Abstract
Objective To investigate the relationship between domestic violence and perinatal, neonatal and infant mortality in rural India using prospective data.
Methods The study is based upon a prospective follow-up study of a cohort selected from the 1998–99 National Family and Health Survey-2 (NSFS-2), which was carried out in 2002–03 in four Indian states. Data for a total of 3909 birth outcomes that took place during this 4-year period were analysed using bivariate analysis and hazards regression analysis to control for truncated observations and possible other confounding factors.
Findings After controlling for other potentially confounding factors, births to mothers who experienced two or more episodes of recent domestic violence experienced higher perinatal [hazards ratio (HR) = 1.85, 95% confidence interval (CI) = 1.12, 2.79] and neonatal (HR = 1.62, 95% CI = 1.11, 2.53) mortality, relative to births to women whose mothers reported no violence. Overall, these births to women who experienced violence had 68% higher risk of infant mortality compared with the ‘no violence’ group. Births to women who experienced a single episode of violence were not at higher risk of mortality.
Conclusions Our study provides additional and more conclusive evidence on the importance of domestic violence for early childhood mortality in low-resource settings such as rural India. The results argue for a greater focus upon such violence within current child survival programmes.
Keywords: Domestic violence, perinatal mortality, neonatal mortality, infant mortality, hazards regression analysis, rural India
Introduction
Over the past decade, domestic violence has been increasingly recognized as a major public health concern. It has been estimated that between 10 and 64% of adult women have experienced lifetime physical or sexual violence at the hands of their male partners, with estimates generally substantially higher in developing countries.1–3 Some of the highest reported rates of violence have been reported in studies from the South Asian region.4–6
A substantial body of evidence exists highlighting the negative consequences of domestic violence for women’s health and well-being.7 A number of studies have also reported an association between domestic violence and women’s mental health and depression.8,9 A growing body of evidence has also highlighted the potential linkages between such violence and reproductive health outcomes, including non-use of contraception,10,11 unintended pregnancy,10,12,13 gynaecological problems and sexually transmitted infections,14,15 and HIV/AIDS.16,17
Given evidence that pregnancy is often not a protective period for women against the risk of violence, considerable attention has also been devoted to the potential adverse role of such violence for the health and survival of infants. A number of US and European population-based studies have reported significant adverse effects of domestic violence upon gestational and birth outcomes.18–21 This effect appears to operate in part through the association between domestic violence and prematurity or low birthweight.22,23
Evidence on the relationship between domestic violence and perinatal, neonatal and/or infant mortality is much more limited, and almost all of it is based on studies from developed countries.24,25 Evidence from developing countries on these relationships remains limited in number and based largely upon retrospective study designs. An earlier study from North India reported significant associations between lifetime domestic violence and infant mortality risks.26 In the most conclusive study of the subject to date, men reporting perpetuating violence against their wives around the time of pregnancy was associated with significantly risks of perinatal, neonatal and infant (but not early childhood) mortality risks for the most recent pregnancy.27 A recent study using nationally representative data from women of reproductive age in India found that the experience of physical violence from a male partner was associated with an increased risk of infant and child mortality.28 A case–control study from Nicaragua also reported significant associations between abuse-during-pregnancy and <5-year mortality.29 A recent study from Kenya using Demographic and Health Survey data also found consistent associations between the risks of infant mortality and various forms of lifetime domestic violence.30 In the only contrasting findings on this association, a recent study from Bangladesh failed to find a significant association between lifetime experience of domestic violence and the risk of stillbirth.31 The present analysis builds upon the existing literature by using prospectively collected data to examine the relationship between physical violence and perinatal, neonatal and infant mortality among a representative sample of rural Indian women.
Study setting
The analysis examines women in rural areas of four economically and culturally contrasting states: Bihar, Jharkhand, Maharashtra and Tamil Nadu. The four states vary widely across a range of indicators related to socio-economic and women’s status, with a principal demarcation between the North Indian states of Bihar and Jharkhand (formerly one state) and the states of Maharashtra and Tamil Nadu, situated in Western and South India, respectively. On all indicators of women’s status—age at marriage, mass media exposure, literacy and ability to avail child health services—women in Bihar and Jharkhand fare considerably worse relative to women in Maharashtra and Tamil Nadu. These data demonstrate the marked developmental, social and cultural divide that distinguishes the North Indian region from the South and Western Indian region.32 The principal difference between the states is the unique kinship structure of North India, which ascribes little autonomy to females.32,33 Under these conditions, physical abuse and punishment of women is a common feature of North Indian society; previous studies have suggested that levels of domestic violence are so high in North India that domestic violence is a normative and tolerated element of society.34 Although lower levels of violence are reported in Southern India, previous studies have identified levels of violence that are high by international comparisons.35
Methods
Two linked data sets are utilized for this analysis: the National Family Health Survey-2 (NFHS-2)—the Indian equivalent of the Demographic and Health Survey—was India’s second national survey, carried out in 1998–99, and a prospective follow-up study for a subgroup of women in four states carried out in 2002–03.
The NFHS-2 sample covered 99% of India’s population, residing in its 26 states, and ultimately included a total of 89 199 reproductive-aged (15–49 years) women.36 The NFHS-2 included three questionnaires—a household questionnaire, which collected basic socio-demographic information on all usual residents of the household; a village questionnaire, which collected information on the availability of specific facilities, programmes and services in the village; and a women’s questionnaire, which collected a range of information concerning women’s socio-demographic characteristics, fertility behaviour and intentions, and experience of domestic violence. Overall response rates for sampled women respondents were very high, ranging from 94 to 99% in the states included in the present study.
Following completion of the NFHS-2 survey, a prospective follow-up study of original NFHS-2 respondents was planned by the International Institute for Population Sciences (IIPS) in Mumbai, India, which also implemented the NFHS-2, and the Johns Hopkins Bloomberg School of Public Health. IIPS had conducted the NFHS-2 and so had access to the information necessary to identify and locate respondents. The follow-up study was prompted by a number of research interests—including the relationship between family planning service quality and subsequent contraceptive use, and the predictive validity of stated fertility intentions.37 Ethical approval for the study and resulting analysis was provided by institutional review board at Johns Hopkins Bloomberg School of Public Health. The sampling frame for the NFHS-2 follow-up survey consisted of all rural respondents interviewed in the original 1998–99 NFHS-2 study in four Indian states: Bihar and Jharkhand in the North (originally the state of Bihar at the time of the NFHS-2 survey), Maharashtra in the West and Tamil Nadu in the South, chosen to represent differing demographic, socio-economic and service delivery contexts within India. Given its focus on service quality and contraceptive use, and the multi-faceted nature of family planning service delivery in urban areas, the follow-up survey was restricted to rural respondents. The sample was further restricted to currently married women aged 15–39 years of age, who were usual residents of the household at the time of the 1998–99 NFHS-2 interviews, given the focus on subsequent fertility and contraceptive behaviour. The survey instrument included questions pertaining to respondent background characteristics, reproductive behaviour and intentions, quality of family planning care, use of family planning methods and services, an event calendar covering the intervening months between the baseline (NFHS-2) and the follow-up survey (to assess intervening pregnancies, pregnancy outcomes and monthly contraceptive use status), and domestic violence experience.
High re-interview rates were achieved in all four states: 76% in Maharashtra, 80% in Bihar, 82% in Jharkhand and 94% in Tamil Nadu. As documented elsewhere, with the exception of somewhat lower prevalence levels of baseline contraceptive and domestic violence in Bihar and Tamil Nadu, the reinterviewed and non-reinterviewed samples of women were generally similar in terms of characteristics, indicating no significant selectivity in our reinterviewed sample.11,37 The data set for analysis is comprised of linked data from the NFHS-2 and the follow-up survey and consists of all inter-survey births, producing a total sample of 3909 live births.
Following conventional Demographic and Health Survey (DHS) approaches, respondents were asked at the follow-up survey about all live birth outcomes that occurred during the 48-month inter-survey period (1998–99 to 2002–03). For each reported live birth, detailed questions were then asked concerning the survival/death of each birth, and, among deaths, the precise timing (day of death during the first month, month of death during ages 1–23 months, year of death subsequently). Respondents were then queried regarding all non-live birth outcomes (stillbirths, spontaneous and induced abortions) that occurred during the inter-survey period, with gestational age and calendar month and year of outcome recorded for each such event. All pregnancy outcome information was also copied to the monthly event calendar. The calendar approach was then used to further probe for possible pregnancy events when extended periods of non-pregnancy without contraception were detected. The calendar approach is now widely used in DHS surveys, and evaluations have shown it to be highly accurate in capturing both pregnancy and contraceptive events.38,39 Questions related to domestic violence were included in both the 1998–99 NFHS-2 and 2002–03 NFHS-2 follow-up surveys. However, given that the outcomes modelled (infant mortality) are measured at the follow-up survey, it was preferable to use a measure of violence that temporally preceded the outcome of interest; thus, our violence exposure measure is taken from the 1998–99 NFHS-2 survey.
In the 1998–99 NFHS-2 survey, a limited set of questions were asked of all female respondents regarding their experience with domestic violence:
Since you completed 15 years of age, have you been beaten or mistreated physically by any person?
Who has beaten you or mistreated you physically?
How often have you been beaten or mistreated physically in the last 12 months: once, a few times, many times, or not at all?
The analysis considered three outcomes: perinatal mortality (stillbirths plus deaths during the first 7 days of life), neonatal mortality (deaths during the first month of life) and infant mortality (deaths during months 0–11 of life). Deaths during the post-neonatal period (deaths during months 1–11 of life) were too few to provide stable estimates, and were therefore not estimated. Under 5-year mortality was not estimated because of the shorter observation period during the follow-up.
Statistical differences in childhood mortality rates by violence status were estimated with Wilcoxon’s chi-square and log-rank tests of the survival curves. Separate Cox hazard regression models were fitted for each outcome, with a death during the 48-month exposure period representing the failure event after validating the proportionally assumptions of the models. All models were adjusted for the possible effects of clustering at the primary sampling unit level: there were insufficient cases of women to control for clustering at the household level. The key covariate of interest in each of the models is whether the respondent reported experiencing physical domestic violence from her husband in the 12 months prior to the 1998–99 NFHS-2 survey, categorized as: no violence, one act of violence, and more than 2 acts of violence in the 12 months prior to the baseline survey. Women who reported that they had never experienced physical violence from their husbands and women who reported that they had not experienced violence in the 12 months prior to the survey were coded as zero, women who reported only one act of violence in the last 12 months were coded as 1, and women who reported multiple acts of violence were coded as 2. The models also control for maternal age, parity, education (of both respondent and husband), household assets and state of residence. Household assets are measured by the ownership of nine goods (fan, telephone, cycle, refrigerator, vehicle, washing machine, television, radio and motorcycle) and are categorized into terciles (low, medium and high). Interactions between child’s age and other covariates were examined and found not to be present.
Results
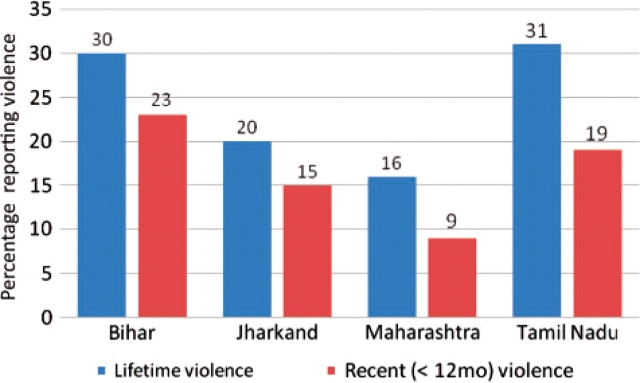
Lifetime rates of physical beating or mistreatment for our study sample range from a low of 16% in Maharashtra to a high of 31% in Tamil Nadu (Figure 1). Figure 1 also shows the state-wise frequency distributions of domestic violence by husbands in the previous 12 months, the exposure variable used in the present analysis. The percentage age of women reporting one or more episodes of violence in the past 12 months ranged from 9% in Maharashtra to 23% in Bihar. These rates—from women who had given at least one birth during the past 4 years—were similar or slightly higher than the all women of reproductive age rates reported in the NFHS-2. Infant mortality levels ranged from 44 to 57 per 1000 live births in the four states. This primarily reflects the persistence of moderately high levels of neonatal mortality, as post-neonatal mortality levels were substantially lower in all four states. Perinatal mortality rates varied from 36 to 45 per 1000 live births across the four states. Reporting of violence was higher among women aged >35 years, living in Bihar, at higher parity (over four children), women who were illiterate and women living in less wealthy households (Table 1).
Figure 1.
Lifetime and recent (<12 months) physical domestic violence
Table 1.
Distribution of independent variables and domestic violence (n = 3909)
| Percentage | Percentage reporting one recent violent episode | Percentage reporting more than one recent violent episode | |
|---|---|---|---|
| Mother experienced physical domestic violence in the past 12 months | |||
| None | 80.3 | ||
| One episode | 5.4 | ||
| More than one episode | 14.4 | ||
| Maternal age, years | |||
| <24 | 34.3 | 4.2 | 8.9 |
| 25–29 | 35.4 | 4.8 | 13.6 |
| 30–34 | 20.4 | 6.6 | 18.2 |
| >35 | 9.7 | 6.3 | 18.8 |
| Parity | |||
| 1–2 | 6.8 | 4.9 | 6.7 |
| 3–4 | 46.6 | 3.9 | 11.3 |
| >4 | 46.6 | 6.6 | 19.6 |
| Woman’s education | |||
| None | 72.8 | 6.6 | 17.2 |
| Primary | 13.6 | 2.8 | 9.9 |
| Secondary/higher | 13.6 | 3.6 | 6.9 |
| Husband’s education | |||
| None | 40.3 | 5.2 | 18.7 |
| Primary | 15.4 | 6.7 | 14.7 |
| Secondary | 34.0 | 5.4 | 12.2 |
| Higher | 10.3 | 2.5 | 6.6 |
| Sex of child | |||
| Male | 51.6 | 5.23 | 16.2 |
| Female | 48.4 | 5.26 | 13.5 |
| Household assets | |||
| Low | 58.4 | 5.5 | 18.1 |
| Medium | 35.1 | 5.3 | 11.2 |
| High | 6.5 | 2.2 | 2.2 |
| Caste | |||
| Scheduled caste | 32.0 | 4.3 | 9.8 |
| Schedules tribe | 51.7 | 3.9 | 10.4 |
| Other | 16.3 | 4.3 | 11.4 |
| Received prenatal care in last pregnancy | |||
| No | 47.0 | 4.6 | 10.8 |
| Yes | 53.0 | 3.4 | 9.4 |
| State | |||
| Bihar | 59.2 | 5.8 | 17.2 |
| Jharkhand | 14.0 | 4.6 | 11.1 |
| Maharashtra | 11.2 | 2.7 | 6.7 |
| Tamil Nadu | 15.6 | 5.3 | 13.7 |
The characteristics of the 3909 births in the analysis are shown in Table 1. Most births in the study are parity 3 or higher, reflecting the selectivity of births to higher parity women during the inter-survey period. More than 70% of births occur to mothers who are uneducated; fathers are also characterized by low levels of educational attainment. Almost three in five households in the sample could be classified as having low household assets. Almost three-quarters of inter-survey births come from the states of Bihar or Jharkhand, a reflection of the much lower levels of fertility control in these North Indian states.
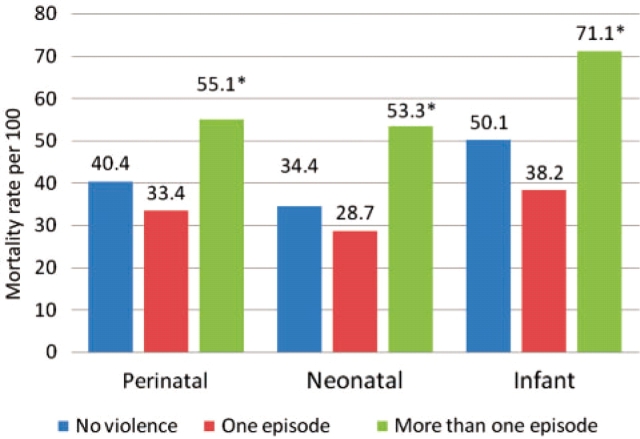
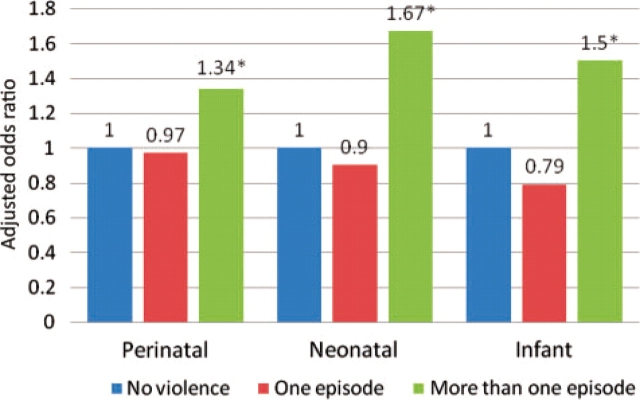
Figure 2 shows the bivariate associations between reported violence and mortality outcomes. For all three mortality outcomes, no differences in mortality were observed for births whose mothers experienced one episode of recent violence vs no episodes of violence. In contrast, births to mothers who experienced two or more recent episodes of domestic violence were more likely to experience all three mortality outcomes. Figure 3 shows the unadjusted hazard ratios (HRs) for the effects of violence on mortality; in all three periods mortality risks were higher among women who had experienced multiple episodes of recent physical violence. Table 2 shows the adjusted Cox proportional hazards results. Relative to the reference group of women who experienced no recent domestic violence, perinatal mortality levels were higher HR = 1.85, 95% confidence interval (CI) = 1.12, 2.79] among women who reported multiple episodes of recent violence. Older maternal age (>35 years) and lower parity (one to two living children) were both associated with higher risks of perinatal mortality. Relative to uneducated mothers, births born to mothers with primary school education face lower risks of perinatal mortality. Finally, after controlling for other covariates, female offspring experience lower risks of perinatal mortality compared with male children.
Figure 2.
Perinatal, neonatal and infant mortality rates (per 1000) by violence exposure. 'Asterisk' indicates rate significantly different from the ‘no violence rate’ at the 5% level
Figure 3.
Unadjusted HRs for perinatal, neonatal and infant mortality. 'Asterisk' indicates rate significantly different from the ‘no violence rate’ at the 5% level
Table 2.
Adjusted Cox hazard regression models for perinatal, neonatal and infant mortality (n = 3909)
| Covariates | Perinatal | Neonatal | Infant |
|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Mother experienced recent domestic violence (none) | |||
| One violent episode | 0.77 (0.34, 1.57) | 0.78 (0.45, 1.34) | 0.59 (0.25, 1.31) |
| More than one violent episode | 1.85 (1.12, 2.79) | 1.62 (1.11, 2.53) | 1.68 (1.10, 2.57) |
| Maternal age (<24), years | |||
| 25–29 | 1.10 (0.70, 1.81) | 1.04 (0.66, 1.64) | 1.18 (0.83, 1.68) |
| 30–34 | 1.24 (0.65, 2.47) | 0.84 (0.48, 1.52) | 0.75 (0.44, 1.27) |
| >35 | 2.05 (1.02, 3.99) | 1.50 (0.73, 3.05) | 1.29 (0.70, 2.38) |
| Parity (1–2) | |||
| 3–4 | 0.35 (0.19, 0.74) | 0.79 (0.32, 1.87) | 0.77 (0.33, 1.64) |
| >4 | 0.32 (0.17, 0.65) | 1.19 (0.47, 2.97) | 1.17 (0.57, 2.47) |
| Maternal education (none) | |||
| Primary | 0.47 (0.22, 0.96) | 0.76 (0.43, 1.38) | 0.64 (0.39, 1.12) |
| Secondary | 1.11 (0.55, 2.20) | 1.43 (0.72, 2.86) | 0.96 (0.49, 1.91) |
| Higher | 0.53 (0.21, 1.31) | 0.58 (0.18, 1.71) | 0.54 (0.32, 0.91) |
| Paternal education (none) | |||
| Primary | 0.96 (0.59, 1.61) | 1.23 (0.75, 2.02) | 1.04 (0.68, 1.58) |
| Secondary | 0.87 (0.61, 1.32) | 0.85 (0.53, 1.35) | 0.92 (0.63, 1.34) |
| Higher | 0.83 (0.45, 1.65) | 0.68 (0.29, 1.57) | 0.66 (0.33, 1.34) |
| Sex of child (male) | |||
| Female | 0.70 (0.50, 0.91) | 0.74 (0.52, 1.05) | 0.65 (0.42, 0.94) |
| Household assets (low) | |||
| Medium | 1.32 (0.88, 1.96) | 1.30 (0.90, 1.89) | 1.14 (0.83, 1.58) |
| High | 1.22 (0.54, 3.02) | 0.83 (0.34, 2.33) | 0.51 (0.17, 1.51) |
| Caste (scheduled caste) | |||
| Schedules tribe | 1.03 (0.68, 1.23) | 1.10 (0.54, 1.49) | 1.13 (0.67, 1.38) |
| Other | |||
| Received prenatal care in last pregnancy (no) | |||
| Yes | 0.84 (0.64, 1.12) | 0.82 (0.58, 1.32) | 0.82 (0.54, 1.42) |
| State (Bihar) | |||
| Jharkhand | 0.89 (0.46, 1.56) | 1.10 (0.67, 1.83) | 0.89 (0.58, 1.38) |
| Maharashtra | 0.76 (0.53, 1.27) | 1.12 (0.61, 1.95) | 1.03 (0.63, 1.72) |
| Tamil Nadu | 0.79 (0.41, 1.52) | 1.02 (0.60, 2.05) | 0.85 (0.52, 1.47) |
Figures in italics are significant at the 5% level.
Higher mortality rates persisted through the neonatal period among women reporting more frequent abuse (HR = 1.62, 95% CI = 1.11, 2.53); no other covariates were predictive of neonatal mortality. In terms of overall infant mortality risks, women experiencing more frequent violence faced hazards of infant mortality risk ∼70% higher (HR = 1.68, 95% CI = 1.10, 2.57) than women who did not experience violence. In terms of other covariates, only being a female child was associated with a decreased risk of infant mortality. Surprisingly, there was no association between household wealth and mortality.
Conclusions
Over the past decade, there has been increased recognition of the serious health implications of domestic violence for both women and their families. Much of this evidence has focused on the consequences of such violence for birth outcomes and early childhood mortality, drawn mainly from special populations in more developed countries. Evidence from developing countries, characterized by high levels of both domestic violence and early childhood mortality, remains much more limited. Evidence on levels of domestic violence in Africa and South Asia indicate that between 10 and 28% of women experienced some form of violence during their current or most recent pregnancy,40 with studies from India reporting prevalence levels toward the upper end of this range.41–43
Using a more rigorous prospective design than the cross-sectional design of previous studies, our study adds to the presently slender body of empirical evidence on the association between domestic violence and adverse birth outcomes. Overall, we find that births to mothers subjected to violence may experience infant mortality risks ∼70% higher than those free from such violence. Several possible pathways exist which may explain the relationship between domestic violence and poor birth outcomes.44–46 One pathway could be the role of blunt trauma to the fetus in precipitating adverse pregnancy and birth outcomes, explaining the association between violence and perinatal/neonatal mortality.7,47,48 A second pathway may be through the link between domestic violence and elevated levels of maternal stress, which in turn has been shown to be related to low birthweight/prematurity, that are known risk factors for poor birth outcomes: again this mechanism may explain the relationship between violence and perinatal/neonatal mortality.48,49 Alternatively, recent studies have shown an association between domestic violence and anaemia for women in India:50 thus, the effects of violence on child mortality may be operating through the poor physical health of the mother created by exposure to violence. A third mechanism could be the deterrent effect of violence (or the fear of such violence) upon maternal health care seeking behaviour.51,52 Investigation of the specific pathways through which domestic violence might influence perinatal/early infant mortality should be a high priority for future research. A surprising result identified here is the association between multiple episodes of violence and mortality, and the finding that a single episode of violence was not associated with increased risks of mortality. A plausible explanation could be that there was a marked difference in the frequency and severity of violence between the mothers reporting a single act of physical violence vs a few/many violent acts.
Two potential limitations of our study should also be noted. One potential limitation concerns the measurement of domestic violence using the 1998–99 baseline (NFHS-2) survey. In contrast to the detailed module of questions on both physical and sexual domestic violence in the 2002–03 follow-up study, the domestic violence questions included in the 1998–99 NFHS-2 survey were limited in both number and specificity, and focused only upon physical violence. While interviews were conducted in private and confidentiality in information was maintained, the possibility exists that domestic violence levels may still be underreported.53 A second related limitation is the absence of specific questions regarding domestic violence during each index pregnancy. [While this question was asked at the follow-up survey, it referred only of the most recent pregnancy, yielding too few cases (and too few deaths) for meaningful analysis.] In the absence of such information, we have assumed that violence levels reported do not vary during the pre-pregnancy, pregnancy and post-partum periods, an assumption supported by previous work from the USA.54 While we note these potential limitations, the advantages of using a prospective study design—which allows us to establish temporal ordering between violence and birth outcomes and limit the possibility of reverse causality (birth outcomes influencing responses to domestic violence questions)—in our view significantly outweighs the potential limitations associated with the available data. We can also not rule out the possibility of the existence of other not measured confounding factors that result in both high mortality and high levels of violence: thus, although we can disentangle temporality, we cannot identify causality.
While significant progress has been made over the past two decades in reducing levels of early childhood mortality, levels remain unacceptably high in many developing countries.55,56 While efforts have focused upon a wide range of preventive and curative child health interventions, the issue of violence to mothers during pregnancy has remained largely outside the purview of current child survival programmes. A central contributing factor has been the absence of rigorous empirical evidence on both levels of domestic violence in low-resource settings as well as evidence linking such violence to adverse birth and child survival outcomes. The present study represents an important step toward redressing this dearth of evidence. Although additional prospective studies from developing countries are needed with improved measures of exposure to violence during pregnancy, our results suggest that the violence prevention may represent a significant intervention for lowering current levels of perinatal and infant mortality in settings such as rural India. Thus, in addition to the health and human rights benefits for women themselves, the incorporation of violence prevention into current programmes may offer significant dividends in terms of improvements in child survival.
Funding
This research was funded by the National Institute of Child Health and Human Development, grant number R01HD039405.
KEY MESSAGES.
Children born to mothers who experience more than one episode of physical violence from their husband are at an increased risk of mortality throughout the first year of life.
Current maternal and child health programmes, in particular prenatal care, need to include screening for domestic violence among female clients.
References
- 1.Heise L, Pitanguy J, Germain A. World Bank Discussion Paper No. 255. Washington, DC: The World Bank; 1994. Violence against women: The hidden health burden. [Google Scholar]
- 2.Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. The Lancet. 2002;360:1083–88. doi: 10.1016/S0140-6736(02)11133-0. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Moreno C, Jansen HAFM, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet. 2006;368:1260–69. doi: 10.1016/S0140-6736(06)69523-8. [DOI] [PubMed] [Google Scholar]
- 4.Jejeebhoy SJ, Cook RJ. State accountability for wife-beating: the Indian challenge. The Lancet. 1997;349:SI10–12. doi: 10.1016/s0140-6736(97)90004-0. [DOI] [PubMed] [Google Scholar]
- 5.International Institute for Population Sciences (IIPS) and Macro International. 2007. National Family Health Survey (NFHS-3), 2005–06: India: Volume I. Mumbai: IIPS [Google Scholar]
- 6.Naved RT, Persson LA. Factors associated with spousal physical violence against women in Bangladesh. Stud Fam Plann. 2005;36:289–300. doi: 10.1111/j.1728-4465.2005.00071.x. [DOI] [PubMed] [Google Scholar]
- 7.Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359:1331–36. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 8.Mullen PE, Romans-Clarkson SE, Walton VA, Herbison GP. Impact of sexual and physical abuse on women’s mental health. Lancet. 1988;8590:841–45. doi: 10.1016/s0140-6736(88)91600-5. [DOI] [PubMed] [Google Scholar]
- 9.Ellsberg M, Caldera T, Herrera A, Winkvist A, Kullgran G. Domestic violence and emotional distress among Nicaraguan women: Results from a population-based study. Am Psychologist. 1999;54:30–36. [Google Scholar]
- 10.Kishor S, Johnson K. Reproductive health and domestic violence: are the poorest women uniquely disadvantaged? Demography. 2006;43:293–307. doi: 10.1353/dem.2006.0014. [DOI] [PubMed] [Google Scholar]
- 11.Stephenson R, Koenig MA, Acharya R, Roy TK. Domestic violence, contraceptive use and unwanted pregnancy in rural India. Stud Family Planning. 2008;39:177–86. doi: 10.1111/j.1728-4465.2008.165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jewkes R, Vundule C, Maforah F, Jordaan E. Relationship dynamics and teenage pregnancy in South Africa. Social Sci Med. 2001;52:733–44. doi: 10.1016/s0277-9536(00)00177-5. [DOI] [PubMed] [Google Scholar]
- 13.Pallito CC, O’Campo P. The relationship between intimate partner violence and unintended pregnancy: analysis of a national sample from Colombia. Int Family Planning Perspect. 2004;30:165–73. doi: 10.1363/3016504. [DOI] [PubMed] [Google Scholar]
- 14.Schei B, Bakketeig LS. Gynaecological impact of sexual and physical abuse by spouse: a study of a random sample of Norwegian women. Br J Obstetrics Gynaecol. 1989;96:1379–83. doi: 10.1111/j.1471-0528.1989.tb06298.x. [DOI] [PubMed] [Google Scholar]
- 15.Champion JD, Shain RN. The context of sexually transmitted disease: life histories of woman abuse. Issues Mental Health Nurs. 1998;19:463–79. doi: 10.1080/016128498248908. [DOI] [PubMed] [Google Scholar]
- 16.Quigley MA, Morgan D, Malamba SS, et al. Case-control study of risk factors for incident HIV infection in rural Uganda. J Acquired Immune Deficiency Syndr. 2000;5:418–25. doi: 10.1097/00126334-200004150-00009. [DOI] [PubMed] [Google Scholar]
- 17.Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet. 2004;363:1415–21. doi: 10.1016/S0140-6736(04)16098-4. [DOI] [PubMed] [Google Scholar]
- 18.Petersen R, Gazmararian JA, Spitz MA, et al. Violence and adverse pregnancy outcomes: A review of the literature and directions for future research. Am J Preventive Med. 1997;13:366–73. [PubMed] [Google Scholar]
- 19.Murphy CC, Schei B, Myhr TL, Du Mont J. Abuse: a risk factor for low birth weight? A systematic review and meta-analysis. Canadian Med Assoc J. 2001;164:1567–72. [PMC free article] [PubMed] [Google Scholar]
- 20.Valladares E, Ellsberg M, Pena R, Hogberg U, Persson LÅ. Physical partner abuse during pregnancy: A risk factor for low birth weight in Nicaragua. Obstetrics Gynecol. 2002;100:700–5. doi: 10.1016/s0029-7844(02)02093-8. [DOI] [PubMed] [Google Scholar]
- 21.Newberger EH, Barkan SE, Lieberman ES, McCormick MC, Yllo K, Gary LT. Abuse of pregnant women and adverse birth outcome: current knowledge and implications for practice. JAMA. 1992;267:2370–72. [PubMed] [Google Scholar]
- 22.McFarlane J, Parker B, Soeken K. Abuse during pregnancy: Associations with maternal health and infant birth weight. Nurs Res. 1996;45:37–42. doi: 10.1097/00006199-199601000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Rodrigues T, Rocha L, Barros H. Physical abuse during pregnancy and preterm delivery. Am J Obstetrics Gynecol. 2008;198:171e1–e6. doi: 10.1016/j.ajog.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 24.Yost NP, Bloom SL, McIntire DD, Leveno KJ. A prospective observational study of domestic violence during pregnancy. Obstetrics Gynecol. 2005;106:61–65. doi: 10.1097/01.AOG.0000164468.06070.2a. [DOI] [PubMed] [Google Scholar]
- 25.Lipsky S, Holt VL, Easterling TR, Critchlow CW. Impact of police-reported intimate partner violence during pregnancy on birth outcomes. Obstetrics Gynecol. 2003;102:557–64. doi: 10.1016/s0029-7844(03)00573-8. [DOI] [PubMed] [Google Scholar]
- 26.Jejeebhoy SJ. Associations between wife-beating and fetal and infant death: Impressions from a survey in rural India. Stud Family Planning. 1998;29:300–8. [PubMed] [Google Scholar]
- 27.Ahmed S, Koenig MA, Stephenson RB. Effect of domestic violence on early childhood mortality: evidence from North India. Am J Pub Health. 2006;96:1423–28. doi: 10.2105/AJPH.2005.066316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ackerson SL, Subramanian SV. Intimate partner violence and death among infants and children in India. Pediatrics. 2009;124:e878–89. doi: 10.1542/peds.2009-0524. [DOI] [PubMed] [Google Scholar]
- 29.Asling-Monemi K, Peña R, Ellsberg MC, Persson LÅ. Violence against women increases the risk of infant and child mortality: A case-referent study in Nicaragua. Bull WHO. 2003;81:10–6. [PMC free article] [PubMed] [Google Scholar]
- 30.Emenike E, Lawoko S, Dalal K. Intimate partner violence and reproductive health of women in Kenya. Int Nursing Rev. 1998;55:97–102. doi: 10.1111/j.1466-7657.2007.00580.x. [DOI] [PubMed] [Google Scholar]
- 31.Silverman J, Gupta J, Decker M, Kapur N, Raj A. Intimate partner violence and unwanted pregnancy, miscarriage, induced abortion, and stillbirth among a national sample of Bangladeshi women. Br J Obstetrics Gynaecol. 2007;114:1246–52. doi: 10.1111/j.1471-0528.2007.01481.x. [DOI] [PubMed] [Google Scholar]
- 32.Dyson T, Moore M. On kinship structure, female autonomy and demographic behavior in India. Population Dev Rev. 1983;9:35–60. [Google Scholar]
- 33.Griffiths P, Hinde A, Matthews Z. Infant and child mortality in three culturally contrasting states of India. J Biosocial Sci. 2001;33:603–22. doi: 10.1017/s0021932001006034. [DOI] [PubMed] [Google Scholar]
- 34.Koenig MA, Stephenson RB, Ahmed SA. Individual and contextual determinants of domestic violence in North India. Am J Pub Health. 2006;96:132–38. doi: 10.2105/AJPH.2004.050872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rao V. Wife-beating in rural South India: a qualitative and econometric analysis. Soc Sci Med. 1997;44:1169–80. doi: 10.1016/s0277-9536(96)00252-3. [DOI] [PubMed] [Google Scholar]
- 36.International Institute for Population Sciences (IIPS), ORC Macro. National Family Health Survey (NFHS-2), 1998-99: India. Mumbai: IIPS; 2000. [Google Scholar]
- 37.International Institute for Population Sciences (IIPS) Quality of Care in Indian Family Planning Programme and Reproductive Behaviour of Women in Four Indian States: A Follow-up Study of NFHS-2. Mumbai: IIPS; 2005. Johns Hopkins Bloomberg School of Public Health. [Google Scholar]
- 38.Strickler JA, Magnani RJ, McCann HG, Brown LF, Rice JC. The reliability of reporting of contraceptive behavior in DHS calendar data: Evidence from Morocco. Stud Family Planning. 1997;28:44–53. [PubMed] [Google Scholar]
- 39.Bairagi R, Becker S, Kantner A, Allen KB, Dutta A, Purvis K. Asian-Pacific Population Research Reports. An evaluation of the 1993-94 Bangladesh Demographic and Health Survey within the Matlab area. 11(1997), Honolulu, Hawaii: East-West Population Center. [PubMed] [Google Scholar]
- 40.Nasir K, Hyder AA. Violence against pregnant women in developing countries: review of evidence. Eur J Pub Health. 2003;13:105–07. doi: 10.1093/eurpub/13.2.105. [DOI] [PubMed] [Google Scholar]
- 41.Muthal-Rathore A, Tripathi R, Arora R. Domestic violence against pregnant women interviewed at a hospital in New Delhi. Int J Gynecol Obstetrics. 2002;76:83–85. doi: 10.1016/s0020-7292(01)00533-1. [DOI] [PubMed] [Google Scholar]
- 42.Peedicayil A, Sadowski LS, Jeyaseelan L, et al. India SAFE Group. Spousal physical violence against women during pregnancy. Br J Obstetrics Gynaecol. 2004;111:682–87. doi: 10.1111/j.1471-0528.2004.00151.x. [DOI] [PubMed] [Google Scholar]
- 43.Purwar MB, Jeyaseelan L, Varhadpande U, Motghare V, Pimplakute S. Survey of physical abuse during pregnancy GMCH, Nagpur, India. J Obstetrics Gynaecol Res. 1999;25:165–71. doi: 10.1111/j.1447-0756.1999.tb01142.x. [DOI] [PubMed] [Google Scholar]
- 44.Cokkinides VE, Coker A, Sanderson M, Addy C, Bethea L. Physical violence during pregnancy: Maternal complications and birth outcomes. Obstetrics Gynecol. 1999;93:661–66. doi: 10.1016/s0029-7844(98)00486-4. [DOI] [PubMed] [Google Scholar]
- 45.Coker AL, Sanderson M, Dong B. Partner violence during pregnancy and risk of adverse pregnancy outcomes. Paediatric Perinatal Epidemiol. 2004;18:260–69. doi: 10.1111/j.1365-3016.2004.00569.x. [DOI] [PubMed] [Google Scholar]
- 46.Gazmararian JA, Lazorick S, Spitz AM, Ballard TJ, Saltzman LE, Marks JS. Prevalence of violence against pregnant women: A review of the literature. JAMA. 1996;275:1915–20. [PubMed] [Google Scholar]
- 47.Jasinski JL. Pregnancy and domestic violence: a review of the literature. Trauma Viol Abuse. 2004;5:47–64. doi: 10.1177/1524838003259322. [DOI] [PubMed] [Google Scholar]
- 48.Omer H, Everly GS. Psychological factors in pre-term labor: critical review and theoretical synthesis. Am J Psychiatry. 1988;145:1507–13. doi: 10.1176/ajp.145.12.1507. [DOI] [PubMed] [Google Scholar]
- 49.Paarlberg MK, Vingerhoets JJM, Passchier J, Dekker GA, Van Geijin HP. Psychosocial factors and pregnancy outcome: a review with emphasis on methodological issues. J Psychosomatic Res. 1995;39:563–95. doi: 10.1016/0022-3999(95)00018-6. [DOI] [PubMed] [Google Scholar]
- 50.Ackerson LK, Subramanian SV. Domestic violence and chronic malnutrition among women and children in India. Am J Epidemiol. 2008;167:1188–96. doi: 10.1093/aje/kwn049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dietz PM, Gazmararian JA, Goodwin MM, Bruce FC, Johnson CH, Rochat RW. Delayed entry into prenatal care: effect of physical violence. Obstetrics Gynecol. 1997;90:221–24. doi: 10.1016/s0029-7844(97)00252-4. [DOI] [PubMed] [Google Scholar]
- 52.Webster J, Chandler J, Battistutta D. Pregnancy outcomes and health care use: effects of abuse. Am J Obstetrics Gynecol. 1996;174:760–67. doi: 10.1016/s0002-9378(96)70461-1. [DOI] [PubMed] [Google Scholar]
- 53.Ellsberg M, Heise L, Pena R, Agurto S, Winkvist A. Researching domestic violence against women: methodological and ethical considerations. Stud Family Planning. 2001;32:1–16. doi: 10.1111/j.1728-4465.2001.00001.x. [DOI] [PubMed] [Google Scholar]
- 54.Martin SL, Mackie L, Kupper LL, Buescher PA, Moracco KE. Physical abuse of women before, during, and after pregnancy. JAMA. 2001;285:1581–84. doi: 10.1001/jama.285.12.1581. [DOI] [PubMed] [Google Scholar]
- 55.Bryce J, Black RE, Walker N, Bhutta ZA, Lawn JE, Steketee RW. Can the world afford to save the lives of 6 million children each year? Lancet. 2005;365:2193–200. doi: 10.1016/S0140-6736(05)66777-3. [DOI] [PubMed] [Google Scholar]
- 56.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS the Bellagio Child Survival Study Group. How many child deaths can we prevent this year? The Lancet. 2003;362:65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]