Abstract
Objective
Using an interview-guided survey, our descriptive study aimed to document the extent to which cancer patients perceive they are involved in making treatment decisions and the factors that influence patient involvement.
Patients and methods
Our study enrolled patients from a Canadian ambulatory oncology program who were undergoing chemotherapy or radiation therapy, or both, for cancer. The adapted Control Preferences Scale was used to survey perceived and preferred roles in decision-making. The study survey also included items from the Decisional Conflict Scale and the Preparation for Decision-Making Scale.
Results
Of 192 participants, 98 (51%) perceived that they were offered treatment choices. Of those 98, 47 (48%) thought that the options were presented equally. Compared with the patients not offered choices, those who were given choices were less passive (4% vs. 29%, p < 0.001) and more satisfied (100% vs. 95%, p < 0.03) in decision-making. Participants whose preferred and perceived roles were different would have preferred more involvement in decision-making. To attain the preferred involvement, patients wanted to receive more information on treatment options, to be given a choice, to have more discussion with the health care team, and to have providers better listen to their needs.
Conclusions
Only half of surveyed patients thought that they were offered choices for their cancer treatment. When offered choices, patients were more active in decision-making. Further initiatives are required to determine approaches for supporting patients with cancer so that they can be more involved in decision-making.
Keywords: Cancer, shared decision-making, preferences, decision quality, role in decision-making
1. INTRODUCTION
People facing serious illnesses such as cancer have a great stake in the decision-making process. Cancer treatments can result in toxicity, changes in body image, and lifestyle disruptions; cancer screening has the potential for psychological distress, particularly with false positive results 1. These potential outcomes are likely to be valued differently by different patients, and guidelines for patient-centred care require that clinical decisions be based on the preferences and values of patients with regard to the outcomes of options 2,3.
Given the need to weigh benefits, harms, and inconveniences across options, patients are likely to experience personal uncertainty about the best option and to require support to participate in decision-making. Personal uncertainty, also called “decisional conflict,” is more prevalent when patients are uninformed, have unclear values, and do not feel adequately supported 4. The extent to which patients are involved in decision-making in ways they prefer and the manner in which they resolve their personal uncertainty are unclear.
The constituents of an ideal level of patient participation are not obvious. Studies have found that an independent or shared role in decision-making is preferred by more than 90% of people in good health and of men newly diagnosed with prostate cancer 1,5–7, but by only 64% of patients with breast cancer 8. Furthermore “risk communication and involvement in treatment decisions” is described as 1 of 6 key indicators of patient engagement in health care 9. However, despite the desires of patients to be more actively involved, patients are not necessarily engaged in making decisions about treatment.
As part of a multi-country comparison, just over half of 1410 healthy Canadians and 751 with health problems (for example, recent hospitalization, surgery, other major health problems) reported being exposed to health care professionals who involved them in treatment choices (62% healthy, 56% with health problems) or having treatment risks explained clearly to them (57% with health problems) 9. Findings for Canadians with health problems were similar to those for people with health problems in Australia, New Zealand, Germany, the United Kingdom, and the United States.
A review of 22 studies, mostly with cancer patients, found that 34%–80% of the patients (median: 60%) experienced a level of decision-making that matched their preferred level; when mismatches occurred, the patients had typically wanted a role that was more active 10. Furthermore, when the preferred and perceived levels of involvement matched, patients were more satisfied and less depressed; mismatches resulted in poorer outcomes for the patients (for example, depression, fatigue, less satisfaction, anxiousness after consultation) 10. Few patients are asked their desired level of involvement, however. A study by Elwyn and colleagues 11 found that the primary care physician asked the patient about preferred involvement during only 2.1% of 186 consults.
Two studies found that patients do better when they are actively engaged in the decision-making process about cancer screening or treatment 12,13. Canadian women actively involved in making the decision about breast cancer treatment had a higher quality of life, better health outcomes, and less fatigue 2 years later than did women passive in decision-making 12. An Australian study of cancer patients found that, regardless of the match in preferred and perceived roles, patients who shared in the decision were more satisfied with the consultation, treatment information, and emotional support received 13.
Shared decision-making and decision aids for patients are interventions that can engage patients in decision-making. Shared decision-making is the process by which health care choices are made by practitioners together with the patient 14–17. In a review of 161 conceptual definitions of shared decision-making, the essential elements (consistent across prominently cited models of shared decision-making) are these 17:
Define the problem
Present options
Discuss pros and cons, patient values and preferences
Discuss patient ability, doctor knowledge
Check/clarify understanding
Make (or explicitly defer) the decision
Arrange for follow-up
Decision aids for patients are evidence-based tools that, at a minimum, provide information on options and their benefits and harms, and that implicitly help patients to clarify their values associated with the outcomes of options 18. In a systematic review of 23 trials evaluating decision aids for patients making cancer decisions, the authors found that, in addition to improved knowledge, realigned expectations, and values clarification, participation increased 50% in patients exposed to a decision aid 19. Being explicit about the options is therefore a fundamental aspect of engaging patient participation in decision-making. Although interventions to improve patient engagement in decision-making are available, few are routinely used in clinical practice, and several studies have identified barriers to their use 20.
The objectives of the present study were to determine whether patients perceived that they were involved in making the decision about their current treatment, and to identify factors influencing their involvement in treatment decision-making. The Ottawa Decision Support Framework was used for these purposes.
2. PATIENTS AND METHODS
2.1. Study Design
This descriptive study, which received approval from the research ethics board at The Ottawa Hospital (#2007105-01H), used an interviewer-guided survey based on the Ottawa Decision Support Framework 21. The Ottawa Framework asserts that decision-making can be adversely affected by factors such as
decisional conflict;
inadequate knowledge of options and unrealistic expectations of benefits and harms;
unclear values associated with the outcomes of options;
inadequate support or resources (for instance, pressure to choose an option, unclear perception of personal role in decision-making);
complex decision type (for example, needing to weigh benefits and harms across options);
urgent timing (within minutes or hours, for instance); and
participant characteristics (for example, age, cognitive limitations, limited education).
People whose decisional needs are unresolved are more likely to delay decisions, to feel regret, to express dissatisfaction, and to blame the practitioner for poor outcomes 22,a.
2.2. Participants and Setting
Patients diagnosed with cancer and receiving radiation or chemotherapy (or both) at a large ambulatory cancer program were invited to participate. Patients were ineligible if they did not have a cancer diagnosis, if they were unable to respond to the survey questions, and if they were not able to understand spoken English or French.
The ambulatory cancer program is located within a large academic hospital serving a general population of about 1.3 million. The program offers chemotherapy, radiation therapy, and consultation by oncology specialists. At the time of the study, 250–300 patients were receiving radiation therapy and 200–300 were receiving chemotherapy each week. For patients who were receiving radiation therapy, treatment was usually scheduled every day from Monday to Friday. For patients on chemotherapy, the number of treatment days in a given week depended on the treatment regimen.
2.3. Survey Procedure
Patients arriving for radiation therapy or chemotherapy were informed about the study by the receptionists. Interested patients were directed to a research assistant in the waiting area. After signing the study consent, participants were interviewed by a trained research assistant to complete the survey questions. Surveys took about 10 minutes to complete.
The survey was developed based on questions from instruments commonly used to evaluate the effect of interventions on patient involvement in health decisions. It was guided by the Ottawa Decision Support Framework and the Population Needs Assessment tool 21,23. Of 20 items in total, 11 were based on valid and reliable instruments relevant to shared decision-making (see “Outcome Measurement Tools,” next). Additionally, patients were asked if their doctor had talked with them about being able to choose between treatment options, whether the doctor had recommended one type of treatment over another or had presented the treatments as equal options, whether they as patients had had enough time to make the choice, whether they had been satisfied with the time available to discuss the decision with their doctor, and how much time had passed since the last decision was made. Finally, in an open-question format, participants were asked what would have helped them to be involved in the treatment decision to the level that they would have liked, and which individuals had been involved in the decision-making process. Demographic information was also collected.
The final survey was reviewed for face validity by experts in shared decision-making, patient teaching, and oncology, and it was pilot tested with 2 people who had either personally had cancer or who had experienced health decisions with a family member.
2.4. Outcome Measurement Tools
A modified version of the Control Preferences Scale was used to determine the perceived and preferred roles of the patients in decision-making 24. According to the Ottawa Decision Support Framework, the patient’s role in decision-making in relation to others is included within the key concept of support 21. In the Control Preferences Scale, participants choose from among five statements about the various roles that they prefer to assume when making a decision: patient alone, patient after considering doctor’s opinion, shared between patient and doctor, doctor after considering patients’ opinion, doctor alone. Face validity for the scale was established by researchers and cancer patients during instrument development, and the scale has been shown to be responsive to variations in health states 24.
The clinical version of the Decisional Conflict Scale was used. This 4-item scale measures the perception of the patient concerning feeling sure about the best option, being informed about options, having values clarity, and having support 4. Each item has a 3-point response of “no,” “unsure,” and “yes,” with “yes” answers indicating lower levels of decisional conflict. The test–retest and alpha coefficients for the original scale exceed 0.78, and the scale is known to be sensitive to change after exposure to decision support interventions 4,25.
Of 10 items on the Preparation for Decision Making scale, 4 were used to determine the perceptions of patients about support received as part of the process of decision-making: help in recognizing that a decision needs to be made, help with knowing the benefits and risks of each option, help with knowing that the decision depends on what matters most to the patient, and help with thinking about how involved the patient wants to be in the decision. Each item has a 5-point response (“not at all,” “a little,” “somewhat,” “quite a bit,” and “a great deal”), with higher scores indicating higher support in preparation for decision-making. This instrument has good internal consistency (>0.91). Item response theory analysis found that it has excellent item discrimination (range: 2.12–3.80). Also, it discriminates between patients who do and do not find a decision aid helpful 26.
2.5. Analysis
All data were entered into Microsoft Excel (Microsoft Corporation, Redmond, WA, U.S.A.) and transferred to SPSS for Windows (version 16.0: SPSS, Chicago, IL, U.S.A.). Data verification revealed errors (0.5%, 35/6720) that were corrected. Participants were classified according to whether they thought they had been able to choose between treatment options. Using this categorization, differences in involvement in decision-making, decisional conflict, preparation for decision-making, patient satisfaction, and demographic characteristics were compared. A Pearson chi-square test (or Fisher exact test, when appropriate) was used to compare selected characteristics between participants. The subscores of the Decisional Conflict Scale for certainty, being informed, values clarity, and support were compared using a stratified two-sample t-test. All reported p values are two-sided and were declared statistically significant when they reached a 0.05 probability level. Thematic content analysis was conducted for responses to open questions.
3. RESULTS
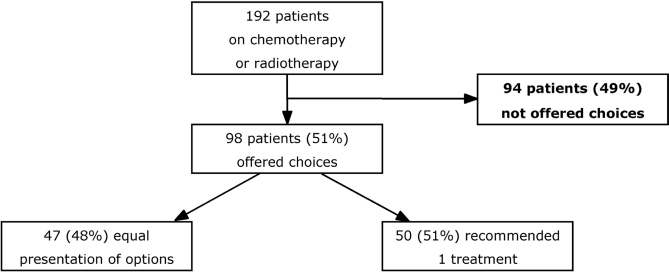
From mid-April to mid-May 2007, a nonrandomized convenience sample of 192 patients consented to participate and completed the survey. Of those 192 patients, 98 (51%) agreed that they had been offered treatment choices, and 94 (49%) perceived they had not been offered choices. Of the 98 offered choices, 47 (48%) thought that the options had been presented equally, and 50 (51%) indicated that one treatment option was recommended.
The typical participant was a mean of 59.6 years of age and English-speaking, had completed postsecondary education, was employed full time, and had been diagnosed with cancer within the preceding 6 months. On average, the time since the last treatment decision had been made was 3 months. Demographics were similar for participants who perceived that they were or were not offered choices (Table i).
TABLE I.
Demographic characteristics of participants
| Characteristic |
Offered choices |
|
|---|---|---|
| Yes | No | |
| Patients (n) | 98 | 94 |
| Age [n (%)] | ||
| 30–49 Years | 19 (19) | 23 (24) |
| 50–69 Years | 53 (54) | 49 (52) |
| 70–89 Years | 22 (22) | 22 (23) |
| Not reported | 4 (4) | 0 |
| Sex [n (%)] | ||
| Male | 40 (41) | 35 (37) |
| Female | 55 (56) | 59 (63) |
| Not reported | 3 (3) | 0 |
| Diagnosis [n (%)] | ||
| Breast | 47 (48) | 39 (41) |
| Prostate | 15 (15) | 10 (11) |
| Colon | 9 (9) | 8 (9) |
| Lung | 5 (5) | 12 (13) |
| Othera | 17 (17) | 23 (24) |
| Not reported | 5 (5) | 2 (2) |
| Months since diagnosis [n (%)] | ||
| <3 | 9 (9) | 17 (18) |
| <6 | 25 (26) | 14 (15) |
| <12 | 22 (22) | 24 (26) |
| >12 | 36 (37) | 36 (38) |
| Not reported | 6 (6) | 3 (3) |
| Spoken language [n (%)] | ||
| English | 74 (76) | 84 (89) |
| French | 13 (13) | 6 (6) |
| Bilingual | 8 (8) | 1 (1) |
| Other | 0 | 2 (2) |
| Not reported | 3 (3) | 1 (1) |
| Employment status | ||
| Full time | 42 (43) | 50 (53) |
| Retired | 32 (33) | 32 (34) |
| Part time | 8 (8) | 3 (3) |
| Other | 13 (13) | 8 (9) |
| Not reported | 3 (3) | 1 (1) |
| Education [n (%)] | ||
| <High school | 2 (2) | 8 (9) |
| High school | 38 (39) | 36 (38) |
| University | 22 (22) | 17 (18) |
| College/technical | 18 (18) | 22 (23) |
| Graduate | 14 (14) | 9 (10) |
| Not reported | 4 (4) | 2 (2) |
| Time since last decision [n (%)] | ||
| 1 Week | 8 (8) | 7 (7) |
| 1 Month | 23 (23) | 17 (18) |
| 3 Months | 25 (26) | 27 (29) |
| 6 Months | 16 (16) | 22 (23) |
| >6 Months | 24 (24) | 21 (22) |
| Not reported | 2 (2) | 0 |
Skin cancer, melanoma, rectal cancer, lymphoma, pancreatic cancer, esophageal cancer, stomach cancer, throat cancer, tongue cancer, brain cancer, liver cancer, uterine cancer, kidney cancer, endometrial cancer, testicular cancer, ovarian cancer, thyroid cancer, eye cancer, renal cell cancer.
3.1. Role in Decision-Making
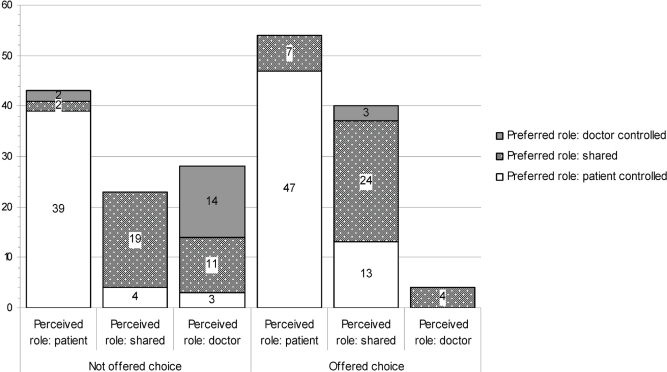
Compared with patients who perceived that they were not offered choices, patients who perceived they were offered choices indicated that they were more actively involved (55% vs. 44%), were more likely to share in decision-making (41% vs. 26%), and were less likely to defer the decision to their physician (4% vs. 29%, p < 0.001; see Table ii). Compared with the perceived level of involvement and whether a choice was perceived to have been offered, most patients would prefer to be more actively involved in subsequent decision-making (p< 0.001; see Figure 2). Of 98 participants who perceived being offered a choice, 53 involved their spouse in the treatment decision (54%), 26 involved family members (27%), 7 involved friends (7%), and 3 involved their family doctor (3%).
TABLE II.
Role of patients in decision-making
| Role |
Offered choices [n (%)] |
|||
|---|---|---|---|---|
|
Yes (N=98) |
No (N=94) |
|||
| Perceiveda | Preferredb | Perceiveda | Preferredb | |
| Patient-controlled | ||||
| Patient made decision | 9 (9) | 7 (7) | 12 (13) | 11 (12) |
| Patient made decision after seriously considering doctor’s opinion | 45 (46) | 53 (54) | 31 (33) | 35 (37) |
| Shared | ||||
| Patient and doctor shared responsibility for making the decision | 40 (41) | 35 (36) | 23 (24) | 32 (34) |
| Doctor-controlled | ||||
| Doctor made decision after seriously considering patients opinion | 1 (1) | 2 (2) | 10 (11) | 9 (10) |
| Doctor made decision | 3 (3) | 1 (1) | 18 (19) | 7 (7) |
p < 0.001.
p = 0.009.
Figure 2.
Comparison between the perceived and the preferred role of patients in decision-making.
3.2. Decisional Conflict
All four items from the Decisional Conflict Scale were similar in participants offered and not offered choices (see Table iii). Decisional conflict scores were not significantly different for patients who would have preferred to be more actively involved in decision-making [41/194 (21.1%)] and for those who achieved their preferred role in decision-making [129/194 (66.5%)].
TABLE III.
Decisional conflict with modifiable factors interfering with decision-making
| Items |
Offered choices |
|||||
|---|---|---|---|---|---|---|
|
Yes (N=98) |
No (N=94) |
|||||
| (n) | Scorea | Proportion | (n) | Scorea | Proportion | |
| Feel sure about the best choice | 97 | 89 | 91.7 | 90 | 82 | 91.1 |
| Know the benefits and harms of each option | 93 | 88 | 94.6 | 89 | 79 | 88.8 |
| Clear about which benefits or harms matter most | 96 | 88 | 91.7 | 88 | 78 | 88.6 |
| Enough support and advice to make a choice | 96 | 94 | 97.9 | 88 | 82 | 93.2 |
Responses are scored as follows: Yes= 1; Unsure= 0; No= 0. Scores of less than 1 indicate some difficulty: lack of knowledge, unclear values, and need for support.
3.3. Preparation for Decision-Making
We observed no statistically significant differences between participants offered and not offered treatment choices on their rating of preparation for decision-making. Both groups selected “quite a bit” or “a great deal” for the doctor’s role in preparation for a decision by helping them to recognize the decision (87.8% vs. 79.4%), to think about the benefits and risks (89.8% vs. 81.1%), to know that the decision depended on what matters most to them (86.5% vs. 73.5%), and to consider their own involvement in decision-making (85.4% vs. 74.6%). Of patients who were offered treatment choices, 93.7% (89/95) thought they were given the information necessary to help them make the decision; in group who had not been offered choices, that percentage was 84.4% (76/90). Of patients who were offered treatment choices, 99% (97/98) thought that they had been given enough time to make the choice; in the group that had not been offered choices, that percentage was 92% (84/91).
3.4. Satisfaction with Involvement in Decision-Making
All 98 patients offered choices (100%) were satisfied with their level of involvement in decision-making, as compared with 86 of the 91 patients (94.5%) not offered choices (p < 0.03). Reasons for being less satisfied included not being given options, wanting to be more involved, having to do their own research to find information, and feeling that the physician was too overworked. When asked about their satisfaction with the amount of discussion with their doctor about the treatment, responses indicated that more discussion was needed to answer questions, that the quality of the discussion could be improved (for example, “have to learn how to make it a two-way conversation,” “doctor doesn’t initiate information... feel like need to pull it out”), and that more clarity was needed about whom questions were to be addressed to (for example, “when presented with three doctors... it’s hard to find the right person for the question”).
3.5. Helping Patients with Preferred Level of Involvement in Treatment Decisions
Qualitative findings revealed that, for participants to be involved in treatment decision-making to their desired level, they wanted to be offered a choice, to receive more information, to be helped to understand the information, and to be heard. For example, one patient said that it would be better if the “doctor gives opinions [and] facts; both make the decision.” Another patient said that nothing can be done “without doctor’s approval: rather be in situation where I can make decision rationally.” Others suggested that, to support decision-making, they needed more information on benefits and, in particular, on harms (for example, “knowing benefits of each treatment... [such as] best case/worst case, what’s the norm, know percentage-wise how sick people get,” “easy to say what benefits will be—wanted to know more about harms”). Given that some patients felt that the “information is overwhelming and extremely technical,” some would have liked to have more help in understanding the information. Finally, patients would prefer if the health care team listened to their needs and preferences, as demonstrated in comments such as “some acknowledgement of your ideas; validation of alternative treatments” and “ask about level of involvement prior to treatment.”
4. DISCUSSION
Our results confirm that there is a need to increase participation in the decision-making process for our cancer patients. Findings at this ambulatory oncology program indicate that only 50% of patients perceived being offered treatment choices. As well, patients wanted to have more involvement in the process of decision-making than they felt they were afforded. This result falls below the role preference expressed in the general public (>90%), in men with prostate cancer (92.5%), and in women with breast cancer (64%) 5,7,8,10. Furthermore, it brings into question whether the patients were exposed to known interventions (such as patient decision aids or practitioners skilled in shared decision-making) to enhance their level of involvement. Although more than 85% of all participants indicated that they thought they knew the benefits and harms, the general comments by respondents about the information provided revealed that only 3 described that information as including benefits and harms—another important element for decision-making 27. Finally, research is emerging to suggest that, regardless of preferred role, patients who are more engaged in decision-making have better outcomes 10.
Another component of informed consent (recognized within the International Patient Decision Aid Standards) is a “do nothing” option 27,28. Although some may argue that “do nothing” is not a viable option, understanding the consequences of not undergoing treatment for cancer may help some patients to come to agreement sooner with an active treatment option. Furthermore, a review of the clinical evidence for various treatments revealed that 11% of treatments had clear benefits that outweighed harms, and that most treatments required a weighing of benefits and harms 29.
To facilitate achievement of their preferred level of involvement in decision-making, respondents suggested that they needed more information and more help in understanding the information provided—two essential elements of shared decision-making 17. That finding highlights a mismatch between the perceptions of the patients about their most recent experience (for example, more than 80% felt that they were helped to know the benefits and risks of the options) and the preferences of those patients for support with subsequent decisions. Some respondents reported that their practitioner focused mostly on the benefits when they would have liked more information on the harms associated with the treatment options or on complementary or alternative therapy options. The definition of a quality decision includes being provided with the latest evidence and having realistic expectations of the potential outcomes (both the benefits and the harms) of the various treatment options 27,30. It is therefore unclear whether the treatment decision-making process was adequate for some patients.
Guidelines for client-centred care make explicit the importance of including patient preferences in the decision-making process and of supporting the participation of patients in decision-making (possibly facilitated by decision coaches) 2,3,31. However, research indicates that current practice among health professionals is inadequate and that these professionals need supportive environments that provide opportunities for them to further develop their knowledge and skills for supporting patient involvement in decision-making 11,20,32.
Perceived level of decisional conflict and feelings of preparedness for decision-making did not appear to differ significantly between patients offered and not offered choices. Both of those measures are often used within 2 weeks of exposure to an intervention designed to prepare the respondent for decision-making 4,26. However, in the present study, most patients had made the decision 3 or more months before the survey; they were therefore considering the decision retrospectively, and as a result, they may not have remembered how they felt about the decision or the decision-making process.
Our findings need to be interpreted within the limitations of a survey-based design that collected retrospective information from patients about their experiences of treatment decision-making.
First, there could be response or recall bias (or both): respondents who chose to participate might have been more interested in decision-making, or might have provided responses perceived to be “more acceptable.” In addition, some participants may have had difficulty recalling the requested information, given that there was significant variation in the time since the most recent decision had been made (range: 1 week to >6 months).
A second limitation unique to this study is the inclusion of patients with many different types of cancer and at varying stages in their disease trajectory. Future studies of the perceptions of patients concerning satisfaction with the support received in relation to their participation in treatment decision-making should focus on patients experiencing widely recognized “crossroads decisions”—for example, early-stage breast cancer or early-stage prostate cancer. Another potential limitation is the way in which responses were recorded: the research assistant wrote the responses from the patients on the survey tool. No audio-recording of the interviews was done. This approach limited the depth of the comments captured in the database, necessarily excluding a rich context in which to situate the comment.
Still, although our findings are limited to a single academic centre and to a population of somewhat younger participants (mean age of approximately 60 years as compared with the Canadian mean of 70 years for men with cancer 33), they are likely to be relevant to other health service organizations delivering ambulatory cancer care.
5. CONCLUSIONS
Despite surveys showing that patients want to be involved in making health decisions, only about 50% of patients on chemotherapy or radiation therapy perceived that they were offered treatment choices. Patients offered choices are more likely to take an active role in decision-making, to be more satisfied, and to prefer to be involved in subsequent health-related decisions. When preferred and perceived roles are mismatched, patients prefer more involvement in decision-making.
To support patients to be more involved in making decisions about cancer treatment, providers need to give those patients treatment options and more information on the benefits and risks of those options, to provide them with more time for discussion with the health care team, and to have the health care team better listen to their needs.
Figure 1.
Perception of patients concerning treatment choices.
6. ACKNOWLEDGMENTS
This study was funded by the Ottawa Regional Cancer Foundation. Mistral Pratt and radiation therapy students assisted in the data collection; Sarah Mullan assisted in drafting the manuscript.
Footnotes
O’Connor AM, Sun Q, Dodin S, et al. Predicting downstream effects of high decisional conflict. Presented at the Third International Shared Decision Making Conference; Ottawa, Ontario; June 14–16, 2005.
7. REFERENCES
- 1.Degner LF, Sloan JA. Decision making during serious illness: what role do patients really want to play? J Clin Epidemiol. 1992;45:941–50. doi: 10.1016/0895-4356(92)90110-9. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 3.Registered Nurses’ Association of Ontario (rnao) Client Centred Care Nursing Best Practice Guideline. Toronto: RNAO; 2006. pp. 1–8. [Google Scholar]
- 4.O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 5.Magee M. Relationship-Based Health Care in the United States, United Kingdom, Canada, Germany, South Africa, and Japan. A Comparative Study of Patient and Physician Perceptions Worldwide. Ferney–Voltaire, France: World Medical Association; 2003. [Available online at: www.wma.net/en/40news/20archives/2003/2003_15/2003_15.pdf; cited June 10, 2010] [Google Scholar]
- 6.O’Connor AM, Drake ER, Wells GA, Tugwell P, Laupacis A, Elmslie T. A survey of the decision-making needs of Canadians faced with complex health decisions. Health Expect. 2003;6:97–109. doi: 10.1046/j.1369-6513.2003.00215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davison BJ, Gleave ME, Goldenberg SL, Degner LF, Hoffart D, Berkowitz J. Assessing information and decision preferences of men with prostate cancer and their partners. Cancer Nursing. 2002;25:42–9. doi: 10.1097/00002820-200202000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Degner LF, Kristjanson LJ, Bowman D, et al. Information needs and decisional preferences in women with breast cancer. JAMA. 1997;277:1485–92. [PubMed] [Google Scholar]
- 9.Coulter A. Engaging Patients in Their Healthcare: How Is the UK Doing Relative to Other Countries? Oxford, UK: Picker Institute Europe; 2006. [Google Scholar]
- 10.Kiesler DJ, Auerbach SM. Optimal matches of patient preferences for information, decision-making and interpersonal behaviour: evidence, models and interventions. Patient Educ Couns. 2006;61:319–41. doi: 10.1016/j.pec.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 11.Elwyn G, Hutchings H, Edwards A, et al. The option scale: measuring the extent that clinicians involve patients in decision-making tasks. Health Expect. 2005;8:34–42. doi: 10.1111/j.1369-7625.2004.00311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hack TF, Degner LF, Watson P, Sinha L. Do patients benefit from participating in medical decision making? Longitudinal follow-up of women with breast cancer. Psychooncology. 2006;15:9–19. doi: 10.1002/pon.907. [DOI] [PubMed] [Google Scholar]
- 13.Gattellari M, Butow PN, Tattersall MHN. Sharing decisions in cancer care. Soc Sci Med. 2001;52:1865–78. doi: 10.1016/s0277-9536(00)00303-8. [DOI] [PubMed] [Google Scholar]
- 14.Elwyn G, Edwards A, Kinnersley P, Grol R. Shared decision making and the concept of equipose: the competencies of involving patients in healthcare choices. Br J Gen Pract. 2000;50:892–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (Or it takes at least two to tango) Soc Sci Med. 1997;44:681–92. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 16.Towle A, Godolphin W. Framework for teaching and learning informed shared decision making. BMJ. 1999;319:766–71. doi: 10.1136/bmj.319.7212.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60:301–12. doi: 10.1016/j.pec.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 18.O’Connor AM, Bennett CL, Stacey D, et al. Cochrane Database Syst Rev. 2009. Decision aids for people facing health treatment or screening decisions; p. CD001431. [DOI] [PubMed] [Google Scholar]
- 19.Stacey D, Samant R, Bennett C. Decision making in oncology: a review of patient decision aids to support patient participation. CA Cancer J Clin. 2008;58:293–304. doi: 10.3322/CA.2008.0006. [DOI] [PubMed] [Google Scholar]
- 20.Legare F, Ratte S, Gravel K, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns. 2008;73:526–35. doi: 10.1016/j.pec.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 21.O’Connor AM, Tugwell P, Wells G, et al. A decision aid for women considering hormone therapy after menopause: decision support framework and evaluation. Patient Educ Couns. 1998;33:267–79. doi: 10.1016/s0738-3991(98)00026-3. [DOI] [PubMed] [Google Scholar]
- 22.Gattellari M, Ward JE. Men’s reactions to disclosed and undisclosed opportunistic psa screening for prostate cancer. Med J Aust. 2005;182:386–9. doi: 10.5694/j.1326-5377.2005.tb06756.x. [DOI] [PubMed] [Google Scholar]
- 23.Jacobsen MJ, O’Connor A. Population Needs Assessment: A Workbook for Assessing Patients’ and Practitioners’ Decision Making Needs. Ottawa, ON: Ottawa Hospital Research Institute; 2006. [Google Scholar]
- 24.Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. Can J Nurs Res. 1997;29:21–43. [PubMed] [Google Scholar]
- 25.O’Connor AM, Drake E, Fiset V, Graham I, Laupacis A, Tugwell P. The Ottawa patient decision aids. Eff Clin Pract. 1999;2:163–70. [PubMed] [Google Scholar]
- 26.Bennett C, Graham ID, Kristjansson E, Kearing SA, Clay KF, O’Connor AM. Validation of a preparation for decision making scale. Patient Educ Couns. 2010;78:130–3. doi: 10.1016/j.pec.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 27.Elwyn G, O’Connor A, Stacey D, et al. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ. 2006;333:417–22. doi: 10.1136/bmj.38926.629329.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ontario. Health Care Consent Act, 1996. Toronto, ON: Service Ontario, Queen’s Printer for Ontario; 2010. [Available online at: www.e-laws.gov.on.ca/html/statutes/english/elaws_statutes_96h02_e.htm; cited June 18, 2010] [Google Scholar]
- 29.BMJ Publishing Group, Clinical Evidence Web site Home > About Us> A Guide to the Text London, U.K: BMJ Publishing Group; 2003[Available online at: clinicalevidence.bmj.com/ceweb/about/knowledge.jsp;cited June 10, 2010] [Google Scholar]
- 30.Sepucha KR, Fowler FJ, Mulley AG., Jr Policy support for patient-centered care: the need for measurable improvements in decision quality. Health Aff (Millwood) 2004;(suppl):VAR 54–62. doi: 10.1377/hlthaff.var.54. [DOI] [PubMed] [Google Scholar]
- 31.Stacey D, Murray MA, Legare F, Dunn S, Menard P, O’Connor A. Decision coaching to support shared decision making: a framework, evidence, and implications for nursing practice, education, and policy. Worldviews Evid Based Nurs. 2008;5:25–35. doi: 10.1111/j.1741-6787.2007.00108.x. [DOI] [PubMed] [Google Scholar]
- 32.Guimond P, Bunn H, O’Connor AM, et al. Validation of a tool to assess health practitioners’ decision support and communication skills. Patient Educ Couns. 2003;50:235–45. doi: 10.1016/s0738-3991(03)00043-0. [DOI] [PubMed] [Google Scholar]
- 33.Canadian Cancer Society, Public Health Agency of Canada, and Statistics Canada . Canadian Cancer Statistics 2009. Toronto: Canadian Cancer Society; 2009. [Available online at: www.cancer.ca/Canada-wide/About%20cancer/Cancer%20statistics/~/media/CCS/Canada%20wide/Files%20List/English%20files%20heading/pdf%20not%20in%20publications%20section/Stats%202009E%20Cdn%20Cancer.ashx; cited June 18, 2010] [Google Scholar]