Abstract
Statewide hospital discharge data were used to assess the economic burden of neurocysticercosis in Los Angeles County (LAC) from 1991 through 2008. A neurocysticercosis hospitalization was defined as having a discharge diagnosis of cysticercosis in addition to convulsions, seizures, hydrocephalus, cerebral edema or cerebral cysts. This study identified 3,937 neurocysticercosis hospitalizations, with the number of annual hospitalizations remaining relatively unchanged over the study period (R2 = 0.01), averaging 219 per year (range 180–264). The total of all neurocysticercosis hospitalization charges over the study period was $136.2 million, averaging $7.9 million per year. The average charge per patient was $37.6 thousand and the most common payment method was Medicaid (43.9%), followed by private insurance (24.5%). The average length of stay was 7.2 days. The substantial number of hospitalizations and significant economic cost underscore the importance of neurocysticercosis in LAC.
Introduction
Cysticercosis is a parasitic infection caused by the larval form of the tapeworm Taenia solium found worldwide. Humans and pigs are infected after ingestion of tapeworm eggs, which are shed in the feces of human tapeworm carriers who are often asymptomatic. Ingested eggs hatch in the intestine, invade the intestinal wall, and migrate to striated muscles, the brain, liver and other tissues, where they develop into cysticerci. In humans, cysts can cause serious illness and sometimes death if they localize in the central nervous system (neurocysticercosis). Neurocysticercosis is a major cause of late-onset epilepsy in persons in developing countries.1,2 Pigs are the intermediate hosts of the parasite, and the parasite life cycle is completed in regions where humans are living in close contact with pigs. Humans consuming undercooked pork containing cysticerci from these regions may become tapeworm carriers (taeniasis). Recent studies of cysticercosis prevalence in pigs have revealed that up to 33% of pigs in villages of central Mexico3 and 31% of pigs in villages in Peru harbor the infection.4
Previous studies have identified Southern California as a region bearing a large part of the national disease burden for cysticercosis. One recent study reported that Los Angeles County (LAC) accounts for nearly a third of all cysticercosis deaths in the United States (70/221 from 1990 to 2002).5 Another study among migrant farm workers in rural Southern California6 (N = 449) revealed a T. solium cysticercosis seroprevalence of 1.8% and a T. solium taeniasis sero-prevalence of 1.1%. An earlier study of cysticercosis hospitalizations in four major LAC hospitals7 (1973–1983, N = 497) indicated a dramatic rise in the number of cases after 1977, which coincided with the introduction of the computed tomographic scan (CT scan). In response to the increase in the number of cases, the Department of Health Services (currently the Department of Public Health [DPH]) initiated an intervention program in 1988 requiring clinicians to report cases and the public health department to screen close contacts to identify and treat T. solium carriers.8 Of the reported cysticercosis cases where household contacts were tested by the public health department from 1988 to 1990 (N = 72), carriers were identified in 7% of the households (N = 5).
In the years that followed the number of reported cysticercosis cases in LAC has steadily dropped from 52 cases reported in 1991 to only six reported in 2008. This reduction is even more dramatic considering the growth in population over this time period (9.0 million in 1991 to 9.9 million in 2008, U.S. Census). However, in the absence of active disease surveillance, the true number of cysticercosis and neurocysticercosis in LAC are largely unknown. In addition to the considerable hardship that this disease presents to cases and families affected, it also presents a financial burden to institutions managing persons with such illness, as it often involves costly procedures. To provide some insight into the health care costs associated with neurocysticercosis, a review of neurocysticercosis hospitalizations in LAC for the years 1991–2008 was performed using jurisdiction-wide hospital discharge data available through the California Office of Statewide Health Planning and Development (OSPHD).
Methods
We used the OSHPD annual hospitalization discharge data sets from 1991 to 2008 for this analysis. The OSHPD collects data from all acute care hospitals licensed by the California Department of Public Health. This includes general acute care hospitals, acute psychiatric hospitals, chemical dependency recovery hospitals, and psychiatric health facilities. The hospitals are required to report their data and are charged a daily penalty for data not submitted by the established due dates. The dataset included demographic information, primary diagnosis, up to 24 additional diagnoses and up to 20 procedures performed while hospitalized. Also included in this data set are length of each hospitalization and resulting hospitalization charge.
We developed a method to capture the majority of the health care cost caused by neurocysticercosis hospitalizations in LAC. Because there is no specific ICD9 code for neurocysticercosis, cases were defined by selecting the code for cysticercosis (123.1) and then qualified as neurocysticercosis by selecting only those diagnosed with any of five commonly associated neurologic comorbidities: seizure (345.9), convulsion (780.3), hydrocephalus (331.4), cerebral edema (348.5), and cerebral cyst (348.0). Only hospitalizations occurring in California for LAC residents were used for this analysis. Hospitalizations occurring among non-LAC residents were excluded from the analysis. Demographics and comorbidities of cysticercosis hospitalizations that did not meet our neurocysticercosis case definition were also reviewed. Because this study aimed to capture the overall financial burden of neurocysticercosis, repeat hospitalizations by chronically infected persons with neurocysticercosis were not excluded.
Demographics and other comorbid medical conditions listed in the 24 hospitalization diagnostic fields were summarized. Common surgical and therapeutic procedures with risk of complications among the 20 procedural fields were reviewed. Length of hospitalization and hospitalization charges were calculated. Charges included daily hospital services, ancillary services, and any patient care services. Hospital-based physician fees are not reported to OSHPD and therefore were not included in this analysis. Years of life lost for those that died in the hospital were calculated by subtracting age at death from 75 years.
Results
There were 7,169 hospitalizations listing cysticercosis in the primary or additional diagnosis fields among LAC residents over the 18-year study period (1991 through 2008). These hospitalizations averaged 398 per year, from a low of 340 to a high of 459, with little change over time (R2 = 0.01). Of these, there were 3,937 neurocysticercosis hospitalizations identified for this analysis also diagnosed with seizure or convulsion (72.8%), hydrocephalus (30.9%), cerebral cyst (6.2%), or cerebral edema (2.2%) in the primary or additional diagnosis fields. Many of these neurocysticercosis hospitalizations listed cysticercosis in the primary diagnosis field (37.8%), followed by seizure or convulsion (15.2%), hydrocephalus (9.1%), and other diagnosis (37.9%). Additional diagnoses identified among neurocysticercosis hospitalizations included disorders of the eye (7.0%), diseases of skin or subcutaneous tissue (4.1%), headaches (3.3%), and psychosis (1.1%). Neurocysticercosis hospitalizations among LAC residents were reported from 143 different acute care health facilities across California, although 31.7% of these were reported from four LAC public hospitals.
Neurocysticercosis hospitalizations occurred primarily among Latinos (91.6%), many between 20 and 39 years of age (47.8%), with little difference by gender (male 53.0%, female 47.0%) (Table 1). The demographics of these hospitalizations changed little over time, with the exception of age. The mean age of neurocysticercosis hospitalizations distinctly increased by 0.8 years per year (R2 = 0.88) over the study period from a mean age of 31.3 years in 1991 to 43.1 years in 2008. The annual number of neurocysticercosis hospitalizations remained relatively unchanged over the study period (R2 = 0.01) averaging 219 per year, ranging from a low of 180 to a high of 264 per year (Figure 1). Of note, there were a smaller proportion of neurocysticercosis hospitalizations listing cysticercosis as the primary diagnosis in the second half of the study period (2000–2008, 34.6%) as compared with the first half (1991–99, 40.8%), possibly indicating a decrease in first time neurocysticercosis hospitalizations.
Table 1.
Demographics of neurocysticercosis hospitalizations, Los Angeles County 1991–2008 (N = 3937)
| n | % | |
|---|---|---|
| Race/ethnicity | ||
| Latino | 3,605 | 91.6 |
| Caucasian | 206 | 5.2 |
| API* | 25 | 0.6 |
| African American | 38 | 1.0 |
| Other or unknown | 63 | 1.4 |
| Gender | ||
| Male | 2,087 | 53.0 |
| Female | 1,850 | 47.0 |
| Age Group | ||
| 0–9 | 143 | 3.6 |
| 10–19 | 304 | 7.7 |
| 20–39 | 1,883 | 47.8 |
| 40–59 | 1,056 | 26.8 |
| 60+ | 551 | 14.0 |
| Mean Age (years) | Range | |
| Overall | 38.4 | 0–94 |
| 1991 (N = 211) | 31.3 | 1–87 |
| 2008 (N = 180) | 43.1 | 10–94 |
API = Asian/Pacific Islander.
Figure 1.
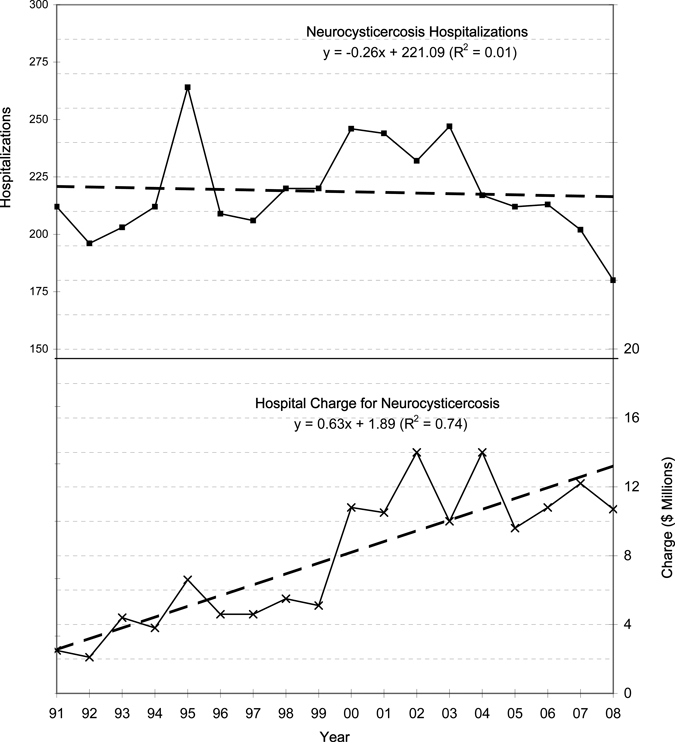
Neurocysticercosis hospitalizations and hospital charge by year.
Charges were available for 91.9% of the neurocysticercosis hospitalizations over the study period (N = 3618). The total in hospitalization charges over the study period was over $136 million, with an average annual charge of $7.9 million, ranging from a low of $2.1 million to a high of $14.0 million, as shown in Figure 1. Hospitalization charges increased an average of $631 thousand per year (R2 = 0.74). The average charge per hospitalization over the study period was $37.6 thousand; $66.1 thousand for the last year analyzed (2008) (Table 2). Neurocysticercosis hospitalizations involving a ventricular shunt procedure had the highest average charge per hospitalization of the procedures reviewed here ($122.4 thousand) and were performed in 14.3% of these hospitalizations. Neurocysticercosis hospitalizations involving a brain excision procedure also had a high average charge per patient ($103.0 thousand) and were performed in 3.7% of these hospitalizations.
Table 2.
Neurocysticercosis hospital charges and payment methods, Los Angeles County, 1991–2008
| Hospital charges (N = 3618) | $ | |
|---|---|---|
| Total charges | 136,157,683 | |
| Average annual charge | 7,877,778 | |
| Average charge per patient | 37,633 | |
| Brain excision procedure | 103,398 | |
| Shunt procedure | 122,358 | |
| Payment type (N = 3914) | n | % |
| MediCaid | 1,717 | 43.9 |
| Private insurance | 960 | 24.5 |
| Medicare | 412 | 10.5 |
| Self payment | 305 | 7.8 |
| County indigent program | 291 | 7.4 |
| Other payment* | 229 | 5.9 |
Other government or other payer.
Payment type was available for 99.4% of neurocysticercosis hospitalizations (N = 3,914). The most common hospitalization payment type was Medicaid (43.9%), followed by private insurance (24.5%), and Medicare (10.5%) (Table 2). Overall, public funds accounted for 67.7% of neurocysticercosis hospitalization charges, with little difference between the first and last half of the study period (69.4% versus 66.4%). The mean length of a hospital stay for a neurocysticercosis hospitalization was 7.2 days with no difference between the first and last half of the study period.
A central nervous system procedure was performed frequently during neurocysticercosis hospitalizations (32.3%), often involving lumbar punctures (12.0%), or a ventricular shunt insertion or replacement (14.3%) (Table 3). The replacement of a shunt, an indicator of a repeat hospitalization of a chronic case, occurred in 5.5% of neurocysticercosis hospitalizations with little change between the first and second half of the study period (5.8% versus 5.3%). The procedural codes were not detailed enough to indicate if newer endoscopic techniques might have been used to remove cysts in more recent cases. Neurological imaging (magnetic resonance imaging [MRI] or CT scan) was performed in 31.9% of neurocysticercosis hospitalizations. Imaging was used much more in the first half of the study period (23.5%) than the second half (40.4%).
Table 3.
Neurocysticercosis hospitalization procedures, Los Angeles County 1991–2008 (N = 3937)*
| Procedure | n | % |
|---|---|---|
| CNS procedure | 1,273 | 32.3 |
| Lumbar pucture | 472 | 12.0 |
| Brain procedure | 842 | 21.4 |
| Any ventricular shunt | 564 | 14.3 |
| Shunt removal/replace | 217 | 5.5 |
| Ventriculostomy | 155 | 3.9 |
| Brain excision | 131 | 3.3 |
| Craniotomy | 23 | 0.6 |
| MRI or CT scan of brain | 1,256 | 31.9 |
CNS = central nervous system; MRI = magnetic resonance imaging, CT = computed tomographic.
This study identified 77 fatal hospitalized cases of neurocysticercosis, representing 2.0% of all neurocysticercosis hospitalizations over the study period. Deaths ranged in age from 19 to 89 years. Compared with neurocysticercosis hospitalizations that survived, persons who died were similar by race and ethnicity (Latino 91.6% versus 90.0), but more likely to be female (61.0% versus 46.7%) and older in age (mean age 49.7 versus 38.2 years). Neurocysticercosis deaths were also more likely to have been diagnosed with hydrocephalus (52.0% versus 30.3%) compared with those that survived. The length of hospital stay was considerably longer for those that died during their hospitalization (14.3 days versus 7.1 days). These 77 deaths amount to an estimated 2,058 years of life lost and had an average hospitalization charge of $110 thousand per patient. The proportion and frequency of mortality among neurocysticercosis hospitalizations was higher in the second half of the study period (2.4%, N = 46) than in the first half (1.6%, N = 31).
There were an additional 3,232 cysticercosis hospitalizations identified over the study period that could not be classified as a neurocysticercosis hospitalization. These hospitalizations undoubtedly contributed to the economic burden of cysticercosis, with total hospital charges of $98.4 million. However, the component of neurocysticercosis burden associated with these hospitalizations may be difficult to assess in light of the other diseases or illnesses listed for these hospitalizations. Some of these hospitalizations may represent asymptomatic infection, as when a person is hospitalized for other reasons, such as head trauma, and cysts are discovered incidentally on neurological imaging. The demographics of these non-neurocysticercosis hospitalizations were similar to the neurocysticercosis hospitalizations, which were mostly Latino (88.4%) and similar by gender (female = 46.8%, male = 53.2%), but older in age (mean age 46.0 years). These non-neurocysticercosis hospitalizations had a slightly higher frequency of lumbar punctures (14.1% versus 12.5%), but much lower frequency of central nervous system (CNS) procedures excluding lumbar punctures (6.6% versus 21.3%) as would be expected. However, the frequency of mortality among non-neurocysticercosis hospitalizations (1.8%) was similar to that seen among neurocysticercosis hospitalizations (2.0%).
Discussion
The findings of this study underscore the considerable economic burden caused by neurocysticercosis in LAC. This disease causes frequent, often prolonged and costly hospitalization stays and considerable mortality. Hospital discharge data were useful in determining the economic burden of neurocysticercosis in LAC and could also be used for assessment by other jurisdictions with large numbers of immigrants from regions where the disease is endemic.
Although our neurocysticercosis hospitalization data set is not directly comparable to other studies of individual cases, some comparison was performed here to validate our method of selecting neurocysticercosis hospitalizations. The race and ethnicity of neurocysticercosis hospitalizations identified in this study (91.6% Latino) were similar to that found in an earlier study of reported cysticercosis cases in LAC from 1988–1991 (90.6% Latino),8 however our study population was older (mean age 38.4 years) than cysticercosis cases identified in the earlier study (mean age 27.5 years). In comparison to another study of hospitalized neurocysticercosis patients in Houston, TX9 (N = 114, 1994–1997), our neurocysticercosis hospitalizations had similar frequency of seizures or convulsions (73% versus 75%) and hydrocephalus (31% versus 25%), indicating that our case definition produced comparable estimates of these sequelae. In comparison to another earlier study of hospitalized cysticercosis patients at an LAC hospital10 (N = 238, 1981–86) our neurocysticercosis hospitalizations had a higher frequency of seizures or convulsions (73% versus 56%), and hydrocephalus (31% versus 21%), but required fewer ventricular shunt procedures (14% versus 30%). This may indicate that our method of capturing hospitalization procedures using procedural codes may under represent the actual number of procedures performed. Alternatively, it may represent a temporal trend in less aggressive surgical approaches in favor of medical management of neurocysticercosis cases.
The annual number of neurocysticercosis hospitalizations remained relatively unchanged over the study period, indicating the burden of disease has not changed substantially since it was first recognized as a problem in LAC in the 1980s. Many factors are likely influencing the trend of neurocysticercosis hospitalizations over time, including changes in immigration patterns, changes in access to care and timely diagnosis and treatment. The large discrepancy between the number of hospitalizations and the number of cases reported to the health department in LAC indicate that many cases go unreported. The LAC Department of Public Health has been successful in identifying and treating T. solium tapeworm carriers when a cysticercosis case is reported to the public health department, thus eliminating sources of new infection. However, the information presented here indicates that many hospitalized cases go unreported and (N = 6, 2008) many opportunities to screen cases and household contacts of persons with cysticercosis are being missed.
We describe a decrease in the number of neurocysticercosis hospitalizations listed as the primary discharge diagnosis. The cause of this trend is uncertain, but when taken in combination with the increasing age may indicate a decrease in the incidence of first time hospitalizations for neurocysticercosis. If this were true, then the number of neorcysticercosis hospitalizations caused by repeat visits of older chronic cases with multiple comorbidities may be increasing. However, if this were the case, one might expect the number of replacement shunt procedures to be increasing over time, which was not the case.
The increasing age of neurocysticercosis hospitalizations may reflect changes in access to care, immigration patterns, early diagnosis, or treatment. The 2007 LAC Health Survey indicates that over one-quarter (27%) of LAC adults reported difficulty accessing medical care when needed. Latinos were much more likely to report difficulty accessing care (40%) than other racial/ethnic groups.11 In addition, during the 1990s there was much emphasis placed on cysticercosis disease awareness and recognition including physician education from the public health department that may have resulted in earlier disease detection at a younger age.
The notable decrease in the use of CT and MRI scans in the second half of the study period is somewhat concerning, as these methods provide the best way to visualize viable cysts to determine their position. X-ray images cannot be used to image cysts in the brain and serological tests do not yield information such as the number of cysts involved and whether they are viable or in an anatomically important position within the brain. This information is important for determining the best treatment course for the patient and whether an antihelminthic agent is necessary.
Neurocysticercosis hospitalizations in LAC were compared with all hospitalizations occurring in the United States to contrast the severity and impact of these hospitalizations. Only hospitalizations for 2006 were used for this comparison. The average length of stay for neurocysticercosis hospitalizations in LAC (6.5 days) was 41% longer than the average hospital stay in the United States (4.6 days).13 The average charge for a neurocysticercosis hospitalization in LAC ($56.5 thousand) was nearly double that of an average hospitalization charge in the United States ($24.0 thousand).12 Neurocysticercosis hospitalizations in LAC were also younger (mean age 43.7 years) than an average hospitalization in the United States (mean age 52.5 years).13 The frequency of deaths among neurocysticercosis hospitalizations in LAC for 2006 (4.2%, 9/204) was higher than that seen for hospitalization in the United States for that year (2.0%), but deaths among neurocysticercosis hospitalizations in LAC for the entire study period (1991–2008) in LAC was comparable (2.0%).
Any conclusions based on hospital discharge data may be limited by billing incentives, which over-estimate the actual burden of the disease. The total number of hospitalizations listed in this review cannot be used to estimate the number of new incidents because of repeat visits by chronically infected persons. An earlier study of cysticercosis hospitalizations found that 14% of cases are hospitalized multiple times and that 33% of these hospitalized patients had more than two admissions.8 This data set did not capture the use of more recent serological testing methods used for diagnosis or more recent endoscope techniques developed for managing neurocysticercosis patients.
Neurocysticercosis hospitalizations occur predominately among adult Latinos in LAC. In response to the continued problem, the LAC Department of Public Health will be involved in a new effort to encourage reporting by hospital radiologists, neurologists, and infection control practitioners at key medical centers where a majority of the neurocysticercosis hospitalizations occur. Increased reporting from hospitals and clinicians will allow for public health follow-up of cases, identification and treatment of T. solium tapeworm carriers, prevention of additional cases, and reduction of the burden of disease in LAC. In addition, the LAC Department of Public Health will begin using new serological diagnostic techniques developed by the Centers for Disease Control and Prevention (CDC) with the intent of replacing the traditional stool specimen exams for detection of taeniasis carriers. This new testing, which requires only a finger prick, is more sensitive, simpler to implement, and more efficient in identifying T. solium carriers.14,15
Acknowledgments
Special thanks to Grace Run in the LAC ACDC unit for assisting in the design of the cysticercosis study database and to OSHPD for providing the Hospital Discharge Data. Special thanks to Caitlin Reed, David Dassey, Soodtida Tangpraphaphorn, and Michael Tormey for their comments and advice. The American Society of Tropical Medicine and Hygiene (ASTMH) assisted with publication expenses.
Footnotes
Authors' addresses: Curtis Croker, Roshan Reporter, and Laurene Macsola, Los Angeles County Department of Public Health, Acute Communicable Disease Control Unit, Los Angeles, CA, E-mails: ccroker@ph.lacounty.gov, rreporter@ph.lacounty.gov, and lmascola@ph.lacounty.gov.
References
- 1.Lescano AG, Garcia HH, Gilman RH, Gavidia CM, Tsang VC, Rodriguez S, Moulton LH, Villaran MV, Montano SM, Gonzalez AE. Taenia solium cysticercosis hotspots surrounding tapeworm carriers: clustering on human seroprevalence but not on seizures. PLoS Negl Trop Dis. 2009;3:e371. doi: 10.1371/journal.pntd.0000371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Willingham AL, 3rd, Harrison LJ, Fevre EM, Parkhouse ME. Inaugural meeting of the Cysticercosis Working Group in Europe. Emerg Infect Dis. 2008;14:e2. doi: 10.3201/1412.080889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morales J, Martinez JJ, Rosetti M, Fleury A, Maza V, Hernandez M, Villalobos N, Fragoso G, de Aluja AS, Larralde C, Sciutto E. Spatial distribution of Taenia solium porcine cysticercosis within a rural area of Mexico. PLoS Negl Trop Dis. 2008;2:e284. doi: 10.1371/journal.pntd.0000284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lescano AG, Garcia HH, Gilman RH, Guezala MC, Tsang VC, Gavidia CM, Rodriguez S, Moulton LH, Green JA, Gonzalez AE. Swine cysticercosis hotspots surrounding Taenia solium tapeworm carriers. Am J Trop Med Hyg. 2007;76:376–383. [PubMed] [Google Scholar]
- 5.Sorvillo FJ, DeGiorgio C, Waterman SH. Deaths from cysticercosis, United States. Emerg Infect Dis. 2007;13:230–235. doi: 10.3201/eid1302.060527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeGiorgio C, Pietsch-Escueta S, Tsang V, Corral-Leyva G, Ng L, Medina MT, Astudillo S, Padilla N, Leyva P, Martinez L, Noh J, Levine M, del Villasenor R, Sorvillo F. Sero-prevalence of Taenia solium cysticercosis and Taenia solium taeniasis in California, USA. Acta Neurol Scand. 2005;111:84–88. doi: 10.1111/j.1600-0404.2005.00373.x. [DOI] [PubMed] [Google Scholar]
- 7.Richards FO, Jr, Schantz PM, Ruiz-Tiben E, Sorvillo FJ. Cysticercosis in Los Angeles County. JAMA. 1985;254:3444–3448. [PubMed] [Google Scholar]
- 8.Sorvillo FJ, Waterman SH, Richards FO, Schantz PM. Cysticercosis surveillance: locally acquired and travel-related infections and detection of intestinal tapeworm carriers in Los Angeles County. Am J Trop Med Hyg. 1992;47:365–371. doi: 10.4269/ajtmh.1992.47.365. [DOI] [PubMed] [Google Scholar]
- 9.del la Garza Y, Graviss EA, Daver NG, Gambarin KJ, Shandera WX, Schantz PM, White AC., Jr Epidemiology of neurocysticercosis in Houston, Texas. Am J Trop Med Hyg. 2005;73:766–770. [PubMed] [Google Scholar]
- 10.Scharf D. Neurocysticercosis. Two hundred thirty-eight cases from a California hospital. Arch Neurol. 1988;45:777–780. doi: 10.1001/archneur.1988.00520310087022. [DOI] [PubMed] [Google Scholar]
- 11.Los Angeles County Department of Public Health Office of Health Assessment and Epidemiology. Los Angeles County Health Survey Data. 2010. http://www.lapublichealth.org/ha/HA_DATA_TRENDS.htm Available at. Accessed February 2.
- 12.Agency for Health Care Research and Quality U.S. Department of Health and Human Service/HCUPnet.s. 2010. http://hcupnet.ahrq.gov Available at. Accessed February 2, 2010.
- 13.DeFrances CJ. National Health Statistics Reports. 2008. 2006 National Hospital Discharge Survey. No 5.
- 14.Wilkins PP. Development of a serologic assay to detect Taenia solium taeniasis. Am J Trop Med Hyg. 1999;60:199–204. doi: 10.4269/ajtmh.1999.60.199. [DOI] [PubMed] [Google Scholar]
- 15.Tsang VC, Brand JA, Boyer AE. An enzyme-linked immunoelectrotransfer blot assay and glycoprotein antigens for diagnosing human cysticercosis (Taenia solium) J Infect Dis. 1989;159:50–59. doi: 10.1093/infdis/159.1.50. [DOI] [PubMed] [Google Scholar]


