ABSTRACT
A simple method for filtering water to reduce the incidence of cholera was tested in a field trial in Matlab, Bangladesh, and proved effective. A follow-up study was conducted 5 years later to determine whether the filtration method continued to be employed by villagers and its impact on the incidence of cholera. A total of 7,233 village women collecting water daily for their households in Bangladesh were selected from the same study population of the original field trial for interviewing. Analysis of the data showed that 31% of the women used a filter of which 60% used sari filters for household water. Results showed that sari filtration not only was accepted and sustained by the villagers and benefited them, including their neighbors not filtering water, in reducing the incidence of cholera, the latter being an unexpected benefit.
IMPORTANCE
A simple method for filtering pond and river water to reduce the incidence of cholera, field tested in Matlab, Bangladesh, proved effective in reducing the incidence of cholera by 48%. A follow-up study conducted 5 years later showed that 31% of the village women continued to filter water for their households, with both an expected and an unexpected benefit that filtration had both a direct and indirect effect in reducing cholera (chi-square statistic of 1,591.94; P = <0.0001). Results of the study showed that the practice of filtration not only was accepted and sustained by the villagers but also benefited those who filtered their water as well as neighbors not filtering water for household use in reducing the incidence of cholera.
INTRODUCTION
Diarrheal diseases are a major cause of death of children less than 5 years old in developing countries, and cholera, the most severe form of diarrhea, is characterized by massive loss of body fluid and electrolytes. Toxigenic Vibrio cholerae, the causative agent of cholera, is native to the aquatic environment, is present in Bangladesh (1), and is transmitted to humans, mainly via contaminated drinking water. According to a recent report, more than one billion people lack access to safe drinking water worldwide, and over five million die each year from diseases caused by unsafe drinking water (2). Recent studies suggest that improving drinking water quality at the point of use (POU) has a highly beneficial effect in combating waterborne disease (3, 4). Several POU technologies that involve both chemical treatment and filtration of water have become available during the past decade. However, compliance and sustainability are serious challenges because of many factors that range from cost, ease of use, production of sufficient quantities of clean water with minimal effort, social acceptance at the end user level, and most importantly, availability under natural disaster conditions when obtaining the bare necessities for daily life is a challenge.
Cholera remains a global concern, affecting those most economically deprived who lack access to safe drinking water. As is the case for diarrheal diseases, cholera is dose dependent, and the infective dose has been shown to be ca. 103 to 106 Vibrio cholerae O1 cells. Ingestion of this dose causes clinical symptoms (5, 6). V. cholerae is commensal to planktonic crustacean copepods, i.e., part of the copepod natural microbial flora, with a single copepod carrying up to 103 to 104 V. cholerae bacteria (7–9).
A method for simple filtration of water for domestic use, including drinking, was devised; this method employs cotton sari cloth, a material readily available to village women in Bangladesh (10). When this method was tested in the laboratory, using 1 to 4 layers of sari cloth to filter pond and river water containing V. cholerae attached to small crustacean zooplanktonic copepods and particulate matter, this simple procedure successfully reduced the number of V. cholerae bacteria by 2 log units (10–12). Whether 1, 2, 3, or 4 layers of sari cloth was used as a filter, the number of V. cholerae bacteria in the water was reduced by ca. 90%. Four layers of sari cloth were considered optimal for water filtration, since it consistently removed >99% of the bacteria, but 2 or 3 layers were approximately equally effective (10). After the laboratory-based tests were completed, a field trial using cotton sari cloth was performed, and as a reference, a commercially available nylon material that was used to eradicate dracunculiasis in Africa was included. Both were field tested for efficacy in reducing cholera in Matlab, Bangladesh. That is, village women responsible for collecting water, in a population of 30,000 (15,000 in each group, one group using sari filters and the other using nylon filters), were taught how to use folded cotton sari cloth or nylon mesh to filter their daily water. A third group of 15,000 villagers, receiving no instruction with respect to filtration of their water, served as the control group. Results of the field trial showed that the number of cholera cases was reduced approximately 50% in the group using cotton sari cloth to filter water at the time of collection, with nylon filtration slightly less effective and also very expensive compared to sari cloth (11).
Although POU technologies have been shown to be effective in laboratory experiments, they do not necessarily perform equally well in the field over an extended period of time (13). The objective of the original study was to determine whether the incidence of cholera could be reduced by sari filtration, since filtering out plankton and particulate matter removed >99% of V. cholerae associated with zooplankton. Although 50% reduction in cholera cases was observed among sari filter users, there was concern that the practice of sari water filtration would not be sustained among villagers once the original study had been completed. Hence, the study reported here was undertaken.
Therefore, 5 years after the original field trial, a follow-up study was conducted to determine whether sari water filtration continued to be practiced by the same population of participants and, if it was, whether there would continue to be a beneficial effect of reduced incidence of cholera. The site of study is located within the Matlab Demographic Surveillance System of the International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR,B). The objective, simply stated, was to determine the sustainability and efficacy of filtration that was introduced earlier to the community.
RESULTS AND DISCUSSION
From the survey data, 2,207 (31%) of 7,233 interviewed respondents reported using a filter of any type and 1,327 (60%) of the filter users reported using cotton sari cloth (either one, two, three, or four layers of cloth). Within the original sari filter group, 635 (74%) of the filter users used sari cloth; of the 635, 117 (18%) used four layers of sari cloth for filtering, 157 (25%) used three layers, 271 (43%) used two layers, and 90 (14%) used one layer of cloth. Results of laboratory studies on which the intervention was based had previously shown that two and three layers of sari cloth were effective in removing up to 99% of the attached V. cholerae bacteria (10). The intervention recommended for prevention of cholera based on the laboratory study was four layers of sari cloth because it was slightly more effective in consistently removing ≥99% of the V. cholerae bacteria (10). In the original field trial, four layers of sari cloth were used and proved effective in reducing the incidence of cholera by ca. 50% (11). We found that 74% of those using sari cloth filters, whether one or more layers, in the follow-up study received a beneficial effect, even though filtration using the recommended four layers was practiced by only 18% of the population of the original group of villagers who had been taught to use a sari cloth filter. Among the 2,351 households originally assigned to the nylon filter group, 713 (30%) reported that they continued filtering their water, of which 342 (48%) used sari cloth. The numbers of households filtering water from the original different groups using sari cloth or any other material are shown in Table 1.
TABLE 1 .
Number of households filtering water
| Group | No. (%) of households using the following filter: |
Total no. of households | ||
|---|---|---|---|---|
| Sari | Nylon | Other | ||
| Sari filter | 635 (74.4) | 218 (25.6) | 853 | |
| Nylon filter | 342 (47.8) | 180 (25.3) | 191 (26.8) | 713 |
| Control | 350 (54.6) | 291 (45.4) | 641 | |
Of 2,426 households from the control group, i.e., those from the original study not receiving education and training about filtration, 641 (26%) used some kind of filter, of which 350 (55%) used 1 to 3 layers of sari cloth, but not 4 layers. People have been filtering water for aesthetic purposes, e.g., to remove leaves, insects, and other visible particulate matter from drinks sweetened with sugar or molasses (the latter are especially attractive to ants), but not for the purposes of water safety as they had been taught during the original field trial. In the follow-up of 11-hrs observation of 50 randomly selected households that reported they filtered their water with cotton sari cloth, only 19 (38%) were observed to consistently filter their water with sari cloth and only 2 (4%) folded the sari cloth into at least four layers. These data indicate that, although a reduced number of households continued to use sari filtration as originally recommended, i.e., four layers of sari cloth, overall, the use of some kind of filtration was practiced by 31% of the villagers, of which 60% used sari cloth. The rate of use of one or more layers of sari cloth showed that the number of villagers who were sari filter users (n = 853) surveyed from the original sari filtration group was significantly higher (74%) than the number from the control group (54%) (χ2 = 63.91; P < 0.001) of the original study, indicating the sustainability of the practice of filtering water 5 years after the intervention was introduced. It is unclear whether control households practicing sari filtration may have done so as a longstanding practice, but it is highly probable that diffusion of the practice of filtration from the original groups occurred based on observations made in the original study, when some of the villagers showed their neighbors how to filter water and they began to filter their water as well. From the results of this study, it is clear that the population taught to use sari filter comprised the largest number of sari filter users and fewer were from the control group (not taught to use a sari filter), indicating that training played an important role in the practice of sari filtration by these villagers. In addition, it is important to note that 25% (180/713) of the nylon filter group were still using the nylon filters provided 5 years earlier, although its effectiveness was not determined (Table 1). Eighteen percent of the sari filter group reported using four layers of sari cloth as filter, while only 1.1% of the control group used three layers and none used four layers. From the interview, we also determined that when villagers from the original study who had been instructed to use a single layer of the nylon filter switched to sari cloth filter, 76.3% of them continued to use one layer of sari cloth, as they were taught to do with the nylon filter, and only 0.6% used four layers. This is a clear indication of both compliance with instructions and the sustainability of the method, but it also shows the need for continuing education in the appropriate use and benefits of simple filtration.
Determining the sustainability of this method was the primary objective of the study. However, although not statistically significant, a reduced incidence (25%) of hospitalization for cholera was observed for the evaluation period (2003 to 2006) among households filtering their water compared to those households not filtering. With the lower rate of filtration in this follow-up study, it is not surprising that the observed reduction in disease rate was not as high as the 48% observed in the original trial (11), suggesting that active reinforcement would have been effective in ensuring higher protection.
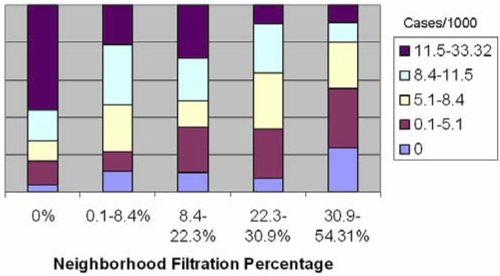
Additional analysis that was not part of the original study plan, was employed to explore the potential for indirect protection from cholera of households using sari cloth filtration, was done based on an earlier report (19). The percentage of villagers using some kind of filtration (sari, nylon, or gamcha, the local name for a thin towel) and living in proximity to participants of the original study was also calculated. Table 2 presents the 7,470 neighborhood clusters as five levels of cholera incidence (range, 0 to 33.3 per 1,000) stratified by neighborhood filtration percentage (range, 0 to 54.3%). Categories of approximately equal size were used, with zero values restricted to those neighborhoods with no cases as a separate category. Households not filtering water and located in neighborhoods where water filtration was not practiced were more likely to be in the highest incidence category (11.5 to 33.3 per 1,000). Households not filtering their water and in neighborhoods where water filtration was practiced (30.0 to 54.3%) rarely fell into the highest cholera incidence category and more than 50% of the time had an incidence rate lower than 5.1/1,000. This inverse relationship between neighborhoods where filtration was practiced and the incidence of cholera in the unprotected group is shown in Fig. 1. Figure 1 is a graphic presentation of data taken from Table 2 to illustrate the incidence of cholera by neighborhood filtration rate. The distribution shown is unlikely to have occurred by chance (chi-square statistic of 1,591.94; P ≤ 0.0001). Moreover, it is important to note that filtration was carried out by many households employing two or three layers of sari cloth, not the recommended four layers. Thus, this effect, although significant, could be further improved by reinforcement of the recommended practice.
TABLE 2 .
Neighborhood incidence of cholera in a total population of 7,470 relative to the number of cholera cases per 1,000 individuals not protected by water filtration
| Cholera incidence category (no. of cases of cholera/1,000) | No. (%) of cases of cholera in neighborhoods with a water filtration rate of: |
||||
|---|---|---|---|---|---|
| 0% | 0.1 to 8.4% | 8.4 to 22.3% | 22.3 to 30.9% | 30.9 to 54.3% | |
| 0 | 34 (3.8) | 178 (10.8) | 173 (10.51) | 118 (7.2) | 389 (23.6) |
| 0.1-5.1 | 114 (12.8) | 174 (10.6) | 398 (24.2) | 437 (26.6) | 523 (31.8) |
| 5.1-8.4 | 94 (10.6) | 415 (25.2) | 237 (14.4) | 495 (30.1) | 405 (24.6) |
| 8.4-11.5 | 150 (16.9) | 537 (32.6) | 371 (22.5) | 434 (26.4) | 173 (10.5) |
| 11.5-33.3 | 496 (55.9) | 342 (20.8) | 467 (28.4) | 161 (9.8) | 155 (9.4) |
FIG 1 .
Incidence of cholera in non-water-filtering households by neighborhood use of water filtration. The number of cases of cholera per 1,000 individuals (Cases/1000) is shown in the key to the right of the graph.
Examination of the practice of filtration relative to household socioeconomic status, measured by asset index (with the lowest quintile representing the lowest socioeconomic level and the highest quintile representing the most affluent) revealed a statistically significant negative association between socioeconomic status and the use of filtration. The most affluent quintile used filtration the least (22.1%), followed by the second most affluent group (28%), whereas the lowest, second lowest, and middle economic groups filtered their water the most with values of 34%, 36%, and 32%, respectively. Affluent people usually have the resources to boil their water or have access to safe drinking water, e.g., bottled water.
Interestingly, during the original trial, several families had to be removed from the control group because they became convinced filtration would protect their children from contracting cholera and began using sari filtration (11). The study team complied with their wishes for ethical reasons, despite its effect on the study. It is important to note that the filtration method did not require financial resources or extensive training on the part of the village women, and it was easy to include in their daily activity. Shallow tube well water, once considered a source of safe drinking water, has unfortunately been found to contain high levels of arsenic in many regions of Bangladesh, with the concentration of arsenic in the tube well water exceeding 50 ppb and concentrations 10 times higher in some areas of Bangladesh (15, 16). In the affected geographic regions, the population returned to surface water for household use, making simple filtration an important consideration.
In summary, the primary goal of this study was achieved, namely, to determine compliance in practicing simple filtration. Subsequent reduced incidence of cholera in the households filtering water was expected. Of the 2,456 women included in the original study who were taught to use sari cloth as a filter, 853 (35%) reported that they consistently used some kind of filter and 635 (26%) reported that they continued to use sari cloth filtration. A minority of the women who reported that they used sari filtration actually did so during the 11 h of structured observation, suggesting that, like other behavior changes, the practice of filtration would benefit from a focused effort to enhance its sustainability and provide a further reduction in the incidence of cholera. Sari filtration is easy to use, does not require extensive training, is socially acceptable, and, most importantly, involves no additional cost to the household. Where conditions of extreme poverty or local disasters prevent access to potable water, notably in areas where cholera is endemic and areas subject to social disruptions, simple filtration can be deployed with a beneficial outcome to public health.
MATERIALS AND METHODS
Study site.
The study, conducted in Matlab, Bangladesh, at the same location of the original sari filtration field trial, was carried out September 1999 through July 2002. The largest continuously operating Health and Demographic Surveillance System (HDSS) in the world, first established in 1966, is located in Matlab, Bangladesh, providing an eminently suitable site for both the original field trial and the present survey (14). The original field trial included a population of approximately 45,000 individuals (assigned in equal numbers to sari or nylon filtration groups and the control group) from a total population of more than 220,000 under the HDSS in Matlab, Bangladesh. In this follow-up study, a total of 7,470 village women responsible for collecting water for their household and available to participate in this study were selected from the original field trial population. Also, 772 neighboring households not part of the original study were also included to determine whether the practice of filtering diffused by social contact and had become part of the daily routine. In addition, 50 households were randomly selected 1 month after completion of the interviews from among the group of households reporting that they were using sari filtration. These households were subjected to structured observation designed to record systematically all water-related activities of each of the 50 households. Field staff members with experience in qualitative research and recruited from the community were educated on the topic of the research and trained to carry out the structured observation, with an anthropologist included in the research team overseeing the study.
Since village women begin their daily household activities, including collecting water for their family, in these rural Bangladesh villages early in the morning, structured observations began at 6 a.m. each day and continued until 5 p.m. As in the earlier study, the households observed were those with children under 5 years of age.
Sample size was calculated using a chi-square 2-by-2 table, where the total number of households was determined, but specific row and column totals were random, with the constraint that 50% of the study population filtered their water and that cases of cholera had been reported in 2.4% of the households over the previous 2-year period. An odds ratio of 1 under the null hypothesis and an odds ratio of 1.50 under the alternative were assumed. In the original study, an odds ratio closer to 2 had been observed. Because in that study the practice of filtration was reinforced by regular visits of staff, compliance in filtration in this follow-up study was not expected to be as high as in the original study.
In the Matlab HDSS study area, each household is assigned a unique identification (ID) code. Thus, every household included in the current study from the original filtration field trial could be identified. Covariates specific to each household, such as the number of children less than 5 years old, which treatment group (sari filter, nylon filter, or control) a given village was assigned to during the previous study, and other covariates were considered when explaining differences in cholera incidence between the households practicing filtration and those not practicing filtration.
In the original field trial performed in 1999 to 2002, a team of two field workers visited each participating household every 2 weeks on a regular basis during the entire period of the study (11). During this visit, the person responsible for collecting water was interviewed (with a set of questions in a questionnaire) to determine whether filtration was being practiced according to previously established instructions. The field workers examined the condition of the filter, and the filter was replaced if it was damaged. Any type of illness, including diarrhea, any difficulty in filtering when following the method taught, any travel by the family members to, or visitors from, other villages, or any major change in water use in the household was recorded, and records were maintained on a biweekly basis. In the present study, a similar survey instrument was employed. This survey or questionnaire included questions concerning personal demographics, level of education, socioeconomic status, water use, and illnesses other than those reported to the hospital, which are recorded by the ICDDR,B field hospital and available from that data bank. Most importantly, several of the questions were designed to determine water use behavior, namely, source of water, whether filtration or other treatment was employed, and frequency of use. It should be noted that the major difference in this study from the original was that each family was interviewed once during the 8 months of the survey. Hospital reports of confirmed cases of cholera, based on laboratory confirmation and covering a period of 4 years after completion of the original field trial, were examined to measure effectiveness, that is, severity of illness as recorded in the hospital records or hospitalization reports. Eight teams, each of which comprised two field workers, visited 10 households per day, requiring 8 months to complete the survey. To assess the validity of reported behavior, 50 households that reported using sari cloth filter in the interview were randomly selected and revisited 1 month later. This was a one-time revisit by a female observer who stayed with the family and observed all water-related activities during the day from 6 a.m. to 5 p.m.
Using the ICDDR,B geographic information system (GIS), households in close proximity to those households in Matlab, Bangladesh, drawing on a common source of water and included in the earlier study were also queried to determine whether diffusion of the innovation had occurred. Also, using GIS, the incidence of cholera was calculated for 7,470 non-water-filtering villagers in a 1-kilometer neighborhood cluster in the Matlab area, Bangladesh, employing a method described elsewhere (17–19). These 1-km Euclidean distance neighborhoods were used as proxy for the local-level area of influence of each household.
Data forms from the field workers, hospitals, and laboratories were scanned, and the data were entered into the computer at the Matlab Project Office. The results of the questionnaires were reviewed in detail, and if concerns were raised or additional information was required, the forms were returned to the specific field worker for correction and/or update. All data were entered in repositories at both the ICDDR,B and University of Maryland. All forms and data collection procedures were approved by the Institutional Review Board (IRB) at the ICDDR,B and the Western Institutional Review Board assigned by the University of Maryland.
ACKNOWLEDGMENTS
The original study to develop sari filtration was supported by the Thrasher Research Fund (grant no. 02903-3) and the field trial was supported by the National Institute of Nursing Research of the National Institutes of Health (grant RO 1 NR0427-01A1). This research activity was supported by the Thrasher Research Fund through the University of Maryland Biotechnology Institute to carry out the follow up study (grant GR-00443/01). We acknowledge with gratitude the commitment of the Thrasher Research Fund to the research efforts of the ICDDR,B. We are indebted to the Thrasher Research Fund (2005 to 2006) for generous support to carry out this follow-up study.
Footnotes
Citation Huq, A., M. Yunus, S. S. Sohel, A. Bhuiya, M. Emch, et al. 2010. Simple sari cloth filtration of water is sustainable and continues to protect villagers from cholera in Matlab, Bangladesh. mBio 1(1):e00034-10. doi:10.1128/mBio.00034-10.
REFERENCES
- 1. Colwell R., Huq A. 1994. Vibrios in the environment: viable but non-culturable Vibrio cholerae, p. 117–133 In Wachsmuth I., Blake P., Olsvik O., Vibrio cholerae and cholera: molecular to global perspectives. ASM Press, Washington, DC [Google Scholar]
- 2. WHO-UNICEF 2006. Meeting the MDG drinking water and sanitation target: the urban and rural challenge of the decade. WHO-UNICEF, Geneva, Switzerland [Google Scholar]
- 3. Clasen T., Schmidt W. P., Rabie T., Roberts I., Cairncross S. 2007. Interventions to improve water quality for preventing diarrhoea: systematic review and meta-analysis. BMJ 334:782–792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fewtrell L., Kaufmann R. B., Kay D., Enanoria W., Haller L., Colford J. M. J. 2005. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect. Dis. 5:42–52 [DOI] [PubMed] [Google Scholar]
- 5. Cash R., Music S., Libonati J., Snyder M., Wenzel R., Hornick R. 1974. Response of man to infection with Vibrio cholerae. I. Clinical, serologic, and bacteriologic responses to a known inoculum. J. Infect. Dis. 129:45–52 [DOI] [PubMed] [Google Scholar]
- 6. Hornick R. B., Music S. I., Wenzel R. 1971. The Broad Street pump revisited: response of volunteers to ingested cholera vibrios. Bull. N. Y. Acad. Med. 47:1181–1191 [PMC free article] [PubMed] [Google Scholar]
- 7. Colwell R. R. 1996. Global climate and infectious disease: the cholera paradigm. Science 274:2025–2031 [DOI] [PubMed] [Google Scholar]
- 8. Heidelberg J., Heidelberg K., Colwell R. 2002. Bacteria of the gamma-subclass Proteobacteria associated with zooplankton in Chesapeake Bay. Appl. Environ. Microbiol. 68:5498–5507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Huq A., Small E. B., West P. A., Huq M. I., Rahman R., Colwell R. R. 1983. Ecological relationships between Vibrio cholerae and planktonic crustacean copepods. Appl. Environ. Microbiol. 45:275–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Huq A., Xu B., Chowdhury M., Islam M., Montilla R., Colwell R. 1996. A simple filtration method to remove plankton-associated Vibrio cholerae in raw water supplies in developing countries. Appl. Environ. Microbiol. 62:2508–2512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Colwell R., Huq A., Islam M., Aziz K., Yunus M., Khan N., Mahmud A., Sack R., Nair G., Chakraborti J., Sack D., Russek-Cohen E. 2003. Reduction of cholera in Bangladesh villages by simple filtration. Proc. Natl. Acad. Sci. U. S. A. 100:1051–1055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Huq A., Sack R., Colwell R. 2001. Cholera and global environmental changes, p. 327–352 In Aron J., Patz J., Ecosystem change and public health—a global perspective. Johns Hopkins University Press, Baltimore, MD. [Google Scholar]
- 13. Sobsey M. D., Stauber C. E., Casanova L. M., Brown J. M., Elliott M. A. 2008. Point of use household drinking water filtration: a practical, effective solution for providing sustained access to safe drinking water in the developing world. Environ. Sci. Technol. 42:4261–4267 [DOI] [PubMed] [Google Scholar]
- 14. Aziz K. M. A., Mosley W. H. 1994. Historical perspective and methodology of the Matlab project, p. 29–50 In Fauveau V., Matlab: women, children and health. ICDDR, Dhaka, Bangladesh [Google Scholar]
- 15. Smith A., Lingas E., Rahman M. 2000. Contamination of drinking-water by arsenic in Bangladesh: a public health emergency. Bull. World Health Organ. 78:1093–1103 [PMC free article] [PubMed] [Google Scholar]
- 16. Van Geen A., Ahsan H., Horneman A., Dhar R., Zheng Y., Hussain I., Matin K., Gelman A., Stute M., Simpson H., Wallace S., Small C., Parvez F., Slavkovich V., Lolacono N., Becker M., Cheng Z., Momotaj H., Shanewaz M., Seddique A., Graziano J. 2002. Promotion of well-switching to mitigate the current arsenic crisis in Bangladesh. Bull. World Health Organ. 80:732–737 [PMC free article] [PubMed] [Google Scholar]
- 17. Ali M., Emch M., Von Seidlein L., Yunus M., Sack D. A., Rao M., Holmgren J., Clemens J. D. 2005. Herd immunity conferred by killed oral cholera vaccines in Bangladesh: a reanalysis. Lancet 366:44–49 [DOI] [PubMed] [Google Scholar]
- 18. Emch M., Ali M., Acosta C., Yunus M., Sack D. A., Clemens J. D. 2007. Efficacy calculation in randomized trials: global or local measures? Health Place 13:238–248 [DOI] [PubMed] [Google Scholar]
- 19. Emch M., Ali M., Park J. K., Yunus M., Sack D. A., Clemens J. D. 2006. Relationship between neighbourhood-level killed oral cholera vaccine coverage and protective efficacy: evidence for herd immunity. Int. J. Epidemiol. 35:1044–1050 [DOI] [PubMed] [Google Scholar]