How did the study come about?
In The Secrets of Long Life in the National Geographic1 Buettner explored longevity among three communities in Sardinia Italy, Okinawa Japan, and Loma Linda California. Loma Linda is largely a community of 7th-day Adventists. In 1969 initial research2 found that among individuals surviving past age 35 Adventist women in California lived 3.7 years longer than their counterparts and Adventist men 6.2 years longer. In a later, larger California sample3 the differences were even stronger—4.4 years for women and 7.3 years for men. Exercise, vegetarian diet, not smoking, eating nuts and social support have been found to predict longevity in Adventists.4 Yet even when these and several psychological variables are controlled church attendance still predicts greater longevity.5
Interest has been increasing regarding the association of both mental and physical health with religion or spirituality.6 There have been a number of literature reviews that have concluded that the associations of religion and health are largely positive.7–9 In fact, Hall10 concluded religious attendance was more cost-effective in increasing longevity than statin-type medications. While some have questioned the quality of these research conclusions11 and others have pointed out that the benefits or costs of religion may vary depending on the indicator of religious involvement,12,13 there is general agreement regarding the need for more and better research on the subject. Nonetheless, Hummer and his colleagues14 concluded there was consistent evidence that religious attendance was associated with lower mortality risk in cross-sectional and prospective studies. They also concluded there was a need for more diverse measures of religious involvement, comparison among specific subpopulations, and a better understanding of the pathways by which religion might influence health (p. 1226). It was with this goal in mind that this Biopsychosocial Religion and Health Study was developed.
What does the study cover?
Conceptual model
The coverage of the study is best understood in the framework of our conceptual model. Two central concepts in this model are allostatic load and cumulative risk exposure. Allostasis is the process of achieving biologic stability through change—specifically, dynamic adjustments in multiple physiological systems to maintain equilibrium and set points (homeostasis) when responding to environmental demands.15 Healthy functioning requires allostasis, which is adaptive and protective over the short term. However, allostasis ‘has a potential cost to the body when allostasis is either called upon too often or is inefficiently managed, and that cost is referred to as “allostatic load” ’ (p. 174).16 Allostatic load can occur when chronic stressors place a burden on the organism but can also result from a lifetime of exposure to events demanding allostatic adjustment. We refer to this lifetime exposure as cumulative risk exposure. Allostatic load, over the life course, ultimately results in increased morbidity and mortality.17,18
In our model cumulative risk exposure aggregates an individual's risk level across physical risks such as poverty, poor housing quality, and violence exposure (which often co-occur), as well as psychosocial risks such as poor parental or marital bond, or poor job satisfaction.19 Cumulative risk exposure influences allostasis to affect allostatic load. Allostatic load, in turn, produces changes in morbidity, mortality and quality of life. However, the effects of cumulative risk exposure are both mediated and moderated by positive and negative aspects of religion. These positive and negative aspects have at least part of their influence by causing changes in lifestyle, psychological and social factors.
Aims
We use the term manifestations to refer to beliefs and behaviors as they show themselves in psychosocial and biological responses. Our primary aims were to examine: (i) how religious experience moderates the impact of cumulative risk exposure on quality of life, health, and mortality; (ii) the mechanisms by which these manifestations of religion might operate; (iii) how manifestations of religious experience relate to biologic indicators of allostatic load within the context of cumulative risk exposure, and (iv) whether these manifestations operate differently in non-Blacks and Blacks—Blacks being a group for whom religion may be more central in life and, perhaps, in health.13,20,21
Who is in the sample?
We could answer aims i, ii and iv with new questionnaire data and with the mortality and hospitalization data being collected by AHS-2.22 However, obtaining biologic samples as required by aim iii is much more difficult and expensive. Hence, we divided our study into two sub-studies: the Psychosocial Manifestations of Religion Sub-study (PsyMRS) and the Biological Manifestations of Religion Sub-study (BioMRS). PsyMRS is a large prospective study of approximately 11 000 individuals from the AHS-2 population who completed the supplemental PsyMRS questionnaire.
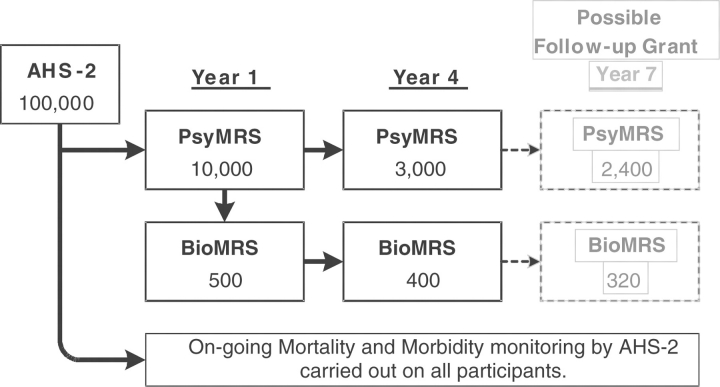
Figure 1 shows our sampling plan. The sample will be surveyed at 3-year intervals while the study continues. AHS-2 will provide data on mortality and hospitalizations as described later. BioMRS is an approximately 530-person sub-study embedded within the larger PsyMRS. All members of BioMRS complete the PsyMRS questionnaire and, in addition, attend a clinic where biologic indicators are assessed. All individuals in both PsyMRS and BioMRS were selected from those participating in AHS-2. The AHS-2 recruitment methods and sampling strategy are described elsewhere.22
Figure 1.
Sampling plan. AHS-2 is the Adventist Health Study 2. PsyMRS is the Psychosocial Manifestations of Religion Sub-study involving collection of questionnaire data. BioMRS is the Biological Manifestations of Religion Sub-study that includes assessment of biometrics, blood/saliva/urine markers, and memory/learning ability. Numbers are targets. For example, while our year one target for PsyMRS was 10 000, as August 2007, 11 004 were in the dataset
Psychosocial manifestations of religion sub-study (PsyMRS)
We randomly sampled 20 000 AHS-2 participants and sent each the 20-page religion and health questionnaire with up to three reminder cards. Based on pilot studies we expected response rates of 55% from Caucasian and 26% from African American participants. Our goal was to enroll 3400 Blacks and 6600 Caucasians. Data collection started in September 2006 and was largely completed by August 2007. Our return rate was higher than expected with 60% from Caucasians and 31% from Blacks.
Biological manifestations of religion sub-study (BioMRS)
Recruitment for BioMRS was through an initial letter followed by phone calls. Our goal was to obtain 300 non-Black and 200 Black participants; this moderately overweighs Black participants when compared with the overall AHS-2 sample and the PsyMRS study. Only individuals living within driving distance of our clinic sites in Loma Linda, Riverside, and Los Angeles were contacted. There were 536 participants (296 Whites, 239 Blacks, and 1 Hispanic).
How often will they be followed up?
In the 3rd year after the initial sample we aim for a minimum of 3000 PsyMRS participants and 400 BioMRS participants. If further funding is obtained, both PsyMRS and BioMRS data will be collected at additional time points to allow latent growth curve modelling of the relations among study variables.23
What has been measured?
PsyMRS
Our conceptual framework suggested four categories of variables relevant to the PsyMRS questionnaire: cumulative risk exposure, religion, mediating and outcome variables. Allostatic load cannot be directly assessed from the questionnaire. In almost all cases we have used scales which have been validated in other studies or, where they are not available, validated our own.
Cumulative risk exposure
Cumulative risk exposure variables are included to assess a broad spectrum of cumulative and acute stressors that have been associated with health or quality of life.19,24 Most available single measures do not assess risk exposure at more than one point in the person's life so we broadly sampled cumulative risk across the life course. The measures include physical and socioeconomic stress: housing quality, family size, and poverty; and psychosocial stress: perceived stress, job stress/control/satisfaction, unfair treatment and discrimination, parent bonding, marital satisfaction, and trauma exposure.
Religion
Religion variables were selected to include four aspects of religion: (i) affective—gratitude, forgiveness, loving vs controlling God, positive and negative eschatological attitudes; (ii) cognitive—intrinsic religiosity, some forms of religious coping, spiritual meaning; (iii) behavioural—church attendance, Sabbath keeping, prayer types, church organizational activity; and (iv) social—congregational sense of community, religious support.
Mediating variables
Mediating variables were selected based on Ellison and Levin's typology of six mechanisms for the religion/health connection25—(i) health behaviors and personal lifestyle variables (from AHS-2), (ii) social integration and social support, (iii) self-esteem and personal efficacy, (iv) positive vs negative emotions, (v) healthy beliefs (e.g. optimism) and (vi) coping resources and behaviors. Additionally we included measures of neuroticism, impression management and self-deception to serve as control variables.
Outcome variables
Outcome variables included health related quality of life (the SF-12)26 and life satisfaction as well as various medical history, symptom frequency, medication use and sleep disturbance questions and an adaptation of the Charlson comorbidity index.27 Finally, total and coronary disease mortality will be available on followup.
BioMRS
All BioMRS participants completed a PsyMRS questionnaire, provided a waking saliva sample and a 12-h, overnight urine sample. At the clinic, fasting blood and adipose samples were taken; biometrics and percentage body fat (bioimpedence) were also assessed. Participants then provided physical and cognitive function data—Independent Activities of Daily Living; physical performance, based on five separate tests of physical ability—balance, gait, chair stands, manual ability, and grip strength; and the California Verbal Learning Test.28 Our measure of allostatic load (Table 1) is designed to summarize levels of physiological activity across a wide range of regulatory systems pertinent to disease risk, as previously described.29–31
Table 1.
Biological parameters used to determine the allostatic load index
| Biological parameter | Description |
|---|---|
| Cardiovascular/Metabolic factors | |
| Blood pressure | |
| Systolic BP (mmHg) | Resting, seated systolic and diastolic BP were measured 3 times and determined |
| Diastolic BP (mmHg) | by averaging the 2nd and 3rd readings |
| Lipid Profile | |
| Total/HDL cholesterol ratio | Measured in fasting blood samples collected in heparinized tubes by venipuncture |
| HDL cholesterol (mg/dl) | Total cholesterol, triglycerides and HDL cholesterol were measured using a |
| Triglycerides (mg/dl) | Cholestech LDX Analyzer (Cholestech Corp., Hayward, CA). LDL cholesterol (LDL) |
| Total cholesterol | was calculated using the Friedewald equation [total cholesterol minus high-density lipoprotein (HDL) cholesterol minus very-low-density lipoprotein (VLDL) cholesterol (estimated as triglyceride divided by 5)] |
| Metabolism | |
| HbA1c (%) | Determined in heparinized blood samples by a boronate affinity assay using a Cholestech GDX Analyzer (Cholestech Corp., Hayward, CA) |
| Body mass index (kg/m2) | Weight was determined using the scale function of the Tanita Body Fat Analyzer. Height was measured using a portable stadiometer. BMI was calculated as weight (kg)/height (m)2 |
| Waist–hip ratio | Waist circumference was measured at its narrowest point between the ribs and iliac crest, and hip circumference was measured at the maximal buttocks as previously described48 |
| Percentage body fat (%) | Foot-to-foot bioelectrical impedance analysis was conducted using the Tanita Scale plus body fat monitor (Model BF-350). Subjects were measured standing erect with bare feet on the analyzer footpads. Percentage body fat was estimated using the Tanita's programmed height, weight, age, and sex-specific equation |
| Plasma Albumin (mg/dl) | Measured using colorimetric ELISA assay kits (Assaypro, St. Charles, MO) |
| Activity of stress pathways | |
| HPA Axis | |
| Waking Salivary cortisol (μg/ml) | Determined using enzyme immunoassay kits developed for use in saliva (Salimetrics, Inc., State College, PA, USA) |
| Sympathetic nervous system | |
| Urinary NE (μg/g creatinine) Urinary EPI (μg/g creatinine) | Urine was collected over a 12-h period. Determined by high-performance liquid chromatography with electrochemical detection (HPLC). Creatinine was determined using a colorimetric enzymatic diagnostic kit (R & D Systems, Minneapolis, MN) |
| Inflammation markers | |
| Plasma IL-6 (pg/ml) | Measured using high sensitivity ELISA kits (IL-6, R & D Systems, Minneapolis, MN |
| Plasma CRP (μg/ml) | CRP, Assaypro, St. Charles, MO) |
| Specific organ systems | |
| Creatinine clearance (mg/dl) | Estimated using the modified Cockcroft-Gault equation, as follows: [[140-age (year)] × lean body weight (kg)]/72 × serum creatinine (mg/dl)]. For women 15% was deducted. Lean body weight for males is computed as 50 kg plus 2.3 kg for each inch of height over 5 feet, and in women as 45.5 kg plus 2.3 kg for every inch of height over 5 feet |
AHS-2
The AHS-2 questionnaire was completed by BRHS participants 1–3 years before the PsyMRS questionnaire. The AHS-2 data set includes 130 food frequency items, daily physical activity, detailed ethnicity and other demographics, country of birth, religion of mother and father who raised participant, religion at age 15–25, age at baptism, medical history, women's health conditions and history, alcohol and tobacco use, and medications used at baseline. AHS-2 will provide hospitalization history information based on a biennial survey and causes of mortality by matching the sample with the National Death Index.22
What attrition is expected?
Based on previous studies of Adventists in California32 we expect good retention in our sample. With the planned cohort maintenance and retention activities of AHS-222 we hope to trace a high percentage of the participants over at least a 3-year period.
What has been found?
The demographics of the PsyMRS sample are shown in Table 2 along with comparisons with the 2006 General Social Survey, a survey based on national probability sample.33 Ages below 35 are omitted as the inclusion criteria for AHS-2 in the first several years was age 35+ for non-Blacks and age 30+ for Blacks.
Table 2.
Comparison of demographics in the biopsychosocial religion and health study (BRHS) and the general social survey (GSS) by ethnicity and gender
| BRHS |
GSS |
|||||||
|---|---|---|---|---|---|---|---|---|
| Black |
White |
Black |
White |
|||||
| % | n | % | n | % | n | % | n | |
| Gender | ||||||||
| Male | 26.3 | 910 | 36.5 | 2230 | 38.7 | 164 | 44.8 | 1130 |
| Female | 73.7 | 2549 | 63.5 | 3886 | 61.3 | 260 | 55.2 | 1395 |
| Education | ||||||||
| Male | ||||||||
| High school or less | 17.3 | 156 | 16.1 | 357 | 53.0 | 87 | 41.0 | 460 |
| Some college | 34.7 | 313 | 29.0 | 646 | 30.5 | 50 | 24.5 | 275 |
| College or more | 47.9 | 432 | 54.9 | 1221 | 16.5 | 27 | 34.5 | 387 |
| Female | ||||||||
| High school or less | 19.9 | 497 | 20.5 | 793 | 45.3 | 116 | 42.8 | 595 |
| Some college | 40.8 | 1020 | 42.6 | 1645 | 33.6 | 86 | 28.8 | 401 |
| College or more | 39.2 | 980 | 36.9 | 1424 | 21.1 | 54 | 28.4 | 395 |
| Marital status | ||||||||
| Male | ||||||||
| Married | 82.3 | 721 | 88.3 | 1884 | 39.0 | 64 | 59.8 | 674 |
| Widowed | 2.3 | 20 | 3.5 | 75 | 4.9 | 8 | 4.7 | 53 |
| Divorced | 7.3 | 64 | 5.3 | 113 | 23.8 | 39 | 20.2 | 228 |
| Separated | 2.2 | 19 | 0.4 | 9 | 7.3 | 12 | 2.6 | 29 |
| Never married | 5.9 | 52 | 2.4 | 52 | 25.0 | 41 | 12.8 | 144 |
| Female | ||||||||
| Married | 50.6 | 1237 | 70.8 | 2645 | 28.8 | 75 | 51.9 | 724 |
| Widowed | 12.5 | 306 | 15.0 | 559 | 17.3 | 45 | 16.9 | 236 |
| Divorced | 20.0 | 489 | 9.7 | 361 | 20.8 | 54 | 20.4 | 285 |
| Separated | 3.4 | 82 | 0.7 | 28 | 6.2 | 16 | 2.7 | 38 |
| Never married | 13.5 | 330 | 3.8 | 143 | 26.9 | 70 | 8.0 | 112 |
| Age | ||||||||
| Male | ||||||||
| 35–44 | 12.1 | 110 | 8.0 | 179 | 30.5 | 50 | 25.4 | 287 |
| 45–54 | 26.7 | 243 | 17.3 | 386 | 30.5 | 50 | 29.4 | 332 |
| 55–64 | 29.3 | 267 | 24.8 | 554 | 21.3 | 35 | 21.9 | 248 |
| 65–74 | 19.1 | 174 | 25.2 | 561 | 13.4 | 22 | 12.9 | 146 |
| 75–84 | 10.8 | 98 | 19.0 | 423 | 4.3 | 7 | 7.8 | 88 |
| 85+ | 2.0 | 18 | 5.7 | 127 | 0 | 0 | 2.6 | 29 |
| Female | ||||||||
| 35–44 | 14.5 | 370 | 8.8 | 343 | 35.4 | 92 | 25.1 | 350 |
| 45–54 | 26.3 | 671 | 19.0 | 737 | 30.8 | 80 | 25.9 | 361 |
| 55–64 | 28.4 | 724 | 24.7 | 961 | 17.3 | 45 | 20.9 | 292 |
| 65–74 | 19.6 | 500 | 23.3 | 907 | 9.2 | 24 | 14.1 | 197 |
| 75–84 | 9.3 | 236 | 18.3 | 710 | 4.6 | 12 | 10.8 | 150 |
| 85+ | 1.9 | 48 | 5.9 | 228 | 2.7 | 7 | 3.2 | 45 |
Notes: Only individuals older than 35 were included from both samples since that was an initial inclusion criteria for BRHS. All GSS vs BRHS comparisons on education, marital status, and age within genders are statistically significant.
One concern is the relatively small number of Black male Adventist participants. However, there are sufficient numbers for data analysis in the middle ranges of age, education and income. There are no large education differences between male and female or Black and White Adventists. While not shown in Table 2 there are no large percentage differences in income though females and Black Adventists have slightly lower income than males and White Adventists respectively. One interesting figure is the relatively low number of Black Adventist women who are married and a correspondingly high number who are divorced or never married relative to both Black male Adventists and to both male and female White Adventists.
Comparing the PsyMRS sample and the GSS sample, the BRHS sample has more females, more college educated individuals especially among the Blacks, more married individuals and more individuals above age 65 in all genders and ethnicities. The educational difference may be the result of the literacy level implied by being able to fill out the 50 page AHS-2 questionnaire and possibly the emphasis on education among 7th-day Adventists—e.g. though in the 2000 Census only the 18th largest denominational group,34 Adventists have the 5th largest number of denominational schools35 and the 9th largest number of students enrolled in such schools.36 The difference between Adventists and the GSS sample is consistently larger for Black males than other groups. Adventists are more likely to be married and less likely to be divorced than the GSS sample. Black Adventist women are also less likely to be widowed (P = 0.022 by Fisher's exact Test) and never married (P < 0.0005) than Black women in the GSS sample.
Table 3 compares the BRHS and GSS data for two religious questions. BRHS participants were much more likely to report attending church. On the other hand, while prayer was more frequent for Adventists than for those in the GSS participants, the frequency of daily prayer for Black Adventist females was similar to that found in GSS Black females.
Table 3.
Comparison of religion variables in the biopsychosocial religion and health study and the general social survey by ethnicity and gender
| BRHS |
GSS |
|||||||
|---|---|---|---|---|---|---|---|---|
| Black |
White |
Black |
White |
|||||
| % | n | % | n | % | n | % | n | |
| Church Attendance | ||||||||
| Male | ||||||||
| Never | 0.3 | 3 | 0.5 | 12 | 20.5 | 32 | 27.6 | 298 |
| A few times a year or less | 1.7 | 15 | 3.8 | 84 | 30.8 | 48 | 33.6 | 363 |
| Monthly or several times a month | 3.2 | 29 | 6.2 | 138 | 18.6 | 29 | 12.9 | 139 |
| Weekly or more often | 94.8 | 860 | 89.5 | 1987 | 30.1 | 47 | 25.9 | 280 |
| Female | ||||||||
| Never | 0.1 | 3 | 0.6 | 23 | 12.3 | 30 | 22.1 | 286 |
| A few times a year or less | 1.5 | 39 | 4.3 | 168 | 12.7 | 31 | 32.2 | 417 |
| Monthly or several times a month | 4.7 | 119 | 6.1 | 237 | 23.4 | 57 | 13.2 | 171 |
| Weekly or more often | 93.6 | 2372 | 88.9 | 3441 | 51.6 | 126 | 32.5 | 420 |
| Prayer frequency | ||||||||
| Male | ||||||||
| Several times a day | 56.7 | 513 | 51.5 | 1138 | 38.1 | 40 | 21.4 | 155 |
| Once a day | 20.3 | 184 | 23.6 | 520 | 33.3 | 35 | 25.7 | 186 |
| Several times a week | 15.4 | 139 | 16.1 | 356 | 6.7 | 7 | 12.6 | 91 |
| Once a week | 2.9 | 26 | 2.2 | 48 | 5.7 | 6 | 6.8 | 49 |
| <Once a week | 3.8 | 34 | 5.9 | 130 | 8.6 | 9 | 16.7 | 121 |
| Never | 1.0 | 9 | 0.7 | 16 | 7.6 | 8 | 16.9 | 122 |
| Female | ||||||||
| Several times a day | 66.1 | 1663 | 60.2 | 2313 | 64.4 | 116 | 39.6 | 364 |
| Once a day | 18.0 | 453 | 22.5 | 863 | 25.0 | 45 | 30.4 | 280 |
| Several times a week | 11.7 | 294 | 13.2 | 508 | 7.2 | 13 | 11.0 | 101 |
| Once a week | 1.4 | 35 | 1.2 | 46 | 2.2 | 4 | 5.8 | 53 |
| <Once a week | 2.5 | 64 | 2.6 | 101 | 0.6 | 1 | 8.3 | 76 |
| Never | 0.2 | 6 | 0.3 | 12 | 0.6 | 1 | 5.0 | 46 |
Notes: All GSS versus BRHS comparisons on church attendance and prayer frequency within genders are statistically significant except for prayer in Black females.
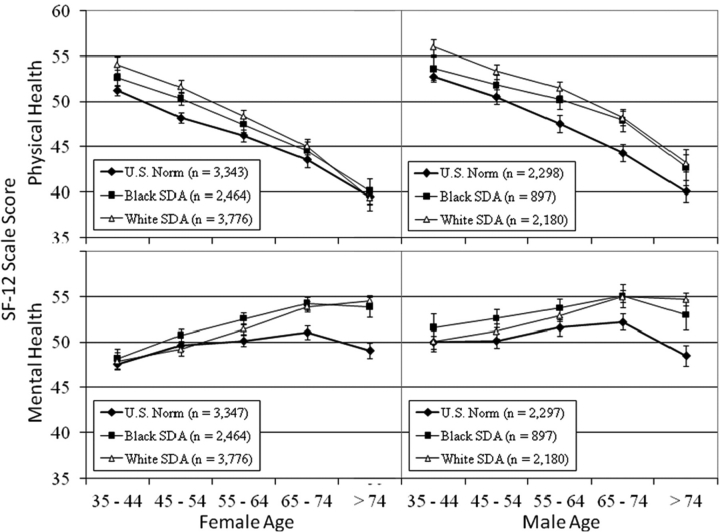
Previous research with earlier Adventist cohorts has shown that 7th-day Adventists have lower mortality rates than the general population.4 However, until now we have had no data on quality of life. Figure 2 shows physical and mental quality of life on the SF-12v2 for Black and White Adventists compared with the national norms taken from the 2002 SF-12v2 manual based on data collected in 1999 and 2000.37 Unfortunately, national norms for the SF-12v2 are not available by ethnicity but the comparisons are nonetheless interesting. It appears that both Black and White Adventists in our sample report better physical and mental health than the national norms but the patterns differ by age group. For physical health Adventist females tend to be higher than national norms in the 45–54 age group and the differences tend to get smaller as the age of the groups increase. For males the differences tend to be there at all ages but are more pronounced in the 55- to 74-year old age range. Adventists and non-Adventists have similar levels of mental health in the 35- to 44-year old age group but the mental health of both Black and White Adventists is better in the older age groups. Interestingly, Black Adventists at some ages seem to report better mental health than even White Adventists.
Figure 2.
Physical and Mental Health based on SF-12 composite scores for 7th-day Adventist Blacks and Whites and for SF-12 national norms.38 Numbers are scale scores (mean 50, SD 10) for individuals over 35 years of age
The overall better level of physical and mental health for Adventists could be a volunteer effect since our respondents had to fill out long questionnaires. On the other hand, the national norms were also based on volunteers though the questionnaires involved were not as extensive. Still, the fact that the gaps were bigger for mental health and that that gap is greater at older ages is interesting and harder to explain as a volunteer bias alone. These patterns will warrant further examination as our study progresses. The better physical health of Black Adventists than the national norms also warrants attention given the data on health disparities suggests Blacks score lower on physical health measures.38
Main strengths and weaknesses
One potential weakness of this study is that the data are collected exclusively on 7th-day Adventists. While this means that cross-denominational differences cannot be explored this is no different from other studies which have focused on single denominations such as Baptists,39,40 Catholics,41 Mormons,38–40 and Presbyterians.43 Additionally, our preliminary examination of the data shows a wide range of responses on most religion variables. While other approaches are useful,43–45 examination of the religion-health association within a single denomination has several strengths: (i) single denomination studies eliminate the need to control for denominational differences; (ii) because members of a single denomination have a shared religious tradition they will have less variation in how they interpret more nuanced religious questions, even as they differ in their responses to such questions; (iii) in addition, the examination of Blacks is easier because confounding by socio-economic status is less pronounced and thus easier to control than in the U.S. population due to the Adventist education emphasis;46 (iv) finally, just as one cannot learn about economic mobility and success solely by studying the urban underclass and focusing on barriers to achievement, one cannot learn about health and longevity by focusing exclusively on causes of death and studying persons who die prematurely. It behoves us to examine groups that defy the odds and enjoy better-than-average health and longevity; there is no better source of good biopsychosocial, quality of life and religious data on one of these strategically important groups, the 7th-day Adventists, than the data from this study.
This study has a number of strengths. First, it includes a much wider range of religious variables than previous epidemiological studies.14,43–45 Second, we used a systematic theoretical scheme for inclusion of possible mediators of the religion and health relationship and, hence, the study includes a wide range of potential psychosocial- and lifestyle-mediating variables. Third, it includes a variety of biologic and functional assessments of allostatic load that have not been incorporated in previous studies of the religion and health connection. Fourth, the quality of life measures, assessed for the first time on an Adventist population, will allow us to determine whether the longer lives of Adventists are accompanied by a longer span of high quality life or whether these longer lives just stretch out the period of poor quality life. The Biopsychosocial Religion and Health Study has potential to greatly increase our understanding of the religion-health relationship and its implications for public health.
Where can I find out more and potential for collaboration?
We are still in the process of cleaning data and prospective data collection has yet to begin. Thus, the data are not freely available. However, BRHS researchers would welcome contacts from other investigators interested in collaboration on projects relating to specific aspects of the data we are collecting. Contacts can be made through the writers of this paper or through the Adventist Health Study office at Loma Linda University.
Funding
National Institute on Aging (1R01AG026348) for their support of this study; National Cancer Institute for their support of the Adventist Health Study 2 (5R01 CA094594); which is the parent study for the Biopsychosocial Religion and Health Study.
Acknowledgements
Drs Neal Krause, David Williams, Harold Koenig, William Strawbridge, Arthur A Stone; and Teresa Seeman have been serving as consultants on this project and to the extent that the choices we have made in design and assessment are good ones, we owe them a debt. We would like to add a special thanks to Jessica Tolman and Shveta Sanghani for performing the assays on the BioMRS biological samples, and to Christine Molinaro for facilitating all aspects of the BioMRS sub-study. We would also like to thank the graduate students who have worked in our clinics and on the phones contacting participants.
Conflict of interest: None declared.
References
- 1.Buettner D. The secrets of long life. (Cover story) Nat Geogr. 2005;208:2–27. [Google Scholar]
- 2.Lemon FR, Kuzma JW. A biologic cost of smoking. Decreased life expectancy. Arch Environ Health. 1969;18:950–55. doi: 10.1080/00039896.1969.10665519. [DOI] [PubMed] [Google Scholar]
- 3.Fraser GE, Shavlik DJ. Ten years of life: is it a matter of choice? Arch Intern Med. 2001;161:1645–52. doi: 10.1001/archinte.161.13.1645. [DOI] [PubMed] [Google Scholar]
- 4.Fraser GE. Diet, Life Expectancy, and Chronic Disease: Studies of Seventh-Day Adventists and Other Vegetarians. Oxford/New York: Oxford University Press; 2003. [Google Scholar]
- 5.Lee JW, Stacey GE, Fraser GE. Social support, religiosity, other psychological factors, and health. In: Fraser GE, editor. Diet, Life Expectancy, and Chronic Disease: Studies of Seventh-day Adventists and Other Vegetarians. New York: Oxford University Press; 2003. pp. 149–76. [Google Scholar]
- 6.Weaver AJ, Pargament KI, Flannelly KJ, Oppenheimer JE. Trends in the scientific study of religion, spirituality, and health: 1965–2000. J Relig Health. 2006;45:208–14. [Google Scholar]
- 7.McCullough ME, Hoyt WT, Larson DB, Koenig HG, Thoresen C. Religious involvement and mortality: a meta-analytic review. Health Psychol. 2000;19:211–22. doi: 10.1037//0278-6133.19.3.211. [DOI] [PubMed] [Google Scholar]
- 8.Powell LH, Shahabi L, Thoresen CE. Religion and spirituality. Linkages to physical health. Am Psychol. 2003;58:36–52. doi: 10.1037/0003-066x.58.1.36. [DOI] [PubMed] [Google Scholar]
- 9.Seybold KS, Hill PC. The role of religion and spirituality in mental and physical health. Curr Dir Psychol Sci. 2001;10:21–24. [Google Scholar]
- 10.Hall DE. Religious attendance: more cost-effective than Lipitor? J Am Board Fam Med. 2006;19:103–9. doi: 10.3122/jabfm.19.2.103. [DOI] [PubMed] [Google Scholar]
- 11.Sloan RP, Bagiella E. Religion and health. Health Psychol. 2001;20:228. doi: 10.1037//0278-6133.20.3.228. [DOI] [PubMed] [Google Scholar]
- 12.Krause N, Wulff KM. Religious doubt and health: exploring the potential dark side of religion. Sociol Relig. 2004;65:35–56. [Google Scholar]
- 13.Pargament KI. The bitter and the sweet: an evaluation of the costs and benefits of religiousness. Psychol Inq. 2002;13:168–81. [Google Scholar]
- 14.Hummer RA, Ellison CG, Rogers RG, Moulton BE, Romero RR. Religious involvement and adult mortality in the United States: review and perspective. South Med J. 2004;97:1223–30. doi: 10.1097/01.SMJ.0000146547.03382.94. [DOI] [PubMed] [Google Scholar]
- 15.McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 16.McEwen BS. The neurobiology of stress: from serendipity to clinical relevance. Brain Res. 2000;886:172–89. doi: 10.1016/s0006-8993(00)02950-4. [DOI] [PubMed] [Google Scholar]
- 17.Seeman TE, Crimmins E, Huang M-H, et al. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Soc Sci Med. 2004;58:1985–97. doi: 10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- 18.Karlamangla AS, Singer BH, Seeman TE. Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: MacArthur studies of successful aging. Psychosom Med. 2006;68:500–7. doi: 10.1097/01.psy.0000221270.93985.82. [DOI] [PubMed] [Google Scholar]
- 19.Evans GW. A multimethodological analysis of cumulative risk and allostatic load among rural children. Dev Psychol. 2003;39:924–33. doi: 10.1037/0012-1649.39.5.924. [DOI] [PubMed] [Google Scholar]
- 20.Ferraro KF, Koch JR. Religion and health among black and white adults: examining social support and consolation. J Sci Study Relig. 1994;33:362–75. [Google Scholar]
- 21.Krause N. Church-based social support and health in old age: exploring variations by race. J Gerontol: Ser B: Psychol Sci Social Sci. 2002;57:S332–S47. doi: 10.1093/geronb/57.6.s332. [DOI] [PubMed] [Google Scholar]
- 22.Butler TL, Fraser GE, Beeson WL, et al. Cohort profile: the adventist health study-2 (AHS-2) Int J Epidemiol. 2008;37:260–65. doi: 10.1093/ije/dym165. [DOI] [PubMed] [Google Scholar]
- 23.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford/New York: Oxford University Press; 2003. [Google Scholar]
- 24.Evans GW, Kim P, Ting AH, Tesher HB, Shannis D. Cumulative risk, maternal responsiveness, and allostatic load among young adolescents. Dev Psychol. 2007;43:341–51. doi: 10.1037/0012-1649.43.2.341. [DOI] [PubMed] [Google Scholar]
- 25.Ellison CG, Levin JS. The religion-health connection: evidence, theory, and future directions. Health Educ Behav. 1998;25:700–20. doi: 10.1177/109019819802500603. [DOI] [PubMed] [Google Scholar]
- 26.Ware JE, Kosinski M, Turner-Bowker DM, Gandek B. How to Score Version 2 of the SF-12® Health Survey (With a Supplement Documenting Version 1) Lincoln, RI: QualityMetric Incorporated; 2002. [Google Scholar]
- 27.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 28.Woods SP, Delis DC, Scott JC, Kramer JH, Holdnack JA. The California verbal learning test – second edition: test-retest reliability, practice effects, and reliable change indices for the standard and alternate forms. Arch Clin Neuropsychol. 2006;21:413–20. doi: 10.1016/j.acn.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 29.McEwen BS, Seeman T. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- 30.Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci USA. 2001;98:4770–75. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation–allostatic load and its health consequences. MacArthur studies of successful aging. Arch Intern Med. 1997;157:2259–68. [PubMed] [Google Scholar]
- 32.Beeson WL, Mills PK, Phillips RL, Andress M, Fraser GE. Chronic disease among Seventh-day Adventists, a low-risk group. Rationale, methodology, and description of the population. Cancer. 1989;64:570–81. doi: 10.1002/1097-0142(19890801)64:3<570::aid-cncr2820640303>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 33.Davis JA, Smith TW, Marsden PV. General Social Surveys, 1972–2006. Chicago, IL: National Opinion Research Center; 2007. [Google Scholar]
- 34.U.S. Census Bureau. [(5 March 2008, date last accessed)];Self-Described Religious Identification of Adult Population: 1990 and 2001. 2008 The Statistical Abstract: Religion February 27, 2008. Available from: http://www.census.gov/compendia/statab/tables/08s0074.xls. [Google Scholar]
- 35.National Center for Education Statistics. Number and Percentage Distribution of Private Schools, by School Level and Religious or Nonsectarian Orientation of School: United States, 2003–04. 2008. [(5 March 2008, date last accessed)]. Available from: http://nces.ed.gov/surveys/pss/tables/table_2004_03.asp.
- 36.National Center for Education Statistics. Number and Percentage Distribution of Private School Students, by School Level and Religious or Nonsectarian Orientation of School: United States, 2003–04. 2008. [(5 March 2008, date last accessed)]. Available from: http://nces.ed.gov/surveys/pss/tables/table_2004_09.asp.
- 37.Ware JE, Kosinski M, Turner-Bowker DM, Gandek B. How to Score Version 2 of the SF-12® Health Survey. Lincoln, RI: QualityMetric Incorporated; 2002. [Google Scholar]
- 38.Centers for Disease Control & Prevention. Health disparities experienced by Black or African Americans–United States. MMWR: Morbidity Mortality Weekly Rep. 2005;54:1–3. [PubMed] [Google Scholar]
- 39.Blazer DG, Hays JC, Musick MA. Abstinence versus alcohol use among elderly rural Baptists: a test of reference group theory and health outcomes. Aging Mental Health. 2002;6:47–54. doi: 10.1080/13607860120101086. [DOI] [PubMed] [Google Scholar]
- 40.Musick MA, Blazer DG, Hays JC. Religious activity, alcohol use, and depression in a sample of elderly Baptists. Res Aging. 2000;22:91–116. [Google Scholar]
- 41.Levin JS, Markides KS. Religious attendance and subjective health. J Sci Study Relig. 1986;25:31–40. [Google Scholar]
- 42.Hoge DR, Johnson B, Luidens DA. Determinants of church involvement of young adults who grew up in Presbyterian churches. J Sci Study Relig. 1993;32:242–55. [Google Scholar]
- 43.Ellison CG, Boardman JD, Williams DR, Jackson JS. Religious involvement, stress, and mental health: findings from the 1995 Detroit area study. Soc Forces. 2001;80:215–49. [Google Scholar]
- 44.Strawbridge WJ, Cohen RD, Shema SJ, Kaplan GA. Frequent attendance at religious services and mortality Over 28 Years. Am J Public Health. 1997;87:957–61. doi: 10.2105/ajph.87.6.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Strawbridge WJ, Shema SJ, Cohen RD, Kaplan GA. Religious attendance increases survival by improving and maintaining good health behaviors, mental health, and social relationships. Ann Behav Med. 2001;23:68–74. doi: 10.1207/s15324796abm2301_10. [DOI] [PubMed] [Google Scholar]
- 46.Fraser GE, Sumbureru D, Pribis P, Neil RL, Frankson MA. Association among health habits, risk factors, and all-cause mortality in a black California population. Epidemiology. 1997;8:168–74. doi: 10.1097/00001648-199703000-00008. [DOI] [PubMed] [Google Scholar]
- 47.Lohman TG, Roche AF, Martorell R. Anthropometric Standardization Reference Manual. Champaign, IL: Human Kinetics Books; 1988. [Google Scholar]