier. This barrier is composed of glomerular endothelial cells (GEnCs), a glomerular basement membrane and glomerular epithelial cells. It has been thought that GEnCs do not have an important role in the filtration barrier because of the many small pores, known as fenestrae, which are 60 to 80 nm in diameter [7]. It has recently been reported that GEnCs are covered by an endothelial surface layer (ESL), containing glycocalyx and cell coat [7], which extends into the fenestrae [8]. The ESL covers the cellular surface and is composed of large amounts of glycoprotein, such as heparan sulphate proteoglycan (HSPG) [9]. Because of the presence of sulphated sugar chains in HSPG, the ESL is highly negatively charged, thereby regulates vascular permeability. A decrease in the thickness of the ESL is associated with an increase in vascular permeability [10] and the onset of albuminuria [11]. Furthermore, decreased ESL thickness was found to increase the GEnC permeability in an vitro study [8]. However, the relationship between glomerular endothelial dysfunction, perturbation of the ESL and the appearance of albuminuria in vivo remains to be elucidated.
We hypothesised that the glomerular ESL contributes to regulation of glomerular permeability and the development of albuminuria. Using the diabetic Zucker fatty (ZF) rat as a model of metabolic syndrome, we therefore investigated the relationship between perturbation of the ESL and development of albuminuria, as well as the molecular mechanisms involved and the influence of the angiotensin II receptor blocker (ARB), irbesartan.
Methods
In vivo study: animals
Male Zucker lean (ZL) and ZF rats (6 weeks old) were purchased from Charles River Laboratories Japan (Kanagawa, Japan). Obese rats weighing 140 to 150 g were randomly divided into two groups: ZF rats treated with vehicle (n = 8) or those treated with irbesartan (ZF + ARB, n = 8, 25 mg kg−1 day−1; Dainippon Sumitomo Pharma, Osaka, Japan). ZL rats weighing 100 to 110 g were treated with vehicle (n = 8). All rats were kept under controlled temperature and humidity conditions with 12 h light/dark cycles and had free access to water. The experimental protocol (number 08-007) was approved by the Animal Research Committee of Kawasaki Medical School and was conducted according to the Guide for the Care and Use of Laboratory Animals of Kawasaki Medical School based on the National Institutes of Health Guide for the Care and Use of Laboratory Animals (NIH Publications No. 80-23, revised 1996).
Physiological and biochemical measurements
At 12 weeks after the start of treatment, systolic arterial blood pressure was measured in pre-warmed rats using the tail-cuff method (BP-98A; Softron, Tokyo, Japan). Glucose tolerance was assessed by intraperitoneal glucose tolerance test after fasting for 16 h. A bolus of glucose (2 g/kg i.p.) was injected and blood samples were collected from the tail vein at intervals of 0 and 120 min, and tested for glucose. Glucose was measured using a glucose meter (Medisafe-Mini; Terumo, Tokyo, Japan). To collect urine samples at 12 weeks, rats were placed in metabolism cages for 24 h and given access to tap water, but no food. Albumin concentration in 24 h urine samples was measured by enzyme-linked immunosorbent assay (Exocell, Philadelphia, PA, USA). After collection of urine, the rats were killed under sevoflurane inhalation anaesthesia and blood samples were obtained immediately. Serum creatinine and fasting serum glucose levels were measured.
Histological assessment
Kidney sections (4 μm thick) were stained with periodic acid–Schiff’s (PAS) and tetramethylrhodamine isothiocyanate-conjugated wheat germ agglutinin (WGA) (Vector Laboratories, Burlingame, CA, USA). PAS-stained kidney sections were photographed using a microscope (Eclipse E800; Nikon, Tokyo, Japan) and digitised into 1,372- to 1,024-pixel colour scale images using a software program (ACT-1C DXM 1200C; Nikon). Histological scores were assessed using a Coolscope (Nikon). Tetramethylrhodamine isothiocyanate-conjugated WGA-stained kidney sections were analysed using TCS-NT system software (Leica-Microsystems, Tokyo Japan). Three nephrologists semiquantitatively analysed PAS- and WGA-stained sections in a blind fashion. The severity of glomerular injury was evaluated by glomerulosclerosis score from 0 to 4 as described previously [12]. The glomerular ESL was also evaluated by the WGA staining score with respect to the amount of degradation as follows: 0, none; 1, mild; 2, moderate; 3, severe; 4, global degradation. At least 50 glomeruli were randomly selected from each rat and the mean score was calculated.
Lanthanum nitrate staining
Lanthanum nitrate staining was performed as described previously [13]. A 5 ml bolus of lanthanum nitrate solution (1.0%, wt/vol., pH 7.1) was injected into the aorta. Fixed tissues were embedded in Spurr’s low-viscosity resin (Electron Microscopy Sciences, Hatfield, PA, USA) and polymerised. They were then cut with a diamond knife on an Ultracut UCT microtome (Leica-Microsystems), mounted on copper grids coated with Formvar films and stained with uranyl acetate and lead citrate. Ultrathin sections were examined with an electron microscope (H-7100; Hitachi, Tokyo, Japan).
In vivo imaging of macromolecule hyperfiltration
For fluorescent probes, 40 kDa fluorescein–dextran (anionic, excitation 494 nm, emission 518 nm) was obtained from Invitrogen (Tokyo, Japan). A multiphoton excitation laser-scanning fluorescence microscopy confocal microscope system (TCS SP2 AOBS MP; Leica-Microsystems) was used in these studies. In vivo imaging of the glomerular microcirculation was performed as described previously [14]. For analysis of glomerular permeability, a 40 kDa fluorescein–dextran solution was infused through the jugular venous catheter immediately.
In vitro study: cells
Primary normal human GEnCs were purchased from Cell System (Kirkland, WA, USA) and cultured according to the manufacturer’s instructions. Human GEnCs were cultured in endothelial cell basal medium-2 (Lonza, Walkersville, MD, USA) containing v/v 2% fetal bovine serum under humidified conditions (95% air, 5% CO2) at 37°C. Confluent cells from seven to ten passages were used in the experiments. These cells were divided into three groups: LG, low glucose (5 mmol/l); HG, high glucose (30 mmol/l); and HG + ARB, high glucose plus irbesartan (5 µmol/l). The cells were incubated at 37°C for 2 to 24 h (2 h for reactive oxygen species [ROS] detection and NAD(P)H oxidase assay, 4 h for RNA isolation and nuclear protein preparation, and 24 h for total protein preparation).
Fluorescence spectrometric assay for production of ROS
Glomeruli were isolated by sieving as previously described [15]. Production of ROS, including H2O2 and peroxynitrite, was measured in isolated glomeruli using the 2′,7′-dichlorodihydrofluorescein-diacetate (DCFH-DA) method, as previously described [15]. The mean fluorescence intensity of the isolated glomeruli (600 glomeruli from six rats in each group) was analysed using TCS-NT system software (Leica-Microsystems). Intracellular ROS levels were measured using fluorescence-activated cell sorting [16]. Cells were incubated for 15 min with 20 μmol/l DCFH-DA in medium at 37°C in the dark. In each sample, a minimum of 10,000 cells was subjected to fluorescence-activated cell sorting using a FACS Calibur (Nippon Becton Dickinson, Tokyo, Japan) and CellQuest software (Nippon Becton Dickinson).
Lucigenin chemiluminescence assay for NAD(P)H oxidase activity
Superoxide production by NAD(P)H oxidase in isolated glomeruli or cultured cells was measured by lucigenin chemiluminescence as described previously [17]. Lucigenin chemiluminescence was expressed in units min−1 mg−1.
RNA isolation and real-time quantitative polymerase chain reaction
Total RNA extraction from isolated glomeruli or cultured cells, reverse transcriptase reaction and real-time quantitative polymerase chain reaction were performed as described previously [17]. The primers and probes used for rat gp91phox (also known as Cybb), rat p67phox, rat heparanase and human heparanase were listed in Electronic supplementary material [ESM] Table 1.
Western blotting
Extraction of total cellular protein and nuclear protein was performed using extraction reagent (T-PER tissue protein extraction reagent, NE-PER nuclear and cytoplasmic extraction kit; Thermo Fisher Scientific, Rockford, IL, USA) according to the manufacturer’s instructions. Sodium dodecyl sulphate–polyacrylamide gel electrophoresis was performed on portions of the isolated glomeruli (100 μg/lane) or cultured cells (20 μg/lane for heparanase-1, 5 μg/lane for v-ets erythroblastosis virus E26 oncogene homologue 1 [avian] [ETS-1]). Anti-perlecan antibody (Santa Cruz Biotechnology, Santa Cruz, CA, USA), anti-syndecan-1 antibody (Santa Cruz), anti-heparanase-1 antibody (Santa Cruz), anti-ETS-1 antibody (Abcam, Cambridge, MA, USA), anti-tubulin alpha antibody (Lab vision, Thermo Scientific, CA, USA) and anti-beta tubulin antibody (Santa Cruz) were used as the primary antibodies. Coomassie Brilliant Blue staining of the membrane confirmed equal loading and transfer. Signals were detected using the ECL system (Amersham Biosciences, Piscataway, NJ, USA). The relative optical densities of bands were quantified using Image J analysis software V1.42 (http://rsbweb.nih.gov/ij//, accessed 1 January 2010).
Statistical analysis
Values are expressed as mean ± SD. All variables except the glomerular damage score and WGA staining score were evaluated with two-tailed unpaired Student’s t test or Welch’s t test. The glomerular damage score and WGA staining score were evaluated with Mann–Whitney’s U test. A p value of p < 0.05 denoted a statistically significant difference.
Results
Physiological data and glomerular injury in ZF rats
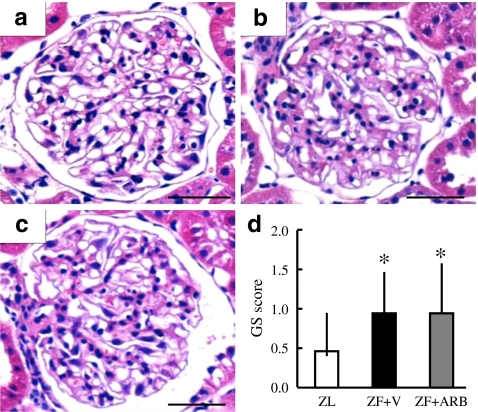
Table 1 shows physiological data for the three groups. There were statistically significant increases in body weight, glucose-loaded serum glucose level and albuminuria, and a decrease in serum creatinine levels in the ZF vehicle compared with the ZL rat groups. In contrast, administration of irbesartan (ZF + ARB) led to significant decreases in body weight, systolic blood pressure and albuminuria compared with the ZF vehicle group, but had no effect on glucose-loaded serum glucose level. Glomerular injury was evaluated by glomerulosclerosis score with PAS staining in all groups (Fig. 1). There was a slight expansion of the mesangial area in the ZF compared with the ZL animals (glomerulosclerosis score 1.0 ± 0.5 vs 0.5 ± 0.5, respectively, p < 0.05). ARB administration did not affect the glomerulosclerosis score. The grading scores, however, remained low in all three groups, because the histological changes were unremarkable even in untreated ZF rats.
Table 1.
Physiological data
| Characteristics | ZL (n = 6) | ZF vehicle (n = 8) | ZF + ARB (n = 8) |
|---|---|---|---|
| Body weight (g) | 381 ± 21 | 691 ± 32a | 594 ± 47a,b |
| Systolic BP (mmHg) | 128 ± 5 | 122 ± 17 | 104 ± 7a,b |
| FSG (mmol/l) | 4.2 ± 0.7 | 4.2 ± 1.7 | 3.6 ± 1.6 |
| Glucose-loaded SG (mmol/l) | 7.7 ± 1.4 | 10.9 ± 2.4a | 9.9 ± 1.7a |
| S-Crn (µmol/l) | 19.5 ± 5.3 | 13.3 ± 2.7a | 12.4 ± 3.5a |
| ACR (mg/mmol) | 23.6 ± 13.1 | 288.5 ± 26.2a | 65.6 ± 7.9b |
Data are expressed as mean ± SD
a p < 0.05 vs ZL; b p < 0.05 vs ZF vehicle
ACR, urinary albumin:creatinine ratio; FSG, fasting serum glucose; S-Crn, serum creatinine; SG, serum glucose
Fig. 1.
Pathological glomerular changes. a Glomerular morphological changes (PAS staining) in ZL, b ZF vehicle-treated (ZF + V) and c ZF + ARB rats. Scale bar, 50 μm. d Glomerulosclerosis (GS) score, data are mean ± SD; *p < 0.05 vs ZL
Evaluation of glomerular ESL
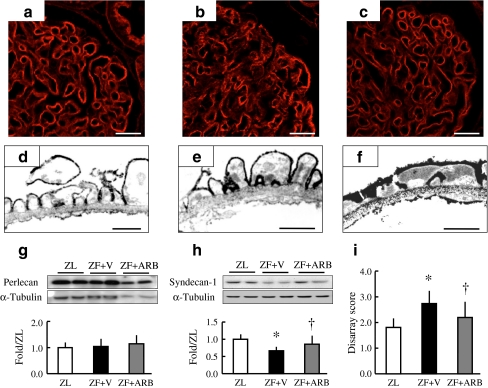
First, glomerular ESL was detected by lectin staining. Paraffin-embedded specimens were stained with WGA lectin, which binds to sugar residues, sialic acid and N-acetylglucosaminyl residues of glycoproteins. WGA lectin was observed on the glomerular loop including endothelial cells, podocytes and the glomerular basement membrane in ZL rats (Fig. 2a). The disarray of WGA staining was demonstrated in ZF vehicle-treated rats (Fig. 2b), but was significantly ameliorated by treatment with irbesartan (Fig. 2c). The degree of WGA disarray was examined semi-quantitatively using a scoring system (Fig. 2i). The score was significantly increased in ZF vehicle-treated compared with the ZL rats (2.5 ± 0.7 vs 1.8 ± 0.3, respectively, p < 0.05) and ameliorated by irbesartan treatment (2.1 ± 0.5, p < 0.05 vs ZF vehicle). Second, the glomerular ESL was evaluated using the lanthanum nitrate perfusion method. To delineate the glomerular ESL by electron microscopy, we perfused the kidneys with the cationic reagent lanthanum nitrate, which is commonly used as an efficient marker of anionic sites on the ESL. In the ZL rats, deposits of lanthanum nitrate were found on the surface of endothelial cells and podocytes (Fig. 2d). However, in the ZF vehicle-treated rats, lanthanum nitrate deposits were only observed on the surface of the podocytes (Fig. 2e). In the ZF + ARB group, the deposits were observed again on the surface of endothelial cells (Fig. 2f). Third, the amount of proteoglycan core proteins was examined by western blot analysis using lysates from isolated glomeruli. Perlecan (a cross-linked extracellular matrix molecule) and syndecan (which is cell membrane-bound) are HSPGs, which are major components of the glycocalyx [18]. Perlecan levels were not changed in any of the groups (Fig. 2g), but syndecan levels were significantly reduced in the ZF vehicle-treated compared with the ZL animals (0.7 ± 0.1-fold, p < 0.05 vs ZL). The reduction was ameliorated by administration of irbesartan (p < 0.05 vs ZF vehicle).
Fig. 2.
Evaluation of glomerular ESL. a Glomerular ESL shown by WGA staining in ZL, b ZF vehicle-treated (ZF + V) and c ZF + ARB rats. Scale bar, 20 µm. d Glomerular capillary anionic sites shown by lanthanum nitrate staining in ZL, e ZF vehicle and f ZF + ARB rats. Scale bar 1 µm. g Western blot with bar graph quantification of perlecan and h syndecan. i Disarray score of WGA staining. Data (g–i) are expressed as mean ± SD. *p < 0.05 vs ZL; † p < 0.05 vs ZF vehicle
Visualisation of glomerular hyperfiltration of macromolecules
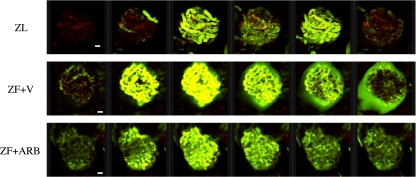
Glomerular hyperfiltration of macromolecules was examined by intravenous injection of fluorescein isothiocyanate-conjugated dextran as previously reported [14]. We used 40 kDa dextran, which is not easily filtrated in ESL-preserved endothelium, to visualise glomerular filtration in all groups. There was a very small volume of filtered 40 kDa fluorescein isothiocyanate-labelled dextran in the Bowman’s capsule space in the ZL group (Fig. 3, ESM Video clip 1), but massive leakage of this dextran was seen in ZF vehicle-treated animals (Fig. 3, ESM Video clip 2). Only a small amount of 40 kDa dextran was observed in the glomeruli of the ZF + ARB rats (Fig. 3, ESM Video clip 3).
Fig. 3.
Glomerular hyperfiltration of macromolecules. Representative series of images showing hyperfiltration of macromolecules in glomeruli per rat groups as indicated. Green, 40 kDa fluorescein isothiocyanate-labelled dextran. Scale bar, 40 µm. Time per frame, 870 ms. ZF + V, ZF vehicle-treated
Evaluation of heparanase expression and ROS production
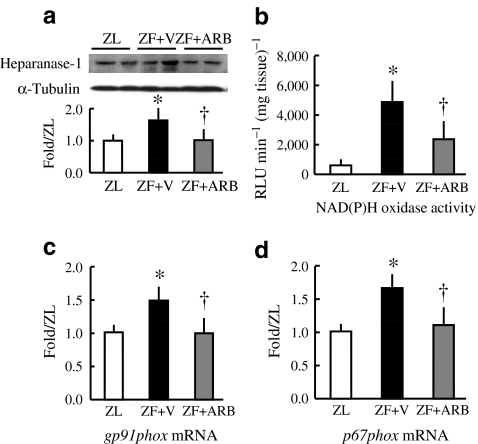
In the ZF vehicle-treated rats, heparanase protein levels were significantly increased compared with the ZL group (p < 0.05) (Fig. 4a). ARB administration significantly restored the increase of heparanase levels (p < 0.05). Production of heparanase has been shown to be regulated by oxidative stress [19]. Therefore, ROS production in glomeruli was evaluated by confocal laser-scanning microscopy using DCFH-DA staining. The glomerular 2′, 7′-dichlorofluorescein intensity was increased in ZF vehicle-treated compared with ZL rats (1.9 ± 0.9-fold, p < 0.05) and reduced by ARB treatment (1.4 ± 0.7-fold, p < 0.05 vs ZF vehicle). NAD(P)H oxidase activity in isolated glomeruli as a source of ROS production was determined by lucigenin chemiluminescence assay (Fig. 4b). ROS production by NAD(P)H oxidase was significantly increased in the ZF vehicle-treated compared with the ZL rats (p < 0.05), while irbesartan treatment significantly reduced NAD(P)H oxidase activity (p < 0.05 vs ZF vehicle). The mRNA expression of the NAD(P)H oxidase component genes gp91phox and p67phox were increased in the ZF vehicle-treated compared with the ZL rats (Fig. 4c, d). These changes were ameliorated by administration of irbesartan.
Fig. 4.
Glomerular heparanase levels and expression, and NAD(P)H oxidase activity. a Western blot with bar graph quantifying glomerular heparanase-1. b Glomerular NAD(P)H oxidase activity assessed by lucigenin chemiluminescence assay. c Expression of gp91phox and (d) p67phox mRNA. Data are expressed as mean ± SD. *p < 0.05 vs ZL; † p < 0.05 vs ZF vehicle (ZF + V)
Mechanisms of heparanase induction in glomerular endothelial cells
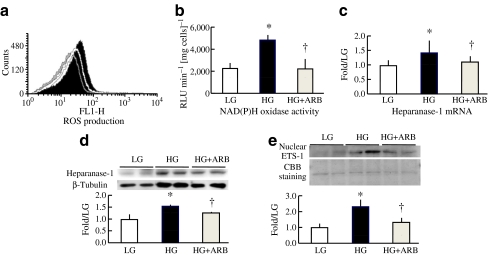
The rate of ROS production was increased in the human GEnCs treated with high glucose compared with those treated with low glucose. ROS production in the ARB-treated group was reduced to the same level as in the low glucose-treated group (Fig. 5a). NAD(P)H oxidase activity assessed by lucigenin chemiluminescence was enhanced in the high glucose compared with the low glucose and was ameliorated in the high glucose + ARB group (Fig. 5b). The expression of heparanase mRNA and heparanase protein levels were also increased in the human GEnCs by high glucose treatment (Fig. 5c, d), these increases being normalised by co-incubation with irbesartan. ETS-1 is one of the key transcription factors that regulate heparanase gene expression [20]. Protein levels of ETS-1 in the nuclei of human GEnCs were also increased by high glucose treatment and restored by co-treatment with irbesartan (Fig. 5e).
Fig. 5.
High-glucose-induced ROS production, NAD(P)H oxidase activity and heparanase expression in human GEnCs. a Evaluation of ROS production by flow cytometry in DCFH-stained cells. White, low glucose (LG); black, high glucose (HG); grey, high glucose plus ARB. b NAD(P)H oxidase activity assessed by lucigenin chemiluminescence assay; c heparanase mRNA expression assessed by quantitative real-time polymerase chain reaction; and d heparanase-1 protein levels assessed by western blot analysis. e ETS-1 protein levels in nuclei assessed by western blot analysis. Data are expressed as mean ± SD; *p < 0.05 vs LG; † p < 0.05 vs HG
Discussion
The aim of this study was to examine whether the glomerular ESL contributes to regulation of glomerular permeability and the development of albuminuria. We have shown that glomerular ESL perturbation coincides with increased glomerular vascular permeability and albuminuria in a rat model of metabolic syndrome. We also found that the increased ROS production in GEnCs upregulated expression of heparanase, an endoglycosidase that degrades HSPG, a major constituent of the vascular glycocalyx. Furthermore, we found that irbesartan treatment ameliorated oxidative stress, preserved the integrity of the glomerular ESL and also exerted an antiproteinuric effect.
The ESL covers the systemic vascular endothelium and coats the luminal surface of the glomerular capillaries. Previous studies have indicated that the glycocalyx, a component of the ESL, regulates vascular permeability [10], senses shear stress as a mechano-transduction sensor [21], attaches to blood cells [22], regulates enzyme activity [23, 24] and anchors enzymes to the cell surface [25]. However, the role of the glomerular ESL remains poorly defined. Recently, Singh et al. reported that enzymatic removal of glycocalyx from GEnCs leads to increased permeability of albumin across the cell layer [8]. Reduction of the glomerular endothelial glycocalyx was detected and demonstrated to be involved in deterioration of permselectivity in an adriamycin-induced rat model of nephrotic syndrome [26]. In the present study, we revealed that the glomerular ESL is decreased in ZF rats as visualised by WGA and lanthanum nitrate staining methods. Furthermore, the results of lanthanum nitrate staining indicated that the ESL on the epithelial side along the glomerular basement membrane was well preserved, although the ESL is significantly decreased in this disease model. These results suggest a causal relationship between decreased glomerular ESL and enhanced glomerular permeability of macromolecules in vivo.
Podocyte slit diaphragm also plays an important role in glomerular permeability. Previous studies have reported that injured podocytes with foot process effacements developed a large degree of proteinuria [27]. On the other hand, albuminuria can be observed without podocyte foot process effacement in some disease models. Injection of antibodies to vascular endothelial growth factor or soluble vascular endothelial growth factor receptor 1 [28] cause albuminuria, hypertension and endothelial cell dysfunction without affecting podocyte morphology. These data indicate that GEnCs may play a role in the successful retention of albumin. Disruption of slit diaphragms, as in nephrin-knockout mice, causes massive proteinuria, with not a small degree of albuminuria [29].
At present, it is not clear whether glomerular permeability is dependent on ESL thickness or a change in ESL quality. van den Hoven et al. reported that reduction of anionic sites did not lead to proteinuria in heparanase-overexpressed mice, but these mice had a mild but significant increase in urinary albumin excretion [30]. Also perlecan-deficient mice did not develop glomerular abnormalities and albuminuria under physiological conditions [31], but did develop albuminuria under albumin-loaded conditions. These studies suggest that even if one of the HSPGs did decrease in physiological conditions, it might not be enough to develop morphological changes or proteinuria. We have demonstrated that syndecan, one of the glomerular HSPGs, decreased in ZF rat. However, we were unable to exclude the possibility that other components of glomerular ESL were altered. We speculate that quantitative and qualitative alterations of ESL developed in this model and resulted in perturbation of glomerular permeability.
We observed that heparanase expression was stimulated in the glomeruli of ZF rats. HSPG confers anionic charge to the glomerular vascular wall so that the ESL regulates permselectivity of the glomerulus [10]. HSPG is initially internalised from the cell surface mainly by endocytosis [32]. Glycosaminoglycan chains are degraded by heparanase, an endo-β-d-glucuronidase that specifically reacts with heparan sulphate. Increased levels of heparanase and a concomitant decrease in glomerular heparan sulphate glycosaminoglycan have been demonstrated in a variety of disease models, including streptozotocin-induced diabetes, adriamycin-induced nephrotic syndrome and Heymann’s nephritis [19, 33, 34]. Decreased levels of glomerular heparan sulphate have also been demonstrated in human renal diseases, including diabetic nephropathy [35], but levels are minimally changed in nephritic syndrome [36]. Moreover, it has been reported that heparanase, which degrades the glycocalyx, is regulated by high glucose [37], angiotensin II and ROS [19]. The results of the present study also demonstrated the upregulation of heparanase by high glucose concentration and the simultaneous decrease in glycocalyx, a major component of ESL.
Sulphated portions of glycosaminoglycan side chains in HSPG play an important role in charge-dependent selectivity of glomerular filtration of plasma proteins. N-deacetylase/N-sulfotransferase (NDST [also known as NDST1]), which substitutes the N-acetyl moiety of glucosamine for a sulphate group, is the key enzyme regulating sulphation of glycosaminoglycan chains. Williams et al. have reported that hepatic NDST mRNA, NDST protein and enzymatic activities were suppressed in a rat model of diabetes and suggested that angiotensin II contributes to the suppression of NDST protein and enzymatic activity [38]. We also examined glomerular expression of NDST and confirmed that expression was decreased in the ZF group compared with ZL group and that ARB treatment increased NDST expression (data not shown). Using another model of renal nephritis, Nakayama et al. reported that NDST mRNA is decreased in glomeruli during the nephritic period [39]. These data suggest an important role for this enzyme in heparan sulphate assembly in GEnCs and in the pathogenesis of albuminuria.
It has been reported that ACE inhibitors and ARBs suppress heparanase expression and preserve HSPGs from degradation [19, 40]. Similar effects were achieved by antioxidant administration, suggesting that the antioxidant activities of ACE inhibitors and ARBs are involved in the protection of HSPGs. Angiotensin II is known to directly induce expression of NAD(P)H oxidase components and enhance ROS generation [41]. The results of the present study demonstrated that irbesartan suppresses NAD(P)H oxidase activation and possesses antioxidant activity. ARBs are multifunctional agents, which effectively reduce blood nitrotyrosine levels in patients with type 1 diabetes [42] and restore impaired catalase and glutathione peroxidase activities [43, 44]. The ability of irbesartan to decrease ROS production and activate the antioxidant defence system could prevent upregulation of heparanase in this rat model of metabolic syndrome.
Blood pressure was significantly decreased by irbesartan treatment in ZF rats. Thus, the hypotensive effect of irbesartan would affect glomerular hypertension and glomerular permeability. We have previously reported that intra-glomerular hypertension induces glomerular ROS production that is dependent on NAD(P)H oxidase activity [15]. ARB treatment improves glomerular hypertension through dilation of efferent arterioles and reduction of oxidative stress in glomeruli. In this study, irbesartan may have improved glomerular permeability by reducing ROS production in a way that was dependent on and independent of the intra-glomerular pressure-lowering effect.
The glycocalyx is ubiquitously distributed on vascular endothelial cells throughout the body. A series of animal studies revealed that disruption of the glycocalyx was associated with vascular disease such as adhesion of inflammatory cells to the vessel wall and hypertrophy of the vascular wall [45]. The glycocalyx also serves as a mechanosensor, sensing vascular shear stress to regulate vascular tone by nitric oxide generation [21]. Taken together, these results suggest that impairment of the ESL can affect vascular function and may be the first sign of vascular disorders. A correlation between acute hyperglycaemia and the onset of cardiovascular events has been shown by a large-scale clinical study [46]. Considering that the levels of glycocalyx decrease upon a rapid increase in blood sugar level [47], deterioration of the ESL is likely to be a risk factor for cardiovascular disease. The results of a separate clinical study demonstrated that albuminuria is indicative of systemic endothelial dysfunction in diabetes mellitus [6], whereas the Hoorn study showed that microalbuminuria correlates with the degree of impairment of flow-mediated dilation, which is indicative of vascular endothelial dysfunction in diabetic and non-diabetic patients [48]. This strongly suggests that deterioration of the ESL induces endothelial dysfunction and that such deterioration in the kidney leads to the onset of albuminuria.
We demonstrated an association between the deterioration of the ESL and albuminuria, an established surrogate marker of cardiovascular events. A limitation of the present study is that we were not able to determine the mechanism of this association. Studies using endothelial cell-specific transgenic mice that are deficient in or overexpress heparanase and/or NDST will elucidate the effects of these enzymes on glycocalyx production in the glomerular endothelium and any role of the ESL in the development of albuminuria. Another limitation of this study is that the ZF rat is a model of obesity and metabolic syndrome, not of diabetic nephropathy. The ZF rat shows postprandial hyperglycaemia and presents albuminuria, not proteinuria; it therefore resembles an early stage of diabetic nephropathy with microalbuminuria in humans. Thus, the results of the present study cannot apply to all stages of diabetic nephropathy.
In conclusion, we have demonstrated that the glomerular ESL is implicated in regulation of glomerular wall permeability and that ROS-induced deterioration of the ESL exacerbates glomerular permeability. The ARB irbesartan prevented deterioration of the ESL and suppressed albuminuria. It is highly likely that protection of the ESL would not only be effective in suppressing development of albuminuria, but also in slowing the progression of atherosclerosis. Therefore, the ESL is a potential therapeutic target for cardiovascular diseases.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 8.19 kb)
Glomerular filtration of 40 kDa fluorescein isothiocyanate-labelled dextran in ZL rat (MOV 1396 kb)
Glomerular filtration of 40 kDa fluorescein isothiocyanate-labelled dextran in ZF vehicle-treated rat (MOV 1725 kb)
Glomerular filtration of 40 kDa fluorescein isothiocyanate-labelled dextran in ZF+ARB rat (MOV 693 kb)
Acknowledgements
This work was supported by Grants-in-Aid for Scientific Research from the Japan Society of the Promotion of Science (No. 21591047 to N. Kashihara), Okayama Medical Foundation (to M. Satoh), Ryobi Teien Memory Foundation (to M. Satoh) and Kawasaki Foundation for Medical Science and Medical Welfare (to M. Satoh). Irbesartan was kindly supplied by Dainippon Sumitomo Pharma (Osaka, Japan). We thank S. Hanada, E. Yorimasa, K. Ehara and M. Ishihara (Kawasaki Medical School) for animal care and technical assistance.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Abbreviations
- ARB
Angiotensin II receptor blocker
- DCFH-DA
2′,7′-Dichlorodihydrofluorescein-diacetate
- ESL
Endothelial surface layer
- ETS-1
v-Ets erythroblastosis virus E26 oncogene homologue 1 (avian)
- GEnC
Glomerular endothelial cell
- HSPG
Heparan sulphate proteoglycan
- NDST
N-Deacetylase/N-sulfotransferase
- PAS
Periodic acid–Schiff’s
- ROS
Reactive oxygen species
- WGA
Wheat germ agglutinin
- ZF
Zucker fatty
- ZL
Zucker lean
References
- 1.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 2.Hillege HL, Fidler V, Diercks GF, et al. Urinary albumin excretion predicts cardiovascular and noncardiovascular mortality in general population. Circulation. 2002;106:1777–1782. doi: 10.1161/01.CIR.0000031732.78052.81. [DOI] [PubMed] [Google Scholar]
- 3.Jager A, Kostense PJ, Ruhe HG, et al. Microalbuminuria and peripheral arterial disease are independent predictors of cardiovascular and all-cause mortality, especially among hypertensive subjects: five-year follow-up of the Hoorn Study. Arterioscler Thromb Vasc Biol. 1999;19:617–624. doi: 10.1161/01.atv.19.3.617. [DOI] [PubMed] [Google Scholar]
- 4.Arnlov J, Evans JC, Meigs JB, et al. Low-grade albuminuria and incidence of cardiovascular disease events in nonhypertensive and nondiabetic individuals: the Framingham Heart Study. Circulation. 2005;112:969–975. doi: 10.1161/CIRCULATIONAHA.105.538132. [DOI] [PubMed] [Google Scholar]
- 5.Gerstein HC, Mann JF, Yi Q, et al. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA. 2001;286:421–426. doi: 10.1001/jama.286.4.421. [DOI] [PubMed] [Google Scholar]
- 6.Stehouwer CD, Nauta JJ, Zeldenrust GC, Hackeng WH, Donker AJ, den Ottolander GJ. Urinary albumin excretion, cardiovascular disease, and endothelial dysfunction in non-insulin-dependent diabetes mellitus. Lancet. 1992;340:319–323. doi: 10.1016/0140-6736(92)91401-S. [DOI] [PubMed] [Google Scholar]
- 7.Haraldsson B, Nystrom J, Deen WM. Properties of the glomerular barrier and mechanisms of proteinuria. Physiol Rev. 2008;88:451–487. doi: 10.1152/physrev.00055.2006. [DOI] [PubMed] [Google Scholar]
- 8.Singh A, Satchell SC, Neal CR, McKenzie EA, Tooke JE, Mathieson PW. Glomerular endothelial glycocalyx constitutes a barrier to protein permeability. J Am Soc Nephrol. 2007;18:2885–2893. doi: 10.1681/ASN.2007010119. [DOI] [PubMed] [Google Scholar]
- 9.Adamson RH, Clough G. Plasma proteins modify the endothelial cell glycocalyx of frog mesenteric microvessels. J Physiol. 1992;445:473–486. doi: 10.1113/jphysiol.1992.sp018934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van den Berg BM, Vink H, Spaan JA. The endothelial glycocalyx protects against myocardial edema. Circ Res. 2003;92:592–594. doi: 10.1161/01.RES.0000065917.53950.75. [DOI] [PubMed] [Google Scholar]
- 11.Nieuwdorp M, Mooij HL, Kroon J, et al. Endothelial glycocalyx damage coincides with microalbuminuria in type 1 diabetes. Diabetes. 2006;55:1127–1132. doi: 10.2337/diabetes.55.04.06.db05-1619. [DOI] [PubMed] [Google Scholar]
- 12.Namikoshi T, Tomita N, Fujimoto S, et al. Isohumulones derived from hops ameliorate renal injury via an anti-oxidative effect in Dahl salt-sensitive rats. Hypertens Res. 2007;30:175–184. doi: 10.1291/hypres.30.175. [DOI] [PubMed] [Google Scholar]
- 13.Hjalmarsson C, Johansson BR, Haraldsson B. Electron microscopic evaluation of the endothelial surface layer of glomerular capillaries. Microvasc Res. 2004;67:9–17. doi: 10.1016/j.mvr.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Satoh M, Kobayashi S, Kuwabara A, Tomita N, Sasaki T, Kashihara N. In vivo visualization of glomerular microcirculation and hyperfiltration in streptozotocin-induced diabetic rats. Microcirculation. 2010;17:103–112. doi: 10.1111/j.1549-8719.2009.00010.x. [DOI] [PubMed] [Google Scholar]
- 15.Fujimoto S, Satoh M, Horike H, et al. Olmesartan ameliorates progressive glomerular injury in subtotal nephrectomized rats through suppression of superoxide production. Hypertens Res. 2008;31:305–313. doi: 10.1291/hypres.31.305. [DOI] [PubMed] [Google Scholar]
- 16.Satoh M, Kashihara N, Fujimoto S, et al. A novel free radical scavenger, edarabone, protects against cisplatin-induced acute renal damage in vitro and in vivo. J Pharmacol Exp Ther. 2003;305:1183–1190. doi: 10.1124/jpet.102.047522. [DOI] [PubMed] [Google Scholar]
- 17.Satoh M, Fujimoto S, Arakawa S, et al. Angiotensin II type 1 receptor blocker ameliorates uncoupled endothelial nitric oxide synthase in rats with experimental diabetic nephropathy. Nephrol Dial Transplant. 2008;23:3806–3813. doi: 10.1093/ndt/gfn357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bjornson A, Moses J, Ingemansson A, Haraldsson B, Sorensson J. Primary human glomerular endothelial cells produce proteoglycans, and puromycin affects their posttranslational modification. Am J Physiol Ren Physiol. 2005;288:F748–F756. doi: 10.1152/ajprenal.00202.2004. [DOI] [PubMed] [Google Scholar]
- 19.Kramer A, van den Hoven M, Rops A, et al. Induction of glomerular heparanase expression in rats with adriamycin nephropathy is regulated by reactive oxygen species and the renin–angiotensin system. J Am Soc Nephrol. 2006;17:2513–2520. doi: 10.1681/ASN.2006020184. [DOI] [PubMed] [Google Scholar]
- 20.Lu WC, Liu YN, Kang BB, Chen JH. Trans-activation of heparanase promoter by ETS transcription factors. Oncogene. 2003;22:919–923. doi: 10.1038/sj.onc.1206201. [DOI] [PubMed] [Google Scholar]
- 21.Tarbell JM, Pahakis MY. Mechanotransduction and the glycocalyx. J Intern Med. 2006;259:339–350. doi: 10.1111/j.1365-2796.2006.01620.x. [DOI] [PubMed] [Google Scholar]
- 22.Constantinescu AA, Vink H, Spaan JA. Endothelial cell glycocalyx modulates immobilization of leukocytes at the endothelial surface. Arterioscler Thromb Vasc Biol. 2003;23:1541–1547. doi: 10.1161/01.ATV.0000085630.24353.3D. [DOI] [PubMed] [Google Scholar]
- 23.Wilsie LC, Orlando RA. The low density lipoprotein receptor-related protein complexes with cell surface heparan sulfate proteoglycans to regulate proteoglycan-mediated lipoprotein catabolism. J Biol Chem. 2003;278:15758–15764. doi: 10.1074/jbc.M208786200. [DOI] [PubMed] [Google Scholar]
- 24.Allen BL, Filla MS, Rapraeger AC. Role of heparan sulfate as a tissue-specific regulator of FGF-4 and FGF receptor recognition. J Cell Biol. 2001;155:845–858. doi: 10.1083/jcb.200106075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kato H. Regulation of functions of vascular wall cells by tissue factor pathway inhibitor: basic and clinical aspects. Arterioscler Thromb Vasc Biol. 2002;22:539–548. doi: 10.1161/01.ATV.0000013904.40673.CC. [DOI] [PubMed] [Google Scholar]
- 26.Jeansson M, Bjorck K, Tenstad O, Haraldsson B. Adriamycin alters glomerular endothelium to induce proteinuria. J Am Soc Nephrol. 2009;20:114–122. doi: 10.1681/ASN.2007111205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shankland SJ. The podocyte's response to injury: role in proteinuria and glomerulosclerosis. Kidney Int. 2006;69:2131–2147. doi: 10.1038/sj.ki.5000410. [DOI] [PubMed] [Google Scholar]
- 28.Sugimoto H, Hamano Y, Charytan D, et al. Neutralization of circulating vascular endothelial growth factor (VEGF) by anti-VEGF antibodies and soluble VEGF receptor 1 (sFlt-1) induces proteinuria. J Biol Chem. 2003;278:12605–12608. doi: 10.1074/jbc.C300012200. [DOI] [PubMed] [Google Scholar]
- 29.Wartiovaara J, Ofverstedt LG, Khoshnoodi J, et al. Nephrin strands contribute to a porous slit diaphragm scaffold as revealed by electron tomography. J Clin Invest. 2004;114:1475–1483. doi: 10.1172/JCI22562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van den Hoven MJ, Wijnhoven TJ, Li JP, et al. Reduction of anionic sites in the glomerular basement membrane by heparanase does not lead to proteinuria. Kidney Int. 2008;73:278–287. doi: 10.1038/sj.ki.5002706. [DOI] [PubMed] [Google Scholar]
- 31.Morita H, Yoshimura A, Inui K, et al. Heparan sulfate of perlecan is involved in glomerular filtration. J Am Soc Nephrol. 2005;16:1703–1710. doi: 10.1681/ASN.2004050387. [DOI] [PubMed] [Google Scholar]
- 32.Yanagishita M. Glycosylphosphatidylinositol-anchored and core protein-intercalated heparan sulfate proteoglycans in rat ovarian granulosa cells have distinct secretory, endocytotic, and intracellular degradative pathways. J Biol Chem. 1992;267:9505–9511. [PubMed] [Google Scholar]
- 33.van den Hoven MJ, Rops AL, Bakker MA, et al. Increased expression of heparanase in overt diabetic nephropathy. Kidney Int. 2006;70:2100–2108. doi: 10.1038/sj.ki.5001985. [DOI] [PubMed] [Google Scholar]
- 34.Levidiotis V, Freeman C, Tikellis C, Cooper ME, Power DA. Heparanase is involved in the pathogenesis of proteinuria as a result of glomerulonephritis. J Am Soc Nephrol. 2004;15:68–78. doi: 10.1097/01.ASN.0000103229.25389.40. [DOI] [PubMed] [Google Scholar]
- 35.Wijnhoven TJ, van den Hoven MJ, Ding H, et al. Heparanase induces a differential loss of heparan sulphate domains in overt diabetic nephropathy. Diabetologia. 2008;51:372–382. doi: 10.1007/s00125-007-0879-6. [DOI] [PubMed] [Google Scholar]
- 36.Wijnhoven TJ, Geelen JM, Bakker M, et al. Adult and paediatric patients with minimal change nephrotic syndrome show no major alterations in glomerular expression of sulphated heparan sulphate domains. Nephrol Dial Transplant. 2007;22:2886–2893. doi: 10.1093/ndt/gfm301. [DOI] [PubMed] [Google Scholar]
- 37.Maxhimer JB, Somenek M, Rao G, et al. Heparanase-1 gene expression and regulation by high glucose in renal epithelial cells: a potential role in the pathogenesis of proteinuria in diabetic patients. Diabetes. 2005;54:2172–2178. doi: 10.2337/diabetes.54.7.2172. [DOI] [PubMed] [Google Scholar]
- 38.Williams KJ, Liu ML, Zhu Y, et al. Loss of heparan N-sulfotransferase in diabetic liver: role of angiotensin II. Diabetes. 2005;54:1116–1122. doi: 10.2337/diabetes.54.4.1116. [DOI] [PubMed] [Google Scholar]
- 39.Nakayama K, Natori Y, Sato T, et al. Altered expression of NDST-1 messenger RNA in puromycin aminonucleoside nephrosis. J Lab Clin Med. 2004;143:106–114. doi: 10.1016/j.lab.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 40.van den Hoven MJ, Waanders F, Rops AL, et al. Regulation of glomerular heparanase expression by aldosterone, angiotensin II and reactive oxygen species. Nephrol Dial Transplant. 2009;24:2637–2645. doi: 10.1093/ndt/gfp182. [DOI] [PubMed] [Google Scholar]
- 41.Sachse A, Wolf G. Angiotensin II-induced reactive oxygen species and the kidney. J Am Soc Nephrol. 2007;18:2439–2446. doi: 10.1681/ASN.2007020149. [DOI] [PubMed] [Google Scholar]
- 42.Ceriello A, Assaloni R, Da Ros R, et al. Effect of irbesartan on nitrotyrosine generation in non-hypertensive diabetic patients. Diabetologia. 2004;47:1535–1540. doi: 10.1007/s00125-004-1487-3. [DOI] [PubMed] [Google Scholar]
- 43.Chiarelli F, Di Marzio D, Santilli F, et al. Effects of irbesartan on intracellular antioxidant enzyme expression and activity in adolescents and young adults with early diabetic angiopathy. Diab Care. 2005;28:1690–1697. doi: 10.2337/diacare.28.7.1690. [DOI] [PubMed] [Google Scholar]
- 44.Anjaneyulu M, Chopra K. Effect of irbesartan on the antioxidant defence system and nitric oxide release in diabetic rat kidney. Am J Nephrol. 2004;24:488–496. doi: 10.1159/000080722. [DOI] [PubMed] [Google Scholar]
- 45.van den Berg BM, Spaan JA, Rolf TM, Vink H. Atherogenic region and diet diminish glycocalyx dimension and increase intima-to-media ratios at murine carotid artery bifurcation. Am J Physiol Heart Circ Physiol. 2006;290:H915–H920. doi: 10.1152/ajpheart.00051.2005. [DOI] [PubMed] [Google Scholar]
- 46.Tominaga M, Eguchi H, Manaka H, Igarashi K, Kato T, Sekikawa A. Impaired glucose tolerance is a risk factor for cardiovascular disease, but not impaired fasting glucose. The Funagata Diabetes Study. Diab Care. 1999;22:920–924. doi: 10.2337/diacare.22.6.920. [DOI] [PubMed] [Google Scholar]
- 47.Nieuwdorp M, van Haeften TW, Gouverneur MC, et al. Loss of endothelial glycocalyx during acute hyperglycemia coincides with endothelial dysfunction and coagulation activation in vivo. Diabetes. 2006;55:480–486. doi: 10.2337/diabetes.55.02.06.db05-1103. [DOI] [PubMed] [Google Scholar]
- 48.Henry RM, Ferreira I, Kostense PJ, et al. Type 2 diabetes is associated with impaired endothelium-dependent, flow-mediated dilation, but impaired glucose metabolism is not; The Hoorn Study. Atherosclerosis. 2004;174:49–56. doi: 10.1016/j.atherosclerosis.2004.01.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 8.19 kb)
Glomerular filtration of 40 kDa fluorescein isothiocyanate-labelled dextran in ZL rat (MOV 1396 kb)
Glomerular filtration of 40 kDa fluorescein isothiocyanate-labelled dextran in ZF vehicle-treated rat (MOV 1725 kb)
Glomerular filtration of 40 kDa fluorescein isothiocyanate-labelled dextran in ZF+ARB rat (MOV 693 kb)