Abstract
This study aimed to determine the psychosocial factors associated with delayed test-seeking among tuberculosis patients. The duration of symptoms before seeking medical care was assessed by interview for 108 newly diagnosed pulmonary tuberculosis patients in the city of Iquitos in the Peruvian Amazon, which has high tuberculosis incidence. Beliefs associated with test-seeking behavior and delay was assessed in these patients. The median delay from symptom onset to seeking diagnostic testing was 61 days (inter-quartile range 30–91 days). The belief that tuberculosis is curable was associated with a 100% longer test-seeking delay; the perception that tuberculosis was common was associated with a 57% longer delay; male gender was associated with a 48% longer delay; and education less than complete secondary schooling was associated with a 44% longer delay. In conclusion, current health promotion activities that emphasize tuberculosis curability and high prevalence may paradoxically increase test-seeking delay and therefore require prospective evaluation.
INTRODUCTION
Tuberculosis is a serious global public health problem. Peru has high tuberculosis incidence 1 despite a model control program. 2,3 Research in Peru has shown low levels of tuberculosis-related knowledge and considerable delays in diagnosis.4 These patterns contribute to tuberculosis-related morbidity and mortality 5 and growing drug resistance.6
Early detection and treatment of tuberculosis is critical to controlling the disease. 7 Delay before test-seeking can result in more serious illness by the time of diagnosis 8 and increased tuberculosis transmission within the community. 9 The implementation of directly observed treatment shortcourse (DOTS) has been associated with improvements in treatment completion and outcomes. 10 However, only 61% of cases worldwide and 70% of cases in Peru were estimated by the World Health Organization (WHO) to have been detected in 2006. 1 Unless tuberculosis cases are identified and treated earlier and in greater numbers, tuberculosis-related morbidity, mortality, and drug resistance may be expected to increase.
Analysis of the factors delaying tuberculosis diagnosis may help tuberculosis control programs to diagnose and treat patients more effectively. 11-14 Studies suggest that psychosocial and cultural-based factors are dominant forces in test-seeking behavior both in general and specifically related to tuberculosis. 11,15-18 Individuals' understanding of the cause and nature of the disease and their perceptions of the personal, social, and economic barriers against tuberculosis diagnosis and treatment affect their likelihood of seeking testing. 19-21 The strong impact of psychosocial and cultural factors delaying tuberculosis diagnosis are well-recognized in many countries, but there have been few studies in Latin America.22
The objective of this study was to determine the psychosocial factors associated with delayed test-seeking behavior among tuberculosis patients in a city in the Peruvian Amazon.
MATERIALS AND METHODS
Study setting
This study was conducted in Iquitos in the region of Loreto, which covers more than a quarter of the Peruvian national territory. This area spans almost 4,000 km 2 of Amazonian jungle and shares borders with Brazil, Colombia, and Ecuador. Loreto has among the poorest socio-economic conditions in the country, with 41% of people living in extreme poverty, and a further 25% living in moderate poverty with associated deficiencies in other social indicators. 4,23 Iquitos is the largest city in the Peruvian Amazon, with a population of 337,000. The city has a diagnosed tuberculosis disease incidence of 106 per 100,000 people 5 and most healthy adults have evidence of latent tuberculosis infection.24
Study population
All of the patients (N = 108) 14 years of age or older who were diagnosed with pulmonary tuberculosis and began treatment with the national tuberculosis control program in the recruitment area over a 4-month period chose to provide informed written consent and were recruited to this project. The recruitment area included treatment clinics at the Hospital de Apoyo in the center of Iquitos, health posts in the urban shantytown of Belen, and the peri-urban city districts of San Antonio and San Juan. This study received ethical approval from Asociación Benéfica PRISMA, a non-governmental organization that carries out biomedical research in Lima, Peru and Imperial College in London, UK.
Study design
A cross-sectional, quantitative survey was used to explore the impact of psychosocial and cultural-based factors on delay in test-seeking behavior for symptoms caused by tuberculosis. The original survey instruments were piloted with 25 patients and then modified based on participants' responses and feedback. The final survey instruments were carried out as face-to-face interviews (by Carolyn Ford). Patients were interviewed at the health facility or in their homes, according to their preference.
Measures
Delay in tuberculosis test-seeking was defined as the interval between when the respondent first noted tuberculosis symptoms, and the date of the clinic visit that led to tuberculosis diagnosis. Tuberculosis testing and care is free in Peru and the national control program guidelines recommend that patients seek testing for tuberculosis if they have symptoms suggestive of this disease for 14 days or more. Subsequent health service delay, from when the patient made the clinic visit until laboratory confirmed diagnosis, was not considered in this study because it is the subject of separate research and was generally brief in comparison to test-seeking delay (data not shown). Factors that may be associated with delayed test-seeking behavior were considered in five thematic groups:
Socio-demographic factors were gender, age, educational level (grade of schooling completed), number of household residents, crowding (number of persons per room in the household), and socio-economic level assessed with spending and ownership indices. The spending index was comprised of the sum of six yes/no questions about the household's spending practices during the last month. Four of the items: spending on extra household items (household repairs, artifacts, vehicles); spending on recreational activities outside of the household; spending on clothing/shoes; and payment of all utilities (electricity, water), received a score of one for “yes” responses and zero for “no” responses. Two of the items, selling or pawning artifacts or furniture or requesting a loan to purchase food, were reverse scored. The ownership index was comprised of the sum of four yes/no questions and one multiple-response question about the households' ownership of different items. Four of the items (ownership of a television, radio, refrigerator, and poultry) were scored one for “yes” responses and zero for “no” responses. Mode of transportation received a zero score for no independent transportation, one for a bicycle, and two for motorized transport. Spending and ownership indices ranged from 0 to 6 and were analyzed as dichotomous variables greater or less than the median values.
Factors related to patients' perceptions were tuberculosis severity and contagiousness (both scored 1–10) and whether patients perceived that tuberculosis was common in their community (yes/no).
Factors related to patients' actual risk of tuberculosis were whether someone in the patient's household or someone that the patient knew had a history of tuberculosis.
Stigma-related factors were whether patients would try to distance themselves from someone with tuberculosis or would feel embarrassed if a family member had tuberculosis.
Access to health services was assessed as the amount of time the patient required to reach the nearest health service facility by the transport method that they usually used (generally walking).
Statistical analyses
Statistical analyses were performed using STATA (version 10.0, STATA Corp., College Station, TX). Categoric data are shown as % (number) when data are available for all participants and as % (number/sample size) when data are only available for a subset of the study population. Normally distributed data are expressed as mean (SD) and non-Gaussian data are expressed as a median (inter-quartile range [IQR]). Univariate and multiple linear regression analyses (see results) were carried out on the natural log of the dependent variable (test-seeking delay) to transform it into a Gaussian distribution. The coefficients of the predictor variables were then multiplied by 100 to determine the percent increase in each independent variable, holding all other factors constant. 25 All P values were two-sided and a P value of < 0.05 was considered to be statistically significant.
RESULTS
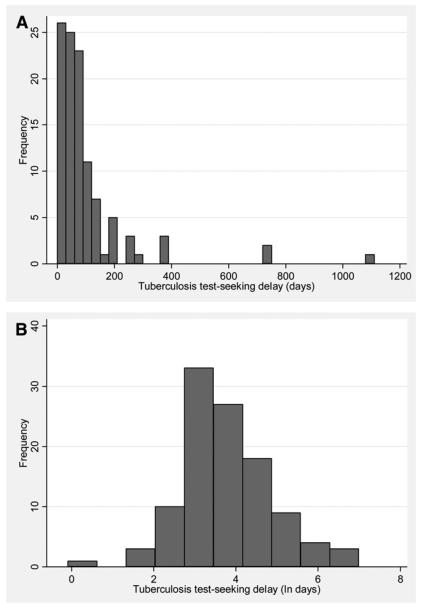
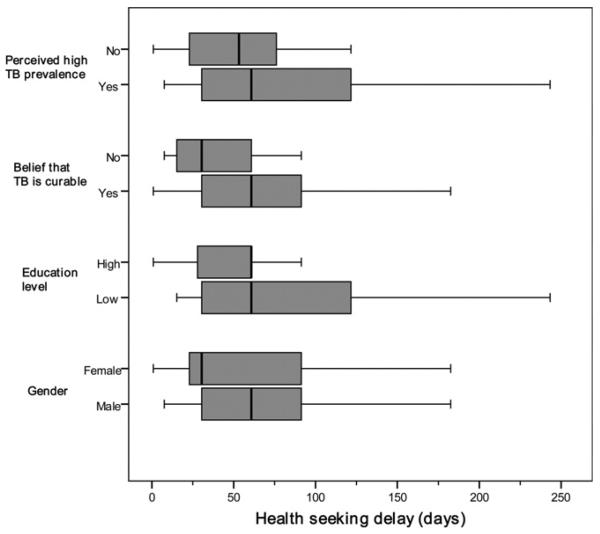
Table 1 and Table 2 present univariate and multiple regression analysis, respectively, of the patient characteristics of interest and their association with test-seeking delay. Figure 1 indicates the distribution of test-seeking delay in patients and Figure 2 illustrates the associations between patient characteristics and test-seeking delay.
Table 1.
Patient factors and their unadjusted association with test-seeking delay*
| Univariate regression of patient delay in test-seeking behavior† |
|||
|---|---|---|---|
| Factor | Tuberculosis patients (N = 108) | Coefficient | P value |
| Socio-demographic factors | |||
| Female gender; % (number) | 40% (43) | 0.27 | 0.2 |
| Age; median years (IQR) | 33 (IQR 21–46) | 0.012 | 0.047 |
| Education less than completion of secondary schooling; % (number) | 57% (62) | 0.33 | 0.1 |
| Household spending index (low, scored 0–3); % (number) | 59% (64) | −0.0080 | 0.9 |
| Household ownership index (low, 0–2 items); % (number) | 65% (63/97) | 0.11 | 0.1 |
| Number of household residents; mean (SD) | 7.3 ± 3.5 | −0.029 | 0.3 |
| Crowding (no. of people per room); mean (SD) | 2.7 ± 2.4 | 0.0020 | 1.0 |
| Perceived risk factors | |||
| Belief that TB is curable (yes response); % (number) | 92% (99) | 0.64 | 0.08 |
| Perceived severity (1–10 scale); mean (SD) | 6.5 ± 2.2 | 0.0070 | 0.9 |
| Perceived contagious. (1–10 scale); mean (SD) | 7.1 ± 2.3 | 0.013 | 0.8 |
| Perceived high prevalence of TB in local community; % (number) | 41% (42/102) | 0.46 | 0.03 |
| Actual risk factors | |||
| History of household cohabitant with TB; % (number) | 39% (42/107) | −0.049 | 0.8 |
| History of known contact with TB; % (number) | 63% (67/106) | 0.49 | 0.02 |
| Stigma-related factors | |||
| Would avoid neighbor with TB; % (number) | 68% (71/105) | 0.020 | 0.9 |
| Would be embarrassed by TB in family member; % (number) | 40% (43/107) | −0.053 | 0.8 |
| Access to health services | |||
| Time to travel to closest health service; median minutes (IQR) | 15 (IQR 6.0–22) | −0.000060 | 1.0 |
TB = tuberculosis; IQR = inter-quartile range; SD = standard deviation.
The dependent variable was the natural logarithm of the days delay in test-seeking for tuberculosis symptoms.
Table 2.
Patient factors and their adjusted association with test-seeking delay*
| Multiple regression of patient delay in test-seeking behavior† |
||
|---|---|---|
| Factor | Coefficient | P value |
| Belief that TB is curable | 1.002 | 0.01 |
| Perceived high prevalence of TB in the local community | 0.57 | < 0.01 |
| Male gender | 0.48 | 0.02 |
| Education less than complete secondary schooling | 0.44 | 0.03 |
| History of known contact with TB anywhere | – | – |
| Household ownership index | – | – |
| Age (in years) | – | – |
TB = tuberculosis.
The dependent variable was the natural logarithm of the days delay in test-seeking for tuberculosis symptoms.
This table features the same patients as Table 1 and all variables with P ≤ 0.2 in Table 1 are shown in Table 2 and were included in the initial multiple linear regression model. Non-significant variables were then removed from the model in turn (indicated by “–”) according to the log-likelihood test until only the significant associations remained in the final model, in Table 2.
Figure 1.
Delay in test-seeking behavior for tuberculosis symptoms in tuberculosis patients (N = 108). A, Number of days between tuberculosis symptom onset and test-seeking behavior. Each bar represents one month. B, The natural logarithm (ln, loge) of the number of days between tuberculosis symptom onset and test-seeking behavior.
Figure 2.
Association between days of test-seeking delay and patient factors. (The educational level was classified as low for patients who had failed to commence or complete secondary schooling and high for those who completed secondary schooling.)
Socio-demographic results
Table 1 shows the participant characteristics and their association with test-seeking delay in univariate regression analysis. There was no more than one patient per participating household. A total of 60% (65) of the participants were male, the median age was 33 years (IQR 21–46) and 9.3% (10) of the participants had post-secondary education.
Delay in patient test-seeking behavior
The median delay in test-seeking behavior was 61 days (IQR 30-91) and the mean was 95 days (SD 151, Figure 1). The distribution of test-seeking delay was skewed (Figure 1A) and the natural logarithm of the test-seeking delay had an approximately Gaussian distribution (Figure 1B). Only a quarter of patients sought testing within 1 month (30 days) of symptom onset; half of the patients in more than 2 months (61 days), and three-quarters of patients within 3 months (91 days). Other patients waited longer between symptom identification and their initial visit to a health post or hospital: 22% (24) waited 4–6 months, 4% (4) waited 7–9 months, and the remaining 6% (6) said that they had waited 1–3 years.
Reasons that patients initiated test-seeking behavior
The principal reason that patients gave for having initiated the clinical visit that led to tuberculosis diagnosis was having been sick for a long time (identified by 23% [25/107] of patients interviewed). Others described the onset of specific symptoms as the reasons for seeking care: 17% (18/107) because they began to cough blood, 14% (15/107) developed fever, and 25% (27/107) had other symptoms including, “feeling sick in general,” having head or body aches, and experiencing weight loss and coughing. Another 15% (16/107) stated that they sought services because of advice from family members. The remaining 6% (6/107) had mistakenly attributed their tuberculosis-related symptoms to being caused by other diseases, including malaria and dengue, and had accessed the health-care system in search of testing for diseases other than tuberculosis.
Reasons for delayed test-seeking behavior
When asked to state the principal reason why they had not sought services earlier in the course of their illness, 29% (31) of patients said they had attributed their symptoms to another illness; 21% (23) responded it was because of responsibilities such as work, child care, or studies; 20% (22) stated they were already taking medications or home remedies for these symptoms and had awaited a response to these treatments; 10% (11) felt they had not been sick enough to justify tuberculosis testing; 9% (10) said they did not have enough money to pay for medical care, implying that they had been unaware that tuberculosis testing and treatment is free in Peru; 6% (6) said they did not want to go to the health care establishment; and the remaining 5% (5) had thought that the problem would go away on its own.
Univariate analysis of factors associated with delayed test-seeking behavior
Table 1 shows the univariate linear regression analysis of factors associated with the delay in test-seeking for tuberculosis symptoms. Longer test-seeking delay was significantly associated with a history of known contact with TB in any location including the patient's household (P = 0.02), with a belief that tuberculosis had high prevalence in the local community (P = 0.03) and with increased age (P = 0.047). Longer test-seeking delay also tended to be associated with the belief that tuberculosis is curable (P = 0.08), less schooling (P = 0.1), poverty (assessed by ownership index, P = 0.1), and male gender (P = 0.2). On direct questioning, 92% (99/108) of patients believed tuberculosis to be curable and 41% (42/102) perceived there to be a high prevalence of tuberculosis in the community (Table 1).
Multiple regression analysis of factors associated with delayed test-seeking behavior
The statistically significant associations and non-significant trend associations between test-seeking delay and patient characteristics (P ≤ 0.2) were included in a multiple linear regression analysis. Non-significant associations were then removed from the model in turn according to the log-likelihood test until only the contributory associations remained in the final model that is shown in Table 2, in which the coefficients represent the independent association of each variable with test-seeking delay, holding all other factors constant. Factors independently significantly associated with test-seeking delay in the multiple linear regression analysis were: the belief that tuberculosis is curable was associated with a 100% longer test-seeking delay; the perception that tuberculosis was common in the patient's local community was associated with a 57% longer test-seeking delay; male gender was associated with a 48% longer test-seeking delay; and education less than completion of secondary schooling was associated with a 44% longer test-seeking delay. Figure 2 shows the association between the actual days of test-seeking delay and each of these independently associated factors.
DISCUSSION
Early detection and treatment of tuberculosis is critical to controlling the disease. 7,26 However, most patients in the current study waited until their symptoms had persisted for more than 2 months before they sought medical care. This delay in test-seeking behavior is likely to have increased their risk of morbidity, mortality, and tuberculosis transmission to contacts. Understanding delayed test-seeking behavior is important for designing tuberculosis case-finding and health promotion activities to improve community health. 11-14 This study also revealed unexpected associations between the considerable delay in test-seeking behavior and beliefs promoted by health-education campaigns. These paradoxical findings have important implications for re-evaluating tuberculosis case-finding health promotion.
A surprising finding in the current research was that delay in test-seeking was more prolonged in patients who believed that tuberculosis was common and curable. This finding is noteworthy because health promotion campaigns in documents, radio, and television organized by the tuberculosis control program in Peru and elsewhere promote the message that tuberculosis is common and curable, probably in an attempt to reduce stigma. It seems paradoxical that the beliefs that tuberculosis is common and curable were strongly associated with prolonged delay in seeking tuberculosis testing and this finding raises the possibility that some tuberculosis health promotion efforts could have unexpected adverse effects if they reduce the perceived importance attributed to tuberculosis symptoms and tuberculosis severity.
Tuberculosis patients who had lived with another tuberculosis patient and who would therefore be expected to be knowledgeable about tuberculosis symptoms, diagnosis, and treatment also had more prolonged test-seeking delay in the univariate regression analysis. This counter-intuitive finding of greater test-seeking delay in those with prior experience of the disease is concordant with our larger but not yet published analysis in peri-urban shanty-towns, which confirms this association in univariate and multiple regression analysis (personal observation, CAE). This has prompted us to focus our ongoing research on reducing test-seeking delay in household tuberculosis contacts because this group appears to be at high risk of both secondary tuberculosis and prolonged test-seeking delay. 4
Another factor associated with delayed test-seeking behavior for tuberculosis in the current study was a lower educational level, consistent with findings in Zambia. 27 Tuberculosis detection efforts therefore need to be focused on people who are illiterate or have only primary or incomplete secondary education, ensuring that educational materials are adapted to their level of education and literacy and are culturally appropriate. Populations with lower levels of education may also live and work in settings that put them at higher risk of tuberculosis, for example crowding, poor ventilation, poor nutrition, and slum dwellings. In summary, individuals with fewer years of formal education were most in need of health promotion to raise awareness of tuberculosis risk and facilitate tuberculosis test-seeking behavior.
Although tuberculosis-associated stigma was not associated with test-seeking delay in the current study, the prevalence of stigmatizing beliefs related to tuberculosis was strikingly high, as reported in other developing countries. 16,19,28 Stigma is linked to concealment of symptoms, treatment default, isolation from support networks, and decreased self-esteem, self-perception, and self-care. 29 Health education should aim to reduce tuberculosis-related stigma, although the current research did not provide evidence that this would reduce test-seeking delay.
Male gender was associated with delayed test-seeking behavior for tuberculosis symptoms. Although one study in South India also found a longer diagnostic delay among men, 30 several studies in other developing countries reported longer diagnostic delay in women. 27, 31 Tuberculosis-related health promotion in Peru often focuses on women and this finding emphasizes the importance of encouraging men to seek tuberculosis testing and ensuring that health services are “male-friendly.” Further research should explore the reasons why men in this setting delayed their care-seeking. For example, studies in other settings found that the main barrier for diagnosis among men was fear of the costs of diagnosis and treatment, 28,32,33 although in Peru tuberculosis testing and treatment are free from direct costs. In this study, several patients commented that males may delay seeking medical attention because it may be seen as a sign of weakness in the “macho” Latin culture. In addition, many men in Loreto work on the river or in the forest, causing them to be absent from home for prolonged periods, potentially delaying male test-seeking behavior, as reported by more than a fifth of the patients in the current study. Traditional healer consultations may be associated with prolonged diagnostic delay in some settings 27,31,34 but our previous research did not support this hypothesis elsewhere in Peru. 35
Socio-economic measures indicated considerable poverty in tuberculosis patients, which is consistent with the well-known geographic and temporal association between tuberculosis and poverty. 7 In this setting, reliable information on household income was difficult to determine because salaried employment was infrequent. The spending index assessed recent expenditure that may be rapidly affected by fluctuations in household income. In contrast, the ownership of assets index was used to provide a more stable socio-economic assessment because asset indices are constructed from variables that describe household ownership of durable goods and therefore capture a dimension of economic status that is stable in the mediumto long-term. 30 A limitation of the present research was that socio-economic assessment of patients was only done after tuberculosis disease had developed and had potentially already caused lost work, stigmatization, and tuberculosis- related costs. Nonetheless, ownership-based poverty assessment is less influenced by recent socio-economic challenges than expenditure-based socio-economic scores 36 and the ownership-based socioeconomic indicators may therefore be considered to be evidence of poverty prior to the tuberculosis disease in this study.
A general criticism of cross-sectional studies of this kind is their inability to show with certainty a causative link between factors studied and the outcome of interest, and it is possible that recall bias may have affected our findings. Strengths of the current study include the participation of all consecutively diagnosed patients, without selection bias, and the adjustment for interactions and potentially confounding factors with a multiple regression analysis.
In conclusion, this study provides insight into the factors associated with delayed tuberculosis test-seeking and has implications for control initiatives. Delayed test-seeking considerably delayed diagnosis and treatment of most tuberculosis patients. Limited education and poverty were associated with delayed test-seeking, emphasizing the need for health promotion in impoverished and marginalized groups, including interventions specifically aimed at illiterate and poorly educated people. Our finding that men had significantly more delayed test-seeking contrasts with the current health promotion emphasis on women and implies a need for additional prevention efforts targeted at males. Most importantly, current health promotion activities aiming to encourage tuberculosis test-seeking emphasize the curability and high prevalence of this disease. However, in the current research both of these beliefs were associated with delayed test-seeking. Thus, the intuitively appealing public health messages that tuberculosis is common and curable may have paradoxical adverse effects and health promotion interventions require prospective evaluation in controlled trials to ensure their efficacy.
Acknowledgments
Financial support: This research was funded by the charity Innovation For Health And Development (IFHAD), The Wellcome Trust, and the Department For International Development of the British Government (DFID). CF was funded by Voluntary Services Overseas.
REFERENCES
- 1.World Health Organization . WHO report 2008. World Health Organization; Geneva: 2008. Global tuberculosis control: surveillance, planning, financing. [Google Scholar]
- 2.Suarez PG, Watt CJ, Alarcon E, Portocarrero J, Zavala D, Canales R, Luelmo F, Espinal MA, Dye C. The dynamics of tuberculosis in response to 10 years of intensive control effort in Peru. J Infect Dis. 2001;184:473–478. doi: 10.1086/322777. [DOI] [PubMed] [Google Scholar]
- 3.Pelly T, Moore DA, Gilman R, Evans C. Recent tuberculo sis advances in Latin America. Curr Opin Infect Dis. 2004;17:397–403. doi: 10.1097/00001432-200410000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baldwin MR, Yori PP, Ford C, Moore DA, Gilman RH, Vidal C, Ticona E, Evans CA. Tuberculosis and nutrition: disease perceptions and health seeking behavior of household contacts in the Peruvian Amazon. Int J Tuberc Lung Dis. 2004;8:1484–1491. [PMC free article] [PubMed] [Google Scholar]
- 5.Ministerio de Salud Programa Nacional de Control de la Tuberculosis . Tuberculosis en el Perú: Informe 2000. Lima, Peru: 2001. [Google Scholar]
- 6.Campos PE, Suarez PG, Sanchez J, Zavala D, Arevalo J, Ticona E, Nolan CM, Hooton TM, Holmes KK. Multidrug-resistant Mycobacterium tuberculosis in HIV-infected persons, Peru. Emerg Infect Dis. 2003;9:1571–1578. doi: 10.3201/eid0912.020731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization Global tuberculosis control sur- veillance, planning, financing. WHO report 2003. 2003 [Google Scholar]
- 8.Gibson N, Boillot F, Jalloh H. The cost of tuberculosis to patients in Sierra Leone's war zone. Int J Tuberc Lung Dis. 1998;2:726–731. [PubMed] [Google Scholar]
- 9.Styblo K. Epidemiology of TB. Royal Netherlands Tuberculosis Association; The Hague: 1991. [Google Scholar]
- 10.Bayer R, Wilkinson D. Directly observed therapy for tuberculosis: history of an idea. Lancet. 1995;345:1545–1548. doi: 10.1016/s0140-6736(95)91090-5. [DOI] [PubMed] [Google Scholar]
- 11.Barnhoorn F, Adriaanse H. In search of factors responsible for noncompliance among tuberculosis patients in Wardha District, India. Soc Sci Med. 1992;34:291–306. doi: 10.1016/0277-9536(92)90271-q. [DOI] [PubMed] [Google Scholar]
- 12.Farmer P, Robin S, Ramilus SL, Kim JY. Tuberculosis, poverty, and “compliance”: lessons from rural Haiti. Semin Respir Infect. 1991;6:254–260. [PubMed] [Google Scholar]
- 13.Rubel AJ, Garro LC. Social and cultural factors in the successful control of tuberculosis. Public Health Rep. 1992;107:626–636. [PMC free article] [PubMed] [Google Scholar]
- 14.Wilkinson D. High-compliance tuberculosis treatment programme in a rural community. Lancet. 1994;343:647–648. doi: 10.1016/s0140-6736(94)92640-9. [DOI] [PubMed] [Google Scholar]
- 15.Jaramillo E. Pulmonary tuberculosis and health-seeking behaviour: how to get a delayed diagnosis in Cali, Colombia. Trop Med Int Health. 1998;3:138–144. doi: 10.1046/j.1365-3156.1998.00202.x. [DOI] [PubMed] [Google Scholar]
- 16.Liefooghe R, Baliddawa JB, Kipruto EM, Vermeire C, De Munynck AO. From their own perspective. A Kenyan community's perception of tuberculosis. Trop Med Int Health. 1997;2:809–821. doi: 10.1046/j.1365-3156.1997.d01-380.x. [DOI] [PubMed] [Google Scholar]
- 17.Mata JI. Integrating the client's perspective in planning a tuberculosis education and treatment program in Honduras. Med Anthropol. 1985;9:57–64. doi: 10.1080/01459740.1985.9965918. [DOI] [PubMed] [Google Scholar]
- 18.Sumartojo E. When tuberculosis treatment fails. A social behavioral account of patient adherence. Am Rev Respir Dis. 1993;147:1311–1320. doi: 10.1164/ajrccm/147.5.1311. [DOI] [PubMed] [Google Scholar]
- 19.Alvarez-Gordillo GC, Alvarez-Gordillo JF, Dorantes-Jimenez JE, Halperin-Frisch D. Perceptions and practices related with tuberculosis and treatment compliance in Chiapas, Mexico. Salud Publica Mex. 2000;42:520–528. [PubMed] [Google Scholar]
- 20.Kelly P. Isolation and stigma: the experience of patients with active tuberculosis. J Community Health Nurs. 1999;16:233–241. doi: 10.1207/S15327655JCHN1604_3. [DOI] [PubMed] [Google Scholar]
- 21.Liam CK, Lim KH, Wong CM, Tang BG. Attitudes and knowledge of newly diagnosed tuberculosis patients regarding the disease, and factors affecting treatment compliance. Int J Tuberc Lung Dis. 1999;3:300–309. [PubMed] [Google Scholar]
- 22.Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health. 2008;8:15. doi: 10.1186/1471-2458-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Banco Central de Reserva del Peru Informe. 2004 [Google Scholar]
- 24.Pelly TF, Santillan CF, Gilman RH, Cabrera LZ, Garcia E, Vidal C, Zimic MJ, Moore DA, Evans CA. Tuberculosis skin testing, anergy and protein malnutrition in Peru. Int J Tuberc Lung Dis. 2005;9:977–984. [PMC free article] [PubMed] [Google Scholar]
- 25.Wooldridge JM. Introductory Econometrics: A Modern Approach. Third edition South-Western College Publication; Mason, OH: 2006. [Google Scholar]
- 26.Kawai V, Soto G, Gilman RH, Bautista CT, Caviedes L, Huaroto L, Ticona E, Ortiz J, Tovar M, Chavez V, Rodriguez R, Escombe AR, Evans CA. Tuberculosis mortality, drug resistance, and infectiousness in patients with and without HIV infection in Peru. Am J Trop Med Hyg. 2006;75:1027–1033. [PMC free article] [PubMed] [Google Scholar]
- 27.Needham DM, Foster SD, Tomlinson G, Godfrey-Faussett P. Socio-economic, gender and health services factors affecting diagnostic delay for tuberculosis patients in urban Zambia. Trop Med Int Health. 2001;6:256–259. doi: 10.1046/j.1365-3156.2001.00709.x. [DOI] [PubMed] [Google Scholar]
- 28.Johansson E, Long NH, Diwan VK, Winkvist A. Gender and tuberculosis control: perspectives on health seeking behaviour among men and women in Vietnam. Health Policy. 2000;52:33–51. doi: 10.1016/s0168-8510(00)00062-2. [DOI] [PubMed] [Google Scholar]
- 29.Giorgianni SJ. The health repercussions of stigma. The Pfizer Journal. 2004;5:13–23. [Google Scholar]
- 30.Rajeswari R, Chandrasekaran V, Suhadev M, Sivasubramaniam S, Sudha G, Renu G. Factors associated with patient and health system delays in the diagnosis of tuberculosis in south India. Int J Tuberc Lung Dis. 2002;6:789–795. [PubMed] [Google Scholar]
- 31.Yamasaki-Nakagawa M, Ozasa K, Yamada N, Osuga K, Shimouchi A, Ishikawa N, Bam DS, Mori T. Gender difference in delays to diagnosis and health care seeking behaviour in a rural area of Nepal. Int J Tuberc Lung Dis. 2001;5:24–31. [PubMed] [Google Scholar]
- 32.Johansson E, Long NH, Diwan VK, Winkvist A. Attitudes to compliance with tuberculosis treatment among women and men in Vietnam. Int J Tuberc Lung Dis. 1999;3:862–868. [PubMed] [Google Scholar]
- 33.Long NH, Johansson E, Diwan VK, Winkvist A. Fear and social isolation as consequences of tuberculosis in Viet Nam: a gender analysis. Health Policy. 2001;58:69–81. doi: 10.1016/s0168-8510(01)00143-9. [DOI] [PubMed] [Google Scholar]
- 34.Eastwood SV, Hill PC. A gender-focused qualitative study of barriers to accessing tuberculosis treatment in The Gambia, West Africa. Int J Tuberc Lung Dis. 2004;8:70–75. [PubMed] [Google Scholar]
- 35.Oeser CC, Escombe AR, Gilman RH, Friedland JS, Evans CA, Moore DA. Does traditional medicine use hamper efforts at tuberculosis control in urban Peru? Am J Trop Med Hyg. 2005;73:571–575. [PubMed] [Google Scholar]
- 36.DFID Health Systems Resource Centre . Measuring Health and Poverty: A Review of Approaches to Identifying the Poor. DFID; London, UK: 2002. [Google Scholar]