Abstract
OBJECTIVE
Insulin resistance is commonly associated with obesity. Studies conducted in obese mouse models found that endoplasmic reticulum (ER) stress contributes to insulin resistance, and treatment with tauroursodeoxycholic acid (TUDCA), a bile acid derivative that acts as a chemical chaperone to enhance protein folding and ameliorate ER stress, increases insulin sensitivity. The purpose of this study was to determine the effect of TUDCA therapy on multiorgan insulin action and metabolic factors associated with insulin resistance in obese men and women.
RESEARCH DESIGN AND METHODS
Twenty obese subjects ([means ± SD] aged 48 ± 11 years, BMI 37 ± 4 kg/m2) were randomized to 4 weeks of treatment with TUDCA (1,750 mg/day) or placebo. A two-stage hyperinsulinemic-euglycemic clamp procedure in conjunction with stable isotopically labeled tracer infusions and muscle and adipose tissue biopsies were used to evaluate in vivo insulin sensitivity, cellular factors involved in insulin signaling, and cellular markers of ER stress.
RESULTS
Hepatic and muscle insulin sensitivity increased by ∼30% (P < 0.05) after treatment with TUDCA but did not change after placebo therapy. In addition, therapy with TUDCA, but not placebo, increased muscle insulin signaling (phosphorylated insulin receptor substrateTyr and AktSer473 levels) (P < 0.05). Markers of ER stress in muscle or adipose tissue did not change after treatment with either TUDCA or placebo.
CONCLUSIONS
These data demonstrate that TUDCA might be an effective pharmacological approach for treating insulin resistance. Additional studies are needed to evaluate the target cells and mechanisms responsible for this effect.
The ability of insulin to decrease hepatic glucose production, suppress adipose tissue lipolytic rate, and stimulate skeletal muscle glucose uptake is critical for normal metabolic function. Obesity is an important cause of multiorgan insulin resistance (1–3), and insulin sensitivity decreases linearly with increasing BMI (4,5). Insulin resistance has important clinical implications because it is involved in the pathogenesis of many of the metabolic complications associated with obesity. The precise mechanisms responsible for the link between obesity and insulin resistance are not known but likely involve alterations in fatty acid metabolism, excess triglyceride accumulation in the liver and muscle (6–11), and systemic low-grade inflammation (12–14).
Recently, endoplasmic reticulum (ER) stress has been identified as a contributor to insulin resistance associated with obesity in experimental models (15,16). The ER is responsible for the synthesis, folding, and trafficking of secretory and membrane proteins. Disruption of ER homeostasis results in an adaptive unfolded protein response (UPR), which aims to restore ER folding capacity and mitigate stress. ER stress can also inhibit insulin signaling, at least in part, by activating the c-Jun NH2-terminal kinase (JNK) pathway through inositol-requiring enzyme (IRE)-1 (15,17–20) or RNA-dependent protein kinase (PKR)-mediated mechanisms (21). Increased ER stress is associated with impaired insulin action in obese mice (15), and chemical or genetic amelioration of this stress improves insulin sensitivity and glucose homeostasis (18). Increased ER stress in liver and adipose tissue and insulin resistance are also associated with obesity in humans (22,23), whereas weight loss decreases ER stress and improves insulin sensitivity (22).
Tauroursodeoxycholic acid (TUDCA) is a bile acid derivative that has been used in Europe to treat cholelithiasis and cholestatic liver disease. TUDCA can also act as a chemical chaperone to enhance protein folding and protect cells against ER stress (18). In obese mice, parenteral TUDCA treatment reduces ER stress, improves systemic insulin resistance, and decreases intrahepatic triglyceride (IHTG) content (18). Although data from studies conducted in animal models and cell systems demonstrate beneficial metabolic effects, the effect of TUDCA on insulin action has not been studied in human subjects.
The purpose of the present study was to determine whether chemical interventions targeting the ER stress pathway results in metabolic benefits in people. Accordingly, we conducted a randomized controlled trial in insulin-resistant, obese subjects to evaluate the effect of treatment with TUDCA on insulin sensitivity in the liver (glucose production), muscle (glucose uptake), and adipose tissue (lipolysis). We hypothesized that treatment with TUDCA would improve multiorgan insulin signaling and sensitivity and other metabolic factors associated with insulin resistance. The hyperinsulinemic-euglycemic clamp procedure, in conjunction with stable isotopically labeled tracer infusions, was used to determine in vivo insulin sensitivity, and adipose tissue and skeletal muscle biopsies were obtained to assess ER stress markers, phosphorylation of JNK, and components of the insulin-signaling pathway before and after 4 weeks of treatment with TUDCA or placebo.
RESEARCH DESIGN AND METHODS
Twenty obese adults ([means ± SD] 8 men and 12 women, aged 48 ± 11 years, BMI 37 ± 4 kg/m2) participated in this single-blinded, randomized, placebo-controlled trial. All subjects were insulin resistant, defined as a homeostasis model assessment of insulin resistance (HOMA-IR) value of ≥3.0 at the time of screening (24). Subjects completed a comprehensive medical evaluation, including a detailed history, physical examination, blood tests, and a 2-h oral glucose tolerance test. Those who had diabetes, chronic liver disease other than nonalcoholic fatty liver disease (NAFLD), severe hypertriglyceridemia (fasting serum triglyceride concentrations >400 mg/dl), and those who smoked cigarettes or were taking medications known to alter glucose or lipid metabolism were excluded. We purposely studied obese subjects who were insulin resistant but did not have diabetes to provide the best chance for detecting an improvement in insulin sensitivity by TUDCA therapy, without the potential confounding influences of treatment with diabetes medications and differences in glucose control among study subjects. All subjects were sedentary (regular exercise <1 h/week and ≤1 time/week) and weight stable (<2% weight change) for at least 3 months before the study. Subjects provided written informed consent before participating in this study, which was approved by human research protection office of Washington University School of Medicine in St. Louis, Missouri.
Body composition.
Body composition analyses were performed ∼1 week before the hyperinsulinemic-euglycemic clamp procedure was performed. Body fat mass and fat-free mass were determined by using dual-energy X-ray absorptiometry (QDR 4500; Hologic, Waltman, MA). Abdominal subcutaneous adipose tissue and intra-abdominal adipose tissue volumes were determined by using magnetic resonance imaging; the sum of 10 axial images of 1-cm thickness, beginning at the L4–L5 interspace and extending proximally, was used to determine each fat depot volume. Intrahepatic triglyceride content was determined by using magnetic resonance spectroscopy (3T Siemens Magnetom Trio scanner; Siemens, Erlanger, Germany); three 15 × 15 × 15–mm voxels were examined in each subject, and the values were averaged to provide an estimate of the percent of total liver volume comprised of triglycerides (25).
Hyperinsulinemic-euglycemic clamp procedure.
Subjects were admitted to the clinical research unit at Washington University School of Medicine in the afternoon on the day before the clamp procedure. At 1800 h, they consumed a standard meal containing 12 kcal/kg fat-free mass, with 55% of total energy provided as carbohydrates, 30% as fat, and 15% as protein. Subjects then fasted, except for water, until completion of the clamp procedure the next day. At 0500 h the following morning, a catheter was inserted into a forearm vein to infuse stable isotopically labeled tracers (purchased from Cambridge Isotope Laboratories, Andover, MA), dextrose and insulin. A second catheter was inserted into the contralateral radial artery to obtain blood samples. Radial artery cannulation was not successful in four subjects, so a catheter was inserted into a hand vein, which was heated to 55°C by using a thermostatically controlled box to obtain arterialized blood samples (26). At 0600 h, a primed-continuous infusion of [6,6-2H2]glucose (priming dose 22.5 μmol/kg body wt; infusion rate 0.25 μmol/kg body wt/min) was started and maintained for 9.5 h. At 0800 h, a continuous infusion of [2,2-2H2]palmitate (infusion rate 0.035 μmol/kg body wt/min) bound to 25% human albumin was started and maintained for 7.5 h. At 0930 h, 3.5 h after starting the glucose tracer infusion, a two-stage hyperinsulinemic-euglycemic clamp procedure was started and continued for 6 h. During stage 1 of the clamp procedure (3.5–6.5 h), insulin was infused at a rate of 7 mU/m2 body surface area [BSA]/min (initiated with a priming dose of 28 mU/m2 BSA/min for 5 min and then 14 mU/m2 BSA/min for another 5 min) for 3 h. During stage 2 of the clamp procedure (6.5–9.5 h), the rate of insulin infusion was increased to 50 mU/m2 BSA/min (initiated with a priming dose of 200 mU/m2 BSA/min for 5 min and then 100 mU/m2 BSA/min for another 5 min). These insulin infusion rates were chosen to evaluate adipose tissue insulin sensitivity (low-dose insulin infusion to submaximally suppress lipolysis of adipose tissue triglycerides) and skeletal muscle insulin sensitivity (high-dose insulin infusion to stimulate muscle glucose uptake) (27). Euglycemia was maintained at a blood concentration of ∼5.6 mmol/l (100 mg/dl) by infusing 20% dextrose enriched to 2.5% with [6,6-2H2]glucose. The infusion rate of [6,6-2H2]glucose was reduced by 50% of basal during stage 1 and by 75% of basal during stage 2 of the clamp procedure to account for the expected decline in endogenous glucose production. The infusion rate of [2,2-2H2]palmitate was reduced by 50% of basal during stage 1 to account for the expected decline in lipolytic rate.
Blood samples were obtained before the start of the tracer infusions to determine background plasma tracer-to-tracee ratios of glucose and palmitate and every 10 min during the final 30 min of the basal period and stages 1 and 2 of the clamp procedure to determine glucose, free fatty acid (FFA), and insulin concentrations and substrate kinetics. Blood samples were collected in chilled heparinized tubes to determine glucose and insulin concentration. All other blood samples were collected in chilled tubes containing EDTA. Samples were placed on ice, and plasma was separated by centrifugation within 30 min of collection. Plasma samples were stored at −80°C until final analyses were performed.
Subcutaneous abdominal adipose tissue and muscle tissue (vastus lateralis portion of the quadriceps femoris) were obtained during the basal period to determine the expression and regulation of ER stress markers. Additional muscle tissue was obtained at ∼30 min after starting stage 2 of the clamp procedure to determine the levels and the extent of phosphorylation of JNK and elements of the insulin-signaling pathway. The biopsy sites were cleaned and draped, and the skin and underlying tissues were anesthetized with lidocaine. A small (∼0.5 cm) skin incision was made with a scalpel; adipose tissue was aspirated through a 4-mm liposuction cannula, and muscle tissue was obtained by using Tilley-Henkel forceps (Sontec Instruments, Centennial, CO). Muscle and adipose tissue samples were immediately rinsed in ice-cold saline, frozen in liquid nitrogen, and stored at −80°C until final analyses were performed.
Intervention.
After the baseline clamp procedure was completed, each subject was randomized to 4 weeks of oral treatment with either TUDCA (1,750 mg/day) or placebo. Both TUDCA and placebo were kindly provided by Bruschettini S.r.l (Genova, Italy). During the 4-week intervention period, subjects were seen every week to review any study-related issues, reinforce treatment compliance, check body weight, and assess vital signs. After 4 weeks of treatment, the body composition analyses and clamp procedure performed at baseline were repeated. Stage 2 of the clamp procedure was not completed in 2 of 10 subjects who received TUDCA treatment because of technical difficulties in obtaining blood samples. Treatment with drug or placebo was continued until all evaluations were finished.
Sample processing and analyses.
Plasma glucose concentration was determined by using an automated glucose analyzer (YSI 2300 STAT Plus; Yellow Springs Instruments, Yellow Springs, OH). Plasma FFA concentrations were quantified by using gas chromatography (HP 5890 Series II GC; Hewlett-Packard, Palo Alto, CA) (28). Plasma insulin concentration was measured by using a chemiluminescent immunometric assay (Immulite 1000; Diagnostic Products, Los Angeles, CA). Plasma C-reactive protein and interleukin-6 concentrations were measured by using commercially available high-sensitivity immunoassays (R&D Systems, Minneapolis, MN). Total and high–molecular weight adiponectin concentrations were determined by using fast protein liquid chromatography (AKTA FPLC system; GE Healthcare) and fluorescent Western blotting (LI-COR Biotechnology, Lincoln, NE), as previously described (29). Plasma glucose and palmitate tracer-to-tracee ratios were determined by using gas chromatography/mass spectroscopy (MSD 5973 system with capillary column; Hewlett-Packard), as previously described (30).
To determine the activation of the insulin signaling and the JNK pathways in muscle and adipose tissue, we measured the site-specific phosphorylation of insulin receptor substrate (IRS)-1, Akt, and JNK. Tissue samples were cryopulverized, and the powdered tissue transferred to a tube containing cell lysis solution (Cell Signaling, Beverly, MA) and homogenized using a polytron (PowerGen 125; Fisher, Pittsburgh, PA). Homogenates were spun for 15 min at 2000g at 4°C to pellet insoluble material. The total protein concentration in the supernatant was measured (DC Protein Assay; Bio-Rad, Hercules, CA), and 25–50 μg protein were electrophoresed by SDS-PAGE and transferred to nitrocellulose membranes. Blots were probed with polyclonal antibodies directed against total Akt, AktSer473, total JNK, and JNKThr183/Tyr185 (all Cell Signaling, Beverly, MA) in Western analyses. To evaluate IRS-1 tyrosine phosphorylation, blots were concurrently probed with a rabbit polyclonal antibody against IRS-1 (gift of Mike Mueckler, Washington University School of Medicine, St. Louis, MO) and a mouse monoclonal phospho-tyrosine antibody (Cell Signaling, Danvers, MA) and then incubated with secondary antibodies tagged with red (anti-mouse) or green (anti-rabbit) fluorophores. Detection was performed with the LiCor dual-color system (Li-Cor Biosciences, Lincoln, NE). All band intensities were visualized and quantified by using the LiCor system and Odyssey 3.0 software, and phosphorylation levels were expressed as a function of total protein levels.
Real-time quantitative PCR was performed as previously described to determine the mRNA expression of ER stress markers (glucose-regulated protein 78 [Grp78], spliced X-box binding protein-1 [XBP-1], and C/EBP homologous protein [CHOP]) in adipose tissue (22). Frozen adipose tissue samples were homogenized in TRIzol reagent (Invitrogen, Carlsbad, CA), and cDNA synthesis was performed by using 1 μg of sample RNA reverse transcribed with high-capacity cDNA archive system (Applied Biosystems, Foster City, CA); quantitative RT-PCR was performed by using SybrGreen reagent in an ABI 7300 real-time PCR system (Applied Biosystems). The mRNA expression of ER stress markers were normalized to 18S rRNA. The protein expression of homocysteine-induced ER protein (HERP) and the concentrations of eukaryotic elongation initiation factor 2α (eIF2α) phosphorylated at serine 52 and JNK phosphorylated at threonine 183 and tyrosine 185 in adipose tissue were determined by Western analyses using rabbit polyclonal anti–p-eIF2α (Invitrogen) and mouse monoclonal anti–p-JNK (Cell Signaling, Danvers, MA) antibodies as previously described (22). Anti-HERP antibody was a gift from Dr. Yasuhiko Hirabayashi of Tohoku University (Sendai Japan). The band intensities of p-(eIF2α), p-JNK, and HERP were normalized to actin.
Calculations.
Isotopic steady-state conditions were achieved during the final 30 min of the basal period and stages 1 and 2 of the clamp procedure, so the Steele equation for steady-state conditions was used to calculate glucose rate of appearance (Ra), glucose rate of disappearance (Rd), and palmitate Ra (31). The hepatic insulin sensitivity index was determined as the reciprocal of the hepatic insulin resistance index, which was calculated as the product of the basal hepatic glucose production rate (in μmol/min) and basal plasma insulin concentration (in μU/ml) (32). Adipose tissue insulin sensitivity was assessed by calculating the relative decrease from basal in palmitate Ra into plasma during stage 1 of the clamp procedure. Skeletal muscle insulin sensitivity was assessed by calculating the relative increase from basal in glucose Rd from plasma during stage 2 of the clamp procedure. The HOMA-IR score was calculated as the product of fasting plasma insulin (in mU/l) and glucose (in mmol/l) concentrations divided by 22.5 (24).
Statistical analyses.
Statistical analyses were performed by using SPSS for Windows (version 16.0; SPSS, Chicago, IL). Results are reported as means ± SD (normally distributed datasets) or medians and quartiles (skewed datasets). Two-way repeated-measures ANOVA was used to determine whether the changes in outcomes (normally distributed datasets) in response to either TUDCA or placebo treatment were different. Skewed data sets were evaluated by using nonparametric analyses. A P value ≤0.05 was considered statistically significant. Results are reported as means ± SD (normally distributed datasets) or medians and quartiles (skewed datasets).
Based on data on glucose kinetics we obtained in obese subjects previously (33), we estimated that a sample size of 10 participants per group would allow us to detect a 25% difference in insulin sensitivity after treatment between groups, with an α value of 0.05 and power of 80% (β = 0.2). A difference in insulin sensitivity of this magnitude is clinically meaningful because it represents the lower end of the observed effect of current treatment strategies for insulin resistance, such as moderate weight loss (33) or pharmacotherapy (e.g., metformin and thiazolidinediones) (34–41).
RESULTS
Subject characteristics, metabolic variables, and body composition.
Subjects randomized to receive TUDCA and placebo were similar in age, sex, BMI, and body composition (Table 1). Body weight, total body fat, and fat distribution (intra-abdominal fat volume and IHTG content) did not change after 4 weeks of treatment with either TUDCA or placebo (Table 1). Baseline (before treatment) plasma concentrations of glucose, insulin, FFAs, triglycerides, aspartate aminotransferase, alanine aminotransferase, total adiponectin, high–molecular weight adiponectin, and markers of inflammation were not different between groups and did not change after either TUDCA or placebo treatment (Table 1). The HOMA-IR score did not change after placebo treatment but was ∼20% lower after TUDCA treatment (Table 1); however, the decrease in HOMA-IR after TUDCA therapy was not statistically significant.
TABLE 1.
Subjects' characteristics, metabolic variables, and body composition
| Placebo |
TUDCA |
|||
|---|---|---|---|---|
| Before | After | Before | After | |
| n (male/female) | 10 (4/6) | — | 10 (4/6) | — |
| Age (years) | 49 ± 14 | — | 47 ± 9 | — |
| BMI (kg/m2) | 37 ± 5 | 38 ± 5 | 35 ± 3 | 35 ± 3 |
| Total body mass (kg) | 109 ± 18 | 110 ± 17 | 100 ± 12 | 100 ± 12 |
| Fat mass (%) | 39 ± 7 | 39 ± 7 | 39 ± 8 | 39 ± 8 |
| Subcutaneous abdominal fat volume (cm3) | 5,087 ± 1,749 | 4,999 ± 1,672 | 4,803 ± 1,202 | 4,716 ± 1,188 |
| Intra-abdominal fat volume (cm3) | 2,146 ± 789 | 2,172 ± 716 | 2,724 ± 846 | 2,818 ± 924 |
| IHTG content (%) | 14.0 ± 10.7 | 13.7 ± 9.6 | 8.2 ± 5.5 | 9.3 ± 7.2 |
| HOMA-IR | 4.2 ± 1.8 | 4.3 ± 1.7 | 4.4 ± 2.7 | 3.8 ± 3.4 |
| Plasma concentrations | ||||
| Glucose (mg/dl) | 97 ± 9 | 97 ± 10 | 96 ± 9 | 94 ± 5 |
| Insulin (μU/ml) | 18 ± 7 | 18 ± 7 | 19 ± 12 | 16 ± 15 |
| FFAs (mmol/l) | 0.59 ± 0.13 | 0.63 ± 0.15 | 0.62 ± 0.15 | 0.62 ± 0.19 |
| Triglycerides (mg/dl) | 154 ± 52 | 145 ± 77 | 136 ± 67 | 141 ± 66 |
| AST (IU/l) | 25.9 ± 10.3 | 27.9 ± 14.5 | 22.4 ± 5.9 | 22.5 ± 6.1 |
| ALT (IU/l) | 30.3 ± 24.7 | 35.6 ± 34.9 | 26.9 ± 9.6 | 24.6 ± 8.1 |
| CRP (mg/l) | 5.67 ± 5.69 | 5.00 ± 3.87 | 5.40 ± 4.11 | 4.43 ± 2.94 |
| IL-6 (pg/ml) | 2.60 ± 0.95 | 2.44 ± 0.86 | 2.32 ± 0.65 | 2.60 ± 1.17 |
| Total adiponectin (mg/l) | 6.7 ± 3.8 | 6.9 ± 4.6 | 8.3 ± 3.1 | 8.3 ± 3.1 |
| HMW adiponectin (mg/l) | 2.2 ± 2.6 | 2.2 ± 2.9 | 3.1 ± 1.9 | 3.4 ± 2.4 |
Data are means ± SD. ALT, alanine aminotransferase; AST, aspartate aminotransferase; CRP, C-reactive protein; HMW, high molecular weight; IL, interleukin.
Insulin sensitivity assessed by using the hyperinsulinemic-euglycemic clamp technique.
During the hyperinsulinemic-euglycemic clamp procedure, euglycemia was maintained at ∼100 mg/dl in all subjects (average plasma glucose concentration: 100.0 ± 2.1 mg/dl during stage 1 and 102.0 ± 2.7 mg/dl during stage 2 of the clamp procedure) and plasma insulin concentration increased to 29 ± 17 μU/ml during stage 1 and to 81 ± 19 μU/ml during stage 2.
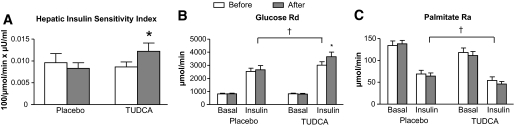
The hepatic insulin sensitivity index increased by ∼30% after TUDCA treatment but was not affected by placebo therapy (Fig. 1A). Glucose Rd increased by ∼150% (P < 0.001) from basal values during stage 2 of the clamp procedure in both the TUDCA and placebo groups before treatment. Compared with baseline (pretreatment) values, the increase in glucose Rd above basal values during stage 2 was 34 ± 23% greater after treatment with TUDCA (P < 0.05) but did not change after treatment with placebo (Fig. 1B). Insulin infusion suppressed palmitate Ra by ∼50% in both TUDCA and placebo groups before treatment, and this remained the same after treatment with either TUDCA or placebo (Fig. 1C).
FIG. 1.
Liver, muscle, and adipose tissue insulin sensitivity before (□) and after ( ) 4 weeks of placebo or TUDCA treatment. A: Hepatic insulin sensitivity index. B: Glucose rate of disappearance (Rd); data represent only 8 of 10 subjects who received TUDCA treatment because of technical difficulties in obtaining blood samples in two subjects. C: Palmitate rate of appearance. Values are means ± SD. *Value significantly different from corresponding value before treatment, P < 0.05. †Main effect of insulin, P < 0.0001.
) 4 weeks of placebo or TUDCA treatment. A: Hepatic insulin sensitivity index. B: Glucose rate of disappearance (Rd); data represent only 8 of 10 subjects who received TUDCA treatment because of technical difficulties in obtaining blood samples in two subjects. C: Palmitate rate of appearance. Values are means ± SD. *Value significantly different from corresponding value before treatment, P < 0.05. †Main effect of insulin, P < 0.0001.
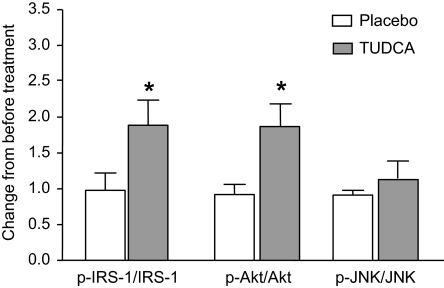
Consistent with our kinetic data, TUDCA therapy increased insulin signaling in muscle but not adipose tissue. Compared with placebo treatment, TUDCA treatment increased insulin-stimulated phosphorylation of IRSTyr and AktSer473 in muscle (both P < 0.05) (Fig. 2). In contrast, TUDCA therapy did not alter insulin-stimulated phosphorylation of IRSTyr and AktSer473 in adipose tissue (data not shown). No difference in skeletal muscle phosphorylation of JNKThr183/Tyr185 was detected between subjects treated with placebo or TUDCA (Fig. 2).
FIG. 2.
Effect of placebo (□) or TUDCA ( ) treatment on skeletal muscle IRSTyr, AktSer473, and JNKThr183/Tyr185 levels. Values are means ± SD and expressed relative to values before treatment, which were set to one for each person. *Value significantly different from corresponding placebo value, P < 0.05.
) treatment on skeletal muscle IRSTyr, AktSer473, and JNKThr183/Tyr185 levels. Values are means ± SD and expressed relative to values before treatment, which were set to one for each person. *Value significantly different from corresponding placebo value, P < 0.05.
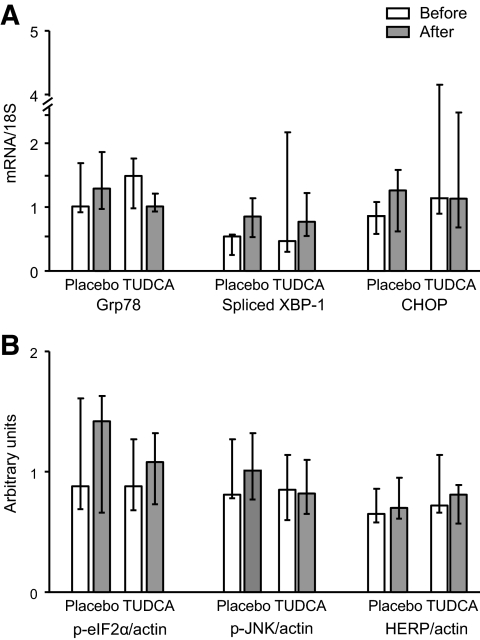
ER stress markers in muscle and adipose tissue.
Adipose tissue mRNA expression of spliced XBP-1, Grp78, and CHOP (Fig. 3A) and protein levels of HERP, eIF2αSer52, and JNKThr183/Tyr185 (Fig. 3B) were not affected by either placebo or TUDCA treatment. Spliced XBP-1, Grp78, and CHOP mRNA expression in skeletal muscle were very low (below the limit of reliable detection for spliced XBP-1) and did not change after TUDCA treatment (data not shown).
FIG. 3.
Endoplasmic reticulum stress markers before (□) and after ( ) placebo or TUDCA therapy. A: Gene expression (relative to 18S rRNA). B: Protein content (relative to actin). Values are medians and quartiles.
) placebo or TUDCA therapy. A: Gene expression (relative to 18S rRNA). B: Protein content (relative to actin). Values are medians and quartiles.
DISCUSSION
Data from recent studies (15,18,22,23) conducted in both rodent models and human subjects have demonstrated that obesity is associated with liver and adipose tissue but not muscle ER stress. Treating obese mice with TUDCA, which acts as a chemical chaperone that reduces ER stress in liver and adipose tissue, results in improved insulin sensitivity in liver, muscle, and adipose tissue (18). However, the use of agents that can decrease ER stress to treat obesity-associated insulin resistance has not been evaluated in people. Accordingly, we conducted a randomized controlled trial to determine the effect of 4 weeks of treatment with TUDCA on multiorgan insulin sensitivity and factors involved in regulating insulin action in obese subjects with insulin resistance. Our data demonstrate that TUDCA therapy increases hepatic and muscle insulin action in vivo with a concomitant increase in the phosphorylation of components of the muscle insulin-signaling pathway. Moreover, the magnitude of the improvement in hepatic and muscle insulin sensitivity (both ∼30%) is similar to the insulin-sensitizing effects of currently available diabetes medications, such as thiazolinediones and metformin (35–41). However, we did not detect an effect of TUDCA on adipose tissue insulin sensitivity or ER stress, making it unlikely that a reduction in adipocyte ER stress was responsible for the effect on insulin action in this trial. These data suggest that TUDCA therapy might provide a novel pharmacological approach for improving glucose homeostasis in insulin-resistant obese people.
The precise cellular mechanisms responsible for the improvement in hepatic insulin sensitivity after TUDCA therapy are not clear. Data from studies conducted in human hepatocyte cultures have shown that TUDCA activates Akt and its downstream targets via a G-protein–coupled receptor–dependent mechanism (42,43). In addition, activation of the nuclear farnesoid X receptor (FXR) by bile acids or FXR agonists improves insulin sensitivity in vitro in cell systems and in vivo in animal models (44,45). However, TUDCA, unlike some other bile acids, is a relatively poor substrate for FXR (46). In animal models and cultured liver cells, TUDCA treatment can suppress ER stress and increase insulin signaling (18). Therefore, it is possible that TUDCA therapy affected hepatic ER stress in our subjects, but we did not obtain liver tissue in our subjects to directly evaluate this possibility.
The mechanisms responsible for the TUDCA-induced improvement in skeletal muscle insulin sensitivity and insulin signaling in our subjects and in the previous study (18) conducted in mice are also not clear. In contrast with adipose tissue and liver, ER stress indicators are not increased in skeletal muscle from obese mice (15,18) or obese people (23), and TUDCA treatment did not affect muscle ER stress markers in our study. In addition, muscle does not express the FXR (46), which precludes the possibility of an FXR-mediated improvement in muscle insulin action. However, G-protein receptors are expressed ubiquitously, so some of the effects of TUDCA in muscle might be mediated by G-protein receptor activation of Akt.
Although we found that TUDCA therapy improved hepatic and muscle insulin sensitivity, we did not find a significant effect of TUDCA therapy on HOMA-IR and many of the metabolic variables associated with insulin resistance, such as plasma glucose, insulin, and FFA concentrations. It is likely that these measures were not adequate to detect an effect of TUDCA, which required a more sensitive assessment of insulin action by using stable isotopically labeled tracers and the hyperinsulinenmic-euglycemic clamp procedure.
Unlike data obtained from mouse models (18), we did not detect an effect of TUDCA therapy on adipose tissue insulin sensitivity or signaling or the expression of adipose tissue ER stress markers. Several factors might be responsible for the apparent difference observed after TUDCA therapy in mice and our study in human subjects. First, it is possible that the amount of TUDCA we gave our subjects, which is the maximum dose used to treat biliary disease, was insufficient to generate changes in adipose tissue ER stress; in the previous study, ∼30 times more TUDCA relative to body weight was given to mice than to our subjects. Second, TUDCA was given intraperitoneally in the mice but orally to our subjects. It is likely this difference in route of administration further limited the systemic availability of TUDCA in our subjects, because TUDCA is effectively metabolized by the liver and there is minimal splanchnic escape of bile acid conjugates into the systemic circulation (47). Finally, the expression of transporters responsible for TUDCA tissue uptake is very low in most extrahepatic tissues (48,49), so large plasma concentrations might be needed to achieve adequate tissue uptake to affect intracellular function. These pharmacokinetic factors raise the possibility that adipose tissue did not get sufficient exposure to orally administered TUDCA to affect ER stress in our subjects. Future studies with different dosing regimens are needed to address this issue.
In summary, insulin resistance is involved in the pathogenesis of the key metabolic disorders associated with obesity (1–3,6–14). The results from the present study demonstrate that TUDCA therapy increases liver and muscle insulin sensitivity in obese, insulin-resistant subjects. Additional studies are needed to determine the specific cellular mechanisms responsible for this effect and to determine the therapeutic potential of this class of compounds for obese people with insulin resistance.
ACKNOWLEDGMENTS
This study was supported by National Institutes of Health Grants DK 37948, DK52539, DK 56341 (Nutrition Obesity Research Center), RR 00954 (Biomedical Mass Spectrometry Resource), UL1 RR024992 (Institute for Clinical and Translational Science), and T32 ES007155-24 (Environmental Health Training grant). This study also received support from the Nutricia Research Foundation (2009-26), Syndexa Pharmaceuticals, a mentor-based postdoctoral fellowship from the American Diabetes Association, and a Donald and Sue Pritzker Scholar award.
G.S.H. is a shareholder and member of the scientific advisory board at Syndexa Pharmaceuticals. No other potential conflicts of interest relevant to this article were reported.
M.K., B.M., G.S.H., and S.K. were involved in designing and conducting the infusion studies, processing the study samples, collecting data, performing the final data analyses, and writing the manuscript. B.S.M. was involved in conducting the infusion studies. M.F.G., L.Y., T.A.P., B.N.F., B.W.P., and J.D.H. were involved in sample processing and sample analyses.
The authors thank Adewole Okunade, Freida Custodio, and Jennifer Shew for their technical assistance, Ken Schechtman for assistance with statistical analyses, Melisa Moore and the staff of the Clinical Research Unit for their help in performing the studies, and the study subjects for their participation.
Footnotes
Clinical Trials reg. no. NCT00771901, clinicaltrials.gov.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, Natale S, Vanni E, Villanova N, Melchionda N, Rizzetto M: Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 2003;37:917–923 [DOI] [PubMed] [Google Scholar]
- 2.Ioannou GN, Weiss NS, Boyko EJ, Mozaffarian D, Lee SP: Elevated serum alanine aminotransferase activity and calculated risk of coronary heart disease in the United States. Hepatology 2006;43:1145–1151 [DOI] [PubMed] [Google Scholar]
- 3.Adams LA, Lymp JF, St. Sauver J, Sanderson SO, Lindor KD, Feldstein A, Angulo P: The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology 2005;129:113–121 [DOI] [PubMed] [Google Scholar]
- 4.Ferrannini E, Natali A, Bell P, Cavallo-Perin P, Lalic N, Mingrone G: Insulin resistance and hypersecretion in obesity: European Group for the Study of Insulin Resistance (EGIR). J Clin Invest 1997;100:1166–1173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Esteghamati A, Khalilzadeh O, Anvari M, Ahadi MS, Abbasi M, Rashidi A: Metabolic syndrome and insulin resistance significantly correlate with body mass index. Arch Med Res 2008;39:803–808 [DOI] [PubMed] [Google Scholar]
- 6.Neschen S, Morino K, Hammond LE, Zhang D, Liu ZX, Romanelli AJ, Cline GW, Pongratz RL, Zhang XM, Choi CS, Coleman RA, Shulman GI: Prevention of hepatic steatosis and hepatic insulin resistance in mitochondrial acyl-CoA:glycerol-sn-3-phosphate acyltransferase 1 knockout mice. Cell Metab 2005;2:55–65 [DOI] [PubMed] [Google Scholar]
- 7.Savage DB, Choi CS, Samuel VT, Liu ZX, Zhang D, Wang A, Zhang XM, Cline GW, Yu XX, Geisler JG, Bhanot S, Monia BP, Shulman GI: Reversal of diet-induced hepatic steatosis and hepatic insulin resistance by antisense oligonucleotide inhibitors of acetyl-CoA carboxylases 1 and 2. J Clin Invest 2006;116:817–824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Korenblat KM, Fabbrini E, Mohammed BS, Klein S: Liver, muscle, and adipose tissue insulin action is directly related to intrahepatic triglyceride content in obese subjects. Gastroenterology 2008;134:1369–1375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deivanayagam S, Mohammed BS, Vitola BE, Naguib GH, Keshen TH, Kirk EP, Klein S: Nonalcoholic fatty liver disease is associated with hepatic and skeletal muscle insulin resistance in overweight adolescents. Am J Clin Nutr 2008;88:257–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gastaldelli A, Kozakova M, Hojlund K, Flyvbjerg A, Favuzzi A, Mitrakou A, Balkau B: Fatty liver is associated with insulin resistance, risk of coronary heart disease, and early atherosclerosis in a large European population. Hepatology 2009;49:1537–1544 [DOI] [PubMed] [Google Scholar]
- 11.Seppala-Lindroos A, Vehkavaara S, Hakkinen AM, Goto T, Westerbacka J, Sovijarvi A, Halavaara J, Yki-Jarvinen H: Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men. J Clin Endocrinol Metab 2002;87:3023–3028 [DOI] [PubMed] [Google Scholar]
- 12.Hotamisligil GS: Inflammation and metabolic disorders. Nature 2006;444:860–867 [DOI] [PubMed] [Google Scholar]
- 13.Cai D, Yuan M, Frantz DF, Melendez PA, Hansen L, Lee J, Shoelson SE: Local and systemic insulin resistance resulting from hepatic activation of IKK-beta and NF-kappaB. Nat Med 2005;11:183–190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shoelson SE, Herrero L, Naaz A: Obesity, inflammation, and insulin resistance. Gastroenterology 2007;132:2169–2180 [DOI] [PubMed] [Google Scholar]
- 15.Ozcan U, Cao Q, Yilmaz E, Lee AH, Iwakoshi NN, Ozdelen E, Tuncman G, Gorgun C, Glimcher LH, Hotamisligil GS: Endoplasmic reticulum stress links obesity, insulin action, and type 2 diabetes. Science 2004;306:457–461 [DOI] [PubMed] [Google Scholar]
- 16.Gregor MF, Hotamisligil GS: Thematic review series: adipocyte biology. Adipocyte stress: the endoplasmic reticulum and metabolic disease. J Lipid Res 2007;48:1905–1914 [DOI] [PubMed] [Google Scholar]
- 17.Hirosumi J, Tuncman G, Chang L, Gorgun CZ, Uysal KT, Maeda K, Karin M, Hotamisligil GS: A central role for JNK in obesity and insulin resistance. Nature 2002;420:333–336 [DOI] [PubMed] [Google Scholar]
- 18.Ozcan U, Yilmaz E, Ozcan L, Furuhashi M, Vaillancourt E, Smith RO, Gorgun CZ, Hotamisligil GS: Chemical chaperones reduce ER stress and restore glucose homeostasis in a mouse model of type 2 diabetes. Science 2006;313:1137–1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aguirre V, Uchida T, Yenush L, Davis R, White MF: The c-Jun NH(2)-terminal kinase promotes insulin resistance during association with insulin receptor substrate-1 and phosphorylation of Ser(307). J Biol Chem 2000;275:9047–9054 [DOI] [PubMed] [Google Scholar]
- 20.Urano F, Wang X, Bertolotti A, Zhang Y, Chung P, Harding HP, Ron D: Coupling of stress in the ER to activation of JNK protein kinases by transmembrane protein kinase IRE1. Science 2000;287:664–666 [DOI] [PubMed] [Google Scholar]
- 21.Nakamura T, Furuhashi M, Li P, Cao H, Tuncman G, Sonenberg N, Gorgun CZ, Hotamisligil GS: Double-stranded RNA-dependent protein kinase links pathogen sensing with stress and metabolic homeostasis. Cell 2010;140:338–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gregor MF, Yang L, Fabbrini E, Mohammed BS, Eagon JC, Hotamisligil GS, Klein S: Endoplasmic reticulum stress is reduced in tissues of obese subjects after weight loss. Diabetes 2009;58:693–700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma NK, Das SK, Mondal AK, Hackney OG, Chu WS, Kern PA, Rasouli N, Spencer HJ, Yao-Borengasser A, Elbein SC: Endoplasmic reticulum stress markers are associated with obesity in nondiabetic subjects. J Clin Endocrinol Metab 2008;93:4532–4541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC: Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–419 [DOI] [PubMed] [Google Scholar]
- 25.Frimel TN, Deivanayagam S, Bashir A, O'Connor R, Klein S: Assessment of intrahepatic triglyceride content using magnetic resonance spectroscopy. J Cardiometab Syndr 2007;2:136–138 [DOI] [PubMed] [Google Scholar]
- 26.Jensen MD, Heiling VJ: Heated hand vein blood is satisfactory for measurements during free fatty acid kinetic studies. Metabolism 1991;40:406–409 [DOI] [PubMed] [Google Scholar]
- 27.Groop LC, Bonadonna RC, DelPrato S, Ratheiser K, Zyck K, Ferrannini E, DeFronzo RA: Glucose and free fatty acid metabolism in non-insulin-dependent diabetes mellitus: evidence for multiple sites of insulin resistance. J Clin Invest 1989;84:205–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patterson BW, Zhao G, Klein S: Improved accuracy and precision of gas chromatography/mass spectrometry measurements for metabolic tracers. Metabolism 1998;47:706–712 [DOI] [PubMed] [Google Scholar]
- 29.Schraw T, Wang ZV, Halberg N, Hawkins M, Scherer PE: Plasma adiponectin complexes have distinct biochemical characteristics. Endocrinology 2008;149:2270–2282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patterson BW, Zhao G, Elias N, Hachey DL, Klein S: Validation of a new procedure to determine plasma fatty acid concentration and isotopic enrichment. J Lipid Res 1999;40:2118–2124 [PubMed] [Google Scholar]
- 31.Steele R: Influences of glucose loading and of injected insulin on hepatic glucose output. Ann N Y Acad Sci 1959;82:420–430 [DOI] [PubMed] [Google Scholar]
- 32.Matsuda M, DeFronzo RA: Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 1999;22:1462–1470 [DOI] [PubMed] [Google Scholar]
- 33.Kirk E, Reeds DN, Finck BN, Mayurranjan SM, Patterson BW, Klein S: Dietary fat and carbohydrates differentially alter insulin sensitivity during caloric restriction. Gastroenterology 2009;136:1552–1560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schrauwen-Hinderling VB, Mensink M, Hesselink MK, Sels JP, Kooi ME, Schrauwen P: The insulin-sensitizing effect of rosiglitazone in type 2 diabetes mellitus patients does not require improved in vivo muscle mitochondrial function. J Clin Endocrinol Metab 2008;93:2917–2921 [DOI] [PubMed] [Google Scholar]
- 35.Nolan JJ, Ludvik B, Beerdsen P, Joyce M, Olefsky J: Improvement in glucose tolerance and insulin resistance in obese subjects treated with troglitazone. N Engl J Med 1994;331:1188–1193 [DOI] [PubMed] [Google Scholar]
- 36.Frias JP, Yu JG, Kruszynska YT, Olefsky JM: Metabolic effects of troglitazone therapy in type 2 diabetic, obese, and lean normal subjects. Diabetes Care 2000;23:64–69 [DOI] [PubMed] [Google Scholar]
- 37.Kruszynska YT, Yu JG, Olefsky JM, Sobel BE: Effects of troglitazone on blood concentrations of plasminogen activator inhibitor 1 in patients with type 2 diabetes and in lean and obese normal subjects. Diabetes 2000;49:633–639 [DOI] [PubMed] [Google Scholar]
- 38.Yu JG, Javorschi S, Hevener AL, Kruszynska YT, Norman RA, Sinha M, Olefsky JM: The effect of thiazolidinediones on plasma adiponectin levels in normal, obese, and type 2 diabetic subjects. Diabetes 2002;51:2968–2974 [DOI] [PubMed] [Google Scholar]
- 39.Shadid S, Jensen MD: Pioglitazone increases non-esterified fatty acid clearance in upper body obesity. Diabetologia 2006;49:149–157 [DOI] [PubMed] [Google Scholar]
- 40.Giugliano D, De Rosa N, Di Maro G, Marfella R, Acampora R, Buoninconti R, D'Onofrio F: Metformin improves glucose, lipid metabolism, and reduces blood pressure in hypertensive, obese women. Diabetes Care 1993;16:1387–1390 [DOI] [PubMed] [Google Scholar]
- 41.Mannucci E, Ognibene A, Cremasco F, Bardini G, Mencucci A, Pierazzuoli E, Ciani S, Messeri G, Rotella CM: Effect of metformin on glucagon-like peptide 1 (GLP-1) and leptin levels in obese nondiabetic subjects. Diabetes Care 2001;24:489–494 [DOI] [PubMed] [Google Scholar]
- 42.Dent P, Fang Y, Gupta S, Studer E, Mitchell C, Spiegel S, Hylemon PB: Conjugated bile acids promote ERK1/2 and AKT activation via a pertussis toxin-sensitive mechanism in murine and human hepatocytes. Hepatology 2005;42:1291–1299 [DOI] [PubMed] [Google Scholar]
- 43.Fang Y, Studer E, Mitchell C, Grant S, Pandak WM, Hylemon PB, Dent P: Conjugated bile acids regulate hepatocyte glycogen synthase activity in vitro and in vivo via Galphai signaling. Mol Pharmacol 2007;71:1122–1128 [DOI] [PubMed] [Google Scholar]
- 44.Cariou B, van Harmelen K, Duran-Sandoval D, van Dijk TH, Grefhorst A, Abdelkarim M, Caron S, Torpier G, Fruchart JC, Gonzalez FJ, Kuipers F, Staels B: The farnesoid X receptor modulates adiposity and peripheral insulin sensitivity in mice. J Biol Chem 2006;281:11039–11049 [DOI] [PubMed] [Google Scholar]
- 45.Cipriani S, Mencarelli A, Palladino G, Fiorucci S: FXR activation reverses insulin resistance and lipid abnormalities and protects against liver steatosis in Zucker (fa/fa) obese rats. J Lipid Res 2010;51:771–784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nguyen A, Bouscarel B: Bile acids and signal transduction: role in glucose homeostasis. Cell Signal 2008;20:2180–2197 [DOI] [PubMed] [Google Scholar]
- 47.Hylemon PB, Zhou H, Pandak WM, Ren S, Gil G, Dent P: Bile acids as regulatory molecules. J Lipid Res 2009;50:1509–1520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bouscarel B, Ceryak S, Gettys TW, Fromm H, Noonan F: Alteration of cAMP-mediated hormonal responsiveness by bile acids in cells of nonhepatic origin. Am J Physiol 1995;268:G908–G916 [DOI] [PubMed] [Google Scholar]
- 49.Li N, Hartley DP, Cherrington NJ, Klaassen CD: Tissue expression, ontogeny, and inducibility of rat organic anion transporting polypeptide 4. J Pharmacol Exp Ther 2002;301:551–560 [DOI] [PubMed] [Google Scholar]