Abstract
Of the key Health Plan patient satisfaction measures used in Kaiser Permanente Colorado, ease of contacting the physician's office with a medical question was consistently rated as the lowest quarterly patient satisfaction measure. Furthermore, medical office staff had become dissatisfied with their inability to contact patients who had previously left messages. In addition to the shear volume of messages, the return calls were often unanswered, leading to subsequent attempts to reach patients, creating additional work for medical office staff.
DirectConnect—the project name for a system and set of processes focused on improving patient satisfaction with the ability to contact Primary Care delivery teams by telephone—focuses on isolating medical advice calls from the other types of calls handled by the centralized Call Center. The system identifies the patient using his/her unique electronic medical record number, then automatically routes medical advice calls directly to the appropriate Primary Care Physician (PCP) or staff. The clinician may then evaluate and respond to the patient's need quickly, thus managing more of their panel's requests in real time.
How is DirectConnect different from simply having the patient contact their PCP's office directly? The primary difference is “one-number” convenience that allows all patients to dial one number to access their PCP's team. In addition, calls are routed to various staff as available to reduce long telephone queues and wait times.
The DirectConnect system has resulted in statistically significant improvement in key service quality measures. Patient satisfaction improved from a pre-implementation nine quarter mean of 55.9% to a post-implementation 12 quarter mean of 70.2%. Fourteen percent to 17% of all Primary Care calls are now handled by the patient's home medical office team, creating a 54% improvement in the centralized Call Center's speed of answering calls in the first quarter post implementation—making no additions to medical office staffing levels. The efficiencies gained by directly connecting medical advice-seeking patients with their Primary Care team resulted in an estimated savings of 198 and 247 cumulative hours per week in unnecessary telephone work for Call Center and medical office staff regionwide.
Introduction
Problem Definition
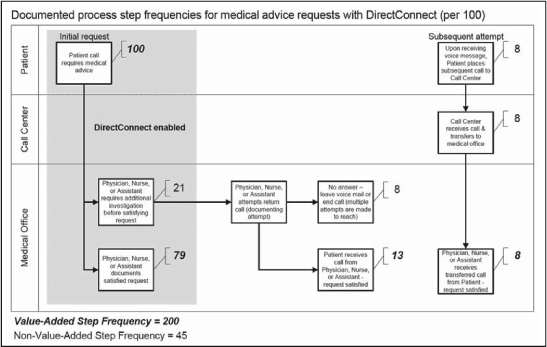
For the nine quarters prior to DirectConnect's implementation, on average only 55% of Kaiser Permanente Colorado (KPCO) patients rated the ability to contact their physician as “extremely easy” or “easy” with a range between 44% and 59% (Figure 1). This served as evidence of KPCO's “big system” feel when compared to its care delivery competitors. Patients routinely expressed their frustration with the process of leaving a message with someone they didn't know (Call Center agent) and awaiting a call back at some unpredictable time in the future. The following patient comments on the system of leaving telephone messages were documented in KPCO's QIII 2005 and QIV 2005 patient satisfaction study:
“It makes it more difficult to wait for them to call back. It might be sometime later in the day, so it's not convenient because you don't know when they could call you back.”
“It is just hard to give them a call back number if you don't know where you are going to be and they can't tell you exactly when [they will] call.”
“I would tell [KPCO] that they need to have a different way to actually contact a physician or triage nurse when needed, a lot easier than it is now.”
Figure 1.
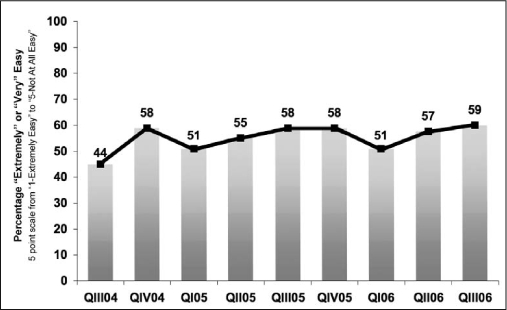
Quarterly patient satisfaction with ability to contact physician before DirectConnect.
Before DirectConnect, patients with a medical question would call the regional Primary Care Call Center with the hope of speaking with someone from their home medical office. Instead, centralized Call Center agents, located away from all primary care medical office buildings were forced to use an electronic message to route questions to the appropriate medical office building. Patients then awaited a return call from their trusted Primary Care team. Although patients ultimately received the appropriate level of care, the process rarely met preferred service expectations.
Beyond the well-documented issues of poor patient satisfaction, the internal system of managing telephone messages was fraught with waste and rework—although the full extent of this waste and rework had not been formally quantified.
From the centralized Call Center perspective, inbound call volumes were projected to increase at a rate of 3% to 10% per year and the ability to increase staffing was not available. These challenges resulted in 64% of calls answered within 60 seconds for the year prior to implementation of DirectConnect with an average speed to answer calls of 101 seconds during that period. These statistics are evidence of less than desired telephone service for any need related to Primary Care, be it for appointments or medical questions.
Current State Measurement and Analysis
Process improvement expert W Edwards Deming, one of the fathers of Lean Manufacturing concepts noted: “Workers are responsible for only 15% of the problems, the system for the other 85%. The system is the responsibility of management.”1p94 In keeping with this philosophy, a small team of management, frontline employee representatives, internal consultants, and analysts were identified to focus on improving the system of telephone message management and to develop the methods by which ongoing measurement of that workflow could be realized (Table 1).
Table 1.
Primary team members and sponsors
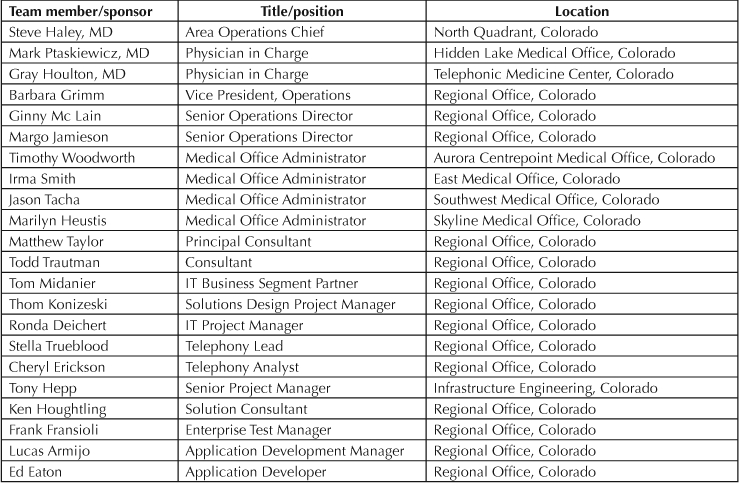
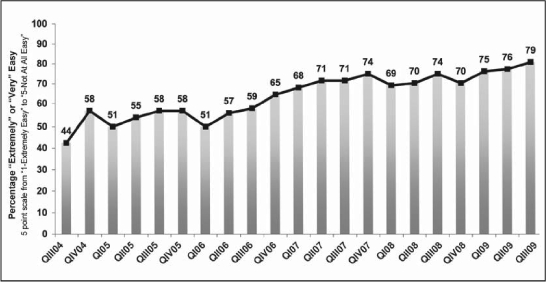
Figure 2 depicts the high-level process flow yielded by the analysis of the telephone messaging system. Four to seven process steps were needed to highlight the vast majority of scenarios related to the telephone message system. Weekly volumes were tabulated to capture the average number of electronic messages routed to each medical office building from the Call Center, the average number of documented attempts made by the medical office staff to call the patient back, and any subsequent return calls into the Call Center for transfer to the medical office building because the patient was not available to receive the first call back. For every 100 electronic messages routed from Call Center to medical office, an average of 130 call attempts were made from medical office staff back to the patient and another 21 calls were made from the patient back to the Call Center—ultimately receiving a call transfer to the Primary Care team in the medical office.
Figure 2.
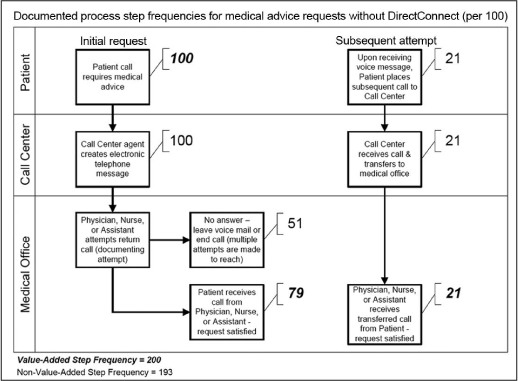
Average frequencies at key points of telephone advice message process prior to DirectConnect.
Scope
The scope of the improvement effort focused on medical advice telephone messages that were routed electronically from the centralized Call Center to each of 17 Primary Care medical offices. These messages required a nonclinically trained Call Center agent to answer the call and document the chief complaint and symptoms. The Call Center agent then routed the message to the appropriate medical office where clinical staff and physicians would sort through the messages and return those calls at some future point. These calls represented 20% of the Call Center's two million annual calls received. The remaining calls handled by the Call Center included appointment requests for Primary Care and other medical specialties, pharmacy requests and general information requests. These calls were considered outside the scope of the improvement effort.
Methods
Using Lean Manufacturing and Six Sigma concepts coupled with Call Center industry technology, a new program was developed to transform the way telephone-based medical questions from a Primary Care Physician's (PCP's) panel would be handled. The Six Sigma DMAIC (Define, Measure, Analyze, Improve, and Control) method was heavily leveraged in the development of the solution. During the analysis phase, Lean Manufacturing methods, in particular value stream mapping, flow,2 and root cause analysis were used. Lean's concepts of reducing work in process to decrease completion time3 and removing wastes, most notably those related to overproduction and defects, governed many of the decision points of the effort.
Measuring and Analyzing the Current State
To measure the overproduction and delays associated with the medical advice telephone messaging process, 1) time and motion studies were performed, 2) data was retrieved from Call Center reports, 3) reports were developed to specifically measure the responsiveness of medical offices staff to telephone messages as captured by the electronic medical record, and 4) a third party administered a satisfaction survey sent quarterly to patients.
Time and motion studies found that, on average, Call Center agents spent 124 seconds per medical advice telephone message and medical office staff spent, on average, 44 seconds calling back the caller, waiting for the phone to ring, and leaving a message when unable to reach the originator of the request. All of this time was non-value-added4 in the system. From a patient satisfaction perspective, value is primarily added to these types of calls only when speaking to their PCP or a clinical team member of that PCP in their home medical office.
Standard Call Center reports were used to assess the impact process and system change would have in the Call Center. Key metrics included the average speed of answer for all inbound calls and the percentage of calls answered within 60 seconds. The number of Call Center agent full-time employee resources needed to provide improved service was also tracked.
The electronic medical record (EMR) documentation yielded more evidence of waste in the system. For every 100 telephone messages routed to the medical office by the Call Center on average, EMR documentation revealed that 130 return call attempts were made by that medical office. This highlights the frequency of occurrence that the medical office staff or clinician received no answer or was forced to leave a voice message to have the patient call back. Furthermore, the analysis showed that on average 21% of patients were required to place a second call back to the Call Center before being manually transferred to the medical office after having previously left a message. This loop of wasteful overproduction in the system was referred to as the ratio of telephone tag in the system.
Patient satisfaction with the ability to contact physicians or care delivery teams with a medical question was tabulated on a quarterly basis by a third party survey administrator. Before DirectConnect, this measure maintained a nine quarter mean of 54.6% satisfaction with ease of contacting clinician with a range from 44.0% to 59.0%, an upper control limit of 68.9%, and a lower control limit of 40.3%.
Intervention
DirectConnect seeks to provide a way to more efficiently and effectively handle increases in Primary Care-related call volume that comes with growing patient demand and with increasing use of the telephone as a key channel of communication between patient and physician. By streamlining this channel of communication, DirectConnect aims to increase the level of trust between patients and physicians by increasing the frequency that medical advice is delivered to the patient by a caregiver known and trusted by the patient—typically by their personal PCP or their physician's team. Increasing the frequency of real-time response to a patient's medical question by a known, trusted caregiver became the hallmark of the DirectConnect process of telephone request management for PCPs and their care delivery teams.
Pilot
With the data made available as a result of the analysis phase, a manual system was designed to pilot the removal of the telephone tag associated with the medical advice telephone messaging. Three medical offices—one housing general Internal Medicine physicians, one with Pediatricians, and the third with a mixed Primary Care model of general Internal Medicine, Family Medicine, and Pediatrics—were selected. These medical offices began a pilot in which, when a call was received, the Call Center agent would remain on the line and would transfer the call directly to the patient's home medical office, instead of creating an electronic message. Although this pilot required that the Call Center absorb the cost of spending more time on the line with patients while waiting for the medical office staff to answer—the return call volume declined dramatically. This decline was as a result of handling a greater percentage of would-be electronic messages in real time—a Lean Manufacturing concept known as single-piece flow, versus the prior method of electronic messaging, which was more akin to the Lean Manufacturing concept of batch-and-queue.
Technological Intervention
Once the initial pilot was successfully completed, a technological intervention pilot was funded and implemented that allowed the system to automatically identify the PCP, capture the nature of the call—whether a medical question or appointment request—match these attributes, and direct the call to the appropriate staff member. Additional attributes were included in the design that allowed the system to evaluate and to predict the next available staff member and that ensured calls would not be queued for longer than an agreed-upon threshold. Further system revisions were made throughout the implementation to present any waiting callers with the option to remain holding or be immediately transferred to a Call Center agent to leave an electronic message. This put the decision to remain on hold in the hands of the patient. If the caller selected the option to leave a message instead of remaining on hold, the call would be seamlessly routed to the next available Call Center agent where an electronic message would be sent to the medical office in traditional fashion (Figure 3).
Figure 3.
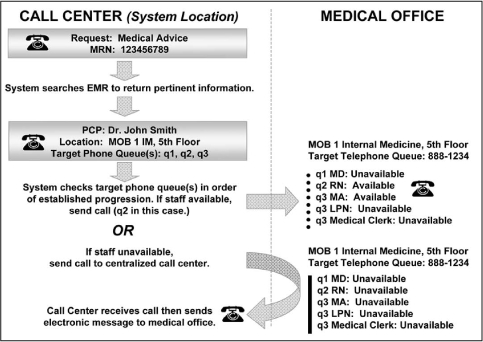
DirectConnect system flow diagram.
Models and Options
During the first two months of deployment, several call routing models and medical office workflow options were tested. Best practices were shared and adopted. The result has been sustained improvement in all 12 quarters following implementation. Weekly reports indicating medical office performance are posted and accountabilities are in place to ensure results are sustained. Since full deployment in July 2007, DirectConnect calls consistently represent between 15% to 20% of overall Primary Care telephone volume, with one outlier of 22% in November 2008 (Figure 4). This suggests that patients who learn the system are not inclined to abuse the service beyond what is required on the basis of their request. Although medical office staff answers 98% to 100% of all DirectConnect calls to the medical office, some physicians have chosen to log into the system as part of their daily routine when returning calls to patients. This capability allows physicians who wish to deliver a significantly higher level of service to their patients the opportunity to do so.
Figure 4.

DirectConnect system calls as percentage of total Primary Care calls.
Results
With the system and associated processes implemented, dramatic gains have been achieved without adding any resources in the medical offices and while reducing the resource requirements of the Call Center. Today, 14% to 17% of total annual inbound call volume is answered by the home medical office. For each of these calls, the Call Center need not answer them, create telephone messages for them, or route them to the medical office where the patient must await a return call later in the day. Furthermore, the Call Center's speed of answering calls improved by 54% in the first quarter after implementation compared to the same quarter from the year before.
Now, for every 100 documented inbound telephone advice encounters that fall within the scope of DirectConnect on average, 79 requests are handled on the first call by the patient's home medical office physician or team. Although the remaining 21 requests require additional research or a higher skill set to be satisfied, the return calls required to reach the patient are lower when the telephone encounter originates in the home medical office—presumably because the medical office team can provide a more targeted call back time than the centralized Call Center. This increases the odds of reaching the patient when the return call is made. Thus, the system has experienced a documented 26.9% reduction in required return calls because of DirectConnect. This reduces the number of non-value-added steps associated with the medical advice request process from 193 (Figure 2) to 45 (Figure 5). The removal of these non-value-added process steps yields a weekly time savings of between 198 and 247 hours per week in unnecessary telephone work for Call Center and medical office staff.
Figure 5.
Average frequencies at key points of telephone advice message process with DirectConnect.
Patient satisfaction with the ability to contact their PCP or Primary Care delivery team with a medical question, the key driver of improvement, has improved a statistically significant 14% and maintained a nine quarter mean of 70.2% satisfied with a range from 65% to 79% and an upper control limit of 77.9% and a lower control limit of 62.6% since implementation.
Discussion
Key Successes
DirectConnect enabled significant improvements for the patients of KPCO while eliminating system barriers that hampered PCPs and staff from providing the high level of service they desired (Table 2). By systematically driving 14% to 17% of KPCO's inbound telephone volume directly to the home medical office of the patient, Call Center service levels have improved beyond the internal target of 80% answered within 60 seconds (Figure 6) while maintaining an average speed of answering inbound calls below the 60 second mark in each month following the DirectConnect deployment. These Call Center improvements occurred without adding Call Center staff. In fact, the DirectConnect system's financial breakeven point occurred ten months after full deployment as a result of savings generated by Call Center agent attrition—while maintaining these improved levels of service.
Table 2.
Key Results

Figure 6.

Call Center percentage of calls answered within 60 seconds by month.
Removing call volume from the centralized Call Center and routing those calls directly to the home medical office of the patient will, on the surface, appear to necessitate a need to shift resources to those medical office buildings to handle the volume; however, because of the single-piece flow nature of the new system, this process is far more efficient for the medical office staff than the previous batch-and-queue process associated with electronic messages. Medical office staff and PCPs make 26.9% fewer return calls; this equates to a time savings 198 to 247 hours per week across the system.
Most importantly, these measurable improvements in both Call Center and medical office areas have led to statistically significant improvements in patient satisfaction—the ultimate objective of the DirectConnect implementation. From the pre-DirectConnect mean of 55.9% satisfaction with the patient's ability to contact their physician, this measure increased to a mean of 70.2%—14.3% higher than the mean of the previous process, and 3.3% higher than the eight quarter upper control limit of the previous process (Figure 7).
Figure 7.
Quarterly patient satisfaction with ability to contact physician before and after implementation of DirectConnect beginning in QIV 2006.
DirectConnect has brought KPCO patients closer to their physicians and the Primary Care delivery teams that know them. The barriers that once existed as a result of the desire to gain economies of scale through a large, centralized Call Center have been mitigated. This system has pleased physicians, medical office staff, and those seeking care (Table 3). As health care seeks to better meet the needs of the population, systems like DirectConnect lend credence to the concept that large health plans and provider groups can foster better communication with members and patients without sacrificing affordability of care.
Table 3.
Physician and staff comments

Future
The future implications of this marriage between Call Center technology and the electronic medical record are exciting. Once a technical interface is created between the caller's EMR and the Personal Physician—as in the DirectConnect system—new opportunities to creatively connect patient and physician exist. For example, on the basis of diagnosis, stratification of patients may occur to automatically route them to the nurse who is most equipped to handle questions related to their condition. Additionally, physicians may be able to establish one-time clinical rules that permit the patient to be directly routed to the physician's mobile phone upon their next call if important information exchange is needed. Within the context of the telephone system, a mobile phone could be considered part of the greater call routing system, thereby falling under the umbrella of load balancing and call handling redundancy to ensure that calls are not left unanswered. This system creates a foundation on which the relationship between the patient and their personal physician can be further enhanced.
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- Walton M. The Deming management method. New York: Penguin Putnam; 1986. [Google Scholar]
- Womack JP, Jones DT. Lean thinking: banish waste and create wealth in your corporation. New York: Simon & Schuster; 2003. [Google Scholar]
- Gerst R. The little known law. Six Sigma Forum Magazine. 2004 Feb;3(2):18–23. [Google Scholar]
- George ML. Lean six sigma for service: How to use lean speed and six sigma quality to improve services and transactions. New York: McGraw-Hill; 2003. [Google Scholar]


