Abstract
To calculate the frequency of clinically important improvement in function over 30 months and identify risk factors in people who have or are at risk of knee OA. Subjects were from MOST, a longitudinal study of persons with or at high risk of knee OA. We defined Minimal Clinically Important Improvement (MCII) with WOMAC physical function using three different methods. Baseline risk factors tested for improvement included age, gender, educational attainment, presence of radiographic knee OA (ROA), the number of comorbidities, Body Mass Index (BMI), knee pain, walking speed, isokinetic knee extensor strength, depressive symptoms, physical activity, and medication usage. We used logistic regression to evaluate the association of baseline risk factors with MCII. Of the 1801 subjects (age= 63, BMI= 31, 63% female), most had mild limitations in baseline function (WOMAC = 19 +/− 11). Regardless how defined, a substantial percentage of subjects (24%–39%) reached MCII at 30 months. Compared to their counterparts, people with MCII were less likely to have ROA and to use medications, and were more likely to have a lower BMI, less knee pain, a faster walking speed, more knee strength, and fewer depressive symptoms. After adjustment, MCII was 40% to 50% less likely in those with ROA, and 1.9 to 2.0 times more likely in those walking 1.0 m/s faster than counterparts. Clinically important improvement is frequent in people with or at high risk of knee OA. The absence of ROA and a faster walking speed appear to be associated with clinically important improvements.
Keywords: Osteoarthritis, Functional limitation, Rehabilitation
INTRODUCTION
The natural history of knee pain and osteoarthritis (OA) often leads to difficulty performing functional activities(1), yet a number of persons maintain a high level of functioning(2), improve(3, 4), or recover from previous limitations(5). While this may seem contrary to the chronic progressive nature of OA, recent large observational studies from the past decade confirm this phenomenon to occur(2, 6, 7). Closer examination of these studies reveals, however, that the magnitude or clinical significance of improvement is largely unknown. In particular, it is not clear how much of the improvement in these and other studies represent change that is relevant to the patient or provider.
Beaton and others have emphasized the need to delineate between improvements in outcome which are merely statistically significant versus those which are clinically meaningful or important(8). One method to qualify the clinical significance of improvement is to use a minimally clinically important improvement (MCII) threshold, which represents the smallest improvement that is important from the subject’s perspective(9). Despite the fact that different thresholds of MCII for the Western Ontario McMaster Universities Osteoarthritis Index (WOMAC) physical function scale have been reported(9, 10), to date only one study with 44 subjects has examined the longitudinal occurrence of MCII in function in people with symptomatic hip or knee OA. This study found that eight subjects had meaningful improvement as measured by the WOMAC physical function scale over five years(11). Further study of the frequency of clinically important improvement within a larger cohort of people with knee OA is needed.
There is a robust literature examining risk factors of functional decline for persons with knee OA, however there is little known about risk factors for improvement. Previous research has identified age(4, 12), body mass index (BMI)(12–15), pain at baseline(4, 12–14, 16), and walking speeds(17, 18) to be associated with decline in function in people with knee pain, symptomatic knee OA, and older individuals. However, it is not clear if these factors for decline are also associated with clinically important improvements in function. In particular, we are interested in identifying baseline risk factors associated with MCII to help clinicians better identify which of their patients evaluated for the first time are likely to make future improvements in function. Additionally, recognizing modifiable baseline risk factors associated with improvement may provide therapeutic targets for interventions to facilitate functional gains. We will examine if factors of decline are also important for meaningful improvement in function.
Thus, the purpose of this study is 1) to examine the frequency of clinically important improvement in WOMAC physical function over 30 months using three definitions of MCII in people with or at risk of symptomatic knee OA with existing limitations in function and 2) to examine baseline risk factors associated with clinically meaningful improvement.
MATERIALS AND METHODS
Participants were recruited from the Multicenter Osteoarthritis (MOST) study, a large multicenter prospective cohort study of 3026 community-dwelling persons who had or who were at high risk of developing symptomatic knee osteoarthritis (OA) at baseline. MOST was designed to evaluate the effects of a variety of potential risk factors on the occurrence and progression of radiographic and symptomatic knee OA. Subjects aged 50 to 79 years were recruited from Birmingham, Alabama and Iowa City, Iowa. Baseline assessments took place between May 2003 and March 2005, and follow-up assessments 30 months later. Participants were defined as being at risk of developing knee OA based on known risk factors, including older age, female gender, previous knee injury or operation, and high body weight. A more detailed description of recruitment and sampling for MOST has been published elsewhere(19).
For the present study, we focused on MOST subjects with at least a minimal degree of self reported functional limitation at baseline to permit us to study possible improvement in these limitations. We defined this as a baseline WOMAC physical function score of at least a 4/68, which is consistent with a previous definition of minimal limitation in function(2). We anticipated that subjects undergoing a knee or hip replacement would likely improve in function. However we wanted to focus on the natural history of functional improvement uninfluenced by these surgical procedures. As a consequence we excluded those who underwent a new total knee or hip replacement after the baseline assessment.
The MOST study protocol was approved by the institutional review boards at the University of Iowa, University of California San Francisco, University of Alabama, and Boston University Medical Center.
Outcome measures
We selected three definitions of MCII for WOMAC physical function. Our rationale for choosing these definitions were that they were anchored to patient-based indicators of improvement and defined meaningful improvement relative to baseline WOMAC physical function scores. All MCII definitions were dichotomous outcomes (improved/not improved) and were decreases in WOMAC physical function scores since lower scores on WOMAC represent less limitation. The first two definitions, MCII 26% and MCII Tertile, were estimated from a study of 1362 people with knee pain reporting a “good, satisfactory effect with occasional episodes of pain or stiffness” following a 4 week course of non-steroidal anti-inflammatory medication(9). The last definition, MCII 17% was from a study of 192 people with knee OA who underwent 3 to 4 weeks of inpatient rehabilitation(10).
MCII 26% and MCII 17% defines meaningful improvement as a 26% and 17% decrease in WOMAC physical function ((final value − baseline value)/baseline value), respectively, with a minimum absolute decrease of 2 out of 68. For instance a baseline WOMAC Physical function score of 30 would need a 5.1 point decrease to meet meaningful improvement for MCII 17% criteria, and a 7.8 point improvement to meet MCII 26% criteria.
MCII Tertile defines meaningful improvement as absolute values (final value − baseline value) dependent on baseline WOMAC physical function scores. We considered those with a decrease of 3.6, 8.0, and 13.9 out of 68 to reach meaningful improvement within low, medium, and high baseline tertile categories, respectively. These cutoff values were employed from the previous study of a 4 week course of non-steroidal anti-inflammatory medication in persons with knee pain(9).
Baseline risk factors
All participants underwent bilateral weight-bearing posteroanterior (PA) and lateral fixed-flexion radiographic evaluation of the knee, as described elsewhere(19). We noted the presence or absence of radiographic knee osteoarthritis (ROA) in either knee. We defined ROA based on radiographic findings in either tibiofemoral or patellofemoral joints. For the tibiofemoral jont this was a Kellgren and Lawrence (KL) grade ≥ 2, and for the patellofemoral joint an osteophyte score ≥ 2, or any joint space narrowing score ≥ 2 with any osteophyte, sclerosis, or cyst score of ≥ 1 on a lateral plain view film(20, 21). The inter-rater reliability weighted kappa for the KL grade at baseline was 0.80. For persons with ROA, we noted if subjects had ROA in one or both knees.
Subjects self-reported age in years, gender, and educational attainment as attending some college or not. Comorbidities were estimated as none or one or more with a validated self report measure, the modified Charlson comorbidity index (22). Body Mass Index (BMI) was classified according to the World Health Organization categories(23) and computed from standardized weight and height assessments. Knee pain (VAS) of the more painful knee was used for analysis and was quantified as the average knee pain over the past 30 days as measured on a horizontal line with 0 and 10 as endpoints. Walking speed was measured continuously in meters per second from walking at a usual pace over 20 meters. Knee strength was classified in tertiles using the weaker knee as a data point, and was calculated from the mean of four isokinetic knee extensor torque repetitions at 60 deg/sec* measured in Newton-Meters. Depressive symptoms were classified by risk of significant depressive symptomatology measured with the Center for Epidemiologic Studies Depression Scale (CES-D: 0–60) greater or equal to 16 (24). Physical activity was measured in tertiles with the Physical Activity Scale for the Elderly (PASE:0–360)(25).
We also examined if subjects were or were not taking medications or had a steroid injection up to the baseline assessment. Specifically, we asked subjects if they took the following medications for arthritis every day or almost everyday: Aspirin, Ibuprofen, Acetominophen, Cox2 inhibitors, or other non-steroidal or anti-inflammatory medications. We also asked if subjects had a steroid injection, such as Cortisone, in either knee in the past 12 months from the baseline assessment.
Statistical Analysis
To examine differences between people with and without clinically meaningful improvement, means and 95% confidence intervals were applied for continuous variables and odds ratios and chi-square tests for categorical variables. We used multiple logistic regression for each of the three definitions of MCII mutually adjusting for all baseline risk factors. We applied the Hosmer and Lemeshow Test to examine the goodness of fit of the regression models.
We investigated the association between the following baseline risk factors with clinically meaningful improvement based on existing evidence linking them to changes in function(1, 2, 19, 26–28): age, gender, educational attainment, ROA, comorbidities, BMI, knee pain, walking speed, knee extensor strength, depressive symptoms, physical activity, and medications. We performed additional analyses restricted to those only with ROA at baseline given these subjects may have a different frequency of improvement and associated risk factors than those without ROA. We examined the same baseline risk factors with the addition of the presence of ROA in one or both knees.
RESULTS
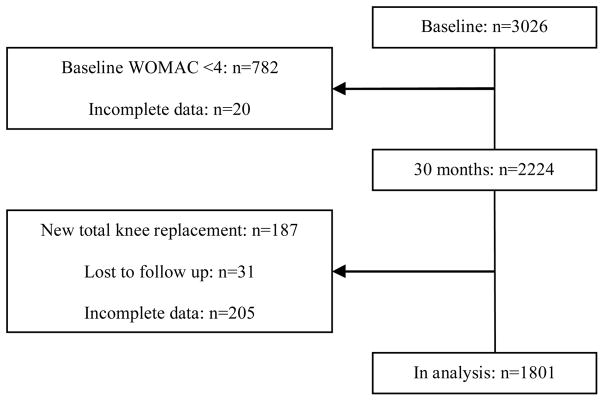
Of the 3026 subjects from the MOST study at baseline, 782 had WOMAC physical function scores less than 4, and 20 did not have complete data. At the 30 month follow up, 187 had a new total hip or knee replacement, 31 were lost of follow up, and 205 did not have complete data or did not complete the 30 month assessment, leaving 1801 subjects used for the present analyses. Figure 1. Compared to those included for analysis (n=1801), the excluded sample (n= 1225) had a lower percentage of females (56% vs 63%), fewer people with ROA (52% vs 59%), and less people with comorbidities (40% vs 45%) (all p<0.05). There was no difference in age, education, or BMI. The most frequently missing risk factor among the 1801 included in the analyses was ROA status (n=15) followed by level of education (n=13).
Figure 1.
Flow chart of subjects though baseline and 30 months.
Of the subjects included, the mean age was 62.7 years [sd]= 8.0. Most subjects were female (63%), had some college education (71%), had radiographic knee osteoarthritis (ROA) (59%), had no comorbidities (55%), and were overweight (BMI =30.8, sd=6.0 kg/m2). A little over one-third reported taking medication for arthritis or having a steroid injection in either knee at baseline (39%). Most subjects had mild to moderate limitations in function (mean WOMAC 18.7 sd 11.2). Table 1. Using different definitions of MCII, clinically meaningful improvement occurred in 615 (34%) for the MCII 26% method, 704 (39%) for the MCII 17% method, and 425 (24%) for the MCII Tertile method. There were 425 subjects meeting criteria for all three definitions of MCII. The percentage of subjects meeting MCII across the range of baseline WOMAC physical function scores is depicted in Figure 2.
Table 1.
Subject characteristics and modifiable factors at baseline (n= 1801)
| Age [years (sd)] | 62.7 (8.0) |
| Gender [n (%) female] | 1135 (63) |
| Education [ n (%) some college] | 1279 (71) |
| ROA* [n (%)] | 1045 (58.5) |
| Patelofemoral ROA [n (%)] | 80 (4.5) |
| Tibiofemoral ROA [n (%)] | 604 (33.8) |
| Patelofemoral and Tibiofemoral ROA [n (%)] | 361 (20.2) |
| Comorbidities [ n (%) none] | 991 (55) |
| BMI† [kg/m2(sd)] | 30.9 (6.0) |
| Knee Pain [VAS‡ 0–10 (sd)] | 3.0 (2.2) |
| Walking Speed [m/s (sd)]§ | 1.18 (0.2) |
| Knee Strength [Newton Meters (sd)]** | 68 (36) |
| Depressive Symptoms [CES-D†† 0–60 (sd)] | 8 (7.7) |
| Physical Activity [PASE‡‡ 0–360 (sd)] | 171 (87) |
| Arthritis medications or steroid injection§§ [n (%)] | 698 (39) |
| Baseline WOMAC*** Physical Function Score [4–68 (sd)] | 18.7 (11.2) |
ROA = Radiographic knee osteoarthritis
BMI = Body Mass Index
VAS = Visual Analogue Scale
Walking Speed measured in meters per second (m/s) over a 20 meter walk at a usual pace
Isokinetic knee extensor strength. Weaker value of two knees used for analysis.
CES-D = Center for Epidemiologic Studies Depression Scale
PASE = Physical Activity Scale for the Elderly
Arthritis medication taken every day or almost everyday including Aspirin, Ibuprofen, Acetominophen, Cox2 inhibitors, or other non-steroidal or anti-inflammatory medications, or a steroid injection, such as Cortisone, in either knee in the past 12 months.
WOMAC = Western Ontario McMaster Universities Osteoarthritis Index
Figure 2.
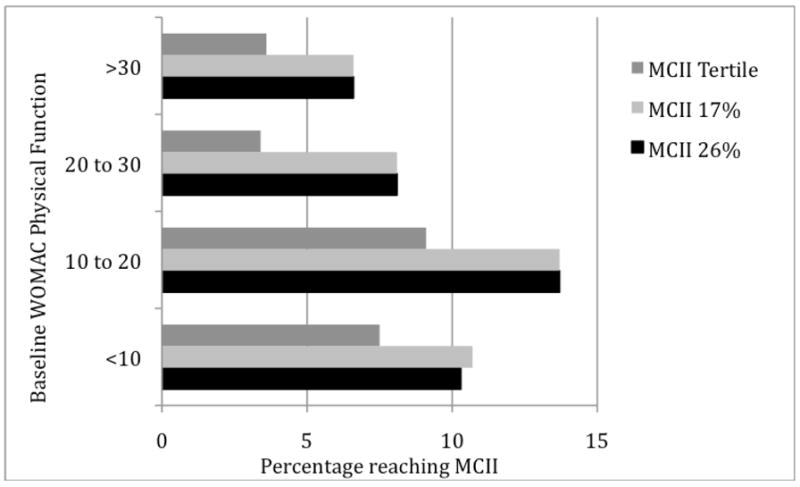
The percentage of subjects with meaningful improvement by MCII 26%1, MCII 17%2, and MCII Tertile3 by baseline WOMAC4 physical function score groups.
126% decrease in WOMAC physical function to reach meaningful clinically important improvement
217% decrease in WOMAC physical function to reach meaningful clinically important improvement
3 3.6, 8.0, and 13.9 out of 68 for those in low, medium, and high baseline WOMAC physical function tertiles, respectively
4WOMAC = Western Ontario McMaster Universities Osteoarthritis Index (0–68)
Baseline risk factors associated with meaningful improvement
For risk factors at baseline measured continuously, people with clinically important improvement had statistically significant lower BMI, faster walking speeds, and fewer depressive symptoms across all three MCII methods, less knee pain for the MCII 26% and MCII Tertile methods, and more knee strength using the MCII Tertile method compared to their counterparts. Table 2. For risk factors measured categorically, people with ROA were 40% to 60% less likely to have clinically important improvement across all three MCII methods, and people with at least some college education were 1.3 times more likely to have clinically important improvement for the MCII 26% and Tertile methods compared to their counterparts. Lastly, persons who take arthritis medication or who had had a steroid injection in the last 12 months were 20% to 40% less likely to have clinically important improvement across all three MCII methods compared with their counterparts. Table 3
Table 2.
Differences (without MCII – with MCII) and 95% confidence intervals in risk factors measured continuously at baseline between those with and without Meaningful Clinical Important Improvement (MCII)**.
| MCII Definitions | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| MCII 26%* | MCII 17%† | MCII Tertile‡ | |||||||
| Meaningful Improvement [mean (sd)] | No Meaningful Improvement [mean (sd)] | Difference [95 CI] | Meaningful Improvement [mean (sd)] | No Meaningful Improvement [mean (sd)] | Difference [95 CI] | Meaningful Improvement [mean (sd)] | No Meaningful Improvement [mean (sd)] | Difference [95 CI] | |
| Age in years | 62.17 (8) | 62.7 (8) | 0.0 [−0.8,0.8] | 62.7 (8.0) | 62.7 (8.0) | 0.0 [−0.7,0.8] | 62.5 (7.6) | 62.8 (8.1) | 0.3 [−0.5,1.2] |
| BMI§ [kg/m] | 30.2 (5.8) | 31.2 (6.0) | 1.0 [0.4,1.6] | 30.3 (5.8) | 31.2 (6.1) | 0.9 [0.3,1.5] | 30.0 (5.6) | 31.1 (6.1) | 1.1 [0.5,1.8] |
| Knee Pain [VAS 0–10] | 2.8 (2.3) | 3.2 (2.3) | 0.4 [0.2,0.6] | 3.0 (2.3) | 3.1 (2.3) | 0.1 [−0.9,3.5] | 2.8 (2.3) | 3.2 (2.3) | 0.4 [0.2,0.7] |
| Walk Speed in m/s | 1.21 (0.2) | 1.17 (0.2) | −0.04 [−0.06, −0.02] | 1.20 (0.2) | 1.17 (0.2) | −0.03 [−0.06, −0.02] | 1.22 (0.2) | 1.17 (0.2) | −0.05 [−0.07, −0.03] |
| Knee Strength in Newton meters | 70.7 (36.1) | 67.1 (35.8) | −3.6 [−7.3,0.0] | 70.1 (36.3) | 67.1 (35.8) | −2.9 [−6.5,0.6] | 73.0 (35.5) | 66.9 (36.1) | −6.1 [−10.3, −2.1] |
| Depressive Symptoms [CES-D 0–60] | 7.3 (7.3) | 8.5 (8.0) | 1.2 [0.5,2.0] | 7.4 (7.3) | 8.5 (8.0) | 1.1 [0.4,1.8] | 7.4 (7.4) | 8.3 (7.9) | 0.9 [0.1,1.7] |
| Physical Activity [PASE 0–360] | 175.8 (90.7) | 169.6 (85.1) | −6.2 [−14.7,2.3] | 173.8 (89.9) | 170.4 (85.3) | [−3.4−11.7,4.8] | 177.1 (93.5) | 170.0 (85.0) | −7.1 [−16.5,2.5] |
26% decrease in WOMAC physical function to reach meaningful clinically important improvement
17% decrease in WOMAC physical function to reach meaningful clinically important improvement
3.6, 8.0, and 13.9 out of 68 for those in low, medium, and high baseline WOMAC physical function tertiles, respectively
BMI = Body Mass Index
Bolded items represent p<0.05.
Table 3.
Odds of Meaningful Clinical Important Improvement (MCII)** and 95% confidence intervals (CI) for risk factors measured categorically at baseline. Higher odds represent a higher likelihood of meaningful improvement.
| MCII Definitions | ||||||
|---|---|---|---|---|---|---|
| MCII 26%* | MCII 17%† | MCII Tertile‡ | ||||
| Meaningful Improvement (%) | OR [95% CI] | Meaningful Improvement (%) | OR [95% CI] | Meaningful Improvement (%) | OR [95% CI] | |
| Female | 34 | 1.0 (reference) | 39 | 1.0 (reference) | 23 | 1.0 (reference) |
| Male | 34 | 1.0 [0.8,1.2] | 38 | 1.0 [0.8,1.2] | 25 | 1.2 [0.9, 1.5] |
| Less than some college | 30 | 1.0 (reference) | 36 | 1.0 (reference) | 20 | 1.0 (reference) |
| At least some college education | 36 | 1.3 [1.1,1.6] | 41 | 1.2 [1.0,1.5] | 25 | 1.4 [1.1, 1.8] |
| ROA§ absent | 43 | 1.0 (reference) | 47 | 1.0 (reference) | 33 | 1.0 (reference) |
| ROA present | 27 | 0.5 [0.4,0.6] | 33 | 0.6 [0.5,0.7] | 17 | 0.4 [0.3, 0.5] |
| No comorbidities | 36 | 1.0 (reference) | 41 | 1.0 (reference) | 24 | 1.0 (reference) |
| One or more comorbidities | 31 | 1.0 [1.0,1.0] | 36 | 1.0 [1.0,1.0] | 22 | 1.0 [1.0, 1.0] |
| No arthritis medications or steroid injection | 37 | 1.0 (reference) | 41 | 1.0 (reference) | 26 | 1.0 (reference) |
| Arthritis medications or steroid injection | 28 | 0.7 [0.5,0.9] | 35 | 0.8 [0.6,1.0] | 17 | 0.6 [0.5,0.8] |
26% decrease in WOMAC physical function to reach meaningful clinically important improvement
17% decrease in WOMAC physical function to reach meaningful clinically important improvement
3.6, 8.0, and 13.9 out of 68 for those in low, medium, and high baseline WOMAC physical function tertiles, respectively
ROA = Radiographic knee osteoarthritis
Bolded items represent confidence intervals which do not cross 1.0.
After mutual adjustment for all risk factors, ROA status and walking speed remained associated with MCII across all three methods of estimating MCII. People with ROA were 40% to 50% less likely to have clinically important improvement compared to those without ROA, and people able to walk 1.0 meters per second (m/s) faster than their counterparts were 1.9 to 2.0 times more likely to have clinically important improvement. Table 4
Table 4.
Odds ratios (OR) and 95% confidence intervals among all subjects for risk factors associated with Minimally Clinically Important Improvement (MCII) in WOMAC* physical function mutually adjusted for for other factors†, with higher OR representing greater likelihood of MCII.
| n | MCII Definitions | ||||
|---|---|---|---|---|---|
| MCII 26%‡ | MCII 17%§ | MCII Tertile** | |||
| ROA †† | Absent | 756 | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) |
| Present | 1045 | 0.6 [0.4,0.7] | 0.6 [0.5,0.7] | 0.5 [0.4,0.6] | |
| Walking Speed [meters/second (m/s)] | OR of MCII per 1.0 m/s | 1801 | 1.9 [1.0,3.4] | 1.9 [1.1,3.3] | 2.0 [1.0,3.9] |
| Number of subjects included in logistic models | 1768 | 1768 | 1768 | ||
| Hosmer and Lemeshow Test (p-value) | 8 degrees of freedom | 0.08 | 0.61 | 0.32 | |
WOMAC = Western Ontario McMaster Universities Osteoarthritis Index
Mutually adjusted for age, gender, education, comorbidities, body mass index, knee pain, knee strength, depressive symptoms, physical activity, and medication usage at baseline.
26% decrease in WOMAC physical function to reach meaningful clinically important improvement
17% decrease in WOMAC physical function to reach meaningful clinically important improvement
3.6, 8.0, and 13.9 out of 68 for those in low, medium, and high baseline WOMAC physical function tertiles, respectively
ROA= Radiographic knee osteoarthritis
Analysis including only those with ROA
Of the 1045 subjects with ROA, 470 (45%) had ROA in one knee and 575 (55%) had ROA in both knees. Clinically meaningful improvement occurred in 288 (28%) for the MCII 26% method, 346 (33%) for the MCII 17% method, and 179 (17%) for the MCII Tertile method. People with clinically important improvement had faster walking speeds and were more likely to have ROA in one knee across all three methods of estimating MCII, fewer depressive symptoms for the MCII 26% and MCII 17% methods, and less knee pain and a lower BMI for the MCII 26% and MCII 17%, methods, respectively, compared to their counterparts (data not shown). After mutual adjustment, we found persons in the highest strength tertile to be 1.9 to 2.2 times more likely to have clinically meaningful improvement across all three methods of estimating MCII compared with those in the lowest strength tertile. Table 5
Table 5.
Odds ratios (OR) and 95% confidence intervals among persons with ROA at baseline for risk factors associated with Minimally Clinically Important Improvement (MCII) in WOMAC* physical function mutually adjusted for other factors†, with higher OR representing greater likelihood of MCII.
| Mean (sd) | n | MCII Definitions | |||
|---|---|---|---|---|---|
| MCII 26%‡ | MCII 17%§ | MCII Tertile** | |||
| Knee strength [Newton-Meters] | |||||
| Low | 27.1 (9.7) | 316 | 1.0 (reference) | 1.0 (reference) | 1.0 (reference) |
| Medium | 54.75 (8.1) | 313 | 1.5 [1.0,2.2] | 1.4 [1.0,2.0] | 1.6 [1.0,2.6] |
| High | 104.0 (28.3) | 315 | 1.9 [1.1,3.0] | 1.7 [1.1,2.7] | 2.2 [1.2,4.0] |
| Number of subjects included in logistic models | 935 | 935 | 935 | ||
| Hosmer and Lemeshow Test (p-value) | 8 degrees of freedom | 0.18 | 0.31 | 0.37 | |
WOMAC = Western Ontario McMaster Universities Osteoarthritis Index
Mutually adjusted for age, gender, education, comorbidities, body mass index, knee pain, depressive symptoms, physical activity, ROA in one or both knees, and medication usage at baseline.
26% decrease in WOMAC physical function to reach meaningful clinically important improvement
17% decrease in WOMAC physical function to reach meaningful clinically important improvement
3.6, 8.0, and 13.9 out of 68 for those in low, medium, and high baseline WOMAC physical function tertiles, respectively
DISCUSSION
A substantial percentage of persons (24% – 39%) in our study had clinically important improvements in WOMAC physical function 30 months after initial assessment. People who had clinically important improvement had a lower BMI, faster walking speeds, and fewer depressive symptoms across all three definitions of MCII unadjusted for other risk factors. After mutual adjustment for other risk factors, people who improved walked faster and did not have radiographic evidence of knee OA at baseline compared with those who did not improve.
The MCII allows one to estimate how many people had clinically meaningful improvement, and represents the smallest improvement in score which can be regarded as important. Limiting investigation of longitudinal changes to group level analysis, such as mean change and standard deviation summary statistics, may create a perception that subjects’ functional status is fixed. For instance, Botha-Scheepers and colleagues recently reported little change in functional limitations in a cohort of 115 people with symptomatic knee and hip OA over 2 years as evidenced by a mean increase of 2.2 and standard deviation of 12.7 in WOMAC physical function(29). We found similar mean change in WOMAC physical function (mean=0.7, standard deviation of 9.8), however our evaluation of change at the level of the individual revealed a large percentage of people with substantial improvement. Improvements in functional limitation have been reported elsewhere. Most recently, Aysis and Dieppe found that 107 (19.6%) of 545 subjects with functional limitation at baseline had improvement when measured 8 years later, though these changes were not necessarily measured at a level of clinically meaningful improvement(14).
Our study findings reveal that people with ROA had at least a 40% reduction in odds of clinically important improvement in function across all three definitions of MCII than those without ROA. Several studies support the notion that ROA influences changes in function. Roos and colleagues found that the presence of tibiofemoral OA was predictive of decline in sport and recreation activities 4 to 10 years later(30), and Davis and coauthors reported people with ROA at baseline were more likely to report difficulty with mobility related activities 10 years later than those without ROA(31). While some studies did not find an association between ROA status and function(32, 33), several reasons exist which may have contributed to this association in our study. First, we had ample power and heterogeneity of age to detect this association. We included 1801 people who were at least 50 years of age. Second, our primary outcome was clinically meaningful improvement in function, which was not used in previous studies(32, 33). Lastly, our study took knee radiographs with a standing fixed-flexion body position which has been shown to have high test-retest reliability(34). Other studies used a full extended position of the knee(32, 33), which has been shown to be less reliable and accurate with estimating the severity of radiographic changes in the knee than a standing fixed-flexion body position(35).
Walking speed over 20 meters was also found to be associated with meaningful improvement in function across all three definitions of MCII. This is consistent with previous studies which show that slow walking speed in older adults is associated with a variety of adverse outcomes including incident functional limitation(18), hospital admission(36), and mortality(37–39). Our findings extend walking speed as a marker of meaningful improvement in younger adults over the age of 50 with or at high risk of knee OA. The speed of walking can be considered an estimate of walking ability. Given that the WOMAC physical function subscale measures self reported difficulty with walking and several tasks for which walking is prerequisite, we expected faster walking speeds to be associated of clinically important improvement in function.
Certainly it is plausible that interventions which took place over 30 months may be responsible for subsequent meaningful improvements in function. However, our cohort had mild to moderate limitations in function at baseline, as evidenced by a mean WOMAC physical function score was 18.7. Hence most study subjects would not have been referred for physical rehabilitation. For medications, we found persons taking prescription medication or those who had a steroid injection by the baseline examination to be less likely to have meaningful improvements in function in the unadjusted analysis. It is likely that these individuals had greater functional involvement and were hence less likely to improve. Thus, the association of persons starting to take medications over the 30 month period with meaningful improvement in function would be confounded by indication(40).
There are some limitations in our study. First, we employed cutoff values for MCII from pervious studies that used patient anchored definitions of meaningful improvements, and not other anchoring methods such as clinician or consensus cutoffs. Second, Gill and colleagues have recently suggested that fluctuations between states of ability and inability are much higher when outcomes are measured monthly compared to longer assessment intervals(41). Since we calculated change in WOMAC physical function using only two reference points, baseline and 30 months, it is possible the proportion of those with transient meaningful improvement on a monthly basis may be even more common than we estimated over 30 months. Future studies should employ repeated measures within shorter time intervals to investigate the cumulative frequency of meaningful improvement and time course of fluctuations in function. Third, we measured the construct of function using a self report instrument, and lower rates of improvement have been reported for performance based measures compared to self report measures(33). Future study should incorporate both self-report and performance-based outcomes to better measure the construct of function. Fourth, we only used one measure, VAS, to estimate the construct of knee pain, which may underestimate the ability of knee pain to predict meaningful improvements in function. We were reluctant to use the WOMAC pain score as a modifiable factor due to its high correlation with the WOMAC physical function score(42). Fifth, potential bias may exist in our estimate of 24–39% of subjects achieving MCII. We excluded those with new total joint replacements, and included those who had or were at high risk of symptomatic knee OA. Also, it is important to note that the percentage of those with meaningful improvement will naturally be higher using the MCII 17% cut-point compared with MCII 26%, given that less change is needed for meaningful improvement. Sixth, we arbitrarily selected a WOMAC physical function cutoff of 4/68 to represent those with at least a minimal amount of functional limitation. We have analyzed the data using other cutoffs (range 3–6) and found similar percentages of recovery across all methods of calculating MCII. Lastly, we did not differentiate between persons who had one versus two painful knees, which could have an effect on meaningful improvement in function. Future research should investigate if persons with one painful knee are more likely to have meaningful improvement in function compared with those with two painful knees.
Nonetheless, our study has two important clinically relevant conclusions. First, meaningful improvement is common among those with generally mild to moderate self reported limitations in function who have or are at high risk for knee over a two and a half year period. Our study found a robust percentage of people to have these improvements irrespective of the method used to estimate improvement. We emphasize that our definition of meaningful improvement excluded those with unchanged or worsening WOMAC physical function scores over 30 months. Second, people without radiographic evidence of knee OA and those with fast walking speeds are more likely to have improvements than those with ROA and slower walking speeds. Providers may want to consider these risk factors when determining who may benefit from therapeutic intervention.
Acknowledgments
We would like to acknowledge the study subjects for their participation in the MOST study.
Supported by NIH U01 AG18820, U01 AG 18832, U01 AG 18947, U01 AG 19069 NIDRR ARRT Grant H133P050001, AR47785, AR007598 and the ARHP New Investigator Award
Footnotes
COMPETING INTERESTS:
None.
This paper was presented at the Association of Rheumatology Health Professionals. Annual Meeting, San Francisco, CA, November 2008, and the American Physical Therapy Association, Combined Section Meeting, Las Vegas, NV, February 2009.
Cybex 350 Isokinetic Test and Exercise System and HUMAC software version 4.3.2/CYBEX 300 for Windows98 Software Package
Publisher's Disclaimer: This is a pre-copy-editing, author-produced PDF of an article accepted for publication in The Journal of Rheumatology following peer review. The definitive publisher-authenticated version White D, Keysor J, LaValley M, Lewis C, Torner J, Nevitt M, et al. Clinically important improvement in function is common in people with or at high risk of knee OA: the MOST study. J Rheumatol 2010;37:1244-51. is available online at: http://www.jrheum.org/content/37/6/1244.abstract
References
- 1.Guccione AA, Felson DT, Anderson JJ. Defining arthritis and measuring functional status in elders: methodological issues in the study of disease and physical disability. Am J Public Health. 1990 Aug;80(8):945–9. doi: 10.2105/ajph.80.8.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003 Dec;48(12):3359–70. doi: 10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- 3.Belo JN, Berger MY, Koes BW, Bierma-Zeinstra SM. The prognostic value of the clinical ACR classification criteria of knee osteoarthritis for persisting knee complaints and increase of disability in general practice. Osteoarthritis Cartilage. 2009 Apr 16; doi: 10.1016/j.joca.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 4.van der Waal JM, Bot SD, Terwee CB, van der Windt DA, Scholten RJ, Bouter LM, et al. Course and prognosis of knee complaints in general practice. Arthritis Rheum. 2005 Dec 15;53(6):920–30. doi: 10.1002/art.21581. [DOI] [PubMed] [Google Scholar]
- 5.Ayis S, Ebrahim S, Williams S, Juni P, Dieppe P. Determinants of reduced walking speed in people with musculoskeletal pain. J Rheumatol. 2007 Sep;34(9):1905–12. [PubMed] [Google Scholar]
- 6.Dieppe P, Cushnaghan J, Tucker M, Browning S, Shepstone L. The Bristol ‘OA500 study’: progression and impact of the disease after 8 years. Osteoarthritis Cartilage. 2000 Mar;8(2):63–8. doi: 10.1053/joca.1999.0272. [DOI] [PubMed] [Google Scholar]
- 7.Peters TJ, Sanders C, Dieppe P, Donovan J. Factors associated with change in pain and disability over time: a community-based prospective observational study of hip and knee osteoarthritis. Br J Gen Pract. 2005 Mar;55(512):205–11. [PMC free article] [PubMed] [Google Scholar]
- 8.Beaton DE, Bombardier C, Katz JN, Wright JG. A taxonomy for responsiveness. J Clin Epidemiol. 2001 Dec;54(12):1204–17. doi: 10.1016/s0895-4356(01)00407-3. [DOI] [PubMed] [Google Scholar]
- 9.Tubach F, Ravaud P, Baron G, Falissard B, Logeart I, Bellamy N, et al. Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: the minimal clinically important improvement. Ann Rheum Dis. 2005 Jan;64(1):29–33. doi: 10.1136/ard.2004.022905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Angst F, Aeschlimann A, Michel BA, Stucki G. Minimal clinically important rehabilitation effects in patients with osteoarthritis of the lower extremities. J Rheumatol. 2002 Jan;29(1):131–8. [PubMed] [Google Scholar]
- 11.Johnson SR, Archibald A, Davis AM, Badley E, Wright JG, Hawker GA. Is self-reported improvement in osteoarthritis pain and disability reflected in objective measures? J Rheumatol. 2007 Jan;34(1):159–64. [PubMed] [Google Scholar]
- 12.Mallen CD, Peat G, Thomas E, Lacey R, Croft P. Predicting poor functional outcome in community-dwelling older adults with knee pain: prognostic value of generic indicators. Ann Rheum Dis. 2007 Nov;66(11):1456–61. doi: 10.1136/ard.2006.067975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomas E, Peat G, Mallen C, Wood L, Lacey R, Duncan R, et al. Predicting the course of functional limitation among older adults with knee pain: do local signs, symptoms and radiographs add anything to general indicators? Annals of the rheumatic diseases. 2008 Feb 4; doi: 10.1136/ard.2007.080945. [DOI] [PubMed] [Google Scholar]
- 14.Ayis S, Dieppe P. The natural history of disability and its determinants in adults with lower limb musculoskeletal pain. The Journal of rheumatology. 2009 Mar;36(3):583–91. doi: 10.3899/jrheum.080455. [DOI] [PubMed] [Google Scholar]
- 15.Rejeski WJ, Ip EH, Marsh AP, Zhang Q, Miller ME. Obesity influences transitional states of disability in older adults with knee pain. Arch Phys Med Rehabil. 2008 Nov;89(11):2102–7. doi: 10.1016/j.apmr.2008.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jinks C, Jordan K, Croft P. Osteoarthritis as a public health problem: the impact of developing knee pain on physical function in adults living in the community: (KNEST 3) Rheumatology (Oxford) 2007 May;46(5):877–81. doi: 10.1093/rheumatology/kem013. [DOI] [PubMed] [Google Scholar]
- 17.Cesari M, Kritchevsky SB, Penninx BW, Nicklas BJ, Simonsick EM, Newman AB, et al. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005 Oct;53(10):1675–80. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 18.Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000 Apr;55(4):M221–31. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 19.Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, et al. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007 Sep;56(9):2986–92. doi: 10.1002/art.22851. [DOI] [PubMed] [Google Scholar]
- 20.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957 Dec;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Felson DT, McAlindon TE, Anderson JJ, Naimark A, Weissman BW, Aliabadi P, et al. Defining radiographic osteoarthritis for the whole knee. Osteoarthritis Cartilage. 1997 Jul;5(4):241–50. doi: 10.1016/s1063-4584(97)80020-9. [DOI] [PubMed] [Google Scholar]
- 22.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996 Jan;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 23.WHO. WHO Technical Report Series 894. Geneva: World Health Organization; 2000. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. Contract No.: Document Number. [PubMed] [Google Scholar]
- 24.Radloff L. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 25.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993 Feb;46(2):153–62. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 26.Jordan J, Luta G, Renner J, Dragomir A, Hochberg M, Fryer J. Knee pain and knee osteoarthritis severity in self-reported task specific disability: the Johnston County Osteoarthritis Project. J Rheumatol. 1997 Jul;24(7):1344–9. [PubMed] [Google Scholar]
- 27.Eyler AA, Brownson RC, Bacak SJ, Housemann RA. The epidemiology of walking for physical activity in the United States. Med Sci Sports Exerc. 2003 Sep;35(9):1529–36. doi: 10.1249/01.MSS.0000084622.39122.0C. [DOI] [PubMed] [Google Scholar]
- 28.Penninx BW, Guralnik JM, Ferrucci L, Simonsick EM, Deeg DJ, Wallace RB. Depressive symptoms and physical decline in community-dwelling older persons. Jama. 1998 Jun 3;279(21):1720–6. doi: 10.1001/jama.279.21.1720. [DOI] [PubMed] [Google Scholar]
- 29.Botha-Scheepers S, Watt I, Rosendaal FR, Breedveld FC, Hellio le Graverand MP, Kloppenburg M. Changes in outcome measures for impairment, activity limitation, and participation restriction over two years in osteoarthritis of the lower extremities. Arthritis Rheum. 2008 Dec 15;59(12):1750–5. doi: 10.1002/art.24080. [DOI] [PubMed] [Google Scholar]
- 30.Roos EM, Bremander AB, Englund M, Lohmander LS. Change in self-reported outcomes and objective physical function over 7 years in middle-aged subjects with or at high risk of knee osteoarthritis. Ann Rheum Dis. 2008 Apr;67(4):505–10. doi: 10.1136/ard.2007.074088. [DOI] [PubMed] [Google Scholar]
- 31.Davis MA, Ettinger WH, Neuhaus JM, Mallon KP. Knee osteoarthritis and physical functioning: evidence from the NHANES I Epidemiologic Followup Study. J Rheumatol. 1991 Apr;18(4):591–8. [PubMed] [Google Scholar]
- 32.Barker K, Lamb SE, Toye F, Jackson S, Barrington S. Association between radiographic joint space narrowing, function, pain and muscle power in severe osteoarthritis of the knee. Clin Rehabil. 2004 Nov;18(7):793–800. doi: 10.1191/0269215504cr754oa. [DOI] [PubMed] [Google Scholar]
- 33.Miller ME, Rejeski WJ, Messier SP, Loeser RF. Modifiers of change in physical functioning in older adults with knee pain: the Observational Arthritis Study in Seniors (OASIS) Arthritis Rheum. 2001 Aug;45(4):331–9. doi: 10.1002/1529-0131(200108)45:4<331::AID-ART345>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 34.Kothari M, Guermazi A, von Ingersleben G, Miaux Y, Sieffert M, Block JE, et al. Fixed-flexion radiography of the knee provides reproducible joint space width measurements in osteoarthritis. Eur Radiol. 2004 Sep;14(9):1568–73. doi: 10.1007/s00330-004-2312-6. [DOI] [PubMed] [Google Scholar]
- 35.Buckland-Wright JC, Macfarlane DG, Williams SA, Ward RJ. Accuracy and precision of joint space width measurements in standard and macroradiographs of osteoarthritic knees. Ann Rheum Dis. 1995 Nov;54(11):872–80. doi: 10.1136/ard.54.11.872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Studenski S, Perera S, Wallace D, Chandler JM, Duncan PW, Rooney E, et al. Physical performance measures in the clinical setting. Journal of the American Geriatrics Society. 2003 Mar;51(3):314–22. doi: 10.1046/j.1532-5415.2003.51104.x. [DOI] [PubMed] [Google Scholar]
- 37.Perera S, Studenski S, Chandler JM, Guralnik JM. Magnitude and patterns of decline in health and function in 1 year affect subsequent 5-year survival. The journals of gerontology. 2005 Jul;60(7):894–900. doi: 10.1093/gerona/60.7.894. [DOI] [PubMed] [Google Scholar]
- 38.Hardy SE, Perera S, Roumani YF, Chandler JM, Studenski SA. Improvement in usual gait speed predicts better survival in older adults. Journal of the American Geriatrics Society. 2007 Nov;55(11):1727–34. doi: 10.1111/j.1532-5415.2007.01413.x. [DOI] [PubMed] [Google Scholar]
- 39.Dumurgier J, Elbaz A, Ducimetiere P, Tavernier B, Alperovitch A, Tzourio C. Slow walking speed and cardiovascular death in well functioning older adults: prospective cohort study. BMJ. 2009;339:b4460. doi: 10.1136/bmj.b4460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Signorello LB, McLaughlin JK, Lipworth L, Friis S, Sorensen HT, Blot WJ. Confounding by indication in epidemiologic studies of commonly used analgesics. Am J Ther. 2002 May–Jun;9(3):199–205. doi: 10.1097/00045391-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 41.Gill TM, Hardy SE, Williams CS. Underestimation of disability in community-living older persons. J Am Geriatr Soc. 2002 Sep;50(9):1492–7. doi: 10.1046/j.1532-5415.2002.50403.x. [DOI] [PubMed] [Google Scholar]
- 42.Terwee CB, van der Slikke RM, van Lummel RC, Benink RJ, Meijers WG, de Vet HC. Self-reported physical functioning was more influenced by pain than performance-based physical functioning in knee-osteoarthritis patients. J Clin Epidemiol. 2006 Jul;59(7):724–31. doi: 10.1016/j.jclinepi.2005.11.019. [DOI] [PubMed] [Google Scholar]