Abstract
Background
Monthly intravenous cyclophosphamide for six months has been the standard induction regimen for lupus nephritis, followed by a maintenance regimen of quarterly infusions for two years.
Methods
A prospective randomized trial of traditional IV cyclophosphamide (MIC, monthly IV cyclophosphamide 750 mg/m2 body mass index for 6 months followed by quarterly IV cyclophosphamide) versus high-dose (HDIC, 50 mg/kg daily for 4 days) was performed. Entry criteria included renal lupus, neurologic lupus, or other organ systems with moderate-to-severe activity.
Results
51 patients were randomized: 3 withdrew before treatment and one committed suicide two months after treatment with HDIC. Twenty-two had renal lupus, 14 had neurologic lupus and 11 “other” organ involvement. The outcome measure was the Responder Index for Lupus Erythematosus (complete response, partial response, no change or worsening). At six months (end of induction) 11/21 (52%) in the HDIC group had a complete response compared to 9/26 (35%) in the MIC group (p=.13). At the final visit (30 months), 10/21 (48%) in the HDIC group had a complete response, compared to 13/20 (65%) who continued on MIC (p=.13). Six patients crossed over from MIC to HDIC because of lack of response, of whom three became complete responders.
Conclusion
There was not strong evidence that monthly IV cyclophosphamide and high-dose cyclophosphamide differed in complete or in any (complete or partial) response for induction or maintenance therapy. However, nonresponders to monthly IV cyclophosphamide can sometimes be rescued by high-dose cyclophosphamide.
Introduction
Systemic lupus erythematosus (SLE) remains a therapeutic challenge. No new therapy has achieved US Food and Drug Administration (FDA) approval in over forty years. One of the most successful therapies for severe SLE has been monthly intravenous cyclophosphamide for 6 months followed by maintenance quarterly infusion for two years (1, 2). However, the side-effects of long-term exposure to cyclophosphamide include infection, bone marrow damage, malignancy, hemorrhagic cystitis and premature ovarian failure. Alternative therapies such as mycophenolate mofetil for lupus nephritis are neither more effective nor safer (3, 4).
High-dose cyclophosphamide without bone marrow transplant was first determined to be effective in severe aplastic anemia. A slow but progressive response was found suggesting induction of immunologic tolerance to autoantigens, in addition to potent immunosuppressive, without secondary clonal disease (5). Benefit was then found in multiple autoimmune diseases (6), including durable responses in SLE patients refractory to other therapies (7). Because stem cells were able to metabolize cyclophosphamide, they re-populated the bone marrow, reconstituting a naïve immune system. Other groups also found benefit of high-dose cyclophosphamide for SLE, but included stem cell rescue to shorten the period of aplasia (8, 9).
We sought to compare high-dose cyclophosphamide without stem cell rescue versus the traditional regimen of monthly intravenous cyclophosphamide for 6 months followed by quarterly intravenous cyclophosphamide for two years in terms of induction (6 month results), maintenance (final results) and safety in SLE patients with moderately to severely active SLE.
Methods
The trial (clinicaltrials.gov NCT00010400) was approved by the Johns Hopkins University School of Medicine Institutional Review Board. All patients signed informed consent. The trial was conducted at two sites, Johns Hopkins Hospital and Hahnemann Hospital. It was a prospective randomized trial (with 1:1 randomization) of traditional IV cyclophosphamide (MIC) (monthly IV cyclophosphamide 750 mg/m2 body mass index (BMI) for 6 months followed by quarterly IV cyclophosphamide) versus high-dose (HDIC) (50 mg/kg daily for 4 days). SLE patients after randomization were seen monthly for six months and then quarterly for two years.
Entry Criteria
SLE patients met four or more of the revised American College of Rheumatology classification criteria for SLE (10, 11), with moderate to severe activity as defined as an “A” score on the British Isles Lupus Activity Group (BILAG) measure (12), a high score for that organ on the Systemic Lupus Activity Measure (SLAM) (13) or hospitalization for that organ involvement. An additional requirement was lack of response or expected lack of response to moderate-to-high dose corticosteroids, equivalent degree of immunosuppression, or appropriate other treatment. During the trial the Data Safety Monitoring Committee added additional requirements including: a) SLE patients with cutaneous lupus needed to have failed combination therapy with both hydroxychloroquine and quinacrine as well as immunosuppression; and b) musculoskeletal lupus was removed from eligible organ involvement.
Randomization
Randomization was stratified by primary system involved: renal lupus, neurologic lupus or other organ involvement, to ensure equal numbers with each treatment for each type of patient.
Outcome Measures
The major outcome measure was response as determined by the Responder Index for Lupus Erythematosus. This measure defined complete response, partial response, no change or worsening for each organ manifestation and has been used in past studies of high-dose cyclophosphamide with stem cell rescue (9).
Renal
A complete response requires that the 24-hour urine (or equivalent) be less than 0.500, normal urine sediment, normal serum creatinine, and normal creatinine clearance (or equivalent measure of glomerular filtration rate). This outcome was analyzed at two time points: 6 months (the induction period) and 30 months (the maintenance period). For one patient, whose response at 30 months was not available, we substituted the patient’s response at 12 months.
Neurologic
For encephalopathy (acute confusional state, cerebritis, organic brain syndrome), worsening was defined as new coma or deteriorating level of consciousness, partial response was ≥ 50% improvement, and resolution was “not present”. For mononeuritis multiplex worsening was new mononeuropathy or progression of existing monneuropathy, partial response was improvement in sensory, motor or reflexes but not to normal in 3 months, and resolution was a normal neurologic examination.
Mucocutaneous
For discoid, worsening was new lesions or worsening (number, frequency or distribution), partial response was a decrease by ≥ 50% in number, frequency or distribution, and resolution was no lesions in 3 months. For vasculitis, worsening was new lesions or worsening (number, frequency or distribution), partial response was a decrease by ≥ 50% in number, frequency or distribution, and resolution was no lesions in 3 months.
Musculoskeletal
For arthritis, worsening was any new tender or swollen joint (even if synovitis in previous joints had improved), partial response was ≥ 50% reduction in tender or swollen joints, and resolution was no tender or swollen joints. For myositis, worsening was new myositis, or increasing weakness in 2 muscle groins, or increase of ≥ 50% in creatine kinase and for aldolase, partial response was a decrease by ≥ 50%, and resolution was no myositis.
Gastrointestinal
For gastrointestinal vasculitis, worsening was new or worsening symptoms or signs, partial response was improvement by imaging study such as endoscopy, and resolution was asymptomatic, stool negative for blood, and normal endoscopy or equivalent procedure.
Results
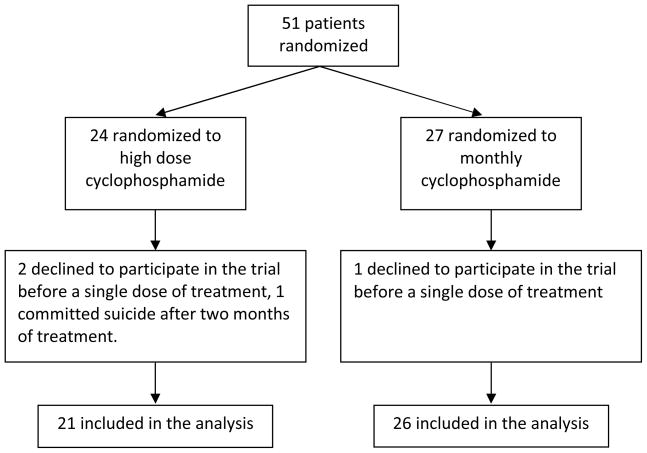
A total of 51 patients were randomized: 24 to high-dose IV cyclophosphamide, and 27 to monthly IV cyclophosphamide (Figure 1). Four patients were excluded from the primary analysis (3 who had withdrawn consent before taking a single dose and one who committed suicide after two months of HDIC treatment), leaving 21 and 26 patients in the two treatment groups.
Figure 1.
Patients Randomized in the Trial to High Dose and Monthly Dose Cyclophosphamide
Table 1 summarizes the characteristics of the participants. The large majority was female, and roughly half were enrolled due to renal disease activity.
Table 1.
The baseline characteristics of the 47 treated SLE patients
| Characteristic | Total | MIC group | HDIC group |
|---|---|---|---|
| Total | 47 | 26 | 21 |
| Gender | |||
| Male | 5 | 3 | 2 |
| Female | 42 | 23 | 19 |
| Ethnicity | |||
| White | 15 | 7 | 8 |
| Black | 25 | 15 | 10 |
| Hispanic | 4 | 2 | 2 |
| Asian | 3 | 2 | 1 |
| Age | |||
| 18–39 | 27 | 13 | 14 |
| 40–59 | 20 | 13 | 7 |
| Major Organ Involved | |||
| Renal | 22 | 12 | 10 |
| Neurologic | 14 | 7 | 7 |
| Other | 11 | 7 | 4 |
The induction (6 months) response is shown in Table 2. There was no difference in 6 month response for the total group (35% complete response with monthly IV cyclophosphamide versus 52% complete response with high-dose IV cyclophosphamide, p =.13). The 95% confidence interval for the difference in complete response between the two treatments ranged from −10% (i.e., the complete response rate was 10 percentage points better in the MIC group) to 45% (i.e., the complete response rate was 45 percentage points better in the HDIC group). In addition, there was no significant difference for any subset (renal SLE, or “other” organ involvement), but in both treatment groups, the response rate for patients with neurologic manifestations was much higher that the response rate for those with renal manifestations.
Table 2.
Response at 6 months, by study group and major organ system.
| Complete Response | Partial Response | No response | P-value (comparing groups with respect to complete response) | P-value (comparing groups with respect to any response) | |
|---|---|---|---|---|---|
| Overall | 0.131 | 0.131 | |||
| High Dose | 11 (52%) | 4 (19%) | 6 (29%) | ||
| Monthly | 9 (35%) | 4 (15%) | 13 (50%) | ||
| Renal | 1.02 | 1.02 | |||
| High Dose | 1 (10%) | 3 (30%) | 6 (60%) | ||
| Monthly | 1 (8%) | 4 (33%) | 7 (58%) | ||
| Neural | 0.462 | 0.462 | |||
| High Dose | 7 (100%) | 0 | 0 | ||
| Monthly | 5 (71%) | 0 | 2 (29%) | ||
| Other | 0.552 | 0.192 | |||
| High Dose | 3 (75%) | 1 (25%) | 0 | ||
| Monthly | 3 (43%) | 0 | 4 (57%) |
Based on a Mantel-Haenszel test controlling for system differences.
Based on Fisher’s Exact Test
The maintenance (30 month) response is shown in Table 3, with the subset of renal patients in Table 3A. Excluding 6 non-responsive MIC patients who crossed over to the HDIC group, the 6 monthly IV cyclophosphamide followed by quarterly IV cyclophosphamide group had a numerically superior complete response rate over high dose IV cyclophosphamide that did not reach statistical significance (65% vs 48%. p=0.13). The 95% confidence interval for the difference in complete response between the two treatments ranged from −47% (i.e., the complete response rate was 47 percentage points better in the MIC group) to 13% (i.e., the complete response rate was 13 percentage points better in the HDIC group). There was no difference in the maximum time of remission in days. There was some evidence that MIC resulted in better response among those in the renal subset (p=.081). Again, the neurologic SLE subset did the best (regardless of cyclophosphamide treatment group).
Table 3.
Response at 30 months, by study group and major organ system.
| Complete Response | Partial Response | No response | P-value1 (comparing groups with respect to complete response) | P-value1 (comparing groups with respect to any response) | |
|---|---|---|---|---|---|
| Overall | .132 | .442 | |||
| High Dose | 10 (48%) | 4 (19%) | 7 (33%) | ||
| Monthly | 13 (65%) | 2 (10%) | 5 (25%) | ||
| Crossover | 3 (50%) | 1 (17%) | 2 (33%) | ||
| Renal | .0813 | .0813 | |||
| High Dose | 2 (20%) | 2 (20%) | 6 (60%) | ||
| Monthly | 7 (64%) | 2 (18%) | 2 (18%) | ||
| Crossover | 1 (100%) | 0 | 0 | ||
| Neural | 1.03 | 1.03 | |||
| High Dose | 6 (86%) | 0 | 1 (14%) | ||
| Monthly | 5 (100%) | 0 | 0 | ||
| Crossover | 1 (50%) | 0 | 1 (50%) | ||
| Other | 1.03 | .143 | |||
| High Dose | 2 (50%) | 2 (50%) | 0 | ||
| Monthly | 1 (25%) | 0 | 3 (75%) | ||
| Crossover | 1 (33%) | 1 (33%) | 1 (33%) | ||
Compares high dose to monthly, ignoring the crossovers
Based on a Mantel-Haenszel test controlling for system differences.
Based on Fisher’s Exact Test.
Table 3A.
Renal Response
| High Dose Cyclophosphamide | ||
|---|---|---|
| Renal Biopsy Class | Baseline Urine Protein/24 hrs | End of Study* Urine Protein/24 hrs |
| III | 1.150 | 0.238 |
| III + V | 3.200 | 0.506 |
| III | 10.700 | 1.100 |
| IV +V | 7.400 | 1.485 |
| III + V | 1.078 | 1.173 |
| IV | 5.149 | 0.141 |
| V | 4.000 | 0.080 |
| III | 16.490 | 1.000 |
| IV + V | 4.380 | 0.065 |
| III | 4.500 | 8.044 |
| Monthly NIH regimen cyclophosphamide | ||
|---|---|---|
| Renal Biopsy Class | Baseline Urine Protein/24 hrs | End of Study * Urine Protein/24 hrs |
| III + IV | 3.862 | 0.862 |
| III | 2.800 | 0.640 |
| IV | 3.952 | 0.209 |
| III + V | 28.060 | 0.100 |
| III + V | 4.550 | 0.114 |
| IV | 0.560 | 0.080 |
| II + V | 6.580 | 0.150 |
| IV | 1.496 | 0.063 |
| III + V | 4.466 | 0.368 |
| IV | 0.840 | 0.110 |
| II + IV | 0.800 | 0.135 |
| V | 0.780 | 0.390 |
Or last visit before cross-over to alternate regimen
SLE patients not achieving a complete response were allowed to switch from the monthly IV cyclophosphamide group to high dose IV cyclophosphamide (Table 4). There was no particular pattern of organ subset that led to cross-over. Three patients achieved a complete response, two had no change, and one worsened.
Table 4.
Cross-over Patients from MIC to HDIC
| Organ System | Type | Response |
|---|---|---|
| Neurological | Cerebritis | complete response |
| Neurological | Mononeuritis Multiplex | complete response |
| Renal | FPGN (III) / DPGN (IV) | no change |
| Renal | DPGN (IV) | complete response |
| Cutaneous | Discoid | no change |
| Cutaneous | Discoid | worsening |
FPGN = focal proliferative glomerulonephritis
DPGN = diffuse proliferative glomerulonephritis
The response of antiphospholipid antibodies was also assessed in a subsample of patients. Among those with MIC, the median change in IgM anticardiolipin, from baseline to the end of the study was a reduction of 5.0 MPL (p=.0075). In contrast, among those in the HDIC group, the median change in IgM anticardiolipin was an increase of 4.5 MPL (p=.072 for a comparison between the groups with respect to median change in IgM anticardiolipin). Similarly, among those in the MIC group, the median change in IgG anticardiolipin was a decline of 5.0 GPL (p=.0013), whereas among those in the HDIC group, the median change was a decline of 2.5 GPL (p=.14 for a comparison between the groups).
There was no difference in serious adverse events, regardless of hospitalizations, serious infections, or deaths (Table 5). Hospitalizations for infections in the high dose group included pneumonia, zoster, neutropenic fever, pyelonephritis, staph bacteremia, genital herpes, and C. difficile. Hospitalizations for infection in the monthly group included pneumonia, line infection, BK virus, bronchitis, zoster, abscess, cellulitis, oral candida, meningococcemia, and otitis. One death occurred at Hahnemann Hospital in a patient in the HDIC arm. The patient died of pneumonia and pulmonary fibrosis attributable to SLE (determined by post-mortem examination), and was not related to cyclophosphamide. Premature ovarian failure occurred with both regimens. At 12 months, 3/10 (30%) of susceptible women in the HDIC group had premature ovarian failure, compared to 3/7(43%) of susceptible women in the MIC group (p=0.64).
Table 5.
Adverse Events
| HDIC | MIC | |
|---|---|---|
| total | total | |
| Hospitalizations (n) | 29 | 29 |
| Serious infections (n) + | 11 | 15 |
| Deaths (n) * | 1 late pneumonia/ARDS 1 suicide |
1 cardiac arrest |
There were no CMV, tuberculosus, or other opportunistic infections
-
breast cancer (randomized to HDIC)graft vs host disease (randomized to MIC)
The safety of high dose IV cyclophosphamide in SLE has previously been reported (7). In this trial, patients treated with high dose IV cyclophosphamide had an average of 10.2 ± 2.3 (± standard deviation) days where the WBC was less than 500, 3.8 ± 2.8 RBC transfusions and 4.4 ± 3.0 platelet transfusions.
Discussion
Cyclophosphamide remains a viable treatment for severe SLE, with several trials in lupus nephritis showing it to be equivalent to mycophenolate (3, 14, 15) and not toxic (3). However, the complete response rate with the traditional IV cyclophosphamide regimen for lupus nephritis was an astonishingly low 6% at 6 months in the trial of Ginzler et al. In lupus nephritis, the rapidity of response is highly correlated with retention of renal function (16). In an open-label series, we have had extensive experience with high-dose cyclophosphamide in SLE patients with severe disease resistant to other therapies, and found it to often give durable remissions (7). This experience has been mirrored by other groups using a variation, in which stem cell rescue is given after high dose cyclophosphamide to shorten the period of bone marrow aplasia (9).
This trial was very different from our open-label experience in that the trial represented the first use of cyclophosphamide for severe organ involvement. Complete response rates at 6 months were high (35% and 52%), but the lowest complete response rates were in the renal lupus subset (8% with monthly IV cyclophosphamide and 10% with high dose IV cyclophosphamide).
There was no statistically significant difference in complete response rates or duration of remission between the two groups at the final visit. However, given the small sample size, and the width of the confidence intervals for differences in response rates, this study cannot rule out the possibility that one treatment is substantially better than another. There was some suggestion that those in the renal SLE subset did better with monthly IV cyclophosphamide for 6 months followed by quarterly maintenance (p=.081). Thus, another important message from this trial is that monthly IV cyclophosphamide should remain the preferred cyclophosphamide regimen for lupus nephritis. However, the low 6 month complete response rate for renal lupus with either cyclophosphamide regimen makes it clear that other, more efficacious therapies need to be developed.
This study also replicated our open-label experience that SLE patients who had failed monthly IV cyclophosphamide could still achieve a complete response with high-dose IV cyclophosphamide, as occurred in three of the 6 crossovers. However, here there was no response for SLE patients with severe discoid lupus.
Neurologic SLE did the best, regardless of cyclophosphamide assignment. Our results indicate that either regimen of cyclophosphamide is very effective for severe neurologic lupus. The benefit of monthly IV cyclophosphamide for neurologic SLE has been known for some time (17).
Monthly IV cyclophosphamide led to greater reduction in antiphospholipid antibodies. Thus, we cannot recommend high-dose cyclophosphamide for SLE patients with antiphospholipid syndrome, although there are case reports of efficacy (18). However, even with monthly IV cyclophosphamide, the median reduction in anticardiolipin titers was not clinically important.
There were no differences in adverse events between the two cyclophosphamide regimens. We have previously reported our experience that the period of aplasia in SLE patients is limited, such that stem cell rescue is not required (7).
We were surprised that premature ovarian failure can occur after high-dose cyclophosphamide, since there is only ovarian exposure for 4 days. Given our findings, future use of high-dose cyclophosphamide (with or without stem cell rescue) in young women should include leuprolide as ovarian protection (19).
In conclusion, high-dose cyclophosphamide appeared to be equivalent to the traditional regimen in complete response rate, duration of remission, and toxicity. The subset of lupus nephritis, however, may do better with the traditional regimen.
Acknowledgments
Supported by NIAMS
Contributor Information
Michelle Petri, Email: mpetri@jhmi.edu, Professor of Medicine Division of Rheumatology, Johns Hopkins University School of Medicine, 1830 East Monument Street, Suite 7500, Baltimore, Maryland 21205, Phone: 410-955-3823, Fax: 410-614-0498.
Robert A. Brodsky, Director, Division of Hematology, Professor of Medicine and Oncology, Johns Hopkins University School of Medicine.
Richard J. Jones, Director, Bone Marrow Transplantation Program, Co-Director, Hematologic Malignancies Program, Professor of Oncology and Medicine, Johns Hopkins University School of Medicine.
Douglas Gladstone, Associate Professor of Medicine, The Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins University School of Medicine.
Michael Fillius, Division of Rheumatology, Johns Hopkins University School of Medicine.
Laurence S. Magder, Professor of Biostatistics, Division of Biostatistics and Bioinformatics, University of Maryland.
References
- 1.Klippel JH. Indications for, and use of, cytotoxic agents in SLE. Baillieres Clin Rheumatol. 1998;12(3):511–27. doi: 10.1016/s0950-3579(98)80033-2. [DOI] [PubMed] [Google Scholar]
- 2.Gourley MF, Austin HA, 3rd, Scott D, Yarboro CH, Vaughan EM, Muir J, et al. Methylprednisolone and cyclophosphamide, alone or in combination, in patients with lupus nephritis. A randomized, controlled trial. Ann Intern Med. 1996;125(7):549–57. doi: 10.7326/0003-4819-125-7-199610010-00003. [DOI] [PubMed] [Google Scholar]
- 3.Silva-Fernandez L, Nadig RS, Von Gizycki H, Ginzler EM. Efficacy, toxicity and tolerability of mycophenolate mofetil in patients with lupus nephritis, based on dose/weight ratio [abstract] Arthritis Rheum. 2007;56(9, Suppl):S211. [Google Scholar]
- 4.Appel GB, Contreras G, Dooley MA, Ginzler EM, Isenberg D, Jayne D, et al. Mycophenolate mofetil versus cyclophosphamide for induction treatment of lupus nephritis. J Am Soc Nephrol. 2009 May;20(5):1103–12. doi: 10.1681/ASN.2008101028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brodsky RA, Sensenbrenner LL, Jones RJ. Complete remission in severe aplastic anemia after high-dose cyclophosphamide without bone marrow transplantation. Blood. 1996;87:491–4. [PubMed] [Google Scholar]
- 6.Brodsky RA, Petri M, Smith BD, Seifter EJ, Spivak JL, Styler M, et al. Immunoblative high-dose cyclophosphamide without stem cell rescue for refractory, severe autoimmune disease. Ann Int Med. 1998;129:1031–5. doi: 10.7326/0003-4819-129-12-199812150-00007. [DOI] [PubMed] [Google Scholar]
- 7.Petri M, Jones RJ, Brodsky RA. High dose immunoblative cyclophosphamide without stem cell transplantation in systemic lupus erythematosus. Arthritis Rheum. 2003;48:166–73. doi: 10.1002/art.10752. [DOI] [PubMed] [Google Scholar]
- 8.Jayne D, Passweg J, Marmont A, et al. Autologous stem cell transplantation for systemic lupus erythematosis. Lupus. 2004;13:168–76. doi: 10.1191/0961203304lu525oa. [DOI] [PubMed] [Google Scholar]
- 9.Burt RK, Traynor A, Statkute L, Barr WG, Rosa R, Schroeder J, et al. Nonmyeloablative hematopoietic stem cell transplantation for systemic lupus erythematosus. J Amer Med Assoc. 2006;295:527–35. doi: 10.1001/jama.295.5.527. [DOI] [PubMed] [Google Scholar]
- 10.Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfeld NF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–7. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 11.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus [letter] Arthritis Rheum. 1997;40:1725. doi: 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 12.Isenberg DA, Rahman A, Allen E, Farewell V, Akil M, Bruce IN, et al. BILAG 2004. Development and initial validation of an updated version of the British Isles Lupus Assessment Group's disease activity index for patients with systemic lupus erythematosus. Rheumatology (Oxford, England) 2005 Jul;44(7):902–6. doi: 10.1093/rheumatology/keh624. [DOI] [PubMed] [Google Scholar]
- 13.Liang MH, Larson MG, Cullen KE, Schwartz JA. Comparative measurement efficiency and sensitivity of five health status instruemnts for arthritis research. Arthritis Rheum. 1985;28:542–7. doi: 10.1002/art.1780280513. [DOI] [PubMed] [Google Scholar]
- 14.Chan TM, Li FK, Tang CS, Wong RW, Fang GX, Ji YL, et al. Efficacy of mycophenolate mofetil in patients with diffuse proliferative lupus nephritis. Hong Kong-Guangzhou Nephrology Study Group. N Engl J Med. 2000 Oct 19;343(16):1156–62. doi: 10.1056/NEJM200010193431604. [DOI] [PubMed] [Google Scholar]
- 15.Ginzler EM, Dooley MA, Aranow C, Kim MY, Buyon J, Merrill JT, et al. Mycophenolate mofetil or intravenous cyclophosphamide for lupus nephritis. N Engl J Med. 2005 Nov 24;353(21):2219–28. doi: 10.1056/NEJMoa043731. [DOI] [PubMed] [Google Scholar]
- 16.Ioannidis JP, Boki KA, Katsorida ME, Drosos AA, Skopouli FN, Boletis JN, et al. Remission, relapse, and re-remission of proliferative lupus nephritis treated with cyclophosphamide. Kidney Int. 2000 Jan;57(1):258–64. doi: 10.1046/j.1523-1755.2000.00832.x. [DOI] [PubMed] [Google Scholar]
- 17.McCune WJ, Golbus J, Zeldes W, Bohlke P, Dunne R, Fox DA. Clinical and immunologic effects of monthly administration of intravenous cyclophosphamide in severe systemic lupus erythematosus. N Engl J Med. 1988;318:1423–31. doi: 10.1056/NEJM198806023182203. [DOI] [PubMed] [Google Scholar]
- 18.Gladstone DE, Prestrud AA, Pradhan A, Styler MJ, Topolsky DL, Crilley PA, et al. High- dose cyclophosphamide for severe systemic lupus erythematosus. Lupus. 2002;11(7):405–10. doi: 10.1191/0961203302lu229oa. [DOI] [PubMed] [Google Scholar]
- 19.Somers EC, Marder W, Christman GM, Ognenovski V, McCune WJ. Use of a gonadotropin-releasing hormone analog for protection against premature ovarian failure during cyclophosphamide therapy in women with severe lupus. Arthritis Rheum. 2005 Sep;52(9):2761–7. doi: 10.1002/art.21263. [DOI] [PubMed] [Google Scholar]