Abstract
Background
Ingrown toenail, or onychocryptosis, is a common source of morbidity worldwide. The current standard of care focuses on the nail as the causative agent, and, in cases that are resistant to medical management, surgical correction via nail avulsion and phenol matrix ablation is used. Unfortunately, this treatment leads to poor cosmetic results, high rates of recurrence and low patient satisfaction.
Methods
We retrospectively reviewed a case series of 124 consecutive patients who underwent surgical correction of ingrown toenails from 1988 to 2004. We recorded the operative technique and postoperative wound healing via photographs. We assessed outcomes and patient satisfaction using self-reports and 7-point Likert scale questionnaires.
Results
Our surgical approach involved the excision of excessive nail-fold granulation tissue with preservation of the nail and its matrix. In total, 72.5% of patients were under the age of 29 (69.4% men). Before surgical intervention, 78.8% of patients scored their pain as severe, 69.9% had difficulty wearing normal footwear and 64.3% had difficulty with normal activities because of their ingrown toenails. A total of 212 surgical sites were analyzed, with a median follow-up of 8 years. No recurrences were identified in any patients (100%, n = 124). Overall, 94.3% (n = 116) stated that they were highly satisfied with the procedure. Only 1.6% (n = 2) reported a loss of sensation at the surgical site.
Conclusion
Surgical correction of ingrown toenails via soft-tissue excision of the nail folds, coupled with preservation of the nail and its matrix, had excellent cosmetic results, no recurrences and high rates of patient satisfaction.
Ingrown toenails are frequently encountered in clinical practice, with an estimated 10 000 new cases per year in the United Kingdom.1 Young men are most frequently affected, and the associated morbidities have significant economic impact, secondary to decreased mobility and work absenteeism.1,2 Currently, a wide variety of treatment options exist; however, they are associated with poor cosmetic results, low rates of patient satisfaction and high rates of recurrence.1–5
Initial treatment of an ingrown toenail, or onychocryptosis, is conservative management, including avoiding tight-fitting shoes and using warm water baths and soft compresses.6 Surgical intervention is ultimately required in refractory cases. Many approaches have been described, with most targeting the nail as the causative agent. Partial nail avulsion coupled with chemical destruction of the nail matrix (matricectomy) with phenol remains the most preferred surgical technique.1,6–8
Vandenbos and Bowers9 suggested that pressure necrosis of the soft tissue surrounding the nail contributes to the pathogenesis of ingrown toenails. Indeed, increased nail-fold skin width in patients with ingrown toenails, greater weight-bearing on the soft tissue of the nail fold and repetitive rotation of the toe have all been suggested to be important contributing factors.8–10 A study by Pearson and colleagues11 helped to draw the focus away from the nail as the causative agent. They reported no differences in the shape of the toenails among patients with ingrown toenails and healthy controls. It is tempting to speculate that the current surgical interventions that target the nail (i.e., nail avulsion and matricectomy) do not directly address the causative soft-tissue pathology.
In this study, we used a modification of the surgical approach described by Vandenbos and Bowers9 in a large patient population to show that soft-tissue nail-fold resection leads to surgical correction of ingrown toenails. Our approach yields excellent cosmetic results with no recurrences and high rates of patient satisfaction. The treatment is cost effective, technically simple and can be performed easily in any physician’s office.
Methods
We retrospectively reviewed the charts of 126 consecutive patients who underwent surgical correction of ingrown toenails between 1988 and 2004. All surgeries were performed at the Thorndale Lions Medical Centre in Thorndale, Ontario. A single doctor (H.C.) performed and/or supervised all operations.
All of the patients in this case series had detailed medical histories obtained and physical examinations performed before surgical intervention. Initial conservative management strategies attempted before consultation included alterations in footwear, soft compresses, saline soaks and rest. Of the patients studied, 22.8% had previous failed attempts to surgically correct their ingrown toenails by other physicians. No exclusion criteria were set, and a consecutive cohort of patients was used (n = 126). Patients lost to follow-up (n = 2) were not included in the analysis.
To subjectively assess outcomes, we mailed a standardized questionnaire to all patients. Each questionnaire was identical and involved patient self-assessment with responses recorded on a 7-point Likert scale. The questions were scored with a value of 1 as “strongly agree” and a value of 7 as “strongly disagree.” In cases where the results were taken as aggregates, “agree” was the combined totals for values 1–3 and “disagree” was the combined values of 5–7. A value of 4 was “neutral.”
Statistical analyses were performed using GraphPad Prism software, and the means are reported.
Surgical approach
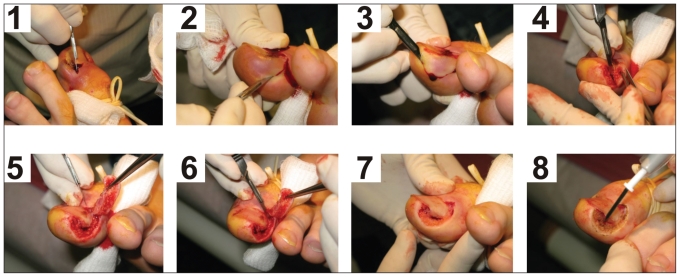
We used the fundamental principles of the surgical technique initially described by Vandenbos and Bowers9 for all procedures (Fig. 1). The details of the procedure used in the current study are shown in Figure 2. First, the involved toe was prepared in a sterile fashion, and ring nerve block anesthesia was applied with 2% xylocaine without epinephrine. An elastic tourniquet was placed at the base of the toe to maintain a clear and bloodless surgical field and to allow local anesthetic penetration into the tissue. An initial incision of 5 mm was made proximally from the base of the nail, about 3 mm from the border of the nail at the proximal nail fold. Care was taken to leave the nail matrix intact. An elliptical sweep was made out to the side and bottom of the toe, extending distally to encompass all involved granulation tissue and nail-fold skin (Fig. 1, Fig. 2). The incision was continued superiorly to end up under the tip of the nail about 3–5 mm in from the edge. All skin and subcutaneous tissues at the edge of the nail were removed. The excision was generous and adequate, often leaving a skin and soft-tissue defect measuring 1.5 × 3 cm and occasionally exposing a portion of the distal phalanx. Application of silver nitrate or electrocautery was used to reduce postoperative bleeding by lightly cauterizing areas along the skin edge and subcutaneous nail bed. Care was taken at all times to not damage the nail matrix. The wound was then allowed to close via secondary intention.
Fig. 1.
Examples of the severity of ingrown toenails surgically corrected by soft-tissue nail-fold excision. The preoperative appearance (left) highlights the extensive medial and lateral nail-fold granulation tissue. The images obtained in the postoperative period (centre, right) show the surgical site following nail-fold excision. The excision of soft tissue was typically generous and adequate, with all portions of the granulation tissue removed.
Fig. 2.
The soft-tissue nail-fold excision procedure for ingrown toenails. In step 1, the toe is cleansed with an iodine solution, and ring block anesthesia is applied with 2% xylocaine without epinephrine. A tight elastic tourniquet is placed at the base of the toe to maintain a clear surgical field. An initial incision of 5–10 mm is made proximally from the base of the nail and about 3–5 mm from the lateral border of the nail to encompass the proximal nail fold. Care is taken to leave the nail matrix intact. In steps 2 to 4, the lateral nail fold is excised using a lateral elliptical sweep that proceeds distally to encompass all involved granulation tissue and adjacent soft tissues. In steps 5 and 6, all skin and subcutaneous tissues at the edge of the nail is removed. Occasionally, a portion of the distal phalanx is exposed. The operative site following complete excision of soft-tissue nail folds is shown in step 7. Note the intact nail and preservation of the nail matrix. The applied tourniquet successfully minimizes bleeding in the surgical field. In step 8, electrocautery is used to obtain hemostasis, and the wound is left open to close by secondary intention following the application of gauze dressings.
Mesh tulle gauze (10 × 10 cm) was folded and applied over the site of the excision followed by 2 gauze pads (5 × 5 cm) and a snug dressing of rolled gauze (5-cm width). The patients were instructed to soak their feet after 48 hours in a warm water bath for 15–20 minutes, during which time the dressings were removed and replaced with new clean dressings. Patients were instructed to subsequently soak their toes 3 times per day for 15–20 minutes in a warm water bath for 4–6 weeks. Pain control was achieved with acetaminophen–codeine or ibuprofen or both. No antibiotics were prescribed. Patients were followed in the family medicine clinic once per week for 4–6 weeks to monitor healing (Fig. 3). The patients were advised that, once healed they could trim their nails in any way they liked and that they could wear any footwear they choose.
Fig. 3.
Images showing healing by secondary intention following surgical nail-fold excision. Post-op = postoperative.
Results
Our study population was a consecutive cohort of 126 patients (2 were lost to follow-up) who underwent surgical correction of ingrown toenails. As shown in Figures 1, 2 and 3, patients with even the most severe stages of the condition were treated. Given the high recurrence rates for nail and matrix ablation,1,6–8 we used a technique involving only soft-tissue excision. This approach was pioneered by Vandenbos and Bowers9 and is illustrated in Figures 1 and 2.
Most patients were under the age of 29 (72.5%), with a 69.4% male predominance (Table 1). This patient population is representative and corresponds to previously published work.2,12 To appropriately assess the effectiveness of our surgical intervention, we calculated follow-up times based on surgical site. This was done to account for several patients who had ingrown toenails on different toes at different times of onset.
Table 1.
Demographic characteristics of 124 patients who underwent surgical correction of ingrown toenails
| Characteristic | % of patients |
|---|---|
| Age, yr | |
| < 19 | 50.8 |
| 20–29 | 21.7 |
| 30–39 | 8.3 |
| 40–49 | 9.2 |
| 50–59 | 5.0 |
| > 60 | 5.0 |
| Sex | |
| Male | 69.4 |
| Female | 30.6 |
We conducted surgeries on 124 patients (164 toes) with a total of 212 surgical sites. Specifically, this included 65 left lateral, 38 left medial, 68 right lateral and 41 right medial toes. The follow-up times per surgical site were a mean of 4.8 years and a median of 8 years. Antibiotics were not prescribed before surgery, and no cases of infection or osteomyelitis were reported.
We initially sought to determine the characteristics of patients requiring surgical correction of ingrown toenails. Preoperatively, we asked how many of our patients experienced severe pain before surgery. In total, 78.8% of patients agreed, with 26.8% strongly agreeing, that they experienced severe pain (Table 2). In all, 69.9% of patients stated that they had difficulty wearing normal footwear, and 64.3% reported having difficulty with normal activities because of their ingrown toenails (Table 2). As such, most of our patients were significantly affected by their condition.
Table 2.
Preoperative responses of patients who underwent surgical correction of ingrown toenails
| Characteristic | % of patients |
|---|---|
| No prior treatment of the affected toe | 77.2 |
| Experienced severe pain | |
| Strongly agree | 78.8 |
| Neutral | 13.0 |
| Strongly disagree | 8.2 |
| Difficulty with regular footwear | |
| Strongly agree | 69.9 |
| Neutral | 10.6 |
| Strongly disagree | 19.5 |
| Difficulty with regular activities | |
| Strongly agree | 64.3 |
| Neutral | 12.2 |
| Strongly disagree | 23.6 |
To estimate postoperative recovery time, we asked patients if it took longer than 1 week to return to some normal activities. In total, 53.2% agreed and 13.7% strongly disagreed; 79% stated that it took less than 4 weeks to return to all normal activities.
A major postoperative complication that can occur following excision of soft tissue is a loss of cutaneous innervation.1 In our population, 88.7% of patients agreed that they did not have any loss of sensation around the operative site. However, 1.6% (n = 2) stated that they had significant loss of sensation around the area of surgery. The remainder had minimal loss of sensation (9.7%).
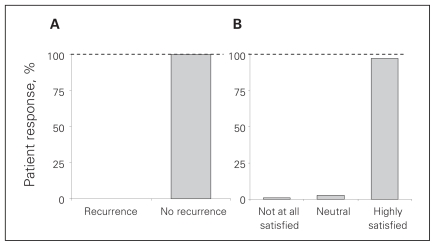
Previous studies targeting the nail have reported high rates of recurrences with subsequent low rates of patient satisfaction.1,3–5,7 In our cohort, 100% (n = 124 patients, 212 surgical sites) of patients reported that the problem had not recurred (Fig. 4). Our questionnaire defined recurrence as the patient requiring “further medical or surgical treatment on the area where the nail-fold excision was performed.” The question was direct and required a “yes” or “no” answer. We further sought to ensure appropriate responses by asking patients if “the problem they had surgically corrected reappeared at the same location.” The responses to this question were directly correlated with the finding that no patients experienced a direct recurrence.
Fig. 4.
Postoperative recurrence (A) and patient satisfaction (B) in 124 patients (212 sites) following surgical correction of ingrown toenails using soft-tissue nail-fold excision.
On chart review, we found that 1 patient experienced a fungal nail infection 5 years after surgery and another experience a traumatic foot injury, neither of which were counted as recurrences. Overall, 94.3% of respondents (n = 116) strongly agreed that they were satisfied with the procedure (n = 107), and none of the patients were highly dissatisfied with the surgery.
Discussion
Ingrown toenails are common worldwide, and diverse treatment options exist.1 An ideal surgical technique is not currently available, but theoretically, such an approach would be technically simple, cost effective and yield good cosmetic results with low recurrence rates. Furthermore, the procedure would be done on an outpatient basis with a quick return to normal activities and low complication rates. The approach described in this study meets all of these criteria and is the first to detail the long-term outcomes of soft-tissue nail-fold excision in the treatment of ingrown toenails.
Multiple surgical approaches to the correction of ingrown toenails have been suggested. Initially, the preferred treatment was simple nail avulsion alone; however, this approach has fallen out of favour given the high recurrence rates (about 70%).13,14 Unfortunately, the current standard of care (partial nail avulsion and matrix ablation) is still associated with poor outcomes. A randomized control trial comparing nail matrix destruction using either surgical excision or phenol ablation reported recurrence rates at 1 year to be 13.8% for phenol ablation and 40.7% for surgical excision.7 A more recent trial noted an improved but still unsatisfactory 1-year recurrence rate of 6.9% for partial nail avulsion and surgical matricectomy.4 Other studies have also found differences in recurrence rates among the types of physicians performing the procedure. Overall recurrence rates of 34% were found when the surgery was performed by general practitioners with an increase to 50% when performed by general surgeons.5 Not surprisingly, the level of patient satisfaction reflects these poor results.1
The belief that the nail is the causative agent is so ingrained in modern medicine that a recent review1 by the Cochrane Collaboration limited its scope to types of interventions that removed all or part of the nail. The first description of nail-fold soft-tissue pathology contributing to ingrown toenails was in 1959 by Vandenbos and Bowers.9 They proposed a theory whereby the excess skin surrounding the nail was burdened with daily weight-bearing resulting in the bulging of nail-fold soft-tissues and subsequent pressure necrosis.9 More recent work has confirmed that the width of the nail fold and rotation of the toe medially contributed to this tissue breakdown,8 with the resultant ulceration and inflammation forming granulation tissue that eventually embeds the advancing nail plate into the lateral nail folds.6,15 In agreement with these findings, a study by Pearson and colleagues11 found no differences in nail shape between patients with ingrown toenails and controls, suggesting that treatment should not be based on the correction of a nonexistent nail deformity.
Vandenbos and Bowers9 described an approach that left the nail intact and involved resection of a large portion of the adjacent nail-fold tissue. When healed, the nail-fold skin remained low and tight at the side of the nail with a good overall cosmetic result.9 Our study used this technique of nail-fold excision and matrix preservation with great success. Recently, Noël16 described a similar procedure with placement of simple interrupted sutures at the wound edges to reapproximate the remaining tissue. In that study, a 12-month follow-up of 23 patients identified no recurrences, excellent cosmetic results and no postoperative complications.16
The current study revisits a classical pathophysiologic model for the surgical management of ingrown toenails. Whereas the results and experiences with nail-fold excision and nail matrix–sparing presented in this study are impressive, there are a few limitations. All surgeries were conducted at a single site, and no randomization was performed. Furthermore, the analysis was retrospective, and patient self-reports may be biased owing to prior experiences and perceptions. Given that the results presented in this study are a significant improvement compared with the current literature,1,9,11,16 a randomized control trial with clearly defined outcomes comparing soft-tissue nail-fold excision with nail avulsion and phenol matricectomy would clearly be of benefit.
In summary, we present a surgical approach to the treatment of ingrown toenails that focuses on the excision of nail-fold granulation tissue with preservation of the nail and nail matrix. Our findings show excellent cosmetic results, no recurrences and high rates of patient satisfaction.
Acknowledgments
The authors thank the medical students and residents who assisted in data collection and background research. Dr. Henry Chapeskie acknowledges the many discussions with and support from Dr. Kermit Vandenbos, who died on Aug. 26, 2007. Dr. Chapeskie also thanks his father, Dr. Andrew Chapeskie, for teaching him the procedure. Dr. Chapeskie is the recipient of a University of Western Ontario Family Medicine Research Grant.
Footnotes
Competing interests: None declared.
Contributors: Dr. Chapeskie designed the study and acquired the data. Drs. Chapeskie and Kovac analyzed the data, wrote and reviewed the article and approved its publication.
References
- 1.Rounding C, Bloomfield S. Surgical treatments for ingrowing toenails. Cochrane Database Syst Rev. 2005;(2):CD001541. doi: 10.1002/14651858.CD001541.pub2. [DOI] [PubMed] [Google Scholar]
- 2.Cöloglu H, Koçer U, Sungur N, et al. A new anatomical repair method for the treatment of ingrown nail: prospective comparison of wedge resection of the matrix and partial matricectomy followed by lateral fold advancement flap. Ann Plast Surg. 2005;54:306–11. discussion 312. [PubMed] [Google Scholar]
- 3.Sykes PA, Kerr R. Treatment of ingrowing toenails by surgeons and chiropodists. BMJ. 1988;297:335. doi: 10.1136/bmj.297.6644.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kruijff S, van Det RJ, van der Meer GT, et al. Partial matrix excision or orthonyxia for ingrowing toenails. J Am Coll Surg . 2008;206:148. doi: 10.1016/j.jamcollsurg.2007.06.296. [DOI] [PubMed] [Google Scholar]
- 5.Laxton C. Clinical audit of forefoot surgery performed by registered medical practitioners and podiatrists. J Public Health Med . 1995;17:311. [PubMed] [Google Scholar]
- 6.Zuber TJ. Ingrown toenail removal. Am Fam Physician . 2002;65:2547. [PubMed] [Google Scholar]
- 7.Bos AM, van Tilburg MW, van Sorge AA, et al. Randomized clinical trial of surgical technique and local antibiotics for ingrowing toenail. Br J Surg . 2007;94:292. doi: 10.1002/bjs.5691. [DOI] [PubMed] [Google Scholar]
- 8.Langford DT, Burke C, Robertson K. Risk factors in onychocryptosis. Br J Surg . 1989;76:45. doi: 10.1002/bjs.1800760114. [DOI] [PubMed] [Google Scholar]
- 9.Vandenbos K, Bowers W. Ingrowing toenail: a result of weight bearing on soft tissue. U S Armed Forces Med J. 1959;10:1168–73. [Google Scholar]
- 10.Antrum RM. Radical excision of the nailfold for ingrowing toenail. J Bone Joint Surg Br . 1984;66:63. doi: 10.1302/0301-620X.66B1.6693479. [DOI] [PubMed] [Google Scholar]
- 11.Pearson HJ, Bury RN, Wapples J, et al. Ingrowing toenails: Is there a nail abnormality? A prospective study. J Bone Joint Surg Br . 1987;69:840. doi: 10.1302/0301-620X.69B5.3680356. [DOI] [PubMed] [Google Scholar]
- 12.van der Ham AC, Hackeng CA, Yo TI. The treatment of ingrowing toenails. A randomised comparison of wedge excision and phenol cauterisation. J Bone Joint Surg Br . 1990;72:507. doi: 10.1302/0301-620X.72B3.2341458. [DOI] [PubMed] [Google Scholar]
- 13.Palmer BV, Jones A. Ingrowing toenails: the results of treatment. Br J Surg . 1979;66:575. doi: 10.1002/bjs.1800660818. [DOI] [PubMed] [Google Scholar]
- 14.Gupta S, Sahoo B, Kumar B. Treating ingrown toenails by nail splinting with a flexible tube: an Indian experience. J Dermatol . 2001;28:485. doi: 10.1111/j.1346-8138.2001.tb00016.x. [DOI] [PubMed] [Google Scholar]
- 15.Mozena JD. The Mozena Classification System and treatment algorithm for ingrown hallux nails. J Am Podiatr Med Assoc . 2002;92:131. doi: 10.7547/87507315-92-3-131. [DOI] [PubMed] [Google Scholar]
- 16.Noël B. Surgical treatment of ingrown toenail without matricectomy. Dermatol Surg . 2008;34:79. doi: 10.1111/j.1524-4725.2007.34012.x. [DOI] [PubMed] [Google Scholar]