Introduction
Pressure ulcer treatment is one of many aspects of patient care in which nursing care interfaces directly with clinician-provided medical services. Traditionally, the treatment of pressure ulcers has been left to nurses. No less an authority than Florence Nightingale said in 1859, “If he has a bedsore, it's generally not the fault of the disease, but of the nursing.”1 Physicians have tended to be passive participants, routinely cosigning orders written by hospital-based wound-care nurses or home health nurses. Realization of the costs associated with the treatment of pressure ulcers and recent requirements by third-party payers have prompted physicians to become more actively engaged in the prevention, identification, and treatment of pressure ulcers.
Pressure ulcers are localized areas of tissue damage or necrosis that develop because of pressure over a bony prominence. They have previously been called pressure sores, bedsores, and decubitus ulcers, terms that imply that only bed-bound, nonambulatory patients develop pressure ulcers. It is important to recognize that patients who are ambulatory can also develop pressure ulcers, although reduced mobility is still a major risk factor.
The purpose of this article is to familiarize physicians and other clinicians who provide care to hospitalized patients, such as physician assistants, certified nurse midwives, and nurse practitioners, with some of the terminology associated with pressure ulcers, so that they can better assess patients at risk for the development of pressure ulcers and properly identify and describe pressure ulcers.
Costs
For a sense of the total costs of the treatment of pressure ulcers, data from the 1990s, although old, can shed a light on current costs. In 1996, $6.4 billion was spent on pressure ulcers, which was 1.2% of total health care costs in the US.2 In 2006, excluding neonatal and maternal conditions, almost $11 billion was paid out for hospital stays in which pressure ulcer was either a primary or secondary diagnosis.3 For the individual patient, the current costs of providing care for one pressure ulcer can range from $3500 to over $60,000, depending on the stage of the ulcer.4
Pressure ulcers have also attracted the attention of the medicolegal community. Some courts regard pressure ulcers as evidence of elder abuse, and some lawsuits have awarded judgments of more than $10 million.5 If the presence of pressure ulcers is considered to indicate elder abuse, such legal judgments are not covered by conventional medical malpractice insurance policies, nor are such awards limited by the caps imposed by many US states in medical malpractice lawsuits.
In November 2008, the Center for Medicare and Medicaid Services instituted a policy to withhold reimbursement due to be made to acute-care hospitals for the costs of treating hospital-acquired conditions,6 such as pressure ulcers. Although hospitals will be paid for the care of pressure ulcers that originated before admission, hospital-acquired pressure ulcers would be the responsibility of the admitting hospital. Because of this change in policy, there is now an incentive for hospitals to accurately assess for skin problems in all patients being admitted and to identify all patients at risk for developing pressure ulcers so that preventive measures can be put in place. Increasingly physicians are being called on to identify at-risk patients and accurately classify skin conditions present at admission.
Identification and Risk Assessment
On admission to an acute-care hospital, all patients should undergo a thorough skin assessment to determine if they are being admitted with skin conditions, including pressure ulcers, that were already present. Any such condition must be clearly documented on the record of the admission physical examination. This documentation is ultimately the responsibility of the admitting physician.
In addition to performing a complete skin assessment, it is also important to identify the patient who may be at risk for developing a pressure ulcer after admission to the hospital. Such identification should then initiate interventions intended to maintain skin integrity and prevent skin breakdown. The most common assessment tool used for this purpose is the Braden scale,7,8 which evaluates the severity of several different factors that would place the patient at risk for the development of a pressure ulcer:
Sensory: how well a patient can process sensory input from the skin as well as how effectively s/he can communicate level of sensation
Moisture: to what degree the skin is exposed to moisture
Activity: how active a patient is, irrespective of his or her degree of mobility
Mobility: how well the patient can change and control his or her body position
Nutrition: what constitutes the usual pattern and amount of caloric intake
Friction and shear: how the patient moves within his or her confines.
Each of these factors is ranked on a numeric scale from 1 to 4, with the exception of friction and shear, which only has three points on its scale. Scores are then totaled. Ultimate risk is determined by the total Braden score, with the highest possible score being 23. Patients with scores of 18 or less are considered to be at varying degrees of risk. Individual hospitals will establish their own criteria for the specific levels of risk associated with the range of Braden score.
The performance of an assessment using the Braden scale is within the scope of practice of all registered nurses who have been educated to use the tool. Braden-scale assessments should be done on a regular basis, with the frequency determined by individual hospital policy, for all confined patients, as well as for patients who experience any change of condition, who have been transferred between different hospital units, or who have just returned from surgery. A physician should be able to ask for and to receive an up-to-date Braden score for any patient admitted to the hospital. The frequency of Braden-scale assessments should be at least every three days. Interventions can then be based on the specific deficiency identified by the assessment.
Patients who have problems with mobility will have to be physically turned by hospital staff on a regular basis. Repositioning frequency will be determined by the individual's tissue tolerance, level of activity and mobility, general medical condition, the overall treatment objectives for the patient, and assessments of the individual's skin condition.9 Patients with excess skin moisture will have to be treated with drying agents and compounds intended to protect exposed areas from maceration. Friction and shear can result in the disruption of capillaries and other small vessels, producing ischemia in subcutaneous tissues. When patients must move in bed, they must be lifted and repositioned, not slid across the mattress.
Nutritional deficits are common in many hospital-based patient populations and deserve special consideration. Protein supplementation is important, but there should be ongoing assessment with review of albumin and prealbumin levels. It can be useful to identify a patient at risk for nutritional deficiency by checking the initial serum albumin level. However, to assess for effectiveness of nutritional intervention, a prealbumin level, with a half-life of two days, is far more useful and will change during a period of days to one week with effective nutritional support.10
Nutritional deficits are common in many hospital-based patient populations and deserve special consideration. Protein supplementation is important …
Using the Braden scale allows for a systematic approach to risk assessment and provides a road map that clinicians can use to efficiently manage the interventions intended to prevent the development of pressure ulcers.
Staging
When ulcers are identified in a hospitalized patient, it is essential to carefully document the circumstances that led to the formation of the ulcer, where the ulcer is, how large it is, and what stage it is. Different interventions and types of reimbursed procedures are required, depending on the stage of the ulcer. Only pressure ulcers can be staged. Ulcers that may have other causes, such as venous insufficiency, arterial occlusive disease, and diabetes mellitus, are not appropriate for the type of staging that is described here.
The stage of a pressure ulcer depends on the depth of the ulcer. Figure 1 shows the various stages of pressure ulcers by layer of skin or subcutaneous tissue involvement.11 The total surface area that the ulcer encompasses is not the determining factor. For example, a stage I or II pressure ulcer may have a fairly large surface area, but a stage III or IV may be of relatively smaller diameter but of greater depth. The development of pressure ulcers is a progressive process. If a patient has a lower-stage pressure ulcer and if preventive measures are not implemented to address the factors contributing to its development, then it will progress into a more complicated and severe ulcer.
Figure 1.
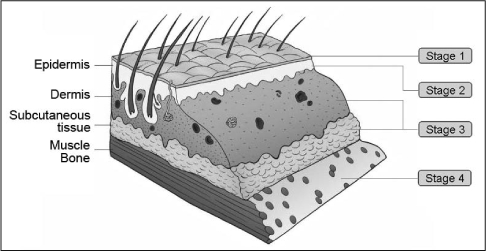
Pressure ulcer staging.
Adapted and reprinted with permission from Auerbach PS. Wilderness medicine. 5th ed. Figure 13-3. Oxford (UK): Mosby. Copyright Elsevier, 2007.
In stage I ulcers, there is a change in the color, consistency, or temperature of the skin, but the skin is intact and the underlying tissues are unaffected. Figure 2 demonstrates a typical appearance; however, in some cases the skin may appear normal, and it is only by tactile examination that any changes in skin integrity can be identified. A stage I pressure ulcer is a warning sign that there is a problem. Interventions at this point can help prevent further, more problematic skin conditions.
Figure 2.
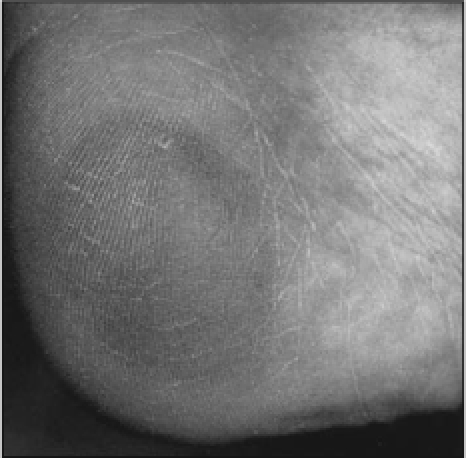
Stage I pressure ulcer.
Reprinted with permission from Kaiser Permanente MultiMedia Communications, Los Angeles, CA.
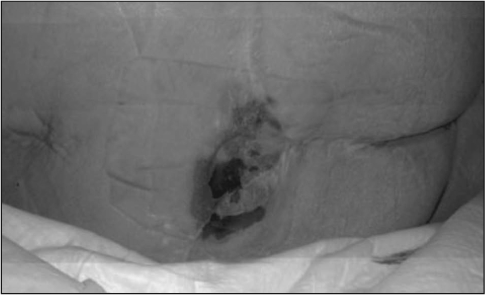
Stage II pressure ulcers involve the epidermal layer of skin and may extend into the dermis as well. These usually appear as shallow, open areas or intact serum-filled or serosanguineous blisters. Although the skin is physically intact in a stage I pressure ulcer, a stage II pressure ulcer involves a break in the skin's integrity. Figure 3 depicts a typical example of a stage II pressure ulcer, with excoriation of the involved skin and extension into deeper tissues. When a patient develops a stage II pressure ulcer, it is common to have to contend with issues such as serous drainage that complicate skin care and can cause problems with adjacent areas of the skin that would not otherwise be affected.
Figure 3.
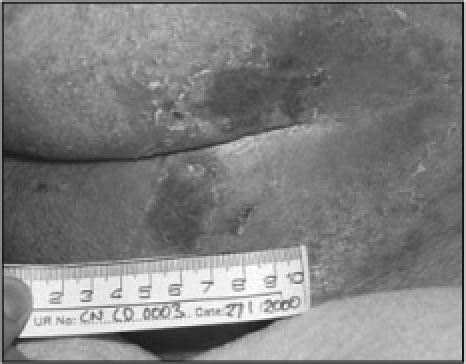
Stage II pressure ulcer.
Reprinted with permission from Kaiser Permanente MultiMedia Communications, Los Angeles, CA.
Stage III pressure ulcers, such as the one seen in Figure 4, extend into the subcutaneous tissue, and although underlying bone, muscle, and fascia may be visible, the ulcer has no direct involvement of these structures. The presence of any necrotic slough in an ulcer that otherwise appears to be a stage II pressure ulcer automatically qualifies that ulcer to be a stage III ulcer. Stage III pressure ulcers may also involve tunneling and undermining, wherein the ulcer extends beneath normal tissue.
Figure 4.
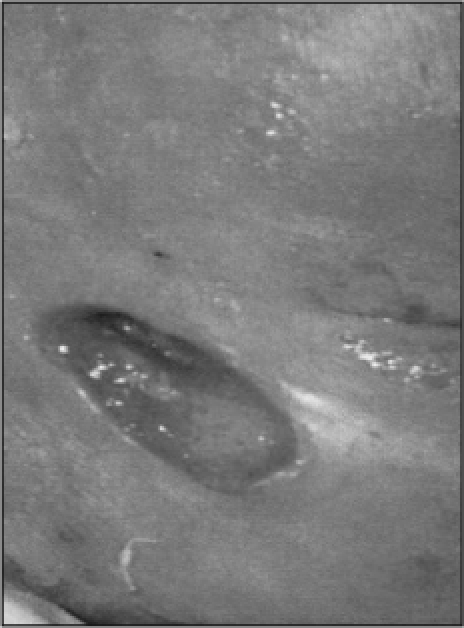
Stage III pressure ulcer.
Reprinted with permission from Kaiser Permanente MultiMedia Communications, Los Angeles, CA.
Stage IV pressure ulcers extend into bone or muscle, as is seen in Figure 5. Patients outside of acute-care hospitals with stage III and stage IV pressure ulcers qualify for Medicare Durable Medical Equipment coverage for more specialized mattresses and hospital beds.
Figure 5.
Stage IV pressure ulcer.
Reprinted with permission from Kaiser Permanente MultiMedia Communications, Los Angeles, CA.
Because staging is based on the depth of involvement, it is essential to be able to visualize the bottom of the ulcer. If the bottom of the ulcer is covered by thick eschar or adherent slough, then it cannot be staged and is referred to as unstageable. Only when the eschar is débrided and the base of the ulcer is fully visualized can the ulcer be accurately staged. An example of this is shown in Figure 6.
Figure 6.
Unstageable pressure ulcer.
Reprinted with permission from Kaiser Permanente MultiMedia Communications, Los Angeles, CA.
Another type of pressure ulcer that is difficult to stage is designated a deep tissue injury. The surface of the skin may appear to be like that of a stage I or II ulcer, as is shown in Figure 7,12 but the damage to underlying tissues is severe. Because the pressure forces are greatest at the interface between bone and surrounding soft tissue, tissues not visible may be severely compromised, even necrotic. Figure 8 shows how severe and how deep the damage can be to deep tissues.13 Areas of the skin with deep tissue injury can rapidly progress into deep stage III or IV ulcers, appearing to seemingly materialize overnight. The clinician's index of suspicion regarding these ulcers must be high. A patient with what appears to be a large stage I or II pressure ulcer who also has a low Braden score may very well have deep tissue injury. In Europe, deep tissue injury and unstageable pressure ulcers are classified as stage IV.9 Whatever classification is used, these patients should be treated as if they have a stage III or IV pressure ulcer.
Figure 7.
Deep tissue injury.
Reprinted from Black JM, Black SB. Unusual wounds: deep tissue injury. Wounds 2003 Nov 10;15(11):38, with permission from HMP Communications, Malvern, PA; 2003.
Figure 8.
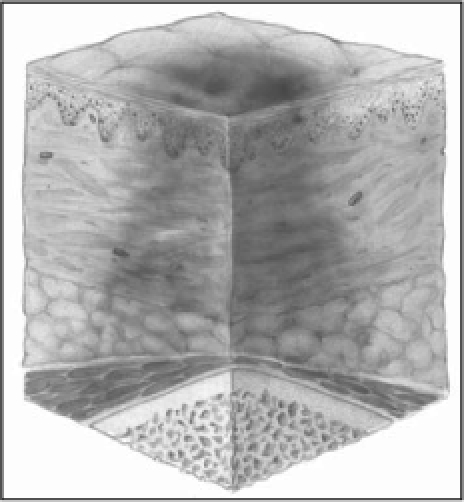
Deep tissue injury.
Reprinted with permission from Pressure ulcer staging illustrations [monograph on the Internet]. Washington, DC: National Pressure Ulcer Advisory Panel; 2007 [cited 2010 Apr 24]. Available from: www.npuap.org/resources.htm.
Treatment
Although it is only too easy to fall into the paradigm of watching pressure ulcers progress from stage I to stages III or IV, treatment must be rendered with the expectation of the ulcer healing from a stage III or IV to stage I and hopefully even back to more normal skin and tissue integrity.
The major principles of pressure ulcer treatment are as follows:
Eliminating external pressure on affected area(s) of the body
Preserving the integrity of surrounding normal skin and tissues
Facilitating the body's own mechanisms of natural healing
Removing necrotic and devitalized tissue
Providing adequate pain relief
Reducing bacterial load
Treating conditions that place the patient at risk for developing pressure ulcers, such as malnutrition and anemia.
It is beyond the scope of this article to review in detail the spectrum of treatment modalities available to treat pressure ulcers. The European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel have recently published a joint report on guidelines for treatment of pressure ulcers.9 Recommendations related to each of these principles are provided in that report, which can be accessed at www.npuap.org.
… more involvement by physicians … will increase scientific study of the pathophysiology of pressure ulcers and effective treatment options.
A 2008 review of treatment options that comprehensively surveyed the medical literature for all studies related to the treatment of pressure ulcers concluded, “Clinicians should make decisions regarding pressure ulcer therapy based on fundamental wound care principles, cost, ease of use, and patient preference.”14 A more practical recommendation for clinicians is to consult the certified wound-care specialists at the particular medical center in which they practice regarding what is available and what would be best to offer their patients with pressure ulcers.
Conclusion
Whether they were called bed sores or decubitus or some other even more archaic terms, pressure ulcers have been part of the spectrum of medical and nursing care since even before Florence Nightingale attended to the wounded soldiers of the Crimean War. For most of that time, our nursing colleagues might have thought that they had to contend by themselves with treating these conditions. It can be hoped that more involvement by physicians with the treatment of pressure ulcers will increase scientific study of the pathophysiology of pressure ulcers and effective treatment options. With such knowledge, it is possible that recommendations based on evidence can be made so that efficacy will improve and cost will decrease. Partnerships between physicians and nurses can help solve clinical problems by bringing fresh perspectives to the analysis process. The ultimate beneficiaries will be our patients, who depend on the collaboration of physicians and nurses to successfully address their personal health care needs.
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
Acknowledgments
Katharine O'Moore-Klopf, ELS, of KOK Edit provided editorial assistance.
Exist
And although our bodies are bounded with skin, and we can differentiate between outside and inside, they cannot exist except in a certain kind of natural environment.
— Alan Watts, 1915–1973, British philosopher and writer
References
- Nightingale Florence. Notes on nursing: what it is, and what it is not. New York: D Appleton and Company; 1860. [Google Scholar]
- Pompeo MQ. The role of “wound burden” in determining the costs associated with wound care. Ostomy Wound Manage. 2001 Mar;47(3):65–71. [PubMed] [Google Scholar]
- Russo CA, Steiner C, Spector W. Statistical Brief #64: Hospitalizations related to pressure ulcers among adults 18 years and older, 2006 [monograph on the Internet] Rockville, MD: US Agency for Healthcare Research and Quality: Healthcare Cost and Utilization Project (HCUP); 2008 Dec. [cited 2010 Apr 5]. Available from: www.hcup-us.ahrq.gov/reports/statbriefs/sb64.jsp. [PubMed] [Google Scholar]
- Pressure ulcers [monograph on the Internet] Publication 1999/23. The Hague: Health Council of the Netherlands; 1999 Dec 31. [cited 2010 Apr 5]. Available from: www.gezondheidsraad.nl/en/publications/pressure-ulcers. [Google Scholar]
- Voss AC, Bender SA, Ferguson ML, Sauer AC, Bennett RG, Hahn PW. Long-term care liability for pressure ulcers. J Am Geriatr Soc. 2005 Sep;53(9):1587–92. doi: 10.1111/j.1532-5415.2005.53462.x. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services (CMS), HHS. Medicare program; changes to the hospital in-patient prospective payment systems and fiscal year 2008 rates. Fed Regist. 2007 Aug 22;72(162):47129–8175. [PubMed] [Google Scholar]
- Braden B, Bergstrom N. A conceptual schema for the study of the etiology of pressure sores. Rehabil Nurs. 1987 Jan–Feb;12(1):8–12. doi: 10.1002/j.2048-7940.1987.tb00541.x. [DOI] [PubMed] [Google Scholar]
- Bergstrom N, Braden BJ, Laguzza A, Holman V. The Braden Scale for Predicting Pressure Sore Risk. Nurs Res. 1987 Jul–Aug;36(4):205–10. [PubMed] [Google Scholar]
- European Pressure Ulcer Advisory Panel & National Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers: quick reference guide [monograph on the Internet] Washington DC: National Pressure Ulcer Advisory Panel; 2009. [cited 2010 Apr 5]. Available from: www.epuap.org/guidelines/Final_Quick_Prevention.pdf. [Google Scholar]
- Shenkin A. Serum prealbumin: is it a marker of nutritional status or of risk of malnutrition? Clin Chem. 2006 Dec;52(12):2177–9. doi: 10.1373/clinchem.2006.077412. [DOI] [PubMed] [Google Scholar]
- Auerbach PS. Wilderness medicine. 5th ed. St Louis, MO: Mosby; 2007. [Google Scholar]
- Black JM, Black SB. Unusual wounds: deep tissue injury. Wounds. 2003 Nov 10;15(11):38. [Google Scholar]
- Pressure ulcer staging illustrations [monograph on the Internet] Washington, DC: National Pressure Ulcer Advisory Panel; 2007. [cited 2010 Apr 24]. Available from: www.npuap.org/resources.htm. [Google Scholar]
- Reddy M, Gill SS, Kalkar SR, Wu W, Anderson PJ, Rochon PA. Treatment of pressure ulcers: a systematic review. JAMA. 2008 Dec 10;300(22):2647–62. doi: 10.1001/jama.2008.778. [DOI] [PubMed] [Google Scholar]


