Abstract
1. Purpose of review
Osteoporosis is a growing problem worldwide, with the greatest burden resulting from fractures. Currently available are several treatment options that are effective in reducing fracture risk. Patient adherence to these medications is required for benefit to be seen. Yet similar to other chronic, asymptomatic diseases, adherence to osteoporosis therapies is poor. The reasons for suboptimal adherence are multiple but include fear of possible side effects, dosing requirements, and an unwillingness to take a medication for a “silent” disease. Poor adherence leads to reduced effectiveness, increased morbidity and increased medical costs.
2. Recent findings
Efforts to improve adherence to osteoporosis treatments are ongoing. The first obstacle in improving adherence to osteoporosis treatments is determining causes of poor adherence. Despite several identifiable causes, improving adherence is difficult. Passive patient education with printed information alone does not appear very effective. Physician-patient interaction, including discussion of bone mineral density results, discussion of osteoporosis medication benefits, and feedback of treatment effects, may be more effective.
3. Summary
Improved patient education, better tolerated and less frequently-dosed medications, and more health care provider-patient interaction, may improve adherence and lead to greater fracture reduction.
Keywords: Osteoporosis, Medication, Adherence, Compliance, Bisphosphonate
Introduction and Definitions
The National Osteoporosis Foundation estimates that 10 million Americans are currently afflicted with osteoporosis and its prevalence is estimated to exceed 14 million in 2020 [1]. The efficacy of osteoporosis medications to prevent osteoporosis and reduce fracture risk relies on appropriate administration. Unfortunately, adherence to osteoporosis medications is suboptimal, similar to medications for other chronic illnesses [2–5]. Poor medication adherence leads to increased morbidity and medical costs [6]. Medication adherence has been described in the past using multiple terms: compliance, persistence, and adherence. Recent work [7] has attempted to harmonize these terms as follows: compliance may be defined as “the extent to which a patient acts in accordance with the prescribed interval, and dose of a dosing regimen.” Medication persistence refers to the act of continuing the treatment for the prescribed duration. It may be defined as “the duration of time from initiation to discontinuation of therapy.” Adherence sometimes is used as a synonym for compliance or as a more ‘over-arching’ term that encompasses both compliance and persistence. This latter definition is what will be used in this review.
Adherence with Osteoporosis Medications
The number of treatment options for osteoporosis continues to grow. The most commonly used are the bisphosphonates, which can be dosed orally daily, weekly, or monthly, or intravenously every three months or annually. In addition to bisphosphonates, treatment options include estrogen, selective estrogen receptor modulators (SERMs), calcitonin, and teriparatide (parathyroid hormone). Despite the numerous options, adherence with all osteoporosis therapies is poor. One might assume that adherence with estrogen therapy in postmenopausal women would be superior to other treatments since it is frequently taken for vasomotor symptom relief, and thus, there is a self-reinforcing benefit to high adherence. However, at least in some studies, adherence with bisphosphonates was found to be higher than with hormone replacement therapy [8] and calcitonin [4]. In a meta-analysis of 24 observational studies conducted in large populations, overall adherence for all osteoporosis therapies was low, ranging from approximately 40–70% [8].
Methods to Measure and Quantify Adherence
Measuring adherence is done using a variety of types of information and quantified in various ways [9], which may explain some of the differences between studies. For example, patient surveys (i.e. self-report) report higher persistence rates than studies conducted using claims data or other objective data (e.g. pill count monitoring) [8, 10]. For that reason, the latter may be preferable to determine adherence. However, these data sources cannot assess whether patients are actually taking the medication under optimal dosing conditions (e.g. fasting), an important factor for oral bisphosphonates.
A common way to quantify compliance in administrative claims data sources is to sum the number of pills dispensed across all filled prescriptions divided by calendar time; this is described as a Medication Possession Ratio (MPR) [9]. As one recent example of a number of similar reports on this topic, for women 45 years of age or older with an osteoporosis diagnosis, only 50% of new bisphosphonate users were compliant at three months; compliance dropped to 30% at 1 year and 16% after 3 years [4].
Persistence
Most studies define non-persistence as a gap in treatment which may vary between 30 and 120 days. However, only approximately one-half of patients persist with treatment at 6 months, and this number falls even further after two years of treatment [8]. One flaw in the definition of persistence is that it does not account for the fact that patients may stop and but later restart medication. Re-initiation rates for bisphosphonate therapy among persons who discontinue have been estimated to be as high as 30% within 6 months and 50% within 2 years [11]. Predictors of treatment re-initiation include the occurrence of a hip fracture and reassessment of bone mineral density [11].
Reasons for Nonadherence
The reasons behind noncompliance with bisphosphonate therapy are multifactorial. Although the cost of these medications is a concern for patients, cost has not been found to significantly affect osteoporosis medication adherence [12, 13], and the availability of generic alendronate may further temper concerns about medication costs. The reasons most strongly associated with noncompliance include medication side effects and patients’ perception of effectiveness and safety [12]. In considering non-compliance due to side effects, it may be a fear of potential side effects rather than the actual occurrence of side effects that leads to non-adherence in many patients [13, 14]. Patients who have had side effects from other medications or have heard from others about possible side effects are less willing to take the medications [14].
Perceived lack of benefit, especially if a patient develops a fracture while taking a bisphosphonate medication, is another common reason for non-adherence [13, 15]. Patients are frequently unwilling to take a medication for an asymptomatic disease, particularly if they have little confidence that the medication is ‘working’. Most insurance companies (including Medicare) typically pay for repeat bone mineral density (BMD) testing only every 2 or more years [16]. Although bone turnover markers might provide earlier information about whether medications are exerting their intended effect, poor reimbursement and difficult specimen collection requirements (i.e. fasting, second morning void urine specimen) due to diurnal variation in turnover markers generally preclude their routine use in most non-research settings.
Some patients perceive medications as not necessary if they are otherwise healthy or prefer a “natural” treatment and feel calcium and vitamin D supplementation are sufficient [14]. Patients may be more adherent if they fear the consequences of fracture, but this requires that they perceive themselves to be at-risk, which may require education [14]. The availability of the FRAX calculator [17] that allows health providers to calculate 10-year absolute fracture risk may promote patients’ better understanding of their fracture risk and thereby improve adherence.
Other major barriers to osteoporosis medication include complicated dosing instructions and specific time restrictions [13]. It has been well described that the more complicated a dosing regimen, the poorer the adherence [18]. It might be assumed that decreased dosing frequency would improve compliance. One study showed that less frequent dosing was the strongest predictor of persistence. Overall adherence with both daily and weekly medications was poor, and more than 50% of women in both groups discontinued at 1 year [2]. There is some evidence that once monthly bisphosphonates may be preferred by more patients compared to more frequently dosed options for reasons such as a perceived lower likelihood of side effects and less time spent thinking about the disease being treated [19]. However, several studies have not shown a significant difference in adherence between weekly and monthly preparations [4, 19–21].
The recent addition of a once yearly intravenous bisphosphonate (zoledronic acid) to the armamentarium of available osteoporosis therapies has the potential to significantly improve the issue of adherence to medications. With this treatment option, adherence is guaranteed for a year. Additionally, it also negates one of the main barriers to patient compliance with oral therapies: possible gastrointestinal side effects. However, it adds a new dimension of adherence, in that it now requires physicians to also be responsible for adherence to therapy as it puts the onus of responsibility on them to ensure that the annual infusion schedule is kept. There may be similar benefits on adherence with use of intravenous ibandronate, which is dosed every three months.
Despite a number of well-described factors known to be strongly associated with high bisphosphonate adherence such as age, history of fracture, and history of BMD testing, these are relatively poor in aggregate to discriminate between compliant and non-compliant persons [22, 23]. One recent study found that prior compliance with medications used to treat other chronic asymptomatic conditions (e.g. hyperlipidemia), was a strong predictor of high future adherence to oral bisphosphonates [24]. This suggests the possibility that considering osteoporosis medication adherence only in the context of the disease itself may not adequately address more general behavioral issues related to medication adherence.
Effect of Poor Adherence
The clinical benefit from osteoporosis therapies has a clear association with medication adherence. Differential changes in BMD changes can be seen within one year of osteoporosis medication initiation among adherent versus non-adherent persons. In one study, BMD of the lumbar spine significantly improved in those taking at least two-thirds of the prescribed doses compared to those taking less than two-thirds (3.8% increase vs. 2.1% increase) [25]. Another study showed improved BMD of the hip (but not lumbar spine) (p = 0.01) and suppression of bone turnover markers after one year in those > 75% compliant [26].
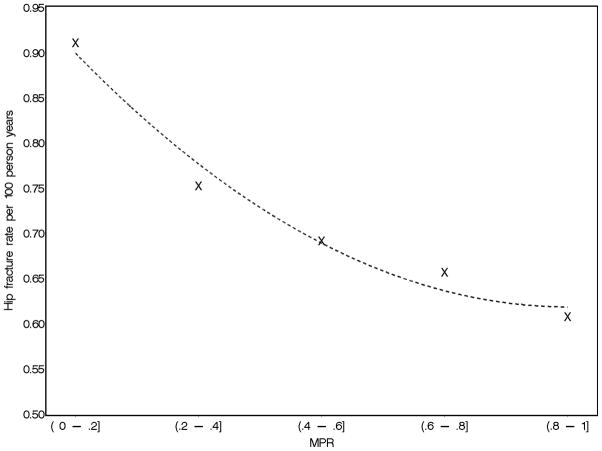
More importantly, good compliance is necessary for fracture risk reduction, with increasing benefit seen with improved compliance [15, 27, 28]. Persistence with bisphosphonate therapy was associated with up to a 60% reduced risk of hip fracture [29]. Although there is a clear association between fracture risk reduction and level of adherence, there is considerable variation across age groups and fracture types [15]. High medication adherence has been found to reduce the risk of all clinical fractures by 20–45% [27, 30]. Although it remains unclear as to whether there is a ‘threshold’ effect for non-adherence, such that below a certain level patients receive no anti-fracture benefit, the beneficial effects of medication compliance can be seen with as little as 50% adherence and are even greater with at least 75–80% adherence (Figure 1) [15, 27]. If undetected, poor compliance and the resulting lack of benefit may lead the physician to make changes in therapy based upon concern that the medication is not working, which may be unwarranted [31].
Figure 1.
Relationship between adherence to oral bisphosphonates (quantified by the Medication Possession Ratio, or MPR) (x-axis) and rate of hip fracture among persons 65–78 years of age, adapted from [15].
A key unresolved question in the adherence literature is whether patients who have been adherent for some period of time (e.g. years) and take a ‘drug holiday’ might be protected from fracture for some ensuing period of time. In an extension to a randomized controlled trial of women treated for 5 years with alendronate, 1099 continued and were subsequently randomized to ongoing treatment versus placebo [32]. There was a similar rate of non-vertebral fractures between both groups, although vertebral fracture rates were lower among those who continued on therapy. In another study of 9063 women who were compliant for at least 2 years (i.e. MPR of >66%), discontinuation of bisphosphonates led to a two to three-fold increased risk of hip fracture. Despite limitations due to a small number of fractures, this increased risk was not observed until approximately one year after discontinuation [33]. Similarly, ongoing vertebral fracture risk protection was seen up to one year after discontinuation of daily risedronate after three years of persistence [34].
The predicted expenditures for fracture related health care costs are calculated to surpass $25 billion by 2025 [35]. A recent evaluation of the cost-effectiveness of improved osteoporosis medication adherence did show a reduction in health care costs as long as the cost of medications does not rise significantly [36]. In a three-year study of new bisphosphonate users, total health care costs were 8.9% lower among patients with no refill gap >30 days (p < 0.001) and 3.5% lower for compliant patients with an MPR >80% (p = 0.014). Persistence was associated with a 47% lower likelihood of inpatient admission [37].
Adherence as a Proxy for Other Healthy Behaviors
A major concern with these observational data relates to the potential bias associated with adherence as a behavior, independent of the medication effect. It is highly plausible that adherent persons also engage in other healthy lifestyle behaviors that put them at lower risk for adverse outcomes. These unmeasured behaviors are likely to be confounders of the relationship between osteoporosis medication adherence and fracture outcomes.
Relevant for osteoporosis, these healthy behaviors may include weight bearing exercise, use of calcium and vitamin D supplements, and avoidance of tobacco and alcohol. To reinforce the concern for lower adverse event rates associated with confounding by adherence, data from the placebo arms of some randomized controlled trials of cardiovascular medications (e.g. statins, beta-blockers, ACE inhibitors) have shown a substantial reduction in mortality among persons adherent to placebo compared to those non-adherent to placebo [38–40].
Despite the strong possibility that medication adherence is a proxy for healthy behaviors that are associated with a lower risk for adverse outcomes, it also is possible that persons with more severe osteoporosis (i.e. prior clinical fractures or lower T-scores) are more likely to adhere to osteoporosis medications. If this were the case, persons with high adherence to osteoporosis medications may have a higher baseline risk of fracture. The net effect of confounding due to greater adherence related to a higher severity of osteoporosis and that related to unmeasured healthy behaviors is unknown.
Improving Adherence
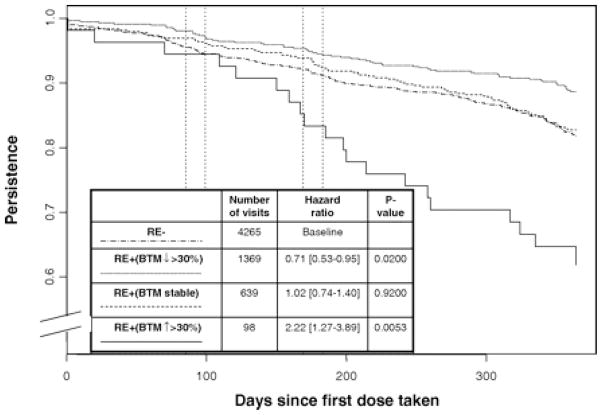
Four randomized trials have studied various means of improving adherence. One study looked at patient education through an educational osteoporosis leaflet [41]. The difference in raloxifene adherence between the intervention group and the control group did not differ significantly at 12 months (p = 0.38), with similar compliance being seen in both groups (47.4% and 52.5%, respectively) [41]. The other three trials involved individualized patient education in the form of discussion of changes in bone turnover markers. In one study, patients that met with a nurse had similar adherence to those that received bone turnover marker information; adherence in both groups was better than the group that received neither [26]. In a second study, there was no difference between those receiving general patient education, bone turnover marker information, a combination of general information and bone turnover marker information, and those receiving no intervention [42]. The third study was a multicenter study of 2302 women who either received bone turnover marker information after 10 weeks and 22 weeks of therapy or received no information [43]. Some benefit was seen in the intervention group but it was not significant (p = 0.16). However, when the intervention group was divided into those with improved (>30% reduction) vs. stable vs. worsening bone turnover markers, those with positive results (i.e. >30% reduction) were significantly more likely to adhere to treatment (p=0.020) (Figure 2).
Figure 2.
(from [43])
Kaplan-Meier survival curves showing the effect of providing bone turnover marker results (urinary n telopeptide, or uNTX) on persistence (n = 2302). Bone turnover marker response was categorized as good (more than 30% decrease from baseline in uNTX at wk 10 and 22); stable, at least one stable uNTX response at wk 10 or 22 and no increase in uNTX more than 30%; or poor, at least one uNTX increase more than 30% at wk 10 or 22. The numbers of patient visits with a good (1369 visits) or stable uNTX response (639 visits) was higher than the number of visits with a poor response (98 visits).
A recurring finding has been that persistence is better among patients with whom bone mineral density testing results are discussed [8]. As the majority of patients started on bisphosphonate therapy undergo evaluation with a DXA (dual energy x-ray absorptiometry) scan, discussing the results with the patient may lead to significant improvement of medication adherence. In one study of ibandronate vs. other bisphosphonates, increasing patient participation in determining the treatment option was associated with improved patient adherence [44].
Patient confidence in their health care providers is also reflected by the improved adherence to treatment when the medications are prescribed by a specialist rather than a general practitioner [45]. Patient reminder programs (reminder phone calls to patients 1–3 days prior to scheduled dosing) and the use of nurse monitoring appears to be beneficial [26, 46], especially when considering medications with extended dosing intervals. Information technology may also facilitate use of other types of reminders, such as text messaging, paging systems on medication devices, or email. One patient reminder system found that the majority of patients prefer email reminders [47].
Conclusion
Much of the morbidity, mortality, and costs associated with osteoporosis and fractures can be prevented with the use of effective osteoporosis therapies currently available and on the horizon. However, current adherence to such medications is poor, and a full understanding of the causes for poor adherence and methods of improving adherence is lacking. It is hopeful that with improved patient education, better tolerated treatment options with less frequent dosing intervals, more health care provider-patient interaction, and multifaceted systems-based interventions, better adherence will lead to improved fracture risk reduction.
References
- 1.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007 Mar;22(3):465–75. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 2.Cramer JA, Amonkar MM, Hebborn A, Altman R. Compliance and persistence with bisphosphonate dosing regimens among women with postmenopausal osteoporosis. Current medical research and opinion. 2005 Sep;21(9):1453–60. doi: 10.1185/030079905X61875. [DOI] [PubMed] [Google Scholar]
- 3.Cramer JA, Silverman S. Persistence with bisphosphonate treatment for osteoporosis: finding the root of the problem. The American journal of medicine. 2006 Apr;119(4 Suppl 1):S12–7. doi: 10.1016/j.amjmed.2005.12.018. [DOI] [PubMed] [Google Scholar]
- 4.Weycker D, Macarios D, Edelsberg J, Oster G. Compliance with drug therapy for postmenopausal osteoporosis. Osteoporos Int. 2006;17(11):1645–52. doi: 10.1007/s00198-006-0179-x. [DOI] [PubMed] [Google Scholar]
- 5.Miller NH. Compliance with treatment regimens in chronic asymptomatic diseases. The American journal of medicine. 1997 Feb 17;102(2A):43–9. doi: 10.1016/s0002-9343(97)00467-1. [DOI] [PubMed] [Google Scholar]
- 6.Osterberg L, Blaschke T. Adherence to medication. The New England journal of medicine. 2005 Aug 4;353(5):487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- **7.Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008 Jan–Feb;11(1):44–7. doi: 10.1111/j.1524-4733.2007.00213.x. This article defines the terms used for medication compliance. Consistent definitions of terms related to compliance are needed for comparablility in assessing results across studies. [DOI] [PubMed] [Google Scholar]
- **8.Kothawala P, Badamgarav E, Ryu S, Miller RM, Halbert RJ. Systematic review and meta-analysis of real-world adherence to drug therapy for osteoporosis. Mayo Clinic proceedings. 2007 Dec;82(12):1493–501. doi: 10.1016/S0025-6196(11)61093-8. This meta-analysis of osteoporosis treatment adherence from 1990–2006 combines results from various studies to provide summary results pertaining to compliance, persistence and adherence. [DOI] [PubMed] [Google Scholar]
- 9.Lekkerkerker F, Kanis JA, Alsayed N, Bouvenot G, Burlet N, Cahall D, et al. Adherence to treatment of osteoporosis: a need for study. Osteoporos Int. 2007 Oct;18(10):1311–7. doi: 10.1007/s00198-007-0410-4. [DOI] [PubMed] [Google Scholar]
- 10.Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB. The concordance of self-report with other measures of medication adherence: a summary of the literature. Medical care. 2004 Jul;42(7):649–52. doi: 10.1097/01.mlr.0000129496.05898.02. [DOI] [PubMed] [Google Scholar]
- 11.Brookhart MA, Avorn J, Katz JN, Finkelstein JS, Arnold M, Polinski JM, et al. Gaps in treatment among users of osteoporosis medications: the dynamics of noncompliance. The American journal of medicine. 2007 Mar;120(3):251–6. doi: 10.1016/j.amjmed.2006.03.029. [DOI] [PubMed] [Google Scholar]
- 12.McHorney CA, Schousboe JT, Cline RR, Weiss TW. The impact of osteoporosis medication beliefs and side-effect experiences on non-adherence to oral bisphosphonates. Current medical research and opinion. 2007 Dec;23(12):3137–52. doi: 10.1185/030079907X242890. [DOI] [PubMed] [Google Scholar]
- 13.Cook PF, Emiliozzi S, McCabe MM. Telephone counseling to improve osteoporosis treatment adherence: an effectiveness study in community practice settings. Am J Med Qual. 2007 Nov–Dec;22(6):445–56. doi: 10.1177/1062860607307990. [DOI] [PubMed] [Google Scholar]
- *14.Lau E, Papaioannou A, Dolovich L, Adachi J, Sawka AM, Burns S, et al. Patients’ adherence to osteoporosis therapy: exploring the perceptions of postmenopausal women. Canadian family physician Medecin de famille canadien. 2008 Mar;54(3):394–402. Thirty-seven postmenopausal women on osteoporosis treatment were questioned in a focus group setting regarding their perspectives on osteoporosis treatment adherence and methods for improving adherence. [PMC free article] [PubMed] [Google Scholar]
- **15.Curtis JR, Westfall AO, Cheng H, Lyles K, Saag KG, Delzell E. Benefit of adherence with bisphosphonates depends on age and fracture type: results from an analysis of 101,038 new bisphosphonate users. J Bone Miner Res. 2008 Sep;23(9):1435–41. doi: 10.1359/JBMR.080418. This study was one among several that has evaluated the effect of medication adherence and fracture risk. Among its unique results, it showed that the relationship between osteoporosis medication adherence and fracture risk varied significantly by the type of fracture and by age. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *16.Curtis JR, Laster AJ, Becker DJ, Carbone L, Gary LC, Kilgore ML, et al. Regional variation in the denial of reimbursement for bone mineral density testing among US Medicare beneficiaries. J Clin Densitom. 2008 Oct–Dec;11(4):568–74. doi: 10.1016/j.jocd.2008.07.004. This study evaluated reasons for denial of DXA reimbursement. The reasons found for denial varied depending on age, sex, time since last DXA, ICD-9 codes, among other factors. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **17.http://www.shef.ac.uk/FRAX/. FRAX WHO Fracture Risk Assessment Tool [cited February 2, 2009]. The FRAX Calculator allows for determination of 10-year absolute fracture risk estimates based on bone mineral density and multiple clinical risk factors for fracture. The fracture risks computed from FRAX have been used by various groups to guide recommendations for use of prescription osteoporosis treatments
- 18.Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clinical therapeutics. 2001 Aug;23(8):1296–310. doi: 10.1016/s0149-2918(01)80109-0. [DOI] [PubMed] [Google Scholar]
- *19.Payer J, Killinger Z, Sulkova I, Celec P. Preferences of patients receiving bisphosphonates--how to influence the therapeutic adherence. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. 2008 Feb;62(2):122–4. doi: 10.1016/j.biopha.2007.07.005. Through use of a questionnaire, osteoporosis medication preferences were determined in a Slovakian population. [DOI] [PubMed] [Google Scholar]
- 20.Emkey R, Koltun W, Beusterien K, Seidman L, Kivitz A, Devas V, et al. Patient preference for once-monthly ibandronate versus once-weekly alendronate in a randomized, open-label, cross-over trial: the Boniva Alendronate Trial in Osteoporosis (BALTO) Current medical research and opinion. 2005 Dec;21(12):1895–903. doi: 10.1185/030079905X74862. [DOI] [PubMed] [Google Scholar]
- *21.Kastelan D, Lozo P, Stamenkovic D, Miskic B, Vlak T, Kolak Z, et al. Preference for weekly and monthly bisphosphonates among patients with postmenopausal osteoporosis: results from the Croatian PROMO Study. Clinical rheumatology. 2008 Nov 25; doi: 10.1007/s10067-008-1039-1. In this study from Croatia, women treated with weekly osteoporosis therapy were switched to once monthly ibandronate. At the end of the study, approximately 95% of the patients stated they preferred the once monthly preparation. [DOI] [PubMed] [Google Scholar]
- 22.Lo JC, Pressman AR, Omar MA, Ettinger B. Persistence with weekly alendronate therapy among postmenopausal women. Osteoporos Int. 2006;17(6):922–8. doi: 10.1007/s00198-006-0085-2. [DOI] [PubMed] [Google Scholar]
- 23.Solomon DH, Avorn J, Katz JN, Finkelstein JS, Arnold M, Polinski JM, et al. Compliance with osteoporosis medications. Archives of internal medicine. 2005 Nov 14;165(20):2414–9. doi: 10.1001/archinte.165.20.2414. [DOI] [PubMed] [Google Scholar]
- **24.Curtis JR, Xi J, Westfall AO, Cheng H, Lyles K, Saag KG, et al. Improving the Prediction of Medication Compliance: The Example of Bisphosphonates for Osteoporosis. Medical care. 2009 Feb 4; doi: 10.1097/MLR.0b013e31818afa1c. This study determined that evaluating a patient’s adherence to medications for other asymptomatic, chronic diseases (e.g. hyperlipidemia) improves the prediction of osteoporosis treatment adherence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *25.Yood RA, Emani S, Reed JI, Lewis BE, Charpentier M, Lydick E. Compliance with pharmacologic therapy for osteoporosis. Osteoporos Int. 2003 Dec;14(12):965–8. doi: 10.1007/s00198-003-1502-4. This study demonstrated that taking at least 2/3 of prescribed osteoporosis medication (i.e. a Medication Possession Ratio of > 66%) resulted in significantly increased BMD compared to lesser amounts of adherence. [DOI] [PubMed] [Google Scholar]
- *26.Clowes JA, Peel NF, Eastell R. The impact of monitoring on adherence and persistence with antiresorptive treatment for postmenopausal osteoporosis: a randomized controlled trial. The Journal of clinical endocrinology and metabolism. 2004 Mar;89(3):1117–23. doi: 10.1210/jc.2003-030501. This study showed that feedback of bone turnover markers had a beneficial effect on adherence to raloxifene. This effect was similar to the effect of more intense nurse follow-up contact with the patient without bone turnover markers. [DOI] [PubMed] [Google Scholar]
- 27.Siris ES, Harris ST, Rosen CJ, Barr CE, Arvesen JN, Abbott TA, et al. Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databases. Mayo Clinic proceedings. 2006 Aug;81(8):1013–22. doi: 10.4065/81.8.1013. [DOI] [PubMed] [Google Scholar]
- 28.Weycker D, Macarios D, Edelsberg J, Oster G. Compliance with osteoporosis drug therapy and risk of fracture. Osteoporos Int. 2007 Mar;18(3):271–7. doi: 10.1007/s00198-006-0230-y. [DOI] [PubMed] [Google Scholar]
- *29.Rabenda V, Mertens R, Fabri V, Vanoverloop J, Sumkay F, Vannecke C, et al. Adherence to bisphosphonates therapy and hip fracture risk in osteoporotic women. Osteoporos Int. 2008 Jun;19(6):811–8. doi: 10.1007/s00198-007-0506-x. This study evaluated the risk of hip fracture based on osteoporosis medication adherence in a Belgian population and found a significant correlation. [DOI] [PubMed] [Google Scholar]
- *30.Penning-van Beest FJ, Erkens JA, Olson M, Herings RM. Loss of treatment benefit due to low compliance with bisphosphonate therapy. Osteoporos Int. 2008 Apr;19(4):511–7. doi: 10.1007/s00198-007-0466-1. This study evaluated differences in fracture risk reduction in new bisphosphonate users. As adherence improves, there is a significant reduction in osteoporotic fracture risk. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stephenson J. Noncompliance may cause half of antihypertensive drug “failures”. Jama. 1999 Jul 28;282(4):313–4. doi: 10.1001/jama.282.4.313. [DOI] [PubMed] [Google Scholar]
- 32.Bone HG, Hosking D, Devogelaer JP, Tucci JR, Emkey RD, Tonino RP, et al. Ten years’ experience with alendronate for osteoporosis in postmenopausal women. The New England journal of medicine. 2004 Mar 18;350(12):1189–99. doi: 10.1056/NEJMoa030897. [DOI] [PubMed] [Google Scholar]
- **33.Curtis JR, Westfall AO, Cheng H, Delzell E, Saag KG. Risk of hip fracture after bisphosphonate discontinuation: implications for a drug holiday. Osteoporos Int. 2008 Nov;19(11):1613–20. doi: 10.1007/s00198-008-0604-4. This study evaluated fracture risk following discontinuation of a bisphosphonate. Women who took bisphosphonates at least 66% of the time for at least two years were at increased risk of hip fracture after subsequent discontinuation. However, those more compliant and those who continued treatment more than 2 years were not at significantly increased risk, suggesting the possibility of that a temporary ‘drug holiday’ after several years of compliance may be safe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **34.Watts NB, Chines A, Olszynski WP, McKeever CD, McClung MR, Zhou X, et al. Fracture risk remains reduced one year after discontinuation of risedronate. Osteoporos Int. 2008 Mar;19(3):365–72. doi: 10.1007/s00198-007-0460-7. This study evaluated the risk of vertebral fracture in women who had taken bisphosphonates for three years and then discontinued. Despite reduction in BMD, risk of vertebral fracture was not significantly increased one year after discontinuation. [DOI] [PubMed] [Google Scholar]
- 35.Fatalities and injuries from falls among older adults--United States, 1993–2003 and 2001–2005. Mmwr. 2006 Nov 17;55(45):1221–4. [PubMed] [Google Scholar]
- *36.Strom O, Borgstrom F, Kanis JA, Jonsson B. Incorporating adherence into health economic modelling of osteoporosis. Osteoporos Int. 2009 Jan;20(1):23–34. doi: 10.1007/s00198-008-0644-9. This study discusses the health benefits vs. increased health care costs using two theoretical medication options to examine the effect of improved adherence but increased cost that some medication options pose. [DOI] [PubMed] [Google Scholar]
- *37.Sunyecz JA, Mucha L, Baser O, Barr CE, Amonkar MM. Impact of compliance and persistence with bisphosphonate therapy on health care costs and utilization. Osteoporos Int. 2008 Oct;19(10):1421–9. doi: 10.1007/s00198-008-0586-2. This 3-year study found that women who were adherent with osteoporosis therapies had lower healthcare costs than those non-adherent. [DOI] [PubMed] [Google Scholar]
- *38.Influence of adherence to treatment and response of cholesterol on mortality in the coronary drug project. The New England journal of medicine. 1980 Oct 30;303(18):1038–41. doi: 10.1056/NEJM198010303031804. One of several studies that demonstrated that adherence to placebo results in better outcomes, illustrating the importance of evaluating adherence as a behavior rather than simply achieving a higher cumulative dose of medication. [DOI] [PubMed] [Google Scholar]
- 39.Granger BB, Swedberg K, Ekman I, Granger CB, Olofsson B, McMurray JJ, et al. Adherence to candesartan and placebo and outcomes in chronic heart failure in the CHARM programme: double-blind, randomised, controlled clinical trial. Lancet. 2005 Dec 10;366(9502):2005–11. doi: 10.1016/S0140-6736(05)67760-4. [DOI] [PubMed] [Google Scholar]
- 40.Horwitz RI, Viscoli CM, Berkman L, Donaldson RM, Horwitz SM, Murray CJ, et al. Treatment adherence and risk of death after a myocardial infarction. Lancet. 1990 Sep 1;336(8714):542–5. doi: 10.1016/0140-6736(90)92095-y. [DOI] [PubMed] [Google Scholar]
- 41.Guilera M, Fuentes M, Grifols M, Ferrer J, Badia X. Does an educational leaflet improve self-reported adherence to therapy in osteoporosis? The OPTIMA study. Osteoporos Int. 2006;17(5):664–71. doi: 10.1007/s00198-005-0031-8. [DOI] [PubMed] [Google Scholar]
- 42.Nattras S, Silverman SBD. Effectiveness of education and/or NTx results as a means of encouraging compliance to alendronate. Presented at World Congress on Osteoporosis. 2000; Chicago, Illinois. June 15–18. [Google Scholar]
- **43.Delmas PD, Vrijens B, Eastell R, Roux C, Pols HA, Ringe JD, et al. Effect of monitoring bone turnover markers on persistence with risedronate treatment of postmenopausal osteoporosis. The Journal of clinical endocrinology and metabolism. 2007 Apr;92(4):1296–304. doi: 10.1210/jc.2006-1526. Women with osteoporosis were started on risedronate and then randomized to groups receiving reinforcement vs. no reinforcement. Overall, there was similar persistence between the two groups. However, within the subgroup of women receiving positive reinforcement, i.e. notification of improved bone turnover markers, there was a significant improvement of persistence compared to the other groups. [DOI] [PubMed] [Google Scholar]
- *44.Lewiecki EM, Babbitt AM, Piziak VK, Ozturk ZE, Bone HG. Adherence to and gastrointestinal tolerability of monthly oral or quarterly intravenous ibandronate therapy in women with previous intolerance to oral bisphosphonates: a 12-month, open-label, prospective evaluation. Clinical therapeutics. 2008 Apr;30(4):605–21. doi: 10.1016/j.clinthera.2008.04.009. In this study, 543 women with osteoporosis or osteopenia were allowed to choose either a monthly oral bisphosphonate or an intravenous bisphosphonate dosed quarterly. When given this option, adherence to treatment improved. [DOI] [PubMed] [Google Scholar]
- 45.Pickney CS, Arnason JA. Correlation between patient recall of bone densitometry results and subsequent treatment adherence. Osteoporos Int. 2005 Sep;16(9):1156–60. doi: 10.1007/s00198-004-1818-8. [DOI] [PubMed] [Google Scholar]
- 46.Cooper A, Drake J, Brankin E. Treatment persistence with once-monthly ibandronate and patient support vs. once-weekly alendronate: results from the PERSIST study. International journal of clinical practice. 2006 Aug;60(8):896–905. doi: 10.1111/j.1742-1241.2006.01059.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Silverman S. Adherence to medications for the treatment of osteoporosis. Rheumatic diseases clinics of North America. 2006 Nov;32(4):721–31. doi: 10.1016/j.rdc.2006.07.003. [DOI] [PubMed] [Google Scholar]