Abstract
We previously demonstrated the ability of an orally administered attenuated Salmonella enterica serovar Typhimurium strain expressing the protective antigen (PA) of Bacillus anthracis to confer protection against lethal anthrax aerosol spore challenge [1]. To extend the utility of this approach to humans we constructed variants of S. enterica serovar Typhi Ty21a, an attenuated typhoid vaccine strain licensed for human use, which expressed and exported PA via two distinct plasmid-based transport systems: the Escherichia coli HlyA haemolysin and the S. Typhi ClyA export apparatus. Murine immunogenicity studies confirmed the ability of these constructs, especially Ty21a expressing the ClyA-PA fusion protein, to stimulate strong PA-specific immune responses following intranasal immunization. These responses were further enhanced by a subsequent boost with either parenterally delivered recombinant PA or the licensed US human alum-adsorbed anthrax vaccine (AVA). Anthrax toxin neutralizing antibody responses using this prime-boost regimen were rapid, vigorous and broad in nature. The results of this study demonstrate the feasibility of employing a mucosal prime with a licensed Salmonella Typhi vaccine strain followed by a parenteral protein boost to stimulate rapid protective immunity against anthrax.
Keywords: Salmonella Typhi, Ty21a, anthrax, live vector vaccines, prime-boost immunization
1. Introduction
Anthrax is a disease caused by the bacterium Bacillus anthracis. Although primarily a disease of animals it also infects humans, sometimes with fatal consequences. Until recently the availability of effective animal vaccines coupled with the scarcity of human disease resulted in the organism receiving little attention outside of the military.
The ability to form heat-resistant spores which infect via the lungs coupled with the availability in nature and the simplicity of the production technology makes the organism an attractive biological weapon for extremist groups [2]. The recent spread of anthrax spores through the U.S. postal system demonstrates the disruption and dramatic consequences that such an attack can inflict [2].
The capacity of B. anthracis to cause disease is dependent on the production of a polyglutamic acid capsule, which confers resistance to phagocytosis, and the expression of a tripartite toxin comprising protective antigen (PA, responsible for cell binding), edema factor (EF, a toxin acting via cAMP modulation) and lethal factor (LF, a metalloprotease which modulates MAP-kinase mediated signal transduction) [3]. The toxin follows the AB model: the A moiety comprises the catalytic subunits LF and EF, while the B moiety, PA, serves to translocate either EF or LF into the cytosol [4]. Numerous animal studies have confirmed the role of PA as the principal protective immunogen in the licensed US and UK human vaccines and have demonstrated its ability to elicit effective protective immunity against aerosol spore challenge [4]. While effective, these vaccines suffer from the requirement for a multiple dose priming series followed by yearly booster shots. In addition, adverse local reactions such as soreness, redness, itching and swelling at the site of injection have been observed [5].
A newer vaccine consisting of recombinant PA protein adsorbed to aluminium hydroxide is under development and while this vaccine is likely to reduce adverse reactions, it is anticipated that it will still require multiple dosing, and administration by needle and syringe, necessitating the involvement of trained medical personnel [6;7]. The inclusion of aluminium hydroxide as the adjuvant will also impose an additional burden since the vaccine will have to be transported and maintained at 4°C, making it difficult to store in remote regions and limiting its shelf life. User friendly anthrax vaccines capable of self administration via the oral route, sufficiently potent to stimulate protective immunity following a single dose and stable at room temperature, would be extremely attractive to authorities seeking to build stockpiles to respond to a large scale future threat [4].
Oral vaccines have proved to be an extremely effective means of immunizing large numbers of at risk individuals and have been used for many years to confer protection against diseases such as polio and typhoid [8;9]. Indeed, an attenuated Salmonella enterica serovar Typhi (S. Typhi) strain, Ty21a, is currently licensed for use in humans as an oral vaccine against typhoid fever [10;11]. The feasibility of employing attenuated strains of Salmonella such as S. Typhi to deliver heterologous antigens and induce protective immunity against a range of pathogens in animal models has been repeatedly demonstrated [12;13]. We have recently reported the construction of an attenuated strain of Salmonella enterica serovar Typhimurium (S. Typhimurium) expressing B. anthracis PA from a multicopy plasmid which was able to protect orally immunized mice against a lethal spore aerosol challenge [1]. While these results demonstrate the potential of this approach, any future human vaccine would have to be based on a strain of Salmonella acceptable for human use.
We thus set out to determine the feasibility of developing a human oral anthrax vaccine by transferring into S. Typhi Ty21a a plasmid-based PA export systems which had previously been shown to confer protection against B. anthracis spore challenge [1;14]. The two systems we examined differed in the manner in which they export and present the foreign antigen to the host immune system. The E.coli derived HlyA haemolysin system directs the export of haemolysin or a haemolysin-fused partner through both the inner and outer membranes directly to the external environment [15;16], whereas the ClyA export apparatus of S. Typhi is though to incorporate the fusion protein into a lipid vesicle, which is subsequently released from the outer membrane [17;18]. We evaluated the immunogenicity of our PA fusion constructs in mice immunized intranasally. We also assessed whether it was possible to further enhance the magnitude and longevity of the PA specific immune response by adopting a prime-boost strategy in which mice mucosally primed with S. Typhi were boosted with either parenterally delivered rPA or the licensed US human alum absorbed anthrax vaccine (AVA). Our results suggest substantial promise for these approaches.
2. Materials and methods
2.1. Construction of recombinant S. Typhi Ty21a strains expressing codon optimized PA from different secretion signals
The construction and properties of the two PA expression plasmids used in this study have been previously described [1;14;17]. Briefly plasmid pVDL9.3PA83ec, a low copy number plasmid (4-6 copies/cell) conferring chloramphenicol resistance, encodes a full-length codon optimized version of the PA gene fused to the carboxyl terminus of the E. coli haemolysin (Hly) export system, in order to enable export of the expressed PA protein from Salmonella [16]. The second plasmid, pSECPA (∼15 copies/cell) employed the same codon optimized version of the PA gene fused to the carboxyl terminus of the S. Typhi ClyA export apparatus downstream of the ompC promoter so that it can be expressed at a high level in Salmonella and exported out of the bacterial cell without causing lysis [1]. This plasmid is similar to those previously described by Galen et al. [17]. It confers resistance to kanamycin and includes the hok-sok post-segregational killing locus and the parA gene encoding an active partitioning system. Each plasmid was electroporated into S. Typhi vaccine strain Ty21a (Berna Biotech, Switzerland). Transformants were screened in LB agar plates containing chloramphenicol (25 μg/ml) or kanamycin (50 μg/ml). Single colonies were selected and stored at -70°C.
2.2. Analysis of PA expression
Bacteria were cultured overnight in Luria-Bertani broth supplemented with kanamycin or chloramphenicol (Sigma-Aldrich, St. Louis, MO) where appropriate, and subcultured in 10 ml of fresh medium until an optical density at 600 nm of ∼1. Bacterial proteins were separated by SDS-PAGE electrophoresis and transferred onto Immun-Blot PVDF membranes (Bio-Rad, Hercules, CA). The membranes were blocked with 10% dry milk (Nestle USA Inc., Glendale, CA) in PBS 0.05% Tween 20 (PBST) and probed with goat anti-PA polyclonal antibody (List Biological Laboratory, Inc., Campbell, CA) followed by horseradish peroxidase (HRP)-labeled anti-goat antibodies (Kirkegaard & Perry Laboratories, Inc. [KPL], Gaithersburg, MD.) and Western Lightning Chemiluminescence substrate (PerkinElmer Life Sciences, Inc., Boston MA).
2.3. Immunization
Female BALB/c mice (8-10 wks old) purchased from Charles River Wilmington, Mass., were immunized with S. Typhi Ty21a alone, Ty21a carrying PA-encoding or empty plasmids, recombinant PA (rPA) or the Anthrax Vaccine Adsorbed (AVA) in different prime-boost combinations as indicated in the Figure legends for each experiment. S. Typhi strains were delivered intranasally (i.n.) in a 10 μl-volume containing 1-2×109 CFU (5 μl/nare) as previously described [19;20]. The rPA (purified from recombinant Bacillus subtilis [21]) was delivered via the intramuscular (i.m.) route in a 100 μl-volume containing 1 or 10 μg of purified protein adsorbed to 0.5% Alhydrogel (Brenntag Stinnes Logistics, Frederikssund, Denmark). PA-Alhydrogel adsorption was performed the day prior to vaccination; rPA was mixed with 0.5% Alhydrogel and incubated for 20 minutes at room temperature and then overnight at 4°C. The AVA vaccine, also known as BioThrax™ (manufactured by BioPort Corporation Lansing, Michigan, U.S. License No. 1260), was administered via subcutaneous (s.c.) injection in a 200 μl-volume. Blood samples were collected throughout the study to determine PA specific antibody responses. All animal studies were approved by the University of Maryland Animal Care and Use Committee.
2.4. Measurement of antibody responses
IgG antibodies
Serum IgG antibodies specific for B. anthracis PA and S. Typhi LPS were measured by ELISA. Briefly, ELISA plates were coated with rPA (List Biological Laboratories) at 2 μg/ml in PBS or with S. Typhi LPS (Sigma-Aldrich) at 10 μg/ml in carbonate buffer (pH 9.6) for 3 h at 37°C. Plates were washed with PBST and blocked overnight with 10% dry milk (Nestle USA Inc., Glendale, Calif.) in PBS. Serially diluted serum samples were incubated for 1 h at 37°C. PA-specific antibodies were revealed with HRP-labeled goat anti-mouse IgG (Roche Diagnostics Corporation, Indianapolis, IN) followed by TMB Microwell Peroxidase Substrate (KPL). The reaction was stopped by adding 100 μl of 1 M H3PO4 after 15 min incubation. End-point titers were calculated through linear regression equations as the inverse of the serum dilution that produces an Absorbance450 mn value of 0.2 above the blank (ELISA units per ml). Sera were run in duplicate; a positive calibrated control was included in each assay.
Toxin Neutralizing Activity (TNA) antibodies
Anthrax TNA antibodies were measured as described by Quinn et al. [22;23]. Serially diluted serum samples were incubated with anthrax lethal toxin (rPA + rLF purchased from List Biological Labs) in 96-well plates for 1 h at 37°C and the mixture was transferred to a monolayer of J774A.1 cells. Viability was assessed by addition of tetrazolium salt MTT at 5 mg/ml. Titers were calculated as the reciprocal of a serum-sample dilution that resulted in 50% neutralization of toxin-mediated cytotoxicity (ED50), corresponding to the inflection point of a 4-parameter logistic-log fit curve. ED50 data were obtained using an end-point algorithm (Taylor method) developed by the U.S. Centers for Disease Controls [23].
2.6. Statistical analysis
Data were log transformed for calculation of GMT and confidence intervals. Differences in antibody titers among groups were assessed by Student's t test and Mann Whitney Rank Sum Test when normality failed. A P value of < 0.05 was considered statistically significant. Statistical analysis was performed using SigmaStat 3.0 (SPPS Inc. Chicago).
3. Results
3.1. In vitro expression of PA by recombinant S. Typhi Ty21a strains
Two plasmid constructs expressing an identical, codon-optimized version of the PA gene fused to ClyA or HlyA, were transferred into S. Typhi Ty21a, and their ability to express the respective proteins was confirmed by Western blot (Figure 1). As expected, the strains carrying pSECPA and the pVDL9.3PA83ec expressed the PA fusion proteins of the predicted sizes, which were 117 kDa (ClyA-PA) and 107 kDa (HlyA-PA) respectively.
Figure 1.
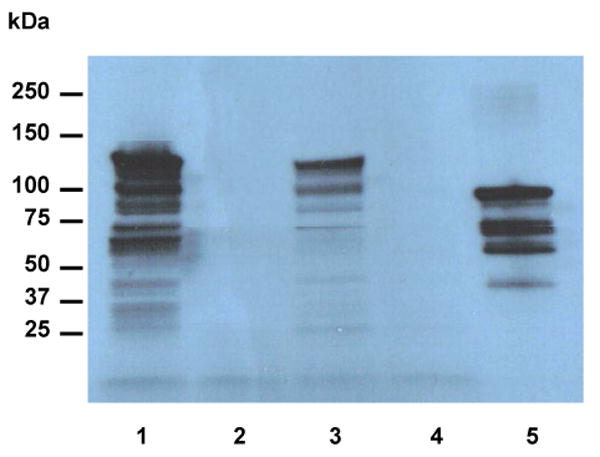
Expression of B. anthracis PA in S. Typhi Ty21a constructs by Western blot analysis. Lane 1: Ty21a(pSECPA); lane 2: Ty21a(pSEC10); lane 3: Ty21a(pVDL9.3PA83ec; lane 4: Ty21a(pVDL9.3); lane 5: rPA.
3.2. Immunogenicity of PA-expressing S. Typhi Ty21a constructs
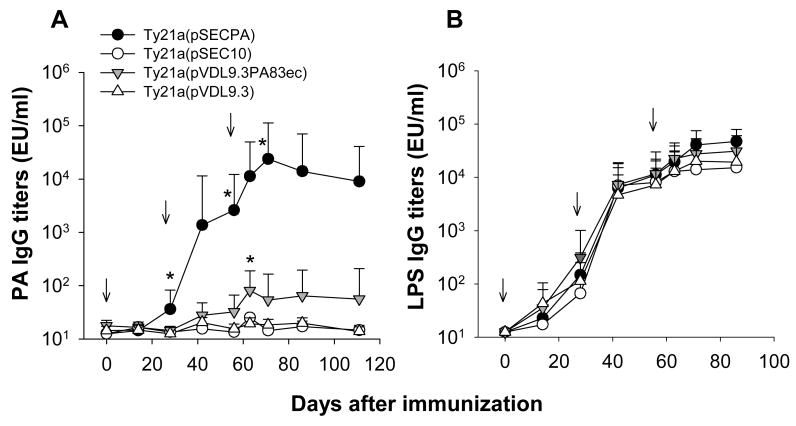
To determine the immunogenicity of the S. Typhi strains expressing B. anthracis PA, BALB/c mice (n=10 per group) were immunized i.n. at 3 time points (days 0, 28 and 56) with Ty21a(pSECPA) or Ty21a(pVLD9.3PA83ec). Mice immunized with Ty21a carrying the empty plasmids pSEC10 or pVLD9.3 were included as controls. Kinetics of PA and LPS-specific IgG antibody titers are shown in Figure 2. Immunization with Ty21a(pSECPA) stimulated an extremely robust PA-specific IgG response, with antibody titers increasing significantly after each immunization (p<0.05) (Figure 2A). In contrast, very low PA antibody levels were generated by Ty21a(pVDL9.3PA83ec). This marked difference in immunogenicity between strains was not due to any failure of the mice to recognize the S. Typhi constructs as all groups produced similar levels of LPS specific IgG antibodies. The LPS titers increased after each immunization (p<0.05) and reached a plateau after the third dose (Figure 2B).
Figure 2.
Serum IgG antibodies to PA (A) and S. Typhi LPS (B) in mice immunized with S. Typhi Ty21a strains expressing B. anthracis PA. Mice were primed i.n. on days 0, 28 and 56 with S. Typhi Ty21a strain carrying PA-encoding plasmids pSECPA and pVDL9.3PA83ec or empty plasmids pSEC10 and pVDL9.3. Curves are plotted upon the GMT for each group and bars indicate the 95% confidence intervals. Arrows indicate each immunization. * indicate differences between PA-expressing strains vs. strains carrying empty plasmids (p<0.001) at peak time points after each dose.
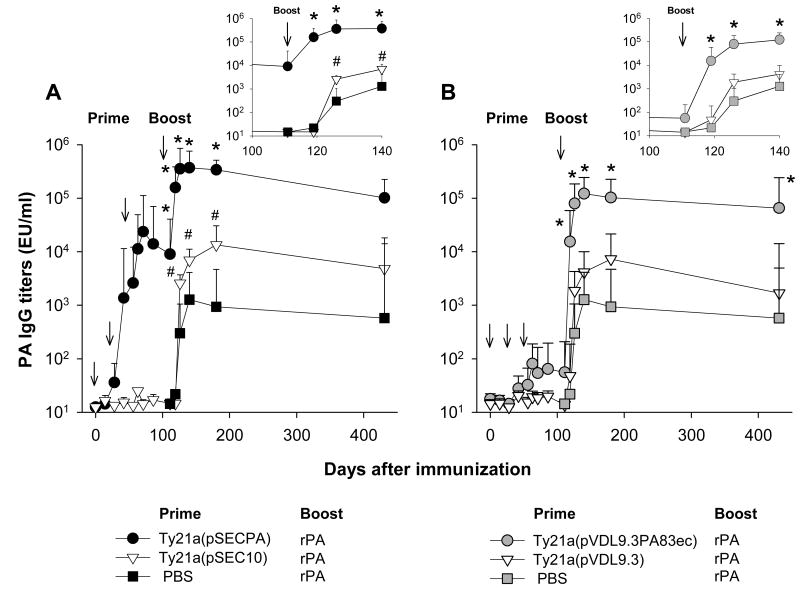
3.3. PA-specific IgG elicited by Ty21a-PA prime rPA-alum boost
It has been shown for a variety of pathogens that protection can be enhanced by administering vaccine antigens in different forms and by alternative routes in so called “prime-boost” regimens [24]. We investigated whether the immune responses elicited by S. Typhi Ty21a expressing PA could be improved when the live attenuated vaccine was administered as the priming agent, followed by parenteral boost with purified rPA. Mice were thus primed i.n. on days 0, 28 and 56 with Ty21a(pSECPA) or Ty21a (pVLD9.3PA83ec) and were boosted on day 112 with a single 1 μg-dose of rPA administered i.m. in the presence of alum (Figure 3). Groups primed with Ty21a carrying empty plasmids or with PBS, and boosted with rPA served as “unprimed” controls. Mice primed with either Ty21a-PA construct elicited very strong anamnestic responses following the rPA boost that markedly surpassed those of unprimed controls (p<0.02, days 120-431).
Figure 3.
PA-specific IgG titers elicited by S. Typhi Ty21a-PA prime followed by rPA-boost. Mice were primed i.n. on days 0, 28 and 56 with either Ty21a(pSECPA) (A) or Ty21a(pVDL9.3PA83ec) (B) and boosted i.m. on day 112 with a single dose of 1 μg of rPA. Mice that received Ty21a carrying empty plasmids pSEC10 (A) and pVDL9.3PBS (B) or PBS (A and B) were included as “unprimed” controls; these animals were boosted on day 112 with 1 μg of rPA in identical manner. Data represent GMT and 95% confidence intervals for each group. Arrows indicate each immunization. * indicate differences between groups primed with Ty21a expressing PA vs. Ty21a carrying empty plasmids (p<0.05); # indicate differences between mice primed with Ty21a carrying empty plasmid vs. PBS. Inserts depict enlarged PA IgG titers between days 100 and 140 (the time points closer to the boost).
Interestingly, the post-boost responses varied depending on the plasmid based export system. Even though Ty21a(pVDL9.3PA83ec) was not as effective as Ty21a(pSECPA) at stimulating a visible PA-specific IgG response after priming, it was capable of mounting a robust, memory recall response upon rPA boost. Indeed, mice primed with Ty21a(pVDL9.3PA83ec) showed a much greater increase in PA IgG titers upon boosting (>1,000-fold) compared with those previously immunized with Ty21a(pSECPA), which exhibited increases of only 1-2 orders of magnitude. The post boost PA IgG responses seen with both constructs were maintained for almost one year (319 days post rPA boost, day 431 after primary immunization) at levels 1-3 orders of magnitude above the pre-boosting titers (Figure 3A and B). An interesting observation was that mice primed with S. Typhi carrying the empty plasmid pSEC10 had a greater post-boost PA response compared with mice primed with PBS (p<0.04, days 126-180). A similar trend was seen in mice primed with S. Typhi(pVDL9.3) vs. those primed with PBS, even though the difference did not reach statistical significance.
3.4. TNA antibodies elicited by Ty21a PA-prime rPA-alum boost
Whereas the PA specific IgG antibody response is a useful indicator of immunogenicity, it does not directly correlate with protection in mice [1]. Recent data have demonstrated that PA-specific antibody-mediated TNA is a more reliable marker of protection in mice, guinea pigs and rabbits [4;25]. We examined the post-boost TNA responses in mice primed with Ty21a(pSECPA), Ty21a(pVLD9.3PA83ec), Ty21a carrying empty plasmids or PBS and boosted with a single dose of 1 μg of rPA. An additional group that received 10 μg of rPA at each priming time points served as positive control. TNA levels measured 68 and 319 days after boosting (days 180 and 431 after primary immunization) are shown in Table 1. The results clearly demonstrate that animals primed with either S. Typhi Ty21a construct expressing PA were able to generate TNA antibodies following a parenteral rPA boost. The levels achieved (GMT range 130-193 ED50) were even higher than those seen previously in mice immunized with S. Typhimurium expressing PA which had survived a lethal aerosol spore challenge [1]. It is also noteworthy that the elevated TNA responses were still evident almost a year later.
Table 1.
Anthrax toxin neutralizing antibody titers in mice immunized with S. Typhi Ty21a strains expressing B. anthracis PA and boosted with rPA-alum.
| Groups | TNA titers (ED50) | ||
|---|---|---|---|
| Prime | Boosta | Day 180 (68 post boost) |
Day 431 (319 post boost) |
| Ty21a(pSECPA) | rPA | 130 (93-180) | 147 (82-265) |
| Ty21a(pSEC10) | rPA | 9 (3-30) | 15 (4-57) |
| Ty21a(pVDL-9.3PA83ec) | rPA | 193 (116-323) | 147 (72-302) |
| Ty21a(pVDL-9.3) | rPA | 11 (3-43) | 2 (1-6) |
| PBS | rPA | 7 (2-30) | 5 (1-30) |
| rPAb | ---- | 10,738 (8,711-13,238) | 4,544 (3,379-6,110) |
Mice were primed i.n. on days 0, 28 and 56 with Ty21a PA-expressing strains, Ty21a carrying empty plasmids or PBS, and boosted i.m. on day 112 with a single dose of 1 μg of rPA. A positive control group received 3 priming doses of 10 μg rPA on days 0, 28 and 56. Data represent GMT and 95% confidence intervals. Days after primary immunization and boost are indicated.
1 μg, single boosting dose
10 μg, 3 priming doses
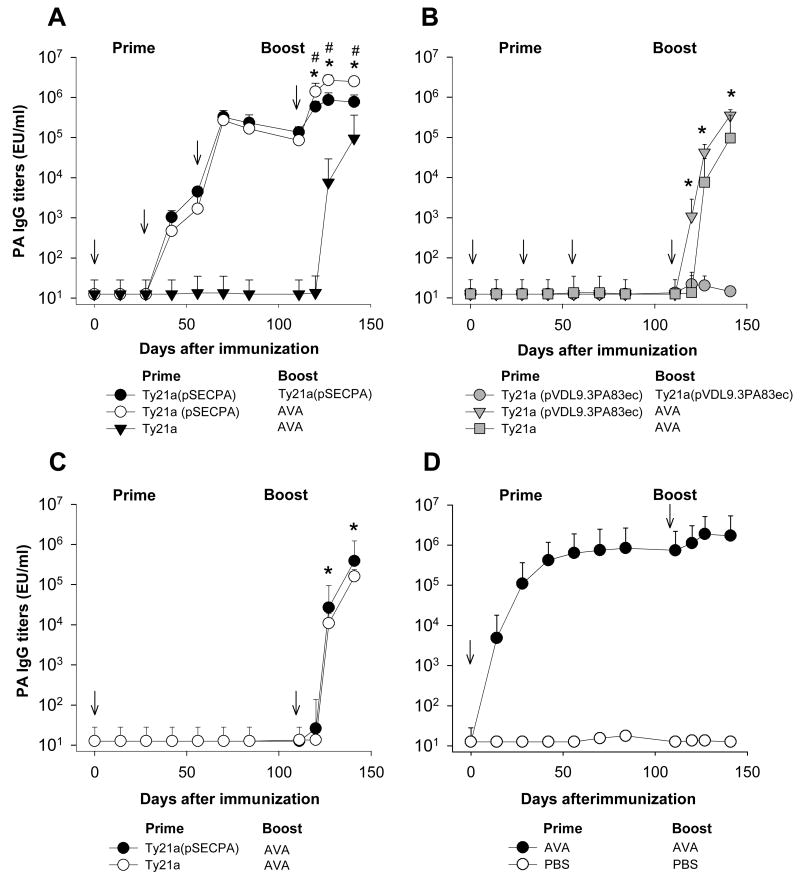
3.5. PA-specific IgG elicited by Ty21a-PA prime AVA-boost
In a subsequent study we investigated the ability of the U.S. licensed human anthrax vaccine (AVA) to boost the immune response primed by the S. Typhi Ty21a-PA constructs (Figure 4). A significant recall response ensued in animals primed with S. Typhi Ty21a expressing PA and boosted with AVA, similar to the effect observed upon boosting with purified rPA. Indeed the magnitude of the PA specific IgG levels generated in response to the AVA boost in animals primed with Ty21a(pSECPA) significantly exceeded those of unprimed mice that received Ty21a, with antibody titers increasing dramatically as early as 8 days after the boost, our first post immunisation sampling point (Figure 4A). Mice primed with Ty21a(pSECPA) and boosted with AVA also achieved higher PA titers than mice primed and boosted only with Ty21a(pSECPA) (p<0.001, days 119-140), further confirming the efficiency of the heterologous prime-boost regimen to enhance immune responses.
Figure 4.
PA-specific IgG titers elicited by S. Typhi Ty21a-PA prime followed by AVA boost. Mice were primed i.n. with Ty21(pSECPA) (A), Ty21a(pVDL9.3PA83ec) (B) or Ty21a empty vector on days 0, 28 and 56 and boosted i.n. on day 112 with Ty21a(pSECPA) (A), Ty21a(pVDL9.3PA83ec) (B) or s.c. with 0.2 ml of AVA (A and B). To compare multiple vs. single priming, a group was immunized on day 0 with Ty21a(pSECPA) or Ty21a empty vector, and boosted on day 112 with 0.2 ml of AVA in identical manner (C). A positive control group received 2 doses of AVA on day 0 and 112 (D). Mice that received only PBS included as negative controls showed no responses (data not shown). Data represent GMT and the 95% confidence intervals for each group. Arrows indicate each immunization. * indicate differences between groups primed with Ty21a-PA strains vs. Ty21a empty vector (p<0.001); # indicate differences between Ty21a-PA prime AVA-boost vs. Ty21a-PA prime and boost.
Again, mice primed with Ty21a(pVLD9.3PA83ec) mounted little if any detectable antibody response prior to boosting but did show a 4-5 log10 increase in PA IgG titers following the AVA boost, also surpassing the titers attained by mice primed with Ty21a alone followed by AVA (p<0.001, days 119-140) (Figure 4B).
We also explored the effect of single vs. repeated priming immunizations using Ty21a(pSECPA), as this strain exhibited visible PA responses during the priming phase. The number of doses in the priming series influenced the magnitude of the antibody responses both before and after the AVA boost. Animals given a single dose of Ty21a(pSECPA) showed no detectable PA-specific antibodies prior to boosting with AVA (Figure 4C) whereas animals that had received multiple priming doses of Ty21a(pSECPA) exhibited PA-specific antibodies as early as day 42, reaching 5 log10 titers prior to the boost (Figure 4A). Subsequent boosting with AVA resulted in a 1.5-3 log10 increase in titers (2 weeks later) for both groups, with the animals that received 3 priming doses of S. Typhi-PA achieving a 100-fold higher GMT compared with mice primed with a single dose (2,664,523 EU/ml vs. 26,482 EU/ml on day 128, p<0.05) (Figure 4C). Mice primed with a single dose of Ty21a(pSECPA) also developed higher responses following the AVA boost compared with mice that received a single dose of Ty21a (GMT: 26,482 and 386,950 EU/ml vs. 10,815 and 158,694 EU/ml on days 128 and 141, p=0.043 and p<0.002, respectively) (Figure 4C).
It is noteworthy that the PA IgG responses elicited through Ty21a(pSECPA) 3-dose prime followed by AVA boost reached higher levels than those attained after the AVA prime-boost, although the difference barely missed statistical significance (GMT: 2,664,523 EU/ml vs. 1,886.051, peak responses on day 128, p=0.065) (Figure 4A and D).
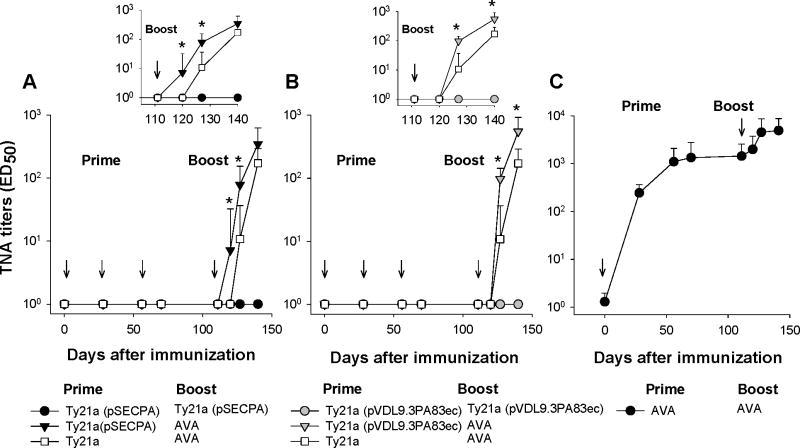
3.6. TNA antibodies elicited by Ty21a PA-prime AVA-boost
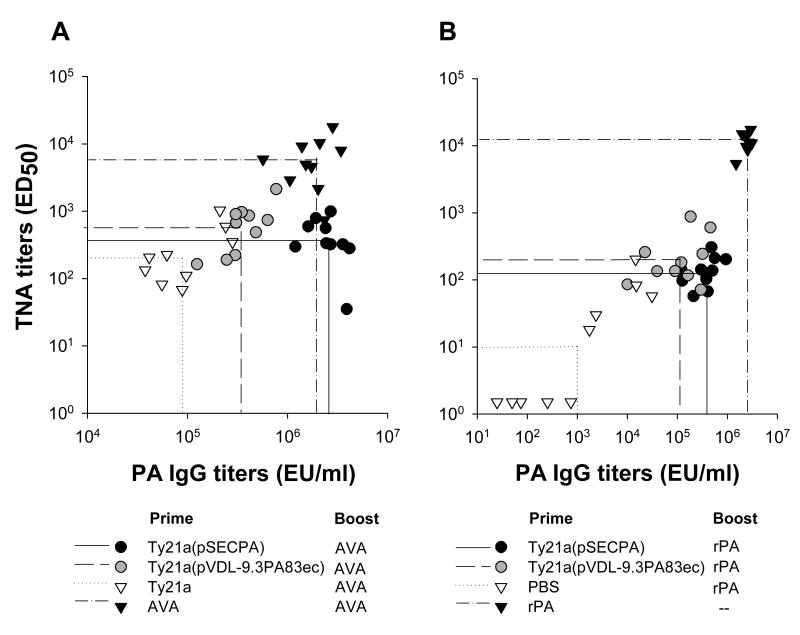
Mice primed with either Ty21a(pSECPA) or Ty21a(pVLD9.3PA83ec) developed a faster and more robust TNA response after a single AVA boosting compared with mice primed with Ty21a alone (Figure 5A and B). Responses remained elevated in Ty21a PA-primed mice over unprimed controls for at least one month after the boost (the last time point measured) (Figure 5A and B). The TNA titers achieved ∼3 weeks following the boost exceeded those seen pre-challenge in animals which had survived a lethal aerosol spore challenge [1]. These responses, however, did not reach the level seen in animals primed and boosted with AVA (Figure 5C).
Figure 5.
TNA antibody titers elicited by S. Typhi Ty21a-PA prime followed by AVA boost. Mice were primed on days 0, 28 and 56 with Ty21a(pSECPA) (A) or Ty21a(pVDL9.3PA83ec) (B) and boosted on day 112 with Ty21a(pSECPA) (A), Ty21a(pVDL9.3PA83ec) (B) or AVA (A-B) as described in Figure 4. A control group was primed and boosted with AVA on days 0 and 112 (C). Data represent GMT and the 95% confidence intervals for each group. Arrows indicate each immunization. * indicates differences between groups primed with Ty21a-PA vs. Ty21a carrying empty plasmids (p<0.001). Inserts depict enlarged TNA titers between days 100 and 140 (the time points closer to the boost).
It was intriguing that while the PA specific IgG antibody responses in mice primed with 3 doses of Ty21a(pSECPA) and boosted with AVA exceeded those of mice primed and boosted with AVA, their TNA titers were an order of magnitude lower. We examined the relationship between PA IgG antibodies and TNA titers through correlation analysis for the different vaccine treatments (Figure 6) and found that the quality of the antibodies produced was vaccine dependent. Regardless of the boosting vaccine, Ty21a(pVDL9.3PA83ec) stimulated much lower overall IgG titers than Ty21a(pSEC10PA) (GMT: 352,222 vs. 2,496,295 EU/ml, p<0.001 and 102,793 vs. 338,513 vs. p<0.02 for AVA- and rPA-boosted groups, respectively) and yet achieved similar TNA levels (GMT: 551 vs. 349 ED50 and 193 vs. 129 and ED50 for AVA- and rPA-boosted groups, respectively) which indicates that proportion of antibodies with toxin neutralizing capacity was considerably higher (Figure 6). Although TNA titers slightly declined over time, the proportion of neutralizing antibodies increased (Figure 6 and data not shown), likely reflecting avidity maturation or shorter life of low affinity clones. Multiple doses of rPA and AVA elicited serum IgG antibodies with high capacity for toxin neutralization (Figure 6).
Figure 6.
Correlation of TNA antibody titers vs. PA IgG levels. Mice were primed with Ty21a(pSECPA) or Ty21a(pVDL9.3PA83ec) on days 0, 28 and 56 and boosted rPA (1 μg) or AVA on day 112. Control groups received 2 doses of AVA on days 0 and 112 (A) or 3 doses of rPA (10 μg/dose) on days 0, 28 and 56 (B). Data represent individual TNA and ELISA titers for each group on days 140 (A) and 180 (B) after primary immunization (28 and 68 days after the boost, respectively). Lines are plotted upon the GMT for each group.
Discussion
The threat of future terrorist attacks with biological weapons has driven the effort to develop a new generation of medical countermeasures capable of protecting at risk populations. While rapid identification of released agents, novel therapeutic interventions and passive immunization will have vital roles to play in mitigating the effects of a potential attack, a protective host-mediated immunity remains the most effective biodefense strategy [4]. Unfortunately, it is currently unfeasible to stimulate a protective immune response against anthrax in a naïve individual in a time frame likely to influence the course of an infection. In contrast, a previously immunized (primed) individual would be expected to rapidly respond to re-exposure to the same immunogen and the infectious agent.
We have demonstrated the ability of orally administered Salmonella expressing the protective antigen of B. anthracis to confer protection against a lethal spore challenge in mice [1]. Building up on these promising data we transferred PA expressing plasmids into the human licensed vaccine strain S. Typhi Ty21a and again demonstrated the ability of a mucosally delivered Salmonella-based vaccine to stimulate a potent immune response at levels previously found to be protective.
The two PA expression and export systems that we examined differed in the degree to which they activated the host immune system. While the ClyA-PA fusion (pSECPA) induced a pronounced PA specific IgG response, the PA-HlyA construct (pVDL9.3PA83ec) stimulated an extremely poor primary antibody response. These differences could be due to a combination of factors including promoter strength and plasmid copy number that can affect the amount of antigen expressed and secreted in vivo. With regard to promoter strength, the ompC promoter in pSECPA is optimally expressed in vivo whereas the T5 promoter in pVDL9.3 PA83ec is expressed constitutively, which can result in metabolic burden and plasmid instability in the absence of antibiotic selection and consequently lower in vivo expression. Differences in plasmid copy number may also affect the level of in vivo protein production. While the Ty21a(pSECPA) construct contains ∼15 copies of pSECPA per cell and hence 15 copies of the PA gene, Ty21a(pVLD9.3PA83ec) contains at most 6 copies of the same gene.
In addition to the amount of antigen delivered, the route by which the protein is exported from the bacterium and the manner in which the antigen is presented to the immune system can also have a profound influence on the quality of the resulting response. In the case of the ClyA-PA construct the immunogen is thought to be incorporated into a lipid vesicle derived from the outer membrane of the bacterium, which presumably enhances the immunogenicity of the protein following release. The inclusion of LPS, a well known trigger of innate immunity, in the membrane of the vesicle may also enhance the host response to the antigen [17]. In contrast, the HlyA haemolysin system directly exports the naked fusion protein to the external environment where it is subsequently captured and processed by the host immune system [16].
The immunogenicity of these vaccine constructs was investigated using a mucosal live vector prime followed by parenteral subunit vaccine boost. The efficiency of prime-boost regimes to enhance protective immunity has been increasingly recognized and different successful prime-boost combinations have been reported for a number of vaccine candidates [24;26-29]. The success of the prime-boosting approach using S. Typhi as a live vector was first described by Londono et al. who demonstrated enhanced protection in mice immunized with Helicobacter pylori urease-expressing strains followed by urease-alum boost [30]. Vindurampulle et. al later showed increased tetanus antitoxin in mice primed with S. Typhi CVD 908-htrA expressing tetanus toxin fragment C and boosted parenterally with tetanus toxoid [31]. Chinchilla et al further described enhanced immunity to Plasmodium falciparum circumsporozoite protein (PfCSP) in mice primed with CVD 908-htrA expressing PfCSP followed by a PfCSP-encoding DNA vaccine boost [32]. An intranasal S. Typhi live vector prime-parenteral protein boost strategy has been recently shown to improve immune response to B. anthracis PA in non-human primates [33] further supporting the use of Salmonella as a potential anthrax priming vaccine for humans.
The mechanisms underlying the prime-boost effects are not fully known but the immune system seems to recognize and respond better to recall antigens displayed in a different context and/or administered by a different route. The number of priming doses was found to affect the magnitude of the PA specific antibody recall responses. Not surprisingly animals that received three priming doses of Ty21a expressing PA mounted stronger antibody recall responses following protein boost than those that were given a single prime with Salmonella expressing PA. Interestingly, while the HlyA export system produced silent primary antibody responses, it was able to imprint a memory response which resulted in substantial recall antibody levels, similar to those achieved by the ClyA, following boosting with parenterally delivered rPA and the licensed US human AVA vaccine. The fact that mice immunized with Ty21a(pSECPA) already had very high levels of PA specific IgG at the time of the rPA boost may have blunted a further rise in response to the boost.
While the robust TNA antibody based recall response seen in these animals relates to the immunogenicity of the antigen, it also provides information on the recognition of protective epitopes and the likelihood of survival to a live agent challenge [1;4]. Albeit the peak TNA titers achieved by the live vector prime-protein boost were significantly lower than those elicited by multiple doses of rPA or AVA, they still surpassed the levels previously found to protect mice immunized with S. Typhimurium expressing PA against lethal aerosol spore challenge [1]. The reasons for the superior TNA responses after several doses of rPA or AVA compared with the Ty21a-PA prime-boost are unclear, but likely reflect the amount of antigen delivered (probably much lower using the live vectors), the antigen delivery vehicle and the route of inoculation.
To better understand the ability of the Ty21a constructs to stimulate a protective immune response we examined the relationship between PA IgG and TNA titers. While Ty21a(pVDL9.3PA83ec) stimulated much lower PA IgG titers than Ty21a(pSECPA), it achieved similar levels of TNA, suggesting that the antibody response stimulated by Ty21a(pVDL9.3PA83ec) contained a higher proportion of antibodies with toxin neutralizing capacity. This difference would indicate that the manner in which the antigen is presented to the immune system directly influences the level of protective immunity. Hence, future Salmonella vaccines should be engineered to maximize the stimulation of antibodies with TNA. Of note, the possibility that these S. Typhi-based vaccines also elicit cell-mediated immunity has not been explored in this work but will be the subject of future studies.
The data presented in this study demonstrate the feasibility of developing a prime-boost immunization strategy based on a licensed attenuated Salmonella vaccine. Such a strategy would be well suited to the military or at-risk personnel who could receive a self-administered oral priming with Salmonella vaccine encoding protective immunogens from potential bio-threat agents. In addition to stimulating protection against typhoid the vaccine would also imprint a memory response against biological weapons that could be activated at a later date if the individuals need to deploy to an at risk environment or in the event of a bioterror emergency. While boosting with a parenterally delivered protein based immunogen is effective, it does not lend itself to a mass vaccination strategy. In addition, the inclusion of the adjuvant alum makes these vaccines expensive to administer and stockpile. To address these issues, researchers are currently developing PA based vaccine formulations capable of stimulating rapid protection following needle-free delivery (nasal, oral or transcutaneous) and stable at room temperature to facilitate stockpiling and mass vaccination programs [4]. Nasal delivery has been shown in numerous animals studies to be an effective means of priming a protective systemic immune response to PA [34-36]. We were the first to demonstrate that nasally delivered PA microencapsulated with poly-L-lactide microspheres, could protect mice against a lethal aerosol spore challenge [35]. In conclusion, an immunization strategy in which individuals previously primed with an oral Salmonella vaccine are subsequently boosted with PA, preferably using a needle free delivery system, could represent an effective strategy for the protection of both military and civilian populations.
Acknowledgments
The authors thank Dr. Karina Ramirez for critical reading of the manuscript and personnel from the CVD Applied Immunology Section for outstanding technical support. This work was supported by NIH grants U19-AI-56578 to J. P. Nataro; AI-56578 (Project 1) to L.W. Baillie and AI-56578 (Project 5) and R01-AI065760 to M.F. Pasetti.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stokes MG, Titball RW, Neeson BN, et al. Oral administration of a Salmonella enterica-based vaccine expressing Bacillus anthracis protective antigen confers protection against aerosolized B. anthracis. Infect Immun. 2007 Apr;75(4):1827–34. doi: 10.1128/IAI.01242-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knight J. Delivering death in the mail. Nature. 2001 Dec 20;414(6866):837–8. doi: 10.1038/414837a. [DOI] [PubMed] [Google Scholar]
- 3.Baillie L, Read TD. Bacillus anthracis, a bug with attitude! Curr Opin Microbiol. 2001 Feb;4(1):78–81. doi: 10.1016/s1369-5274(00)00168-5. [DOI] [PubMed] [Google Scholar]
- 4.Baillie LW. Past, imminent and future human medical countermeasures for anthrax. J Appl Microbiol. 2006 Sep;101(3):594–606. doi: 10.1111/j.1365-2672.2006.03112.x. [DOI] [PubMed] [Google Scholar]
- 5.Wasserman GM, Grabenstein JD, Pittman PR, et al. Analysis of adverse events after anthrax immunization in US Army medical personnel. J Occup Environ Med. 2003 Mar;45(3):222–33. doi: 10.1097/01.jom.0000058345.05741.6b. [DOI] [PubMed] [Google Scholar]
- 6.Williamson ED, Hodgson I, Walker NJ, et al. Immunogenicity of recombinant protective antigen and efficacy against aerosol challenge with anthrax. Infect Immun. 2005 Sep;73(9):5978–87. doi: 10.1128/IAI.73.9.5978-5987.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Campbell JD, Clement KH, Wasserman SS, Donegan S, Chrisley L, Kotloff KL. Safety, reactogenicity and immunogenicity of a recombinant protective antigen anthrax vaccine given to healthy adults. Hum Vaccin. 2007 Sep;3(5):205–11. doi: 10.4161/hv.3.5.4459. [DOI] [PubMed] [Google Scholar]
- 8.Kew OM, Sutter RW, de Gourville EM, Dowdle WR, Pallansch MA. Vaccine-derived polioviruses and the endgame strategy for global polio eradication. Annu Rev Microbiol. 2005;59:587–635. doi: 10.1146/annurev.micro.58.030603.123625. [DOI] [PubMed] [Google Scholar]
- 9.Guzman CA, Borsutzky S, Griot-Wenk M, et al. Vaccines against typhoid fever. Vaccine. 2006 May 1;24(18):3804–11. doi: 10.1016/j.vaccine.2005.07.111. [DOI] [PubMed] [Google Scholar]
- 10.Dietrich G, Griot-Wenk M, Metcalfe IC, Lang AB, Viret JF. Experience with registered mucosal vaccines. Vaccine. 2003 Jan 30;21(7-8):678–83. doi: 10.1016/s0264-410x(02)00579-0. [DOI] [PubMed] [Google Scholar]
- 11.Gentschev I, Spreng S, Sieber H, et al. Vivotif--a ‘magic shield’ for protection against typhoid fever and delivery of heterologous antigens. Chemotherapy. 2007;53(3):177–80. doi: 10.1159/000100515. [DOI] [PubMed] [Google Scholar]
- 12.Pasetti MF, Levine MM, Sztein MB. Animal models paving the way for clinical trials of attenuated Salmonella enterica serovar Typhi live oral vaccines and live vectors. Vaccine. 2003 Jan 17;21(5-6):401–18. doi: 10.1016/s0264-410x(02)00472-3. [DOI] [PubMed] [Google Scholar]
- 13.Garmory HS, Brown KA, Titball RW. Salmonella vaccines for use in humans: present and future perspectives. FEMS Microbiology Reviews. 2002 Sep 1;752:1–15. doi: 10.1111/j.1574-6976.2002.tb00619.x. [DOI] [PubMed] [Google Scholar]
- 14.Garmory HS, Titball RW, Griffin KF, Hahn U, Bohm R, Beyer W. Salmonella enterica serovar typhimurium expressing a chromosomally integrated copy of the Bacillus anthracis protective antigen gene protects mice against an anthrax spore challenge. Infect Immun. 2003 Jul;71(7):3831–6. doi: 10.1128/IAI.71.7.3831-3836.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mackman N, Baker K, Gray L, Haigh R, Nicaud JM, Holland IB. Release of a chimeric protein into the medium from Escherichia coli using the C-terminal secretion signal of haemolysin. EMBO J. 1987 Sep;6(9):2835–41. doi: 10.1002/j.1460-2075.1987.tb02580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tzschaschel BD, Guzman CA, Timmis KN, de L V. An Escherichia coli haemolysin transport system-based vector for the export of polypeptides: export of Shiga-like toxin IIeB subunit by Salmonella typhimurium aroA. Nat Biotechnol. 1996 Jun;14(6):765–9. doi: 10.1038/nbt0696-765. [DOI] [PubMed] [Google Scholar]
- 17.Galen JE, Zhao L, Chinchilla M, et al. Adaptation of the endogenous Salmonella enterica serovar Typhi clyA-encoded haemolysin for antigen export enhances the immunogenicity of anthrax protective antigen domain 4 expressed by the attenuated live-vector vaccine strain CVD 908-htrA. Infect Immun. 2004 Dec;72(12):7096–106. doi: 10.1128/IAI.72.12.7096-7106.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wai SN, Lindmark B, Soderblom T, et al. Vesicle-mediated export and assembly of pore-forming oligomers of the enterobacterial ClyA cytotoxin. Cell. 2003 Oct 3;115(1):25–35. doi: 10.1016/s0092-8674(03)00754-2. [DOI] [PubMed] [Google Scholar]
- 19.Pickett TE, Pasetti MF, Galen JE, Sztein MB, Levine MM. In vivo characterization of the murine intranasal model for assessing the immunogenicity of attenuated Salmonella enterica serovar Typhi strains as live mucosal vaccines and as live vectors. Infect Immun. 2000 Jan;68(1):205–13. doi: 10.1128/iai.68.1.205-213.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pasetti MF, Pickett TE, Levine MM, Sztein MB. A comparison of immunogenicity and in vivo distribution of Salmonella enterica serovar Typhi and Typhimurium live vector vaccines delivered by mucosal routes in the murine model. Vaccine. 2000 Aug 1;18(28):3208–13. doi: 10.1016/s0264-410x(00)00142-0. [DOI] [PubMed] [Google Scholar]
- 21.Miller J, McBride BW, Manchee RJ, Moore P, Baillie LW. Production and purification of recombinant protective antigen and protective efficacy against Bacillus anthracis. Lett Appl Microbiol. 1998 Jan;26(1):56–60. doi: 10.1046/j.1472-765x.1998.00274.x. [DOI] [PubMed] [Google Scholar]
- 22.Quinn CP, Dull PM, Semenova V, et al. Immune responses to Bacillus anthracis protective antigen in patients with bioterrorism-related cutaneous or inhalation anthrax. J Infect Dis. 2004 Oct 1;190(7):1228–36. doi: 10.1086/423937. [DOI] [PubMed] [Google Scholar]
- 23.Li H, Soroka SD, Taylor TH, Jr, et al. Standardized, mathematical model-based and validated in vitro analysis of anthrax lethal toxin neutralization. J Immunol Methods. 2008 Apr 20;333(1-2):89–106. doi: 10.1016/j.jim.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 24.Woodland DL. Jump-starting the immune system: prime-boosting comes of age. Trends Immunol. 2004 Feb;25(2):98–104. doi: 10.1016/j.it.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 25.Albrecht MT, Li H, Williamson ED, et al. Human monoclonal antibodies against anthrax lethal factor and protective antigen act independently to protect against Bacillus anthracis infection and enhance endogenous immunity to anthrax. Infect Immun. 2007 Nov;75(11):5425–33. doi: 10.1128/IAI.00261-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Skeiky YA, Sadoff JC. Advances in tuberculosis vaccine strategies. Nat Rev Microbiol. 2006 Jun;4(6):469–76. doi: 10.1038/nrmicro1419. [DOI] [PubMed] [Google Scholar]
- 27.Robinson HL. HIV/AIDS vaccines: 2007. Clin Pharmacol Ther. 2007 Dec;82(6):686–93. doi: 10.1038/sj.clpt.6100408. [DOI] [PubMed] [Google Scholar]
- 28.Hill AV. Pre-erythrocytic malaria vaccines: towards greater efficacy. Nat Rev Immunol. 2006 Jan;6(1):21–32. doi: 10.1038/nri1746. [DOI] [PubMed] [Google Scholar]
- 29.Pasetti MF, Resendiz-Albor A, Ramirez K, et al. Heterologous prime-boost strategy to immunize very young infants against measles: pre-clinical studies in rhesus macaques. Clin Pharmacol Ther. 2007 Dec;82(6):672–85. doi: 10.1038/sj.clpt.6100420. [DOI] [PubMed] [Google Scholar]
- 30.Londoño-Arcila P, Freeman D, Kleanthous H, et al. Attenuated Salmonella enterica serovar Typhi expressing urease effectively immunizes mice against Helicobacter pylori challenge as part of a heterologous mucosal priming-parenteral boosting vaccination regimen. Infect Immun. 2002 Sep 1;70(9):5096–106. doi: 10.1128/IAI.70.9.5096-5106.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vindurampulle CJ, Cuberos LF, Barry EM, Pasetti MF, Levine MM. Recombinant Salmonella enterica serovar Typhi in a prime-boost strategy. Vaccine. 2004 Sep 9;22(27-28):3744–50. doi: 10.1016/j.vaccine.2004.03.025. [DOI] [PubMed] [Google Scholar]
- 32.Chinchilla M, Pasetti MF, Medina-Moreno S, et al. Enhanced immunity to Plasmodium falciparum circumsporozoite protein (PfCSP) by using Salmonella enterica serovar Typhi expressing PfCSP and a PfCSP-encoding DNA vaccine in a heterologous prime-boost strategy. Infect Immun. 2007 Aug;75(8):3769–79. doi: 10.1128/IAI.00356-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Galen JE, Chinchilla M, Wang JY, Arciniega-Marrtinez I, Pasetti MF, Levine MM. Non-human primate studies with a Salmonella Typhi-based anthrax vaccine; Tenth Annual Conference on Vaccine Research; Baltimore, MD. April 30-May 2; 2007. [Google Scholar]
- 34.Boyaka PN, Tafaro A, Fischer R, Leppla SH, Fujihashi K, McGhee JR. Effective mucosal immunity to anthrax: neutralizing antibodies and Th cell responses following nasal immunization with protective antigen. J Immunol. 2003 Jun 1;170(11):5636–43. doi: 10.4049/jimmunol.170.11.5636. [DOI] [PubMed] [Google Scholar]
- 35.Flick-Smith HC, Eyles JE, Hebdon R, et al. Mucosal or parenteral administration of microsphere-associated Bacillus anthracis protective antigen protects against anthrax infection in mice. Infect Immun. 2002 Apr;70(4):2022–8. doi: 10.1128/IAI.70.4.2022-2028.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gaur R, Gupta PK, Banerjea AC, Singh Y. Effect of nasal immunization with protective antigen of Bacillus anthracis on protective immune response against anthrax toxin. Vaccine. 2002 Jun 21;20(21-22):2836–9. doi: 10.1016/s0264-410x(02)00207-4. [DOI] [PubMed] [Google Scholar]