Abstract
What we eat, when and how much, all are influenced by brain reward mechanisms that generate ‘liking’ and ‘wanting’ for foods. As a corollary, dysfunction in reward circuits might contribute to the recent rise of obesity and eating disorders. Here we assess brain mechanisms known to generate ‘liking’ and ‘wanting’ for foods, and evaluate their interaction with regulatory mechanisms of hunger and satiety, relevant to clinical issues. ‘Liking’ mechanisms include hedonic circuits that connect together cubic-millimeter hotspots in forebrain limbic structures such as nucleus accumbens and ventral pallidum (where opioid/endocannabinoid/orexin signals can amplify sensory pleasure). ‘Wanting’ mechanisms include larger opioid networks in nucleus accumbens, striatum, and amygdala that extend beyond the hedonic hotspots, as well as mesolimbic dopamine systems, and corticolimbic glutamate signals that interact with those systems. We focus on ways in which these brain reward circuits might participate in obesity or in eating disorders.
Introduction
Palatable foods and their cues can carry motivational power. The sight of a cookie or the smell of a favorite food may evoke a sudden urge to eat, and a few bites of a tasty morsel can spur an urge to eat more (“l’appétit vient en mangeant” as the French phrase goes). In a food-rich world, cue-triggered urges contribute to the likelihood that a person will eat right now, or over-eat at a meal, even if one intended to abstain or to only eat moderately. By influencing choices of whether, when, what, and how much to eat, cue-triggered urges contribute bit by bit to long term caloric overconsumption and obesity (Berthoud and Morrison, 2008; Davis and Carter, 2009; Holland and Petrovich, 2005; Kessler, 2009).
It’s not just the food or cue by itself that exerts this motivating power: it’s the response of the perceiver’s brain to those stimuli. For some individuals, brain systems may especially react to generate compelling motivation to overeat. For everyone, evoked urges may become particularly strong at certain moments of the day, and when hungry or stressed. The variation in motivational power from person to person and from moment to moment arises in part from the dynamics of brain reward circuits that generate ‘wanting’ and ‘liking’ for food reward. Those reward circuits are the topic of this paper.
Where does food pleasure or temptation come from? Our fundamental starting point is that the temptation and pleasure of sweet, fatty, or salty foods arise actively within the brain, not just passively from physical properties of foods themselves. ‘Wanting’ and ‘liking’ reactions are actively generated by neural systems that paint the desire or pleasure onto the sensation - as a sort of gloss painted on the sight, smell or taste (Table 1). A tempting chocolate cake is not so much necessarily pleasant, but our brains are biased to actively generate ‘liking’ to its chocolaty creaminess and sweetness. The sweetness and creaminess are keys that potently unlock the generating brain circuits which apply pleasure and desire to the food at the moment of encounter (Berridge and Kringelbach, 2008; James, 1884; Kringelbach and Berridge, 2010). Yet it is the opening of the brain locks that is most crucial, not just the keys themselves, and so we focus here on understanding the brain’s hedonic and motivational locks.
Table 1. Key reward terms.
Definitions of some ‘wanting’ and ‘liking’ terms.
| Reward Terms |
|---|
| Food Reward: A composite process that contains ‘liking’ (hedonic impact), ‘wanting’ (incentive motivation), a learning (associations and predictions) as major components. Normally all occur together but the three psychological components have separable brain systems, which permits dissociation among them in some conditions. |
| Hedonic hotspot: A specific brain site that is capable of amplifying pleasure ‘liking’ reactions when neurochemically stimulated. Hedonic hotspots have so far been found in nucleus accumbens, ventral pallidum, and the brainstem. Each is about 1 mm3 in volume in rats (presumably closer to 1 cm in humans), where opioid, endo-cannabinoid, benzodiazepine-GABA, or orexin neurochemical signals amplify the hedonic impact of palatable foods. Applied to eating disorders, dysfunction in a hedonic hotspot is hypothesized to alter the hedonic impact of foods and so change food consumption. |
| ‘Liking’ (with quotation marks): An objective hedonic reaction detected in behavior or neural signals, and generated chiefly by subcortical brain systems. A ‘liking’ reaction to sweetness produces conscious pleasure by recruiting additional brain circuits, but a core ‘liking’ reaction can sometimes occur without subjective pleasure. |
| Liking (without quotation marks): The everyday sense of the word as a subjective conscious feeling of pleasurable niceness. |
| ‘Wanting’ (with quotation marks): Incentive salience, or motivation for reward typically triggered by reward- related cues. Attribution of incentive salience to the representations makes a cue and its reward more attractive, sought after, and likely to be consumed. Brain mesolimbic systems, especially those involving dopamine, are especially important to ‘wanting’. ‘Ordinarily ‘wanting’ occurs together with other reward components of ‘liking’ and learning, and with subjective desires, but can be dissociated both from other components and subjective desire under some conditions. |
| Wanting (without quotation marks): A conscious, cognitive desire for a declarative goal in the ordinary sense of the word wanting. This cognitive form of wanting involves additional cortical brain mechanisms beyond the mesolimbic systems that mediate ‘wanting’ as incentive salience. |
| Wanting’ without ‘liking’: For example, in addictive incentive-sensitization, a mechanism of drug addiction that leads to compulsive levels of ‘wanting’ for drugs. Mediated by changes in brain dopamine-related mesolimbic systems, sensitized ‘wanting’ can rise even if ‘liking’ declines for the same reward. Hypothetically, if a similar brain mechanism applies to obesity and eating disorders, some individuals could compulsively crave and seek food, but not derive higher pleasure from it. |
Active brain generation is evident by considering that hedonic biases are not fixed but rather are plastic. Even a once- ‘liked’ sweet taste can become unpleasant in some circumstances while remaining sweet as ever. For example, a particular novel sweet taste can be first perceived as nice, but then become disgusting after that taste has been associatively paired with visceral illness to create a learned taste aversion (Garcia et al., 1985; Reilly and Schachtman, 2009; Rozin, 2000). Conversely, a nastily intense salty taste can switch from unpleasant to pleasant, in moments of salt appetite, in which the body lacks sodium (Krause and Sakai, 2007; Tindell et al., 2006). And similarly, although our brains are biased to perceive bitter tastes as especially unpleasant, hedonic plasticity allows many individuals to find the tastes of cranberries, coffee, beer, or other bitter foods quite pleasant once cultural experience has made their bitterness into a key for hedonic brain systems. More transiently but universally, hunger makes all foods more highly ‘liked’, while satiety states dampen ‘liking’ at different times in the same day, a dynamic hedonic shift called ‘alliesthesia’ (Cabanac, 1971).
Roles of brain reward systems in growing rates of obesity?
The incidence of obesity has risen markedly in the past three decades in the USA, so that today nearly 1 in 4 Americans may be considered to be obese (Prevention, 2009). The rise in body weight may be due mostly to the fact that people are simply eating more calories of food, rather than because they are exercising less (Swinburn et al., 2009). Why might people be eating more food now? Of course, there are several reasons (Brownell et al., 2009; Geier et al., 2006; Kessler, 2009). Some experts have suggested that modern temptations to eat and keep on eating are stronger than in the past because contemporary foods contain on average higher levels of sugar, fat, and salt. Modern treats are also easy to obtain at any moment in a nearby refrigerator, vending machine, fast-food restaurant, etc. Cultural traditions that once limited snacking are diminished, so that people eat more outside of meals. Even within meals, the size of portions is often larger than optimal. All of these trends may play into the normal biases of brain reward systems in ways that let us succumb to the desire to eat more.
Brain ‘liking’ and ‘wanting’ systems that respond to these factors are essentially pure ‘go’ systems. They are activated by tasty treats and related cues. While ‘go systems’ can be diminished by satiety influences, they never generate a strong ‘stop’ signal to halt intake, they merely tone down the intensity of the ‘go’. It is hard to turn some ‘go systems’ completely off. For example, a study in our lab once found that even the super-satiety induced by dribbling milk or sucrose solution into the mouths of rats until they consumed nearly 10% of their body weight in a half-hour session, reduced but did not abolish their hedonic ‘liking’ reactions to sweetness immediately afterwards, and never actually converted ‘liking’ into a negative ‘disliking’ gape (Berridge, 1991). Likewise in humans, strong satiation on chocolate by asking people to eat over two whole bars suppressed liking ratings to near zero but did not push ratings into a negative unpleasant domain, even if wanting ratings fell further (Lemmens et al., 2009; Small et al., 2001). There are counter-examples of actual negative ratings for sweetness after satiety too, but given the factors that complicate rating scales (Bartoshuk et al., 2006), it may still be safe to conclude that food pleasure is hard to completely eliminate. You may experience this yourself when you find that desserts remain appealing even after a large meal. And when hungry, of course, palatable foods become even more attractive.
These temptations face everyone. And the more palatable the foods available and the more plentiful their cues in our environment, the more the hedonic ‘liking’ and ‘wanting’ systems in brains generate a ‘go.’ It does not require pathology to overindulge. So what accounts for why some people do over-consume whereas others do not? Mere slight individual differences in reward system reactivity could play a part in incrementally producing obesity in some, as will be considered below. Of course, in cases of more extreme eating patterns, further explanations will be needed.
Potential roles of brain reward systems in obesity and eating disorders
Different cases of obesity will have different underlying causes, and scientific explanations probably cannot be ‘one size fits all’. To aid the classification of individual and types of overeating, here are several ways in which brain reward systems might relate to obesity and related eating disorders.
Reward dysfunction as cause
First, it is possible that some aspects of brain reward function go wrong to cause overeating or a particular eating disorder. Foods might become hedonically ‘liked’ too much or too little via reward dysfunction. For example, pathological over-activation of the opioid or endocannabinoid hedonic hotspots in nucleus accumbens and ventral pallidum described below could cause enhanced ‘liking’ reactions to taste pleasure in some individuals. Excessive activation of ‘liking’ substrates would magnify the hedonic impact of foods, making an individual both ‘like’ and ‘want’ food more than other people, and so contribute to binge eating and obesity (Berridge, 2009; Davis et al., 2009). Conversely, a suppressive form of hotspot dysfunction might conceivably reduce ‘liking’ in anorexia-type eating disorders (Kaye et al., 2009).
Even without pleasure dysfunction, another possibility for distorted reward is that ‘wanting’ to eat might rise alone, if incentive salience detaches from hedonic ‘liking’ (Finlayson et al., 2007; Mela, 2006). Dissociation of ‘wanting’ from ‘liking’ in certain disorders is conceivable because the brain appears to generate ‘wanting’ and ‘liking’ via separable mechanisms, as described below. Cues for palatable food could still evoke excessive ‘wanting’ and consumption even if no longer directly hedonically driven, perhaps via hyper-reactivity in mesocorticolimbic dopamine-glutamate mechanisms of incentive salience (or related CRF or opioid circuits that potentiate these mechanisms). In such cases, the sight, smell, or vivid imagination of food could trigger a compulsive urge to eat, even though the person would not find the actual experience more than ordinarily pleasurable in the end. All of these possibilities have been suggested at one time or another. Each of them deserves consideration because different answers might apply to different disorders or different types of obesity.
Passively distorted reward function as consequence
A second category of possibilities is that brain reward systems might not be the initial cause of disordered eating, but still come to function abnormally as a passive, secondary reaction to excessive food experience, abnormal intake or extra body weight. In such cases, brain systems of ‘liking’ and ‘wanting’ might well attempt to function normally, but appear to be abnormal in neuroimaging studies, and so become a potential red herring to researchers. Still, even passively distorted reward functions could yet provide windows of opportunity for treatments that aim to correct eating behavior in part by modulating reward function back within normal range.
Normal resilience in brain reward
Third, it is possible that in many cases brain reward systems will continue to function normally in obesity or an eating disorder, and not change even secondarily. In such cases, the causes of eating disorder would then lay completely outside brain reward functions. Indeed, brain reward functions might even serve as aids to eventually help spontaneously normalize some eating behavior patterns even without treatment.
Does theory matter? Implications for clinical outcomes and therapy
The answer to which of these alternative possibilities is best may well vary from case to case. Different types of disordered eating may require different answers. Perhaps even different individuals with the ‘same’ disorder will need different answers, at least if there are distinct subtypes within the major types of eating disorders as well as within obesity (Davis et al., 2009).
Which answer above is true about a particular eating disorder or type of obesity carries implications for what treatment strategy might be best. For example, should one try to restore normal eating by reversing brain reward dysfunction via medications? That would be appropriate if reward dysfunction is the underlying cause. Or should one use drugs instead only as compensating medications, not cures? Then a medication might aim to boost aspects of brain reward function and so correct eating, even while not addressing the original underlying cause. That could be a bit similar to using aspirin to treat pain, even though the original cause of pain was not a deficit in endogenous aspirin. Even just treating the symptom can still be helpful.
Or instead should treatment be focused entirely on mechanisms that are unrelated to food reward? That might be the best choice if brain reward systems simply remain normal in all cases of eating disorders, and thus perhaps essentially irrelevant to the expression of pathological eating behavior.
Placing these alternatives side by side helps illustrate that there are therapeutic implications that would follow from a better understanding of brain reward systems and their relations to eating patterns. Only if one knows how food reward is processed normally in the brain will we be able to recognize pathology in brain reward function. And only if one can recognize reward pathology when it occurs will one be able to design or choose the best treatment.
Underlying brain reward systems for food ‘liking’ and ‘wanting’
These considerations provide grounds for trying to understand the brain mechanisms that generate ‘liking’ and ‘wanting’ for foods, and how they are modulated by hunger and satiety. This next section turns to recent findings regarding the basic brain systems of food pleasure and desire.
‘Wanting’ as separate from ‘liking’
It is possible that sometimes brain systems of ‘wanting’ can motivate increases in consumption even if hedonic ‘liking’ does not rise. By ‘wanting’, we refer to incentive salience, a fundamental type of incentive motivation (Figure 1). ‘Wanting’ most relevantly influences food intake, but is also much more. Incentive salience can be conceived as a mesolimbically-generated tag for perceptions and representations in the brain of particular stimuli, especially those that have Pavlovian associations with reward. The attribution of incentive salience to a reward stimulus representation makes that stimulus attractive, attention grabbing, sought after and ‘wanted.’ The stimulus effectively becomes a motivational magnet that pulls appetitive behavior toward itself (even if it is only a Pavlovian cue for the reward), and makes the reward itself more ‘wanted’.
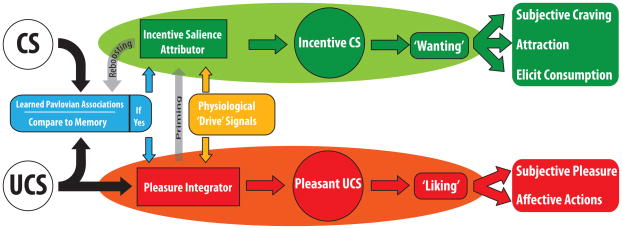
Figure 1.
Model of incentive motivation that separates reward ‘wanting’ (incentive salience) from ‘liking’ (hedonic impact of sensory pleasure). This model of incentive salience was originally proposed by Robinson and Berridge (1993), derived from incentive motivation concepts of Toates (1986) and Bindra (1978), and was recently translated into computational form by Zhang et al. (2009). Normal hunger acts as a physiological ’drive’ signal to magnify the incentive’ wanting’ and hedonic ‘liking’ triggered by tasty foods and their associated cues, whereas satiety dampens the multiplicative impact of cues and foods. Relevant to obesity, individuals with endogenously reactivity higher in mesolimbic circuits would have higher incentive salience for foods, and possibly higher hedonic impact, leading to greater ‘wanting’ and-or ‘liking’ to eat, in ways that would promote obesity.
When attributed to the smell emanating from cooking, incentive salience can rivet a person’s attention and trigger sudden thoughts of eating - and perhaps even vividly imagining the food can do so in the absence of a physical smell. When attributed by rats to a cue for sugar reward, incentive salience may make the object cue appear rather food-like to the perceiver, even causing the animal to frenziedly try to eat the cue that is only an inedible metal object (especially if the rat’s brain is in a state of limbic activation to magnify the ‘wanting’ attribution) (Flagel et al., 2008; Jenkins and Moore, 1973; Mahler and Berridge, 2009; Tomie, 1996).
Incentive salience or ‘wanting’ is quite distinct from more cognitive forms of desire meant by the ordinary word, wanting, which involve declarative goals or explicit expectations of future outcomes and which are largely mediated by cortical circuits. Incentive salience has a much closer dependence on cues and physical reward stimuli (or at least imagery of cues and stimuli), yet no need for clear cognitive expectations of future ‘wanted’ outcomes that are mediated by more cortically-weighted brain circuits.
A cue’s incentive salience power depends on the state of the brain that encounters it, as well as on prior associations with a food reward (Figure 1). ‘Wanting’ is produced by a synergistic interaction between the current neurobiological state (including appetite states) and the presence of foods or their cues. Neither a food cue by itself nor mesolimbic activation by itself is very powerful. But together in the right combinations they are motivationally compelling in a synergy that is greater than the sum of the parts (Zhang et al., 2009).
That synergistic relationship means that ‘wanting’ suddenly rises when a food cue is encountered in a mesolimbically primed state (or if cues are vividly imagined then). Cue presence is important because a cue carries a high association with food reward. Physiological hunger or mesolimbic reactivity is important because the motivating power of a cue encounter changes with hunger or satiety (or may vary across individuals due to differences in their brains)(Zhang et al., 2009).
Producing ‘wanting’ without ‘liking’
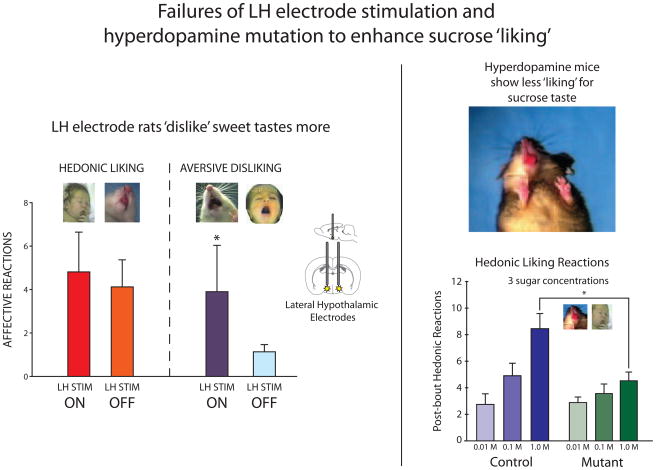
The most dramatic demonstrations of incentive salience as a distinct entity come from cases in which ‘wanting’ has been neurally enhanced alone, without raising hedonic ‘liking’ for the same reward. Our first discovery of enhanced ‘wanting’-without-‘liking’ came two decades ago from a study on eating evoked by electrical stimulation of the lateral hypothalamus in rats, conducted collaboratively with Elliot Valenstein (Berridge and Valenstein, 1991). Activation of an electrode in the lateral hypothalamus causes stimulated rats to eat voraciously (Valenstein et al., 1970), and such electrodes activate brain circuits that typically include mesolimbic dopamine release (Hernandez et al., 2008). The same electrode stimulation is typically sought out by the animals as a reward, and electrode activation had been hypothesized to induce eating by increasing the hedonic impact of the food. Did the stimulated rats truly ‘want’ to eat more because they ‘liked’ food more? Perhaps surprisingly at first, the answer turned out to be ‘no’: activation of the hypothalamic electrode completely failed to enhance ‘liking’ reactions to sucrose (such as lip licking, described in detail below), though the stimulation made the rats eat twice as much food as normal (Berridge and Valenstein, 1991)(Figures 2 & 3.) Instead of increasing ‘liking’, the electrode only enhanced ‘disliking’ reactions (such as gapes) to sucrose taste, as though, if anything, the sucrose became slightly unpleasant. This and subsequent dissociations of ‘wanting’ from ‘liking’ points to the need to identify separate neural substrates for each. We will next describe brain systems of food ‘wanting’ versus ‘liking’, and then consider how these systems relate to other regulatory systems.
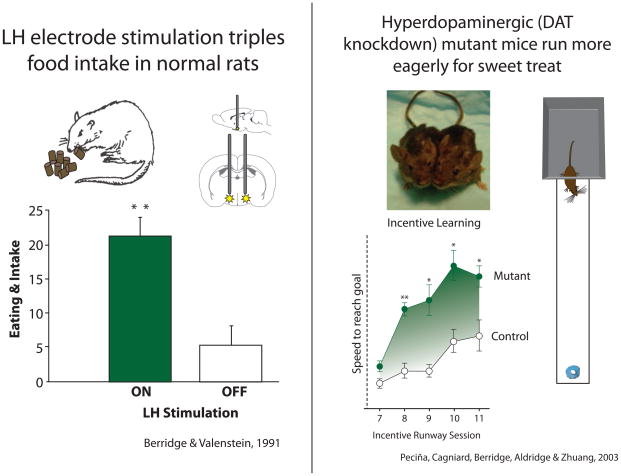
Figure 2. ‘Wanting’ enhancements caused by hypothalamic stimulation or by dopamine elevation.
Electrical stimulation of the lateral hypothalamus makes rats eat triple the amount they ordinarily consume (left). Elevation of extra-synaptic dopamine by knockdown of the gene that codes the dopamine transporter makes mutant mice run more eagerly to obtain a sweet Frootloop treat than their control wild-type counterparts (both shown in photo; right). Modified from Berridge and Valenstein (1991) and from Pecina et al. (2003).
Figure 3. ‘Liking’ for sweetness is never enhanced by hypothalamic electrodes or by dopamine elevation.
Turning on stimulation of lateral hypothalamic electrodes in the same rats as in Figure 4 causes more ‘disliking’ reactions (e.g., gapes) to sucrose, while not altering positive ‘liking’ reactions (e.g., lip licks), even though the stimulation made the same rats avidly eat more food. Elevation of dopamine in mutant mice only suppresses positive ‘liking’ reactions to sucrose at the highest concentration (while not altering lower ‘liking’ for dilute sucrose solution; aversive reactions were not observed and are not shown), even though the mutants ‘wanted’ sweet rewards more than control wild-type mice. Modified from Berridge and Valenstein (1991) and from Pecina et al. (2003).
Mesolimbic dopamine in ‘wanting’ without ‘liking’
The mesolimbic dopamine system is probably the best known neural substrate able to enhance ‘wanting’ without ‘liking’. Dopamine activation is evoked by pleasant foods, other hedonic rewards, and reward cues (Ahn and Phillips, 1999; Di Chiara, 2002; Hajnal and Norgren, 2005; Montague et al., 2004; Norgren et al., 2006; Roitman et al., 2004; Roitman et al., 2008; Schultz, 2006; Small et al., 2003; Wise, 1985). Dopamine has often been called a pleasure neurotransmitter for such reasons, but we believe dopamine fails to live up to its traditional hedonic name.
In two decades of animal studies that manipulated dopamine’s causal role, we’ve consistently found that dopamine fluctuation failed to change ‘liking’ for the hedonic impact of food rewards after all, even when ‘wanting’ for food is profoundly changed. For example, too much dopamine in the brain of mutant mice whose gene mutation causes extra dopamine to remain in synapses (knockdown of dopamine transporter) produces elevated ‘wanting’ for sweet food rewards, but no elevation in ‘liking’ expressions to sweetness (Peciña et al., 2003)(Figure 2 & 3). Similar elevations of ‘wanting’ without ‘liking’ have also been produced in ordinary rats by amphetamine-induced elevation in dopamine release, and by long term drug-sensitization of mesolimbic systems (Peciña et al., 2003; Tindell et al., 2005; Wyvell and Berridge, 2000).
Conversely, mutant mice that lack any dopamine in their brains at all remain able to still register the hedonic impact of sucrose or food rewards, in the sense that they are still able to show preferences, and some learning, for a palatable sweet reward (Cannon and Palmiter, 2003; Robinson et al., 2005). Similarly, taste reactivity studies in rats have shown that dopamine suppression by pimozide (dopamine antagonist) administration or even by massive destruction of 99% of mesolimbic and neostriatal dopamine neurons (by 6-OHDA lesions) does not suppress taste ‘liking’ facial expressions elicited by the taste of sucrose (Berridge and Robinson, 1998; Peciña et al., 1997). Instead, the hedonic impact of sweetness remains robust even in a nearly dopamine-free forebrain.
Several neuroimaging studies of humans have similarly found that dopamine levels may correlate better with subjective ratings of wanting for a reward than with pleasure ratings of liking the same reward (Leyton et al., 2002; Volkow et al., 2002). In related human studies, drugs that block dopamine receptors may completely fail to reduce the subjective pleasure ratings that people give to a reward (Brauer and De Wit, 1997; Brauer et al., 1997; Leyton, 2010; Wachtel et al., 2002).
Still, there remain today some echoes of the dopamine = hedonia hypothesis in the neuroimaging literature and in related studies on levels of dopamine D2 receptor binding (Geiger et al., 2009; Wang et al., 2001). For example, some PET neuroimaging studies have suggested that obese people may have lower levels of dopamine D2 receptor-binding in their striatum (Wang et al., 2001; Wang et al., 2004b). If dopamine causes pleasure, then by the dopamine = hedonia hypothesis, reduced dopamine receptors could reduce the pleasure they get from food. The reduced pleasure has been suggested to cause those individuals to eat more to attain a normal amount of pleasure. This has been called a reward deficiency hypothesis for overeating (Geiger et al., 2009).
It is important to note first that there may be something of a logical difficulty with an anhedonia-driven hypothesis for overeating. It seems to require the assumption that people will eat more of food when they don’t like it than when they do. If that were true, people on a diet of unpalatable gruel might eat more than, say, people whose diet included ice cream, cake and potato chips. Instead of course, humans and rats alike tend to eat less of food that is unpalatable, and to seek and eat more when available foods are more palatable (Cooper and Higgs, 1994; Dickinson and Balleine, 2002; Grigson, 2002; Kelley et al., 2005b; Levine and Billington, 2004). If dopamine deficiency caused all food to taste less good, people might be expected to eat less overall rather than more, at least if palatability directly promotes consumption as it so often seems to. The empirical facts about eating and palatability seem to point in an opposite direction from what is presumed by dopamine anhedonia formulations of obesity. This logical puzzle flags the explanatory contradictions that can plague a reward deficiency hypothesis.
Therefore alternatives are worth entertaining. One alternative, involving a reverse, interpretation of reduced dopamine D2 binding in obese people is that the receptor availability reduction is a consequence of overeating and obesity, rather than its cause (Davis et al., 2004). Neurons in mesocorticolimbic circuits may respond with homeostatic adjustments to regain normal parameters when pushed by prolonged excessive activations. For example, prolonged exposure to addictive drugs eventually causes dopamine receptors to reduce in number, even if levels were normal to begin with – this is a down-regulation mechanism of drug tolerance and withdrawal (Koob and Le Moal, 2006; Steele et al., 2009). It is conceivable that if some obese individuals had similar sustained over-activation of dopamine systems, eventual down-regulation of dopamine receptors might result.
If that happened, the dopamine suppression might fade once the excessive body weight or excessive reward consumption was stopped. New evidence relevant to this alternative possibility has appeared in a recent PET neuroimaging study, which found that Roux-en-Y gastric bypass surgery, which resulted in weight loss of about 25 lbs after 6 weeks in obese women weighing over 200 lbs, produced a concomitant post-surgical rise in their striatal dopamine D2 receptor binding, roughly proportional to the amount of weight lost (Steele et al., 2009). A rise in dopamine receptor levels after weight loss is more compatible with the idea that the obesity condition caused the previous lower level of dopamine receptors, rather than that an innate dopamine deficit or reward deficiency caused the obesity. In sum, while more remains to be known before a conclusive resolution of this issue can be obtained, there are grounds for caution regarding the idea that reduced dopamine causes anhedonia which causes overeating.
Paradoxical anorectic effects of dopamine (and hyperphagic effects of dopamine blockade)?
Still, there remain inconvenient facts for our hypothesis that dopamine mediates food ‘wanting’, and those facts should be acknowledged too. One inconvenient fact is that atypical antipsychotics that block D2 receptors can increase caloric intake and induce weight gain (Cope et al., 2005; Stefanidis et al., 2009). However, an explanation for this may largely come from blockade by the same antipsychotics of serotonin 1A and 2C receptors, and the histamine H1 receptor, which may correlate better with weight gain than D2 occupancy (Matsui-Sakata et al., 2005).
Perhaps the most important inconvenient fact is that dopamine is reported to have anomalous and opposite role in suppressing appetite, as in the action of well known dieting drugs. At least, systemic amphetamine and chemically-related stimulants that promote dopamine and norepinephrine reliably suppress appetite and intake. However, at least some anorectic effects of amphetamine may actually be attributable to norepinephrine release, which has particular appetite suppressing roles in the medial hypothalamus, perhaps by stimulating alpha-1 –adrenoreceptors (opposite to hyperphagic effects of alpha-2 receptors)(Adan et al., 2008; Wellman et al., 1993). Also, it is important to note that dopamine itself may have different effects on intake in different brain structures, and also at different intensities even in a single structure (Cannon et al., 2004; Kuo, 2003). For example, dopamine has anorectic effects in the hypothalamic arcuate nucleus, in part possibly by reducing neuropeptide Y (Kuo, 2003), and high levels of dopamine may have anorectic effects also in the nucleus accumbens and neostriatum, even though lower levels of dopamine elevation there can facilitate intake and ‘wanting’ for food (Cannon et al., 2004; Evans and Vaccarino, 1986; Inoue et al., 1997; Pal and Thombre, 1993; Wise et al., 1989). Finally, it is also important to note that dopamine’s enhancements of incentive salience are often directed to conditioned stimuli for rewards – allowing the cue’s to trigger ‘wanting’ for reward that leads to pursuit, rather than directly extending meal size and food consumption (Pecina et al., 2006; Smith et al., 2007; Wolterink et al., 1993; Wyvell and Berridge, 2000; Wyvell and Berridge, 2001). Dopaminergic cue-triggered ‘wanting’ could make an individual succumb to a temptation to eat, and once the meal is begun other (e.g., opioid) brain mechanisms could extend meal size from there. In general, dopamine’s role in intake is not exclusively up or down, but rather may vary in different brain systems and under different psychological conditions.
Brain systems for food ‘liking’
At the heart of reward is hedonic impact or pleasure ‘liking’. Many brain sites are activated by food pleasures. Sites activated by pleasant foods include regions of the neocortex such as the orbitofrontal cortex, the anterior cingulate cortex and the anterior insula cortex (de Araujo et al., 2003; Kringelbach, 2004; Kringelbach, 2005; Kringelbach, 2010; O’Doherty et al., 2001; Petrovich and Gallagher, 2007; Rolls, 2006; Rolls et al., 2003; Small and Veldhuizen, 2010; Small et al., 2001; Small et al., 2003). Pleasure-activated sites also include subcortical forebrain structures such as the ventral pallidum, nucleus accumbens, and amygdala, and even lower brainstem systems such as mesolimbic dopamine projections and the parabrachial nucleus of the pons (Aldridge and Berridge, 2010; Berns et al., 2001; Cardinal et al., 2002; Craig, 2002; Everitt and Robbins, 2005; Kringelbach, 2004; Kringelbach et al., 2004; Kringelbach, 2010; Levine et al., 2003; Lundy, 2008; O’Doherty et al., 2002; Pelchat et al., 2004; Rolls, 2005; Schultz, 2006; Small and Veldhuizen, 2010; Small et al., 2001; Volkow et al., 2002; Wang et al., 2004a).
In the cortex, the orbitofrontal region of the prefrontal lobe in particular codes taste and smell pleasure. The clearest fMRI demonstrations of hedonic coding may come from the work of Kringelbach and colleagues (de Araujo et al., 2003; Kringelbach, 2004; Kringelbach, 2005; Kringelbach, 2010). Within the orbitofrontal cortex, the primary site for hedonic coding appears to be located in a mid-anterior position, where fMRI activation discriminates pleasantness from sensory properties of food stimuli, and most importantly, tracks changes in the pleasantness of a particular food stimulus caused by alliesthesia or sensory-specific satiety (Kringelbach et al., 2003; O’Doherty et al., 2001). For example, when people were sated by drinking a liter of chocolate milk the pleasure of that beverage selectively dropped, and this drop was tracked by reduced activation in the mid-anterior orbitofrontal cortex, while the pleasure and neural activation to tomato juice, which had not been consumed, remained relatively unaltered (Kringelbach et al., 2003).
However, it is important to note that not all brain activations that code food pleasure necessarily cause or generate the pleasure (Kringelbach and Berridge, 2010). As a general rule, there are more codes for pleasure in the brain than causes of it. Other brain activations are likely to be secondary, and in turn could cause motivation, learning, cognition or other functions consequent to the pleasure. In particular, it is not yet clear whether orbitofrontal or other cortical activations play strong roles in actually causing the food pleasures they code, or instead some other functions (Berridge and Kringelbach, 2008; Kringelbach and Berridge, 2010; Smith et al., 2010).
Brain causation of pleasure can be identified only by manipulating the activation of a specific brain substrate and finding a consequential change in the pleasure corresponding to that change in activation. We have approached hedonic causation in our laboratory by searching for brain manipulations that cause an increase in psychological and behavioral ‘liking’ reactions to pleasant foods. A useful behavioral ‘liking’ reaction that is employed in our studies to measure food pleasure and its causation is the affective orofacial expressions that are elicited by the hedonic impact of sweet tastes. These facial ‘liking’ reactions were described originally in human infants by Jacob Steiner and extended to rats by Harvey Grill and Ralph Norgren, working with Carl Pfaffmann (Grill and Norgren, 1978b; Pfaffmann et al., 1977; Steiner, 1973; Steiner et al., 2001). For example, sweet tastes elicit positive facial ‘liking’ expressions (rhythmic and lateral tongue protrusions that lick the lips, etc.) in human infants and in rats, whereas bitter tastes instead elicit facial ‘disliking’ expressions (gapes, etc.) (Figure 4 & 5). Confirming the hedonic nature, changes in these affective facial reactions specifically track changes in sensory pleasure induced by hunger/satiety alliesthesia, learned preferences or aversions, and brain shifts (Berridge and Schulkin, 1989; Berridge, 1991; Cabanac and Lafrance, 1990; Cromwell and Berridge, 1993; Grill and Norgren, 1978a; Kerfoot et al., 2007; Parker, 1995; Peciña et al., 2006). Facial ‘liking’ reactions are homologous between humans and other mammals (Berridge and Schulkin, 1989; Berridge, 1990; Berridge, 2000; Steiner et al., 2001) which implies that what is learned about brain mechanisms of pleasure causation in animal studies is useful for understanding pleasure generation in humans too (Berridge and Kringelbach, 2008; Kringelbach and Berridge, 2010; Smith et al., 2010).
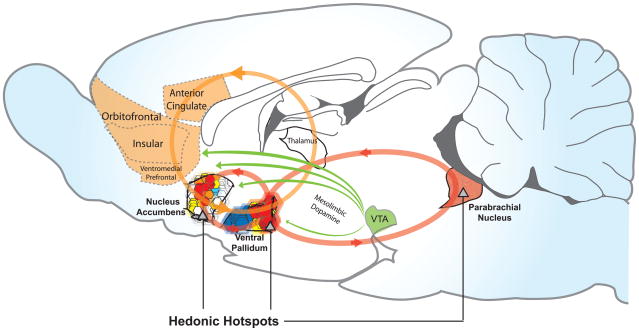
Figure 4. Hedonic hotspots and hedonic circuits.
Hedonic hotspots are shown in nucleus accumbens, ventral pallidum, and brainstem parabrachial nucleus where opioid or other signals cause amplification of core ‘liking’ reactions to sweetness. Reprinted by permission from (Smith et al., 2010), based on (Kringelbach, 2005; Peciña et al., 2006; Smith and Berridge, 2007).
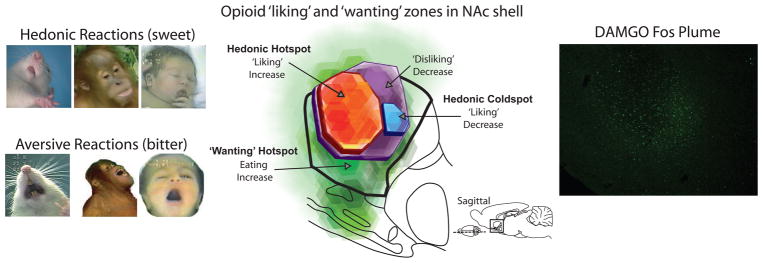
Figure 5. Taste ‘liking’ reactions and detail map of nucleus accumbens hotspot.
Positive ‘liking’ reactions to sweet tastes or aversive ‘disliking’ reactions to bitter tastes are homologous in human newborn, young orangutan, and adult rat (left). Opioid hotspots and coldspots in the nucleus accumbens (medial shell shown in sagittal view; center). Green: the entire medial shell supports opioid-stimulated increases in ‘wanting’ to eat food after microinjections of opioid agonist DAMGO. Red: only a cubic-millimeter sized hedonic hotspot also generates increases in ‘liking’ for sweetness. Blue: in a small hedonic ‘coldspot’ opioid stimulation suppresses ‘liking’ reactions to sucrose, and in a larger purple zone suppresses ‘disliking’ reactions to quinine, all while still stimulating intake. Fluorescent Fos plume to DAMGO microinjection (right). Reprinted by permission from (Smith et al., 2010), based on data from (Peciña and Berridge, 2005).
What has emerged recently from studies of ‘liking’ reactions and mechanisms is a connected brain network of hedonic hotspots in limbic forebrain structures that cause increases in ‘liking’ and ‘wanting’ together for food rewards (Figures 4 and 5). The hotspots form a distributed network of brain islands like an archipelago that connects the limbic forebrain and brainstem (Berridge, 2003; Kelley et al., 2005a; Levine and Billington, 2004; Lundy, 2008; Peciña and Berridge, 2005; Smith and Berridge, 2005; Smith et al., 2010). Hedonic hotspots have been identified so far in the nucleus accumbens and ventral pallidum, and indicated to exist in deep brainstem regions such as the parabrachial nucleus in the pons; possibly others yet unconfirmed could exist in amygdala or in cortical regions such as orbitofrontal cortex (Berridge and Kringelbach, 2008; Smith et al., 2010). We believe these distributed ‘liking’ sites all interact together so that they can function as a single integrated ‘liking’ circuit, which operates by largely hierarchical control across the major levels of the brain (Smith and Berridge, 2007; Smith et al., 2010).
Forebrain hotspots, identified in the nucleus accumbens or ventral pallidum, form the top of the neural hedonic hierarchy, as known so far, actively generating affective reactions in conjunction with networks extending down to the brainstem. In our laboratory, we have found that an opioid or endocannabinoid drug microinjection in a forebrain hedonic hotspot selectively doubles the number of ‘liking’ orofacial reactions elicited by a sweet taste (while suppressing or leaving negative ‘disliking’ reactions unchanged). To aid in pinpointing the ‘liking’ mechanisms initially activated by a drug microinjection, we developed a ‘Fos plume’ tool to measure how far a microinjected drug spreads to activate neurons in the brain. A drug microinjection modulates the activity of nearby neurons. Labeling these neurons for the immediate early gene protein, Fos, marks neuronal activation, and delineates the plume-shaped reactive area around the injection site (Figure 5). That area can be assigned responsibility for any hedonic enhancement caused by the drug microinjection. Hotspot boundaries emerge from comparisons of plume maps for microinjection sites that successfully enhanced ‘liking’ versus nearby ones that failed. This technique helps assign causation of pleasure to the responsible brain sites.
Nucleus accumbens hotspot
The first hotspot discovered was found inside the nucleus accumbens, where it uses opioid and endocannabinoid signals to amplify taste ‘liking’ (Figure 4 & 5). The hotspot lies in the medial shell subdivision of the nucleus accumbens: specifically, in a cubic-millimeter volume of tissue in the rostrodorsal quadrant of the medial shell. In the hedonic hotspot, ‘liking’ for sweetness is amplified by microinjection of drugs that mimic endogenous opioid or endocannabinoid neurochemical signals. This fits the suggestion of a number of investigators who hypothesized that opioid or cannabinoid receptor activation stimulates appetite in part by enhancing ‘liking’ for the perceived palatability of food (Baldo and Kelley, 2007; Barbano and Cador, 2007; Bodnar et al., 2005; Cooper, 2004; Dallman, 2003; Higgs et al., 2003; Jarrett et al., 2005; Kelley et al., 2002; Kirkham and Williams, 2001; Kirkham, 2005; Le Magnen et al., 1980; Levine and Billington, 2004; Panksepp, 1986; Sharkey and Pittman, 2005; Zhang and Kelley, 2000). Our results supported those hedonic hypotheses and, in terms of specific brain substrates, have helped pinpoint the brain sites responsible for pleasure enhancement to particular hotspots. Studies led by Susana Peciña in our laboratory first found the cubic-millimeter hotspot site in the medial shell, using microinjections of an opioid agonist drug (DAMGO; [D-Ala2, N-MePhe4, Gly-ol]-enkephalin). DAMGO selectively activates the mu type of opioid receptor, and in the hotspot this appears sufficient to enhance the pleasure gloss painted by the brain on sweet sensation (Pecina, 2008; Peciña and Berridge, 2005; Peciña et al., 2006; Smith et al., 2010). More than double the usual number of positive ‘liking’ reactions were emitted to sucrose taste by rats with DAMGO microinjections in their hotspots. ‘Disliking’ reactions to quinine were never enhanced, but rather were suppressed by mu opioid activation in and around the hotspot. Thus sweetness pleasure is enhanced, and bitterness displeasure is simultaneously reduced, by neurochemical stimulation of the hedonic hotspot.
Endocannabinoids, brain chemicals similar to the psychoactive tetrahydrocannabinol component of marijuana, have their own hedonic hotspot in nucleus accumbens shell that anatomically overlaps with the opioid hotspot. A study by Stephen Mahler and Kyle Smith in our lab found that anandamide, an endocannabinoid that likely acts in the brain by stimulating the CB1 type of cannabinoid receptor, could act in the nucleus accumbens hotspot similarly to an opioid drug to magnify the pleasure impact of sucrose taste (Mahler et al., 2007; Smith et al., 2010). Anandamide microinjections in the hotspot potently doubled the number of positive ‘liking’ facial reactions that sucrose taste elicited from rats, just as did opioid stimulation, whereas again aversive reactions to bitter taste were not enhanced. One intriguing possibility that might further connect these ‘liking’ enhancements by the shell hotspot is that opioid and endocannabinoid signals might interact or cooperate. Anandamide has been suggested to act in part as a reverse neurotransmitter, which could be released by an intrinsic spiny neuron in the shell to float back to nearby presynaptic axon terminals and stimulate CB1 receptors, and possibly modulate pre-synaptic opioid release (Cota et al., 2006; Kirkham, 2008; Piomelli, 2003). Likewise, opioid signals striking the post-synaptic spiny neuron in shell might recruit endocannabinoid release. Future studies may be able to explore whether endocannabinoid and opioid signals interact by such cooperative positive feedback mechanisms.
Larger opioid sea of ‘wanting’ in nucleus accumbens
In addition to amplifying ‘liking’, microinjections of DAMGO or anandamide in the same accumbens hotspot also simultaneously and directly stimulate ‘wanting’ to eat, shown by a robust increase in food intake. But other nearby parts of the nucleus accumbens generate only ‘wanting’ when activated by opioids, without enhancing ‘liking’ (Figure 5). That is, while opioid neurotransmission in the cubic-millimeter hotspot has a special hedonic capacity to magnify ‘liking’ (compared to, say, dopamine neurotransmission), opioid stimulation outside the hotspot is not hedonic, and induces only ‘wanting’ without ‘liking’ (sometimes even reducing ‘liking’). For example, the opioid hedonic hotspot comprises a mere 10% of the entire nucleus accumbens, and even only 30% of its medial shell. Yet DAMGO microinjections throughout the entire 100% of medial shell potently increased ‘wanting’, more than doubling the amount of food intake. DAMGO enhances ‘wanting’ as effectively even at a more posterior ‘coldspot’ where the same microinjections suppressed ‘liking’ below normal (Peciña and Berridge, 2005). Hedonic specialization is restricted neuroanatomically to hotspots, as well as neurochemically to opioid and endocannabinoid signals (Peciña and Berridge, 2005). Widely spread mechanisms for ‘wanting’ are consistent with previous findings that opioids stimulate food ‘wanting’ throughout the entire nucleus accumbens and even in outside structures that include the amygdala and neostriatum (Cooper and Higgs, 1994; Kelley, 2004; Kelley et al., 2005a; Levine and Billington, 2004; Yeomans and Gray, 2002). Many of those opioid sites may not be hedonic.
Does neostriatum participate in ‘wanting’ or ‘liking’ generation ?
The ventral striatum (nucleus accumbens) is famous for motivation, but recently the dorsal striatum (neostriatum) has become implicated in food motivation and reward too (in addition to the well-known dorsal striatal role in movement) (Balleine et al., 2007; Palmiter, 2007; Schultz and Dickinson, 2000; Volkow et al., 2002; Wise, 2009). For example, dopamine neurons that project to neostriatum in monkeys code reward cues and reward prediction errors (unpredicted juice rewards) similarly to dopamine neurons that project to nucleus accumbens (Schultz and Dickinson, 2000). Human dopamine release in dorsal striatum accompanies craving elicited by viewing food or drug cues (in some studies, more strongly correlated than in ventral striatum) (Volkow et al., 2002; Volkow et al., 2008; Wang et al., 2004a). Neostriatal dopamine is needed to generate normal eating behavior, as food intake is restored to aphagic dopamine-deficient knockout mice by replacement of dopamine in the neostriatum (Palmiter, 2007; Szczypka et al., 2001).
Similarly, mu opioid stimulation of neostriatum can stimulate food intake, at least in the ventrolateral portion (Zhang and Kelley, 2000). Extending this result, we have recently found that other regions of the neostriatum also may mediate opioid-stimulated food intake, including the most dorsal portions of the neostriatum. In particular, our observations suggest that mu opioid stimulation of the dorsomedial quadrant of neostriatum enhances intake of palatable food (DiFeliceantonio and Berridge, personal observations). In a recent pilot study, we observed that rats ate more than twice as much of a chocolate treat (M&M candies) after receiving DAMGO microinjections in dorsomedial striatum than after control vehicle microinjections. Thus our results support the idea that even the most dorsal parts of neostriatum may participate in generating incentive motivation to consume food reward (Balleine et al., 2007; Palmiter, 2007; Schultz and Dickinson, 2000; Volkow et al., 2002; Wise, 2009).
Ventral pallidum: most crucial generator of food ‘liking’ and ‘wanting’?
The ventral pallidum is relatively new in the literature on limbic structures, but is a chief output target of the nucleus accumbens systems discussed above, and we believe is especially crucial to incentive motivation and food pleasure (Heimer and Van Hoesen, 2006; Kelley et al., 2005a; Morgane and Mokler, 2006; Sarter and Parikh, 2005; Smith et al., 2009; Swanson, 2005; Zahm, 2006). The ventral pallidum contains its own cubic-millimeter hedonic hotspot in its posterior half, which is especially crucial both for maintaining normal levels of reward ‘liking’ as well as for enhancing ‘liking’ to elevated levels (Figure 4). This view is based in large part on studies in our lab by Howard Cromwell, Kyle Smith and Chao-Yi Ho (Peciña et al., 2006; Smith and Berridge, 2005; Smith and Berridge, 2007; Smith et al., 2009; Smith et al., 2010), and collaborative studies with Amy Tindell and J. Wayne Aldridge (Tindell et al., 2004; Tindell et al., 2006), and is consistent with reports by other researchers (Beaver et al., 2006; Berridge and Fentress, 1986; Childress et al., 2008; Kalivas and Volkow, 2005; Miller et al., 2006; Napier and Mitrovic, 1999; Pessiglione et al., 2007; Shimura et al., 2006; Zubieta et al., 2003).
The ventral pallidum’s importance is reflected in the surprising fact that it is the only brain region known so far where neuronal death abolishes all ‘liking’ reactions and replaces them with ‘disliking,’ even for sweetness (at least for a period of up to several weeks) (Cromwell and Berridge, 1993). This assertion may surprise readers who remember learning that the lateral hypothalamus was the site where lesions cause aversive gapes to food (Teitelbaum and Epstein, 1962; Winn, 1995), so some explanation is in order. Although large lesions of the lateral hypothalamus have long been known to disrupt ‘liking’ reactions as well as voluntary eating and drinking behaviors (Teitelbaum and Epstein, 1962; Winn, 1995), the pleasure-disrupting lesions of those studies from the 1960s and 1970s typically damaged not only lateral hypothalamus but also the ventral pallidum (Schallert and Whishaw, 1978; Stellar et al., 1979; Teitelbaum and Epstein, 1962).
A more precise lesion study in our laboratory by Howard Cromwell determined that aversion only followed lesions that caused damage to the ventral pallidum (anterior and lateral to the lateral hypothalamus), those that only damaged the lateral hypothalamus did not lead to aversion (Cromwell and Berridge, 1993). Follow-up studies by Chao-Yi Ho in our laboratory recently have confirmed that neuronal death in the posterior ventral pallidum produces sucrose ‘disliking’ and abolishes ‘liking’ reactions to sweetness for days to weeks after the lesions (Ho and Berridge, 2009). Similar aversion is produced by even temporary inhibition of neurons in roughly the same hotspot (via microinjection of GABA agonist muscimol) (Ho and Berridge, 2009; Shimura et al., 2006). Thus the ventral pallidum seems especially needed in forebrain circuitry for normal sweetness ‘liking’.
The hedonic hotspot of ventral pallidum also can generate increased ‘liking’ for food when stimulated neurochemically (Ho and Berridge, 2009; Smith and Berridge, 2005; Smith and Berridge, 2007). Studies by Kyle Smith in our lab first showed that in the hedonic hotspot of ventral pallidum, roughly a cubic-millimeter volume in the posterior part of the structure, microinjections of the opioid agonist DAMGO caused sucrose taste to elicit over twice as many ‘liking’ reactions as normal (Smith and Berridge, 2005) Opioid activation in the posterior ventral pallidum also caused rats to eat over twice as much food. By contrast, if the same opioid microinjections were moved anteriorly outside the hotspot toward the front of the ventral pallidum, they actually suppressed both hedonic ‘liking’ and ‘wanting’ to eat, consistent with the possibility of a disgust-generating zone in the anterior half of ventral pallidum (Calder et al., 2007; Smith and Berridge, 2005). These effects illustrate the hotspot, and seem consistent with the findings of several other laboratories on the importance of ventral pallidum activations in food, drug and other reward (Beaver et al., 2006; Calder et al., 2007; Johnson et al., 1993; Johnson et al., 1996; McFarland et al., 2004; Shimura et al., 2006; Zubieta et al., 2003).
An orexin hedonic hotspot in ventral pallidum?
Are there other hedonic neurotransmitters in the ventral pallidum hotspot that can amplify ‘liking’ reactions? One promising candidate is orexin, thought to be associated with hunger and reward in the lateral hypothalamic region (Aston-Jones et al., 2009; Harris et al., 2005). Orexin neurons project from the hypothalamus to the ventral pallidum, especially its posterior region containing the opioid hedonic hotspot (Baldo et al., 2003). Ventral pallidum neurons thus directly receive orexin inputs, and accordingly express receptors for orexin (Nixon and Smale, 2007).
Results from recent studies in our lab indicate that orexin in the ventral pallidum can enhance ‘liking’ for sweet rewards (Ho and Berridge, 2009). Chao-Yi Ho has found that microinjections of orexin-A in the same posterior site as the opioid hedonic hotspot of ventral pallidum amplify the number of ‘liking’ reactions to sucrose taste. The orexin microinjections in ventral pallidum fail to increase negative ‘disliking’ reactions to quinine, indicating that only positive aspects of sensory pleasure were enhanced and not all taste-elicited reactions (Ho and Berridge, 2009). While more studies are needed, these early results suggest a mechanism by which hunger states might make palatable foods taste even better, perhaps via an orexin hypothalamus-to-ventral-pallidum link.
Final evidence that ventral pallidum mediates hedonic impact of ‘liked’ sensations is that the firing levels of neurons in the posterior hedonic hotspot code ‘liking’ for sweet, salty and other food rewards (Aldridge et al., 1993; Aldridge and Berridge, 2010; Beaver et al., 2006; Calder et al., 2007; Tindell et al., 2004; Tindell et al., 2005; Tindell et al., 2006). Neurons in the hotspot of ventral pallidum fire faster when rats eat a sugar pellet, or even encounter a cue for the reward, as measured by permanently implanted recording electrodes (Tindell et al., 2004; Tindell et al., 2005). The firing of sucrose-triggered neurons appears to specifically code hedonic ‘liking’ for the taste (Aldridge and Berridge, 2010). For example, ventral pallidal neurons fire when a sucrose solution is infused into the mouth but the same neurons will not fire to a NaCl solution that is three-times saltier than seawater and quite unpleasant to drink. However, the ventral pallidum hotspot neurons suddenly begin to fire to the taste of the triple-seawater if a physiological state of salt appetite is induced in the rats (Tindell et al., 2006; Tindell et al., 2009) by administering furosemide and deoxycorticosterone as drugs to mimic the hormonal sodium-depletion signals of angiotensin and aldosterone (Krause and Sakai, 2007), and to increase the perceived ‘liking’ for the intensely salty taste (Berridge and Schulkin, 1989; Tindell et al., 2006). Thus neurons in the ventral pallidum code taste pleasure in a way that is sensitive to the physiological need of the moment. The observation that those hedonic neurons are in the same hedonic hotspot where opioid activation causes increased ‘liking’ reactions to sweet taste suggests that their firing rate might actually be part of the causal mechanism that paints the pleasure gloss onto taste sensation (Aldridge and Berridge, 2010).
One case in which ventral pallidum can enhance ‘wanting’ without ‘liking’ is seen following disinhibition of GABA neurons in the ventral pallidum, (Smith and Berridge, 2005). Kyle Smith microinjected the GABA antagonist, bicuculline, which released neurons from tonic GABAergic suppression, presumably helping them to become electrically depolarized somewhat similarly to a stimulating electrode. The psychological result of ventral pallidal depolarization was almost identical to that of lateral hypothalamic electrode stimulation. Food intake was doubled yet there was no increase at all in ‘liking’ reactions to sucrose taste (in contrast to opioid stimulation by DAMGO microinjections at the site, which increased ‘wanting’ and ‘liking’ together) (Smith and Berridge, 2005).
Cooperative nature of nucleus accumbens and ventral pallidum hotspots
Not only do both nucleus accumbens and ventral pallidum contain hedonic hotspots in which opioid stimulation enhances ‘liking,’ but the two hotspots work together to create a coordinated network for enhancement of ‘liking’ (Smith and Berridge, 2007). In work done in our lab, Kyle Smith found that microinjections of opioid agonist in either hotspot activated distant Fos expression in the other hotspot, indicating that each hotspot recruits the other to enhance hedonic ‘liking’. Additionally, opioid blockade by naloxone in either hotspot could abolish the increased ‘liking’ produced by DAMGO microinjection into the other, indicating that unanimous participation was required. Such observations suggest that the two hotspots interact reciprocally in a single ‘liking’ circuit, and the entire circuit is needed to magnify hedonic impact. However, accumbens activation by itself is capable of causing increased ‘wanting’ and food intake regardless of ventral pallidal participation (and regardless of whether ‘liking’ is simultaneously enhanced) (Smith and Berridge, 2007).
Connecting brain reward and regulatory systems
Great progress has been made in recent years toward understanding neural interactions between mesocorticolimbic reward systems and hypothalamic regulation systems of caloric hunger and satiety (Baldo and Kelley, 2007; Baldo et al., 2004; Berthoud and Morrison, 2008; Carr, 2007; Finlayson et al., 2007; Fulton et al., 2006; Harris et al., 2005; Harris and Aston-Jones, 2006; Kelley et al., 2005b; Mela, 2006; Myers, 2008; Palmiter, 2007; Robertson et al., 2008; Scammell and Saper, 2005; Zheng and Berthoud, 2007; Zheng et al., 2007).
So how might hunger states increase food ‘liking’ in alliesthesia (Cabanac, 1979; Cabanac, 2010), or enhance ‘wanting’ to make food become more attractive? And how might individual differences intersect with this to produce eating disorders or obesity in some people? There are a number of promising mechanisms for such interactions. We will briefly speculate about a few here.
Food as a stronger motivational magnet during hunger
One possibility is to elevate ‘wanting’ for food directly during hunger, and perhaps to magnify that attraction in obese individuals. In people, higher incentive salience for food cues has been measured in some studies by eye movements directed more rapidly or for longer durations or more frequently to the sight of foods, or by related measures of visual attention. For example, obese people have been reported to automatically direct their visual attention more to the sight of foods than non-obese people, particularly when hungry (Nijs et al., 2009). Another report suggests that hunger elevates food cue incentive salience in both normal-weight and obese people, as reflected by increased gaze duration, but that obese individuals have higher gaze measures of incentive salience for food images even when they had recently eaten (Castellanos et al., 2009). Higher incentive salience of food images might also be related to the classic notion from social psychology that obesity involves greater externality or over-reaction to incentive stimuli (Nisbett and Kanouse, 1969; Schachter, 1968).
Opioid alliesthesia during hunger?
Likewise, hedonic ‘liking’ for food is enhanced during hunger. Endogenous opioid activation in hedonic hotspots is a chief candidate to make food taste better during hunger. If the taste of food when hungry evoked higher endogenous opioid release to stimulate mu opioid receptors, food would taste better than when sated. Anyone who had an exaggerated form of this hedonic mechanism would find food to taste especially good. For the nucleus accumbens hotspot, we think the natural mu opioid signal is most likely to come from natural enkephalin release. Endogenous B-endorphin is a more effective ligand for mu opioid receptors than is enkephalin, and B-endorphin neurons have been suggested to project from hypothalamus to other limbic structures (Bloom et al., 1978; Zangen and Shalev, 2003), but endorphins may not be present in the medial shell sufficiently to accomplish this task (S.J. Watson, personal communication, 2009). Therefore enkephalins, rather than B-endorphin, are probably the most available mu-opioid signal in the nucleus accumbens shell. Enkephalin arises from a large population of intrinsic neurons within the shell (the population which expresses enkephalin mRNA along with D2 receptors and GABA mRNA), as well as from projection neurons arriving from the ventral pallidum and related structures which also deliver GABA and enkephalin signals.
An intriguing hypothalamic-thalamic-accumbens brain circuit to boost enkephalin signals in the nucleus accumbens shell during states of caloric hunger was suggested by Ann Kelley and her colleagues (Kelley et al., 2005a). Kelley et al. proposed that orexin neurons in lateral hypothalamus project to activate glutamate neurons in the thalamic paraventricular nucleus. In turn, thalamic paraventricular neurons project to the nucleus accumbens shell where they use glutamate signals to excite large acetylcholine-containing interneurons. Kelley and colleagues suggested that finally the acetylcholine neurons in medial shell specifically activate nearby enkephalin neurons. The enkephalin-releasing neurons should plausibly include those within the cubic-millimeter hedonic hotspot of medial shell (intriguingly, the fields of large acetylcholine neurons span approximately 1 mm in diameter). Thus hunger might conceivably potentiate the endogenous opioid signal in the nucleus accumbens hotspot to amplify ‘liking’ and ‘wanting’ for palatable food.
Endocannabinoid mechanisms of alliesthesia?
Another potential mechanism to make food taste better during hunger is endocannabinoid recruitment within the same hedonic hotspot of medial shell. Evidence suggests that endocannabinoids may similarly be recruited by hunger. For example, Kirkham and colleagues reported that a 24-hr fast in rats raises the levels of endocannabinoids, anandamide and 2-arachidonoyl, glycerol in forebrain limbic structures including nucleus accumbens (Kirkham et al., 2002). An endocannabinoid rise during hunger could therefore enhance hedonic ‘liking’ for food (Kirkham, 2008; Kirkham, 2005). This could potentiate ‘liking’ especially if the potentiated endocannabinoid signals reach the same hotspot in medial shell of nucleus accumbens, where anandamide microinjections are known to enhance ‘liking’ to sweetness (Mahler et al., 2007). It is also noteworthy that endocannabinoids also facilitate mesolimbic dopamine via the ventral tegmental area and other sites, which might facilitate the incentive salience ‘wanting’ of palatable foods independently of hedonic ‘liking’ (Cota et al., 2006; Kirkham, 2005).
Orexin mechanisms of alliesthesia?
Another set of possibilities involves orexin again, but acting in a more direct way than through an intermediary thalamic loop to activate hotspot neurons (Kelley et al., 2005a). The most relevant orexin-producing neurons are found in the lateral hypothalamus, where they have been suggested to mediate reward for food, drugs, sex, etc. (Aston-Jones et al., 2009; Harris et al., 2005; Harris and Aston-Jones, 2006; Muschamp et al., 2007) [additional orexin or hypocretin neurons are also found in other hypothalamic nuclei, which instead may mediate arousal and alertness (Berridge et al., 2009; Espana et al., 2001)].
Reward-related orexin neurons in the lateral hypothalamus are activated by arcuate neuropeptide-Y (NPY) signals during hunger (Berthoud and Morrison, 2008; Gao and Horvath, 2007). Some orexin neurons project to ventral pallidum and to nucleus accumbens (Baldo et al., 2003; Borgland et al., 2009; Korotkova et al., 2003; Peyron et al., 1998; Zheng et al., 2007). As described above, we have recently found that orexin microinjections in the ventral pallidum hotspot can directly potentiate ‘liking’ reactions to sweetness (Ho and Berridge, 2009). Speculatively, then, orexin activation during hunger might directly enhance hedonic impact by stimulating neurons in hedonic hotspots, such as the posterior ventral pallidum. Thus orexin might effectively activate the same hedonic hotspot as mu opioid signals do in ventral pallidum (and conceivably in nucleus accumbens). In addition, orexin could stimulate ‘wanting’ both through these forebrain hotspots and via projections to mesolimbic dopamine neurons in the ventral tegmentum.
Leptin mechanisms of alliesthesia?
In the opposite direction, satiety states suppress ‘liking’ and ‘wanting’ for foods even if it is difficult to completely turn off food reward (Berridge, 1991; Cabanac, 1979; Cabanac and Lafrance, 1990; Kringelbach et al., 2003; O’Doherty et al., 2001; Small et al., 2001). One candidate mechanism to create negative alliesthesia during satiety is leptin, secreted from fat cells in the body. Leptin acts on neurons in the arcuate nucleus, other hypothalamic nuclei and in the brainstem, including in the ventral tegmentum where it may modulate mesolimbic dopamine circuits and food ‘wanting’ (Choi et al., 2010; Figlewicz and Benoit, 2009; Friedman and Halaas, 1998; Fulton et al., 2006; Grill, 2010; Hommel et al., 2006; Leinninger et al., 2009; Robertson et al., 2008). Leptin might also conceivably contribute to alliesthesia-induced ‘liking’ suppression by stimulating hypothalamic arcuate POMC/CART neurons to activate MCR4 receptors on paraventricular neurons, or by suppressing arcuate NPY-AGrP neurons to suppress orexin neurons in lateral hypothalamus, and thus finally reducing the opioid or orexin stimulation of hedonic hotspots in ventral pallidum or nucleus accumbens.
In humans, Farooqi and O Rahilly and colleagues have reported fascinating results implicating malfunction of leptin’s ability to suppress ‘wanting’ or ‘liking’ in a particular form of genetic obesity: people born with a monogenic-based deficiency of leptin, who as children constantly demand food and soon become obese (Farooqi et al., 2007; Farooqi and O’Rahilly, 2009). In the absence of leptin these individuals have exaggerated liking ratings for foods that directly correlates with nucleus accumbens activation by food stimuli measured by fMRI. Unlike in most people, their accumbens activation is not suppressed by having recently eaten a full meal, suggesting an abnormal persistence of limbic ‘liking’ and ‘wanting’ activation even during satiety. Farooqi and colleagues also report that giving exogenous leptin medication to these individuals allows caloric satiety to regain the capacity to suppress limbic activation by foods, so that liking ratings then correlate with nucleus accumbens activation only when hungry, and no longer when relatively sated after a meal. Such findings seem consistent with the notion that leptin (interacting with other hunger/satiety signals) gates the ability of meal satiety signals to suppress ‘liking’ and ‘wanting’ for foods (Farooqi et al., 2007).
In rats, leptin administration in the ventral tegmental area can produce a suppression of firing rates for mesolimbic dopamine neurons, consistent with a reduction of ‘wanting’, and behaviorally suppress the intake of palatable foods (Hommel et al., 2006). Leptin and insulin both also have been shown in the ventral tegmental area to prevent the stimulation of eating behavior and food intake that otherwise results from mu opioid stimulation of the same structure produced by DAMGO microinjection (Figlewicz et al., 2007; Figlewicz and Benoit, 2009). Insulin’s satiety-like actions in the ventral tegmental area appear to involve the upregulation of dopamine transporter (DAT) in dopamine neurons and consequent reduction of synaptic extracellular dopamine levels in the nucleus accumbens (Choi et al., 2010; Figlewicz et al., 2007; Figlewicz and Benoit, 2009). However, it should be noted that a few loose ends still exist for the idea that leptin suppresses food ‘wanting’ and ‘liking’. Paradoxically, for example, an almost opposite effect has been reported in leptin-deficient mice (ob/ob), in that leptin appeared to stimulate congenitally low levels of accumbens dopamine (Fulton et al., 2006; Myers et al., 2009). This piece of the puzzle remains to be explained.
Stress as a promoter of eating and intake
Stress promotes eating of palatable foods in about 30% of the population (Dallman et al., 2003; Dallman, 2010). Several psychological and neurobiological mechanisms could explain stress-induced hyperphagia. Traditional explanations for stress-induced over-eating generally have focused on the aversive aspects of stress, and the hedonic soothing effects of eating palatable food. That is, increases in eating during stress are traditionally posited to be an attempt at stress reduction by hedonic self-medication (Dallman et al., 2003; Dallman, 2010; Koob, 2004).
Similarly, corticotropin-releasing factor (CRF) release, a brain mechanism of stress, has been postulated to produce an aversive state that indirectly increases intake, by promoting the eating of highly palatable food (comfort food) in order to reduce the aversive state (hedonic self-medication) (Dallman et al., 2003; Dallman et al., 2006; Koob and Kreek, 2007). Supporting the hedonic medication concept, the consumption of sweet comfort foods can reduce HPA responsivity and lower basal levels of CRF in the hypothalamus after stress, whereas stressors increase the release of CRF (Dallman et al., 2003; Dallman, 2010; Koob, 2004). Blockade of CRF receptors may increase intake of less palatable food while suppressing intake of sucrose (Cottone et al., 2009).
However, CRF release is also directly increased in central nucleus of amygdala by eating palatable food (Merali et al., 2003), and experimentally-induced elevations of CRF in hypothalamus or extended amygdala tend to suppress ingestive behaviors and food intake, not enhance them (Ciccocioppo et al., 2003; Koob, 2004). That seems anomalous for the idea that aversive states are necessary for CRF, or that CRF reliably stimulates intake in brain structures that mediate its aversive effects.
An explanation might be that in other brain structures CRF and stress may directly potentiate incentive ‘wanting’ to eat, without necessarily causing aversive states or needing hedonic self-medication to power the eating. For example, in our lab Susana Peciña found that CRF microinjection in the nucleus accumbens shell directly promoted cue-triggered ‘wanting’ for sucrose, under conditions that ruled out an aversive motivational mechanism or hedonic self-medication explanation. Instead, CRF microinjections in the medial shell of nucleus accumbens directly elevated the attribution of incentive salience to sugar-paired cues.
CRF enhanced phasic bursts of effort to obtain sugary treats that were triggered by encounters with sugar cues, in a Pavlovian-Instrumental Transfer test designed to exclude alternative explanations besides incentive salience (Pecina, Schulkin, & Berridge, 2006). The CRF microinjection was as potent as amphetamine microinjection in nucleus accumbens (which would have induced dopamine release) at enhancing peaks of cue-triggered ‘wanting’. Just as dopamine did, the CRF in nucleus accumbens multiplied the motivational potency of sugar cues to trigger a phasic peak of desire for reward, rather than acting as a constant drive or steadily aversive state. That is, CRF-induced elevations of ‘wanting’ came and went with the appearance and disappearance of the physical cue, though CRF remained in the brain throughout the entire period. This synergy of ‘wanting’, which needs the combination of cue plus CRF, is compatible with the incentive salience model of Figure 1, and suggests that CRF did not produce a constant aversive drive to obtain sucrose, but rather multiplied the attractiveness of food cues.
This incentive effect of CRF in nucleus accumbens may provide a novel explanation for why stress may enhance cue-triggered bursts of binge eating. The explanation is that CRF in nucleus accumbens makes the sight, smell, sound, or imagination of food more ‘wanted’, and more able to trigger an intense ‘wanting’ to eat the associated food. Possibly, CRF in the central amygdala and extended amygdala might have similar incentive functions too (Stewart, 2008). The most important clinical implication of these findings is that stress-elicited CRF may enhance cue-triggered ‘wanting’ to eat even if the stress state is not perceived as aversive. Even a happy stress, such as winning the lottery or getting a promotion, could trigger this incentive CRF mechanism. This may also be related to why glucocorticoid administration can increase voluntary intake of palatable foods (Bhatnagar et al., 2000), even though rats will work to obtain intravenous glucocorticoid infusions (Piazza et al., 1993). Although stress and incentive motivation may be traditionally viewed as psychological opposites, the brain mechanisms that mediate them may actually overlap to a surprising extent (Faure et al., 2008; Merali et al., 2003; Pecina et al., 2006; Reynolds and Berridge, 2008). Hedonic self-medication of aversive states may not always be necessary for stress to make people overeat. In short, stress may not always need to distress in order to promote over-consumption.
Food addictions?
While still controversial, the idea of food addiction is increasingly being regarded as having validity, at least for some cases of compulsive overeating (Avena et al., 2008; Dagher, 2009; Dallman, 2010; Davis et al., 2004; Davis and Carter, 2009; Ifland et al., 2009; Kessler, 2009; Lowe and Butryn, 2007; Pelchat, 2009; Rogers and Smit, 2000). What food addiction means can vary somewhat depending on who is defining it. Some definitions focus on the artificially intense sweet, salty or fatty sensory stimulation and technologically-enhanced nature of modern processed foods, positing them to have become super-incentive stimuli which possess drug-like motivating potency (Cocores and Gold, 2009; Corwin and Grigson, 2009; Ifland et al., 2009; Kessler, 2009; Pelchat, 2009; Volkow et al., 2008). Modern foods and their cues may indeed key into brain ‘liking’ and ‘wanting’ mechanisms at intense levels, especially in some individuals (Davis and Carter, 2009; Finlayson et al., 2007; Mela, 2006; Zheng and Berthoud, 2007).
Other views would restrict the food addiction label to relatively few people, in particular to cases of extreme over-eating that border closely on compulsion (Davis et al., 2008; Davis and Carter, 2009; Davis et al., 2009; Gearhardt et al., 2009). For example, Davis and Carter suggest that only particular individuals qualify who are both obese and have an intense binge eating disorder, with addictive-like features of loss of control and relapse. Such individuals are especially prone to describe themselves as “compulsive over-eaters” or as “food addicts” (Davis and Carter, 2009; Davis et al., 2009). Suggesting a potential underlying mechanism, Davis and colleagues recently found that such individuals were far more likely to carry both the G+ allele for the receptor gene that codes a “gain of function” for mu opioid signals, and to simultaneously also carry the A2 allele associated with Taq1A marker that may increase binding to the dopamine D2 receptor (Davis et al., 2009). Davis and colleagues suggest that this genetic combination may heighten brain opioid signals and dopamine signals alike, and so elevate both ‘liking’ and ‘wanting’ for foods in a one-two punch that promotes binge eating and obesity. In a similar vein, Campbell and Eisenberg have suggested that people with genes that promote elevated dopamine functioning might similarly experience stronger cue-triggered urges in the presence of foods and be more liable to developing obesity (Campbell and Eisenberg, 2007).
Such suggestions seem quite compatible with what we know about brain mechanisms of incentive salience and hedonic impact. At the extreme, and when focused on incentive salience, such suggestions could even produce food equivalents of incentive-sensitization, a brain-based theory of addiction that explains why drug addicts may sometimes ‘want’ to take drugs even when they do not particularly ‘like’ them (Robinson and Berridge, 1993; Robinson and Berridge, 2003; Robinson and Berridge, 2008). Compulsive levels of ‘wanting’ to eat might similarly be produced by sensitization-type hyper reactivity in brain mesolimbic circuits of incentive salience. This idea is compatible with suggestions that sensitization-like changes in brain mesolimbic systems are produced by exposure to dieting and binging cycles (Avena and Hoebel, 2003a; Avena and Hoebel, 2003b; Bell et al., 1997; Bello et al., 2003; Carr, 2002; Colantuoni et al., 2001; de Vaca and Carr, 1998; Gosnell, 2005). Certainly the genetically-coded cases of change in human opioid, dopamine or leptin signaling described above might have altered brain reward circuits that function toward foods in much the same way as if they were drug-sensitized. Such a person could be liable to intense peaks of cue-triggered ‘wanting’ for foods at excessive levels that other people simply never experience in normal life, and are unable to experience unless very seriously hungry. That sort of compulsion to eat might well deserve to be called a food addiction.
In general, controversy over whether over-eating more generally should be called addiction will likely continue for some time. Whether ‘wanting’ for food can reach quite the same high levels of intensity that are thought to characterize drug addiction, and in whom, are open empirical questions. Still, not even all habitual drug users are ‘addicts’ in the sense of incentive-sensitization, and over-eaters will vary in psychological routes too. It may be helpful to keep in mind that ‘wanting’ and ‘liking’ vary in graded fashion along continuums, rather than categorically as ‘addicted or not’. There will be many shades of gray.
Conclusion
The roles of ‘liking’ and ‘wanting’ in obesity are just beginning to be understood. We end by returning to the framework of logical possibilities outlined at the beginning.
First, it is possible that dysfunctional elevation of ‘liking’ or ‘wanting’ mechanisms cause at least some cases of over-eating. In principle, hedonic ‘liking’ might be altered in some individuals, such as perhaps in some cases of binge-eating disorder as mentioned above. Alternatively, cue-triggered ‘wanting’ might rise via separate alteration in some people, somewhat similar to the addiction-related phenomenon of incentive-sensitization. Food ‘liking’ and ‘wanting’ can dissociate somewhat even in normal situations, such as when ‘wanting’ declines faster or farther than ‘liking’ for the same food as satiation progresses. Eating disorders might exaggerate this separation, and lead to cases in which ‘wanting’ is too high (or too low) relative to ‘liking’ that remains more normal. Increases in incentive salience of food cues or in underlying dopamine-related parameters of brain function discussed above seem consistent with this possibility.
Second, ‘wanting’ or ‘liking’ mechanisms might change in obesity or eating disorders, but as a marker or consequence of their condition rather than as the cause. For example, it seems conceivable that at least some changes in dopamine D2 receptor binding in obese individuals may be a consequence rather than the cause of their over-eating. Lastly, ‘liking’ and ‘wanting’ may function normally in other cases, so that both the source of the problem and its solution would need to be sought elsewhere.
The growing trend towards increased body weight results from the bountiful availability of foods interacting with a brain reward system that evolved in environments of relative scarcity. In evolutionary environments, brain systems of incentive motivation and appetite that were mostly ‘go’ with little ‘stop’ could remain adaptive, but now some features of these brain systems may work against people’s best interests. A better understanding of ‘wanting’ and ‘liking’ mechanisms tailored to individual types of eating disorders and obesity could lead to better therapeutic strategies, and perhaps help people who wish to more effectively create ‘stop’ signals of their own.
Acknowledgments
This paper is dedicated to the memory of Ann E. Kelley (a leader in the neuroscience of food reward) and of Steven J. Cooper (a leader in the psychopharmacology of food reward). The careers of those outstanding scientists set the stage for many of the issues engaged here, and their recent deaths were sad losses to the field. We thank Ryan Selleck for redrawing Figures 1, 2, and 3. The results described here are from work supported by DA015188 and MH63649 grants from the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adan RAH, Vanderschuren L, la Fleur SE. Anti-obesity drugs and neural circuits of feeding. Trends in Pharmacological Sciences. 2008;29:208–217. doi: 10.1016/j.tips.2008.01.008. [DOI] [PubMed] [Google Scholar]
- Ahn S, Phillips AG. Dopaminergic correlates of sensory-specific satiety in the medial prefrontal cortex and nucleus accumbens of the rat. Journal of Neuroscience. 1999;19:B1–B6. doi: 10.1523/JNEUROSCI.19-19-j0003.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldridge JW, Berridge KC, Herman M, Zimmer L. Neuronal coding of serial order: Syntax of grooming in the neostriatum. Psychological Science. 1993;4:391–395. [Google Scholar]
- Aldridge JW, Berridge KC. Neural Coding of Pleasure: “Rose-Tinted Glasses” of the Ventral Pallidum. In: Kringelbach ML, Berridge KC, editors. Pleasures of the Brain. Oxford University Press; Oxford: 2010. pp. 62–73. [Google Scholar]
- Aston-Jones G, Smith RJ, Sartor GC, Moorman DE, Massi L, Tahsili-Fahadan P, Richardson KA. Lateral hypothalamic orexin/hypocretin neurons: A role in reward-seeking and addiction. Brain Res. 2009 doi: 10.1016/j.brainres.2009.09.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avena NA, Hoebel BG. Amphetamine-sensitized rats show sugar-induced hyperactivity (cross-sensitization) and sugar hyperphagia. Pharmacology Biochemistry and Behavior. 2003a;74:635–639. doi: 10.1016/s0091-3057(02)01050-x. [DOI] [PubMed] [Google Scholar]
- Avena NM, Hoebel BG. A diet promoting sugar dependency causes behavioral cross-sensitization to a low dose of amphetamine. Neuroscience. 2003b;122:17–20. doi: 10.1016/s0306-4522(03)00502-5. [DOI] [PubMed] [Google Scholar]
- Avena NM, Rada P, Hoebel BG. Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. 2008;32:20–39. doi: 10.1016/j.neubiorev.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldo B, Kelley A. Discrete neurochemical coding of distinguishable motivational processes: insights from nucleus accumbens control of feeding. Psychopharmacology (Berl) 2007;191:439–59. doi: 10.1007/s00213-007-0741-z. [DOI] [PubMed] [Google Scholar]
- Baldo BA, Daniel RA, Berridge CW, Kelley AE. Overlapping distributions of orexin/hypocretin- and dopamine-beta-hydroxylase immunoreactive fibers in rat brain regions mediating arousal, motivation, and stress. J Comp Neurol. 2003;464:220–37. doi: 10.1002/cne.10783. [DOI] [PubMed] [Google Scholar]
- Baldo BA, Gual-Bonilla L, Sijapati K, Daniel RA, Landry CF, Kelley AE. Activation of a subpopulation of orexin/hypocretin-containing hypothalamic neurons by GABAA receptor-mediated inhibition of the nucleus accumbens shell, but not by exposure to a novel environment. Eur J Neurosci. 2004;19:376–86. doi: 10.1111/j.1460-9568.2004.03093.x. [DOI] [PubMed] [Google Scholar]
- Balleine BW, Delgado MR, Hikosaka O. The Role of the Dorsal Striatum in Reward and Decision-Making. J Neurosci. 2007;27:8161–8165. doi: 10.1523/JNEUROSCI.1554-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbano MF, Cador M. Opioids for hedonic experience and dopamine to get ready for it. Psychopharmacology (Berl) 2007;191:497–506. doi: 10.1007/s00213-006-0521-1. [DOI] [PubMed] [Google Scholar]
- Bartoshuk LM, Duffy VB, Hayes JE, Moskowitz HR, Snyder DJ. Psychophysics of sweet and fat perception in obesity: problems, solutions and new perspectives. Philos Trans R Soc Lond B Biol Sci. 2006;361:1137–48. doi: 10.1098/rstb.2006.1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaver J, Lawrence A, van Ditzhuijzen J, Davis M, Woods A, Calder A. Individual differences in reward drive predict neural responses to images of food. J Neurosci. 2006;26:5160–6. doi: 10.1523/JNEUROSCI.0350-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell SM, Stewart RB, Thompson SC, Meisch RA. Food-deprivation increases cocaine-induced conditioned place preference and locomotor activity in rats. Psychopharmacology. 1997;131:1–8. doi: 10.1007/s002130050258. [DOI] [PubMed] [Google Scholar]
- Bello NT, Sweigart KL, Lakoski JM, Norgren R, Hajnal A. Restricted feeding with scheduled sucrose access results in an upregulation of the rat dopamine transporter. Am J Physiol Regul Integr Comp Physiol. 2003;284:R1260–8. doi: 10.1152/ajpregu.00716.2002. [DOI] [PubMed] [Google Scholar]
- Berns GS, McClure SM, Pagnoni G, Montague PR. Predictability modulates human brain response to reward. Journal of Neuroscience. 2001;21:2793–2798. doi: 10.1523/JNEUROSCI.21-08-02793.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge CW, Espana RA, Vittoz NM. Hypocretin/orexin in arousal and stress. Brain Res. 2009 doi: 10.1016/j.brainres.2009.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge KC, Fentress JC. Contextual control of trigeminal sensorimotor function. Journal of Neuroscience. 1986;6:325–30. doi: 10.1523/JNEUROSCI.06-02-00325.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge KC, Schulkin J. Palatability shift of a salt-associated incentive during sodium depletion. Quarterly Journal of Experimental Psychology [b] 1989;41:121–38. [PubMed] [Google Scholar]
- Berridge KC. Comparative fine structure of action: Rules of form and sequence in the grooming patterns of six rodent species. Behaviour. 1990;113:21–56. [Google Scholar]
- Berridge KC. Modulation of taste affect by hunger, caloric satiety, and sensory- specific satiety in the rat. Appetite. 1991;16:103–20. doi: 10.1016/0195-6663(91)90036-r. [DOI] [PubMed] [Google Scholar]
- Berridge KC, Valenstein ES. What psychological process mediates feeding evoked by electrical stimulation of the lateral hypothalamus? Behavioral Neuroscience. 1991;105:3–14. doi: 10.1037//0735-7044.105.1.3. [DOI] [PubMed] [Google Scholar]
- Berridge KC, Robinson TE. What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Research Reviews. 1998;28:309–69. doi: 10.1016/s0165-0173(98)00019-8. [DOI] [PubMed] [Google Scholar]
- Berridge KC. Measuring hedonic impact in animals and infants: microstructure of affective taste reactivity patterns. Neuroscience & Biobehavioral Reviews. 2000;24:173–98. doi: 10.1016/s0149-7634(99)00072-x. [DOI] [PubMed] [Google Scholar]
- Berridge KC. Pleasures of the brain. Brain and Cognition. 2003;52:106–28. doi: 10.1016/s0278-2626(03)00014-9. [DOI] [PubMed] [Google Scholar]
- Berridge KC, Kringelbach ML. Affective neuroscience of pleasure: reward in humans and animals. Psychopharmacology (Berl) 2008;199:457–80. doi: 10.1007/s00213-008-1099-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berridge KC. ‘Liking’ and ‘wanting’ food rewards: Brain substrates and roles in eating disorders. Physiology & Behavior. 2009;97:537–550. doi: 10.1016/j.physbeh.2009.02.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berthoud HR, Morrison C. The brain, appetite, and obesity. Annu Rev Psychol. 2008;59:55–92. doi: 10.1146/annurev.psych.59.103006.093551. [DOI] [PubMed] [Google Scholar]
- Bhatnagar S, Bell ME, Liang J, Soriano L, Nagy TR, Dallman MF. Corticosterone facilitates saccharin intake in adrenalectomized rats: does corticosterone increase stimulus salience? J Neuroendocrinol. 2000;12:453–60. doi: 10.1046/j.1365-2826.2000.00487.x. [DOI] [PubMed] [Google Scholar]
- Bloom FE, Rossier J, Battenberg EL, Bayon A, French E, Henriksen SJ, Siggins GR, Segal D, Browne R, Ling N, Guillemin R. beta-endorphin: cellular localization, electrophysiological and behavioral effects. Adv Biochem Psychopharmacol. 1978;18:89–109. [PubMed] [Google Scholar]
- Bodnar RJ, Lamonte N, Israel Y, Kandov Y, Ackerman TF, Khaimova E. Reciprocal opioid-opioid interactions between the ventral tegmental area and nucleus accumbens regions in mediating mu, agonist-induced feeding in rats. Peptides. 2005;26:621–629. doi: 10.1016/j.peptides.2004.11.007. [DOI] [PubMed] [Google Scholar]
- Borgland SL, Chang S-J, Bowers MS, Thompson JL, Vittoz N, Floresco SB, Chou J, Chen BT, Bonci A. Orexin A/Hypocretin-1 Selectively Promotes Motivation for Positive Reinforcers. J Neurosci. 2009;29:11215–11225. doi: 10.1523/JNEUROSCI.6096-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brauer LH, De Wit H. High dose pimozide does not block amphetamine-induced euphoria in normal volunteers. Pharmacology Biochemistry and Behavior. 1997;56:265–72. doi: 10.1016/s0091-3057(96)00240-7. [DOI] [PubMed] [Google Scholar]
- Brauer LH, Goudie AJ, de Wit H. Dopamine ligands and the stimulus effects of amphetamine: animal models versus human laboratory data. Psychopharmacology. 1997;130:2–13. doi: 10.1007/s002130050207. [DOI] [PubMed] [Google Scholar]
- Brownell KD, Schwartz MB, Puhl RM, Henderson KE, Harris JL. The need for bold action to prevent adolescent obesity. J Adolesc Health. 2009;45:S8–17. doi: 10.1016/j.jadohealth.2009.03.004. [DOI] [PubMed] [Google Scholar]
- Cabanac M. Physiological role of pleasure. Science. 1971;173:1103–7. doi: 10.1126/science.173.4002.1103. [DOI] [PubMed] [Google Scholar]
- Cabanac M. Sensory pleasure. Quarterly Review of Biology. 1979;54:1–29. doi: 10.1086/410981. [DOI] [PubMed] [Google Scholar]
- Cabanac M, Lafrance L. Postingestive alliesthesia: the rat tells the same story. Physiology and Behavior. 1990;47:539–43. doi: 10.1016/0031-9384(90)90123-l. [DOI] [PubMed] [Google Scholar]
- Cabanac M. The dialectics of pleasure. In: Kringelbach ML, Berridge KC, editors. Pleasures of the brain. Oxford University Press; Oxford, U.K: 2010. pp. 113–124. [Google Scholar]
- Calder A, Beaver J, Davis M, van Ditzhuijzen J, Keane J, Lawrence A. Disgust sensitivity predicts the insula and pallidal response to pictures of disgusting foods. Eur J Neurosci. 2007;25:3422–8. doi: 10.1111/j.1460-9568.2007.05604.x. [DOI] [PubMed] [Google Scholar]
- Campbell BC, Eisenberg D. Obesity, attention deficit-hyperactivity disorder and the dopaminergic reward system. Collegium Antropologicum. 2007;31:33–8. [PubMed] [Google Scholar]
- Cannon CM, Palmiter RD. Reward without Dopamine. J Neurosci. 2003;23:10827–10831. doi: 10.1523/JNEUROSCI.23-34-10827.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon CM, Abdallah L, Tecott LH, During MJ, Palmiter RD. Dysregulation of Striatal Dopamine Signaling by Amphetamine Inhibits Feeding by Hungry Mice. Neuron. 2004;44:509–520. doi: 10.1016/j.neuron.2004.10.009. [DOI] [PubMed] [Google Scholar]
- Cardinal RN, Parkinson JA, Hall J, Everitt BJ. Emotion and motivation: the role of the amygdala, ventral striatum, and prefrontal cortex. Neuroscience and Biobehavioral Reviews. 2002;26:321–352. doi: 10.1016/s0149-7634(02)00007-6. [DOI] [PubMed] [Google Scholar]
- Carr KD. Augmentation of drug reward by chronic food restriction: Behavioral evidence and underlying mechanisms. Physiology & Behavior. 2002;76:353–364. doi: 10.1016/s0031-9384(02)00759-x. [DOI] [PubMed] [Google Scholar]
- Carr KD. Chronic food restriction: enhancing effects on drug reward and striatal cell signaling. Physiol Behav. 2007;91:459–72. doi: 10.1016/j.physbeh.2006.09.021. [DOI] [PubMed] [Google Scholar]
- Castellanos EH, Charboneau E, Dietrich MS, Park S, Bradley BP, Mogg K, Cowan RL. Obese adults have visual attention bias for food cue images: evidence for altered reward system function. Int J Obes (Lond) 2009;33:1063–73. doi: 10.1038/ijo.2009.138. [DOI] [PubMed] [Google Scholar]
- Childress AR, Ehrman RN, Wang Z, Li Y, Sciortino N, Hakun J, Jens W, Suh J, Listerud J, Marquez K, Franklin T, Langleben D, Detre J, O’Brien CP. Prelude to Passion: Limbic Activation by ‘Unseen’ Drug and Sexual Cues. PLoS ONE. 2008;3:e1506. doi: 10.1371/journal.pone.0001506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi DL, Davis JF, Fitzgerald ME, Benoit SC. The role of orexin-A in food motivation, reward-based feeding behavior and food-induced neuronal activation in rats. Neuroscience. 2010;167:11–20. doi: 10.1016/j.neuroscience.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Ciccocioppo R, Fedeli A, Economidou D, Policani F, Weiss F, Massi M. The bed nucleus is a neuroanatomical substrate for the anorectic effect of corticotropin-releasing factor and for its reversal by nociceptin/orphanin FQ. J Neurosci. 2003;23:9445–51. doi: 10.1523/JNEUROSCI.23-28-09445.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cocores JA, Gold MS. The Salted Food Addiction Hypothesis may explain overeating and the obesity epidemic. Med Hypotheses. 2009 doi: 10.1016/j.mehy.2009.06.049. [DOI] [PubMed] [Google Scholar]
- Colantuoni C, Schwenker J, McCarthy J, Rada P, Ladenheim B, Cadet JL, Schwartz GJ, Moran TH, Hoebel BG. Excessive sugar intake alters binding to dopamine and mu-opioid receptors in the brain. Neuroreport. 2001;12:3549–3552. doi: 10.1097/00001756-200111160-00035. [DOI] [PubMed] [Google Scholar]
- Cooper SJ, Higgs S. Neuropharmacology of appetite and taste preferences. In: Legg CR, Booth DA, editors. Appetite: Neural and Behavioural Bases. Oxford University Press; New York: 1994. pp. 212–242. [Google Scholar]
- Cooper SJ. Endocannabinoids and food consumption: comparisons with benzodiazepine and opioid palatability-dependent appetite. Eur J Pharmacol. 2004;500:37–49. doi: 10.1016/j.ejphar.2004.07.009. [DOI] [PubMed] [Google Scholar]
- Cope MB, Nagy TR, Fernandez JR, Geary N, Casey DE, Allison DB. Antipsychotic drug-induced weight gain: development of an animal model. Int J Obes (Lond) 2005;29:607–14. doi: 10.1038/sj.ijo.0802928. [DOI] [PubMed] [Google Scholar]
- Corwin RL, Grigson PS. Symposium overview--Food addiction: fact or fiction? J Nutr. 2009;139:617–9. doi: 10.3945/jn.108.097691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cota D, Tschop MH, Horvath TL, Levine AS. Cannabinoids, opioids and eating behavior: the molecular face of hedonism? Brain Res Rev. 2006;51:85–107. doi: 10.1016/j.brainresrev.2005.10.004. [DOI] [PubMed] [Google Scholar]
- Cottone P, Sabino V, Roberto M, Bajo M, Pockros L, Frihauf JB, Fekete EM, Steardo L, Rice KC, Grigoriadis DE, Conti B, Koob GF, Zorrilla EP. CRF system recruitment mediates dark side of compulsive eating. Proc Natl Acad Sci U S A. 2009;106:20016–20. doi: 10.1073/pnas.0908789106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig AD. How do you feel? Interoception: the sense of the physiological condition of the body. Nat Rev Neurosci. 2002;3:655–66. doi: 10.1038/nrn894. [DOI] [PubMed] [Google Scholar]
- Cromwell HC, Berridge KC. Where does damage lead to enhanced food aversion: the ventral pallidum/substantia innominata or lateral hypothalamus? Brain Research. 1993;624:1–10. doi: 10.1016/0006-8993(93)90053-p. [DOI] [PubMed] [Google Scholar]
- Dagher A. The neurobiology of appetite: hunger as addiction. Int J Obes (Lond) 2009;33(Suppl 2):S30–3. doi: 10.1038/ijo.2009.69. [DOI] [PubMed] [Google Scholar]
- Dallman MF. Fast glucocorticoid feedback favors ‘the munchies’. Trends Endocrinol Metab. 2003;14:394–6. doi: 10.1016/j.tem.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Dallman MF, Pecoraro N, Akana SF, La Fleur SE, Gomez F, Houshyar H, Bell ME, Bhatnagar S, Laugero KD, Manalo S. Chronic stress and obesity: a new view of “comfort food”. Proc Natl Acad Sci U S A. 2003;100:11696–701. doi: 10.1073/pnas.1934666100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallman MF, Pecoraro NC, La Fleur SE, Warne JP, Ginsberg AB, Akana SF, Laugero KC, Houshyar H, Strack AM, Bhatnagar S, Bell ME. Glucocorticoids, chronic stress, and obesity. Prog Brain Res. 2006;153:75–105. doi: 10.1016/S0079-6123(06)53004-3. [DOI] [PubMed] [Google Scholar]
- Dallman MF. Stress-induced obesity and the emotional nervous system. Trends Endocrinol Metab. 2010;21:159–65. doi: 10.1016/j.tem.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C, Strachan S, Berkson M. Sensitivity to reward: implications for overeating and overweight. Appetite. 2004;42:131–8. doi: 10.1016/j.appet.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Davis C, Levitan RD, Kaplan AS, Carter J, Reid C, Curtis C, Patte K, Hwang R, Kennedy JL. Reward sensitivity and the D2 dopamine receptor gene: A case-control study of binge eating disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:620–8. doi: 10.1016/j.pnpbp.2007.09.024. [DOI] [PubMed] [Google Scholar]
- Davis C, Carter JC. Compulsive overeating as an addiction disorder. A review of theory and evidence Appetite. 2009;53:1–8. doi: 10.1016/j.appet.2009.05.018. [DOI] [PubMed] [Google Scholar]
- Davis CA, Levitan RD, Reid C, Carter JC, Kaplan AS, Patte KA, King N, Curtis C, Kennedy JL. Dopamine for “Wanting” and Opioids for “Liking”: A Comparison of Obese Adults With and Without Binge Eating. Obesity. 2009 doi: 10.1038/oby.2009.52. [DOI] [PubMed] [Google Scholar]
- de Araujo IE, Rolls ET, Kringelbach ML, McGlone F, Phillips N. Taste-olfactory convergence, and the representation of the pleasantness of flavour, in the human brain. Eur J Neurosci. 2003;18:2059–68. doi: 10.1046/j.1460-9568.2003.02915.x. [DOI] [PubMed] [Google Scholar]
- de Vaca SC, Carr KD. Food restriction enhances the central rewarding effect of abused drugs. Journal of Neuroscience. 1998;18:7502–7510. doi: 10.1523/JNEUROSCI.18-18-07502.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Chiara G. Nucleus accumbens shell and core dopamine: differential role in behavior and addiction. Behavioural Brain Research. 2002;137:75–114. doi: 10.1016/s0166-4328(02)00286-3. [DOI] [PubMed] [Google Scholar]
- Dickinson A, Balleine B. The role of learning in the operation of motivational systems. In: Gallistel CR, editor. Stevens’ Handbook of Experimental Psychology: Learning, Motivation, and Emotion. Wiley and Sons; New York: 2002. pp. 497–534. [Google Scholar]
- Espana RA, Baldo BA, Kelley AE, Berridge CW. Wake-promoting and sleep-suppressing actions of hypocretin (orexin): Basal forebrain sites of action. Neuroscience. 2001;106:699–715. doi: 10.1016/s0306-4522(01)00319-0. [DOI] [PubMed] [Google Scholar]
- Evans KR, Vaccarino FJ. Intra-nucleus accumbens amphetamine: dose-dependent effects on food intake. Pharmacology Biochemistry and Behavior. 1986;25:1149–51. doi: 10.1016/0091-3057(86)90102-4. [DOI] [PubMed] [Google Scholar]
- Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8:1481–1489. doi: 10.1038/nn1579. [DOI] [PubMed] [Google Scholar]
- Farooqi IS, Bullmore E, Keogh J, Gillard J, O’Rahilly S, Fletcher PC. Leptin regulates striatal regions and human eating behavior. Science. 2007;317:1355. doi: 10.1126/science.1144599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooqi IS, O’Rahilly S. Leptin: a pivotal regulator of human energy homeostasis. Am J Clin Nutr. 2009;89:980S–984S. doi: 10.3945/ajcn.2008.26788C. [DOI] [PubMed] [Google Scholar]
- Faure A, Reynolds SM, Richard JM, Berridge KC. Mesolimbic dopamine in desire and dread: enabling motivation to be generated by localized glutamate disruptions in nucleus accumbens. J Neurosci. 2008;28:7184–92. doi: 10.1523/JNEUROSCI.4961-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figlewicz DP, MacDonald Naleid A, Sipols AJ. Modulation of food reward by adiposity signals. Physiol Behav. 2007;91:473–8. doi: 10.1016/j.physbeh.2006.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figlewicz DP, Benoit SC. Insulin, leptin, and food reward: update 2008. Am J Physiol Regul Integr Comp Physiol. 2009;296:R9–R19. doi: 10.1152/ajpregu.90725.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlayson G, King N, Blundell JE. Liking vs. wanting food: importance for human appetite control and weight regulation. Neurosci Biobehav Rev. 2007;31:987–1002. doi: 10.1016/j.neubiorev.2007.03.004. [DOI] [PubMed] [Google Scholar]
- Flagel SB, Akil H, Robinson TE. Individual differences in the attribution of incentive salience to reward-related cues: Implications for addiction. europharmacology. 2008 doi: 10.1016/j.neuropharm.2008.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman JM, Halaas JL. Leptin and the regulation of body weight in mammals. Nature. 1998;395:763–70. doi: 10.1038/27376. [DOI] [PubMed] [Google Scholar]
- Fulton S, Pissios P, Manchon R, Stiles L, Frank L, Pothos EN, Maratos-Flier E, Flier JS. Leptin Regulation of the Mesoaccumbens Dopamine Pathway. Neuron. 2006;51:811–822. doi: 10.1016/j.neuron.2006.09.006. [DOI] [PubMed] [Google Scholar]
- Gao Q, Horvath TL. Neurobiology of feeding and energy expenditure. Annu Rev Neurosci. 2007;30:367–98. doi: 10.1146/annurev.neuro.30.051606.094324. [DOI] [PubMed] [Google Scholar]
- Garcia J, Lasiter PS, Bermudez-Rattoni F, Deems DA. A general theory of aversion learning. Ann N Y Acad Sci. 1985;443:8–21. doi: 10.1111/j.1749-6632.1985.tb27060.x. [DOI] [PubMed] [Google Scholar]
- Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale Food Addiction Scale. Appetite. 2009;52:430–6. doi: 10.1016/j.appet.2008.12.003. [DOI] [PubMed] [Google Scholar]
- Geier AB, Rozin P, Doros G. Unit bias. A new heuristic that helps explain the effect of portion size on food intake. Psychol Sci. 2006;17:521–5. doi: 10.1111/j.1467-9280.2006.01738.x. [DOI] [PubMed] [Google Scholar]
- Geiger BM, Haburcak M, Avena NM, Moyer MC, Hoebel BG, Pothos EN. Deficits of mesolimbic dopamine neurotransmission in rat dietary obesity. Neuroscience. 2009;159:1193–9. doi: 10.1016/j.neuroscience.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosnell BA. Sucrose intake enhances behavioral sensitization produced by cocaine. Brain Res. 2005;1031:194–201. doi: 10.1016/j.brainres.2004.10.037. [DOI] [PubMed] [Google Scholar]
- Grigson PS. Like drugs for chocolate: separate rewards modulated by common mechanisms? Physiol Behav. 2002;76:389–95. doi: 10.1016/s0031-9384(02)00758-8. [DOI] [PubMed] [Google Scholar]
- Grill HJ, Norgren R. Chronically decerebrate rats demonstrate satiation but not bait shyness. Science. 1978a;201:267–9. doi: 10.1126/science.663655. [DOI] [PubMed] [Google Scholar]
- Grill HJ, Norgren R. The taste reactivity test. I. Mimetic responses to gustatory stimuli in neurologically normal rats. Brain Research. 1978b;143:263–79. doi: 10.1016/0006-8993(78)90568-1. [DOI] [PubMed] [Google Scholar]
- Grill HJ. Leptin and the systems neuroscience of meal size control. Front Neuroendocrinol. 2010;31:61–78. doi: 10.1016/j.yfrne.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajnal A, Norgren R. Taste pathways that mediate accumbens dopamine release by sapid sucrose. Physiology & Behavior. 2005;84:363–369. doi: 10.1016/j.physbeh.2004.12.014. [DOI] [PubMed] [Google Scholar]
- Harris GC, Wimmer M, Aston-Jones G. A role for lateral hypothalamic orexin neurons in reward seeking. Nature. 2005;437:556–9. doi: 10.1038/nature04071. [DOI] [PubMed] [Google Scholar]
- Harris GC, Aston-Jones G. Arousal and reward: a dichotomy in orexin function. Trends in Neurosciences. 2006;29:571–577. doi: 10.1016/j.tins.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Heimer L, Van Hoesen GW. The limbic lobe and its output channels: Implications for emotional functions and adaptive behavior. Neuroscience & Biobehavioral Reviews. 2006;30:126–147. doi: 10.1016/j.neubiorev.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hernandez G, Rajabi H, Stewart J, Arvanitogiannis A, Shizgal P. Dopamine tone increases similarly during predictable and unpredictable administration of rewarding brain stimulation at short inter-train intervals. Behav Brain Res. 2008;188:227–32. doi: 10.1016/j.bbr.2007.10.035. [DOI] [PubMed] [Google Scholar]
- Higgs S, Williams CM, Kirkham TC. Cannabinoid influences on palatability: microstructural analysis of sucrose drinking after delta(9)-tetrahydrocannabinol, anandamide, 2-arachidonoyl glycerol and SR141716. Psychopharmacology (Berl) 2003;165:370–7. doi: 10.1007/s00213-002-1263-3. [DOI] [PubMed] [Google Scholar]
- Ho C-Y, Berridge KC. Society for Neuroscience 2009 Abstracts. Vol. 583.4. 2009. Hotspots for hedonic ‘liking’ and aversive ‘disliking’ in ventral pallidum; p. GG81. [Google Scholar]
- Holland PC, Petrovich GD. A neural systems analysis of the potentiation of feeding by conditioned stimuli. Physiol Behav. 2005;86:747–61. doi: 10.1016/j.physbeh.2005.08.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hommel JD, Trinko R, Sears RM, Georgescu D, Liu ZW, Gao XB, Thurmon JJ, Marinelli M, Dileone RJ. Leptin receptor signaling in midbrain dopamine neurons regulates feeding. Neuron. 2006;51:801–10. doi: 10.1016/j.neuron.2006.08.023. [DOI] [PubMed] [Google Scholar]
- Ifland JR, Preuss HG, Marcus MT, Rourke KM, Taylor WC, Burau K, Jacobs WS, Kadish W, Manso G. Refined food addiction: A classic substance use disorder. Med Hypotheses. 2009 doi: 10.1016/j.mehy.2008.11.035. [DOI] [PubMed] [Google Scholar]
- Inoue K, Kiriike N, Kurioka M, Fujisaki Y, Iwasaki S, Yamagami S. Bromocriptine Enhances Feeding Behavior Without Changing Dopamine Metabolism. Pharmacology Biochemistry and Behavior. 1997;58:183–188. doi: 10.1016/s0091-3057(97)00004-x. [DOI] [PubMed] [Google Scholar]
- James W. What is an emotion. Mind. 1884;9:188–205. [Google Scholar]
- Jarrett MM, Limebeer CL, Parker LA. Effect of Delta9-tetrahydrocannabinol on sucrose palatability as measured by the taste reactivity test. Physiol Behav. 2005;86:475–9. doi: 10.1016/j.physbeh.2005.08.033. [DOI] [PubMed] [Google Scholar]
- Jenkins HM, Moore BR. The form of the auto-shaped response with food or water reinforcers. Journal of the Experimental Analysis of Behavior. 1973;20:163–81. doi: 10.1901/jeab.1973.20-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson PI, Stellar JR, Paul AD. Regional reward differences within the ventral pallidum are revealed by microinjections of a mu opiate receptor agonist. Neuropharmacology. 1993;32:1305–14. doi: 10.1016/0028-3908(93)90025-x. [DOI] [PubMed] [Google Scholar]
- Johnson PI, Parente MA, Stellar JR. NMDA-induced lesions of the nucleus accumbens or the ventral pallidum increase the rewarding efficacy of food to deprived rats. Brain Research. 1996;722:109–17. doi: 10.1016/0006-8993(96)00202-8. [DOI] [PubMed] [Google Scholar]
- Kalivas PW, Volkow ND. The neural basis of addiction: a pathology of motivation and choice. Am J Psychiatry. 2005;162:1403–13. doi: 10.1176/appi.ajp.162.8.1403. [DOI] [PubMed] [Google Scholar]
- Kaye WH, Fudge JL, Paulus M. New insights into symptoms and neurocircuit function of anorexia nervosa. Nat Rev Neurosci. 2009;10:573–84. doi: 10.1038/nrn2682. [DOI] [PubMed] [Google Scholar]
- Kelley AE, Bakshi VP, Haber SN, Steininger TL, Will MJ, Zhang M. Opioid modulation of taste hedonics within the ventral striatum. Physiology & Behavior. 2002;76:365–377. doi: 10.1016/s0031-9384(02)00751-5. [DOI] [PubMed] [Google Scholar]
- Kelley AE. Ventral striatal control of appetitive motivation: role in ingestive behavior and reward-related learning. Neuroscience and Biobehavioral Reviews. 2004;27:765–776. doi: 10.1016/j.neubiorev.2003.11.015. [DOI] [PubMed] [Google Scholar]
- Kelley AE, Baldo BA, Pratt WE. A proposed hypothalamic-thalamic-striatal axis for the integration of energy balance, arousal, and food reward. J Comp Neurol. 2005a;493:72–85. doi: 10.1002/cne.20769. [DOI] [PubMed] [Google Scholar]
- Kelley AE, Baldo BA, Pratt WE, Will MJ. Corticostriatal-hypothalamic circuitry and food motivation: Integration of energy, action and reward. Physiol Behav. 2005b;86:773–95. doi: 10.1016/j.physbeh.2005.08.066. [DOI] [PubMed] [Google Scholar]
- Kerfoot EC, Agarwal I, Lee HJ, Holland PC. Control of appetitive and aversive taste-reactivity responses by an auditory conditioned stimulus in a devaluation task: A FOS and behavioral analysis. Learn Mem. 2007;14:581–589. doi: 10.1101/lm.627007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler DA. The end of overeating : taking control of the insatiable American appetite. Rodale press (Macmillan); New York: 2009. p. 320. [Google Scholar]
- Kirkham T. Endocannabinoids and the Neurochemistry of Gluttony. J Neuroendocrinol. 2008 doi: 10.1111/j.1365-2826.2008.01762.x. [DOI] [PubMed] [Google Scholar]
- Kirkham TC, Williams CM. Endogenous cannabinoids and appetite. Nutrition Research Reviews. 2001;14:65–86. doi: 10.1079/NRR200118. [DOI] [PubMed] [Google Scholar]
- Kirkham TC, Williams CM, Fezza F, Di Marzo V. Endocannabinoid levels in rat limbic forebrain and hypothalamus in relation to fasting, feeding and satiation: stimulation of eating by 2-arachidonoyl glycerol. Br J Pharmacol. 2002;136:550–7. doi: 10.1038/sj.bjp.0704767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkham TC. Endocannabinoids in the regulation of appetite and body weight. Behav Pharmacol. 2005;16:297–313. doi: 10.1097/00008877-200509000-00004. [DOI] [PubMed] [Google Scholar]
- Koob G, Kreek MJ. Stress, dysregulation of drug reward pathways, and the transition to drug dependence. Am J Psychiatry. 2007;164:1149–59. doi: 10.1176/appi.ajp.2007.05030503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF. Allostatic view of motivation: implications for psychopathology. Nebr Symp Motiv. 2004;50:1–18. [PubMed] [Google Scholar]
- Koob GF, Le Moal M. Neurobiology of Addiction. Academic Press; New York: 2006. p. 490. [Google Scholar]
- Korotkova TM, Sergeeva OA, Eriksson KS, Haas HL, Brown RE. Excitation of Ventral Tegmental Area Dopaminergic and Nondopaminergic Neurons by Orexins/Hypocretins. J Neurosci. 2003;23:7–11. doi: 10.1523/JNEUROSCI.23-01-00007.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause EG, Sakai RR. Richter and sodium appetite: From adrenalectomy to molecular biology. Appetite. 2007 doi: 10.1016/j.appet.2007.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kringelbach ML, O’Doherty J, Rolls ET, Andrews C. Activation of the human orbitofrontal cortex to a liquid food stimulus is correlated with its subjective pleasantness. Cereb Cortex. 2003;13:1064–71. doi: 10.1093/cercor/13.10.1064. [DOI] [PubMed] [Google Scholar]
- Kringelbach ML. Food for thought: hedonic experience beyond homeostasis in the human brain. Neuroscience. 2004;126:807–19. doi: 10.1016/j.neuroscience.2004.04.035. [DOI] [PubMed] [Google Scholar]
- Kringelbach ML, de Araujo IE, Rolls ET. Taste-related activity in the human dorsolateral prefrontal cortex. Neuroimage. 2004;21:781–8. doi: 10.1016/j.neuroimage.2003.09.063. [DOI] [PubMed] [Google Scholar]
- Kringelbach ML. The human orbitofrontal cortex: linking reward to hedonic experience. Nat Rev Neurosci. 2005;6:691–702. doi: 10.1038/nrn1747. [DOI] [PubMed] [Google Scholar]
- Kringelbach ML. The hedonic brain: A functional neuroanatomy of human pleasure. In: Kringelbach ML, Berridge KC, editors. Pleasures of the brain. Oxford University Press; Oxford, U.K: 2010. pp. 202–221. [Google Scholar]
- Kringelbach ML, Berridge KC. Pleasures of the Brain. Oxford University Press; Oxford: 2010. p. 343. [Google Scholar]
- Kuo D-Y. Further evidence for the mediation of both subtypes of dopamine D1/D2 receptors and cerebral neuropeptide Y (NPY) in amphetamine-induced appetite suppression. Behavioural Brain Research. 2003;147:149–155. doi: 10.1016/j.bbr.2003.04.001. [DOI] [PubMed] [Google Scholar]
- Le Magnen J, Marfaing-Jallat P, Miceli D, Devos M. Pain modulating and reward systems: a single brain mechanism? Pharmacology, Biochemistry & Behavior. 1980;12:729–33. doi: 10.1016/0091-3057(80)90157-4. [DOI] [PubMed] [Google Scholar]
- Leinninger GM, Jo YH, Leshan RL, Louis GW, Yang H, Barrera JG, Wilson H, Opland DM, Faouzi MA, Gong Y, Jones JC, Rhodes CJ, Chua S, Jr, Diano S, Horvath TL, Seeley RJ, Becker JB, Munzberg H, Myers MG., Jr Leptin acts via leptin receptor-expressing lateral hypothalamic neurons to modulate the mesolimbic dopamine system and suppress feeding. Cell Metab. 2009;10:89–98. doi: 10.1016/j.cmet.2009.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemmens SGT, Schoffelen PFM, Wouters L, Born JM, Martens MJI, Rutters F, Westerterp-Plantenga MS. Eating what you like induces a stronger decrease of ‘wanting’ to eat. Physiology & Behavior. 2009;98:318–325. doi: 10.1016/j.physbeh.2009.06.008. [DOI] [PubMed] [Google Scholar]
- Levine AS, Kotz CM, Gosnell BA. Sugars: hedonic aspects, neuroregulation, and energy balance. Am J Clin Nutr. 2003;78:834S–842S. doi: 10.1093/ajcn/78.4.834S. [DOI] [PubMed] [Google Scholar]
- Levine AS, Billington CJ. Opioids as agents of reward-related feeding: a consideration of the evidence. Physiology & Behavior. 2004;82:57–61. doi: 10.1016/j.physbeh.2004.04.032. [DOI] [PubMed] [Google Scholar]
- Leyton M, Boileau I, Benkelfat C, Diksic M, Baker G, Dagher A. Amphetamine-Induced Increases in extracellular dopamine, drug wanting, and novelty seeking: a PET/[11C]raclopride study in healthy men. Neuropsychopharmacology. 2002;27:1027–1035. doi: 10.1016/S0893-133X(02)00366-4. [DOI] [PubMed] [Google Scholar]
- Leyton M. The neurobiology of desire: Dopamine and the regulation of mood and motivational states in humans. In: Kringelbach ML, Berridge KC, editors. Pleasures of the brain. Oxford University Press; Oxford, U.K: 2010. pp. 222–243. [Google Scholar]
- Lowe MR, Butryn ML. Hedonic hunger: a new dimension of appetite? Physiol Behav. 2007;91:432–9. doi: 10.1016/j.physbeh.2007.04.006. [DOI] [PubMed] [Google Scholar]
- Lundy RF., Jr Gustatory hedonic value: potential function for forebrain control of brainstem taste processing. Neurosci Biobehav Rev. 2008;32:1601–6. doi: 10.1016/j.neubiorev.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahler SV, Smith KS, Berridge KC. Endocannabinoid hedonic hotspot for sensory pleasure: anandamide in nucleus accumbens shell enhances ‘liking’ of a sweet reward. Neuropsychopharmacology. 2007;32:2267–78. doi: 10.1038/sj.npp.1301376. [DOI] [PubMed] [Google Scholar]
- Mahler SV, Berridge KC. Which cue to ‘want?” Central amygdala opioid activation enhances and focuses incentive salience on a prepotent reward cue. J Neurosci. 2009;29:6500–6513. doi: 10.1523/JNEUROSCI.3875-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsui-Sakata A, Ohtani H, Sawada Y. Receptor occupancy-based analysis of the contributions of various receptors to antipsychotics-induced weight gain and diabetes mellitus. Drug Metab Pharmacokinet. 2005;20:368–78. doi: 10.2133/dmpk.20.368. [DOI] [PubMed] [Google Scholar]
- McFarland K, Davidge SB, Lapish CC, Kalivas PW. Limbic and Motor Circuitry Underlying Footshock-Induced Reinstatement of Cocaine-Seeking Behavior. J Neurosci. 2004;24:1551–1560. doi: 10.1523/JNEUROSCI.4177-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mela DJ. Eating for pleasure or just wanting to eat? Reconsidering sensory hedonic responses as a driver of obesity. Appetite. 2006;47:10–7. doi: 10.1016/j.appet.2006.02.006. [DOI] [PubMed] [Google Scholar]
- Merali Z, Michaud D, McIntosh J, Kent P, Anisman H. Differential involvement of amygdaloid CRH system(s) in the salience and valence of the stimuli. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27:1201–12. doi: 10.1016/j.pnpbp.2003.09.014. [DOI] [PubMed] [Google Scholar]
- Miller JM, Vorel SR, Tranguch AJ, Kenny ET, Mazzoni P, van Gorp WG, Kleber HD. Anhedonia after a selective bilateral lesion of the globus pallidus. Am J Psychiatry. 2006;163:786–8. doi: 10.1176/ajp.2006.163.5.786. [DOI] [PubMed] [Google Scholar]
- Montague PR, Hyman SE, Cohen JD. Computational roles for dopamine in behavioural control. Nature. 2004;431:760–767. doi: 10.1038/nature03015. [DOI] [PubMed] [Google Scholar]
- Morgane PJ, Mokler DJ. The limbic brain: Continuing resolution. Neuroscience & Biobehavioral Reviews. 2006;30:119–125. doi: 10.1016/j.neubiorev.2005.04.020. [DOI] [PubMed] [Google Scholar]
- Muschamp JW, Dominguez JM, Sato SM, Shen R-Y, Hull EM. A Role for Hypocretin (Orexin) in Male Sexual Behavior. J Neurosci. 2007;27:2837–2845. doi: 10.1523/JNEUROSCI.4121-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers MG., Jr Metabolic sensing and regulation by the hypothalamus. Am J Physiol Endocrinol Metab. 2008;294:E809. doi: 10.1152/ajpendo.90282.2008. [DOI] [PubMed] [Google Scholar]
- Myers MG, Jr, Munzberg H, Leinninger GM, Leshan RL. The geometry of leptin action in the brain: more complicated than a simple ARC. Cell Metab. 2009;9:117–23. doi: 10.1016/j.cmet.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napier TC, Mitrovic I. Opioid modulation of ventral pallidal inputs. Annals of the New York Academy of Sciences. 1999;877:176–201. doi: 10.1111/j.1749-6632.1999.tb09268.x. [DOI] [PubMed] [Google Scholar]
- Nijs IM, Muris P, Euser AS, Franken IH. Differences in attention to food and food intake between overweight/obese and normal-weight females under conditions of hunger and satiety. Appetite. 2009 doi: 10.1016/j.appet.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Nisbett RE, Kanouse DE. Obesity, food deprivation, and supermarket shopping behavior. Journal of Personality & Social Psychology. 1969;12:289–94. doi: 10.1037/h0027799. [DOI] [PubMed] [Google Scholar]
- Nixon JP, Smale L. A comparative analysis of the distribution of immunoreactive orexin A and B in the brains of nocturnal and diurnal rodents. Behav Brain Funct. 2007;3:28. doi: 10.1186/1744-9081-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norgren R, Hajnal A, Mungarndee SS. Gustatory reward and the nucleus accumbens. Physiol Behav. 2006;89:531–5. doi: 10.1016/j.physbeh.2006.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Doherty J, Kringelbach ML, Rolls ET, Hornak J, Andrews C. Nature Neuroscience. US Nature America Inc; 2001. Abstract reward and punishment representations in the human orbitofrontal cortex; pp. 95–102. [DOI] [PubMed] [Google Scholar]
- O’Doherty JP, Deichmann R, Critchley HD, Dolan RJ. Neural responses during anticipation of a primary taste reward. Neuron. 2002;33:815–826. doi: 10.1016/s0896-6273(02)00603-7. [DOI] [PubMed] [Google Scholar]
- Pal GK, Thombre DP. Modulation of feeding and drinking by dopamine in caudate and accumbens nuclei in rats. Indian J Exp Biol. 1993;31:750–4. [PubMed] [Google Scholar]
- Palmiter RD. Is dopamine a physiologically relevant mediator of feeding behavior? Trends Neurosci. 2007;30:375–81. doi: 10.1016/j.tins.2007.06.004. [DOI] [PubMed] [Google Scholar]
- Panksepp J. The neurochemistry of behavior. Annual Review of Psychology. 1986;37:77–107. doi: 10.1146/annurev.ps.37.020186.000453. [DOI] [PubMed] [Google Scholar]
- Parker LA. Rewarding drugs produce taste avoidance, but not taste aversion. Neurosci Biobeh Rev. 1995;19:143–151. doi: 10.1016/0149-7634(94)00028-y. [DOI] [PubMed] [Google Scholar]
- Pecina S, Schulkin J, Berridge KC. Nucleus accumbens corticotropin-releasing factor increases cue-triggered motivation for sucrose reward: paradoxical positive incentive effects in stress? BMC Biol. 2006;4:8. doi: 10.1186/1741-7007-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pecina S. Opioid reward ‘liking’ and ‘wanting’ in the nucleus accumbens. Physiol Behav. 2008;94:675–80. doi: 10.1016/j.physbeh.2008.04.006. [DOI] [PubMed] [Google Scholar]
- Peciña S, Berridge KC, Parker LA. Pimozide does not shift palatability: separation of anhedonia from sensorimotor suppression by taste reactivity. Pharmacol Biochem Behav. 1997;58:801–11. doi: 10.1016/s0091-3057(97)00044-0. [DOI] [PubMed] [Google Scholar]
- Peciña S, Cagniard B, Berridge KC, Aldridge JW, Zhuang X. Hyperdopaminergic mutant mice have higher “wanting” but not “liking” for sweet rewards. Journal of Neuroscience. 2003;23:9395–9402. doi: 10.1523/JNEUROSCI.23-28-09395.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peciña S, Berridge KC. Hedonic hot spot in nucleus accumbens shell: Where do mu-opioids cause increased hedonic impact of sweetness? J. Neurosci. 2005;25:11777–11786. doi: 10.1523/JNEUROSCI.2329-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peciña S, Smith KS, Berridge KC. Hedonic hot spots in the brain. Neuroscientist. 2006;12:500–11. doi: 10.1177/1073858406293154. [DOI] [PubMed] [Google Scholar]
- Pelchat ML, Johnson A, Chan R, Valdez J, Ragland JD. Images of desire: food-craving activation during fMRI. 2004;23:1486–1493. doi: 10.1016/j.neuroimage.2004.08.023. [DOI] [PubMed] [Google Scholar]
- Pelchat ML. Food addiction in humans. J Nutr. 2009;139:620–2. doi: 10.3945/jn.108.097816. [DOI] [PubMed] [Google Scholar]
- Pessiglione M, Schmidt L, Draganski B, Kalisch R, Lau H, Dolan R, Frith C. How the brain translates money into force: a neuroimaging study of subliminal motivation. Science. 2007;316:904–6. doi: 10.1126/science.1140459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrovich GD, Gallagher M. Control of food consumption by learned cues: a forebrain-hypothalamic network. Physiol Behav. 2007;91:397–403. doi: 10.1016/j.physbeh.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peyron C, Tighe DK, van den Pol AN, de Lecea L, Heller HC, Sutcliffe JG, Kilduff TS. Neurons containing hypocretin (orexin) project to multiple neuronal systems. J Neurosci. 1998;18:9996–10015. doi: 10.1523/JNEUROSCI.18-23-09996.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaffmann C, Norgren R, Grill HJ. Sensory affect and motivation. Ann N Y Acad Sci. 1977;290:18–34. doi: 10.1111/j.1749-6632.1977.tb39713.x. [DOI] [PubMed] [Google Scholar]
- Piazza PV, Deroche V, Deminiere JM, Maccari S, Le Moal M, Simon H. Corticosterone in the range of stress-induced levels possesses reinforcing properties: implications for sensation-seeking behaviors. Proc Natl Acad Sci U S A. 1993;90:11738–42. doi: 10.1073/pnas.90.24.11738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piomelli D. The molecular logic of endocannabinoid signalling. Nature Reviews Neuroscience. 2003;4:873–884. doi: 10.1038/nrn1247. [DOI] [PubMed] [Google Scholar]
- Prevention CfDCa. US Obesity Trends: Trends by State 1985–2008. US Government; 2009. [Google Scholar]
- Reilly S, Schachtman TR. Conditioned Taste Aversion: Behavioral and Neural Processes. Oxford University Press; New York: 2009. p. 529. [Google Scholar]
- Reynolds SM, Berridge KC. Emotional environments retune the valence of appetitive versus fearful functions in nucleus accumbens. Nat Neurosci. 2008;11:423–5. doi: 10.1038/nn2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson SA, Leinninger GM, Myers MG., Jr Molecular and neural mediators of leptin action. Physiology & Behavior. 2008;94:637–642. doi: 10.1016/j.physbeh.2008.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson S, Sandstrom SM, Denenberg VH, Palmiter RD. Distinguishing whether dopamine regulates liking, wanting, and/or learning about rewards. Behav Neurosci. 2005;119:5–15. doi: 10.1037/0735-7044.119.1.5. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Research Reviews. 1993;18:247–91. doi: 10.1016/0165-0173(93)90013-p. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. Addiction. Annual Review of Psychology. 2003;54:25–53. doi: 10.1146/annurev.psych.54.101601.145237. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. Review. The incentive sensitization theory of addiction: some current issues. Philos Trans R Soc Lond B Biol Sci. 2008;363:3137–46. doi: 10.1098/rstb.2008.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers PJ, Smit HJ. Food Craving and Food “Addiction”: A Critical Review of the Evidence From a Biopsychosocial Perspective. Pharmacology Biochemistry and Behavior. 2000;66:3–14. doi: 10.1016/s0091-3057(00)00197-0. [DOI] [PubMed] [Google Scholar]
- Roitman MF, Stuber GD, Phillips PEM, Wightman RM, Carelli RM. Dopamine Operates as a Subsecond Modulator of Food Seeking. J Neurosci. 2004;24:1265–1271. doi: 10.1523/JNEUROSCI.3823-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roitman MF, Wheeler RA, Wightman RM, Carelli RM. Real-time chemical responses in the nucleus accumbens differentiate rewarding and aversive stimuli. Nat Neurosci. 2008;11:1376–1377. doi: 10.1038/nn.2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolls E. Brain mechanisms underlying flavour and appetite. Phil Trans R Soc Lond B. 2006;361:1123–1136. doi: 10.1098/rstb.2006.1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolls ET, Kringelbach ML, de Araujo IE. Different representations of pleasant and unpleasant odours in the human brain. Eur J Neurosci. 2003;18:695–703. doi: 10.1046/j.1460-9568.2003.02779.x. [DOI] [PubMed] [Google Scholar]
- Rolls ET. Series in affective science. Oxford University Press; Oxford ; New York: 2005. Emotion explained; p. xvii.p. 606. [Google Scholar]
- Rozin P. Disgust. In: Lewis M, Haviland-Jones JM, editors. Handbook of Emotions. Guilford; New York: 2000. pp. 637–653. [Google Scholar]
- Sarter M, Parikh V. Choline transporters, cholinergic transmission and cognition. Nat Rev Neurosci. 2005;6:48–56. doi: 10.1038/nrn1588. [DOI] [PubMed] [Google Scholar]
- Scammell TE, Saper CB. Orexin, drugs and motivated behaviors. Nat Neurosci. 2005;8:1286–8. doi: 10.1038/nn1005-1286. [DOI] [PubMed] [Google Scholar]
- Schachter S. Obesity and Eating - Internal and External Cues Differentially Affect Eating Behavior of Obese and Normal Subjects. Science. 1968;161:751. doi: 10.1126/science.161.3843.751. [DOI] [PubMed] [Google Scholar]
- Schallert T, Whishaw IQ. Two types of aphagia and two types of sensorimotor impairment after lateral hypothalamic lesions: observations in normal weight, dieted, and fattened rats. Journal of Comparative and Physiological Psychology. 1978;92:720–41. doi: 10.1037/h0077504. [DOI] [PubMed] [Google Scholar]
- Schultz W, Dickinson A. Neuronal coding of prediction errors. Annu Rev Neurosci. 2000;23:473–500. doi: 10.1146/annurev.neuro.23.1.473. [DOI] [PubMed] [Google Scholar]
- Schultz W. Behavioral Theories and the Neurophysiology of Reward. Annu Rev Psychol. 2006 doi: 10.1146/annurev.psych.56.091103.070229. [DOI] [PubMed] [Google Scholar]
- Sharkey KA, Pittman QJ. Central and peripheral signaling mechanisms involved in endocannabinoid regulation of feeding: a perspective on the munchies. Sci STKE. 2005;2005:pe15. doi: 10.1126/stke.2772005pe15. [DOI] [PubMed] [Google Scholar]
- Shimura T, Imaoka H, Yamamoto T. Neurochemical modulation of ingestive behavior in the ventral pallidum. Eur J Neurosci. 2006;23:1596–604. doi: 10.1111/j.1460-9568.2006.04689.x. [DOI] [PubMed] [Google Scholar]
- Small D, Veldhuizen M. Human crossmodal studies of taste and smell\ In: Kringelbach ML, Berridge KC, editors. Pleasures of the brain. Oxford University Press; Oxford, U.K: 2010. pp. 320–336. [Google Scholar]
- Small DM, Zatorre RJ, Dagher A, Evans AC, Jones-Gotman M. Changes in brain activity related to eating chocolate - From pleasure to aversion. Brain. 2001;124:1720–1733. doi: 10.1093/brain/124.9.1720. [DOI] [PubMed] [Google Scholar]
- Small DM, Jones-Gotman M, Dagher A. Feeding-induced dopamine release in dorsal striatum correlates with meal pleasantness ratings in healthy human volunteers. Neuroimage. 2003;19:1709–15. doi: 10.1016/s1053-8119(03)00253-2. [DOI] [PubMed] [Google Scholar]
- Smith KS, Berridge KC. The ventral pallidum and hedonic reward: neurochemical maps of sucrose “liking” and food intake. J Neurosci. 2005;25:8637–49. doi: 10.1523/JNEUROSCI.1902-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KS, Berridge KC. Opioid limbic circuit for reward: interaction between hedonic hotspots of nucleus accumbens and ventral pallidum. Journal of Neuroscience. 2007;27:1594–605. doi: 10.1523/JNEUROSCI.4205-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KS, Berridge KC, Aldridge JW. Society for Neuroscience Abstracts. 2007. Ventral pallidal neurons distinguish ‘liking’ and wanting elevations caused by opioids versus dopamine in nucleus accumbens. [Google Scholar]
- Smith KS, Tindell AJ, Aldridge JW, Berridge KC. Ventral pallidum roles in reward and motivation. Behav Brain Res. 2009;196:155–67. doi: 10.1016/j.bbr.2008.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KS, Mahler SV, Pecina S, Berridge KC. Hedonic Hotspots: Generating Sensory Pleasure in the Brain. In: Kringelbach ML, Berridge KC, editors. Pleasures of the Brain. Oxford University Press; Oxford, U.K: 2010. pp. 27–49. [Google Scholar]
- Steele K, Prokopowicz G, Schweitzer M, Magunsuon T, Lidor A, Kuwabawa H, Kumar A, Brasic J, Wong D. Alterations of Central Dopamine Receptors Before and After Gastric Bypass Surgery. Obesity Surgery. 2009 doi: 10.1007/s11695-009-0015-4. [DOI] [PubMed] [Google Scholar]
- Stefanidis A, Verty AN, Allen AM, Owens NC, Cowley MA, Oldfield BJ. The role of thermogenesis in antipsychotic drug-induced weight gain. Obesity (Silver Spring) 2009;17:16–24. doi: 10.1038/oby.2008.468. [DOI] [PubMed] [Google Scholar]
- Steiner JE. The gustofacial response: observation on normal and anencephalic newborn infants. Symposium on Oral Sensation and Perception. 1973;4:254–78. [PubMed] [Google Scholar]
- Steiner JE, Glaser D, Hawilo ME, Berridge KC. Comparative expression of hedonic impact: Affective reactions to taste by human infants and other primates. Neuroscience and Biobehavioral Reviews. 2001;25:53–74. doi: 10.1016/s0149-7634(00)00051-8. [DOI] [PubMed] [Google Scholar]
- Stellar JR, Brooks FH, Mills LE. Approach and withdrawal analysis of the effects of hypothalamic stimulation and lesions in rats. Journal of Comparative and Physiological Psychology. 1979;93:446–66. doi: 10.1037/h0077590. [DOI] [PubMed] [Google Scholar]
- Stewart J. Psychological and neural mechanisms of relapse. Philos Trans R Soc Lond B Biol Sci. 2008;363:3147–58. doi: 10.1098/rstb.2008.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson LW. Anatomy of the soul as reflected in the cerebral hemispheres: neural circuits underlying voluntary control of basic motivated behaviors. J Comp Neurol. 2005;493:122–31. doi: 10.1002/cne.20733. [DOI] [PubMed] [Google Scholar]
- Swinburn B, Sacks G, Ravussin E. Increased food energy supply is more than sufficient to explain the US epidemic of obesity. Am J Clin Nutr. 2009 doi: 10.3945/ajcn.2009.28595. [DOI] [PubMed] [Google Scholar]
- Szczypka MS, Kwok K, Brot MD, Marck BT, Matsumoto AM, Donahue BA, Palmiter RD. Dopamine production in the caudate putamen restores feeding in dopamine-deficient mice. Neuron. 2001;30:819–28. doi: 10.1016/s0896-6273(01)00319-1. [DOI] [PubMed] [Google Scholar]
- Teitelbaum P, Epstein AN. The lateral hypothalamic syndrome: recovery of feeding and drinking after lateral hypothalamic lesions. Psychological Review. 1962;69:74–90. doi: 10.1037/h0039285. [DOI] [PubMed] [Google Scholar]
- Tindell AJ, Berridge KC, Aldridge JW. Ventral pallidal representation of pavlovian cues and reward: population and rate codes. J Neurosci. 2004;24:1058–69. doi: 10.1523/JNEUROSCI.1437-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tindell AJ, Berridge KC, Zhang J, Peciña S, Aldridge JW. Ventral pallidal neurons code incentive motivation: amplification by mesolimbic sensitization and amphetamine. Eur J Neurosci. 2005;22:2617–34. doi: 10.1111/j.1460-9568.2005.04411.x. [DOI] [PubMed] [Google Scholar]
- Tindell AJ, Smith KS, Pecina S, Berridge KC, Aldridge JW. Ventral pallidum firing codes hedonic reward: when a bad taste turns good. J Neurophysiol. 2006;96:2399–409. doi: 10.1152/jn.00576.2006. [DOI] [PubMed] [Google Scholar]
- Tindell AJ, Smith KS, Berridge KC, Aldridge JW. Dynamic computation of incentive salience: “wanting” what was never “liked”. J Neurosci. 2009;29:12220–12228. doi: 10.1523/JNEUROSCI.2499-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomie A. Locating reward cue at response manipulandum (CAM) induces symptoms of drug abuse. Neuroscience and Biobehavioral Reviews. 1996;20:31. doi: 10.1016/0149-7634(95)00023-2. [DOI] [PubMed] [Google Scholar]
- Valenstein ES, Cox VC, Kakolewski JW. Reexamination of the role of the hypothalamus in motivation. Psychological Review. 1970;77:16–31. doi: 10.1037/h0028581. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Fowler JS, Logan J, Jayne M, Franceschi D, Wong C, Gatley SJ, Gifford AN, Ding YS, Pappas N. “Nonhedonic” food motivation in humans involves dopamine in the dorsal striatum and methylphenidate amplifies this effect. Synapse. 2002;44:175–180. doi: 10.1002/syn.10075. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wang G-J, Fowler JS, Telang F. Overlapping neuronal circuits in addiction and obesity: evidence of systems pathology. Philosophical Transactions of the Royal Society B: Biological Sciences. 2008;363:3191–3200. doi: 10.1098/rstb.2008.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wachtel SR, Ortengren A, de Wit H. The effects of acute haloperidol or risperidone on subjective responses to methamphetamine in healthy volunteers. Drug Alcohol Depend. 2002;68:23–33. doi: 10.1016/s0376-8716(02)00104-7. [DOI] [PubMed] [Google Scholar]
- Wang GJ, Volkow ND, Logan J, Pappas NR, Wong CT, Zhu W, Netusil N, Fowler JS. Brain dopamine and obesity. Lancet. 2001;357:354–357. doi: 10.1016/s0140-6736(00)03643-6. [DOI] [PubMed] [Google Scholar]
- Wang GJ, Volkow ND, Telang F, Jayne M, Ma J, Rao M, Zhu W, Wong CT, Pappas NR, Geliebter A, Fowler JS. Exposure to appetitive food stimuli markedly activates the human brain. Neuroimage. 2004a;21:1790–7. doi: 10.1016/j.neuroimage.2003.11.026. [DOI] [PubMed] [Google Scholar]
- Wang GJ, Volkow ND, Thanos PK, Fowler JS. Similarity between obesity and drug addiction as assessed by neurofunctional imaging: a concept review. J Addict Dis. 2004b;23:39–53. doi: 10.1300/J069v23n03_04. [DOI] [PubMed] [Google Scholar]
- Wellman PJ, Davies BT, Morien A, McMahon L. Modulation of feeding by hypothalamic paraventricular nucleus alpha 1- and alpha 2-adrenergic receptors. Life Sci. 1993;53:669–79. doi: 10.1016/0024-3205(93)90243-v. [DOI] [PubMed] [Google Scholar]
- Winn P. The lateral hypothalamus and motivated behavior: an old syndrome reassessed and a new perspective gained. Current Directions in Psychological Science. 1995;4:182–187. [Google Scholar]
- Wise RA. The anhedonia hypothesis: Mark III. Behavioral and Brain Sciences. 1985;8:178–186. [Google Scholar]
- Wise RA, Fotuhi M, Colle LM. Facilitation of feeding by nucleus accumbens amphetamine injections: latency and speed measures. Pharmacology, Biochemistry & Behavior. 1989;32:769–72. doi: 10.1016/0091-3057(89)90031-2. [DOI] [PubMed] [Google Scholar]
- Wise RA. Roles for nigrostriatal--not just mesocorticolimbic--dopamine in reward and addiction. Trends Neurosci. 2009;32:517–24. doi: 10.1016/j.tins.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolterink G, Phillips G, Cador M, Donselaar-Wolterink I, Robbins TW, Everitt BJ. Relative roles of ventral striatal D1 and D2 dopamine receptors in responding with conditioned reinforcement. Psychopharmacology (Berl) 1993;110:355–64. doi: 10.1007/BF02251293. [DOI] [PubMed] [Google Scholar]
- Wyvell CL, Berridge KC. Intra-accumbens amphetamine increases the conditioned incentive salience of sucrose reward: enhancement of reward “wanting” without enhanced “liking” or response reinforcement. Journal of Neuroscience. 2000;20:8122–30. doi: 10.1523/JNEUROSCI.20-21-08122.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyvell CL, Berridge KC. Incentive-sensitization by previous amphetamine exposure: Increased cue-triggered ‘wanting’ for sucrose reward. Journal of Neuroscience. 2001;21:7831–7840. doi: 10.1523/JNEUROSCI.21-19-07831.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeomans MR, Gray RW. Opioid peptides and the control of human ingestive behaviour. Neurosci Biobehav Rev. 2002;26:713–28. doi: 10.1016/s0149-7634(02)00041-6. [DOI] [PubMed] [Google Scholar]
- Zahm DS. The evolving theory of basal forebrain functional--anatomical ‘macrosystems’. Neuroscience & Biobehavioral Reviews. 2006;30:148–172. doi: 10.1016/j.neubiorev.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Zangen A, Shalev U. Nucleus accumbens beta-endorphin levels are not elevated by brain stimulation reward but do increase with extinction. Eur J Neurosci. 2003;17:1067–72. doi: 10.1046/j.1460-9568.2003.02509.x. [DOI] [PubMed] [Google Scholar]
- Zhang J, Berridge KC, Tindell AJ, Smith KS, Aldridge JW. A neural computational model of incentive salience. PLoS Comput Biol. 2009;5:e1000437. doi: 10.1371/journal.pcbi.1000437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M, Kelley AE. Enhanced intake of high-fat food following striatal mu-opioid stimulation: microinjection mapping and fos expression. Neuroscience. 2000;99:267–77. doi: 10.1016/s0306-4522(00)00198-6. [DOI] [PubMed] [Google Scholar]
- Zheng H, Berthoud HR. Eating for pleasure or calories. Curr Opin Pharmacol. 2007;7:607–12. doi: 10.1016/j.coph.2007.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H, Patterson L, Berthoud H. Orexin signaling in the ventral tegmental area is required for high-fat appetite induced by opioid stimulation of the nucleus accumbens. J Neurosci. 2007;27:11075–82. doi: 10.1523/JNEUROSCI.3542-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubieta JK, Ketter TA, Bueller JA, Xu YJ, Kilbourn MR, Young EA, Koeppe RA. Regulation of human affective responses by anterior cingulate and limbic mu-opioid neurotransmission. Archives of General Psychiatry. 2003;60:1145–1153. doi: 10.1001/archpsyc.60.11.1145. [DOI] [PubMed] [Google Scholar]