Abstract
Objective
The aim of the study was to examine the association of religious education and observance with dementia among participants in the Israeli Ischemic Heart Disease study.
Study Design and Setting
We assessed dementia in 1,890 participants among 2,604 survivors of 10,059 participants in the Israeli Ischemic Heart Disease study, a longitudinal investigation of the incidence and risk factors for cardiovascular disease among Jewish male civil servants in Israel. Face-to-face interviews were conducted with 651 subjects identified as possibly demented by the Modified Telephone Interview for Cognitive Status.
Results
Of 1,628 subjects included in this analysis (mean age 82 at assessment), 308 (18.9%) had dementia. The prevalence rates of dementia (and odds ratios (ORs) relative to those with exclusively religious education, adjusted for age, area of birth, and socioeconomic status) were 27.1% for those with exclusively religious education, 12.6% (OR=0.49) for those with mixed education, and 16.1% (OR=0.76) for those with secular education. For religious self-definition and practice, the prevalence rates were 9.7%, 17.7%, 14.1%, 19.3%, and 28.8% for categories from least to most religious (ORs relative to the most religious: 0.43, 0.67, 0.48, 0.55).
Conclusions
Examining lifestyles associated with religiosity might shed light onto environmental risks for dementia. Mechanisms underlying these associations remain elusive.
Keywords: Religion, Dementia, Life style, Education, Risk factors, Prevalence
1. Introduction
Epidemiological evidence suggests that modifiable life style factors, such as diet [1], physical, social, and intellectual activity, are associated with cognitive performance and dementia (summarized in [2]). These life style factors are interrelated with other nonmodifiable factors such as genetic predisposition, which increase the risk for cognitive decline and dementia [3]. Orthodox Jewish men lead a lifestyle, which in many aspects differs from nonreligious individuals. They follow strict dietary rules (kashrut), exercise life-long preference for scholarly activity rather than physical activity, and might under-use medical services [4]. These cultural differences suggest potentially different prevalence and incidence of disease states, including dementia, among orthodox Jews compared to nonorthodox Jews.
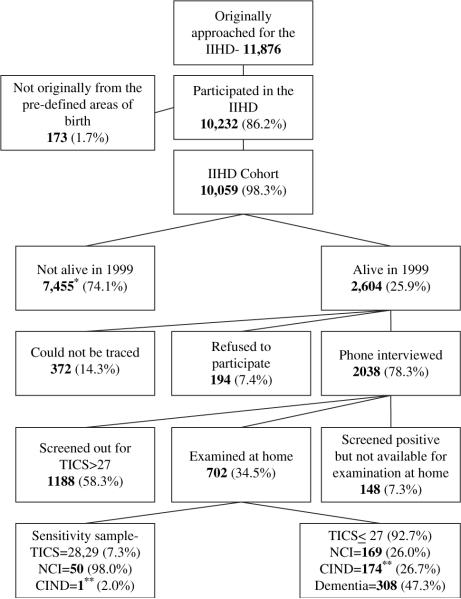
Few studies examined the association between religious lifestyle and cognitive impairment and decline, and to the best of our knowledge, none have examined the association between religious lifestyle and full-fledged dementia. In a large sample of community dwelling elderly followed longitudinally for cognitive decline, the association between religious attendance and cognitive decline varied according to the follow-up period [5]. Religious attendance was associated with better cognitive function in a religiously diverse elderly cohort [6] and with slower cognitive decline [7] in a Mexican American elderly cohort. The preponderance of evidence from the few studies conducted led us to test the hypothesis that orthodox Jews will have a lower prevalence of dementia than nonorthodox Jews in surviving participants in the Israeli Ischemic Heart Disease (IIHD) study (Fig. 1). The IIHD examined 10,232 male Israeli civil servants and municipal employees for cardiovascular disease and its risk factors in 1963, 1965, and 1968.
Fig. 1.
Flow of subjects. *This number consists of 7,136 who died before 1999, 306 who died before they could be interviewed in the 1999 follow up, and 13 who were lost in the matching process. **Not included in the analyses.
What is new?
Among the 20% of surviving men in a largely migrant cohort, initially interviewed in 1965 at age >40 year, the prevalence of dementia in 1999/2000 was 29% in those who had proclaimed themselves to be religiously orthodox. Survivors exposed to an exclusively religious education exhibited similar relations. Previous examinations of rates of dementia with religious related factors have led to diverse conclusions. The conceptualization of religiosity might differ between different faiths and between migrant populations and those living in the same territory for generations.
2. Methods
2.1. Subjects
The IIHD Project (n=11,876) was chosen by stratified sampling of civil servants and municipal employees in 1963 based on (1) men aged 40–65 at the time of inclusion, (2) place of work limited to the three largest urban areas in Israel (Tel-Aviv, Jerusalem, and Haifa), and (3) sampling fractions aimed at obtaining numbers of study subjects from six geographical areas of origin (Central Europe, Eastern Europe, the Balkan countries, the Middle East, Northern Africa, and Israeli born) approximately proportional to the Israeli male population of these ages. 10,232 (86.2%) men agreed to participate. Subjects were seen upon enrollment (1963) and at two follow-up visits (1965 and 1968). Subsequent analyses excluded 173 men who were not born in the six predefined geographical areas. According to the Israel Mortality Registry, 7,136 men died by the beginning of the study in 1999; another 306 died before being approached for a phone interview and 13 subjects were lost in the matching process. The remaining 2,604 subjects qualified for a telephone interview, of which 2,038 had phone contact. The telephone screening (described below) identified 799 potentially demented subjects for a home interview. Of these, 148 could not be examined. Of the remaining 1239 subjects who were not identified as potentially demented by the TICS-m, 51 were examined at home for a sensitivity study of the phone interview instruments; 50 were cognitively intact and one cognitively impaired but not demented [8]. The remaining 1,188 subjects were classified as nondemented. Thus, the follow-up study characterized the presence or absence of dementia in 1,890 subjects: 308 were demented, 175 had cognitive impairment not sufficient to meet diagnostic criteria for dementia (cognitively impaired not demented—CIND [9]), and 1,407 elderly had no cognitive impairment.
A comparison of the characteristics of the subjects alive in 1999 to those who died since 1963 has been published [10]. The 2,604 subjects who were alive in 1999 were younger, and taking age differences into account, were taller and had had lower BMI, total serum cholesterol, systolic and diastolic blood pressures, in the initial examinations, than the 7,455 who had died by this time. Fewer survivors had begun follow up with diabetes and fewer had smoked cigarettes. A greater proportion of Eastern European born and a smaller one of those born in the Middle East survived, and the survivors represent higher socioeconomic status (SES).
2.2. Diagnosis of dementia
Cases of dementia were identified using a two-step procedure as described in detail elsewhere [8,10]. The first step was a screening interview over the phone. For the purpose of the screening phone interview, subjects were located by cross-linking the data base of the original study [11] with the population registry of the Israel Ministry of Interior, using the ID number (equivalent of U.S. social security number) as linking identifier. All identified living participants in the original cohort were phoned, reminded of their participation in the original study, and asked for consent to participate in the new assessment. The subjects who consented to participate were administered a 20-min phone interview, including a sociodemographic questionnaire and the Hebrew version of the Modified Telephone Interview for Cognitive Status (TICS-m [8]). The sociodemographic questionnaire included items that were not recorded during the original study in 1963, or that might have changed with time, such as marital status, retirement age, education, profession, leisure activities, smoking, and drinking habits.
The TICS-m is based on the Mini Mental State Exam (MMSE [12]). It includes questions assessing long and short-term memory, orientation to time and place, attention, language and abstraction. The scores of the TICS-m were highly correlated with the MMSE scores in clinical studies [13] and in the Hebrew version in this cohort [8]. Using a threshold score of 27 out of 50 TICS-m points, the sensitivity of this test was above 99% (CI 95%, 91%–100%) and the specificity was 86% (CI 95%, 85%–87%) for dementia [14].
The second step was a face-to-face interview for all subjects with a TICS-m score of 27 or lower. The aim of the second phase of the study was to ascertain the diagnosis of dementia among subjects who were identified by the TICS-m as possibly cognitively impaired. The patients were assessed at their residences by a physician. All physicians involved in this study were neurologists or psychiatrists with expertise and extensive experience in the diagnosis of dementia. Physicians were blind to the TICS-m score except for knowledge that it was under 28. The clinical assessment included the Dementia Questionnaire (DQ [15,16]), MMSE [12,17], Global Deterioration Scale[18], and the Hachinski Ischemic Scale[19].
For persons with suspected dementia, the DQ assesses, through informants, the symptoms, course, and feature of the dementia, permitting a diagnostic classification for the presence and likely type of dementia. The DQ has previously demonstrated good interinformant and interrater agreement in Alzheimer's disease (AD) probands and normal elderly control populations for detecting the presence or absence of dementia and also, among identified cases of dementia, the type of dementia [15,16]. More recently, several investigations have assessed the validity of this instrument [17]. Compared with a clinical assessment of dementia, the DQ was found to have excellent sensitivity (100%; CI 73%–100%) and very good specificity (90%; CI 63%–100%) [20,21]. In addition, in a series of deceased autopsied elderly, informant-based DQ were compared with independent neuropathological examinations; for AD, the DQ was found to be only slightly less sensitive than direct clinical assessment and its specificity was virtually at the same level [22].
Dementia was diagnosed using the DSM-IV criteria [23]. Subjects were classified as CIND if a memory problem was reported by both subject and informant but they had normal activities of daily living and were not demented. Thus, CIND subjects did not qualify as either demented or no cognitive impairment. The present analysis compares unequivocally demented to unequivocally nondemented subjects, excluding the CIND subjects, who are heterogeneous, with some subjects early in the course of cognitive decline.
A second physician, blind to the diagnosis assigned by the physician who did the face-to-face interview, examined the data gathered from each patient and assigned an independent diagnosis. In case of disagreement between the two physicians the case was presented to a third physician for a consensus diagnosis. In five cases, the patient was approached again for this purpose.
2.3. Assessment of religious self-definition and practice and type of education
Two variables in the original 1963 questionnaire were relevant to religion. Subjects were asked to report if their formal schooling contained either exclusively religious or exclusively secular education, or both types of education (mixed education). The other variable defines the extent of religiosity according to belief and practice on a scale from 1 to 5, in 1965, as follows: (1) The most strict observance of religious rules defines a group named “Haredim” who are distinguished from the rest of the population by their way off dressing, maintaining all the rules of the Jewish “Halakha” to the letter, including most severe demands of Kosher food production and certification, many rules related to married life and practice, keeping all the rules related to the Sabbath (non use of transportation and other mechanized or electric aspects), complete absence of the girls from military service as well as of a large percentage of the boys. In the 1950s and 1960s they also avoided voting in general and local election to a great degree. (2) The “religious” group resembles the former in terms of obeying the Halakha, but differ considerably from the former as unlike them they consist an integral part of the Zionist Israeli Society. They played a significant part in establishing the original Moshavim and Kibbutzim (Israeli specific communities) in preindependence Israel and they and their sons routinely did army service. They also keep strict Kashrut. Quite unlike Haredim they do not reside in a concentrated manner in specific areas of specific townships and with the exception of the Kippa (the small hat) they dress like other persons. (3) The traditional group represents men who are close to the religion but do not pray daily, might travel on the Sabbath, go to theatre or movie theatre and use electricity. Some of them attend service on Rosh Hashanah and Yom Kippur, but not in a regular manner otherwise. Their daughters normally do not abstain from army service on claims of religious orthodoxy. (4) “Secular” represent those who eat freely, disregarding most limitations imposed by the old religious interpretation, and engaging in other activities on the Sabbath, and lived a quasiwestern world mode of life at the time of examination. (5) The part of the latter who declared themselves to be “nonbelievers” were categorized as “agnostic.”
These two categorical variables were the primary independent variables of this study. Extent of religiosity is presented in the tables as group 1 agnostic to group 4 religious and the orthodox subjects (group 5) are the reference group.
Definition of covariates
In addition to age, we controlled for SES (represented by a five-point index based on education [nine levels ranging from no formal schooling to a graduate degree] and occupation [five levels ranging from “laborer” to “professional”] [24]), and area of birth (Israel, East Europe, Central Europe, Balkan countries, Middle East, and North Africa). In secondary analysis, we also controlled for seven clinical and behavioral risk factor variables because of the evidence that such variables are associated with dementia [25–27]. Diagnosis of diabetes was based on serum glucose levels (collected for all subjects in the IIHD study) with an oral glucose tolerance test when indicated, or on use of oral hypoglycemic/insulin therapy or clinical history of diabetes confirmed by the primary care physician. A man diagnosed with diabetes at any of the three visits (1963, 1965, and 1968) was classified as diabetic. Weight (to the nearest kilogram wearing trousers only) was defined as the average of the three visits. Height (to the nearest centimeter without shoes) was measured only in 1963. Smoking habits in 1963 were categorized as a dichotomy—ever and never smoked. Systolic and diastolic blood pressure were measured in the right arm, with the subject in the recumbent position, both 30–45 min after arrival at the clinic and 15–30 min later. The average of the second blood pressure measure, over the three visits, was used in this analysis. Total cholesterol, measured by the Anderson and Keys method [28], was calculated as the average of the three visits.
2.4. Statistical analysis
Confidence intervals for the estimated rates of dementia in categories of qualitative variables and continuous variables were computed using standard deviations elicited from clustered observation, with the center of examination as the cluster. We estimated the odds of dementia prevalence associated with exclusively secular and with mixed education, relative to exclusively religious education; and with the different categories of religious self perception and practice relative to the most religious one, using both logistic regression analysis and the Mantel–Haenszel method. Three sociodemographic variables were controlled for. In addition, in subsidiary analyses, men with exclusively religious education were compared to the combination of the other two categories, and those with extreme religious self-definition and practice were compared with the combination of the other four levels of religious self definition and practice. Goodness of fit for the logistic regression analysis was tested by the Hosmer and Lemeshow method [29]. Stata version 9.2 and SPSS version 13.0 were used for data analyses.
3. Results
Table 1 describes the characteristics of the three stages of attrition leading from the original 9,245 with data on religious variables known in 1965, via the demise of most stud subjects over the long-term follow up and leading to those approachable in 1999/2000, and finally to those assessed for dementia. Subjects approached or assessed for dementia in 1999/2000 were approximately 5 years younger than all subjects with religion variables known in 1965. Those assessed had higher SES than those approached in 1999/2000, who in turn had higher SES than those with religion related variables in 1965. Approachable subjects were more likely to have been born in the Middle East and North Africa and less likely to have been born in Europe than the other groups. Approachable and assessed subjects had lower rates of extreme religious self definition and practice, and those assessed had a lower rate of exclusively religious education than the other groups.
Table 1.
Sociodemographic and religion characteristics of all subjects in 1965, those approachable in 1999, and those assessed for dementia
| Variable | All subjects; (N = 9,245 with religiosity known) | Approachable by 1999/2000; (N = 2604) | Assessed for dementia; (N = 1890) |
|---|---|---|---|
| Age, Mean (SD) | 49.2 (6.7) | 44.8 (4.3) | 44.5 (4.1) |
| Socioeconomic status, Mean (SD) | 2.59 (1.24) | 2.68 (1.20) | 2.76 (1.18) |
| Born in Israel | 14.0 % | 13.6% | 13.6% |
| Born in Europe | 50.5% | 46.9% | 48.6% |
| Born Middle East and North Africa | 35.4% | 39.6% | 37.8% |
| Extreme religious self-definition and practice | 22.8% | 20.6% | 20.0% |
| Exclusively religious education | 32.4% | 32.1% | 30.2% |
Table 2 shows the sociodemographic, clinical, and behavioral characteristics associated with subjects whose upbringing had been exclusively religious and with the most extreme religious self-definition and practice. Although there was a strong overlap for extreme religious education and observance using the two dichotomies (r = .43), notwithstanding, their respective associations with other variables were somewhat different, most strikingly for smoking and diabetes. Subjects with exclusively religious education and also subjects with extreme religious self-definition and practice had lower SES, lower total cholesterol, weight, and height; compared to subjects whose education was not exclusively religious or those with less than extreme religious self definition and practice, respectively. The former also included a greater proportion of men emigrating from North Africa. Subjects who perceived themselves as extremely religious had lower rates of smoking compared to subjects whose self-definition was less orthodox. Subjects with exclusively religious education had lower rates of diabetes compared to those with education that was not exclusively religious. Exclusively religious education and extreme religious self-definition were not associated with age, systolic and diastolic blood pressure.
Table 2.
| Exclusively religious education; (n = 482) | Not exclusively religious education; (n = 1167) | P-value | Extreme religious self definition and practice; (n = 312) | Less extreme religious self definition and practice; (n = 1323) | P-value | |
|---|---|---|---|---|---|---|
| Extremely religious self-perception (%) | 49.5 (n = 215) | 9.1 (n = 94) | < 0.0005 | – | – | – |
| Exclusively religious education (%) | – | – | – | 70.3 (n = 215) | 20.0 (n = 259) | < 0.0005 |
| Age–1963 (mean) | 44.7 (4.1) | 44.2 (4.0) | 45.1 (4.1) | 44.3 (4.0) | ||
| Dementia (%) | 27.2 (n = 131) | 14.1 (n = 165) | < 0.001 | 28.8 (n = 90) | 15.2 (n = 201) | < 0.001 |
| Diabetic–1963/5/8 (%) | 1.6 (n = 10) | 2.6 (n = 33) | < 0.001 | 2.6 (n = 10) | 2.3 (n = 35) | 0.47 |
| Weight–1963/5/8 (kg) | 70.6 (10.2) | 73.0 (9.4) | < 0.001 | 70.9 (10.8) | 72.6 (10.0) | < 0.001 |
| Height–1963 (cm) | 167.1 (6.5) | 168.8 (6.4) | < 0.001 | 167.1 (6.7) | 168.6 (6.3) | < 0.001 |
| Cholesterol–1963/5/8 (mean) | 198.0 (29.4) | 204.6 (29.9) | < 0.001 | 193.6 (28.8) | 204.8 (29.8) | < 0.001 |
| Systolic blood pressure–1963/5/8 (mean) | 129.0 (13.7) | 129.8 (13.3) | 0.23 | 129.6 (12.8) | 129.6 (13.6) | 0.81 |
| Diastolic blood pressure–1963/5/8 (mean) | 82.8 (8.0) | 82.5 (8.1) | 0.18 | 82.6 (7.6) | 82.5 (8.2) | 0.26 |
| % Ever smoked–1963 | 56.4 (n = 288) | 61.5 (n = 733) | 0.31 | 43.0 (n = 150) | 64.4 (n = 861) | < 0.001 |
| SES (%) (1 = low to 5 = high) | 2.06 (1.21) | 3.06 (1.13) | < 0.001 | 2.61 (1.31) | 3.00 (1.13) | < 0.001 |
| Area of birth (%) | ||||||
| Israel | 16.6 (n = 80) | 13.2 (n = 155) | < 0.001 | 14.6 (n = 46) | 14.2 (n = 188) | < 0.001 |
| Eastern Europe | 12.6 (n = 63) | 18.3 (n = 212) | 9.7 (n = 30) | 18.2 (n = 240) | ||
| Central Europe | 15.7 (n = 76) | 16.9 (n = 195) | 21.1 (n = 65) | 15.4 (n = 203) | ||
| Balkan Countries | 13.2 (n = 63) | 17.4 (n = 206) | 14.9 (n = 46) | 16.6 (n = 220) | ||
| Middle East | 24.5 (n = 118) | 24.4 (n = 283) | 21.8 (n = 68) | 24.9 (n = 330) | ||
| North Africa | 17.4 (n = 82) | 9.8 (n = 116) | 17.9 (n = 57) | 10.8 (n = 142) | ||
Diabetes, weight, height, cholesterol, systolic and diastolic blood pressure, and smoking are age adjusted.
Numbers in parenthesis represent standard deviation except when otherwise stated (counts).
T-test was used to compare groups on SES, weight, height, cholesterol, systolic and diastolic blood pressure. Chi-squared test was used for dementia, diabetes, smoking, and area of birth.
The prevalence rates of dementia were 27.1% for those with exclusively religious education, 12.6% for those with mixed education and 16.1% for those with secular education. The odds of dementia adjusted for age, SES, and area of birth were decreased in men whose education was not exclusively religious (odds ratio [OR] = 0.58, Table 3). Those with mixed education (OR = 0.49) and those with only secular education (OR = 0.76), each had less dementia than those with exclusively religious education. Further controlling for smoking, diabetes, body weight and height, blood pressure, and serum cholesterol, resulted in a negligible effect on the estimated odds ratios of dementia in the nonexclusively religious upbringing groups, compared with those exposed to exclusively religious education.
Table 3.
Estimated OR for dementia by religion variables and sociodemographic factors (N for all models = 1,628)
| Logistic Regression; OR (95% CI) | ManteleHaenszel; OR (95% CI) | |
|---|---|---|
| Age | 1.15 (1.11–1.19) | |
| SES | 0.66 (0.57–0.75) | |
| Area of birth (reference group = Israel born) | ||
| East Europe | 0.74 (0.42–1.28) | |
| Central Europe | 0.66 (0.33–1.62) | |
| Balkan Countries | 0.73 (0.32–1.35) | |
| Northern Africa | 1.46 (1.35–1.56) | |
| Middle East | 1.97 (1.40–2.78) | |
| Education contenta (reference group = religious only) | ||
| Model 1 | ||
| Mixed | 0.49 (0.33–0.75) | 0.50 (0.36–0.71) |
| Secular | 0.76 (0.41–1.40) | 0.79 (0.54–1.15) |
| Model 2 | ||
| Mixed or Secular | 0.58 (0.48–0.65) | 0.59 (0.44–0.80) |
| Religious self definition and practicea (Not religious at all [1] to extremely religious [5 = reference group]) | ||
| Model 1 | ||
| 1. Agnostic | 0.43 (0.18–1.01) | 0.36 (0.20–0.62) |
| 2. Secular | 0.67 (0.40–1.11) | 0.62 (0.40–0.94) |
| 3. Traditional | 0.48 (0.33–0.69) | 0.49 (0.30–0.80) |
| 4. Religious | 0.55 (0.40–0.75) | 0.58 (0.37–0.93) |
| Model 2 | ||
| 1 through 4 | 0.54 (0.40–0.74) | 0.52 (0.38–0.73) |
Controlling for age, SES, and area of birth.
For religious self-definition and practice, as reported 35 years prior to the assessment of dementia, the rates of dementia were 9.7%, 17.7%, 14.1%, 19.3%, and 28.8% for categories from least to most religious, respectively. Controlling for sociodemographic variables, the odds of dementia decreased considerably among those who did not define themselves as extremely religious in comparison with that group (ORs = 0.43, 0.67, 0.48, 0.55 for increasing degree of religious self definition and practice; Table 3).
Testing the goodness of fit of both logistic models yielded a P-value of 0.78 for erroneously rejecting a hypothesis of full fit in the religious education model and a 0.06 for the religious self-definition and practice model. Estimation of OR for dementia associated with type of religious education and for the religious self definition and practice model was also carried out applying the method of Mantel–Haenszel, pooling over age, SES, and area of birth (Table 3). The odds ratio of dementia calculated by this method resembled closely the results obtained by the logistic regression.
4. Discussion
Contrary to the hypothesis, the present study found that the prevalence of dementia was increased among men with exclusively religious education and among those with the most strict observance. In both cases, these associations were not altered appreciably after controlling for sociodemographic confounders. Because information about religious education, religious self-definition and practice, and the confounders were collected approximately 35 years before the assessment of dementia, these measurements were not affected by cognitive status.
Other studies examined the association of religion variables and cognition [6,7]. Frequency of attendance to religious services at old ages was associated with better cognitive functioning or slower cognitive decline. Nonetheless, strong religious identity, also measured in one of these studies [6], was associated with cognitive dysfunction, consistent with the results of the present study. Our study differs methodologically in that religious education pertained to childhood, and religious self-definition and practice pertained to midlife in contrast to the other studies that measured religious characteristics close to the cognitive assessment. Early and midlife measures might reflect habits over the course of the life span better than recent activities that might be affected by physical or mental health. Other studies [30,31] have also reported discrepancies between church attendance and self-reported degree of religiosity in their associations with health measures.
A speculative factor in addition to lifelong habits as an explanation for the observed association is consanguineous marriages, which were relatively frequent (approximately 10%) among Jews four decades ago, and even more so among the very religious [32]. In the last decade, intracommunity marriage rates still increased with the degree of religiosity [32]. Several studies [33–36] have indicated that communities that have high rates of inbreeding also display higher rates of dementia compared to communities with low rates of inbreeding. Orthodox Jews might be enriched in potential genes conferring vulnerability for dementia and late onset AD.
Our assessment of SES, based on years of formal schooling and type of employment, was done in 1963, at ages 40 and above. It included both direct and indirect effects of education (in terms of years of schooling), which may be associated with childhood socioeconomic environment. Better socioeconomic conditions in childhood have been associated with relatively more intact later life cognitive ability [37,38]. Although baseline SES was associated with dementia, controlling for it did not alter the association of dementia with religious education and observance.
We found more frequent report of exclusively religious education and more orthodox self-definition and practice in subjects from North Africa and fewer in Europe. Similarly, historical, demographic, social, and other characteristics are likely to be associated with religious education and observance. Accordingly, the implication of these results is not necessarily specific to the effects of religious education and observance per se on dementia, but rather to highlight the importance of habits and behaviors over the life span reflected by differences in religious education and observance.
Years of education, negatively associated with exclusively religious education and religious self-definition and practice in this study, represent a surrogate measure for cognitive reserve [39], consistently shown to be protective against dementia [40]. The Nun study found that idea density and grammatical complexity early in life have different effects on subsequent AD [41]. An additional finding from that study was that memorizing as a learning method early in life did not protect against dementia while using vocabulary elaboration did (Dr. David Snowdon, personal communication). A very speculative explanation for the results of the current study is that focusing intensely over time on repetitive memorizing, which was typically done in an extremely religious education environment, provides less cognitive reserve than using a variety of learning methods.
The process of diagnosing dementia, and especially neuropsychological testing, might be affected by the life style and culture of the patient. This study did not include a neuropsychological battery but was primarily based on the DQ, an in depth clinical dementia assessment performed by a psychiatrist or neurologist expert in the diagnosis of the dementias. These clinicians were based in a Memory Clinic located adjacent to Bnai Brak, a predominantly very religious neighborhood, so that they were experienced in dementia assessment of the full range of religious self-definition and practice.
The results of this study are based on a sample of survivors. The main limitation of this study is the lack of dementia characterization of the 7,453 subjects in the original IIHD study reported dead before the follow-up study was conducted. Those who survived to the time of this study were younger and healthier. The available data do not preclude the possibility that lifelong religious habits might be associated with survival among those who were demented. It might be tempting to assume that an increased prevalence of dementia among men with extreme religious self-definition and practice is associated with selective survival. However, individuals free of diabetes, hypertension, or cigarette smoking enjoy considerably higher survival advantage, yet they showed no excess of dementia among the survivors of this study. The 1,890 survivors who participated in the study were younger and healthier than the 714 survivors who died during the assessment period, could not be traced or refused to participate, but did not differ in religious education or religious self definition and practice.
Finally, in comparing our findings to other studies, an additional complexity is inherent, because our study sample is composed primarily of migrants. The study participants had arrived from diverse corners of the world, and are divided between what was considered the relatively progressive part of Europe, other less economically and socially developed parts of Europe; and other, far less technologically and socially advanced Asian mideastern and African countries. Being Jewish in countries where discrimination on ethnic background was common in the early or middle 20th century, and in many of which fascist or communist regimes prevailed, and given that the horrors of World War II intervened directly or indirectly with the lives of many of these individuals, the childhood and early adulthood living conditions of many of these individuals and interactions with life events remain realistically beyond measurable assessment.
We have chosen to compare unequivocally demented to unequivocally nondemented subjects, excluding the cognitively impaired but not demented subjects, who are heterogeneous with some subjects early in the course of cognitive decline. Furthermore, because CIND characterization in this study relied primarily on subjective memory complains of a subject or informant rather than objective cognitive testing, there was more potential for confounding with cultural background. When CIND subjects were included with the demented subjects as cognitively impaired, or when they were included with the unequivocally nondemented subjects as nondemented, the results of the analyses—more impairment in those with exclusively religious education or who defined themselves as extremely religious—remained essentially unchanged.
Acknowledgments
This research was supported (in part) by the Israel Science Foundation founded by the Israel Academy of Sciences and Humanities (grant no. 67/99 for Michael Davidson and Uri Goldbourt), and by the National Institute on Aging grants P50- AG05138 (for Mary Sano), P01-AG02219 (for Vahram Haroutunian), and K01 AG023515-01A2 (for Michal Schnaider Beeri).
References
- [1].Van DK, Sano M. The impact of nutrition on cognition in the elderly. Neurochem Res. 2007;32:893–904. doi: 10.1007/s11064-006-9241-5. [DOI] [PubMed] [Google Scholar]
- [2].Fratiglioni L, Paillard-Borg S, Winblad B. An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol. 2004;3:343–53. doi: 10.1016/S1474-4422(04)00767-7. [DOI] [PubMed] [Google Scholar]
- [3].Evans RM, Hui S, Perkins A, Lahiri DK, Poirier J, Farlow MR. Cholesterol and APOE genotype interact to influence Alzheimer disease progression. Neurology. 2004;25(62):1869–71. doi: 10.1212/01.wnl.0000125323.15458.3f. [DOI] [PubMed] [Google Scholar]
- [4].Purdy S, Jones KP, Sherratt M, Fallon PV. Demographic characteristics and primary health care utilization patterns of strictly orthodox Jewish and non-Jewish patients. Fam Pract. 2000;17:233–5. doi: 10.1093/fampra/17.3.233. [DOI] [PubMed] [Google Scholar]
- [5].Bassuk SS, Glass TA, Berkman LF. Social disengagement and incident cognitive decline in community-dwelling elderly persons. Ann Intern Med. 1999;131:165–73. doi: 10.7326/0003-4819-131-3-199908030-00002. [DOI] [PubMed] [Google Scholar]
- [6].Van Ness PH, Kasl SV. Religion and cognitive dysfunction in an elderly cohort. J Gerontol B Psychol Sci Soc Sci. 2003;58:S21–9. doi: 10.1093/geronb/58.1.s21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hill TD, Burdette AM, Angel JL, Angel RJ. Religious attendance and cognitive functioning among older Mexican Americans. J Gerontol B Psychol Sci Soc Sci. 2006;61:3–9. doi: 10.1093/geronb/61.1.p3. [DOI] [PubMed] [Google Scholar]
- [8].Beeri MS, Werner P, Davidson M, Schmidler J, Silverman J. Validation of the modified telephone interview for cognitive status (TICS-m) in Hebrew. Int J Geriatr Psychiatry. 2003;18:381–6. doi: 10.1002/gps.840. [DOI] [PubMed] [Google Scholar]
- [9].Tuokko H, Frerichs RJ. Cognitive impairment with no dementia (CIND): longitudinal studies, the findings, and the issues. Clin Neuropsychol. 2000;14:504–25. doi: 10.1076/clin.14.4.504.7200. [DOI] [PubMed] [Google Scholar]
- [10].Schnaider BM, Goldbourt U, Silverman JM, Noy S, Schmeidler J, RavonaSpringer R, et al. Diabetes mellitus in midlife and the risk of dementia three decades later. Neurology. 2004;63:1902–7. doi: 10.1212/01.wnl.0000144278.79488.dd. [DOI] [PubMed] [Google Scholar]
- [11].Groen JJ, Medalie JH, Neufeld HN, Riss E, Bachrach CA, Mount FW, et al. An epidemiologic investigation of hypertension and ischemic heart disease within a defined segment of the adult male population of Israel. Isr J Med Sci. 1968;4:177–94. [PubMed] [Google Scholar]
- [12].Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- [13].Brandt J, Folstein SE, Folstein MF. Differential cognitive impairment in Alzheimer's disease and Huntington's disease. Ann Neurol. 1988;23:555–61. doi: 10.1002/ana.410230605. [DOI] [PubMed] [Google Scholar]
- [14].Gallo JJ, Breitner JC. Alzheimer's disease in the NAS-NRC Registry of aging twin veterans, IV. Performance characteristics of a two-stage telephone screening procedure for Alzheimer's dementia. Psychol Med. 1995;25:1211–9. doi: 10.1017/s0033291700033183. [DOI] [PubMed] [Google Scholar]
- [15].Silverman JM, Keefe RS, Mohs RC, Davis KL. A study of the reliability of the family history method in genetic studies of Alzheimer disease. Alzheimer Dis Assoc Disord. 1989;3:218–23. [PubMed] [Google Scholar]
- [16].Silverman JM, Breitner JC, Mohs RC, Davis KL. Reliability of the family history method in genetic studies of Alzheimer's disease and related dementias. Am J Psychiatry. 1986;143:1279–82. doi: 10.1176/ajp.143.10.1279. [DOI] [PubMed] [Google Scholar]
- [17].Werner P, Heinik J, Mendel A, Reicher B, Bleich A. Examining the reliability and validity of the Hebrew version of the Mini Mental State Examination. Aging (Milano) 1999;11:329–34. doi: 10.1007/BF03339808. [DOI] [PubMed] [Google Scholar]
- [18].Yesavage JA. Geriatric depression scale. Psychopharmacol Bull. 1988;24:709–11. [PubMed] [Google Scholar]
- [19].Wade J, Hachinski V. Revised ischemic score for diagnosing multi-infarct dementia. J Clin Psychiatry. 1986;47:437–8. [PubMed] [Google Scholar]
- [20].Ellis RJ, Jan K, Kawas C, Koller WC, Lyons KE, Jeste DV, et al. Diagnostic validity of the dementia questionnaire for Alzheimer disease. Arch Neurol. 1998;55:360–5. doi: 10.1001/archneur.55.3.360. [DOI] [PubMed] [Google Scholar]
- [21].Kawas C, Segal J, Stewart WF, Corrada M, Thal LJ. A validation study of the Dementia Questionnaire. Arch Neurol. 1994;51:901–6. doi: 10.1001/archneur.1994.00540210073015. [DOI] [PubMed] [Google Scholar]
- [22].Li G, Aryan M, Silverman JM, Haroutunian V, Perl DP, Birstein S, et al. The validity of the family history method for identifying Alzheimer disease. Arch Neurol. 1997;54:634–40. doi: 10.1001/archneur.1997.00550170104021. [DOI] [PubMed] [Google Scholar]
- [23].American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th Edition American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- [24].Eaton CB, Medalie JH, Flocke SA, Zyzanski SJ, Yaari S, Goldbourt U. Self-reported physical activity predicts long-term coronary heart disease and all-cause mortalities. Twenty-one-year follow-up of the Israeli Ischemic Heart Disease Study. Arch Fam Med. 1995;4:323–9. doi: 10.1001/archfami.4.4.323. [DOI] [PubMed] [Google Scholar]
- [25].Luchsinger JA, Mayeux R. Cardiovascular risk factors and Alzheimer's disease. Curr Atheroscler Rep. 2004;6:261–6. doi: 10.1007/s11883-004-0056-z. [DOI] [PubMed] [Google Scholar]
- [26].Luchsinger JA, Reitz C, Honig LS, Tang MX, Shea S, Mayeux R. Aggregation of vascular risk factors and risk of incident Alzheimer disease. Neurology. 2005;65:545–51. doi: 10.1212/01.wnl.0000172914.08967.dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Schnaider BM, Davidson M, Silverman JM, Noy S, Schmeidler J, Goldbourt U. Relationship between body height and dementia. Am J Geriatr Psychiatry. 2005;13:116–23. doi: 10.1176/appi.ajgp.13.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Anderson JT, Keys A. Cholesterol in serum and lipoprotein fractions; its measurement and stability. Clin Chem. 1956;2:145–59. [PubMed] [Google Scholar]
- [29].Hosmer DW, Lemeshow S. Applied logistic regression. Wiley; New York, NY: 1989. [Google Scholar]
- [30].Krause N, Van TT. Stress and religious involvement among older blacks. J Gerontol. 1989;44:S4–S13. doi: 10.1093/geronj/44.1.s4. [DOI] [PubMed] [Google Scholar]
- [31].Anson O, Carmel S, Bonneh DY, Levenson A, Maoz B. Recent life events, religiosity, and health: an individual or collective effect. Hum Relat. 1990;43:1051–66. [Google Scholar]
- [32].Cohen T, Vardi-Saliternik R, Friedlander Y. Consanguinity, intracommunity and intercommunity marriages in a population sample of Israeli Jews. Ann Hum Biol. 2004;31:38–48. doi: 10.1080/0301446032000159255. [DOI] [PubMed] [Google Scholar]
- [33].van der Walt JM, Scott WK, Slifer S, et al. Maternal lineages and Alzheimer disease risk in the Old Order Amish. Hum Genet. 2005;118:115–22. doi: 10.1007/s00439-005-0032-x. [DOI] [PubMed] [Google Scholar]
- [34].Sleegers K, Roks G, Theuns J, Aulchenko YS, Rademakers R, Cruts M, et al. Familial clustering and genetic risk for dementia in a genetically isolated Dutch population. Brain. 2004;127(Pt 7):1641–9. doi: 10.1093/brain/awh179. [DOI] [PubMed] [Google Scholar]
- [35].Farrer LA, Bowirrat A, Friedland RP, Waraska K, Korczyn AD, Baldwin CT. Identification ofmultiple loci forAlzheimerdisease in a consanguineous Israeli-Arab community. HumMolGenet. 2003;12:415–22. doi: 10.1093/hmg/ddg037. [DOI] [PubMed] [Google Scholar]
- [36].Vezina H, Heyer E, Fortier I, Ouellette G, Robitaille Y, Gauvreau D. A genealogical study of Alzheimer disease in the Saguenay region of Quebec. Genet Epidemiol. 1999;16:412–25. doi: 10.1002/(SICI)1098-2272(1999)16:4<412::AID-GEPI7>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- [37].Kaplan GA, Turrell G, Lynch JW, Everson SA, Helkala EL, Salonen JT. Childhood socioeconomic position and cognitive function in adulthood. Int J Epidemiol. 2001;30:256–63. doi: 10.1093/ije/30.2.256. [DOI] [PubMed] [Google Scholar]
- [38].Turrell G, Lynch JW, Kaplan GA, Everson SA, Helkala EL, Kauhanen J, et al. Socioeconomic position across the lifecourse and cognitive function in late middle age. J Gerontol B Psychol Sci Soc Sci. 2002;57:S43–51. doi: 10.1093/geronb/57.1.s43. [DOI] [PubMed] [Google Scholar]
- [39].Stern Y. Cognitive reserve and Alzheimer disease. Alzheimer Dis Assoc Disord. 2006;20(3 Suppl. 2):S69–74. doi: 10.1097/00002093-200607001-00010. [DOI] [PubMed] [Google Scholar]
- [40].Katzman R. Education and the prevalence of dementia and Alzheimer's disease. Neurology. 1993;43:13–20. doi: 10.1212/wnl.43.1_part_1.13. [DOI] [PubMed] [Google Scholar]
- [41].Snowdon DA, Kemper SJ, Mortimer JA, Greiner LH, Wekstein DR, Markesbery WR. Linguistic ability in early life and cognitive function and Alzheimer's disease in late life. Findings from the Nun Study. JAMA. 1996;275:528–32. [PubMed] [Google Scholar]