Abstract
Introduction:
Percutaneous nephrolithotomy (PCNL) has traditionally been performed on an inpatient basis. To the best of our knowledge, this is the first report of tubeless PCNL on a completely outpatient basis. The purposes of this study were to assess the safety and efficacy of outpatient PCNL.
Methods:
We reviewed the initial consecutive outpatient tubeless PCNLs performed at our institution by a single surgeon. Patients were discharged home the day of surgery only after meeting strict discharge criteria. Preoperative, intraoperative and postoperative data were collected prospectively.
Results:
Outpatient tubeless PCNL was performed in 3 patients. The mean maximum stone diameter was 14 mm. The average hospital stay was 175 minutes. All 3 patients were discharged home in stable condition after meeting all of the inclusion criteria. There were no emergency room visits or hospital readmissions postoperatively. The mean follow-up period was 47 days. All stones were calcium oxalate and the stone free rate was 100%. There were no minor or major complications.
Conclusion:
In properly selected patients, outpatient tubeless PCNL is safe and effective. Our initial experience with outpatient PCNL has been favourable and warrants further investigation in a larger patient population.
Introduction
Percutaneous nephrolithotomy (PCNL) is a widely accepted and employed operation for the removal of renal calculi.1,2 Despite the fact that many endourologic procedures are done on an outpatient basis, patients undergoing PCNL routinely require postoperative hospital admission.
The potential advantages of being able to offer patients PCNL as an outpatient operation are not insignificant, and include decreased pain due to lack of nephrostomy tube; earlier and quicker convalescence; lower rate of hospital acquired infections and complications; and significant potential cost savings to the health care system.
Over 20 years ago, Preminger and colleagues first described PCNL as an outpatient procedure to streamline PCNL and reduce costs.3 In their study, nephrostomy tubes were placed to provide hemostasis and drainage of the kidney and to minimize or prevent urinary extravasation. Despite this initial report of outpatient PCNL in 5 patients, over 2 decades later, very few, if any, endourologists are comfortable performing PCNL on an outpatient basis. With the advent of tubeless PCNL, the use of nephrostomy tubes is no longer thought to be necessary in all cases.4–7 Tubeless PCNL relies on ureteral stents to provide adequate drainage and reportedly causes less postoperative pain than traditional PCNL.7
To our knowledge, outpatient tubeless PCNL has not been reported in the literature to date. We describe our initial experience with the first 3 patients who underwent outpatient tubeless PCNL at our institution. Our objectives were to assess the safety and efficacy of performing tubeless PCNL on an outpatient basis, challenging the need for admission following PCNL in an appropriately selected patient population. We hypothesize that tubeless PCNL can be done safely and effectively on an outpatient basis in properly selected patients.
Methods
This is a case series of 3 outpatient PCNL operations done at our institution by a single surgeon (DB). All patients undergoing PCNL were considered for an outpatient PCNL procedure, but only those who met strict discharge criteria were discharged home the same day and included in our case series (Table 1).
Table 1.
Strict discharge criteria for outpatient tubeless percutaneous nephrolithotomy
| Preoperative considerations |
| Normal renal function (i.e.. serum creatinine <1.2 mg/dL or 106 μmol/L) No medical condition necessitating admission (i.e., ASA class 1 or 2) |
| Age >18 |
| Intraoperative considerations |
| Proper technique of percutaneous access at tip of calyx |
| No evidence of UTI (i.e., non-purulent urine and negative pre-op urine culture) |
| No dilation of a long narrow infundibulum |
| Minimal hemorrhage |
| No perforation of collecting system |
| Minimal (less than 2 minutes) or no intracorporeal lithotripsy |
| Stone free endoscopically and fluoroscopically |
| Operating room time <2 hours |
| Postoperative considerations |
| Minimal or no pain |
| Minimal or no flank leakage |
| No urinary retention |
| Minimal or no hematuria |
| Stable vital signs |
| Reliable patient, compliant with postoperative instructions |
| Patient lives/stays close to hospital, quick access to the emergency room |
ASA = American Society of Anesthesiologists; UTI = urinary tract infection.
After we received informed consent from our patients and administered prophylactic intravenous ampicillin and gentamicin, we induced general anaesthesia and each patient was placed in the prone position. The surgical technique used has been previously published,8 and included flexible cystoscopy and retrograde pyelography (Fig. 1); fluoroscopically-guided percutaneous renal access into the calyx of choice; guidewire passage into bladder; tract dilation; rigid nephroscopy and flexible nephroscopy, as necessary; removal of stones intact or minimal ultrasound lithotripsy with removal or suction of fragments; and antegrade or retrograde insertion of a ureteral stent. Postoperatively, patients were transferred to the recovery room for observation and Foley catheter removal. Once all medical discharge criteria were met, each patient was given verbal and written instructions regarding indications for returning to the emergency room. Oral antibiotics and analgesics were prescribed, and follow-up bloodwork, plain abdominal radiograph imaging and appointments were arranged, as necessary.
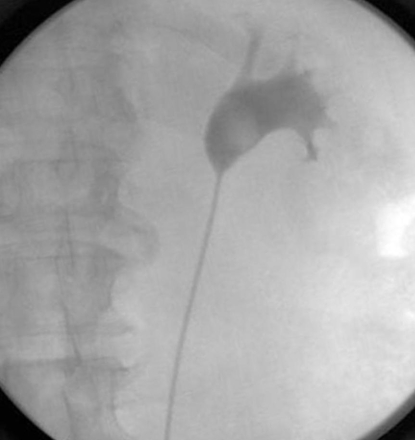
Fig. 1.
Retrograde pyelogram for Case 3, showing a 17-mm stone in the right renal pelvis.
Preoperative, intraoperative and postoperative data were collected and analyzed, with attention on the need for hospital readmission and/or emergency room assessment, postoperative complications and stone-free rates.
Results
Demographic data is shown in Table 2. The mean maximum stone diameter was 14 mm. Perioperative and follow-up results are shown in Table 3 and Table 4, respectively. The mean operating room time was 87 minutes. There were no minor or major intraoperative or postoperative complications. The mean time to discharge home following release from the recovery room was 2 hours and 55 minutes, taking into account that the first patient was mistakenly transferred to the surgical ward. There was no need for second look nephroscopy or any other ancillary procedure in any patient. All 3 patients were stone-free and no patient required re-hospitalization or a postoperative assessment in the emergency room.
Table 2.
Demographic and clinical preoperative data for the 3 outpatient cases of percutaneous nephrolithotomy
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age | 48 | 57 | 59 |
| Gender | Male | Male | Male |
| BMI, kg/m2 | 25.1 | 27.6 | 31.4 |
| No. of stones (size) | 1 (12 mm) | 2 (13 mm, 11 mm) | 1 (17 mm) |
| ASA Class | 2 | 2 | 2 |
| Stone location | Ureteropelvic junction | Renal pelvis, interpolar calyx | Renal pelvis |
| Side of involvement | Left | Right | Right |
| Contralateral Kidney | Normal | Normal | Normal |
| Renal anatomy | Normal | Normal | Normal |
| Preoperative creatinine, μmol/L | 75 | 70 | 92 |
| Preoperative hemoglobin, g/L | 156 | 144 | 148 |
BMI = body mass index; ASA = American Society of Anesthesiologists.
Table 3.
Perioperative data for the 3 outpatient cases of percutaneous nephrolithotomy
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Total operating room time, including cystoscopy and retrograde | 1hr, 35 min | 1 hr, 27 min | 1 hr, 20 min |
| Retrograde pyelogram findings | Stone, mild pelvicaliectasis | Stone, otherwise normal | Stone, pelviectasis, no caliectasis |
| Percutaneous access | Interpolar calyx | Lower pole calyx | Lower pole calyx |
| Ureteral stent | 28 cm x 6 Fr, retrograde technique | 26 cm x 7 Fr, retrograde technique | 26 cm x 6 Fr, antegrade technique |
| Intraoperative complications | None | None | None |
| Analgesia requirements in recovery room | None | None | Fentanyl 100 μg IV, acetaminophen with with codeine, 2 tablets orally, morphine 4 mg IV, Belladonna and Opium suppositories once |
| Length of postoperative stay in hospital after discharge from recovery room | 5 hr, 50 min* | 30 min | 2 hr, 25 min |
Patient was discharged to the floor erroneously.
Table 4.
Follow-up data for the 3 outpatient cases of percutaneous nephrolithotomy
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Length of follow-up | 19 days | 69 days | 35 days |
| Stone-free? | Yes | Yes | Yes |
| Stent indwelling time | 19 days | 17 days | 35 days |
| Stent symptoms? | No | No | No |
| Preoperative Hb / Postoperative Hb (g/L) | 156/154 | 144 / 151 | 148 / 151 |
| Preoperative creatinine / Postoperative creatinine (μmol/L) | 75/63 | 70/81 | 92/97 |
| Blood transfusion? | No | No | No |
| Postoperative complications | None | None | None |
| Stone analysis | Calcium oxalate | Calcium oxalate | Calcium oxalate/carbapatite |
Discussion
It is widely accepted and agreed that PCNL is an operation that necessitates postoperative admission to hospital. There are several reasons supporting the need for hospital admission following PCNL: observation for renal hemorrhage; indwelling nephrostomy tube for tamponade of any potential hemorrhage from the dilated tract and to ensure adequate drainage of kidney thus avoiding urinary stasis, leakage and infection; intravenous antibiotics to prevent urosepsis following this clean-contaminated operation; serial bloodwork to assess for hemorrhage, infection and renal function; radiography to rule out residual stones and/or renal obstruction; and observation for the development of medical complications or other non-hemorrhagic surgical complications.
Traditionally, nephrostomy tubes have been placed in the operating room immediately following PCNL. In the early years of PCNL, Winfield and colleagues reported removing the nephrostomy tube at the end of the operation if the kidney was stone-free, the collecting system remained intact and there was minimal bleeding.9 However, complications were reported in 2 cases where nephrostomy tubes were not used; then they soon became the standard of care.
Tubeless PCNL uses ureteral stents in the place of nephrostomy tubes for renal drainage. Several groups have demonstrated that tubeless PCNL can be safely performed without compromising outcomes.4–7 Some literature suggests an advantage of tubeless PCNL is that patients with ureteral stents have a lower analgesia requirement and return to work or normal activities sooner than those who receive nephrostomy tubes.4 Ureteral stents often cause significant morbidity, including bothersome pain, lower urinary tract symptoms, infection, and discomfort associated with stent removal, especially if a tether is not left and the patient requires cystoscopic removal of the stent. However, bothersome stent symptoms were not observed in our 3 patients.
Several groups have reported their experience with totally tubeless PCNL in patients with varying success.10–12 Totally tubeless PCNL avoids the use of nephrostomy tubes and ureteral stents, and relies upon ureteral peristalsis for kidney drainage. Crook and colleagues recommend this technique in patients with no or minimal residual stone burden and cautions against the totally tubeless approach in patients requiring upper renal access or patients with horseshoe kidneys.12
There have been significant advances in PCNL since it became the procedure of choice for large renal calculi.13 Refinements in the technique used to gain percutaneous access,14–16 the use of “one-step” balloon dilators,17,18 advances in intracorporeal lithotripsy devices,19–21 improvements in nephroscopes22 and tubeless PCNL4–7 have resulted in decreased morbidity without compromising stone-free rates. We believe that outpatient PCNL is a new advance that could potentially have a significant impact.
Due to limited resources and funds in most health care systems, there is a shift toward decreasing length of hospital stay and an interest in performing operations on an outpatient basis where possible. Outpatient PCNL offers several possible advantages, including more rapid patient convalescence, decreased incidence of postoperative nosocomial infections and cost savings to the health care system. Specific potential cost benefits include the cost of early postoperative imaging (kidneys-ureters-bladder radiograph or antegrade nephrostogram) that is often required prior to removal of nephrostomy tube, fee for the interventional radiologist, cost of nursing staff and care, cost of intravenous antibiotics and other medications and cost of the hospital bed for overnight stays. Although our case series does not provide a true cost analysis and conclusions cannot be drawn on potential cost savings, it is hard to argue with the fact that, in general, any outpatient operation holds potential financial advantages over the equivalent inpatient operation provided patients do not require postoperative readmission.
Although ambulatory PCNL has been previously reported,23 careful review of this study reveals that patients were admitted overnight for a stay of less than 24 hours. In our study, our PCNL operations were truly done on an outpatient basis; all patients were discharged within a few hours of their operation.
Our initial experience with outpatient tubeless PCNL has been very favourable. In this small series, we have demonstrated that outpatient tubeless PCNL can be performed safely and effectively; there were no complications and all 3 patients were stone-free. The critical factors to performing this procedure on an outpatient basis are patient selection and proper attention to technical details during percutaneous access. Patients must absolutely satisfy all predetermined preoperative, intraoperative and early postoperative requirements to qualify for an outpatient tubeless PCNL. The inclusion criteria in this study were very strict to ensure safety. Although supracostal puncture was not included in our study as an official exclusion criterion, we feel this would contraindicate outpatient PCNL. Patient education, compliance and reliability are especially crucial in case postoperative complications arise and medical care and/or surgical intervention are required. We fully acknowledge that for most patients, outpatient tubeless PCNL is not appropriate. However, with careful and proper patient selection, we believe that the outpatient procedure can be safely done with excellent outcomes, and could potentially become the standard of care for many patients.
We acknowledge the significant limitations of our study. This is a case series involving a very small number of patients. The potential for selection bias exists, but there were no patients who met the discharge criteria who were admitted postoperatively. Only 3 patients met the discharge criteria and all of them were discharged. Outpatient PCNL was not attempted in any other patients. Additionally, the stones treated were relatively small, and it is fair to question the need for PCNL when the mean maximum stone diameter was only 14 mm. However, all 3 patients were offered ureteroscopy and shock wave lithotripsy and they each wanted a single procedure with the highest chance of being rendered stone-free. We acknowledge that their decision may have been affected by the fact that we do not have a shock wave lithotriptor at our centre.
We believe a properly designed prospective randomized controlled clinical trial in patients who meet the discharge criteria and who are randomized to hospital admission versus discharge home would best determine the safety, efficacy and future role of outpatient PCNL. Future studies should also address the potential cost savings of outpatient PCNL.
Conclusion
In properly selected patient population, outpatient tubeless PCNL may be a safe and effective management option. The keys to successfully performing tubeless PCNL on an outpatient basis are proper technique for gaining percutaneous access and strict patient selection. Our initial experience with this procedure has been favourable and warrants further investigation with a larger patient population.
Footnotes
Competing interests: None declared.
This paper has been peer-reviewed.
References
- 1.Duvdevani M, Razvi H, Sofer M, et al. Third prize: contemporary percutaneous nephrolithotripsy: 1585 procedures in 1338 consecutive patients. J Endourol. 2007;21:824–9. doi: 10.1089/end.2007.9936. [DOI] [PubMed] [Google Scholar]
- 2.Al-Kohlany KM, Shokeir AA, Mosbah A, et al. Treatment of complete staghorn stones: a prospective randomized comparison of open surgery versus percutaneous nephrolithotomy. J Urol. 2005;173:469–73. doi: 10.1097/01.ju.0000150519.49495.88. [DOI] [PubMed] [Google Scholar]
- 3.Preminger GM, Clayman RV, Curry T, et al. Outpatient percutaneous nephrostolithotomy. J Urol. 1986;136:355–7. doi: 10.1016/s0022-5347(17)44867-1. [DOI] [PubMed] [Google Scholar]
- 4.Bellman GC, Davidoff R, Candela J, et al. Tubeless percutaneous renal surgery. J Urol. 1997;157:1578–82. [PubMed] [Google Scholar]
- 5.Delnay KM, Wake RW. Safety and efficacy of tubeless percutaneous nephrostolithotomy. World J Urol. 1998;16:375–7. doi: 10.1007/s003450050084. [DOI] [PubMed] [Google Scholar]
- 6.Goh M, Wolf JS., Jr Almost totally tubeless percutaneous nephrolithotomy: Further evolution of the technique. J Endourol. 1999;13:177–80. doi: 10.1089/end.1999.13.177. [DOI] [PubMed] [Google Scholar]
- 7.Limb J, Bellman GC. Tubeless percutaneous renal surgery: Review of first 112 patients. Urology. 2002;59:527–31. doi: 10.1016/s0090-4295(01)01627-2. [DOI] [PubMed] [Google Scholar]
- 8.Ko R, Soucy F, Denstedt JD, et al. Percutaneous nephrolithotomy made easier: a practical guide, tips and tricks. BJU Int. 2008;101:535–9. doi: 10.1111/j.1464-410X.2007.07259.x. [DOI] [PubMed] [Google Scholar]
- 9.Winfield HN, Weyman P, Clayman RV. Percutaneous nephrostolithotomy: Complications of premature nephrostomy tube removal. J Urol. 1986;136:77–9. doi: 10.1016/s0022-5347(17)44733-1. [DOI] [PubMed] [Google Scholar]
- 10.Aghamir SM, Hosseini SR, Gooran S. Totally tubeless percutaneous nephrolithotomy. J Endourol. 2004;18:647–8. doi: 10.1089/end.2004.18.647. [DOI] [PubMed] [Google Scholar]
- 11.Gupta V, Sadasukhi TC, Sharma KK, et al. Tubeless and stentless percutaneous nephrolithotomy. BJU Int. 2005;95:905–6. doi: 10.1111/j.1464-410X.2005.05432.x. [DOI] [PubMed] [Google Scholar]
- 12.Crook TM, Lockyer CR, Keoghane SR, et al. Totally tubeless percutaneous nephrolithotomy. J Endourol. 2008;22:267–71. doi: 10.1089/end.2006.0034. [DOI] [PubMed] [Google Scholar]
- 13.Deane LA, Clayman RV. Advances in percutaneous nephrostolithotomy. Urol Clin North Am. 2007;34:383–95. doi: 10.1016/j.ucl.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Ko R, Soucy F, Denstedt JD, et al. Percutaneous nephrolithotomy made easier: a practical guide, tips and tricks. BJU Int. 2008;101:535–9. doi: 10.1111/j.1464-410X.2007.07259.x. [DOI] [PubMed] [Google Scholar]
- 15.Miller NL, Matlaga BR, Lingeman JE. Techniques for fluoroscopic percutaneous renal access. J Urol. 2007;178:15–23. doi: 10.1016/j.juro.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 16.Marcovich R, Smith AD. Percutaneous renal access: tips and tricks. BJU Int. 2005;95(Suppl 2):78–84. doi: 10.1111/j.1464-410X.2005.05205.x. [DOI] [PubMed] [Google Scholar]
- 17.Pathak AS, Bellman GC. One-step percutaneous nephrolithotomy sheath versus standard two-step technique. Urology. 2005;66:953–7. doi: 10.1016/j.urology.2005.05.031. [DOI] [PubMed] [Google Scholar]
- 18.Maynes LJ, Desai PJ, Zuppan CW, et al. Comparison of a novel one-step percutaneous nephrolithotomy sheath with a standard two-step device. Urology. 2008;71:223–7. doi: 10.1016/j.urology.2007.09.048. [DOI] [PubMed] [Google Scholar]
- 19.Kim SC, Matlaga BR, Tinmouth WW, et al. In vitro assessment of a novel dual probe ultrasonic intracorporeal lithotriptor. J Urol. 2007;177:1363–5. doi: 10.1016/j.juro.2006.11.033. [DOI] [PubMed] [Google Scholar]
- 20.Hofmann R, Olbert P, Weber J, et al. Clinical experience with a new ultrasonic and LithoClast combination for percutaneous litholapaxy. BJU Int. 2002;90:16–9. doi: 10.1046/j.1464-410x.2002.02814.x. [DOI] [PubMed] [Google Scholar]
- 21.Rané A, Kommu SS, Kandaswamy SV, et al. Initial clinical evaluation of a new pneumatic intracorporeal lithotripter. BJU Int. 2007;100:629–32. doi: 10.1111/j.1464-410X.2007.07003.x. [DOI] [PubMed] [Google Scholar]
- 22.Andonian S, Okeke Z, Anidjar M, et al. Digital nephroscopy: the next step. J Endourol. 2008;22:601–2. doi: 10.1089/end.2008.0019. [DOI] [PubMed] [Google Scholar]
- 23.Singh I, Kumar A, Kumar P. “Ambulatory PCNL” (tubeless PCNL under regional anesthesia): a preliminary report of 10 cases. Int Urol Nephrol. 2005;37:35–7. doi: 10.1007/s11255-004-6706-9. [DOI] [PubMed] [Google Scholar]