Abstract
Light therapy is an effective treatment of seasonal affective disorder (SAD), when administered daily for at least several weeks. We have previously reported a small improvement in mood in SAD patients following exposure to the first hour of treatment. We now reevaluate retrospectively mood changes during shorter exposures comparing depression ratings at baseline, 20, 40, and 60 minutes of light. Participants were 15 depressed patients with SAD, untreated, who were tested during the winter season. The treatment consisted of 10,000 lux of white cool fluorescent light. Depression was measured using the 24-item NIMH scale (24-NIMH). The data were analyzed using ANOVA on ranks and Wilcoxon signed rank tests. Light resulted in significant improvement in mood at every interval when compared with baseline (p< .001). The 40 minute exposure resulted in a greater improvement than the 20 minute exposure (p < .001) but was not different from the 60 minute exposure (p < = .068). We conclude that immediate improvement in mood can be detected after the first session of light with exposures as short as 20 minutes, and that 40 minutes of exposure is not less effective than 60 minutes
Keywords: Seasonal affective disorder, light therapy, mood, psychiatry, depression
INTRODUCTION
Seasonal affective disorder (SAD), winter type, is characterized by recurrent major depression episodes during the fall-winter months, alternating with spontaneous remissions during the spring-summer months (1). Light therapy is an effective and well-tolerated treatment that is underutilized in clinical settings (2). The effectiveness of light treatment for SAD has been reported in randomized controlled studies (3,4). Although these trials reported the results of a course of daily light treatment (3–5), other data suggest that small improvements in depression score may commence as early as after the first hour of treatment. For instance, Sher et al (6) reported an improvement in depressive symptoms after one hour of bright light therapy, which correlated with improvement at the end of two weeks of light therapy. We focused on the temporal dynamic of mood improvement after shorter than 1-hour exposures, i.e. 20 and 40 minutes, with the expectation that these shorter than 1-hour exposures would be sufficient to induce significant mood improvement.
METHODS
This is a secondary, retrospective, analysis of our data from Sher et al (6). The original study was conducted between the months of December and February. The 15 subjects for the study were recruited from the Baltimore Washington Area. Written informed consents were provided by the subjects as approved by the NIMH Institutional Review Board. The mean age of the subjects was 45.7 ± 9.1 years. Ten participants were female and five were males. Screening was performed using the Structural Clinical Interview for DSM-IV (7), clinical interview, physical examination, and routine laboratory tests. The subjects were required to meet lifelong criteria for recurrent major depressive disorder or bipolar disorder (8) and the Rosenthal criteria for SAD (1). Participants were excluded if they met the criteria for Axis I comorbid psychiatric illnesses, including substance abuse. The structured clinical interview was used to eliminate other psychiatric diagnosis. Other exclusion criteria were: any major medical or neurological disorders, pregnancy, concurrent use of psychotropic drugs or medications affecting cerebral functioning. Depressed mood was confirmed using SIGH-SAD (Structured Interview Guide for the Hamilton Depression Rating Scale—Seasonal Affective Disorder Version) on the day of the testing: SIGH-SAD typical score > 13 or SIGH-SAD typical subscore’ > 11 if total (ie. Typical + atypical subscores) SIGH-SAD score > 19. The study started in the morning at about 8.30 am. The light used for the study was cool-white florescent delivered using a light box (Sunbox, Gaithersburg, MD) at 10,000 lux of intensity. The first session was a component of a larger PET (Positron Emision Tomography) study. The light boxes were suspended above the scanner gantry and subjects rested with their eyes open and maintained eye-gaze towards the center of the light box. Mood ratings were completed using the NIMH 24 item scale (9). We calculated the depression scores by adding subscores for dysphoria (items 2, 8, 13), depression (items 1, 6, 15, 18) and functional impairment (items 3, 20, 22). Four conditions (baseline; 20, 40, and 60 minutes) were compared using repeated measure ANOVAs on ranks with Wilcoxon Signed Rank tests. The criterion alpha was set at 0.05, two-tailed. We used Sigma Stat 3 for Windows and Systat 12 (SYSTAT 12 © SYSTAT Software, Inc. 2007) statistical software.
RESULTS
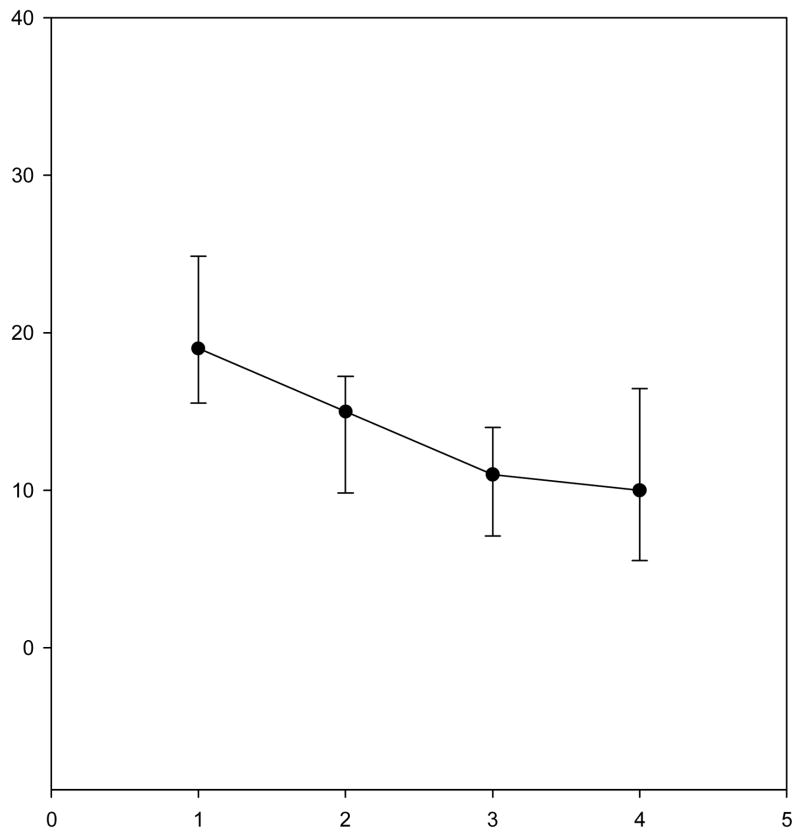
Significant differences were found when comparing the scores after the baseline with the three-onlight exposures using the repeat ANOVA on ranks (χ2 = 26.127, p = .001). Depression scores after 40 minutes of light were lower than after 20 minutes (Z-statistics = −3.124 p < .001). Depression scores after 60 minutes of treatment were not different from scores after 20 minutes of treatment (Z = −1.857, p < .068) or 40 minutes of treatment (Z = −0.395 and p = .733) (see figure 1).
Fig. 1.
Comparison between depression scores (and 95% upper and lower confidence intervals (CI) for baseline in dim light (1), after 20 minutes of bright light (2), 40 minutes (3) and 60 minutes (4) (p < .001). Means of depression scores and 95% CI.
DISCUSSION
Documenting very early mood improvement with bright light exposure in SAD patients is consistent with other studies reporting that brief administration of light is clinically active. Rot et al (10) showed that bright light in contrast to dim light prevents mood lowering, induced by acute tryptophan depletion. Natural bright light in normal subjects for 30 minutes improved one dimension of mood status, ‘pleasantness’, on the Mood Check List 3 (11). In a study by Goel and Etwaroo (12), bright light improved total mood disturbance, depression, and/or anger within 15–30 minutes of treatment and this effect was similar to that of auditory stimulus and high-density negative ions.
Improvements in alertness, attention and vigilance, especially during adverse conditions, after brief exposure to light have been reported by several studies. For instance, Babkoff et al (13) reported that bright light exposure of 1 hour improved subjective alertness and reaction time as compared with dim light. Similar results were found by Wright et al (14). In healthy volunteers, it was shown that a combination of 20 minutes of afternoon nap and exposure of bright light for 1 minute after the nap significantly improved cognitive performance when compared with caffeine after nap (15). In another study, improvement in alertness at night time was seen with 90 minutes of bright light as compared with dim light.
What could be the underlying mechanisms involved in the early improvement in depression scores with bright light treatment? Previous chronobiologic mechanisms implicated in response and remission of depression in SAD patients, such as shortening of nocturnal melatonin secretion, prolonged in SAD patients (17) or phase advancing (18–21) would probably have no role in the effect of brief immediate response to light. On the other hand, the previously reported effect of a course of light on neurotransmitters including serotonin (22–24) and norepinephrine (22,25,26) could be also involved in the effects of short-term exposure to bright light. Supporting serotonin involvement, a study by Lambert et al (27), invasively measuring the serotonin turnover, reported that the light intensity on the day of the test rather than average of previous days correlated best with brain serotonin turnover, suggesting a contemporaneous rather than moving-averaged or lagged response of bright light, suggesting an interaction between immediate bright light treatment and serotonin levels. Short exposure to bright light (as compared with dim light) in mildly seasonal healthy young women prevented mood worsening after tryptophan depletion (8).
Our study has several limitations. The study was retrospective and the sample size of the patient population was small (15 patients). Our study was conducted in an artificial environment, in a scanner, with invasive catheters, with the presence of raters etc, but it was highly precise. Although we report the effects of short exposures, we were unable to determine how long the immediate mood improvement after light would last. So possibly a longer duration of light, although unnecessary for a greater immediate effect, would nevertheless be better in sustaining that effect. In addition, as we did not have a control, we do not know to what degree the immediate response is a nonspecific effect, based on expectation (placebo) or the close interaction with the patients during the PET scanning procedures. Finally, other cardinal symptoms of SAD, such as increased appetite, carbohydrate craving, and sleepiness were not measured.
CONCLUSIONS
In conclusion, a significant immediate reduction of depression scores with light treatment can be identified after 20 minutes and reaches the maximum at 40 minutes, with no additional benefit at 60 minutes. The rate of change is steepest during the first 20 minutes of light as compared with longer intervals. Comparing clinical impact of these durations of administration may yield different results when measured after several daily sessions, as overnight effect on circadian rhythms and sleep were not assessed in our study and are thought to impact mood regulation in SAD. Larger, prospective, controlled, and hypothesis-driven studies in more naturalistic conditions would be desirable to replicate the results of our study and to analyze the temporal dynamic of the persistence of the immediate mood-improvement effects. In addition, in larger samples, one could define early responders and non responders, analyze genetic (e.g. melanopsin related genes), demographic (children, adolescents, adults, elderly, gender), physiological (e.g. pupilary responses), and clinical (e.g. abundant atypical symptoms) predictors for early response. If proven effective and efficacious, shorter exposures to bright light could become a feasible and broadly employed intervention for immediate mood improvement as an early step on the road toward full antidepressant response and remission.
Acknowledgments
The initial study was supported by intramural NIMH (PI Rosenthal, also supporting Postolache and Sher). Statistical work and completion of data interpretation and the completion of this report have been supported by the 1R34MH073797–01A2 (PI Postolache), NIH 1K12RR023250–01 (supporting Dr. Reeves) and the St. Elizabeths Residency Training Program (Drs. Virk and Postolache). The authors also thank Dr. Farooq Mohyuddin for his overall support of this project.
References
- 1.Rosenthal NE, Sack DA, Gillin JC, Lewy AJ, Goodwin FK, Davenport Y, et al. Seasonal affective disorder. A description of the syndrome and preliminary findings with light therapy. Arch Gen Psychiatry. 1984;41:72–80. doi: 10.1001/archpsyc.1984.01790120076010. [DOI] [PubMed] [Google Scholar]
- 2.Golden RN, Gaynes BN, Ekstrom RD, Hamer RM, Jacobsen FM, Suppes T, et al. The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Am J Psychiatry. 2005;162:656–62. doi: 10.1176/appi.ajp.162.4.656. [DOI] [PubMed] [Google Scholar]
- 3.Eastman CI, Young MA, Fogg LF, Liu L, Meaden PM. Bright light treatment of winter depression: a placebo-controlled trial. Arch Gen Psychiatry. 1998;55:883–9. doi: 10.1001/archpsyc.55.10.883. [DOI] [PubMed] [Google Scholar]
- 4.Terman M, Levine SM, Terman JS, Doherty S. Chronic fatigue syndrome and seasonal affective disorder: comorbidity, diagnostic overlap, and implications for treatment. Am J Med. 1998;28:115S–24S. doi: 10.1016/s0002-9343(98)00172-7. [DOI] [PubMed] [Google Scholar]
- 5.Lewy AJ, Bauer VK, Cutler NL, Sack RL, Ahmed S, Thomas KH, et al. Morning vs evening light treatment of patients with winter depression. Arch Gen Psychiatry. 1998;55:861–2. doi: 10.1001/archpsyc.55.10.890. [DOI] [PubMed] [Google Scholar]
- 6.Sher L, Matthews JR, Turner EH, Postolache TT, Katz KS, Rosenthal NE. Early response to light therapy partially predicts long-term antidepressant effects in patients with seasonal affective disorder. J Psychiatry Neurosci. 2001;26:336–8. [PMC free article] [PubMed] [Google Scholar]
- 7.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I disorders-Patient Edition (SCID-I/P, Version 2.0) New York: NY State Psychiatr Inst; 1995. [Google Scholar]
- 8.Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Am Psychiatr Assoc; 2000. text revision. [Google Scholar]
- 9.Garcia-Borreguero D, Jacobsen FM, Murphy DL, Joseph-Vanderpool JR, Chiara A, Rosenthal NE. Hormonal responses to the administration of m-chlorophenylpiperazine in patients with season affective disorder and controls. Biol Psychiatry. 1995;37:740–9. doi: 10.1016/0006-3223(94)00208-K. [DOI] [PubMed] [Google Scholar]
- 10.aan het Rot M, Benkelfat C, Boivin DB, Young SN. Bright light exposure during acute tryptophan depletion prevents a lowering of mood in mildly seasonal women. Eur Neuropsychopharmacol. 2008;18:14–23. doi: 10.1016/j.euroneuro.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Kaida K, Takahashi M, Otsuka Y. A short nap and natural bright light exposure improve positive mood status. Ind Health. 2007;45:301–8. doi: 10.2486/indhealth.45.301. [DOI] [PubMed] [Google Scholar]
- 12.Goel N, Etwaroo GR. Bright light, negative air ions and auditory stimuli produce rapid mood changes in a student population: a placebo-controlled study. Psychol Med. 2006;36:1253–64. doi: 10.1017/S0033291706008002. [DOI] [PubMed] [Google Scholar]
- 13.Babkoff H, French J, Whitmore J, Sutherlin R. Single-dose bright light and/or caffeine effect on nocturnal performance. Aviat Space Environ Med. 2002;73:341–50. [PubMed] [Google Scholar]
- 14.Wright KP, Jr, Badia P, Myers BL, Plenzler SC. Combination of bright light and caffeine as a countermeasure for impaired alertness and performance during extended sleep deprivation. J Sleep Res. 1997;6:26–53. doi: 10.1046/j.1365-2869.1997.00022.x. [DOI] [PubMed] [Google Scholar]
- 15.Hayashi M, Masuda A, Hori T. the alerting effects of caffeine, bright light and face washing after a short daytime nap. Clin neurphysiol. 2003;114:2268–78. doi: 10.1016/s1388-2457(03)00255-4. [DOI] [PubMed] [Google Scholar]
- 16.Badia P, Myers B, Boecker M, Culpepper J, Harsh JR. Bright light effects on body temperature, alertness, EEG and behavior. Physiol Behav. 1991;50:583–8. doi: 10.1016/0031-9384(91)90549-4. [DOI] [PubMed] [Google Scholar]
- 17.Wehr TA, Duncan WC, Jr, Sher L, Aeschbach D, Schwartz PJ, Turner EH, et al. A circadian signal of change of season in patients with seasonal affective disorder. Arch Gen Psychiatry. 2001;58:1108–14. doi: 10.1001/archpsyc.58.12.1108. [DOI] [PubMed] [Google Scholar]
- 18.Lewy AJ, Sack RL, Singer CM, White DM, Hoban TM. Winter depression and the phase-shift hypothesis for bright light’s therapeutic effects: history, theory, and experimental evidence. J Biol Rhythms. 1988;3:121–34. doi: 10.1177/074873048800300203. [DOI] [PubMed] [Google Scholar]
- 19.Terman JS, Terman M, Lo ES, Cooper TB. Circadian time of morning light administration and therapeutic response in winter depression. Arch Gen Psychiatry. 2001;58:69–75. doi: 10.1001/archpsyc.58.1.69. [DOI] [PubMed] [Google Scholar]
- 20.Lewy AJ, Sack RL. The dim light melatonin onset as a marker for circadian phase position. Chrono-biol Int. 1989;6:93–102. doi: 10.3109/07420528909059144. [DOI] [PubMed] [Google Scholar]
- 21.Sack RL, Lewy AJ, White DM, Singer CM, Fireman MJ, Vandiver R. Morning vs evening light treatment for winter depression. Evidence that the therapeutic effects of light are mediated by circadian phase shifts. Arch Gen Psychiatry. 1990;47:343–51. doi: 10.1001/archpsyc.1990.01810160043008. [DOI] [PubMed] [Google Scholar]
- 22.Neumeister A, Turner EH, Matthews JR, Postolache TT, Barnett RL, Rauh M, et al. Effects of tryptophan depletion vs catecholamine depletion in patients with seasonal affective disorder in remission with light therapy. Arch Gen Psychiatry. 1998;55:524–30. doi: 10.1001/archpsyc.55.6.524. [DOI] [PubMed] [Google Scholar]
- 23.Lam RW, Zis AP, Grewal A, Delgado PL, Charney DS, Krystal JH. Effects of rapid tryptophan depletion in patients with seasonal affective disorder in remission after light therapy. Arch Gen Psychiatry. 1996;53:41–4. doi: 10.1001/archpsyc.1996.01830010043007. [DOI] [PubMed] [Google Scholar]
- 24.Lam RW, Levitan RD, Tam EM, Yatham LN, Lamoureux S, Zis AP. L-tryptophan augmentation of light therapy in patients with seasonal affective disorder. Can J Psychiatry. 1997;42:303–6. doi: 10.1177/070674379704200309. [DOI] [PubMed] [Google Scholar]
- 25.Skwerer RG, Jacobsen FM, Duncan CC, Kelly KA, Sack DA, Tamarkin L, et al. Neurobiology of seasonal affective disorder and phototherapy. J Biol Rhythms. 1988;3:135–54. doi: 10.1177/074873048800300204. [DOI] [PubMed] [Google Scholar]
- 26.Anderson JL, Vasile RG, Mooney JJ, Blooming-dale KL, Samson JA, Schildkraut JJ. Changes in norepinephrine output following light therapy for fall/winter seasonal depression. Biol Psychiatry. 1992;32:700–4. doi: 10.1016/0006-3223(92)90299-f. [DOI] [PubMed] [Google Scholar]
- 27.Lambert GW, Reid C, Kaye DM, Jennings GL, Esler MD. Effect of sunshine and season on serotonin turn-over in the brain. Lancet. 2002;360:1840–2. doi: 10.1016/s0140-6736(02)11737-5. [DOI] [PubMed] [Google Scholar]