Abstract
Introduction
A growing number of psychosocial interventions are being offered to cancer patients during and after their medical treatment. Here, we examined whether Mindfulness-Based Stress Reduction (mbsr), a stress management course, helps women to cope better with stress and illness once their breast cancer treatment is completed. Our aim was to understand how mbsr may benefit those who participate in the course.
Methods
Our cohort study enrolled 59 women in an 8-week mbsr program. They completed “before and after” questionnaires pertaining to outcomes (stress, depression, medical symptoms) and process variables (mindfulness, coping with illness, sense of coherence). Paired t-tests examined changes from before to after the mbsr course. Changes in mindfulness were correlated with changes in post-mbsr variables, and a regression analysis examined which variables contributed to a reduction in stress after program participation.
Results
Adherence to the program was 91%. Participants reported significant reductions in stress (p < 0.0001), depression (p < 0.0001), and medical symptoms (p < 0.0001), and significant improvements in mindfulness (p < 0.0001), coping with illness (p < 0.0001), and sense of coherence (p < 0.0001). Changes in mindfulness were significantly related to changes in depression, stress, emotional coping, and sense of coherence. Increases in mindfulness and sense of coherence predicted reductions in stress.
Conclusions
It appears that learning how to be mindful is beneficial for women after their treatment for breast cancer.
Keywords: Stress management, breast cancer, meditation, mbsr
1. INTRODUCTION
The crisis of a cancer diagnosis and the difficulties associated with surgery, chemotherapy, and radiation are readily acknowledged, but less attention has been paid to the challenges confronting women who have already completed breast cancer treatment. It might be surmised that they feel relieved and ready to return to daily activities, but few realize how hard that return often is 1–3. These women may need to sort out their priorities and interpersonal relationships. Perhaps they succeeded in harnessing their energy effectively to meet the demands of medical procedures and had the social support of the medical staff, family, and friends during treatment, but were then caught “off guard” with feelings of isolation and anxiety “once it was over.”
The diagnosis and treatment of cancer is an acute aspect of illness appropriately treated in tertiary care; recovery, which demands confronting the chronic nature of the disease, does not have a set place in the health care system to facilitate that confrontation. The coping skills required in these two phases of illness are different, and women may find themselves struggling to deal with new, unexpected storms after treatment. The diagnosis and treatment of cancer might be considered to be similar to Selye’s classic stress “alarm stage,” with post-treatment as the “recovery” from an extremely stressful life experience.
When patients are “discharged” from medical care, they may be faced with many unresolved existential questions pertaining to the meaning of life and its manageability and comprehensibility 3. Ruminations—that is, repetitive thoughts—about the past or future may clutter their minds; they may wonder whether stress contributed to their disease or worry about how returning to work might affect their health. Some may experience depression 4—with its concomitant symptoms of low energy, insomnia, lack of appetite or sexual desire—and sadness. Women can feel uncomfortable in their own bodies, which may be scarred, changed in shape or ability.
A psychosocial program titled Mindfulness-Based Stress Reduction (mbsr), designed at the University of Massachusetts Medical Center 5 for patients with chronic pain and other chronic illnesses, shows promise in helping women who have completed medical treatment for breast cancer to cope with the aftermath of that medical treatment 6–9. In Canada, the psychosocial team at the Tom Baker Cancer Centre in Calgary, Alberta, has published numerous studies showing improvements in stress-related symptoms, mood, and quality of life in patients with various types of cancer and at various stages of disease 10–13. What remains unclear are the underlying mechanisms for the benefits shown thus far.
Mindfulness-Based Stress Reduction differs from support groups in that information and advice concerning cancer are not provided per se. It also differs from group psychotherapy in that the instructor does not provide interpretations or encourage an exploration of past issues. For patients making the transition back into their “normal” lives, mbsr may help in several ways. Mackenzie et al. 14 conducted a qualitative study of effects of mbsr with a mixed group of cancer patients, noting five major themes:
Openness to change
Self-control through self-awareness
Shared experience
Personal growth
Spirituality
Those findings underscore the idea that mbsr addresses the more existential issues that arise in people living with cancer.
Because rumination can be a source of internal stress, it is logical that a reduction in this cognitive style may mediate the benefits of mbsr 15. Jain et al. 16, in a randomized clinical trial of mbsr with nursing and medical students, supported that hypothesis: Those in the mindfulness training group showed significant reductions in rumination.
Mindfulness meditation is one means by which a person can learn to accept what is in the present moment, not to react in a conditioned way, and to cope effectively by facing rather than avoiding current physical states, emotions, and thoughts 17. To sustain this means of relating to the self, others, and situations (and thus allowing for a greater sense of coherence to emerge), the mbsr program encourages daily meditation practice.
Starting in the fall of 2006 and continuing through the winter of 2009, we offered mbsr to women who had completed breast cancer treatment. Our aims were to provide a service to those patients and to understand the processes underlying the potential benefits that have been shown after mbsr participation 18. Thus, to the psychosocial instruments, we added measures pertaining to coping with illness, mindfulness, and sense of coherence.
2. METHODS
2.1. Procedures
Our cohort study used posters, pamphlets, and e-mail distribution of flyers to recruit women from university-affiliated hospitals and community organizations. Patients were referred by staff at those hospitals, or they themselves called after hearing about the program from another source—for example, another participant in mbsr. In the weeks preceding the start of the program, each patient came to the McGill Programs in Whole Person Care office to complete questionnaires (administered on computer) and to be interviewed by the course instructor (PLD) or by a clinical psychology postdoctoral student (RHM). The interview determined eligibility, addressed the appropriateness of the program for the potential participant, and obtained written informed consent. The study was approved by the Faculty of Medicine Institutional Review Board at McGill University. At the end of the program, women were asked to complete the same questionnaires in the same manner and were interviewed again to discuss pre–post mbsr results and topics related to the program itself. This exit interview also served as a means to encourage continued practice of meditation and yoga.
2.2. Participants
Participants were recruited into the study starting in September 2006 and ending in January 2009. Women were eligible to enrol if they were 18 years or older and had completed medical treatment for breast cancer. Participants with concurrent psychiatric disorders (for example, borderline personality, alcoholism) were excluded, because meditation may be contraindicated for them or full participation in the program may not have been possible. If a woman was considered depressed, she was instructed to talk with her physician and to seek appropriate care. These women were admitted into the program if they had the necessary support and were deemed able to concentrate and practice the types of meditation taught in the program. No one declined to participate in the study.
Using a power analysis 19, the sample size needed to find a moderate-to-large effect size was determined. Results indicated that a sample of 50 subjects would be sufficient to detect a difference of 0.5 standard deviation between standardized means (moderate effect size) using t-tests for a one-tailed test at an alpha level of 0.05 and a power of 0.80, and that 38 subjects would be needed to detect a difference of 0.70 standard deviation between standardized means (large effect size) using regression analyses with 4 variables in the model at an alpha level of 0.05 and a power of 0.80.
2.3. Intervention: MBSR Program
The mbsr program (described in Kabat–Zinn 5) was provided by the same instructor (PLD) to 5 different groups of 10–15 women per group, who met weekly for 2.5-hour classes over 8 consecutive weeks to learn mindfulness meditation and stress management techniques. Patients received a home practice manual and 4 compact discs created by the instructor to teach these meditation practices: body scan, sitting meditation, hatha yoga, and meditation involving visual imagery. The structured classes progressively taught means of coping with stress through meditation practice and dialogue about the practice in and out of the group meeting setting. Participants were asked to complete specific home practice exercises for 45–60 minutes daily. As the program progressed, they could select the type of home practice that was most beneficial for them. “Informal practice” (integrating mindfulness into daily activities) was also included in home assignments. Participation in a 6-hour silent retreat day, provided after week 6, was part of the program; the retreat consolidates what is learned throughout the program.
2.4. Outcome Measures
2.4.1. Perceived Stress Scale-10
Perceived stress, as measured by the Perceived Stress Scale–10 (pss-10), served as the primary outcome measure. The 10-item pss scale was developed to measure, for the preceding month, the extent to which respondents appraise situations in their life to be stressful 20,21. Each item is scored from 0 to 4, producing a global score that ranges from 0 to 40. Higher global scores indicate greater perceived stress. The pss, designed for use in community samples, has been shown to have good internal validity and test–retest reliability. The mean score for women in the community is 14.
2.4.2. Center for Epidemiologic Studies Depression Scale
The 20-item Center for Epidemiologic Studies Depression Scale (ces-d) screens for depression and was developed for use with community populations 22. The total score ranges from 0 to 60, with a higher score indicating more symptoms consistent with clinical depression. For the population at large, a score of 16 or more is a positive screen for depression. The ces-d has very good psychometric properties, with good internal validity and test–retest reliability.
2.4.3. Medical Symptom Checklist
The Medical Symptom Checklist lists medical symptoms that the patient may have experienced in the preceding month. It includes physical symptoms (for example, gastrointestinal, respiratory, pain) and psychosocial symptoms (for example, anxiety, sexual). Post mbsr, clinical trials and cohort studies have consistently demonstrated significant reductions in medical symptoms for patients with various medical conditions 23,24.
2.5. Process Measures
2.5.1. Coping with Health Injuries and Problems
Coping with Health Injuries and Problems (chip), a 32-item self-report questionnaire developed by Endler and Parker 25 has 4 subscales:
Distraction, which refers to the use of actions and cognitions that are aimed at avoiding preoccupation with the health problem
Palliative, which refers to engaging in self-care activities to alleviate the unpleasantness of the situation
Instrumental, which refers to focusing on task-oriented strategies to deal with illness (for example, get information, follow medical advice)
Emotional, which refers to the extent of the focus on the emotional consequences of the health problem (for example, ruminate, get frustrated)
Endler et al. 26 reported these mean (± standard deviation) scores for women with cancer (n = 109): distraction, 27.5 ± 5.8; palliative, 25.7 ± 5.2; instrumental, 33.1 ± 4.5; emotional, 23.6 ± 6.9. The chip has good reliability and validity, and it is considered a psychometrically sound measure of response to illness, applicable across diverse patient populations.
2.5.2. Sense of Coherence
The 29-item Sense of Coherence (soc) questionnaire assesses the extent to which a respondent views their internal and external environments as structured, predictable, and manageable 27. The soc assesses 3 subscales:
Comprehensibility, which refers an interpretation by respondents that the social world is rational, understandable, structured, ordered, consistent, and predictable
Manageability, which involves the extent to which respondents consider their coping resources to be available and adequate to deal with life’s challenges
Meaningfulness, which determines whether respondents appraise a situation as challenging and worth investing in or making a commitment to cope with
Respondents rate the soc items on a 7-point Likert scale, with higher scores indicating greater degrees of comprehensibility, manageability, and meaningfulness. The soc has good internal validity and good test–retest reliability. It has been used extensively in the study of health and well-being 27. In women, total scores on the soc range from 100.50 ± 28.50 to 160.50 ± 17.10 28.
2.5.3. Mindful Attention Awareness Scale
Brown and Ryan 29 developed the 15-item Mindful Attention Awareness Scale (maas) to measure mindfulness, defined as a present-centered attention to, and awareness of, accessible experiences (that is, internal and external events). It has been shown to be inversely related to rumination (mental preoccupation with the past or future), reported physical symptoms, and somatization 16. Scores on the maas range from 1 to 6, with higher scores reflecting greater degrees of mindfulness. The average maas score for a community sample is 4.22 ± 0.63 30.
One study 29 used the maas before and after a mbsr program for patients with cancer, finding that higher maas scores were related with less distress and fewer stress-related symptoms. The mean score of the maas for cancer patients (n= 122) was 4.08 ± 0.74. Compared with the score for individuals in the community, that score was half a standard deviation lower. Carlson and Brown 31 examined the psychometric characteristics of the maas with cancer patients and found that it was valid, with a single factor structure.
2.6. Statistical Analyses
To determine whether changes in the outcome and process variables were statistically significant pre–post mbsr, paired-sample t-tests were performed. To assess the relative magnitude of the treatment effect for each outcome and process variable, effect sizes were calculated; for effect sizes, values of Cohen’s d of 0.5 to 0.8 are considered to be medium, and values over 0.8 are considered to be large 19. To calculate the Cohen’s d effect size, the pre-mbsr mean was subtracted from the post-mbsr mean and divided by the pooled standard deviation of that variable. Next, correlation coefficients were computed to examine the associations between maas change scores and the remaining mbsr process and outcome change scores. Finally, we used a hierarchical regression that controlled for the effects of age and time since completion of treatment to predict the main outcome (pss change score) using 2 process variables. Thus, the pss change scores were first regressed on age and time since completion of treatment in Block 1, and then on the maas change score and the soc total change score in Block 2. All statistical analyses were performed using the SPSS software package (version 11.0: SPSS, Chicago, IL, U.S.A.).
3. RESULTS
3.1. Participants
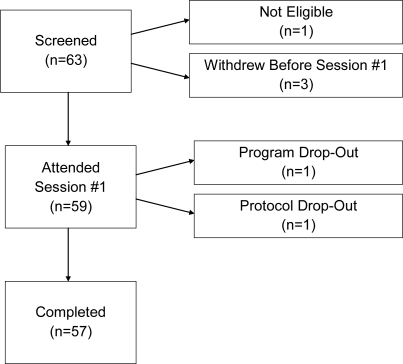
Figure 1 shows the participant flow. A total of 63 women provided written consent to enrol in the study and completed the screening interview. One woman failed to meet the eligibility criteria, and 3 withdrew (citing lack of time or scheduling conflicts) before the program commenced; thus, 59 women began the program. One woman dropped out after the 6th mbsr session, but returned to provide post-mbsr data (Program Drop-Out). Another woman dropped out of the study after the 2nd session and did not return, thus failing to provide post-mbsr data (Protocol Drop-Out).
Figure 1.
Participant recruitment and attendance. Program drop-out: One woman dropped out of the Mindfulness-Based Stress Reduction (mbsr) program but returned to provide post-mbsr data. Protocol drop-out: One woman dropped out of the study and did not return, thus failing to provide post-mbsr data.
Table i shows the participant demographics. Average age was 56.4 ± 10.2 years (range: 28–79 years). All had a high school education or above, and most women had presented with early-stage breast cancer (39/59, 66.1%). In 12 women (20.3%), cancer stage was unknown either because they did not know the stage (n = 5) or because they could not be reached after completion of the study for that information (n = 7). Time since completion of breast cancer treatment was, on average, 28.9 ± 58.8 months (range: 2–340 months).
TABLE I.
Participant (n = 59) demographics
| Variable | Value |
|---|---|
| Age (years) | |
| Mean | 56.4±10.2 |
| Range | 28–79 |
| Time since completion of breast cancer treatment (months) | |
| Mean | 28.9±58.8 |
| Range | 2–340 |
| Years of education [n (%)] | |
| High school leaving | 7 (11.9) |
| College degree | 13 (22.8) |
| Undergraduate degree | 26 (44.1) |
| Master’s degree | 9 (15.3) |
| Doctorate | 4 (6.8) |
| Cancer stage [n (%)] | |
| Stage 0 | 2 (3.4) |
| Stage 1 | 17 (28.8), |
| Stage 2 | 20 (33.9). |
| Stage 3 | 2 (3.4) |
| Stage 4 | 6 (10.2) |
| Unknown | 12 (20.3) |
3.2. Attendance
The average number of mbsr classes attended was 8.2 ± 1.13 (of 9); attendance was 90.9%. The mean number of hours attended was 23.84 ± 3.25 (of 26 hours in total).
3.3. Changes in Outcome and Process Variables Pre–Post MBSR
As seen in Table ii, differences in scores reached statistical significance for most variables. Some outcome measures showed significant change (decrease) after correction for multiple testing (Bonferroni correction with α= 0.05 and 12 tests yielded a corrected p = 0.0042): depressive symptoms (p < 0.0001), perceived stress (p < 0.0001), and medical symptoms (p < 0.0001). Significant changes were also found in the process measures of distraction coping (increased, p < 0.001); emotional coping (decreased, p < 0.0001); and mindfulness, comprehensibility, meaningfulness, and total sense of coherence (all increased, all p < 0.0001).
TABLE II.
Impact of the Mindfulness-Based Stress Reduction program on outcome and process measures (n = 57)
| Variable | Mean score | Difference | d Value | t Value | p Value | |
|---|---|---|---|---|---|---|
| Pre-program | Post-program Value | |||||
| Outcome measures | ||||||
| Depression | 16.30±9.91 | 10.26±7.56 | 6.04 | 0.57 | 4.25 | 0.0001 |
| Perceived stress | 17.95±6.05 | 14.07±6.17 | 3.88 | 0.64 | 4.83 | 0.0001 |
| Medical symptoms | 19.77±12.08 | 11.96±7.99 | 7.80 | 0.77 | 5.46 | 0.0001 |
| Process measures | ||||||
| Mindful awareness | 3.91±0.82 | 4.35±0.68 | 0.44 | –0.77 | –5.59 | 0.0001 |
| Distraction coping | 26.23±5.49 | 28.25±5.75 | 2.02 | –0.47 | –3.51 | 0.001 |
| Palliative coping | 23.72±4.39 | 24.25±3.94 | 0.53 | –0.14 | –1.08 | 0.286 |
| Instrumental coping | 33.68±5.07 | 33.21±5.67 | 0.47 | 0.13 | 1.00 | 0.320 |
| Emotional coping | 22.91±7.07 | 19.84±6.66 | 3.07 | 0.54 | 4.07 | 0.0001 |
| Comprehensibility | 42.74±8.89 | 46.67±6.80 | 3.93 | –0.54 | –3.96 | 0.0001 |
| Manageability | 47.89±7.80 | 49.67±6.19 | 1.77 | –0.27 | –1.96 | 0.055 |
| Meaningfulness | 42.93±7.32 | 46.18±6.72 | 3.25 | –0.62 | –4.62 | 0.0001 |
| Sense of coherence (total) | 133.56±19.61 | 142.51±15.08 | 8.95 | –0.52 | –4.51 | 0.0001 |
Bonferroni correction= α/n, where α= 0.05 and n= number of tests (12) = 0.00417.
Correlation coefficients were computed to examine the associations between maas change scores and the changes in process and outcome variable from pre- to post-mbsr. Using the Bonferroni approach to control for type 1 error across the 36 correlations, a p value of less than 0.0014 was required for significance.
The results of the correlation analyses revealed several statistically significant correlations (see Table iii). Most notably, increases in mindfulness scores were related to reductions in stress (p < 0.0001), depression (p < 0.0001), and emotional coping (p < 0.0001) and to increases in total sense of coherence (p < 0.0001).
TABLE III.
Correlations between change in mindfulness and change in other Mindfulness-Based Stress Reduction outcome and process measures
| Variables | Mindful awareness | Depression | Perceived stress | Medical symptoms | Distraction coping | Palliative coping | Instrumental coping | Emotional coping | Sense of coherence (total) |
|---|---|---|---|---|---|---|---|---|---|
| Depression | –0.517a | — | 0.712a | 0.616a | –0.345 | –0.057 | –0.134 | 0.419b | –0.683a |
| Perceived stress | –0.514a | 0.712a | — | 0.569a | –0.429b | –0.084 | –0.256 | 0.411b | –0.635a |
| Medical symptoms | –0.273 | 0.616a | 0.569a | — | –0.422b | 0.032 | –0.069 | 0.434b | –0.561a |
| Distraction coping | 0.287 | –0.345 | –0.429b | –0.422b | — | 0.104 | 0.161 | –0.419b | 0.567a |
| Palliative coping | 0.141 | –0.057 | –0.084 | 0.032 | 0.104 | — | 0.265 | 0.081 | 0.035 |
| Instrumental coping | 0.210 | –0.134 | –0.256 | –0.069 | 0.161 | 0.265 | — | –0.047 | 0.144 |
| Emotional coping | –0.506a | 0.419b | 0.411b | 0.434b | –0.419b | 0.081 | –0.047 | — | –0.517a |
| Sense of coherence (total score) | 0.541a | –0.683a | –0.635a | –0.561a | 0.567a | 0.035 | 0.144 | –0.517a | — |
p < 0.0001.
p < 0.001.
Bonferroni correction= α /n, where α= 0.05 and n= number of tests (36) = 0.0014.
Hierarchical regression was then performed to predict the main outcome (pss change score) using 2 process variables. As shown in Table iv, the results of the hierarchical linear regression analyses, with age and time since completion of treatment forced into the model as covariates, revealed that neither of these potential confounders predicted a reduction in stress F2,56 = 0.814, p = 0.449. However, when, in the next step, the model included the maas change score and the soc total change score, the model reached significance, accounting for 43.7% of the adjusted variance in the prediction of the change in stress: F4,56 = 11.858, p < 0.0001.
TABLE IV.
Hierarchical regression analysis results for Perceived Stress Scale–10 change score
| R | R2 | Adjusted R2 | Sum of squares | F Change | Significance F Change | df | Mean square | F | |
|---|---|---|---|---|---|---|---|---|---|
| Regressiona | 0.171 | 0.029 | –0.007 | 60.158 | 0.814 | 0.449 | 2 | 30.079 | 0.814 |
| Residual | 1995.983 | 54 | 36.963 | ||||||
| Total | 2056.140 | 56 | |||||||
| Regressionb | 0.691 | 0.477 | 0.437 | 980.833 | 22.261 | 0.000 | 4 | 245.208 | 11.858c |
| Residual | 1075.307 | 54 | 20.679 | ||||||
| Total | 2056.140 | 56 |
Predictors: time since completion of breast cancer treatment, age.
Predictors: time since completion of breast cancer treatment, age, sense of coherence total change score Mindfulness-Based Stress Reduction (mbsr), Mindful Attention Awareness Scale (mbsr) change score.
p < 0.001.
4. DISCUSSION
As occurred in studies pertaining to the benefits of mbsr for patients with other types of chronic illness 32, we found that the women in our study experienced reductions in stress, depression, and medical symptoms. With regard to perceived stress, their scores were above and below the norm pre- and post-mbsr respectively. Lengacher et al. 7 used the same stress measure and found that breast cancer patients randomized to a mbsr program who completed more meditation practice had larger reductions in perceived stress than did those who practiced less. In the present study, the group mean for depressive symptoms were at the “cut-off for case status” pre-mbsr and were below that level post-mbsr. As in other reports 24, medical symptoms were reduced.
With regard to process variables, mindfulness increased significantly from pre- to post-mbsr. That finding differs from the findings of Brown and Ryan 29 and Witek–Janusek et al. 33 who failed to find changes over time using the same questionnaire. Be that as it may, Carlson and Brown 31 reported that higher levels of mindfulness were related to lower levels of mood disturbance and stress both before and after mbsr in 122 cancer outpatients. [We examined correlations for mindfulness with depression and stress pre–post mbsr and found the same result (data not shown).] Notably, increased mindfulness was one of the predictors of reductions in stress.
Sense of coherence (total soc score) increased significantly over time. Only one other group, Shapiro et al. 34, used this measure in an investigation of mbsr with breast cancer patients. In their randomized clinical trial with repeated measures taken at baseline, 1 week, 3 and 9 months post mbsr, no changes were evident. However, Weissbecker et al. 35 reported significant increases in sense of coherence in a randomized clinical trial of mbsr for patients with fibromyalgia, a chronic pain condition. Their means for the total soc score pre- and post-mbsr were similar to ours [pre-mbsr: 130.51 in the treatment group, 132.42 in the control group for patients with fibromyalgia (Weissbecker), and 133.56 in our group; post-mbsr: 139.54 in the treatment group, 130.08 in the control group for patients with fibromyalgia (Weissbecker), and 142.51 in our group]. Furthermore, Weissbecker et al. 35 found a positive, significant association between meditation practice and sense of coherence.
Antonovsky 27 purported that sense of coherence is a stable disposition, but that notion has been challenged 36,37. Indeed, major life stressors, such as diagnosis and treatment of cancer, could be events that affect a person’s views about life meaning, for better or for worse. The mbsr, program designed to help patients reduce stress and cope better with illness, has the potential to affect soc by enabling patients to reappraise stressors, to acquire adaptive coping skills, and to find meaning through the experience of having cancer. Antonovsky 27 purports that individuals with high soc scores are more flexible when stressful events occur—they are more aware of their emotions and feel less threatened by them. The fact that an increase in total sense of coherence predicts reductions in stress supports this idea. Furthermore, individuals with a high sense of coherence manage tension better, which can positively affect their health status 27. This hypothesis is supported by the reductions in medical symptoms found in the present study (as well as by the significant correlation between changes in soc scores and changes in medical symptoms) and the reductions in stress-related symptoms consistently reported by the Carlson group in Calgary.
Garland 38 published a theoretical article about how mindfulness may lead to stress reduction. Our data fit with the notion that being mindful enables a “reappraisal” of stressors (for example, seeing illness as an opportunity for growth rather than as a threat) and inhibits the use of maladaptive coping strategies (for example, worry). Garland called this process “decentering,” which is defined as the capacity to observe thoughts and feelings without identifying with them. Depressed patients have been shown to increase their capacity to “decenter” from “depressogenic” thoughts after Cognitive–Behaviour Therapy and after Mindfulness-Based Cognitive Therapy 39,40, a variant of mbsr designed for patients with a history of recurrent depression. The significant post-mbsr reductions in depressive symptoms found in the present study are consistent with the findings of others. In fact, a score of more than 15 was seen in 26.3% of our cohort post-mbsr as compared with 45.6% pre-mbsr.
In line with the notion that mbsr helps patients to cope better with illness, distraction and emotional coping were the two coping styles that changed significantly.
The distraction score measures engagement in activities that prevent the mind from dwelling on illness (that is, avoidance is not measured per se). Thus, program participants had more opportunity to engage in other meaningful aspects of life. More engagement does not mean that they “forgot about it all” (that is, the cancer experience); rather, the change in score reflected a change toward being a person rather than a patient and not allowing illness to intrude on life.
The emotional coping score measures rumination about illness and feeling overwhelmed by symptoms or the aftermath of treatments. Mindfulness meditation encourages people to let go of those preoccupations by seeing the impermanent nature of internal (thoughts, feelings, bodily sensations) and external events (treatment starts, treatment ends). The mbsr program teaches patients to respond rather than to react to events in the present moment. For example, if a person feels pain, breath can be used to help relax muscles. The practice of yoga can be used to regain strength and stamina and to accept the body as it is now. A body scan can be used to relieve insomnia 34 (a common problem after cancer treatment). In line with this reasoning, Grossman et al. 41 found that women with fibromyalgia were better able to cope with pain both immediately after mbsr and 3 years later. The significant correlation found between increases in mindfulness and decreases in emotional coping suggest that these two processes were helpful for the women in our study, at least in the short term.
Only a few other studies of mbsr have included a measure of coping. Tacon et al. 42 used the Problem-Focused Styles of Coping questionnaire and found significant reductions in reactive and suppressive coping in 30 women with breast cancer. Witek–Janusek et al. 33 administered the Jalowiec Coping Scale, which measures the use and efficacy of various coping behaviours. Effectiveness of 2 of 8 subscales, “optimistic” (that is, positive outlook) and “supportant” coping (that is, use of support systems) were significantly higher in women randomized to the mbsr group than in women randomized to the control group. However, that measure is not as specific to coping with illness as the one we used is.
Thus, although the design of the present study does not allow for a conclusion that the positive effects are directly attributable to participation in mbsr, our results are similar to those from randomized clinical trials that can make that claim 7,11. Sample size restricted the number of variables that we could enter into the regression analyses, and thus we entered only those variables that, theoretically, were the logical choice. Moreover, we were cognizant of the interrelationship between variables and took those interrelationships into account in the selection of variables for the regression analysis. Other limitations of the present study include its lack of a control group and long-term follow-up, and the narrow range of participants (for the most part, highly educated Caucasian women), both of which affect external validity.
It appears that people who are open to this type of program, with mindful meditation as a main component, can learn how to cope better with stress and the aftermath of illness. Thus, in breast cancer patients discharged from medical treatment, mbsr may fill a health service gap, possibly allowing these patients to learn to navigate and stay afloat in what may seem to be the large and small waves of their transformed lives.
5. ACKNOWLEDGMENTS
The authors acknowledge the support provided to Dr. Patricia Dobkin by the Jewish General Hospital, the Segal Cancer Centre, and the Weekend to End Breast Cancer. Dr. Rose Matousek acknowledges support from the Strategic Training Program in Palliative Care Research of the Canadian Institutes of Health Research and the National Cancer Institute of Canada. The authors also thank Ms. Nancy Gair and Ms. Eileen Lavery for their devotion to the patients’ well-being and their tireless “behind the scenes” organization of program logistics.
6. REFERENCES
- 1.Arnold EM. The cessation of cancer treatment as a crisis. Soc Work Health Care. 1999;29:21–38. doi: 10.1300/J010v29n02_02. [DOI] [PubMed] [Google Scholar]
- 2.Cappiello M, Cunningham RS, Knobf MT, Erdos D. Breast cancer survivors: information and support after treatment. Clin Nurs Res. 2007;16:278–93. doi: 10.1177/1054773807306553. [DOI] [PubMed] [Google Scholar]
- 3.Lethborg CE, Kissane D, Burns WI, Snyder R. “Cast adrift”: the experience of completing treatment among women with early stage breast cancer. J Psychosoc Oncol. 2000;18:73–90. [Google Scholar]
- 4.Ashbury FD, Findlay H, Reynolds B, McKerracher K. A Canadian survey of cancer patients’ experience: are their needs being met? J Pain Symptom Manage. 1998;16:298–306. doi: 10.1016/s0885-3924(98)00102-x. [DOI] [PubMed] [Google Scholar]
- 5.Kabat–Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain and Illness. New York: Delacorte Press; 1990. [Google Scholar]
- 6.Ott MJ, Norris RL, Bauer–Wu SM. Mindfulness meditation for oncology patients: a discussion and critical review. Integr Cancer Ther. 2006;5:98–108. doi: 10.1177/1534735406288083. [DOI] [PubMed] [Google Scholar]
- 7.Lengacher CA, Johnson–Mallar V, Post–White J, et al. Randomized controlled trial of mindfulness-based stress reduction (mbsr) for survivors of breast cancer. Psychooncology. 2009;18:1261–72. doi: 10.1002/pon.1529. [DOI] [PubMed] [Google Scholar]
- 8.Smith JE, Richardson J, Hoffman C, Pilkington K. Mindfulness-based stress reduction as supportive therapy in cancer care: systematic review. J Adv Nurs. 2005;52:315–27. doi: 10.1111/j.1365-2648.2005.03592.x. [DOI] [PubMed] [Google Scholar]
- 9.Matchim Y, Armer JM. Measuring the psychological impact of mindfulness meditation on health among patients with cancer: a literature review. Oncol Nurs Forum. 2007;34:1059–66. doi: 10.1188/07.ONF.1059-1066. [DOI] [PubMed] [Google Scholar]
- 10.Mackenzie MJ, Carlson LE, Speca M. Mindfulness-based stress reduction (mbsr) in oncology: rationale and review. Evid Based Integr Med. 2005;2:139–45. [Google Scholar]
- 11.Speca M, Carlson LE, Goodey E, Angen M. A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med. 2000;62:613–22. doi: 10.1097/00006842-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Carlson LE, Speca M, Patel KT, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med. 2003;65:571–81. doi: 10.1097/01.psy.0000074003.35911.41. [DOI] [PubMed] [Google Scholar]
- 13.Garland SN, Carlson LE, Cook S, Lansdell L, Speca M. A non-randomized comparison of Mindfulness-Based Stress Reduction and healing arts programs for facilitating post-traumatic growth and spirituality in cancer outpatients. Support Care Cancer. 2007;15:949–61. doi: 10.1007/s00520-007-0280-5. [DOI] [PubMed] [Google Scholar]
- 14.Mackenzie MJ, Carlson LE, Munoz M, Speca M. A qualitative study of self-perceived effects of Mindfulness-Based Stress Reduction (mbsr) in a psychosocial oncology setting. Stress Health. 2007;23:59–69. [Google Scholar]
- 15.Shapiro SL, Oman D, Thoresen CE, Plante TG, Flinders T. Cultivating mindfulness: effects on well-being. J Clin Psychol. 2008;64:840–62. doi: 10.1002/jclp.20491. [DOI] [PubMed] [Google Scholar]
- 16.Jain S, Shapiro SL, Swanick S, et al. A randomized controlled trial of Mindfulness Meditation versus Relaxation Training: effects on distress, positive states of mind, rumination, and distraction. Ann Behav Med. 2007;33:11–21. doi: 10.1207/s15324796abm3301_2. [DOI] [PubMed] [Google Scholar]
- 17.Dobkin PL. Fostering healing through mindfulness in the context of medical practice. Curr Oncol. 2009;16:4–6. doi: 10.3747/co.v16i2.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dobkin PL. Mindfulness-Based Stress Reduction: what processes are at work? Complement Ther Clin Pract. 2008;14:8–16. doi: 10.1016/j.ctcp.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Cohen J. Statistical Power Analysis for the Behavioural Sciences. Hillsdale, NY: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 20.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 21.Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Thousand Oaks, CA: Sage Publications; 1988. pp. 31–7. [Google Scholar]
- 22.Radloff LS. The ces-d scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 23.Carmody J, Reed G, Kristeller J, Merriam P. Mindfulness, spirituality, and health-related symptoms. J Psychosom Res. 2008;64:393–403. doi: 10.1016/j.jpsychores.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 24.Reibel DK, Jeffrey M, Greeson MS, Brainard GC, Rosenzweig S. Mindfulness-Based Stress Reduction and health related quality of life in a heterogeneous patient population. Gen Hosp Psychiatry. 2001;23:183–92. doi: 10.1016/s0163-8343(01)00149-9. [DOI] [PubMed] [Google Scholar]
- 25.Endler NS, Parker JDA. Coping with Health Injuries Problems (chip). Toronto: Multi-Health Systems; 1992. [Google Scholar]
- 26.Endler NS, Courbasson L, Fillion L. Coping with cancer: the evidence for the temporal stability of the French-Canadian version of the Coping with Health Injuries and Problems. Pers Individ Dif. 1998;25:711–17. [Google Scholar]
- 27.Antonovsky A. Unraveling the Mystery of Health. How People Manage Stress and Stay Well. San Francisco: Jossey–Bass; 1987. [Google Scholar]
- 28.Eriksson M, Lindström B. Validity of Antonovsky’s Sense of Coherence Scale—a systematic review. J Epidemiol Community Health. 2005;59:460–6. doi: 10.1136/jech.2003.018085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown K, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–48. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 30.Brown KW, Kasser T. Are psychological and ecological well-being compatible? The role of values, mindfulness, and lifestyle. Soc Indic Res. 2005;74:349–68. [Google Scholar]
- 31.Carlson LE, Brown KW. Validation of the Mindful Attention Awareness Scale in a cancer population. J Psychosom Res. 2005;58:29–33. doi: 10.1016/j.jpsychores.2004.04.366. [DOI] [PubMed] [Google Scholar]
- 32.Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. 2008;31:23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- 33.Witek–Janusek L, Alburquerque K, Chroniak KR, Chroniak C, Durazo–Arvizu R, Mathews HL. Effect of Mindfulness-Based Stress Reduction on immune function, quality of life and coping in women newly diagnosed with early stage breast cancer. Brain Behav Immun. 2008;22:969–81. doi: 10.1016/j.bbi.2008.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shapiro SL, Bootzin RR, Figueredo AJ, Lopez AM, Schwartz GE. The efficacy of Mindfulness-Based Stress Reduction in the treatment of sleep disturbance in women with breast cancer: an exploratory study. J Psychosom Res. 2003;54:85–91. doi: 10.1016/s0022-3999(02)00546-9. [DOI] [PubMed] [Google Scholar]
- 35.Weissbecker I, Salmon P, Studts JL, Floyd AR, Dedert EA, Sephton SE. Mindfulness-Based Stress Reduction and sense of coherence among women with fibromyalgia. J Clin Psychol Med Settings. 2002;9:297–307. [Google Scholar]
- 36.Geyer S. Some conceptual considerations on the sense of coherence. Soc Sci Med. 1997;44:1771–9. doi: 10.1016/s0277-9536(96)00286-9. [DOI] [PubMed] [Google Scholar]
- 37.Schneider U, Büchi S, Sensky T, Klaghofer R. Antonovsky’s sense of coherence: trait or state? Psychother Psychosom. 2000;69:296–302. doi: 10.1159/000012411. [DOI] [PubMed] [Google Scholar]
- 38.Garland EL. The meaning of mindfulness: a second-order cybernetics of stress, metacognition, and coping. Complement Health Pract Rev. 2007;12:15–30. [Google Scholar]
- 39.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression. New York: The Guilford Press; 2002. [Google Scholar]
- 40.Fresco DM, Segal ZV, Buis T, Kennedy S. Relationship of posttreatment decentering and cognitive reactivity to relapse in major depression. J Consult Clin Psychol. 2007;75:447–55. doi: 10.1037/0022-006X.75.3.447. [DOI] [PubMed] [Google Scholar]
- 41.Grossman P, Tiefenthaler–Gilmer U, Raysz A, Kesper U. Mindfulness training as an intervention for fibromyalgia: evidence of postintervention and 3-year follow-up benefits in well-being. Psychother Psychosom. 2007;76:226–33. doi: 10.1159/000101501. [DOI] [PubMed] [Google Scholar]
- 42.Tacon AM, Caldera YM, Ronaghan C. Mindfulness, psychosocial factors, and breast cancer. J Cancer Pain Symptom Palliation. 2005;1:45–53. [Google Scholar]