Summary
Distance is a crucial feature of health service use and yet its application and utility to health care planning have not been well explored, particularly in the light of large-scale international and national efforts such as Roll Back Malaria. We have developed a high-resolution map of population-to-service access in four districts of Kenya. Theoretical physical access, based upon national targets, developed as part of the Kenyan health sector reform agenda, was compared with actual health service usage data among 1668 paediatric patients attending 81 sampled government health facilities. Actual and theoretical use were highly correlated. Patients in the larger districts of Kwale and Makueni, where access to government health facilities was relatively poor, travelled greater mean distances than those in Greater Kisii and Bondo. More than 60% of the patients in the four districts attended health facilities within a 5-km range. Interpolated physical access surfaces across districts highlighted areas of poor access and large differences between urban and rural settings. Users from rural communities travelled greater distances to health facilities than those in urban communities. The implications of planning and monitoring equitable delivery of clinical services at national and international levels are discussed.
Keywords: geographic information systems, equity, physical access, health services, fevers, Kenya
Introduction
The objective of the Roll Back Malaria (RBM) movement is to halve malaria morbidity and mortality by the year 2010 (Nabarro & Tayler 1998). A number of standardized core and supplementary indicators have been established by RBM to assess progress towards effective malaria control and prevention, in concert with internationally agreed milestones for the year 2005 (Roll Back Malaria/World Health Organization 2000). To ensure efficiency in planning, monitoring and evaluation of malaria control programmes, RBM recommends that data collection be kept to a minimum and existing country mechanisms be used as far as possible. The result of this is that a number of measures vital to the analysis of equity of intervention programmes are not routinely monitored. These include the spatially defined components of equitable access to and use of health services and interventions.
Equity in service provision is increasingly being used as a measure of health system performance (Thaddeus & Maine 1994; WHO 1996, 1999, 2000; Makinen et al. 2000). Equity manifests itself in the distribution, access to and utilization of health services between population groups (Thaddeus & Maine 1994; Division of Statistics, United Nations 1997). Access to health services is influenced by many behavioural, cost and distance factors (Ingram et al. 1978; Igun 1979; Annis 1981; Fiedler 1981; Garner & Giddings 1985; Habib & Vaughan 1986; Thaddeus & Maine 1994; Haddad et al. 1998; Muller et al. 1998; Tanser 2000) and utilization of health services is increasingly being viewed as a function of accessibility (Phillips 1979; Annis 1981; Stock 1983; Hayes et al. 1990). To achieve the target of substantially reducing malaria morbidity and mortality, RBM has recognized access to prompt diagnosis and treatment of malaria as a key strategic objective (Roll Back Malaria/World Health Organisation 2000). In addition, the overall goal of the Government of Kenya health sector policy until the year 2010 will be the deliberate restructuring of the health sector to make all health services more effective, accessible and affordable. Towards achieving these goals, one of the targets suggested in the health policy is that everyone will have access to health services within a 5-km range (Ministry of Health 1997).
The outcome of any disease is influenced by delay in decisions to seek care, timely arrival at appropriate diagnostic and treatment services and the receipt of adequate care from service providers. Distance continues to limit access to more sophisticated diagnostics and ranges of treatments operated by formal health services to manage malaria, where microscopy and second-line drugs are regulated and not provided outside of primary health care or in community-based approaches to malaria management. In this paper we explore the application of spatial analysis of formal government service providers using a geographic information system (GIS) to define the differences between theoretical distance criteria for potential health service use and the actual distances travelled by pediatric patients seeking malaria/fever case management.
Methodology
Study area
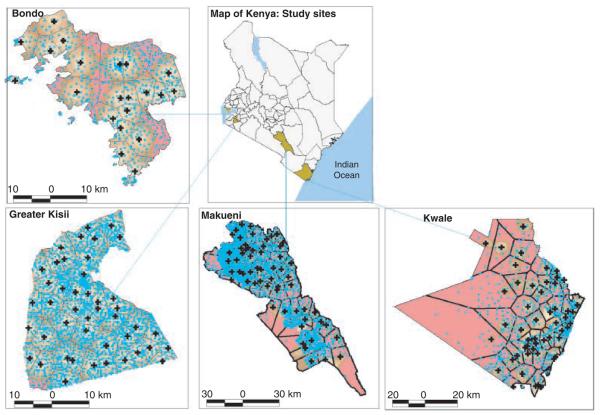
The study was undertaken in four districts across Kenya, encompassing a range of ecological, population and health service conditions prevailing nation-wide. These were (i) Greater Kisii district (divided in 1997 into Kisii Central and Gucha districts) located in the densely populated, high-intensity agricultural western highlands of Nyanza province; (ii) Bondo district, located along the shores of Lake Victoria in Nyanza province; (iii) Kwale district in Coast province, located in the south-eastern corner of Kenya on the border with Tanzania and along the Indian Ocean; and (iv) Makueni district in Eastern province which includes an extensive semi-arid area south of Nairobi (Figure 1).
Figure 1.
A district map of Kenya ( ) showing the study area (
) showing the study area ( ) and maps of each of the four districts showing a surface map of populations overall access to government health facilities (
) and maps of each of the four districts showing a surface map of populations overall access to government health facilities ( ) with varying shades of brown representing areas with access distances between <1–5 km and the red colour representing areas >5 km (
) with varying shades of brown representing areas with access distances between <1–5 km and the red colour representing areas >5 km ( <1,
<1,  1–2,
1–2,  2–3,
2–3,  3–4,
3–4,  4–5 and
4–5 and  >5 km). The populations are represented by light blue point
>5 km). The populations are represented by light blue point  , which are the EA centroids. Almost the entire population in Greater Kisii is within 5 km of a government health facility. In Bondo, Kwale and Makueni, 80%, 65% and 65% of the population were within 5 km of a government health facility, respectively.
, which are the EA centroids. Almost the entire population in Greater Kisii is within 5 km of a government health facility. In Bondo, Kwale and Makueni, 80%, 65% and 65% of the population were within 5 km of a government health facility, respectively.
Developing a GIS layer of population distribution
The most recent population and housing census of Kenya was conducted in August 1999 (Central Bureau of Statistics 2001). The highest spatial resolution data readily accessible in the public domain are provided at the sub-location. This fifth level administrative unit is defined by a population of about 4250 people. Population totals recorded at enumeration areas (EA) level (the smallest census unit) were obtained for the four districts in collaboration with the National Census Bureau. Each EA comprises part of a village, a whole village or group of villages that are usually not more than 100 households (approximately 500 people). The EAs were classified into urban and rural based on expert judgement. Areas with an estimated population of 2000 people or more, a significant amount of commercial activity and well connected to the motorable transport networks were classified urban, and the others as rural (D. Nalo, personal communication). The EA maps used during the national census were digitized using MicroStation 95 (Bentley Systems Inc., USA). All digital map and attribute data for the population were exported into ArcView 3.2 (ESRI Inc., USA) in which the EA population data were linked to EA polygon maps in each district and used to facilitate display and analysis of census data in the GIS. Population totals were represented by a centroid point data within each EA polygon generated using ArcView X-tools functions.
Developing the GIS layer of health services
We developed a national spatially linked database of clinical facilities by compiling provisional district-specific lists from databases, reports and maps held in Nairobi at the Ministry of Health, Christian Health Association of Kenya, Family Planning Logistics Management Organization, Central Bureau of Statistics, the Government's Gazette and topographical maps. These were then checked by District Health Management Teams at the district level to identify omissions, replications and errors. Finally each facility was visited to complete a simple questionnaire on its status, personnel and services provided and to record longitude and latitude readings. Coordinates were recorded using hand-held 12-band global positioning system (GPS) receivers Garmin etrex (Garmin Ltd, Kansas, USA) and Trimble (Trimble Navigation Ltd, California, USA). To minimize recording errors three longitudes and three latitude readings were taken for each facility and the average reading used to position the facility. This is likely to be accurate to ±15 m (URL: http://www.garmin.com). To explore the feasibility of the 5 km target suggested in the health sector reform strategy, we have restricted analysis to use of services provided by the government sector.
Developing GIS data of actual usage of facilities for paediatric treatment
As part of quality-of-care studies in each district, government health facilities were classified according to whether they were a dispensary or a hospital/health centre, and by the numbers of patients they managed each day. All hospitals were purposely selected while a stratified random sampling was used to select facilities in each of the other two categories as discussed in Zurovac et al. (2002). Two survey teams were used in each district during the peak malaria burden seasons of 2001–2002. Each team was assigned one facility per day over 2 days at which caretakers of febrile paediatric patients attending the health facilities were asked to provide information on the patient's home village or EA, village and household heads, nearest school, bus stop and health facility. Using this information, we assigned each patient to the correct EA. Where correct information on the patient's EA was not provided, we used information on the household head, village head, nearest school and bus stop to trace the patient to the village or EA, through repeated field visits.
Analytical methods
Analysis of potential usage of health facilities
The Thiessen polygon technique (ArcView 3.2, ESRI Inc.) was used to generate catchment areas for each government health facility in the four districts. This technique assigned each EA to the nearest health facility based on straight-line distances, creating polygon maps of facility catchment areas. Using ArcView 3.2 GIS geo-processor extension, the population of all EAs falling within a facility's catchment area was summed and recorded as the potential users of that facility. In computing potential users, all facilities, regardless of the type or size were assumed to have the same geographic drawing power for the purpose of this study, as they all provide similar out-patient clinical services (Zurovac et al. 2002).
Using the proximity-spider diagrams program
(Vandervoort 1999) within ArcView GIS, distances in kilometre, between each EA and the nearest health facility were computed. The result was a map of straight-line distance segments between each EA and its nearest health facility. For each district we adopted an 11-point distance scale (<1, 1–2, 2–3, 3–4, 4–5, 5–6, 6–7, 7–8, 8–9, 9–10 and >10) in kilometres. We computed the number of people with access to each government health facility at each distance scale for each district. We further divided the population into those with access within and outside a 5-km threshold. Mean access distances were computed for urban and rural EA in each district. Each urban and rural EA was further stratified by type of nearest health facility and we computed mean access distance by facility type. We interpolated the distance at each EA, using ArcView 3.2, Spatial Analyst, and created access surface maps to demonstrate the variation within each district visually.
Analysis of actual usage of health facilities
We computed the distance each patient travelled to the health facility at which they sought treatment. Using the 11-point scale, we computed the number of patients who use a health facility at each distance point. In addition, we derived the mean distances travelled by all users in a district. We grouped the facilities into hospitals, health centres and dispensaries and computed the sum of patients who used facilities of different types. The mean distances travelled by facility type were then calculated to establish variation in use by facility type. Users were also classified into urban and rural and mean distances travelled by each class analysed. To establish the overall effect of distance on the use of health facilities, we plotted the relationship between the number of patients who used a facility on the 11-point distance scale both as a discrete and as a cumulative use. To determine the nature of health facility's usage against the 5-km threshold, we derived the percentage of patients who used a health facility within this distance for each district. We colour coded users based on whether they used a facility within 5 km or outside. We superimposed these coded points on the potential usage surface maps to compare the relationship between actual use against the underlying distance predicted use.
We made a statistical comparison for each district between the cumulative percentage of potential users of the facilities used in the study and the percentage of actual users based on the 11-point distance scale. We performed a logarithmic transformation of the percentages as the relationship between distance and both potential and actual facility use was positively skewed. We used a simple linear regression to test the correlation between potential use based on distances to nearest facility and actual use revealed in the survey.
Results
Greater Kisii district, with an area of 1310 km2 had a population of 952 725 people across 1975 EAs making it the most densely populated of the four districts. This was followed by Bondo with an area of 960 km2, 238 780 people and 673 EAs and Makueni with an area of 8266 km2, 771 545 people and 1766 EAs. Kwale was least densely populated with an area of 8295 km2, 496 133 people and 822 EAs. Most of the populations in the four districts, 92% in Greater Kisii, 94% in Bondo, 89% in Kwale and 97% in Makueni were rural (Table 1). Greater Kisii had 44 Government of Kenya (GoK) health facilities while Bondo, Makueni and Kwale had 21, 59 and 50, respectively (Table 1). For this study, 19 health facilities in Greater Kisii, 17 in Bondo, 21 in Makueni and 24 in Kwale were randomly selected in which 463, 395, 388 and 422 paediatric patients were presented over the survey period, respectively (Tables 1 and 3).
Table 1.
Demographic and government health service characteristics in four districts of Kenya
| District | Demographics | Number and type of all GoK health facilities |
Number and type of GoK health facilities involved in the study |
|---|---|---|---|
| Greater Kisii | Area: 1310 km2 | Hospitals: 4 | 3 |
| Population: 952 725 | Health centres: 13 | 6 | |
| Percent urban: 6 | Dispensaries: 27 | 10 | |
| Percent rural: 94 Density: 727/km2 EAs: 1975 |
Total: 44 | 19 | |
| Bondo | Area: 960 km2 | Hospitals: 1 | 1 |
| Population: 238 780 | Health centres: 5 | 4 | |
| Percent urban: 8 | Dispensaries: 15 | 12 | |
| Percent rural: 92 Density: 249/km2 EAs: 673 |
Total: 21 | 17 | |
| Kwale | Area: 8295 km2 | Hospitals: 3 | 3 |
| Population: 496 133 | Health centres: 6 | 6 | |
| Percent urban: 11 | Dispensaries: 41 | 15 | |
| Percent rural: 89 Density: 60/km2 EAs: 822 |
Total: 50 | 24 | |
| Makueni | Area: 8266 km2 | Hospitals: 4 | 3 |
| Population: 771 545 | Health centres: 21 | 8 | |
| Percent urban: 3 | Dispensaries: 34 | 10 | |
| Percent rural: 97 Density: 93/km2 EAs: 1766 |
Total: 59 | 21 |
Table 3.
Number of paediatric patients who attended GoK health facilities during the study period and their patterns of use of health facilities for the treatment of fevers determined by distances travelled
| District | Number of patients interviewed |
Mean distance travelled to health facility (km) |
Percent patients using nearest facility |
Correlation between distance predicted and actual use of health facilities* |
||||
|---|---|---|---|---|---|---|---|---|
| Urban | Rural | Total | Urban | Rural | Overall | |||
| Greater Kisii | ||||||||
| Hospitals | 25 | 144 | 169 | 2.6 | 5.9 | 5.5 | 43 (72) | R2 = 0.879 |
| Health centres | 0 | 89 | 89 | – | 3.3 | 3.3 | 54 (48) | P ≤ 0.01 |
| Dispensaries | 3 | 202 | 205 | 5.4 | 2.7 | 2.8 | 67 (138) | |
| Total | 28 | 435 | 463 | 2.9 | 3.9 | 3.9 | 56 (258) | |
| Bondo | ||||||||
| Hospitals | 22 | 48 | 70 | 1.2 | 5.8 | 4.4 | 74 (52) | R2 = 0.706 |
| Health centres | 6 | 101 | 107 | 5.0 | 3.1 | 3.2 | 76 (81) | P ≤ 0.01 |
| Dispensaries | 6 | 212 | 218 | 4.3 | 2.7 | 2.7 | 89 (194) | |
| Total | 34 | 361 | 395 | 2.5 | 3.2 | 3.2 | 83 (327) | |
| Kwale | ||||||||
| Hospitals | 28 | 65 | 93 | 3.4 | 8.1 | 6.8 | 61 (57) | R2 = 0.996 |
| Health centres | 12 | 97 | 109 | 4.1 | 6.0 | 5.8 | 53 (58) | P ≤ 0.01 |
| Dispensaries | 15 | 205 | 220 | 1.2 | 4.9 | 4.7 | 79 (173) | |
| Total | 55 | 367 | 422 | 2.9 | 5.8 | 5.4 | 68 (288) | |
| Makueni | ||||||||
| Hospitals | 9 | 62 | 71 | 0.4 | 6.5 | 5.9 | 72 (44) | R2 = 0.927 |
| Health centres | 4 | 162 | 166 | 0.5 | 5.1 | 5.5 | 60 (100) | P ≤ 0.01 |
| Dispensaries | 0 | 151 | 151 | – | 4.9 | 4.9 | 78 (118) | |
| Total | 13 | 375 | 388 | 0.5 | 5.6 | 5.4 | 68 (262) | |
We performed a logarithmic transformation of percentage potential and actual use at similar distances and used a simple linear regression to test the correlation between potential use based on distances to nearest facility and actual use revealed in the survey.
The analysis of straight-line distances between communities and government health facilities revealed differences between districts with 99% of the population in Greater Kisii, 80% in Bondo, 65% in both Kwale and Makueni within 5 km of the nearest government health facility (Figure 1). The mean distance of access to health facilities was 2.4 km in Greater Kisii, 3.4 km in Bondo, 4.7 km in Kwale and 4.5 km in Makueni (Table 2). In addition, the overall distribution of population around health facilities peaked at 2 and 3 km (Table 2).
Table 2.
Populations theoretical overall mean straight-line distance access to all GoK health facilities in each of the four districts and coverage within the 5-km threshold
| Mean distance access (km) |
Percent population within 5 km of nearest facility |
Distance population around facilities peak (km) |
|||||
|---|---|---|---|---|---|---|---|
| District | Urban | Rural | Overall | Urban | Rural | Overall | Overall |
| Greater Kisii | 1.8 | 2.4 | 2.4 | 100 | 99 | 99 | 2 |
| Bondo | 1.4 | 3.5 | 3.4 | 100 | 78 | 80 | 2 |
| Kwale | 1.6 | 5.2 | 4.7 | 91 | 61 | 65 | 2 |
| Makueni | 1.6 | 4.6 | 4.5 | 85 | 63 | 65 | 3 |
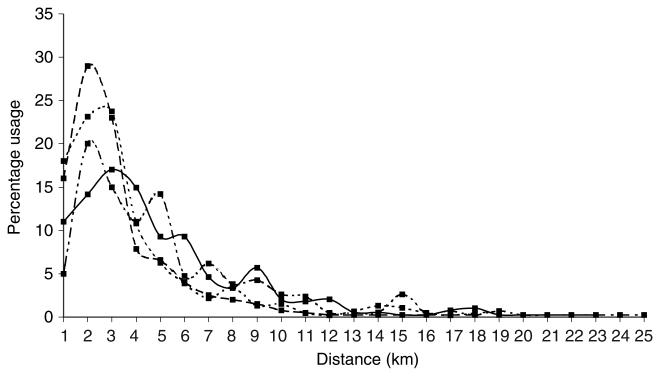
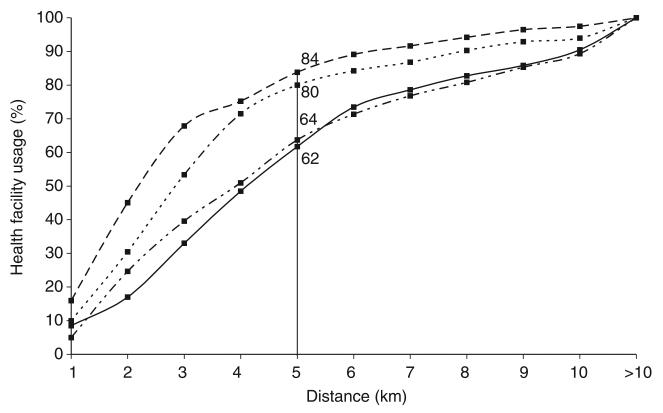
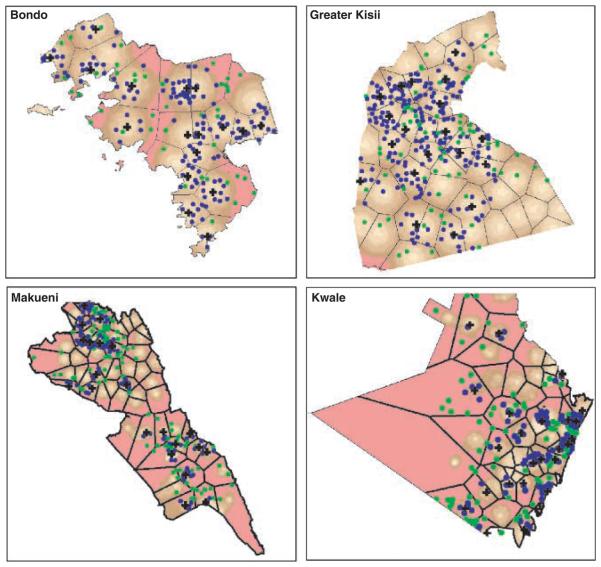
The usage patterns of services by febrile paediatric patients in the districts showed that 80% in Greater Kisii, 84% in Bondo, 64% in Kwale and 65% in Makueni used a government health facility at 5 km with the 5–6 km distance being the location of the point of inflection where the rate of change of usage slowed (Figure 2). There was a general reduction in number of patients using health facilities as distance from facilities increased, with major peaks at 2 or 3 km in the four districts (Figure 3). There was a marked disparity between the districts in terms of the overall mean travel distances to health services. Users in both Kwale and Makueni districts, whose populations had relatively poor access to government health services, travelled a mean distance of 5.4 km while those in Greater Kisii and Bondo travelled mean distances of 3.9 and 3.2 km, respectively. Overall, patients travelled greater distances to hospitals than to health centres and dispensaries (Table 3). Most patients, 56% in Greater Kisii, 68% in both Kwale and Makueni and 83% in Bondo, used the nearest government health facility. The overlay of actual users classified into those using a facility within or outside 5 km showed that most of those who used a facility at distances >5 km, came from areas where overall access was >5 km (Figure 4). Of the 68–205 patients who were 5 km from a health facility but used one at a greater distance, 65–74% of them in the four districts used an inpatient facility (hospital or health centre), mostly the nearest one.
Figure 2.
Cumulative health service use against distance travelled to government health facility where treatment was sought for the four districts. The line - -■- - represents Greater Kisii, – –■– – represents Bondo, – —■— – represents Kwale and —■— represents Makueni. The y-axis shows the cumulative percentage of patients in each district who travelled to a health facility at the distance (km) value shown on the x-axis. The cumulative percentages were computed by summing all patients who went in a district who used a facility at each distance on an 11-point scale (0–1, 1–2, 2–3, 3–4, 4–5, 5–6, 6–7, 7–8, 8–9, 9–10 and >10 km). Eighty-four per cent in Bondo and 80, 64 and 62 of patients in Greater Kisii, Kwale and Makueni used health facilities within 5 km, respectively.
Figure 3.
General decay in use of government health facilities as distance from health facilities increased. The line - -■- - represents Greater Kisii, – –■– – represents Bondo, – —■— – represents Kwale and —■— represents Makueni. The y-axis shows the percentage patients in each district who travelled to a health facility at the distance (km) value shown on the x-axis. The percentage use was based on a discrete number of patients in each district using government health facilities at each distance, from 0–25 km. The logarithmic relationship was worked out using a simple linear regression comparing logarithmically transformed percentage proportion of distance predicted users and actual users at each distance interval. The relationship was significant at 1% level for Bondo, Greater Kisii, Kwale and Makueni with respective R2 values of 0.706, 0.879, 0.996 and 0.927.
Figure 4.
District maps showing EAs, where patients came from, as represented by centroid of EA polygons, the health facilities they used and the underlying overall access to health services. The EAs have been classified into those where patients travelled ≤5 km (blue centroid point  ) and those >5 km (green centroid point
) and those >5 km (green centroid point  ). There was a close relationship between distance travelled by patients and the population's underlying access to GoK health facilities with varying shades of brown representing areas with access distances between <1–5 km and the red colour representing areas >5 km (
). There was a close relationship between distance travelled by patients and the population's underlying access to GoK health facilities with varying shades of brown representing areas with access distances between <1–5 km and the red colour representing areas >5 km ( <1,
<1,  1–2,
1–2,  2–3,
2–3,  3–4,
3–4,  4–5 and
4–5 and  >5 km). The figure also shows the facilities catchment areas
>5 km). The figure also shows the facilities catchment areas  and the position of the facilities [
and the position of the facilities [ ] used in the study for each district.
] used in the study for each district.
The statistical comparison of percentage potential use and percentage actual use on the 11-point distance scale showed a high correlation significant at the 1% level in all the districts (Table 3). In an optimal situation, where all users go to the nearest health facility, the correlation between the percentages of distance predicted potential users and that of actual users revealed in the survey would have a value of one. The statistical analysis revealed a coefficient of determination (R2) in Greater Kisii of 0.879; Bondo 0.706; Kwale 0.996 and Makueni 0.927.
Within all four districts, there were variations in theoretical access between communities, with urban populations generally having good distance access to health services compared with rural populations. Rural populations were 0.6–3.6 km further from the nearest health facility than their urban counterparts. In addition, in all the districts, except Greater Kisii where almost the entire population was within 5 km of a health facility, a greater proportion of the rural population was outside this threshold from GoK health services than urban populations. In Bondo, the entire urban population was within 5 km of a health facility compared with 78% of the rural population. In Kwale these were 97% urban and 61% rural and in Makueni 85% urban and 63% rural (Table 2). The analysis of actual use data revealed that rural populations in all four districts travelled an average 0.7–5.1 km more than urban populations to the health facilities they attended. There was a close relationship between use of health facilities for the treatment of fevers among urban and rural populations and their underlying access to health facilities. Of the patient population seen at the facilities, over 90% of the attendees were from rural areas (Table 3). Rural areas in these districts are home to over 85% of the population (Table 1).
Discussion
We used GIS to define the population's overall access to government health services and their use of these services for the treatment of paediatric fevers in Kenya through straight-line distance analysis. This disclosed marked disparities in theoretical access between districts and within districts, particularly urban and rural differences. The difference in access between urban and rural communities were larger in the relatively large, low population density districts of Kwale and Makueni than in the relatively high density, but small districts of Greater Kisii and Bondo. In both Kwale and Makueni, 35% of the population was more than 5 km from a government health facility. However, while there was greater disparity in access between urban and rural communities in Kwale than in Makueni, overall 15% of urban and 37% of rural population in Makueni were outside the 5-km threshold compared with 3% of urban and 39% of rural populations in Kwale. The results from the analysis of febrile patients attending government facilities show that rural populations on average travelled greater distances to health facilities than urban populations, the greatest difference being in Makueni at 5.1 km and the smallest in Bondo at 0.7 km.
The actual usage analysis of health facilities for the treatment of fevers also showed that 56% or more of the users in all districts attended the nearest government health facility. Further, the number of patients using a facility decreased as the distance from that facility increased. In all districts, however, use peaked at 2–3 km from health facilities corresponding to the peak in population distribution at this distance. A further possible influence on this trend is that the urban population has an increased ability to access private healthcare. In view of the 5-km threshold defined as a target in the health sector reform, over 60% of users in all the districts attended health facilities within this distance. There was a striking congruence between the theoretical proportion of the population having access to health facilities within 5 km, and the proportion of users attending them at this distance. In addition, Figure 2 shows that the 5–6 km distance is the point of inflection, where the rate of change in use slows and the gradient of the curve steadily changes. It appears, from a spatial perspective, that the appropriate access target lies between 5 and 6 km. Of the patients who did not attend the nearest health facility 65–74% used a more distant health centre or a hospital, indicating that there might be other non-distance factors, such as perceived quality of services, which determined the use of health facilities.
Malaria case management is a cornerstone of the Kenyan National Malaria Strategy and the international RBM movement. Case management will be operated at all levels of the health sector and by multiple government and non-government service providers. However, new drug policies, essential drug distribution, regulation and capacity development of health facilities are often limited initially to government service providers. As such our analysis has focused only on government health facilities. We recognize the importance of other sectors such as the informal shopkeepers, community-based health workers, the private clinical services and those provided by NGOs and missions and their interaction with government services in influencing choices of service use for treatment of paediatric fevers. Analysis of these other choices in fever management will be the subject of separate community-based surveys in each of the four districts described in this paper.
In this paper we have explored an important component of access to malaria case management services. The use of Thiessen techniques requires that two assumptions be made; that all clients will use the nearest health facility and that they will all travel along a straight line path. A number of studies have revealed differences in outcome between straight-line distance analysis and that based on actual transport network (Parker & Campbell 1998; Tanser 2000). Under a larger ongoing project aimed at establishing composite indicators of physical access to GoK health services in Kenya, high spatial resolution of population, health facilities, transport network, elevation, drainage, forests, parks and informal outlets that sell anti-malarials have been developed for all four districts. Using GIS, analysis of access to health services based on actual transport network, adjusted for the influence of elevation, drainage, other transport barriers and multiple provider choices will be defined.
The core and supplementary RBM indicators were established with the aim of making the monitoring and evaluation exercise simple and using the existing country mechanisms as far as possible for data collection. Equity in access to services is not considered. The analysis of physical access to and use of interventions and its impact on issues related to equity at the district level is an area that should be possible to capture easily. The potential of GIS/GPS technology in defining access and utilization of health services and its contribution to planning and resource allocation has been the subject of a wide variety of studies and has been found to be an important health research and decision making tool (Twigg 1990; Glass 1991; Andes & Davis 1995; Geertman & van Eck 1995; Division of Statistics, United Nations 1997; Parker & Campbell 1998; Hay et al. 2000; Robinson 2000; Rogers 2000; Tanser 2000). Much work has also focused on investigating environmental correlates of malaria admissions from health facility data with a view to understanding and ultimately predicting temporal variation (Hay et al. 1998, 2001). Detailed information on the distribution of the health facility catchment population for this work is often lacking. These results also provide important evidence that the appropriate area over which to define the catchment population is between 5 and 10 km capturing on average 70 and 90% of admissions in Kenya.
We have demonstrated that readily available combinations of spatial data on health service location and population can be used within GIS to define physical access and that this corresponds closely to actual usage of services for fevers. The implication is that detailed, facility-based surveys of usage may not be required to define populations who have limited access to clinical services and could be used within a more detailed analysis of equity of service provision to gauge performance. The access surfaces produced by interpolating distances to the nearest health facility at each EA classified the districts into areas of different access categories and provided simple but visually powerful tools that can be used for making decisions in resource allocation at the district level. Similar approaches might be applicable to design and analysis of the provision of insecticide-treated net services through social marketing, private sector approaches or through public health institutions.
Acknowledgements
This study received financial support from The Wellcome Trust, UK (no. 058922), the Roll Back Malaria Initiative, AFRO (AFRO/WHO/RBM # AF/ICP/CPC/400/XA/00) and the Kenya Medical Research Institute. The authors are grateful to Mr David Nalo, Head of the Central Bureau of Statistics for helping with the provision of census data and Dr Mike English and Prof. Peter Atkinson for comments on the analysis and manuscript. The authors are also grateful to Abdinasir Amin for his help in the repeat field visits, Priscilla Wairimu, Lydiah Mwangi and Lucy Muhunyo for assistance with data handling and linkage. DZ is grateful for support provided by Médicins Sans Frontière. SIH is a Research Career Development Wellcome Trust Fellow (no. 056642) and RWS a Senior Wellcome Trust Fellow (no. 058992). This paper is published with the permission of the director, KEMRI.
References
- Andes N, Davis JE. Linking public health data using geographic information system techniques: Alaskan community characteristics and infant mortality. Statistics and Medicine. 1995;14:481–490. doi: 10.1002/sim.4780140509. [DOI] [PubMed] [Google Scholar]
- Annis S. Physical access and utilisation of health services in rural Guatemala. Social Science and Medicine. 1981;15D:515–523. doi: 10.1016/0160-8002(81)90046-0. [DOI] [PubMed] [Google Scholar]
- Central Bureau of Statistics . 1999 Population and Housing Census: Counting Our People for Development: Population Distribution by Administrative Areas and Urban Centres. Vol. 1. Central Bureau of Statistics, Ministry of Finance & Planning; GoK, Nairobi: 2001. pp. 1–411. [Google Scholar]
- Division of Statistics, United Nations . Accessibility Indicators in GIS. UN Department for Economic and Social Information and Policy Analysis; New York: 1997. pp. 1–24. [Google Scholar]
- Fiedler JL. A review of literature on access and utilisation of medical care with emphasis on rural primary care. Social Science and Medicine. 1981;15:129–142. doi: 10.1016/0160-7995(81)90028-9. [DOI] [PubMed] [Google Scholar]
- Garner P, Giddings P. Rural health centre use: variations with distance and disease. Papua New Guinea Medical Journal. 1985;30:105–108. [PubMed] [Google Scholar]
- Geertman SCM, van Eck JRR. GIS and models of accessibility potential: an application in planning. International Journal of Geographical Information Systems. 1995;9:67–80. [Google Scholar]
- Glass D. A World Health Organization pilot study involving environment, public health and GIS. Mapping Awareness and GIS in Europe. 1991;6:36–40. [Google Scholar]
- Habib OS, Vaughan JP. The determinants of health services utilisation in southern Iraq: a household interview survey. International Journal of Epidemiology. 1986;15:325–403. doi: 10.1093/ije/15.3.395. [DOI] [PubMed] [Google Scholar]
- Haddad S, Fournier P, Machouf N, et al. What does quality mean to lay people? Community perception of primary health care services in Guinea. Social Science and Medicine. 1998;47:381–394. doi: 10.1016/s0277-9536(98)00075-6. [DOI] [PubMed] [Google Scholar]
- Hay SI, Snow RW, Roger DL. Predicting malaria seasons in Kenya using multitemporal meteorological satellite sensor data. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1998;92:12–20. doi: 10.1016/s0035-9203(98)90936-1. [DOI] [PubMed] [Google Scholar]
- Hay SI, Omumbo JA, Criag MH, et al. Earth observation, geographic information systems and Plasmodium falciparum malaria in sub-Saharan Africa. Advances in Parasitology. 2000;47:174–206. doi: 10.1016/s0065-308x(00)47009-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay SI, Rogers DJ, Shanks GD, et al. Malaria early warning in Kenya. Trends in Parasitology. 2001;17:95–99. doi: 10.1016/s1471-4922(00)01763-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SM, Kearns RA, Moran W. Spatial patterns of attendance at general practitioner services. Social Science and Medicine. 1990;31:773–781. doi: 10.1016/0277-9536(90)90172-o. [DOI] [PubMed] [Google Scholar]
- Igun UA. Stages in health-seeking: a descriptive model. Social Science and Medicine. 1979;13A:445–456. [PubMed] [Google Scholar]
- Ingram DR, Clarke DR, Murdie RA. Distance and the decision to visit the accident and emergency department. Social Science and Medicine. 1978;12:55–62. [PubMed] [Google Scholar]
- Makinen M, Waters H, Rauch M, et al. Inequalities in health care use and expenditures: empirical data from eight developing countries and countries in transition. Bulletin of World Health Organisation. 2000;78:55–65. [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health . Health Policy Framework. Ministry of 5 Health, Government of Kenya; Nairobi: 1997. [Google Scholar]
- Muller I, Smith T, Mellor S, et al. The effects of distance from home on attendance at a small health centre in rural Papua New Guinea. International Journal of Epidemiology. 1998;27:878–884. doi: 10.1093/ije/27.5.878. [DOI] [PubMed] [Google Scholar]
- Nabarro DN, Tayler E. The “Roll Back Malaria” campaign. Science. 1998;280:2067–2068. doi: 10.1126/science.280.5372.2067. [DOI] [PubMed] [Google Scholar]
- Parker EB, Campbell JL. Measuring access to primary medical care: some examples of the use of geographical information systems. Health and Place. 1998;4:183–193. doi: 10.1016/s1353-8292(98)00010-0. [DOI] [PubMed] [Google Scholar]
- Phillips DR. Spatial variations in attendance at general practitioner services. Social Science and Medicine. 1979;13:169–181. doi: 10.1016/0160-8002(79)90004-2. [DOI] [PubMed] [Google Scholar]
- Robinson TP. Spatial statistics and geographical information systems in epidemiology and public health. Advances in Parasitology. 2000;47:82–120. doi: 10.1016/s0065-308x(00)47007-7. [DOI] [PubMed] [Google Scholar]
- Rogers DJ. Satellites, space, time and the African trypanosomiasis. Advances in Parasitology. 2000;47:130–165. doi: 10.1016/s0065-308x(00)47008-9. [DOI] [PubMed] [Google Scholar]
- Roll Back Malaria/World Health Organisation . Framework for Monitoring Progress and Evaluating Outcomes and Impact. Geneva, Switzerland: 2000. WHO/CDS/RBM/2000.25. [Google Scholar]
- Stock R. Distance and the utilisation of health facilities in rural Nigeria. Social Science and Medicine. 1983;17:563–570. doi: 10.1016/0277-9536(83)90298-8. [DOI] [PubMed] [Google Scholar]
- Tanser FC. The application of geographical information systems to infectious diseases and health systems in Africa. Faculty of Medicine, University of Natal; Durban, South Africa: 2000. PhD Thesis. [Google Scholar]
- Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Social Science and Medicine. 1994;38:1091–1110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- Twigg L. Health based geographical information systems: their potential in the light of existing data sources. Social Science and Medicine. 1990;30:143–155. doi: 10.1016/0277-9536(90)90337-r. [DOI] [PubMed] [Google Scholar]
- Vandervoort D. ProxSpid.ave. 1999 http://www.esri.com/arcscripts. [Google Scholar]
- WHO . Investing in Health Research and Development: A Report of the adhoc Committee in Health Research Relating to Future Intervention Options. World Health Organization; Geneva: 1996. p. 278. [Google Scholar]
- WHO . World Health Report: Making a difference. World Health Organization; Geneva: 1999. p. 122. [Google Scholar]
- WHO . World Health Report: Health Systems: Improving Performance. World Health Organization; Geneva: 2000. p. 206. [Google Scholar]
- Zurovac D, Midia B, Ochola SA, et al. The Evaluation of Malaria Case Management of Sick Children Presenting in Out-patient Departments in Government Health Facilities in Kenya. Report submitted to the Division of Malaria Control, Ministry of Health, Government of Kenya; 2002. [Google Scholar]