Abstract
Purpose of review
Hypertension and chronic kidney disease have become major public health challenges in China.
Recent findings
It is estimated that approximately 153 million Chinese adults had hypertension in 2002. It is also estimated that 2.33 million total cardiovascular deaths and 1.27 million premature cardiovascular deaths were attributable to increased blood pressure in 2005 in China. Approximately 39% of Chinese adult populations are highly sensitive to dietary sodium intake, a risk factor for hypertension and cardiovascular disease. The prevalence of chronic kidney disease varied greatly among studies due to differences in study populations and definitions of chronic kidney disease. A large prospective cohort study estimates that incidence and mortality of end-stage renal disease was 30.7 and 20.9 per 100,000 person-years among Chinese adults aged 40 years and older. Hypertension and the metabolic syndrome have been documented as risk factors for chronic kidney disease. In addition, a J-shaped association between body weight and incidence of end-stage renal disease and an inverse association between alcohol consumption and risk of end-stage renal disease were documented.
Summary
These results underscore the urgent need to develop national strategies for the prevention, detection, and treatment of hypertension and chronic kidney disease.
Keywords: Hypertension, Chronic kidney disease, China
Introduction
Hypertension is a major public health challenge worldwide because of its high prevalence and consequent increase in the morbidity and mortality of cardiovascular disease (CVD) and chronic kidney disease (CKD) (1). Kearney and colleagues pooled data from different regions of the world to estimate the overall prevalence and absolute burden of hypertension in 2000, and to project the global burden in 2025 (1). Overall, 26.4% of the world’s adult population in 2000 had hypertension (26.6% of men and 26.1% of women), and 29.2% were projected to have this condition by 2025 (29.0% of men and 29.5% of women). The estimated total number of adults with hypertension in 2000 was 972 million; 333 million in economically developed countries and 639 million in economically developing countries. The number of adults with hypertension in 2025 was predicted to increase by about 60% to a total of 1.56 billion. Most of this rise can be attributed to an expected increase in the number of people with hypertension in economically developing regions; the number of people with hypertension in economically developing countries was projected to increase by 80% from 639 million to 1.15 billion. On the basis of these estimates, almost three-quarters of the world’s hypertensive population will be in economically developing countries by 2025.
Lawes and colleagues assessed the global burden of disease attributable to systolic blood pressure (BP) ≥115 mmHg among individuals aged 30 years and older (2••). Worldwide, 7.6 million premature deaths (about 13.5% of the global total) and 92 million disability-adjusted life years (6.0% of the global total) were attributed to high BP. About 54% of stroke and 47% of ischemic heart disease worldwide were attributable to high BP. Overall, about 80% of the attributable burden occurred in low-income and middle-income economies, and over half occurred in people aged 45–69 years (2••). In addition, estimates for healthcare costs of treating non-optimal BP and its main clinical complications (stroke and myocardial infarction) for those over the age of 30 were US$370 billion globally in 2001. This represents about 10% of the world’s overall healthcare expenditures (3•). Although the majority of the current absolute expenditure occurs in high-income countries, an ever-increasing proportion of the cost is going to be carried by developing countries.
Burden of Blood Pressure-Related Disease in China
The burden of hypertension is high and increasing in the general population in China (4–6). The 2002 China National Nutrition and Health Survey reported the most recent information on the prevalence of hypertension in the general population in China (6••). Data on BP and use of antihypertensive medication were obtained from 141,892 Chinese adults aged 18 years and older. The study estimated that approximately 153 million Chinese adults were hypertensive in 2002. The prevalence of hypertension was 20% in men and 17% in women. The prevalence was higher in urban compared with rural areas in men (23% vs. 18%) and women (18% vs. 16%). Of the individuals with hypertension, only 24% were aware of their condition, 19% were treated and 5% were adequately controlled.
Hypertension is a major risk factor for CVD, stroke, CKD, and premature death in China (7–9). In a prospective cohort study of 169,871 Chinese men and women aged 40 years and older, Gu and colleagues reported a strong, linear, and independent relationship between BP levels and the risk of CVD, coronary heart disease (CHD), and stroke (7•). Systolic BP is a stronger predictor of CVD risk compared to diastolic BP. All hypertension subtypes were associated with significantly increased risk of CVD. For example, compared with normotensives, relative risks (95% CIs) of CVD incidence and mortality were 2.73 (2.60 to 2.86) and 2.53 (2.39 to 2.68) for combined systolic and diastolic hypertension, 1.78 (1.69 to 1.87) and 1.68 (1.58 to 1.78) for isolated systolic hypertension, 1.59 (1.43 to 1.76) and 1.45 (1.27 to 1.65) for isolated diastolic hypertension, 2.01 (1.64 to 2.48) and 1.61 (1.28 to 2.03) for treated hypertension with systolic BP <140 and diastolic BP <90 mm Hg, and 3.37 (3.07 to 3.69) and 2.88 (2.60 to 3.19) for treated hypertension with systolic BP ≥140 and/or diastolic BP ≥90 mm Hg, respectively, after adjustment for important covariables (8••).
In this large Chinese cohort study, prehypertension is related to an increased risk of CVD (9••). For example, compared with normotension (<120/80 mmHg), prehypertension (120–139/80–89mmHg) was significantly associated with an increased relative risk (95% CIs) of CVD incidence 1.34 (1.27, 1.42) and mortality 1.22 (1.15, 1.30). The population-attributable risk (PAR) associated with prehypertension was 10.6 and 7.1% for CVD incidence and mortality. The optimal 5-year number-needed-to-treat (NNT) to prevent a CVD event or death was 53 and 185, 17 and 51, and eight and 22 for prehypertension, stage-1 hypertension, and stage-2 hypertension, respectively. The optimal NNT to prevent a CVD event was significantly smaller in prehypertension patients with a history of CVD or diabetes (34 for incidence and 44 for mortality) compared with those without (115 for incidence and 352 for mortality). This study indicated that treatment of prehypertension among patients with a history of CVD or diabetes was as beneficial as treatment of stage-1 hypertensive patients without a history of CVD or diabetes (9••).
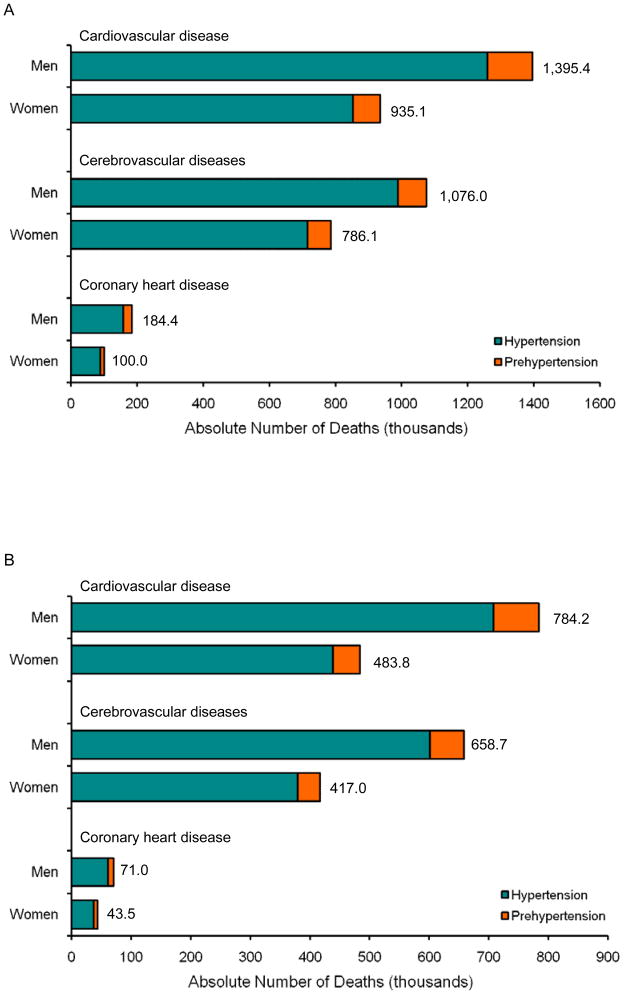
He and colleagues estimated that in 2005, 2.33 million (95% CI 2.21–2.45) CVD deaths were attributable to increased BP in China: 2.11 million (2.03–2.20) in adults with hypertension and 0.22 million (0.19–0.25) in adults with prehypertension (Figure 1). Additionally, 1.27 million (1.18–1.36) premature CVD deaths were attributable to raised BP in China: 1.15 million (1.08–1.22) in adults with hypertension and 0.12 million (0.10–0.14) in adults with prehypertension. Most BP-related deaths were caused by stroke: 1.86 million (1.76–1.96) total deaths and 1.08 million (1.00–1.15) premature deaths (10••).
Figure 1.
Absolute number of deaths from cardiovascular disease, cerebrovascular disease, and coronary heart disease attributable to hypertension and prehypertension by sex in China in 2005 (A) Total deaths. (B) Premature deaths. From He J, Gu D, Chen J, et al. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet. 2009; 374:1765–72.
Sodium-Sensitivity of Blood Pressure
Clinical trials have demonstrated that a reduced intake of dietary sodium lowers BP in both hypertensive and normotensive persons (11). BP reduction in response to a decrease in dietary sodium intake, however, may vary considerably among different individuals–a phenomenon described as sodium-sensitivity (12). The Genetic Epidemiology Network of Salt Sensitivity (GenSalt) study is a family-based dietary feeding study conducted in 1,906 Chinese adults. In GenSalt, a proportional change of mean arterial pressure (MAP) ≥5% was used to define sodium-sensitivity. Based on this criteria, the proportion with salt-sensitivity was 39% among Chinese adults (13••). Therefore, sodium-sensitivity appeared to be a common biological phenomenon in this Chinese population. In addition, sodium-sensitivity was more common in women and in persons who were older and had higher usual BP.
In the GenSalt study, a dose-response relationship between BP responses to the cold pressor test (CPT) and to dietary sodium interventions was identified (14••). After adjustment for important covariates, there were statistically significant associations between the quartiles of BP response to the CPT and BP response to the dietary sodium interventions (all p<0.0001). The GenSalt study also identified a strong, positive, and significant association between the metabolic syndrome and salt-sensitivity of BP among persons without diabetes (15••). Compared to those with zero, participants with 4 or 5 risk factors for the metabolic syndrome had a 3.54-fold increased odds (95% CI: 2.05, 6.11) of high sodium-sensitivity during the low-sodium intervention and a 3.13-fold increased odds (1.80, 5.43) of high sodium-sensitivity during the high-sodium intervention. This association was independent of age, gender, body-mass index (BMI), physical inactivity, cigarette smoking, alcohol consumption, and baseline dietary intake of sodium and potassium. In addition, the association between the metabolic syndrome and salt-sensitivity remained after the participants with hypertension were excluded (15••).
The association between genetic variants and sodium-sensitivity of BP has been examined in several studies (16,17). In the GenSalt study, several genetic variants were associated with sodium sensitivity in the Chinese population. For example, Kelly and colleagues reported a significant association between the rare α-adducin variant rs17833172 and systolic, diastolic, and MAP responses to high-sodium (p-values <0.0001) and diastolic BP response to low-sodium (p-value=0.002) (18•). Participants homozygous for the variant A allele of this marker had systolic, diastolic and MAP responses (95% CI) to high-sodium diet of 1.6 (−1.8, 4.9), −0.8 (−5.6, 4.0), and −0.1 (−4.0, 3.9) mmHg, respectively, vs. corresponding responses of 4.6 (2.5, 6.6), 1.7 (−0.2, 3.6), and 2.7 (0.9, 4.4) mmHg, respectively, for those who were heterozygous or homozygous for the G allele. In addition, participants with at least one copy of the A allele of SNP rs1129649 of the G protein β-polypeptide 3 (GNB3) gene had significantly decreased MAP response to low-sodium diet compared to homozygotes for the C allele (P value = 0.004) with responses of −3.4 (−3.8, −3.0) vs. −4.2 (−4.6, −3.8) mmHg, respectively. These data support a role for the ADD1 and GNB3 genes in sodium-sensitivity.
Burden of Chronic Kidney Disease in China
Several cross-sectional studies examined the prevalence of CKD in the general Chinese population (19–21). Chen and colleagues estimated the prevalence and absolute burden of CKD in a nationally representative sample of 15,540 adults aged 35 to 74 years in China (19). Glomerular filtration rate (GFR) was estimated using the simplified equation developed by the Modification of Diet in Renal Disease study. CKD was defined as an estimated GFR <60 mL/min/1.73m2. Overall, the age-standardized prevalences of CKD (GFR <60 mL/min/1.73m2) was 2.53%, representing 11,966,653 persons (1.31% or 3,185,330 men and 3.82% or 8,781,323 women). Although the prevalence of CKD in China was relatively low, the population absolute burden is substantial.
A more recent study on CKD prevalence was conducted in a representative sample of 13,925 adults in Beijing, China. CKD was defined as estimated-GFR <60 mL/min/1.73m2 or persistent albuminuria and hematuria. The prevalence of CKD in adults aged 18 years and older in Beijing was 13.0% from this study (20). In another population-based study among 6,311 residents aged 20 years and older from Guangzhou in south China, the prevalence of albuminuria, hematuria, reduced estimated GFR (<60 <60 mL/min/1.73m2), and overall CKD was 6.6%, 3.8%, 3.2%, and 12.1%, respectively (21). These data indicated that the prevalence of CKD was high in urban Chinese populations.
The number of patients who have end-stage renal disease (ESRD) and are treated by renal replacement therapy, dialysis, or transplantation has been increasing worldwide but the burden of ESRD in China is less well known. Reynolds and colleagues examined the incidence of ESRD in 158,365 Chinese men and women aged 40 year and older during an average follow-up of 8.3 years (22). The overall incidence and mortality of ESRD was 30.7 and 20.9 per 100,000 person-years among Chinese adults. The leading causes of ESRD were glomerulonephritis, diabetic nephropathy, and hypertensive nephrosclerosis (22).
Risk Factors for Chronic Kidney Disease
The risk factors for CKD and ESRD have been examined in several cross-sectional studies and one prospective cohort study in China (20–25). Chen and colleagues examined the relationship between the metabolic syndrome and risk of CKD in a cross-sectional survey in a nationally representative sample of 15,160 Chinese adults aged 35–74 years (23). The metabolic syndrome was defined as the presence of three or more of the following risk factors: elevated BP, low HDL-cholesterol, high triglycerides, elevated plasma glucose and abdominal obesity. CKD was defined as an estimated GFR<60 ml/min/1.73m2. The multivariate-adjusted odds ratios (95% CI) of CKD in participants with compared to those without the metabolic syndrome were 1.64 (1.16, 2.32). Compared to participants without any components of the metabolic syndrome, the multivariate-adjusted odds ratios (95% CI) of CKD were 1.51 (1.02, 2.23), 1.50 (0.97, 2.32), 2.13 (1.30, 3.50) and 2.72 (1.50, 4.93) for those with 1, 2, 3, and 4 or 5 components, respectively (23). These findings suggest that the metabolic syndrome is an important risk factor for CKD in Chinese adults.
Reynolds and colleagues examined the relationship between level of BP and incidence of ESRD in a prospective cohort study of 158,365 Chinese men and women who were 40 years and older at their baseline examination (22). Measurement of BP and covariables were made in 1991 following a standard protocol. Follow-up evaluations were conducted in 1999 to 2000 and included interviewing participants or proxies and obtaining medical records and death certificates for ESRD cases. Compared with those with normal BP, the multivariate adjusted hazard ratios (95% CI) of all-cause ESRD for prehypertension and stage-1 and stage-2 hypertension were 1.30 (0.98 to 1.74), 1.47 (1.06 to 2.06), and 2.60 (1.89 to 3.57), respectively (p< 0.001 for trend). The corresponding hazard ratios (95% CI) of glomerulonephritis-related ESRD were 1.32 (0.82 to 2.11), 1.48 (0.83 to 2.61), and 3.40 (2.02 to 5.74), respectively (p<0.001 for trend). Systolic BP was a stronger predictor of ESRD than diastolic BP or pulse pressure.
In the same study, a J-shaped association between BMI and all-cause ESRD was observed (24). Compared with those with normal body weight (BMI, 18.5 to 24.9 kg/m2), multivariate-adjusted relative risks (95% CI) for all-cause ESRD for underweight (BMI <18.5 kg/m2), overweight (BMI, 25.0 to 29.9 kg/m2), and obese subjects (BMI ≥30 kg/m2) were 1.39 (1.02 to 1.91), 1.21 (0.92 to 1.59), and 2.14 (1.39 to 3.29), respectively. The J-shaped association existed even after additional adjustment for systolic blood pressure and history of diabetes and cardiovascular disease. In addition, an inverse relationship between alcohol consumption and risk of ESRD was observed in this cohort study (25). Compared to non-drinkers, the relative risk of ESRD was 0.67 among men consuming less than 21 drinks per week and 0.52 among men consuming this amount or more after adjustment for age, geographic region, urbanization, education, BMI, physical activity, and cigarette smoking. The inverse association between alcohol consumption and ESRD existed even after adjustment for systolic BP, and history of diabetes and CVD.
Conclusion
Hypertension is the most common and leading preventable risk factor for premature deaths in China. It is estimated that approximately 153 million Chinese adults were hypertensive in 2002. It is also estimated that 2.33 million total CVD deaths and 1.27 million premature CVD deaths were attributable to increased BP in China. Sodium sensitivity, a risk factor for hypertension and CVD, is common in Chinese adult populations (approximately 39%). The prevalence of CKD varied greatly among studies due to differences in study population, methods for GFR estimation, and definition of CKD. A large prospective cohort study estimates that incidence and mortality of ESRD was 30.7 and 20.9 per 100,000 person-years among Chinese adults. Hypertension and the metabolic syndrome have been documented as risk factors for CKD. In addition, a J-shaped association between BMI and incidence of ESRD and inverse association between alcohol consumption and risk of ESRD were documented.
Acknowledgments
The Genetic Epidemiology Network of Salt Sensitivity is supported by research grants (U01HL072507, R01HL087263, and R01HL090682) from the National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD. Dr. Jing Chen was supported by a grant (P20-RR017659) from the National Center for Research Resources, National Institutes of Health, Bethesda, MD.
Footnotes
Disclosure: The authors declared no conflict of interest.
References and recommended reading
Papers of particular interest, published within the annual period of review, have been highlighted as:
• of special interest
•• of outstanding interest
- 1.Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2••.Lawes CMM, Vander Hoorn S, Rodgers A, et al. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–18. doi: 10.1016/S0140-6736(08)60655-8. Worldwide, 7.6 million premature deaths (about 13.5% of the global total) and 92 million disability-adjusted life years (6.0% of the global total) were attributed to high BP (≥115 mmHg systolic). About 54% of stroke and 47% of ischemic heart disease worldwide were attributable to high BP. [DOI] [PubMed] [Google Scholar]
- 3•.Gaziano TA, Bitton A, Anand S, et al. The global cost of nonoptimal blood pressure. J Hypertens. 2009;27:1472–7. doi: 10.1097/HJH.0b013e32832a9ba3. Estimates for healthcare costs attributed to suboptimal BP for those over the age of 30 were US$370 billion globally in 2001. This represents about 10% of the world’s overall healthcare expenditures. [DOI] [PubMed] [Google Scholar]
- 4.Wu X, Duan X, Gu D, et al. Prevalence of hypertension and its trends in Chinese populations. Int J Cardiol. 1995;52:39–44. doi: 10.1016/0167-5273(95)02443-z. [DOI] [PubMed] [Google Scholar]
- 5.Gu D, Reynolds K, Wu X, et al. Prevalence, awareness, treatment, and control of hypertension in China. Hypertension. 2002;40:920–7. doi: 10.1161/01.hyp.0000040263.94619.d5. [DOI] [PubMed] [Google Scholar]
- 6••.Wu Y, Huxley R, Li L, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118:2679–86. doi: 10.1161/CIRCULATIONAHA.108.788166. The present article estimated that the prevalence of hypertension was 20% in men and 17% in women in China. Of the individuals with hypertension, only 24% were aware of their condition, 19% were treated and 5% were adequately controlled. [DOI] [PubMed] [Google Scholar]
- 7•.Gu D, Kelly TN, Wu X, et al. Blood pressure and risk of cardiovascular disease in Chinese men and women. Am J Hypertens. 2008;21:265–72. doi: 10.1038/ajh.2007.59. This prospective cohort study in 169,871 Chinese men and women aged 40 years and older indicates that there is a strong, linear, and independent relationship between BP levels and the risk of CVD. Systolic BP is a stronger predictor of CVD risk compared to diastolic BP. [DOI] [PubMed] [Google Scholar]
- 8••.Kelly TN, Gu D, Chen J, et al. Hypertension subtype and risk of cardiovascular disease in Chinese adults. Circulation. 2008;118:1558–66. doi: 10.1161/CIRCULATIONAHA.107.723593. This prospective cohort study in 169,871 Chinese adults indicates that all hypertension subtypes are associated with significantly increased risk of CVD. Primary prevention of hypertension should be a public health priority in the Chinese population. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9••.Gu D, Chen J, Wu X, et al. Prehypertension and risk of cardiovascular disease in Chinese adults. J Hypertens. 2009;27:721–9. doi: 10.1097/HJH.0b013e328323ad89. This prospective cohort study in 169–871 Chinese adults aged 40 years and older indicates that prehypertension is related to an increased risk of CVD. Treatment of prehypertension among patients with a history of CVD or diabetes was as beneficial as treatment of stage-1 hypertensive patients without a history of CVD or diabetes. [DOI] [PubMed] [Google Scholar]
- 10••.He J, Gu D, Chen J, et al. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet. 2009;374:1765–72. doi: 10.1016/S0140-6736(09)61199-5. This study estimates that 2.33 million total CVD deaths and 1.27 million premature CVD deaths were attributable to increased BP in China in 2005. Most BP-related deaths were caused by cerebrovascular diseases. [DOI] [PubMed] [Google Scholar]
- 11.Whelton PK, He J, Appel LJ, et al. Primary Prevention of Hypertension. Clinical and Public Health Advisory from the National High Blood Pressure Education Program. JAMA. 2002;288:1882–1888. doi: 10.1001/jama.288.15.1882. [DOI] [PubMed] [Google Scholar]
- 12.Weinberger MH. Salt sensitivity of blood pressure in humans. Hypertension. 1996;27:481–490. doi: 10.1161/01.hyp.27.3.481. [DOI] [PubMed] [Google Scholar]
- 13••.He J, Gu D, Chen J, et al. Gender difference in blood pressure responses to dietary sodium intervention in the GenSalt study. J Hypertens. 2009;27:48–54. doi: 10.1097/hjh.0b013e328316bb87. This large, well-controlled feeding study indicated that BP responses to dietary sodium intake were normally distributed in populations and there was no evidence for a bimodal distribution. Sodium-sensitivity appears to be a common biological phenomenon in human populations. BP responses to dietary sodium intake were greater in women, those aged 45 years or older, and those with a higher baseline BP level. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14••.Chen J, Gu D, Jaquish CE, et al. Association between blood pressure responses to the cold pressor test and dietary sodium intervention in a Chinese population. Arch Intern Med. 2008;168:1740–6. doi: 10.1001/archinte.168.16.1740. This large population-based diet-feeding study identified a dose-response relationship between BP responses to the CPT and to dietary sodium interventions. This relationship was highly statistically significant and independent of other covariates. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15••.Chen J, Gu D, Huang J, et al. Metabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China: a dietary intervention study. Lancet. 2009;373:829–35. doi: 10.1016/S0140-6736(09)60144-6. This large population-based diet-feeding study identified a strong, positive, and significant association between the metabolic syndrome and salt-sensitivity of BP among persons without diabetes. The salt-sensitivity of BP increased progressively with a higher number of metabolic risk factors and this association was independent of age, gender, BMI, physical inactivity, cigarette smoking, alcohol consumption, and baseline dietary intake of sodium and potassium. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beeks E, Kessels AG, Kroon AA, van der Klauw MM, de Leeuw PW. Genetic predisposition to salt-sensitivity: a systematic review. J Hypertens. 2004;22:1243–9. doi: 10.1097/01.hjh.0000125443.28861.0d. [DOI] [PubMed] [Google Scholar]
- 17.Sanders PW. Dietary salt intake, salt sensitivity, and cardiovascular health. Hypertension. 2009;53:442–5. doi: 10.1161/HYPERTENSIONAHA.108.120303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18•.Kelly TN, Rice TK, Gu D, et al. Novel genetic variants in the alpha-adducin and guanine nucleotide binding protein beta-polypeptide 3 genes and salt sensitivity of blood pressure. Am J Hypertens. 2009;22:985–92. doi: 10.1038/ajh.2009.118. This study reported a significant association between genetic variants in the α-adducin (ADD1) gene and guanine nucleotide binding protein (G protein) β-polypeptide 3 (GNB3) gene and sodium-sensitivity of BP in the Chinese population. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen J, Wildman RP, Gu D, et al. Prevalence of decreased kidney function in Chinese adults aged 35 to 74 years. Kidney Int. 2005;68:2837–45. doi: 10.1111/j.1523-1755.2005.00757.x. [DOI] [PubMed] [Google Scholar]
- 20.Zhang L, Zhang P, Wang F, et al. Prevalence and factors associated with CKD: a population study from Beijing. Am J Kidney Dis. 2008;51:373–84. doi: 10.1053/j.ajkd.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 21.Chen W, Chen W, Wang H, et al. Prevalence and risk factors associated with chronic kidney disease in an adult population from southern China. Nephrol Dialysis Transplant. 2009;24:1205–12. doi: 10.1093/ndt/gfn604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reynolds K, Gu D, Muntner P, et al. A population-based, prospective study of blood pressure and risk for end-stage renal disease in china. J Am Soc Nephrol. 2007;18:1928–35. doi: 10.1681/ASN.2006111199. [DOI] [PubMed] [Google Scholar]
- 23.Chen J, Gu D, Chen CS, et al. Association between the metabolic syndrome and chronic kidney disease in Chinese adults. Nephrol Dial Transplant. 2007;22:1100–6. doi: 10.1093/ndt/gfl759. [DOI] [PubMed] [Google Scholar]
- 24.Reynolds K, Gu D, Muntner P, et al. Body mass index and risk of ESRD in China. Am J Kidney Dis. 2007;50:754–64. doi: 10.1053/j.ajkd.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 25.Reynolds K, Gu D, Chen J, et al. Alcohol consumption and the risk of end-stage renal disease among Chinese men. Kidney Int. 2008;73:870–6. doi: 10.1038/sj.ki.5002774. [DOI] [PubMed] [Google Scholar]