Abstract
OBJECTIVE
Defects in insulin/IGF-1 signaling stimulate muscle protein loss by suppressing protein synthesis and increasing protein degradation. Since an herbal compound, berberine, lowers blood levels of glucose and lipids, we proposed that it would improve insulin/IGF-1 signaling, blocking muscle protein losses.
RESEARCH DESIGN AND METHODS
We evaluated whether berberine ameliorates muscle atrophy in db/db mice, a model of type 2 diabetes, by measuring protein synthesis and degradation in muscles of normal and db/db mice treated with or without berberine. We also examined mechanisms for berberine-induced changes in muscle protein metabolism.
RESULTS
Berberine administration decreased protein synthesis and increased degradation in muscles of normal and db/db mice. The protein catabolic mechanism depended on berberine-stimulated expression of the E3 ubiquitin ligase, atrogin-1. Atrogin-1 not only increased proteolysis but also reduced protein synthesis by mechanisms that were independent of decreased phosphorylation of Akt or forkhead transcription factors. Impaired protein synthesis was dependent on a reduction in eIF3-f, an essential regulator of protein synthesis. Berberine impaired energy metabolism, activating AMP-activated protein kinase and providing an alternative mechanism for the stimulation of atrogin-1 expression. When we increased mitochondrial biogenesis by expressing peroxisome proliferator–activated receptor γ coactivator-1α, berberine-induced changes in muscle protein metabolism were prevented.
CONCLUSIONS
Berberine impairs muscle metabolism by two novel mechanisms. It impairs mitochonidrial function stimulating the expression of atrogin-1 without affecting phosphorylation of forkhead transcription factors. The increase in atrogin-1 not only stimulated protein degradation but also suppressed protein synthesis, causing muscle atrophy.
There is evidence that an herbal compound, berberine, improves insulin-mediated glucose metabolism and enhances insulin sensitivity in mice (1–3). For example, Lee et al. (1) reported that administering berberine to insulin-resistant db/db mice led to a decrease in body fat and significant improvement in glucose tolerance. Because catabolic conditions associated with insulin resistance can lead to progressive muscle atrophy, we examined whether berberine improves muscle protein metabolism. This was of interest because successful inhibition of mechanisms causing loss of muscle mass in diabetic mice might be extended to other catabolic conditions that cause muscle atrophy (4–8). However, we found that berberine actually promoted muscle atrophy in both wild-type and db/db mice. This led us to examine potential mechanisms causing berberine-induced muscle atrophy.
Muscle atrophy induced by several catabolic conditions (e.g., cancer, cachexia, diabetes, chronic kidney disease, cardiac failure, sepsis) share a common group of biochemical and transcriptional adaptations (7–12). In atrophying muscles, there is a higher level of expression of the E3 ubiquitin ligase, atrogin-1/MAFbx, which has been closely linked to stimulation of muscle protein degradation by the ubiquitin-proteasome system (UPS) (13–17). The mechanism that increases atrogin-1 expression has been linked to defects in insulin/IGF-1 signaling, specifically, suppression of insulin receptor substrate (IRS)-1–associated phosphatidylinositol 3-kinase (PI3K) activity and a reduction in p-Akt (14–16). The decrease in p-Akt, in turn, reduces phosphorylation of the forkhead transcription factors (FoxOs) that can enter the nucleus to stimulate atrogin-1 expression. The focus on atrogin-1 in conditions stimulating muscle atrophy arises because atrogin-1 expression causes a proportional increase in muscle protein degradation (17).
Besides accelerated protein degradation causing muscle atrophy, a decrease in protein synthesis will cause loss of muscle protein. Mechanisms changing protein synthesis include impaired insulin/IGF-1 signaling, reducing PI3K and p-Akt activities (9). Another mechanism that can impair muscle protein synthesis was recently reported by Gwinn et al. (18). They found that a rise in p–AMP-activated protein kinase (AMPK) inhibits the activity of the mTOR complex I (TORC1). The mechanism for this response involved phosphorylation of raptor, a regulatory protein that is associated with mTOR. A third mechanism that could impair muscle protein synthesis is suggested by the recent report of Lagirand-Cantaloube et al. (19). They found that atrogin-1 will conjugate ubiquitin to eIF-3f, an essential factor regulating protein translation. Since atrogin-1 is exclusively expressed in muscle, it is possible that activation of atrogin-1 could reduce protein synthesis by stimulating eIF-3f degradation by the UPS. If this were the case, changes in protein degradation could be linked to changes in protein synthesis.
We evaluated how berberine-induced mechanisms would cause muscle atrophy in normal and db/db diabetic mice. Specifically, we measured changes in muscle protein turnover and evaluated the influence of atrogin-1 on these processes. We also evaluated the influence of mitochondria in berberine-induced muscle atrophy, because Turner et al. (2) reported that treating cultured muscle cells with berberine led to impaired mitochondrial function. We found that berberine increased p-AMPK in muscle. Therefore, we examined stimulation of mitochondrial function with peroxisome proliferator–activated receptor (PPAR) γ coactivator (PGC)-1α to determine whether it would correct abnormalities in muscle protein turnover.
RESEARCH DESIGN AND METHODS
Animals.
db/db and wild-type control mice (24 weeks old) were randomly assigned to four groups: wild type, wild type + berberine (Sigma-Aldrich, St. Louis, MO), db/db, and db/db + berberine. The studies were approved by the Baylor College of Medicine Institutional Animal Care and Use Committee. Berberine (5 mg/kg body wt) was injected intraperitoneally for 21 days, while food eaten and weights were monitored (1). Subsequently, food was withdrawn in the morning, and ∼6 h later mice were anesthetized (20 mg/kg ketamine + 4 mg/kg xylazine) and arterial blood was obtained to measure blood glucose and plasma insulin using the Accu-CHEK Advantage blood glucose meter (Indianapolis, IN) and the Insulin Immunoassay 1-2–3 Kit (American Laboratories, Windham, NH), respectively. The predominantly oxidative red-fiber soleus, the predominantly glycolytic white-fiber extensor digitorum longus (EDL), and the mixed-fiber lateral gastrocnemius muscles were removed. Protein synthesis and degradation were measured in isolated soleus and EDL muscles; the gastrocnemius was frozen in liquid nitrogen and stored at −80°C. Tibialis anterior muscles were also removed, fixed at resting length and imbedded in HistoPrep Frozen Embedding Media (Fisher Scientific, Pittsburgh, PA).
Muscle protein synthesis and degradation.
Rates of protein synthesis and degradation were measured in isolated soleus and EDL muscles maintained at resting length (4,10). Briefly, muscles were incubated for 30 min in 3 ml Krebs-Henseleit bicarbonate buffer containing 0.5 mmol/l l-phenylalanine, 10 mmol/l glucose, plus 0.05 μCi of l-[U-14C] phenylalanine (MP Biomedicals, Solon, OH). After gassing with 95% O2/5% CO2, muscles were incubated for 30 min and then removed, blotted, and incubated for 2 h in fresh buffer that had been regassed with 95% O2/5% CO2. The rate of protein synthesis was measured as the incorporation of l-[U-14C] phenylalanine into muscle protein. The rate of protein degradation was measured as the rate of release of tyrosine into the media during the 2 h of incubation (4).
Rates of protein synthesis and degradation were also measured in C2C12 myotubes. The rate of protein synthesis was measured from the incorporation of 3 μCi l-[(3,5)-3H] tyrosine (MP Biomedicals) into cellular proteins during a 16-h incubation. Myotubes were then washed three times with ice-cold PBS before adding 10% trichloroacetic acid to precipitate proteins. After three additional PBS washings, the pellets were dissolved in 0.5 ml of 0.15 mol/l NaOH, and the incorporation of radiolabeled tyrosine and protein content (Bio-Rad DC protein assay kit; Bio-Rad, Hercules, CA) were measured. To measure protein degradation, myotubes were prelabeled with -[(3,5)-3H] tyrosine and incubated in DMEM media containing 2% horse serum. At different times, the trichloroacetic acid–soluble radioactivity released from proteins was measured to calculate the rate of protein degradation (10,17). The measurements were made in triplicate and repeated at least twice.
To assess differences in cross-sectional areas of myofibers, 5-μm sections of tibialis anterior muscles were stained with an anti-laminin antibody (Sigma-Aldrich). The diameters of at least 300 myofibers (×100 magnification) per tibialis anterior muscle was measured using Image J software (National Institutes of Health, Frederick, MD). In studies of C2C12 myotubes, the diameters of 200 myotubes were measured in at least 10 fields (×100 magnification) using Image J software.
Cell culture and Western blot analyses.
C2C12 myoblasts were maintained in DMEM with 10% FBS (HyClone, Logan, UT), penicillin (200 units/ml), and streptomycin (50 μg/ml) (Invitrogen, Carlsbad, CA). At 90% confluence, the media was changed to DMEM plus 2% horse serum (American Type Culture Collection) to induce myotube formation. Berberine was prepared in DMSO (25 mmol/l stock solution) and diluted to achieve different concentrations in the media; control cells were treated with equal amounts of DMSO.
To knockdown atrogin-1, C2C12 myotubes were transfected with 6 μl of smart pool Mafbx-32 siRNA (Dharmacon, Waltham, MA) diluted in 100 μl siRNA transfection media (Invitrogen) for 30 min at room temperature. Subsequently, transfected myotubes were incubated 5–7 h at 37°C. One milliliter of DMEM plus 2% horse serum was added; the incubation was continued for an additional 36 h; atrogin-1 knockdown was confirmed by Northern blotting (10). To overexpress PGC-1α, we transfected C2C12 myotubes with an adenovirus bearing PGC-1α for 36 h; control cells were treated with an adenovirus expressing green fluorescent protein.
Lysates of C2C12 myotubes were prepared in radioimmunoprecipitation assay buffer (20 mmol/l Tris, pH 7.5; 5 mmol/l EDTA; 150 mmol/l NaCl; 1% NP40; 0.5% Na-deoxycholate; 0.025% SDS; 1 mmol/l Na-orthovanadate; 10 mmol/l NaF; 25 μmol/l β-glycerophosphate and 1 μmol/l leupeptin; 1 μmol/l pepstatin; and 10 μmol/l aprotinin). After centrifugation at 15,000g for 15 min at 4°C, Western blots were performed as described (4,7,10). Lysates of gastrocnemius muscles were prepared from ∼50 mg muscle by homogenizing in 0.5 ml lysis buffer (50 mmol/l Tris, pH 7.4; 1% NP-40; 0.25% Na-deoxycholate; 150 mmol/l NaCl; 1 mmol/l EDTA; 1 mmol/l phenylmethylsulfonyl fluoride; 1 μg/ml each of aprotinin, leupeptin, and pepstatin; 1 mmol/l Na3VO4; and 1 mmol/l NaF). Western blots were prepared from the supernatant obtained after centrifuging at 16,000g at 4°C for 15 min.
The following antibodies were used in Western blots: eIF3-f from Rockland Immunochemicals (Gilbertsville, PA) and p-Akt (Ser 437), Akt, p–forkhead box class Os (FOXOs), p-p70S6K, p70S6K, p-AMPK (Thr172), AMPK, p-raptor(Ser 792), raptor, p-S6K1(Thr 389), and S6K1 from Cell Signaling (Beverly MA). The PGC1-α, FOXOs, and glyceraldehyde-3-phosphate dehydrogenase (GADPH) antibodies were from Santa Cruz Biotechnology (Santa Cruz, CA).
RNA and quantitative real-time PCR analyses.
RNA from gastrocnemius muscles or cultured cells was isolated (TRI reagent; Invitrogen) and Northern blots were performed as described (4,10,14). α-32P dCTP–labeled cDNA probe of atrogin-1 was synthesized using a random-primer labeling kit (GE Life Science, Piscataway, NJ) and purified using G-25 columns (Roche, Indianapolis, IN). Signals were analyzed by autoradiography and expressed relative to GAPDH.
For real-time PCR, 2 μg RNA was used for first-strand cDNA synthesis using the SuperScript First-Strand Synthesis System for RT-PCR (Invitrogen). Real-time PCR was performed with iQSYBR Green Supermix reagents (Bio-Rad) as described (20). We used the following primers: mouse atrogin-1/MAFbx: forward, 5′-GCAAACACTGCCACATTCTCTC-3′ and reverse, 5′-CTTGAGGGGAAAGTGAGACG-3′. Cytochrome C: forward, 5′-GCAAGCATAAGACTGGACCAAA-3′ and reverse, 5′-TTGTTGGCATCTGTGT AAGAGAATC-3′. The mitochondrial atpase 5b: forward, 5′-ACTGTGT CCCGGGCAAGAAAGATA-3′ and reverse, 5′-AAGGCTTG TTCTGGGAGATGGTCA-3′. Quantum RNA18S primer (Ambion, Austin, TX) was used as the control.
Statistical analysis.
Results are presented as means ± SE. Statistical analysis was performed by ANOVA followed by Tukey or Student-Newman-Keul tests. P < 0.05 was considered statistically significant. Experiments were repeated at least three times.
RESULTS
Berberine stimulates muscle atrophy in mice.
When wild-type or db/db mice were injected intraperitoneally with 5 mg berberine/kg/day for 3 weeks, there was no difference in food intake, but body and epididymal fat pad weights decreased significantly compared with values in saline-injected mice (supplemental Fig. 1A–C, available at http://diabetes.diabetesjournals.org/cgi/content/full/db10-0207/DC1). Blood glucose levels in 6-month-old db/db mice were threefold higher than in littermate wild-type mice (18 ± 4.2 vs. 6 ± 2.3 mmol/l; P < 0.01, n = 12; supplemental Fig. 1D), while plasma insulin was about threefold higher in db/db mice (supplemental Fig. 1E). Berberine administration to db/db mice significantly decreased blood glucose but did not change plasma insulin levels.
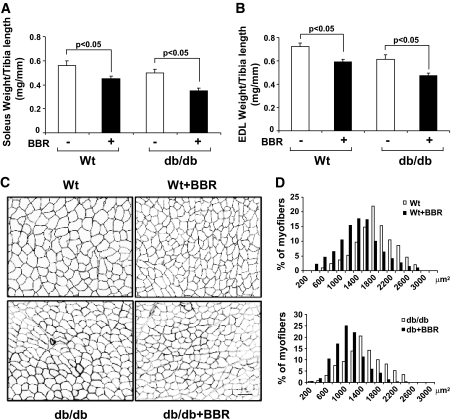
Berberine administration significantly decreased muscle mass in wild-type and db/db mice, as indicated by lower weights of soleus and EDL muscles compared with muscles of saline-treated mice (Fig. 1A and B). Muscle weights were corrected for tibia lengths rather than body weight since db/db mice are disproportionately obese. Berberine-induced loss of muscle mass was confirmed when we measured the average cross-sectional areas of myofibers in muscles of berberine-treated wild-type and db/db mice and compared results of saline-treated mice (Fig. 1C). In wild-type mice, the average myofiber sizes were 2094.8 ± 106.3 μm2 in untreated mice vs. 1,736 ± 208.3 μm2 in berberine-treated mice. In db/db mice, the average values were 1607.7 ± 107.2 μm2 in untreated mice vs. 1,200 ± 78.3 μm2 in berberine-treated mice (P < 0.001; n = 6 in each group). There also was a leftward shift in the distribution of myofiber sizes in muscles from berberine-treated compared with PBS-treated mice, consistent with loss of muscle mass (Fig. 1D). Thus, berberine caused muscle atrophy in both wild-type mice and db/db mice.
FIG. 1.
Berberine (BBR) causes muscle atrophy in wild-type (Wt) and db/db mice. A and B: Wild-type and db/db mice were treated with berberine (5 mg/kg) for 3 weeks. The weights of the soleus and the extensor digitorum longus (EDL) muscles were normalized by the lengths of tibia as db/db mice gain weight disproportionally (n = 8 in each group; means ± SE). C: The cross-sectional of tibialis anterior muscles in wild-type and db/db mice, with and without berberine treatment. Myofibers were outlined using dystrophin staining. D: the distribution of myofiber sizes in muscles from untreated and berberine-treated mice. Data were obtained from six mice in each group.
Berberine suppresses protein synthesis and stimulates protein degradation in muscle.
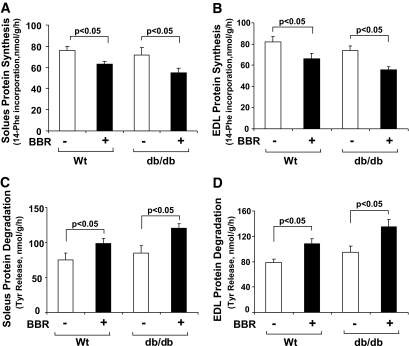
To examine why muscle atrophy occurred, we measured components of protein metabolism in isolated soleus and EDL muscles of wild-type and db/db mice. In berberine-treated mice, protein synthesis was significantly lower in both soleus and EDL muscles compared with values in saline-treated mice (Fig. 2A and B). In berberine-treated wild-type and db/db mice, muscle protein degradation in soleus and EDL muscles were significantly higher than rates measured in either group of mice that was treated with saline (Fig. 2C and D).
FIG. 2.
Berberine (BBR) suppresses protein synthesis and stimulates protein degradation in muscle of wild-type (Wt) and db/db mice. A and B: Protein synthesis was measured from the rate of incorporation of l-[U-14C] phenylalanine into isolated, incubated soleus and EDL muscles. Berberine treatment suppressed protein synthesis in wild-type and db/db mice (n = 6 in each group). C and D: Protein degradation was measured as the rate of tyrosine release from isolated soleus and EDL muscles. Berberine significantly increased protein degradation in both wild-type and db/db mice (n = 6 in each group).
Berberine increases atrogin-1 expression in muscle.
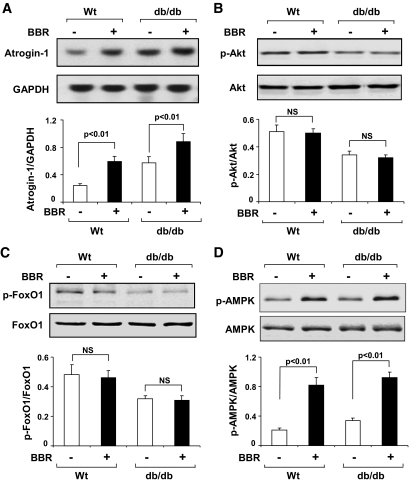
In wild-type and db/db mice, we explored whether activation of the UPS contributes to berberine-induced changes in muscle protein metabolism. We measured atrogin-1 expression because an increase in atrogin-1 is related to the rate of protein degradation in muscle (17). We found that berberine treatment of wild-type or db/db mice significantly upregulated atrogin-1 mRNA in muscle (Fig. 3A). Since one mechanism that activates atrogin-1 is impaired PI3K/Akt signaling (15,16,21), we evaluated the levels of p-Akt and phosphorylated FoxOs in muscle. The levels of both p-Akt and p-FoxOs were lower in muscles of untreated db/db mice compared with the values present in wild-type mice; berberine treatment did not change p-Akt or p-FoxOs further (Fig. 3B and C). Another stimulator of atrogin-1 expression in muscle is p-AMPK (22). When we measured p-AMPK, we found a higher level in muscles of berberine-treated wild-type or db/db mice (Fig. 3D).
FIG. 3.
Berberine (BBR) stimulates atrogin-1 expression in muscle of wild-type and db/db mice. A: Atrogin-1/MAFbx mRNA was accessed by Northern blotting. Berberine increased atrogin-1 expression in muscles of wild-type and db/db mice (n = 6 in each group). B and C: Phosphorylation of Akt and FOXO1 transcription factor was examined by Western blotting in samples from A. Berberine did not change p-Akt (ser 473) or p-FOXO1 (Thr 24) levels in wild-type and db/db mice. D: Berberine increased p-AMPK (Thr 172) in muscles of wild-type and db/db mice from A.
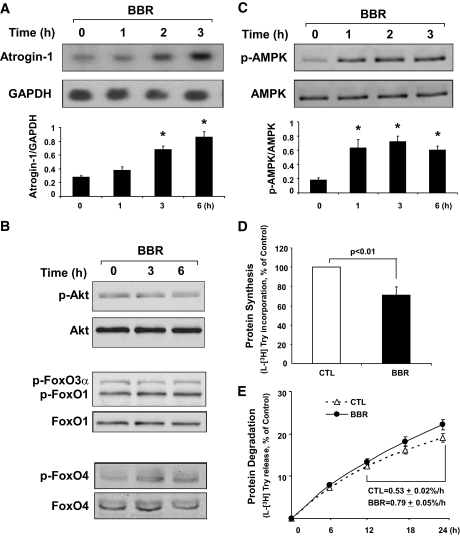
C2C12 myotubes were treated with berberine to determine whether berberine will directly affect atrogin-1 expression and muscle protein metabolism. Increasing concentrations of berberine significantly increased atrogin-1 mRNA in mytotubes, and it caused a progressive decrease in myotube diameters (Fig. 4A) (supplemental Fig. 2). In agreement with the results we obtained in muscles of wild-type and db/db mice, the addition of berberine did not change the levels of p-Akt or p-FoxO1, p-FoxO3α, or p-FoxO4 (Fig. 4B). Likewise, berberine increased the level of p-AMPK in cultured muscle cells (Fig. 4C).
FIG. 4.
In C2C12 myotubes, 3 μmol/l berberine (BBR) directly stimulated atrogin-1 expression without changing the phosphorylation of Akt or FoxOs. A: Upon adding berberine, atrogin-1 mRNA level (Northern blot) increased in a time-dependent manner. (*P < 0.01 vs. values in untreated myotubes; n = 3 independent experiments for each period). B: In C2C12 myotubes, p-Akt (ser 473) and p-FoxO1 (Thr 24), p-FoxO3α(Thr 32), and p-FoxO4 (Ser262) were unchanged by berberine. C: In C2C12 myotubes, berberine increased p-AMPK (Thr 172) (P < 0.01 vs. values in untreated myotubes; n = 3 independent experiments). D: In C2C12 myotubes, berberine suppressed protein synthesis (see research design and methods). P < 0.01 vs. values in untreated myotubes (CTL; n = 3 independent experiments). E: In C2C12 myotubes, berberine stimulated protein degradation (see research design and methods). Rates of proteolysis were calculated from linear slopes present between 12 and 24 h (n = 3 independent experiments).
Berberine-induced changes in muscle protein metabolism in wild-type and db/db mice. Similar events occurred in myotubes treated with berberine; there was a significant decrease in protein synthesis and an increase in protein breakdown compared with results from untreated myotubes (Fig. 4D and E).
Atrogin-1 mediates berberine-induced atrophy of myotubes.
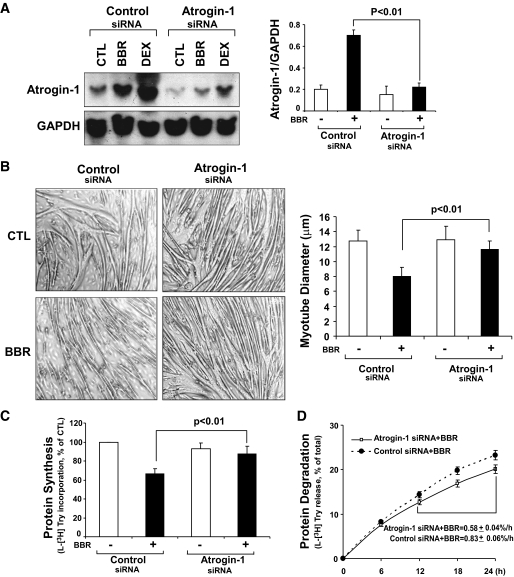
To examine if atrogin-1 impairs muscle protein metabolism in cultured myotubes, we used an siRNA approach and measured protein synthesis and degradation. At 36 h after transfection with atrogin-1 siRNA, the mRNA of atrogin-1 was 90% lower in berberine-treated myotubes compared with control myotubes (Fig. 5A). Atrogin-1 knockdown resulted in an increase in the diameters of berberine-treated myotubes, indicating that the muscle atrophic responses were inhibited (Fig. 5B). As expected, atrogin-1 knockdown significantly inhibited protein degradation in berberine-stimulated myotubes (Fig. 5D). Unexpectedly, we found that the decrease in protein synthesis induced by berberine was no longer present in cells with atrogin-1 knockdown. Specifically, berberine treatment of control myotubes produced a 28.6% (P < 0.05) decrease in synthesis compared with values in untreated myotubes (Fig. 5C). Thus, atrogin-1 mediates the berberine-induced changes in both protein degradation and synthesis in muscle cells.
FIG. 5.
In C2C12 myotubes, atrogin-1 knockdown prevents berberine (BBR)-induced atrophy. A: At 36 h after atrogin-1 siRNA transfection, C2C12 myotubes were treated for 16 h with DMSO, berberine (3 μm), or dexamethasone (DEX) (1 μm DEX, a positive control) before atrogin-1 mRNA was measured by Northern blotting. B: At 36 h after atrogin-1 siRNA transfection, C2C12 myotubes were treated overnight with 3 μmol/l berberine or without (CTL). The diameters of 300 myotubes were measured and averaged (n = 3 independent experiments). C: C2C12 myotubes were treated as in B and then used to measure protein synthesis (see research design and methods). Measurements were made in duplicate in n = 3 independent experiments. D: C2C12 myotubes were treated as in B and then used to measure protein degradation (see research design and methods and the legend to Fig. 4E). Measurements were made in duplicate in n = 3 independent experiments.
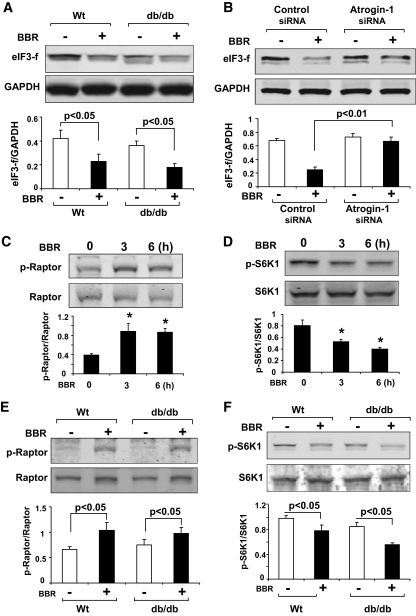
Berberine decreases eIF3-f and protein synthesis by an atrogin-1–dependent mechanism.
In C2C12 myotubes, knockdown of atrogin-1 significantly blocked the berberine-induced decrease in protein synthesis (Fig. 5C). We proposed that this response could be linked to changes in the protein synthesis mediator, eIF3-f, because berberine also decreased the level of eIF3-f in muscles of wild-type and db/db mice (Figs. 2A and B and 6A). To examine this possibility, we measured eIF3-f protein in berberine-treated myotubes and found that it was 50% lower than in atrogin-1 knockdown myotubes. The increase in eIF3-f level was associated with increased protein synthesis (Figs. 5C and 6B). Thus, the stimulation of atrogin-1 expression by berberine can regulate muscle protein metabolism in two ways: it stimulates protein degradation by the UPS and reduces eIF3-f to suppress protein synthesis.
FIG. 6.
Berberine (BBR) administration stimulates atrogin-1 expression and decreases eIF3-f in muscle cells. A: eIF3-f in muscles of wild-type (Wt) and db/db mice treated with or without berberine was evaluated by Western blot analysis. There was a decrease in eIF3-f, which was linked to the increase in atrogin-1 (see Fig. 3A; n = 6 mice in each group). B: In C2C12, myotubes were treated to knockdown atrogin-1 (Fig. 5C), blocking the decrease in eIF3-f protein levels induced by berberine treatment (n = 3 independent experiments). C and D: C2C12 myotubes were treated with 3 μmol/l berberine, and levels of p-Raptor (Thr 798) and p-S6K1 (Thr 389) were accessed by Western blotting. Berberine significantly increased p-Raptor level and inhibited S6K1 phosphorylation (*P < 0.05 vs. values in untreated C2C12 myotubes; n = 3 independent experiments). E and F: p-Raptor and p-S6K levels in muscles of wild-type and db/db mice following treatment with or without berberine administration were assessed by Western blotting. Berberine-induced an increase in p-Raptor and a decrease in p-S6K1 (n = 6, mice in each group).
Results in Fig. 5C show that the knockdown of atrogin-1 did not completely restore protein synthesis, suggesting that berberine activated other protein synthetic mechanisms. One mechanism could involve AMPK-dependent phosphorylation of raptor (the regulatory associated protein of mTOR) at Thr792 (18). This phosphorylation of raptor impairs mTOR activity, resulting in decreased activation of p-S6K1 and, hence, muscle protein synthesis. In studies of berberine-treated C2C12 myotubes, we also found evidence for activation of the same pathway. Berberine increased phosphorylation of raptor and decreased the level of p-S6K1 (Figs. 6C and D). Similar responses were found in berberine-treated wild-type and db/db mice (Fig. 6E and F).
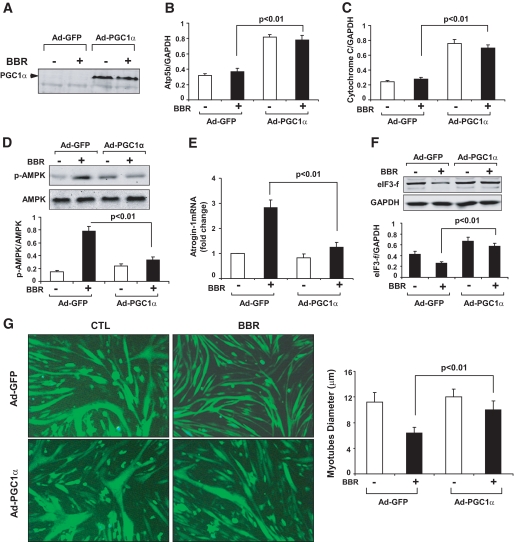
Overexpression of PGC-1α prevents berberine-induced muscle atrophy.
Why are berberine-induced changes in muscle AMPK levels associated with changes in protein metabolism? Krawiec et al. (22) reported that stimulation of AMPK activity by administration of AICAR can increase atrogin-1 expression. Since AMPK is a sensor of cellular energy metabolism, the adverse influence of berberine might involve mitochondrial dysfunction. For example, it has been reported that berberine interferes with mitochondrial complex I function while augmenting the content of uncoupling proteins 2 and 3 (2,23). To examine this possibility, we overexpressed the mitochondrial biogenesis factor, PGC-1α, in C2C12 myotubes (Fig. 7A). As expected, there was increased gene expression of cytochrome C and atpase 5b, along with a decrease in p-AMPK (Fig. 7B–D) (24). In myotubes expressing PGC-1α, there was marked inhibition of the increase in atrogin-1 that berberine induces. In addition, eIF3-f protein was almost returned to the control level despite the presence of berberine (Fig. 7E and F). These changes induced by PGC-1α result in an increase in the sizes of berberine-treated myotubes compared with control myotubes (Figs. 7G). Our results link muscle cell atrophy to a dual influence of atrogin-1 on protein turnover but also indicate that abnormal mitochondrial energy production can cause muscle cell atrophy.
FIG. 7.
Overexpression of PGC-1α prevents berberine (BBR)-induced atrophy of C2C12 myotubes. A: C1C12 myotubes were infected with adenovirus-GFP (Ad-GFP) or adenovirus-PGC-1α for 36 h. Subsequently, 3 μm berberine was added for an additional 12 h and PGC-1α (n = 3 independent experiments). B and C: Following PGC-1α expression in myotubes, there was induction of atpase-5b and cytochrome C (n = 3 independent experiments). D: In C2C12 myotubes treated as in B or C, p-AMPK (Thr172) increased and PGC-1α expression suppressed the berberine-induced increase in p-AMPK (n = 3 independent experiments). E: Berberine-induced expression of atrogin-1 (RT-qPCR) in myotubes was blocked by in PGC-1α expression (n = 3 independent experiments). F: In myotubes, PGC-1α suppressed the decrease in eIF3-f expression that was caused by berberine-induced atrogin-1 expression (n = 3 independent experiments). G: The berberine-induced decrease in myotubes diameter was improved by PGC-1α expression (the diameters of 300 myotubes were measured in three independent experiments). (A high-quality digital representation of this figure is available in the online issue.)
DISCUSSION
The herbal derivative, berberine, has been shown to lower blood glucose and lipid levels in animal models of diabetes, leading to the conclusion that berberine can improve insulin sensitivity (1,3,25). Since defects in insulin/IGF-1 signaling (i.e., decreased activity of PI3K and p-Akt) cause muscle protein losses in catabolic conditions, we hypothesized that berberine could improve muscle protein metabolism when there was insulin resistance (4,10,20,26). Although berberine did ameliorate hyperglycemia and reduce fat mass in db/db mice as a model of insulin resistance (20), it also caused muscle atrophy in both wild-type and db/db mice (Fig. 1). The muscle atrophy occurring in berberine-treated wild-type or db/db mice was associated with stimulation of atrogin-1 expression (Figs. 3A). This led us to uncover two new atrogin-1–linked mechanisms that could play a role in the muscle atrophy that occurs in other catabolic conditions. Specifically, we found that the increase in atrogin-1 not only accelerated protein degradation in muscle but also suppressed protein synthesis. The latter mechanism involved promotion of eIF3-f degradation, reducing its level in muscle (Fig. 6A). In fact, knockdown of atrogin-1 blocked both the increase in protein degradation and the decrease in protein synthesis stimulated by berberine (Fig. 5). Second, we found evidence that impaired mitochondrial function induced by berberine not only resulted in an increase in muscle AMPK levels but also stimulated atrogin-1 expression. This pathway leading to atrogin-1 expression and abnormalities in muscle protein metabolism was blocked in cells expressing PGC-1α (Fig. 7).
Experimental results obtained in wild-type and db/db mice can be influenced by changes in systemic factors (e.g., circulating hormones or cytokines as well as dietary and environmental influences). To exclude these factors, we also studied responses of C2C12 differentiated muscle cells or myotubes and found that berberine directly changes muscle protein metabolism (Fig. 4).
The link between atrogin-1 and protein degradation is well known (17). For example, we have demonstrated that an increase in Ser307 phosphorylation of IRS-1 in muscle of db/db mice is linked to an increase in atrogin-1 and protein degradation in muscle (20). In those studies, administration of the PPAR-γ agonist, rosiglitazone, blocked the increase in Ser307 phosphorylation of IRS-1, raising the p-Akt level with suppression of atrogin-1 and muscle atrophy. Moreover, we and others find that berberine does not change Ser307 phosphorylation of IRS-1 in muscle, nor does it influence PPAR-γ gene expression (3,27).
What could be the berberine-induced mechanism underlying the changes in muscle protein metabolism? One possibility is that berberine suppresses the insulin/IGF-1/Akt pathway. This would reduce phosphorylation of FoxO transcription factors and promotion of atrogin-1 expression in muscle and protein degradation (14–16). However, berberine treatment of wild-type or db/db mice did not decrease p-Akt or p-FoxO1 levels (Fig. 3B and C). Another possibility is that berberine stimulates atrogin-1 expression via activation of AMPK. Krawiec et al. (22) treated mice and muscle cells with AICAR and found an increase in p-AMPK that led to increased atrogin-1 expression. This is relevant because Yin et al. (3) reported that 5 μmol/l berberine increased the phosphorylation of AMPK (p-AMPK) in cultured muscle cells. We confirmed that treatment of cultured CC12 myotubes with 3 μmol/l berberine or administration of berberine to mice increased p-AMPK and atrogin-1 expression in muscle (Figs. 3A and D and 4A and C). The increase in p-AMPK induced by berberine could also influence muscle protein metabolism by interfering with the activity of S6K1 through a mechanism involving phosphorylation of raptor (18,28). We explored this possibility and found increased levels of p-raptor with a decrease in p-S6K1 (Fig. 7). Based on the changes in protein synthesis occurring in berberine-treated muscle cells, we estimate that atrogin-1 contributes ∼70% of the decrease based on results from knocking down atrogin-1. Thus, we estimate that the inhibition of TORC1/S6K1 contributes ∼30% of the decrease in protein synthesis.
The finding that p-AMPK in muscle rises with berberine treatment is consistent with induction of abnormal energy metabolism, yet both blood glucose and fat stores are reduced (supplemental Fig. 1). Others (2) have attributed to these results to berberine-induced inhibition of mitochondrial complex I and, possibly, induction of uncoupling proteins. Our results support a role for impaired energy metabolism in creating berberine-induced abnormalities in protein metabolism. When we treated cells with PGC-1α, we found evidence of increased mitochondrial biogenesis that was associated with correction of the abnormalities in muscle protein metabolism (Fig. 7). Future work will require determining how variations in mitochondrial energy metabolism in muscle actually change atrogin-1 expression and how this influences protein synthesis and degradation.
We recognize that our findings from experiments utilizing mice or cultured cells may not reflect events occurring in patients with type 2 diabetes. Reports of protein turnover in diabetic or insulin-resistant patients find no muscle wasting unless the patients are elderly or sedentary (29–32). Even though obese patients with type 2 diabetes were shown to exhibit some impairment in ATP production, it has also been found that intensive insulin therapy did not change leucine kinetics when compared with results achieved with conventional insulin therapy (33). However, our results do indicate that antidiabetes drugs can cause unexpected consequences, including changes in protein metabolism.
In summary, we have uncovered two factors that affect the control of muscle protein metabolism. First, a decrease in energy metabolism in muscle can stimulate protein losses by raising protein degradation and suppressing protein synthesis. Second, an increase in atrogin-1 expression not only is associated with increased protein degradation by the ubiquitin-proteasome system, but it also can interfere with protein synthesis by promoting the degradation of factors regulating synthesis.
ACKNOWLEDGMENTS
The work was supported by National Institutes of Health Grants R37 DK37175, P50 DK64233, and R01 DK62828.
H.W. researched data. D.L. researched data. P.C. researched data. S.L. reviewed/edited manuscript. Z.H. wrote manuscript/researched data.
H.W. was supported by Shanghai Science and Technology Commission Grant 07QH14020. D.L. was supported by Shenyang Science and Technology Developments Grant 1063314-1-00.
No potential conflicts of interest relevant to this article were reported.
We thank Dr. William E. Mitch for adding helpful comments and encouragement.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Lee YS, Kim WS, Kim KH, Yoon MJ, Cho HJ, Shen Y, Ye JM, Lee CH, Oh WK, Kim CT, Hohnen-Behrens C, Gosby A, Kraegen EW, James DE, Kim JB: Berberine, a natural plant product, activates AMP-activated protein kinase with beneficial metabolic effects in diabetic and insulin-resistant states. Diabetes 2006;55:2256–2264 [DOI] [PubMed] [Google Scholar]
- 2.Turner N, Li JY, Gosby A, To SW, Cheng Z, Miyoshi H, Taketo MM, Cooney GJ, Kraegen EW, James DE, Hu LH, Li J, Ye JM: Berberine and its more biologically available derivative, dihydroberberine, inhibit mitochondrial respiratory complex I: a mechanism for the action of berberine to activate AMP-activated protein kinase and improve insulin action. Diabetes 2008;57:1414–1418 [DOI] [PubMed] [Google Scholar]
- 3.Yin J, Gao Z, Liu D, Liu Z, Ye J: Berberine improves glucose metabolism through induction of glycolysis. Am J Physiol Endocrinol Metab 2008;294:E148–E156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hu Z, Wang H, Lee IH, Du J, Mitch WE: Endogenous glucocorticoids and impaired insulin signaling are both required to stimulate muscle wasting under pathophysiological conditions in mice. J Clin Invest 2009;119:7650–7659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hasselgren P-O, Warner BW, James H, Takehara H, Fischer JE: Effect of insulin on amino acid uptake and protein turnover in skeletal muscle from septic rats: evidence for insulin resistance of protein degradation. Arch Surg 1987;122:228–233 [DOI] [PubMed] [Google Scholar]
- 6.Mitch WE, Medina R, Greiber S, May RC, England BK, Price SR, Bailey JL, Goldberg AL: Metabolic acidosis stimulates muscle protein degradation by activating the ATP-dependent pathway involving ubiquitin and proteasomes. J Clin Invest 1994;93:2127–2133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang L, Du J, Hu Z, Han G, Delafontaine P, Garcia G, Mitch WE: IL-6 and serum amyloid A synergy mediates angiotensin II-induced muscle wasting. J Am Soc Nephrol 2009;20:604–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang L, Wang XH, Wang H, Hu Z, Du J, Mitch WE: Satellite cell dysfunction and impaired IGF-1 signaling contribute to muscle atrophy in chronic kidney disease. J Am Soc Nephrol 2010;21:419–427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lecker SH, Goldberg AL, Mitch WE: Protein degradation by the ubiquitin-proteasome pathway in normal and disease states. J Am Soc Nephrol 2006;17:1807–1819 [DOI] [PubMed] [Google Scholar]
- 10.Hu Z, Lee IH, Wang X, Shang H, Zhang L, Du J, Mitch WE: PTEN expression contributes to the regulation of muscle protein degradation in diabetes. Diabetes 2007;56:2449–2456 [DOI] [PubMed] [Google Scholar]
- 11.Du J, Wang X, Meireles CL, Bailey JL, Debigare R, Zheng B, Price SR, Mitch WE: Activation of caspase 3 is an initial step triggering muscle proteolysis in catabolic conditions. J Clin Invest 2004;113:115–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lecker SH, Jagoe RT, Gomes M, Baracos V, Bailey JL, Price SR, Mitch WE, Goldberg AL: Multiple types of skeletal muscle atrophy involve a common program of changes in gene expression. FASEB J 2004;18:39–51 [DOI] [PubMed] [Google Scholar]
- 13.Bodine SC, Latres E, Baumhueter S, Lai VK, Nunez L, Clark BA, Poueymirou WT, Panaro FJ, Na E, Dharmarajan K, Pan ZQ, Valenzuel DM, DeChiara TM, Stitt TN, Yancopoulos GD, Glass DJ: Identification of ubiquitin ligases required for skeletal muscle atrophy. Sci 2001;294:1704–1708 [DOI] [PubMed] [Google Scholar]
- 14.Lee SW, Dai G, Hu Z, Wang X, Du J, Mitch WE: Regulation of muscle protein degradation: coordinated control of apoptotic and ubiquitin-proteasome systems by phosphatidylinositol 3 kinase. J Am Soc Nephrol 2004;15:1537–1545 [DOI] [PubMed] [Google Scholar]
- 15.Stitt TN, Drujan D, Clarke BA, Panaro F, Timofeyva Y, Klinenber JR, Gonzalez M, Yancopoulos GD, Glass DJ: The IGF-1/PI3K/Akt pathway prevents expression of muscle atrophy-induced ubiquitin ligases by inhibiting FOXO transcription factors. Mol Cell 2004;14:395–403 [DOI] [PubMed] [Google Scholar]
- 16.Sandri M, Sandri C, Gilbert A, Skuck C, Calabria E, Picard A, Walsh K, Schiaffino S, Lecker SH, Goldberg AL: Foxo transcription factors induce the atrophy-related ubiquitin ligase atrogin-1 and cause skeletal muscle atrophy. Cell 2004;117:399–412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sacheck JM, Ohtsuka A, McLary SC, Goldberg AL: IGF-1 stimulates muscle growth by suppressing protein breakdown and expression of atrophy-related ubiquitin ligases, atrogin-1 and MuRF1. Am J Physiol 2004;287:E591–E601 [DOI] [PubMed] [Google Scholar]
- 18.Gwinn DM, Shackelford DB, Egan DF, Mihaylova MM, Mery A, Vasquez DS, Turk BE, Shaw RJ: AMPK phosphorylation of raptor mediates a metabolic checkpoint. Mol Cell 2008;30:214–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lagirand-Cantaloube J, Offner N, Csibi A, Leibovitch MP, Batonnet-Pichon S, Tintignac LA, Segura CT, Leibovitch SA: The initiation factor eIF3-f is a major target for atrogin1/MAFbx function in skeletal muscle atrophy. EMBO J 2008;27:1266–1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang XH, Hu Z, Hu JP, Du J, Mitch WE: Insulin resistance accelerates muscle protein degradation: activation of the ubiquitin-proteasome pathway by defects in muscle cell signaling. Endocrin 2006;147:4160–4168 [DOI] [PubMed] [Google Scholar]
- 21.Bloomfield SA, Allen MR, Hogan HA, Delp MD: Site- and compartment-specific changes in bone with hindlimb unloading in mature adult rats. Bone 2004;31:149–157 [DOI] [PubMed] [Google Scholar]
- 22.Krawiec BJ, Nystrom GJ, Frost RA, Jefferson LS, Lang CH: AMP-activated protein kinase agonists increase mRNA content of the muscle-specific ubiquitin ligases MAFbx and MuRF1 in C2C12 cells. Am J Physiol Endocrinol Metab 2007;292:E1555–E1567 [DOI] [PubMed] [Google Scholar]
- 23.Kim WS, Lee YS, Cha SH, Jeong HW, Choe SS, Lee MR, Oh GT, Park HS, Lee KU, Lane MD, Kim JB: Berberine improves lipid dysregulation in obesity by controlling central and peripheral AMPK activity. Am J Physiol Endocrinol Metab 2009;296:E812–E819 [DOI] [PubMed] [Google Scholar]
- 24.Hanai J, Cao P, Tanksale P, Imamura S, Koshimizu E, Zhao J, Kishi S, Yamashita M, Phillips PS, Sukhatme VP, Lecker SH: The muscle-specific ubiquitin ligase atrogin-1/MAFbx mediates statin-induced muscle toxicity. J Clin Invest 2007;117:3940–3951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheng Z, Pang T, Gu M, Gao AH, Xie CM, Li JY, Nan FJ, Li J: Berberine-stimulated glucose uptake in L6 myotubes involves both AMPK and p38 MAPK. Biochim Biophys Acta 2006;1760:1682–1689 [DOI] [PubMed] [Google Scholar]
- 26.Price SR, Bailey JL, Wang X, Jurkovitz C, England BK, Ding X, Phillips LS, Mitch WE: Muscle wasting in insulinopenic rats results from activation of the ATP-dependent, ubiquitin-proteasome pathway by a mechanism including gene transcription. J Clin Invest 1996;98:1703–1708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang C, Zhang Y, Gong Z, Sheng X, Li Z, Zhang W, Qin Y: Berberine inhibits 3T3–L1 adipocyte differentiation through the PPARgamma pathway. Biochem Biophys Res Commun 2006;348:571–578 [DOI] [PubMed] [Google Scholar]
- 28.Guillet C, Prod'homme M, Balage M, Gachon P, Giraudet C, Morin L, Grizard J, Boirie Y: Impaired anabolic response of muscle protein synthesis is associated with S6K1 dysregulation in elderly humans. FASEB J 2004;18:1586–1587 [DOI] [PubMed] [Google Scholar]
- 29.Halvatsiotis P, Short KR, Bigelow M, Nair KS: Synthesis rate of muscle proteins, muscle functions and amino acid kinetics in type 2 diabetes. Diabetes 2002;51:2395–2404 [DOI] [PubMed] [Google Scholar]
- 30.Park SW, Goodpaster BH, Lee JS, Kuller LH, Boudreau R, de RN, Harris TB, Kritchevsky S, Tylavsky FA, Nevitt M, Cho YW, Newman AB: Excessive loss of skeletal muscle mass in older adults with type 2 diabetes. Diabetes Care 2009;32:1993–1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fujita S, Rasmussen BB, Cadenas JG, Drummond MJ, Glynn EL, Sattler FR, Volpi E: Aerobic exercise overcomes the age-related insulin resistance of muscle protein metabolism by improving endothelial function and Akt/mammalian target of rapamycin signaling. Diabetes 2007;56:1615–1622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fujita S, Glynn EL, Timmerman KL, Rasmussen BB, Volpi E: Supraphysiological hyperinsulinaemia is necessary to stimulate skeletal muscle protein anabolism in older adults: evidence of a true age-related insulin resistance of muscle protein metabolism. Diabetologia 2009;52:1889–1898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stump CS, Short KR, Bigelow ML, Schimke JM, Nair KS: Effect of insulin on human skeletal muscle mitochondrial ATP production, protein synthesis, and mRNA transcripts. Proc Natl Acad Sci U S A 2003;100:7996–8001 [DOI] [PMC free article] [PubMed] [Google Scholar]