Abstract
Background
Although antidepressants and counseling have been shown to be effective in treating patients with depression, non-treatment or under-treatment for depression is common especially among the elderly and minorities. Previous work on patient preferences has focused on medication versus counseling, but less is known about the value patients place on attributes of medication and counseling.
Objective
Conjoint analysis has been recognized as a valuable means of assessing patient treatment preferences. We examine how conjoint analysis be used to determine the relative importance of various attributes of depression treatment at the group level as well as to determine the range of individual-level relative preference weights for specific depression treatment attributes. In addition we use conjoint analysis to predict what modifications in treatment characteristics are associated with a change in the stated preferred alternative.
Study design
86 adults who participated in an internet-based panel responded to an on-line discrete choice task about depression treatment. Participants chose between medication and counseling based on choice sets presented first for a “mild depression” scenario and then for a “severe depression” scenario. Participants were given 18 choice sets which varied for medication based on type of side effect (nausea, dizziness, and sexual dysfunction) and severity of side effect (mild, moderate, and severe); and for counseling based on frequency of counseling sessions (once per week or every other week) and location of the sessions (mental health professional’s office, primary care doctor’s office or office of a spiritual counselor).
Results
Treatment type (counseling vs. medication) appeared to be more important in driving treatment choice than any specific attribute that was studied. Specifically counseling was preferred by most of the respondents. After treatment type, location of treatment and frequency of treatment were important considerations. Preferred attributes were similar in both the mild and severe depression scenarios. Side effect severity appeared to be most important in driving treatment choice as compared with the other attributes studied. Individual-level relative preferences for treatment type revealed a distribution that was roughly bimodal with 27 participants who had a strong preference for counseling and 14 respondents who had a strong preference for medication.
Conclusion
Estimating individual-level preferences for treatment type allowed us to see the variability in preferences and determine which participants had a strong affinity for medication or counseling.
INTRODUCTION
The Institute of Medicine report Crossing the Quality Chasm set forth a vision of a future health care system that is more responsive to the values and preferences of patients.[1] A goal is to customize care based on patient needs and values to meet the most common types of needs and to have the capacity to respond to individual choices and preferences.[2] Despite the importance of patient-centeredness in health care, the National Institute of Mental Health report Bridging Science and Service noted that “little research has been conducted on provider and patient/consumer treatment preferences, how to assess them, or how to incorporate them explicitly into treatment protocols”.[3] The report called for research conducted “in a manner that more closely mirrors individualized patient/consumer monitoring and decision making.” While accommodating patient values into health care constitutes a key component of overarching principles of health care redesign, precisely how to systematically assess and incorporate patient preferences in the clinical setting remains an area with a need for methodological development.
Depression is a condition in which patient preferences and attitudes have a particularly strong influence on acceptance of and adherence to treatment[3–5] , adherence to treatment underline>and patients who receive their preferred method of treatment may have better outcomes.[6] Involving patients in treatment decisions and incorporating preferences might increase uptake of treatment.[7] Clinical decisions regarding depression treatment options require value judgments: possible interventions have different advantages and disadvantages that need to be weighed and these tend to be valued differently from one patient to another.
Despite the significant personal and public health implications of untreated depression, treatment drop-out rates are high among primary care patients with depression.[8] Primary care physicians feel that barriers to depression treatment are most often patient-centered and related to patient attitudes and beliefs about depression and its treatment.[9] For example, some older adults seem to attach high importance to the notion of “pulling yourself up by the bootstraps” or taking personal responsibility for one’s condition in order to get out of depression.[10] Others may be willing to see the doctor’s ability to identify symptoms of depression as helpful to “put it all together” into a diagnosis but may be less likely to accept treatment if the doctor’s viewpoint omits important information about the etiology and feelings of depression grounded in personal experience and social context.[11] Attention to individual preferences for care can have a favorable impact on treatment adherence, clinical outcomes and cost-effectiveness.[12–15] Designing care to be more patient-centered can involve tailoring interventions to match treatment with what patients value most. Nevertheless, understanding who would best benefit from tailored interventions and how patients’ trade-off different features of mental health treatment in decision making has not been well elucidated.
As an initial step towards the development of tailored interventions, we have employed discrete choice conjoint analysis to study decision making around depression treatments. Conjoint analysis was first developed in mathematical psychology[16, 17] and has been frequently used in transport economics[18, 19], environmental economics[20–22], market research[23, 24] and health care[25–27]. Conjoint analysis has been successfully employed to understand patient preferences for great variety of health care issues, such as cataract surgery options[28], hearing aids[29], osteoarthritis treatment options[30], health insurance options[31], patient priority on a surgical wait list[32] and women’s preferences for miscarriage management[33]. In mental health, Flach and coworkers applied conjoint in the design of an alcohol and cigarette cessation program[34] , Shumway and colleagues have used conjoint analysis to assess differences in preferred schizophrenia treatment outcomes between various stakeholders[35] and Dwight-Johnson and colleagues used conjoint analysis to assess the features that low-income Latinos thought would improve acceptability of treatment[36[. While other studies have attempted to assess patient’s stated preferences for types of depression treatment[4, 37], few have taken the approach of understanding what attributes of treatment may be driving these preferences. In this study were particularly interested exploring how the method of conjoint analysis might help with the first steps toward the development of depression treatments that might incorporate the preferred attributes of depression treatment that patients find most important.
Our study focuses on the choice behavior for medication and counseling offered for treatment of depression. Using a web-based convenience sample, we illustrate several features of conjoint analysis in this preliminary investigation: (1) estimating relative preference weights representing trade-offs respondents made for specific features of depression treatment; (2) illustrating the distribution of individual-level relative preference weights representing diversity of strength of preferences for medication or counseling; and (3) exemplifying how our results could be used to address what patients value most in treatment by showing how preference for medicine or counseling would be expected to change based on alternative features of treatments. In contrast to other studies employing conjoint analysis in health applications, we examined the range of individual relative preference weights and how these relate to other important features of treatment that participants discuss. In addition, we show how conjoint can be used to predict what modifications in attributes of treatment are associated with patients switching from desiring medication to counseling. Predicting how patient choice changes as a function of changing attributes of treatment has implications for adaptation of available treatments or to design new treatment packages that improve acceptability and adherence.
METHODS
Recruitment
For this preliminary investigation, a convenience sample was employed. Participants comprise a panel who have participated in studies of judgment and decision-making on the world wide web (http://www.psych.upenn.edu/~baron/q.htm) and responded to a request to complete a questionnaire about depression treatment preferences. [38]. Approximately 1500 panel members have voluntarily participated over the past 10 years in numerous surveys designed to study decision-making processes (for examples, see[38–41]). The panel is roughly representative of the adult U.S. population in terms of income and education but women are overrepresented.[42] For this study, 500 randomly selected members of the panel were sent an e-mail request with a description of the nature of the task and a URL to the discrete choice task, described below. Persons who responded within the first two weeks after the request were participants for this study (n = 86). In this sample 69% were women and the mean age was 41 years. Consistent with past practice, participants received $3 as a token of appreciation for completing the questionnaire. No identifying information was obtained and it is not known to what degree the participants have experience with or knowledge of depression and its treatment.
Conjoint Methods
Typically discrete choice conjoint studies involve several steps. The first step involves identifying the attributes of treatment that are most salient to patients. Next, the conjoint task (described below) is constructed based on the attributes and levels identified. Then, employing the choice data, relative preference weights for each attribute are calculated that indicate the contribution of each attribute to the choice. The resulting model can be used to estimate the change in choice expected as levels of the attributes are changed. We describe each step below.
Identification of attributes and levels
We convened 3 focus groups to elicit the salient attributes of treatments: two focus groups with adults from primary care settings and one focus group with professionals who manage depression (mental health specialists and primary care doctors). Participants were asked to describe their impression of commonly known depression treatments. Patient participants were specifically asked to describe the positive and negative aspects of depression treatments. The professional group was asked to think about features of depression treatments that might act as barriers or facilitators to patient engagement in treatment. Transcripts from the focus groups were analyzed to select the most frequently mentioned depression treatments and attributes (e.g., side effects of medicines, frequency of counseling sessions) to construct the conjoint task.
Choice task
We constructed a conjoint task and presented respondents with choice tasks in which attributes of medications would have to be played off against attributes of counseling in selecting preferred treatment. Discrete choice conjoint analysis simulates selection of services or products in competitive contexts by presenting respondents with a set of products (composed of one level from each attribute) and asking the participant to select which package they prefer. Because medication and counseling share few attributes, we employed an alternative-specific discrete choice design [43] that allowed us to include attributes relevant and specific to medication and counseling (separately) that might be most influential in patient decision making. Prior to each choice set, participants were given definitions for each attribute and level.
Each participant was asked to express their preference for medication or counseling based on choice sets presented first for a “mild depression” scenario and then for a “severe depression” scenario. Consistent with literature on treatment effectiveness, [44] participants were told that counseling and medication were equally effective for the treatment of depression. The text preceding each choice task was as follows: “You complained of feeling more tired than usual and you just aren't interested in doing things that you normally enjoy. Your physician diagnoses mild depression and recommends treatment to help. She gives you two choices for treatment. Select which choice most closely resembles the type of treatment that you would like.” For the second scenario, the text was the same except that the depression was described as “severe depression.”
We selected 18 choice sets with differing attributes of medications and counseling as follows. For medication, there were two attributes: severity of side effects and type of side effect. 9 combinations were possible; namely, 3 levels of severity (mild, moderate, and severe) and 3 types of side effects (nausea, dizziness, and sexual dysfunction); participants were presented with only one type of side effect at a time. For counseling, there were also two attributes: frequency of sessions and location of session. In this case 6 combinations were possible; namely, 2 schedules for frequency of counseling sessions (once per week or every other week) and 3 locations for the sessions (mental health professional’s office, primary care doctor’s office or office of a spiritual counselor). Each choice set required that the respondent choose medication or counseling. With 27 possible combinations for medicines and 6 for counseling, there were 54 possible choice sets. While such a design would allow us to assess interactions between attributes, based on suggested guidelines for the ideal number of discrete choice tasks needed for accurate preference estimation [45] and feedback from participants in an initial pilot phase, we decided such a design would place an undue burden on respondents. The experimental design routines in version 9.1 of SAS were used to select a fractional factorial design of 18 choice sets from the 54 possible sets that allowed us to estimate the main effects of each attribute.[43]
Open ended question
Following the choice tasks, participants were asked “What other features or aspects of depression treatment would be important?” This question was asked in order to obtain information about the reasoning of respondents in making a choice.
Analytic strategy
In preparing discrete choice data for analysis, each response set was represented as two lines of data, one describing medication attributes for that choice set, and one describing counseling attributes for that choice set. An outcome variable was appended to each line that was coded ‘1’ if the respondent made that choice and ‘0’ otherwise.
Our logistic model for calculating individual-level relative preference weights produces a fixed, or overall, effect for each variable, and a random deviation from the overall effect for each respondent. The deviation from the overall effect for each individual is called the random effect because the individual effects are assumed to derive from a random distribution. An emerging standard for analyzing discrete choice data is mixed or random-parameters logic.[46] We use a Bayesian-like approach, called empirical Bayes estimation, because of the advantage of allowing for the estimation of individual-level relative preference weights.[47] The empirical Bayes method has the advantage of borrowing information from the entire sample in estimating the random effect for each person. We obtained an empirical Bayes estimate for the individual random effect and the corresponding standard errors. We used the SAS GLIMMIX macro which operates by calling PROC MIXED iteratively to estimate the effects. For all analyses, we used an α of 0.05 to assess statistical significance, recognizing that statistical tests are guides to interpretation and inference. In addition, we examined respondents’ written comments to the open-ended question that came after the choice scenarios. Two independent researchers coded the comments into main themes. We linked the themes to estimates of strength of preference for medicine or counseling as derived from our statistical model in order to shed light on the thought process reflected in the choice. Finally, we used the conjoint based model to predict the percent of individuals who would choose medication or counseling given different treatment attribute scenarios.
RESULTS
Focus groups
Based on findings from participants in focus groups, we decided to focus on 5 attributes that might be important in making a decision about treatment for depression: (1) type of treatment (medication versus counseling), (2) side effect profile of medication, (3) severity of side effect of medication, (4) number of counseling sessions, and (5) the location of counseling sessions. We assigned levels within each attribute based on how actual treatments differ and on clinical experience (Table 1). While focus group participants did discuss depression treatments other than medication and counseling (such as prayer and talking to friends), medication and counseling were the treatments discussed most frequently by both patient participants and physicians, and medication and counseling were thought to be the most likely to be offered in primary care settings.
Table 1.
Definitions of attributes and levels provided to participants.
| Medication – You take a pill every day for at least 6 months. | |
| Risk of Side Effects (20%) | |
| - | Nausea. You have an upset stomach and feel the urge to vomit. |
| - | Dizziness. If you were to stand up, you might feel unsteady on your feet. |
| - |
Sexual dysfunction. You experience reduced sexual interest or drive. Men might experience difficulty with achieving or maintaining an erection |
| Severity of Side Effect | |
| - |
Mild. You can easily cope with the side effect. The side effect does not interfere with your day to day functioning. |
| - |
Moderate. You find it difficult to cope with the side effect and you may need additional medication to treat it. The side effect interferes with some of your day to day functioning. |
| - |
Severe. You find it very difficult to cope with the side effect and you need additional medication to treat it. The side effect interferes with most or all of your day to day functioning. |
|
Counseling – You schedule appointments to talk with a professional about your life, emotions, and depression and learn new ways to cope with and solve problems. | |
| Number of Counseling Sessions | |
| - | Every week. You attend counseling for 1 hour every week. |
| - | Every 2 weeks. You attend counseling for 1 hour every 2 weeks. |
| Location of Counseling | |
| - |
Primary care doctor’s office. You go to your primary care doctor’s office for your counseling. |
| - |
The office of a mental health professional. You go to the office of a mental health professional for your counseling. |
| - |
Office of a spiritual counselor. You go to the office of a spiritual advisor (priest, pastor, rabbi, imam, etc.) for your counseling. |
Group relative preference weights for treatment of depression in the mild scenario
Here and elsewhere in the paper we use the term “relative preference weights” to describe the numeric value, also known as the “part-worth estimates”, that reflects how desirable different attributes of depression treatment are relative to the other attributes studied. Table 2 provides relative preference weights associated with each attribute of treatment from conjoint analysis in the mild and the severe scenario. Negative relative preference weights are interpreted as less desirable than the omitted category while positive relative preference weights are interpreted as more desirable than the omitted category. In the mild depression scenario (left side of Table 2) mild side effects were relative to other attributes strongly desirable (relative preference weights for “mild” versus “severe” side effect = +5.58, standard deviation (s.d.) = 0.69). Treatment type (medication versus counseling) was associated with the next highest relative preference weights. The negative sign indicates that counseling (the reference category) was preferred over medicine, even accounting for other attributes of treatment (relative preference weights for medicine versus counseling = −2.39, s.d. = 0.11). Respondents preferred location of counseling at the primary care doctor’s office compared to the office of a mental health specialist (relative preference weights for primary care versus specialty mental health = +1.33, s.d. = 0.45). However, the specialty mental health setting was preferred over the office of a spiritual counselor (relative preference weights for office of a spiritual counselor versus specialty mental health = −2.21, s.d. = 0.47). Respondents preferred counseling every 2 weeks over weekly sessions (relative preference weights for counseling once each week versus every 2 weeks = −1.19, s.d. = 0.39). The relative preference weights associated with the nature of the side effect (nausea, dizziness, sexual dysfunction) were small and not statistically significantly different from zero, suggesting that, accounting for other attributes, the nature of the side effect was not strongly associated with choice. Estimates of relative preference weights in the severe depression scenario (right side of Table 2) were similar to relative preference weights in the mild depression scenario.
Table 2.
Group-level relative preference weights for the mild and severe depression scenarios. Negative relative preference weights are interpreted as less desirable than the reference attribute while positive relative preference weights are interpreted as more desirable than the reference attribute.
| Mild-depression scenario | Severe depression scenario | ||||||
|---|---|---|---|---|---|---|---|
| Attribute | Levels | Group- level relative preference weight estimate |
Standard error of the group relative preference weight estimate |
p-value | Group- level relative preference weight estimate |
Standard error of the group relative preference weight estimate |
p-value |
|
Type of treatment |
Medication | −2.39 | 0.11 | < 0.001 | −3.35 | 0.74 | < 0.001 |
| Counseling (reference) |
|||||||
|
Side effect of medication |
Nausea | −0.92 | 0.58 | 0.11 | −0.65 | 0.81 | 0.43 |
| Dizziness | −0.38 | 0.46 | 0.41 | −0.68 | 0.78 | 0.39 | |
| Sexual dysfunction (reference) |
|||||||
|
Severity of medication side effect |
Mild | 5.58 | 0.69 | < 0.001 | 7.98 | 0.96 | < 0.001 |
| Moderate | 0.68 | 0.59 | 0.25 | −0.11 | 0.69 | 0.87 | |
| Severe (reference) |
|||||||
|
Frequency of counseling |
Once each week | −1.19 | 0.39 | 0.003 | −1.32 | 0.59 | 0.01 |
| Every 2 weeks (reference) |
|||||||
|
Location of counseling |
Office of a spiritual counselor |
−2.21 | 0.47 | < 0.001 | −3.04 | 0.72 | < 0.001 |
| Primary care doctor’s office |
1.33 | 0.45 | 0.004 | 1.77 | 0.57 | 0.003 | |
| Mental health professional’s office (reference) |
|||||||
Individual-level relative preference weights
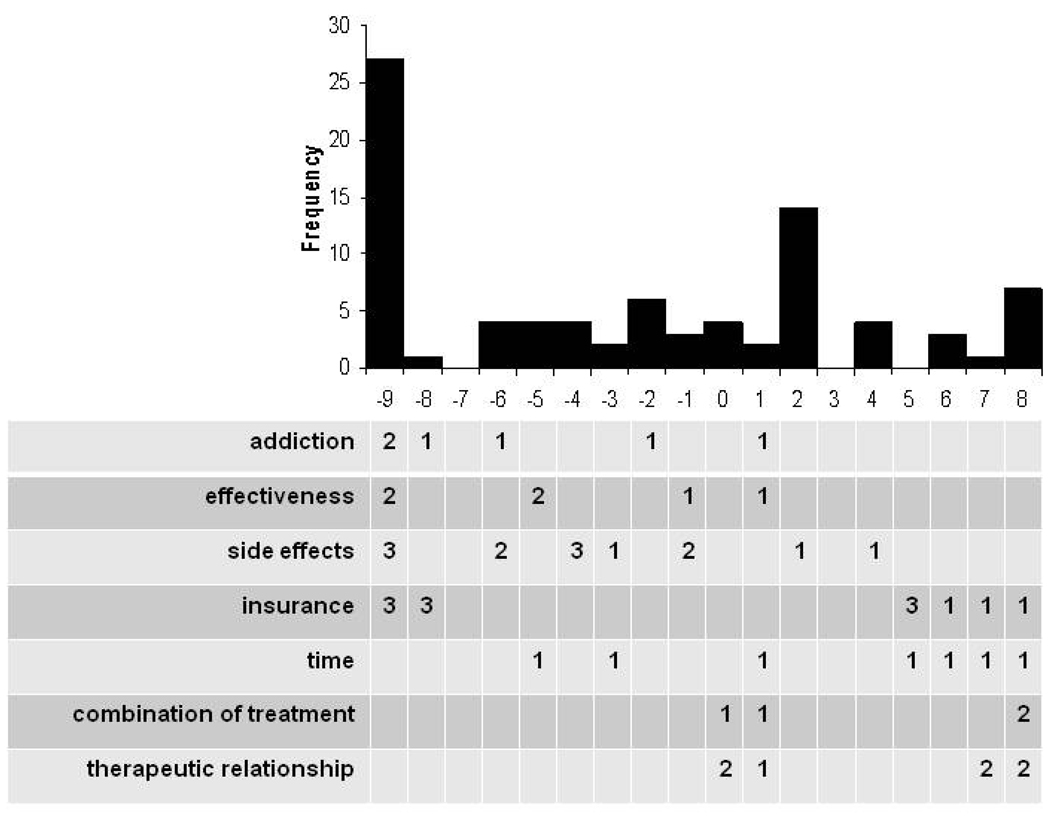
Of interest were the individual-level relative preference weights for the preference for counseling over medication because studying individuals across the entire distribution of preference for counseling over medication may help tailor treatment to persons with strong preferences. Persons at the extreme end of the distribution of individual-level relative preference weights for counseling versus medicines preferred one or the other and were not strongly influenced by other attributes of treatment. We provide the distribution for the individual-level relative preference weights associated with the type of treatment in the Figure. The distribution was roughly bimodal; namely, 27 participants had a strong preference for counseling (27 people had an individual-level relative preference weights for counseling over medicine of −9) with a second mode of 14 participants with a strong preference for medication over counseling (14 participants had an individual-level relative preference weights of 2).
Figure 1.
Individual-level relative preference weights for counseling versus medication linked to comments respondents made after the conjoint task. Distribution of individual-level relative preference weights shown above and the number of persons with a comment under one of seven themes tabulated below. Scores less than zero favor counseling.
Other features of depression treatment respondents thought would be important
We coded responses to the open-ended question into themes. Table 3 lists the main themes and representative comments when participants responded to the question: “What other features of treatment would be important to you?” In all, 47 participants provided a response. Themes fell into 7 categories: (1) concerns about whether treatments might have an addictive quality; (2) the effectiveness of treatment, (3) concerns about side effects of treatment; (4) concerns about insurance coverage and out-of-pocket expenses; (5) the amount of time one would need to devote to issues related to treatments; (6) having the opportunity to combine treatments; and (7) issues related to the therapeutic relationship with the health care provider or counselor. Issues related to treatment side-effects and cost or insurance coverage for treatment were mentioned most frequently.
Table 3.
Themes derived from written comments in response to: “What other features or aspects of depression treatment would be important to you?” after completion of the conjoint task. Letters in the first column are keyed to the figure.
| Theme | Examples of responses | n |
|---|---|---|
| Addiction | “Getting hooked on the medication” | 6 |
| “Addiction to anti-depressants” | ||
| “The fear of dependence” | ||
| Effectiveness | “It also depends very much which method will be more effective.” | 6 |
| “How well the medication works: versus how well counseling works.” | ||
| Side-effects | “Long term effects of medication on other organs (i.e. kidneys, liver, stomach)” |
13 |
| “There are a whole bunch of different anti depressants: and most of them have different side effects” | ||
| “the medication should not leave me more incapacitated than the depression being treated” | ||
| “Counseling can have side effects too.” | ||
| Insurance | “Cost of drugs versus counseling and if insurance covers it.” | 12 |
| “I have awesome prescription coverage, so getting them once a month is easy for me” | ||
| “Affordability: insurance may cover one type of treatment more than another.” | ||
| Time | “Time is always a matter” | 7 |
| “Time: it’s such a hassle to go somewhere far away.” | ||
| “I consider the length of treatment” | ||
|
Combination treatment |
“Possibly a milder medication along with counseling” | 4 |
| “I think that counseling and medication should be combined for the greatest effect.” | ||
|
Therapeutic relationship |
“Reliability of the therapist & trust issues” | 7 |
| “The personality of the doctor: their methods of treatment: beliefs...” | ||
| “Who I would be talking to. Some people I can talk to easier than others” | ||
We lined up the themes from our open-ended question with individual-level relative preference weights for medication versus counseling derived from our model to inspect the concordance between the rationale people gave for their choice and relative preference weights derived from the conjoint analysis (the bottom of the Figure). Participants with a high relative preference weights for medication were more likely to bring up issues related to time, the therapeutic relationship and the possibility of combination treatments. Persons with a strong preference for counseling were more likely to mention medication side effects, addiction and effectiveness. For example, a respondent with an estimated individual-level relative preference weights of −9.0 (negative coefficient indicates a strong preference for counseling over medicine) wrote “I’d want to know how effective the medication was since medication does not solve the problem of why one is depressed and does not teach coping techniques.” Insurance coverage and cost of treatment were raised by persons across the distribution.
Predicting change in choice
To illustrate how the model works to predict change in uptake of specific treatment, we provide both stated choices made by participants along side of model predicted estimates for all possible specific choices related to the side effect of nausea in Table 4. The model prediction of choice was close to the actual proportions stated choices observed, suggesting a good fit of the model (i.e., the relative preference weights) to the data. When participants had to choose between a medication with mild nausea or weekly counseling with a mental health professional, an equal proportion of respondents preferred each option. However, when nausea was described as moderate, the preferred option favored counseling.
Table 4.
Percent of participants who choose medication or counseling in different choice option involving side effect of nausea for mild depression compared with prediction of the conjoint model.
| Medication | Counseling | Actual choice | Prediction of model | |||||
|---|---|---|---|---|---|---|---|---|
| Side Effect |
Severity | Location | Frequency of sessions |
% choosing medication |
% choosing counseling |
% choosing medication |
% choosing counseling |
|
| 1 | nausea | mild | Mental health provider |
Once a week | 50 | 50 | 50 | 50 |
| 2 | nausea | mild | Mental health provider |
Every 2 weeks | 50 | 50 | 46 | 54 |
| 3 | nausea | moderate | Spiritual counselor |
Once a week | 44 | 56 | 46 | 54 |
| 4 | nausea | moderate | Spiritual counselor |
Every 2 weeks | 38 | 62 | 42 | 58 |
| 5 | nausea | severe | Primary care doctor |
Once a week | 17 | 83 | 18 | 82 |
| 6 | nausea | severe | Primary care doctor |
Every 2 weeks | 16 | 84 | 16 | 84 |
DISCUSSION
We used conjoint analysis to study group preferences as well as individual level preferences for depression treatment features. In addition, we were able to learn what might be associated with preferences for the attribute “treatment type” (medicine versus counseling) and predict how the choice of treatment type would change given different treatment options. Using conjoint methods we found that participants preferred counseling over medication, avoided options with severe side effects and wanted to be seen in the primary care doctor’s office as opposed to other venues. With respect to individual level treatment choice, we found a roughly bimodal distribution corresponding to a group of individuals who strongly preferred counseling and another smaller group who strongly preferred medication. In response to an open-ended question about what features of treatment were important (beyond those measured with the task), persons who had a stronger preference for counseling were more likely to bring up concerns about dependence on medication, effectiveness of treatment and issues related to side effects. Individuals who had a stronger preference for medication were more likely to bring up concerns about time and the therapeutic relationship with the provider and were also more likely to wonder about combining medication and counseling. Individuals who preferred counseling and individuals who preferred medication were equally likely to bring up insurance and cost as other important factors to consider when starting a depression treatment. Finally, we used the model to predict how the preferred treatment option changed when treatment attributes were varied and found that as the side effect of nausea changed from mild to moderate to severe, more participants would select counseling. Taken together, the way we used conjoint analysis in this study exemplifies a method for delineating how people make decisions about depression treatment, which individuals have a strong preference for one treatment attribute versus another, and what other treatment-related issues are associated with strong preferences for certain attributes of treatment.
Conjoint analysis allowed us to observe the influence of specific service features on overall choice. The group relative preference weights represent the value respondents associated with particular attributes of treatment. As opposed to simply asking individuals about their preferences for treatment, conjoint analysis can help to uncover what treatment features drive treatment preferences. Isolating what aspects of treatment are desired (and which attributes of treatment are aversive) can help determine ways in which treatments or communication about treatments may need to be adapted to achieve the patient-centered care to which the Quality Chasm report aspires.
In addition to calculating group level relative preference weights, we estimated the individual level relative preference weights for treatment choice. The method we used to calculate individual-level relative preference weights allowed us to examine the distribution of individual relative preference weights to learn about groups of persons within the sample with strong preferences for specific attributes. Specifically, we focused attention on individuals on the ends of the distribution of the relative preference weights associated with preference for counseling or medicine. Ascertaining which individuals have strong preferences for one or the other, linked to treatment, can be a first step in designing patient-centered care. For example, patients who strongly favor having treatment in the primary care doctor’s office might be targeted for a primary care-based intervention while others for whom other features of treatment are compelling, may find other venues acceptable. Further work will determine if individual preferences for treatment attributes are associated with patient characteristics (such as age, gender or comorbid illnesses) as well as whether preferences predict treatment uptake and response.
Our finding that counseling was preferred by most of the participants is consistent with other studies that have looked at preferences for counseling versus medication. [48–50] However, our analyses allowed us to begin to understand more about some of the reasons underlying preference and to predict what might make people switch from desiring counseling to medication, or vice versa. This is especially important for the primary care setting where a patient’s particular treatment preference (such as counseling) may not be readily available, but desired attributes of a treatment (e.g. minimizing side effects) may be feasibly addressed by the physician or through repackaging the way depression treatment is delivered (e.g. counseling in the primary care doctor’s office).
Group relative preference weights did not markedly differ when depression was described as mild or as severe. However, our model allowed us to estimate how proportions of individuals choosing medicine compared to counseling changed as the nausea as a drug side effect was described as mild, moderate, or severe. The proportion of individuals choosing counseling changed most markedly when the side effect was described as severe (proportion choosing counseling increased from 50% for mild nausea from drug to 85% for severe nausea). We asked open-ended questions to obtain information on features of treatment that might be important to respondents that were not included in our conjoint task. We learned that respondents with stronger preferences for counseling had concerns about side-effects and dependency on medication while persons with stronger preferences for medicines cited time and the relationship with the provider as important considerations, and expressed interested in combining treatments.
Before discussing the implications of our study, several limitations deserve comment. First, the participants represented a convenience sample and may react to the hypothetical scenarios very differently than would actual patients. Furthermore, people actually confronting these types of treatment decisions (i.e. patients suffering from depression) might respond very differently to the hypothetical scenarios. Second, with respect to the nature of our conjoint design, side effect severity and type of side effect were only associated with medicine. Had we included attributes related to side effects for counseling we may have seen a different response vis-à-vis the “type of treatment” attribute. In addition, other attributes not included such as cost might have been highly influential. The number and definition of attributes and levels is the critical step in any conjoint analysis task and was based on patient and expert opinion of the most important attributes to include. More work is needed to determine the relative effect of other important attributes on choice tasks.
Conjoint methods sharpen the focus on “what it is about treatment” that drives preferences and provides specific guideposts for how to design packages of treatment that are patient-centered. We plan to study whether there are features of treatment that are desired by depressed patients that could lead to new packages of treatments. Studying how preferences for attributes of treatment are related to treatment adherence, how preferences change over time as depression severity changes and how preferences change with treatment experience are important next steps. In addition, it will be important to look at how the valued attributes of different depression treatments vary among different groups of patients such as persons with co-morbid mental and physical illnesses or the elderly. Conjoint analysis may prove useful in re-thinking how mental health is delivered within primary care. Conjoint analysis has been successfully applied to organizational or service redesign to match with changing consumer needs[51, 52] and is increasingly being considered in medical service redesign.[53–55] For example, conjoint analysis could be used to link patient preferences for specific attributes of both conventional treatments (e.g. medication and/or counseling) and non-conventional depression treatments (such as meditation or spiritual therapy) to observed behavior (initiation and adherence to prescribed treatment). If patients with preferences for specific levels of non-conventional treatment attributes are more likely to be non-adherent to prescribed treatments, then conventional treatments might be adapted to incorporate the desired attributes of non-conventional treatments (e.g. counseling that incorporates aspects of spirituality).
CONCLUSION
Development of more specific treatment approaches based on individual patient’s preferences could lead to a more effective and efficient management of depression. In this paper we outline ways in which conjoint analysis can be used to discover more nuanced information than just what preferences patients have for depression treatment. Conjoint analysis, in combination with other specific patient data, such as demographic variables and health outcomes can help uncover not only how and why patients make depression treatment choices, but what the next steps toward patient-centered approaches may entail.
AKNOWLEDGEMENTS
Dr. Wittink was supported by a NIMH Mentored Patient-Oriented Research Career Development Award (MH19931) and a NIMH sponsored grant entitled “Developing Methods for Tailoring Depression Treatment to Older Adults” (R34 MH085906). The authors gratefully acknowledge the support of the RAND / Hartford Center for Interdisciplinary Health Care Research (PI: Mary Naylor PhD RN FAAN) and Julia Switzer who was supported by a Summer Training on Aging Research Topics - Mental Health (START-MH) Fellowship Program award from the National Institute of Mental Health with Dr. Wittink as the mentor. The authors have no conflicts of interest to declare.
Dr. Wittink also wishes to thank her late father, Dr. Dick R. Wittink, a marketing and econometrics researcher, for introducing her to conjoint analysis.
REFERENCES
- 1.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 2.Committee on Crossing the Quality Chasm. Improving the Quality of Care for Mental and Substance-Use Conditions: Quality Chasm Series. Washington D.C.: National Academies Press; 2006. Adaptation to Mental Health and Addictive Disorders. [Google Scholar]
- 3.Wittink MN, Oslin D, Knott KA, Coyne JC, Zubritsky C. Personal characteristics and depression-related attitudes of older adults and participation in stages of implementation of a multi-site effectiveness trial (PRISM-E) International Journal of Geriatric Psychiatry. 2005;20(10):927–937. doi: 10.1002/gps.1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper LA, Gonzales JJ, Gallo JJ, et al. The acceptability of treatment for depression among African-American and white primary care patients. Medical Care. 2003;41:479–489. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- 5.Glass C, Arnkoff D, Shapiro S. Expectations and preferences. Psychotherapy. 2001;38:455–461. [Google Scholar]
- 6.Swift J, Callahan J. The Impact of Client Treatment Preferences on Outcome: A Meta-Analysis. Journal of Clinical Psychology. 2009;65(4):368–381. doi: 10.1002/jclp.20553. [DOI] [PubMed] [Google Scholar]
- 7.Ryan P, Lauver DR. The efficacy of tailored interventions. Journal of Nursing Scholarship. 2002;34:331–337. doi: 10.1111/j.1547-5069.2002.00331.x. [DOI] [PubMed] [Google Scholar]
- 8.Bogner HR, Lin JY, Morales KH. Patterns of early adherence to the antidepressant citalopram among primary care patients: the PROSPECT study. International Journal of Psychiatry in Medicine. 2006;36(1):103–119. doi: 10.2190/DJH3-Y4R0-R3KG-JYCC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nutting PA, Rost K, Dickinson M, et al. Barriers to initiating depression treatment in primary care practice. Journal of General Internal Medicine. 2002;17:103–111. doi: 10.1046/j.1525-1497.2002.10128.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Switzer J, Wittink M, Karsch BB, Barg FK. "Pull yourself up by your bootstraps": A response to depression in older adults. Qualitative Health Research. 2006;16(9):1207–1216. doi: 10.1177/1049732306290148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wittink MN, Dahlberg B, Biruk C, Barg FK. How older adults combine medical and experiential notions of depression. Qualitative Health Research. 2008 Sep;18(9):1174–1183. doi: 10.1177/1049732308321737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thompson J, Scott N. Counseling service features: Elders' preferences and utilization. Clinical Gerontologist. 1991;(11):39–46. [Google Scholar]
- 13.Dwight-Johnson M, Unützer J, Sherbourne C, Tang L, Wells KB. Can quality improvement programs for depression in primary care address patient preferences for treatment? Medical Care. 2001;39(9):934–944. doi: 10.1097/00005650-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Bedi N, Chilvers C, Churchill R, et al. Assessing effectiveness of treatment of depression in primary care. Partially randomised preference trial. Br J Psychiatry. 2000;177:312–318. doi: 10.1192/bjp.177.4.312. [DOI] [PubMed] [Google Scholar]
- 15.Rokke PD, Tomhave JA, Jocic Z. The role of client choice and target selection in self-management therapy for depression in older adults. Psychol Aging. 1999 Mar;14(1):155–169. doi: 10.1037//0882-7974.14.1.155. [DOI] [PubMed] [Google Scholar]
- 16.Luce D, Tukey J. Simultaneous conjoint measurement: a new type of fundamental measurement. Journal of Mathematical Psychology. 1964;1:1–27. [Google Scholar]
- 17.Anderson N. Functional measurement and psycho-physical judgement. Psychology Review. 1977;77:153–170. doi: 10.1037/h0029064. [DOI] [PubMed] [Google Scholar]
- 18.Louviere JJ. Conjoint Analysis Modelling of Stated Preferences: A Review of Theory, Methods, Recent Developments and External Validity. Journal of Transport Economics and Policy. 1988;22(1):9–119. [Google Scholar]
- 19.Wardman M. A comparison of revealed preference and stated preference models. Journal of Transport Economics and Policy. 1988;22:71–91. [Google Scholar]
- 20.Opaluch J, Swallow S, Weaver T, Wessells C, Wichelns D. Evaluating impacts from noxious facilities: including public preferences in current siting mechanisms. Journal of Environmental Economics and Management. 1993;(24):41–59. [Google Scholar]
- 21.Adamowicz W, Louviere J, Williams M. Combining revealed preference and stated preference methods for valuing environmental amenities. Journal of Environmental Economics and Management. 1994;6:271–292. [Google Scholar]
- 22.Train K, Sonnier G. Mized logit with bounded distributions of correlated partworths. In: Scarpa R, Alberini A, editors. Applications of Simulation Methods in Environmental and Resource Economics. Dordrecht, the Netherlands: Springer; 2005. [Google Scholar]
- 23.Wittink DR, Cattin P. Commercial use of conjoint analysis: An Update. Journal of Marketing. 1981;53:91–96. [Google Scholar]
- 24.Green PE, Srinivasan V. Conjoint Analysis in Marketing: New Developments with Implications for Research and Practice. The Journal of Marketing. 1990;54(4):3–19. [Google Scholar]
- 25.Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. Bmj. 2000 Jun 3;320(7248):1530–1533. doi: 10.1136/bmj.320.7248.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ryan M, Gerard K. Using discrete choice experiements to value health care programmes: current practice and future reflections. Health Economics and Health Policy. 2003;2(1):55–64. [PubMed] [Google Scholar]
- 27.Bridges J, Kinter E, Kidane L, Heinzen R, McCormick C. Things are looking up since we started listening to patients. Trends in the application of conjoint analysis in health 1982–2007. The Patient: Patient Centered Oucomes Research. 2008;1(4):273–282. doi: 10.2165/01312067-200801040-00009. [DOI] [PubMed] [Google Scholar]
- 28.Ross M-A, Avery AJ, Foss AJE. Views of older people on cataract surgery options: an assessment of preferences by conjoint analysis. Quality and Safety in Health Care. 2003;12:13–17. doi: 10.1136/qhc.12.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meister H, Lausberg I, Kiessling J. Identifying the needs of elderly, hearing-impaired persons: the importance and utility of hearing aid attributes. European Archives of Oto-Rhino-Laryngology. 2002;259(10):531–534. doi: 10.1007/s00405-002-0495-5. [DOI] [PubMed] [Google Scholar]
- 30.Ratcliffe J, Buxton M, McGarry T, Sheldon R, Chancellor J. Patients' preferences for characteristics associated with treatments for osteoarthritis. Rheumatology. 2004;43:337–345. doi: 10.1093/rheumatology/keh038. [DOI] [PubMed] [Google Scholar]
- 31.van den Berg B, Van Dommelen P, Stam P, Laske-Aldershof T, Buchmueller T, Schut FT. Preferences and choices for care and health insurance. Soc Sci Med. 2008 Jun;66(12):2448–2459. doi: 10.1016/j.socscimed.2008.02.021. [DOI] [PubMed] [Google Scholar]
- 32.Oudhoff JP, Timmermans DR, Knol DL, Bijnen AB, Van der Wal G. Prioritising patients on surgical waiting lists: a conjoint analysis study on the priority judgments of patients, surgeons, occupational physicians, and general practitioners. Soc Sci Med. 2007 May;64(9):1863–1875. doi: 10.1016/j.socscimed.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 33.Ryan M, Hughes J. Using Conjoint Analysis to Assess Women's Preferences for Miscarriage Management. Health Economics. 1998;6(3):261–273. doi: 10.1002/(sici)1099-1050(199705)6:3<261::aid-hec262>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 34.Flach SD, Diener A. Eliciting patients' preferences for cigarette and alcohol cessation: An application of conjoint analysis. Addictive Behaviors. 2004;29:791–799. doi: 10.1016/j.addbeh.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 35.Shumway M, Saunders T, Shern D, et al. Preferences for Schizophrenia Treatment Outcomes Among Public Policy Makers, Consumers, Families, and Providers. Psychiatric Services. 2003;54:1124–1128. doi: 10.1176/appi.ps.54.8.1124. [DOI] [PubMed] [Google Scholar]
- 36.Dwight-Johnson M, Lagomasino IT, Aisenberg E, Hay J. Using conjoint analysis to assess depression treatment preferences among low-income latinos. Psychiatric Services. 2004;55(8):934–936. doi: 10.1176/appi.ps.55.8.934. [DOI] [PubMed] [Google Scholar]
- 37.Cooper LA, Brown C, Thi Vu H, et al. Primary care patients' opinions regarding the importance of various aspects of care for depression. General Hospital Psychiatry. 2000;22(3):163–173. doi: 10.1016/s0163-8343(00)00073-6. [DOI] [PubMed] [Google Scholar]
- 38.Baron J. Thinking and Deciding. 3 ed. New York: Cambridge University Press; 2000. [Google Scholar]
- 39.Gurmankin AD, Baron J, Hershey JC, Ubel PA. The role of physicians' recommendations in medical treatment decisions. Medical Decision Making. 2002;22:262–271. doi: 10.1177/0272989X0202200314. [DOI] [PubMed] [Google Scholar]
- 40.Gurmankin LA, Baron J. How bad is a 10% chance of losing a toe? Judgments of probabilistic conditions by doctors and laypeople. Memory & Cognition. 2005;33(8):1399–1406. doi: 10.3758/bf03193372. [DOI] [PubMed] [Google Scholar]
- 41.Baron J, Asch DA, Fagerlin A, et al. Effect of assessment method on the discrepancy between judgments of health disorders people have and do not have: a web study. Med Decis Making. 2003 Sep–Oct;23(5):422–434. doi: 10.1177/0272989X03257277. [DOI] [PubMed] [Google Scholar]
- 42.Gurmankin AD, Baron J, Armstrong K. Intended message versus message received in hypothetical physician risk communications: Exploring the gap. Risk Analysis. 2004;24:1337–1347. doi: 10.1111/j.0272-4332.2004.00530.x. [DOI] [PubMed] [Google Scholar]
- 43.Kuhfeld W. Marketing Research Methods for SAS. Experimental Design, Choice, Conjoint, and Graphical Techniques. SAS 9.1 Edition. Cary, NC, USA: SAS Institute Inc; 2005. [Google Scholar]
- 44.Schulberg HC, Katon W, Simon GE, Rush AJ. Treating major depression in primary care: An update of the Agency for Health Care Policy and Research Practice Guidelines. Archives of General Psychiatry. 1998;55:1121–1127. doi: 10.1001/archpsyc.55.12.1121. [DOI] [PubMed] [Google Scholar]
- 45.Johnson R, Orme B. Advanced Research Techniques Forum. Beaver Creek, CO: Sawtooth Software Inc.; 1996. How Many Questions Should You Ask in Choice-Based Conjoint Studies? Sawtooth Software Research Paper Series. [Google Scholar]
- 46.Train K. Discrete choice methods with simulation. Cambridge, England: Cambridge University Press; 2003. [Google Scholar]
- 47.Marshall P, Bradlow ET. A unified approach to conjoint analysis models. Journal of the American Statistical Association. 2002;97:674–682. [Google Scholar]
- 48.Gum A, Areán P, Hunkeler E, et al. Depression treatment preferences in older primary care patients. Gerontologist. 2006;46:14–22. doi: 10.1093/geront/46.1.14. [DOI] [PubMed] [Google Scholar]
- 49.Jaycox L, Asarnow J, Sherbourne C, Rea M, LaBorde A, Wells K. Adolescent Primary Care Patients' Preferences for Depression Treatment. Administration and Policy in Mental Health. 2006;33(2):198–207. doi: 10.1007/s10488-006-0033-7. [DOI] [PubMed] [Google Scholar]
- 50.Givens J. Ethnicity and preferences for depression treatment. General Hospital Psychiatry. 2007;29:254–263. doi: 10.1016/j.genhosppsych.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 51.Wind J, Green P, Shifflet D, Scarbrough M. Courtyard by Marriott: Designing a hotel facility with consumer-based marketing models. Interfaces. 1989 January–February;19:25–47. [Google Scholar]
- 52.Vavra T, Green P, Krieger A. Evaluating EZ-Pass. Marketing Research. 1999;11:5–16. [Google Scholar]
- 53.Chakraborty G, Ettenson R, Gaeth G. How consumers choose health insurance. Journal of Health Care Marketing. 1994;14(1):21–33. [PubMed] [Google Scholar]
- 54.Cunningham CE, Buchanan D, Deal K. Modelling patient-centered children’s health services using choice-based conjoint hierarchical Bayes; Paper presented at: 10th Annual Sawtooth Software Conference Proceedings; San Antonio, TX. 2004. [Google Scholar]
- 55.Cunningham CE, Deal K, Rimas H, et al. Modeling the information preferences of parents of children with mental health problems: A discrete choice conjoint experiment. Journal of Abnormal Psychology. 2008;36(36):1123–1138. doi: 10.1007/s10802-008-9238-4. [DOI] [PubMed] [Google Scholar]