Abstract
Purpose
Male pattern baldness (MPB) and prostate cancer (PCa) share commonality as prevalent, heritable and androgen-related conditions. Studies exploring the relationship between the two conditions have been inconclusive. Using a population-based, case-control study of PCa, we explore the relationship between early onset MPB and PCa risk.
Methods
Cases were men aged 35 – 74 diagnosed with PCa between 2002 – 2005 in King County, Washington. Controls were frequency matched by age and identified by random digit dialing. Hair pattern at age 30 and at 1 year prior to diagnosis (cases) or reference date (controls) was determined using showcards. PCa risk associated with balding was assessed with logistic regression.
Results
Data from 999 cases of PCa and 942 controls were analyzed. Hair loss at age 30 was more common in controls (25.2%) than cases (19.8%, p = 0.005), and those with hair loss at age 30 had a 29% relative risk reduction for PCa (OR 0.71, 95% CI 0.56 – 0.91). No risk reduction was seen for men only reporting hair loss at referent age (OR 0.90, 95% CI 0.73-1.12). In men aged > 60 at referent date, the risk reduction was greater for men with hair loss at age 30 from both the top of head and forehead (OR 0.55, 95% CI 0.33 – 0.93).
Conclusion
Early onset MPB was associated with a reduced relative risk of PCa in this population-based study. Further research into a possible mechanistic link between these prevalent and androgen-related conditions is warranted.
Keywords: prostate cancer, male pattern baldness, relative risk, population-based
Introduction
Male pattern baldness (MPB) is a highly prevalent condition closely related to a man's age. By age 30, approximately 25% – 30% of men will have MPB. By age 50, the prevalence is 50% and reaches nearly 80% by age 70.1 MPB is heritable2, is a complex androgen-regulated process that requires the potent testosterone metabolite dihydrotestosterone (DHT), and has been shown to occur with increased frequency in men with specific polymorphisms in the androgen receptor gene (AR).3-6 Moreover, DHT levels are higher within the hair follicles of men with MPB7, while inhibition of DHT production slows the progression of MPB.8 Prostate cancer (PCa) shares some similarities with MPB. PCa is also heritable with age-dependent prevalence of histologic PCa of 20% – 30% for men in their 50s and up to 80% for men in their 70s.9 Androgens are required for prostate development and homeostasis while alterations in androgen metabolism and DHT production appear to affect subsequent PCa risk.10 Given the similarities between MPB and PCa risk, these entities may share underlying etiologic factors.
Several studies have explored the relationship between MPB and PCa risk.11-14 Results from these analyses have been conflicting with increased13, 14 or no alteration in risk11, 12 observed. These discrepant findings may be affected by small sample sizes in studies with inadequate power and inconsistent exposure assessment (e.g., not measuring age of onset of MPB). If MPB was associated with PCa, early assessment of male hair distribution might provide a non-invasive method to identify at-risk individuals. Therefore, we used a population based case-control datset to evaluate the relationship between early-onset MPB (at age 30) and PCa risk.
Methods
Study participants
The study population consists of participants in a population-based case-control study of PCa. Details of the study participants and data collection have previously been described.15 Briefly, cases were residents of King County, Washington with histologically confirmed PCa ascertained from the Seattle-Puget Sound SEER cancer registry diagnosed between January 1, 2002, and December 31, 2005. Of those eligible men identified, 75% (n = 1,001) agreed to participate. Male residents of King County, Washington with no history of PCa were identified as a comparison group using one-step random digit telephone dialing with a clustering factor of five residences per sampling unit. Controls were frequency matched to cases by five-year age groups, and recruited evenly throughout the ascertainment period for cases. During the first step of random digit dialing, complete household census information was obtained for 81% of the 24,106 residential telephone numbers contacted. Of eligible control men who were identified, 63% (n = 942) completed the study interview.
Data Collection
Subjects completed in-person interviews conducted by trained interviewers. Information regarding demographic and lifestyle factors, medical and family history, and PCa screening in the previous 5 years (PSA and DRE) was collected. Subjects were asked questions about their hair pattern one year prior to age at reference date (date of diagnosis for cases and a randomly assigned date that approximated the distribution of cases' diagnosis dates for controls) and given show cards with different natural hair patterns (Figure 1). Subjects were also asked to describe their natural hair pattern at age 30 (little or no hair loss; loss at forehead only; loss at top of head and forehead). Subjects were asked about any use of finasteride (Proscar and Propecia), androgens and drugs which might interfere with androgen metabolism (anabolic steroids, ketoconozale and spironolactone).
Figure 1.
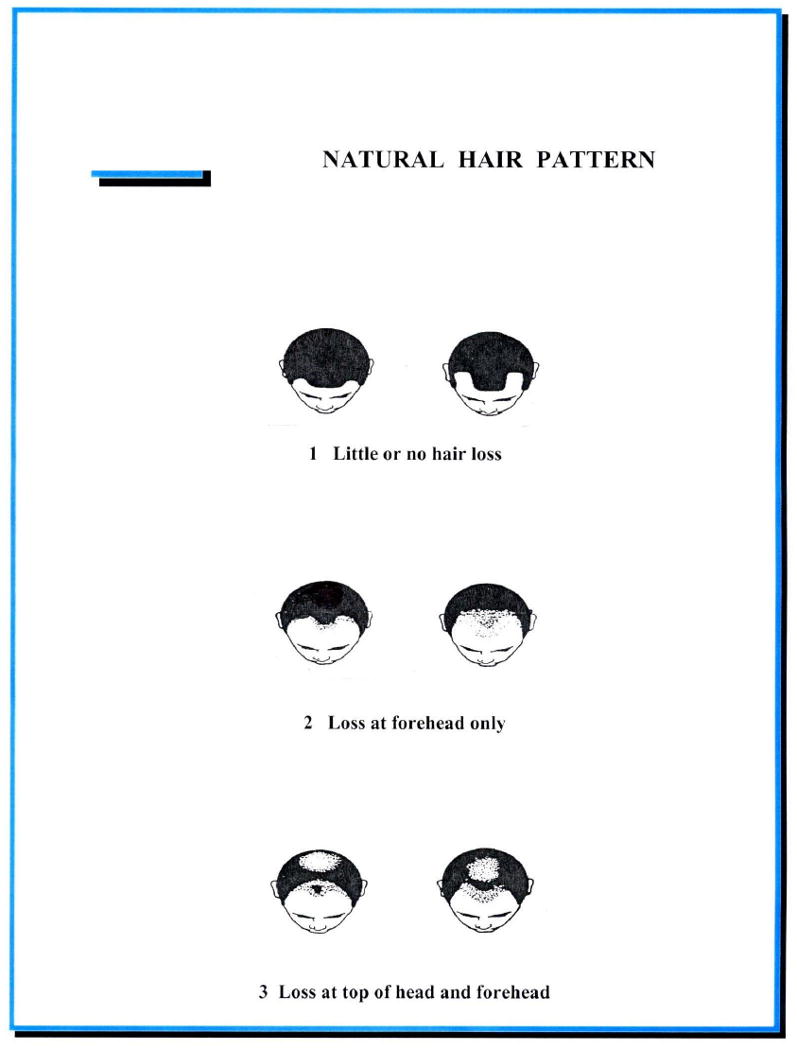
Showcard used for participants to identify their natural hair pattern at age 30 and at one year prior to referent age.
Statistical Analysis
In the primary analysis, 3 categories of hair pattern were created: little or no hair loss; any hair loss at age 30; and any hair loss at one year before referent age (with no hair loss reported at age 30). A second model was created with 5 hair pattern categories with “little or no hair loss” as the referent category and the other two hair patterns were evaluated independently within each age period assessed (age 30 and at referent age minus one).
The risk of PCa by hair patterns was evaluated with unconditional logistic regression. All models were adjusted for age (categorized in five-year age groups) as cases and controls were frequency matched by five-year age groups. A multivariate model was created adjusting for race, PSA screening history, family history of PCa, body mass index (BMI), and use of finasteride. We also evaluated as potential confounders a reported diagnosis of benign prostatic hyperplasia (BPH) or infertility and use of other medications that affect androgen levels (anabolic steroids, androgens, ketoconozale and spironolactone), however these did not alter the risk estimates significantly and were not included in the final model. A subset analysis was performed for men aged 60 or older at reference date to represent those with 30 years of “exposure” to their hair patterns at age 30. Odds ratios (OR) are presented along with 95% confidence intervals (95% CI). Polytomous regression was used to calculate risk estimates by disease aggressiveness (controls, less aggressive cases, more aggressive cases). Disease aggressiveness was based on a composite variable incorporating Gleason score, stage and PSA where more aggressive cases were defined by a Gleason score of 7(4+3) or greater, or non-localized stage, or PSA > 20 ng/mL at time of diagnosis. All statistical analyses were conducted using Stata software, Version 8 (Stata, Inc., College Station, TX).
Results
A total of 1,001 cases of incident prostate cancer and 942 controls were available for analysis. Two cases were missing hair pattern data: one case at age 30 and one case at one year before referent age. Both were excluded from the analysis. In Table 1, the distributions of various characteristics for cases and controls are shown for those with (a) no hair loss, (b) hair loss at age 30, and (c) hair loss at referent age minus one, but no hair loss at age 30. Early onset hair loss at age 30 was more common in Caucasians. For those reporting baldness only at one year before referent date, there was a trend of increasing hair loss reported with increasing age (ptrend < 0.001). 99% of men reporting hair loss at age 30 also reported hair loss at the referent age minus one. Approximately 55% of cases and controls, respectively, reported any hair loss in their 50s. For cases and controls aged 65 years or older, 66% and 74% reported any hair loss, respectively (data not shown).
Table 1. Characteristics of Population-Based Cases and Controls By Hair Loss Pattern at Age 30 Years and at One Year Before Reference Date.
| Cases | Controls | |||||
|---|---|---|---|---|---|---|
| No Hair Loss N (%) | Hair Loss at Age 30 N (%) | Hair Loss at Referent Age Only N (%) | No Hair Loss N (%) | Hair Loss at Age 30 N (%) | Hair Loss at Referent Age Only N (%) | |
| Subjects | 391 | 198 | 410 | 337 | 237 | 368 |
| Age at Reference Date (years) | ||||||
| 40 - 49 | 45 (11.5) | 22 (11.1) | 26 (6.3) | 44 (13.1) | 30 (12.7) | 22 (6.0) |
| 50 – 54 | 51 (13.0) | 27 (13.6) | 30 (7.3) | 49 (14.5) | 22 (9.3) | 42 (11.4) |
| 55 – 59 | 81 (20.7) | 39 (19.7) | 64 (15.6) | 80 (23.7) | 45 (19.0) | 49 (13.3) |
| 60 – 64 | 82 (21.0) | 42 (21.2) | 93 (22.7) | 68 (20.2) | 50 (21.1) | 69 (18.8) |
| 65 – 69 | 75 (19.2) | 33 (16.7) | 101 (24.6) | 58 (17.2) | 48 (20.3) | 96 (26.1) |
| 70 – 74 | 57 (15.9) | 35 (17.7) | 96 (23.4) | 38 (11.3) | 42 (17.7) | 90 (24.5) |
| Race | ||||||
| Caucasian | 328 (83.9) | 174 (87.9) | 339 (82.7) | 292 (86.7) | 221 (93.3) | 331 (90.0) |
| African-American | 63 (16.1) | 24 (12.1) | 71 (17.3) | 45 (13.4) | 16 (6.8) | 37 (10.1) |
| Family History of Prostate Cancer | ||||||
| No | 313 (80.1) | 149 (75.3) | 311 (75.9) | 297 (88.1) | 207 (87.3) | 329 (89.4) |
| Yes | 78 (20.0) | 49 (24.8) | 99 (24.2) | 40 (11.9) | 30 (12.7) | 39 (10.6) |
| PSA Screening History* | ||||||
| No PSA performed | 99 (25.3) | 45 (22.7) | 75 (18.3) | 102 (30.3) | 63 (26.6) | 75 (20.4) |
| 1 – 2 PSAs | 72 (18.4) | 40 (20.2) | 60 (14.6) | 59 (17.5) | 45 (19.0) | 64 (17.4) |
| ≥ 3 PSAs | 199 (50.9) | 101 (51.0) | 245 (60.0) | 113 (33.5) | 95 (38.8) | 175 (47.6) |
| Unknown | 21 (5.4) | 12 (6.1) | 30 (7.3) | 63 (18.7) | 37 (15.6) | 54 (14.7) |
| PSA | ||||||
| < 4.0 ng/mL | 49 (13.5) | 28 (14.5) | 56 (14.7) | 265 (94.0) | 186 (92.5) | 270 (88.8) |
| 4.0 – 9.9 ng/mL | 231 (63.5) | 127 (65.8) | 233 (61.3) | 15 (5.3) | 13 (6.5) | 27 (8.9) |
| > 10 ng/mL | 84 (23.1) | 38 (19.7) | 91 (24.0) | 2 (0.7) | 2 (1.0) | 7 (2.3) |
| BMI | ||||||
| Normal (< 25) | 108 (27.6) | 61 (30.8) | 118 (28.8) | 103 (30.6) | 59 (24.9) | 97 (26.4) |
| Overweight (25 – 29.9) | 197 (50.4) | 93 (47.0) | 201 (49.0) | 155 (46.0) | 110 (46.4) | 179 (48.6) |
| Obese (≥ 30) | 86 (22.0) | 44 (22.2) | 91 (22.2) | 79 (23.4) | 68 (28.7) | 92 (25.0) |
| Propecia Use | ||||||
| Never | 388 (99.2) | 195 (98.5) | 404 (98.5) | 336 (99.7) | 235 (99.2) | 361 (98.1) |
| Ever | 3 (0.8) | 3 (1.5) | 6 (1.5) | 1 (0.3) | 2 (0.8) | 7 (1.9) |
| Proscar Use | ||||||
| Never | 383 (98.0) | 192 (98.5) | 400 (98.3) | 331 (98.5) | 236 (99.6) | 361 (98.1) |
| Ever | 8 (2.1) | 3 (1.5) | 7 (1.7) | 5 (1.5) | 1 (0.4) | 7 (1.9) |
Number of PSA screening tests done within the 5-years before reference date
The mean age of PCa diagnosis in those without any hair loss reported was 60.2 (sd 7.9), which is similar to the mean age of those with hair loss at age 30 (mean age 60.8, sd 8.1). However, men who did not report early onset hair loss, but did report hair loss the year before referent date, were older at diagnosis (mean age 63.0, sd 7.4). This mean age was significantly higher than the mean age at diagnosis for the other two groups (both p-values < 0.001).
Table 2 shows the frequencies of MPB in cases and controls. Any hair loss by age 30 was reported in 19.8% of cases and 25.2% of controls (p = 0.005). Of PCa cases with hair loss reported at age 30, 64% had hair loss at the forehead only and 36% had hair loss at the top of the head and forehead. Controls reporting hair loss at age 30 had loss at the forehead only in 74% and loss at the top of head and forehead in 26%. In contrast, hair loss at referent age only did not differ significantly between cases (41%) and controls (39%).
Table 2. Relative Risk Estimates for Prostate Cancer According to Natural Hair Pattern.
| All Subjects | Age > 60 at Reference Date | |||||||
|---|---|---|---|---|---|---|---|---|
| Hair Pattern | Cases N (%) | Control N (%) | Age-Adjusted OR (95% CI) | Multivariate* OR (95% CI) | Cases N (%) | Controls N (%) | Age-Adjusted OR (95% CI) | Multivariate* OR (95% CI) |
| Little or no hair loss | 391 (39.1) | 337 (35.8) | 1.00 (referent) | 1.00 (referent) | 196 (34.5) | 148 (28.4) | 1.00 (referent) | 1.00 (referent) |
| Hair loss at age 30 | 198 (19.8) | 237 (25.2) | 0.72 (0.56 – 0.91) | 0.71 (0.56 – 0.91) | 108 (18.5) | 130 (25.0) | 0.61 (0.43 – 0.85) | 0.63 (0.45 – 0.90) |
| Loss at forehead only | 127 (44.7) | 157 (55.3) | 0.69 (0.52 – 0.91) | 0.69 (0.52 – 0.92) | 73 (46.2) | 85 (53.8) | 0.65 (0.44 – 0.95) | 0.68 (0.46 – 1.00) |
| Loss at top of head & forehead | 71 (47.0) | 80 (52.3) | 0.76 (0.53 – 1.09) | 0.75 (0.52 – 1.07) | 32 (41.6) | 45 (58.4) | 0.53 (0.32 – 0.88) | 0.55 (0.33 – 0.93) |
| Hair loss at one year before referent age ˆ | 410 (41.0) | 368 (39.1) | 0.95 (0.77 – 1.16) | 0.90 (0.73 – 1.12) | 267 (47.0) | 243 (46.6) | 0.83 (0.63 – 1.10) | 0.83 (0.62 – 1.10) |
| Loss at forehead only ˆ | 130 (49.3) | 133 (50.6) | 0.83 (0.63 – 1.11) | 0.79 (0.59 – 1.06) | 79 (49.7) | 80 (50.3) | 0.74 (0.51 – 1.08) | 0.73 (0.49 – 1.08) |
| Loss at top & forehead ˆ | 280 (54.4) | 235 (45.6) | 1.01 (0.80 – 1.28) | 0.97 (0.76 – 1.23) | 188 (53.6) | 163 (46.4) | 0.88 (0.65 – 1.08) | 0.88 (0.64 – 1.19 |
Adjusted for age at referent date, race, PSA screening history, family history of PCa, BMI and finasteride use
No hair loss reported at age 30
Table 2 also shows the results of the logistic regression. In the multivariate model, men with any significant hair loss at age 30 had a 29% risk reduction (OR 0.71, 95% CI 0.56 – 0.91) for PCa compared to those with no hair loss; whereas no difference in risk was seen in those with hair loss only at one year before referent age (OR 0.90, 95% CI 0.73 – 1.12). The relative risk reduction was greater when the analysis was restricted to men over the age of 60 years at reference date, with an approximately 40% reduction in the relative risk of PCa (OR 0.63, 95% CI 0.45 – 0.90) in men with early onset baldness. In the second multivariate model with “hair loss at forehead only” and “loss at top of head & forehead” considered separately, a 31% reduction in PCa risk was seen in those with “loss at forehead only” (OR 0.69, 95% CI 0.52 – 0.92). There was a non-significant reduction in the relative risk of PCa for those with “loss at top of head & forehead” at age 30 (OR 0.75, 95% CI 0.52 – 1.07). In the subset analysis of men over the age of 60 years at reference date, a 45% reduction in the risk of PCa was seen in those with “loss at top of head & forehead” compared to those with little/no hair loss (OR 0.55, 95% CI 0.33 – 0.93).
In the multivariate polytomous model, the relative risk reduction was present for both less aggressive and more aggressive PCa. Compared to those with no hair loss, men with any significant hair loss at age 30 had a reduction in the risk of less aggressive (OR 0.74, 95% CI 0.56 – 0.97) and more aggressive (OR 0.65, 95% CI 0.56 – 0.94) PCa. There was no difference between these risk estimates (p = 0.53).
Discussion
In this population-based, case-control study, we found that early onset MPB was associated with a reduced relative risk of PCa. These conditions share some similarities, including a high prevalence, age dependence, and association with androgens, as well as having an inherited susceptibility component. Despite these commonalities, limited research has been conducted to explore the relationship between MPB and subsequent risk of developing PCa. We found that early onset MPB was associated with a lower estimated relative risk of PCa. In our subset analysis of men aged 60 or older at the reference date, such that they would have the longest period of exposure reflected by early onset MPB, we observed a greater decrease in the relative risk (47% reduction) for men with loss of hair at the top of the head and forehead compared to those with loss of hair at the forehead only (35% reduction in risk). Our findings, if replicated, may provide an opportunity for adding this easily identifiable phenotypic trait of MPB to the risk stratification for PCa.
A small number of studies have explored the relationship between MPB and PCa risk showing either an increased relative risk13, 14 or no effect11, 12 on PCa risk in men with MPB. In a large case-control study of PCa from Australia, vertex balding was associated with a 50% increased relative risk of PCa.13 However, the investigators assessed MPB at the time of study entry (56% of cases and 57% of controls were over the age of 60) such that the prevalence of MPB was 77% and 75% in cases and controls, respectively. Given the long latency of prostate cancer and the presumed related effects of the androgen pathway in the pathogenesis of MPB and PCa, assessment of early-onset MPB may be a more relevant measure to evaluate for its potential association with subsequent PCa, which has a median age at diagnosis of 68 years.16 A study of MPB and PCa from the NHANES I cohort assessed MPB at study entry and followed participant for 18 years, finding an increased risk of PCa in men reporting MPB at study entry.14 However, given the wide range of ages of participants at entry, there was no standard baseline age assessment of exposure for the group and 50% were assessed at ages > 55. In our study, when looking at a comparable assessment time (age one year prior to reference date), we found no association between MPB and PCa risk (OR 0.95, 95% CI 0.77 – 1.16).
The relationship between androgens and MPB is clearly complex. Based on published data, 30% of men by age 30 have MPB.1 Similarly, in our control group, 25% reported early onset (age 30) MPB. Approximately 50% of controls in their 50s and 75% of men > 65 years of age reported baldness one year prior to reference date, which also agrees with published data.1 Thus the prevalence of MPB increases with age, while androgen levels are gradually falling.17 Yet androgens, particularly DHT, appear to have a critical role in the development of MPB. Inhibition of 5α-reductase type II, one of two isozymes responsible for the conversion of testosterone to DHT, slows the progression of, and in some cases partially reverses, MPB. The relative risk of MPB has been associated with specific polymorphisms in the AR gene in some studies3, 4 and with polymorphisms in the gene encoding 5α-reductase type II.18 Biopsies of balding scalps showed elevated levels of both type I and II 5α-reductase enzyme expression and AR by immunohistochemistry compared to non-balding regions of the scalp.19 Similarly, frontal/vertex scalp and hair levels of DHT are higher in balding men compared to controls7, 20 and treatment with finasteride decreases scalp DHT levels.21, 22 However, new evidence supports the concept that androgens may not be the only contributor to MPB. Two recent genome-wide association studies of MPB found a susceptibility locus in a coding region on chromosome 20p11,5, 6 suggesting that a yet unidentified, perhaps androgen-independent pathway, may play a critical role in MPB.
The relationship between androgens and PCa is also complex. Maintaining an intact and functional androgen signaling axis is necessary for differentiation of prostate epithelium.23 DHT is the dominant androgen within the prostate and binds the AR with higher affinity than testosterone.24 The relationship between DHT, prostate homeostasis and MPB can be assessed indirectly from studies of men with 5α-reductase deficiency. These men have small prostates and they do not develop MPB or PCa.25, 26 In addition, men with enlarged prostates given 5α-reductase inhibitors (i.e., finasteride) experience a reduction in prostate size and increased scalp hair.8, 27 A few investigators have explored the relationship between benign prostatic hyperplasia (BPH) and MPB and found higher rates of MPB in men with larger prostates.28, 29 Moreover, multiple studies have failed to find an association between circulating androgen levels and the risk of PCa 30-32 and, like MPB, PCa cancer incidence increases directly with age and is most frequent in men > 65 years of age, when androgen levels are at their lowest since puberty even in otherwise healthy older men.17
There are a number of possible explanations for the apparent contradiction between the effects of 5α -reductase inhibitors, which treat both MPB and BPH presumably by lowering DHT levels, and the results presented here showing an inverse relationship between MPB and risk of PCa. First, our findings are consistent with those of Hayes et al. who found that an allelic variant of the 5α -reductase type II gene was associated with an increased relative risk of PCa and a decreased relative risk of MPB,18 suggesting that the expression of these isozymes might have tissue-specific effects. Secondly, while treatment with a 5α-reductase inhibitor has modest effects on serum hormone levels, within the prostate it not only lowers DHT but raises testosterone concentrations 7 to10-fold.33 Thus, tissue-specific effects on the hormonal environment, or tissue specific coactivators/repressors of androgen action might play a role in determining the impact of hormonal manipulation within a given tissue microenvironment. Finally, tissue-specific, non-androgen regulated processes likely play a role in MPB and the development of PCa.
Our study has a number of strengths in comparison to some prior studies of MPB and PCa, namely improved power to evaluate MPB, avoidance of the potential biases of some study designs, and use of a consistent exposure measurement of early-onset MPB (at age 30). However, there are limitations that should be considered, including the potential for recall and selection bias. Men at the reference date were asked to recall their natural hair pattern at age 30 and misclassification is possible. However, 30% of men from other studies reported early onset (age 30) MPB similar to the frequency reported in our controls (25%). In addition, self-reported MPB may be less reliable than that determined by trained personnel, but self-assessment of both current and retrospective hair patterns has been found to be reliable.34 Yet, recall bias cannot be excluded and photographs of participants at age 30 to confirm their hair pattern were not available. The prevalence of self-reported finasteride use (either as Proscar or Propecia) was 3.0% and 2.4% in cases and controls, respectively. This may represent underreporting of use which could alter the risk estimates considering the effects of finasteride on both MPB and PCa. However, in a separate analysis of a subset of this study population that was designed to validate use of statin medications, there was 87% agreement between self-reported use and computerized pharmacy records.15 Finally, although participation levels were 75% for cases and 63% for controls, we cannot exclude the possibility of selection bias such that those who agreed to be in the study had different hair patterns than those who chose not to participate.
In conclusion, in this population-based, case-control study of PCa, we found early-onset MPB (at age 30) to be associated with a statistically significant 28% to 39% reduction in the relative risk of PCa. If our findings of an inverse association between these two common, androgen-related male conditions are confirmed, the easily identifiable phenotypic trait of early onset MBP may assist in the identification of men at lower risk for subsequent PCa.
Acknowledgments
NIH Grants: R01 CA 56678; R01 CA 092579; R01 CA097186, T32 CA009168-30; with additional support from the Fred Hutchinson Cancer Research Center.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ellis JA, Sinclair R, Harrap SB. Androgenetic alopecia: pathogenesis and potential for therapy. Expert Rev Mol Med. 2002;4(22):1–11. doi: 10.1017/S1462399402005112. [DOI] [PubMed] [Google Scholar]
- 2.Nyholt DR, Gillespie NA, Heath AC, Martin NG. Genetic basis of male pattern baldness. J Invest Dermatol. 2003;121(6):1561–4. doi: 10.1111/j.1523-1747.2003.12615.x. [DOI] [PubMed] [Google Scholar]
- 3.Ellis JA, Stebbing M, Harrap SB. Polymorphism of the androgen receptor gene is associated with male pattern baldness. J Invest Dermatol. 2001;116(3):452–5. doi: 10.1046/j.1523-1747.2001.01261.x. [DOI] [PubMed] [Google Scholar]
- 4.Hayes VM, Severi G, Eggleton SA, Padilla EJ, Southey MC, Sutherland RL, et al. The E211 G>A androgen receptor polymorphism is associated with a decreased risk of metastatic prostate cancer and androgenetic alopecia. Cancer Epidemiol Biomarkers Prev. 2005;14(4):993–6. doi: 10.1158/1055-9965.EPI-04-0778. [DOI] [PubMed] [Google Scholar]
- 5.Hillmer AM, Brockschmidt FF, Hanneken S, Eigelshoven S, Steffens M, Flaquer A, et al. Susceptibility variants for male-pattern baldness on chromosome 20p11. Nat Genet. 2008;40(11):1279–81. doi: 10.1038/ng.228. [DOI] [PubMed] [Google Scholar]
- 6.Richards JB, Yuan X, Geller F, Waterworth D, Bataille V, Glass D, et al. Male-pattern baldness susceptibility locus at 20p11. Nat Genet. 2008;40(11):1282–4. doi: 10.1038/ng.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bang HJ, Yang YJ, Lho DS, Lee WY, Sim WY, Chung BC. Comparative studies on level of androgens in hair and plasma with premature male-pattern baldness. J Dermatol Sci. 2004;34(1):11–6. doi: 10.1016/j.jdermsci.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Gormley GJ, Stoner E, Bruskewitz RC, Imperato-McGinley J, Walsh PC, McConnell JD, et al. The effect of finasteride in men with benign prostatic hyperplasia. The Finasteride Study Group. N Engl J Med. 1992;327(17):1185–91. doi: 10.1056/NEJM199210223271701. [DOI] [PubMed] [Google Scholar]
- 9.Delongchamps NB, Singh A, Haas GP. The role of prevalence in the diagnosis of prostate cancer. Cancer Control. 2006;13(3):158–68. doi: 10.1177/107327480601300302. [DOI] [PubMed] [Google Scholar]
- 10.Thompson IM, Goodman PJ, Tangen CM, Lucia MS, Miller GJ, Ford LG, et al. The influence of finasteride on the development of prostate cancer. N Engl J Med. 2003;349(3):215–24. doi: 10.1056/NEJMoa030660. [DOI] [PubMed] [Google Scholar]
- 11.Demark-Wahnefried W, Lesko SM, Conoway MR, RObertson CN, Clark RV, Lobaugh B, et al. Serum androgens: associations with prostate cancer risk and hair patterning. J Andro. 1997;18(5):495–500. [PubMed] [Google Scholar]
- 12.Denmark-Wahnefried W, Schildkraut JM, Thompson D, Lesko SM, McIntyre L, Schwingl P, et al. Early onset baldness and prostate cancer risk. Cancer Epidemiol Biomarkers Prev. 2000;9(3):325–8. [PubMed] [Google Scholar]
- 13.Giles GG, Severi G, Sinclair R, English DR, McCredie MR, Johnson W, et al. Androgenetic alopecia and prostate cancer: findings from an Australian case-control study. Cancer Epidemiol Biomarkers Prev. 2002;11(6):549–53. [PubMed] [Google Scholar]
- 14.Hawk E, Breslow RA, Graubard BI. Male pattern baldness and clinical prostate cancer in the epidemiologic follow-up of the first National Health and Nutrition Examination Survey. Cancer Epidemiol Biomarkers Prev. 2000;9(5):523–7. [PubMed] [Google Scholar]
- 15.Agalliu I, Salinas CA, Hansten PD, Ostrander EA, Stanford JL. Statin use and risk of prostate cancer: results from a population-based epidemiologic study. Am J Epidemiol. 2008;168(3):250–60. doi: 10.1093/aje/kwn141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ries L, Melbert D, Krapcho M, Stinchcomb D, Howlader N, Horner M, et al. In: SEER Cancer Statistics Review, 1975-2005, based on November 2007 SEER data submission, posted to the SEER web site. Institute NC, editor. Bethesda, MD: 2008. [Google Scholar]
- 17.Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Baltimore Longitudinal Study of Aging. J Clin Endocrinol Metab. 2001;86(2):724–31. doi: 10.1210/jcem.86.2.7219. [DOI] [PubMed] [Google Scholar]
- 18.Hayes VM, Severi G, Padilla EJ, Morris HA, Tilley WD, Southey MC, et al. 5alpha-Reductase type 2 gene variant associations with prostate cancer risk, circulating hormone levels and androgenetic alopecia. Int J Cancer. 2007;120(4):776–80. doi: 10.1002/ijc.22408. [DOI] [PubMed] [Google Scholar]
- 19.Sawaya ME, Price VH. Different levels of 5alpha-reductase type I and II, aromatase, and androgen receptor in hair follicles of women and men with androgenetic alopecia. J Invest Dermatol. 1997;109(3):296–300. doi: 10.1111/1523-1747.ep12335779. [DOI] [PubMed] [Google Scholar]
- 20.Choi MH, Yoo YS, Chung BC. Biochemical roles of testosterone and epitestosterone to 5 alpha-reductase as indicators of male-pattern baldness. J Invest Dermatol. 2001;116(1):57–61. doi: 10.1046/j.1523-1747.2001.00188.x. [DOI] [PubMed] [Google Scholar]
- 21.Camacho FM, Garcia-Hernandez MJ, Fernandez-Crehuet JL. Value of hormonal levels in patients with male androgenetic alopecia treated with finasteride: better response in patients under 26 years old. Br J Dermatol. 2008;158(5):1121–4. doi: 10.1111/j.1365-2133.2008.08509.x. [DOI] [PubMed] [Google Scholar]
- 22.Ryu HK, Kim KM, Yoo EA, Sim WY, Chung BC. Evaluation of androgens in the scalp hair and plasma of patients with male-pattern baldness before and after finasteride administration. Br J Dermatol. 2006;154(4):730–4. doi: 10.1111/j.1365-2133.2005.07072.x. [DOI] [PubMed] [Google Scholar]
- 23.Cunha GR, Ricke W, Thomson A, Marker PC, Risbridger G, Hayward SW, et al. Hormonal, cellular, and molecular regulation of normal and neoplastic prostatic development. J Steroid Biochem Mol Biol. 2004;92(4):221–36. doi: 10.1016/j.jsbmb.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 24.Keller ET, Ershler WB, Chang C. The androgen receptor: a mediator of diverse responses. Front Biosci. 1996;1:d59–71. doi: 10.2741/a116. [DOI] [PubMed] [Google Scholar]
- 25.Imperato-McGinley J, Zhu YS. Androgens and male physiology the syndrome of 5alpha-reductase-2 deficiency. Mol Cell Endocrinol. 2002;198(1-2):51–9. doi: 10.1016/s0303-7207(02)00368-4. [DOI] [PubMed] [Google Scholar]
- 26.Zhu YS, Sun GH. 5alpha-Reductase Isozymes in the Prostate. J Med Sci. 2005;25(1):1–12. [PMC free article] [PubMed] [Google Scholar]
- 27.Kaufman KD, Olsen EA, Whiting D, Savin R, DeVillez R, Bergfeld W, et al. Finasteride in the treatment of men with androgenetic alopecia. Finasteride Male Pattern Hair Loss Study Group. J Am Acad Dermatol. 1998;39(4 Pt 1):578–89. doi: 10.1016/s0190-9622(98)70007-6. [DOI] [PubMed] [Google Scholar]
- 28.Chen W, Yang CC, Chen GY, Wu MC, Sheu HM, Tzai TS. Patients with a large prostate show a higher prevalence of androgenetic alopecia. Arch Dermatol Res. 2004;296(6):245–9. doi: 10.1007/s00403-004-0514-z. [DOI] [PubMed] [Google Scholar]
- 29.Oh BR, Kim SJ, Moon JD, Kim HN, Kwon DD, Won YH, et al. Association of benign prostatic hyperplasia with male pattern baldness. Urology. 1998;51(5):744–8. doi: 10.1016/s0090-4295(98)00108-3. [DOI] [PubMed] [Google Scholar]
- 30.Barrett-Connor E, Garland C, McPhillips JB, Khaw KT, Wingard DL. A prospective, population-based study of androstenedione, estrogens, and prostatic cancer. Cancer Res. 1990;50(1):169–73. [PubMed] [Google Scholar]
- 31.Mohr BA, Feldman HA, Kalish LA, Longcope C, McKinlay JB. Are serum hormones associated with the risk of prostate cancer? Prospective results from the Massachusetts Male Aging Study. Urology. 2001;57(5):930–5. doi: 10.1016/s0090-4295(00)01116-x. [DOI] [PubMed] [Google Scholar]
- 32.Roddam AW, Allen NE, Appleby P, Key TJ. Endogenous sex hormones and prostate cancer: a collaborative analysis of 18 prospective studies. J Natl Cancer Inst. 2008;100(3):170–83. doi: 10.1093/jnci/djm323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Norman RW, Coakes KE, Wright AS, Rittmaster RS. Androgen metabolism in men receiving finasteride before prostatectomy. J Urol. 1993;150(5 Pt 2):1736–9. doi: 10.1016/s0022-5347(17)35882-2. [DOI] [PubMed] [Google Scholar]
- 34.Taylor R, Matassa J, Leavy JE, Fritschi L. Validity of self reported male balding patterns in epidemiological studies. BMC Public Health. 2004;4:60. doi: 10.1186/1471-2458-4-60. [DOI] [PMC free article] [PubMed] [Google Scholar]


