Abstract
A central component of Dialectical Behavior Therapy (DBT) is the teaching of specific behavioral skills with the aim of helping individuals with Borderline Personality Disorder (BPD) replace maladaptive behaviors with skillful behavior. Although existing evidence indirectly supports this proposed mechanism of action, no study to date has directly tested it. Therefore, we examined the skills use of 108 women with BPD participating in one of three randomized control trials throughout one year of treatment and four months of follow-up. Using a hierarchical linear modeling approach we found that although all participants reported using some DBT skills before treatment started, participants treated with DBT reported using three times more skills at the end of treatment than participants treated with a control treatment. Significant mediation effects also indicated that DBT skills use fully mediated the decrease in suicide attempts and depression and the increase in control of anger over time. DBT skills use also partially mediated the decrease of nonsuicidal self-injury over time. Anger suppression and expression were not mediated. This study is the first to clearly support the skills deficit model for BPD by indicating that increasing skills use is a mechanism of change for suicidal behavior, depression, and anger control.
Keywords: Dialectical Behavior Therapy, Borderline Personality Disorder, Mechanism of Change, Suicidal Behavior, Major Depression, Anger
Dialectical Behavior Therapy (DBT) is a cognitive-behavioral treatment program originally developed to treat suicidal individuals with Borderline Personality Disorder (BPD). The model of BPD that informs DBT suggests that: 1) BPD is a disorder of emotion dysregulation stemming from important deficits in interpersonal, emotion-regulation (including regulation of mood dependent behaviors), and distress tolerance skills, 2) adaptive behavioral skills that individuals do have in their repertoire are often inhibited or interfered with by maladaptive behavior, and 3) maladaptive behaviors (that constitute many of the criteria of BPD) such as suicidal behaviors or other impulsive behaviors are strengthened through processes of reinforcement. For example, suicidal behavior is viewed as maladaptive problem-solving behavior resulting from a deficit in alternative, adaptive problem solving skills and is reinforced by either an immediate reduction in emotional arousal and/or by the environment's response (Linehan, 1993a). Thus, DBT focuses on teaching new behavioral skills and facilitating the replacement of maladaptive behaviors with skillful behavior.
A growing body of research on individuals with BPD supports the DBT skills deficit model. Evidence suggests that BPD individuals experience difficulties in emotion regulation (Linehan, Bohus, & Lynch, 2007), interpersonal relationships (Kremers, Spinhoven, Van der Does, & Van Dyck, 2006), and distress tolerance (Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2006). Furthermore, suicidal BPD individuals often report that suicidal behaviors function to relieve negative emotions (Brown, Comtois, & Linehan, 2002). Intense negative emotions, and the inability to modulate them, are important precipitators in self-injurious behavior (Nixon, Cloutier, & Aggarwal, 2002). In addition, imagery of both self-injurious and suicidal behaviors are associated with immediate reductions in physiological and subjective measures of negative emotions (Welch, Linehan, Sylvers, Chittams, & Rizvi, 2008).
Additional support for the model comes from evidence suggesting that DBT is an efficacious intervention in reducing suicidal behavior and emotional problems in individuals with BPD. DBT treatment, which includes weekly behavioral skills training, has been shown effective across a wide variety of behavioral outcomes, including suicidal behavior, and emotional distress indicators such as depression and anger (Lynch, Trost, Salsman & Linehan, 2007a). With highly suicidal BPD clients, DBT has been shown effective in two randomized control trials (Linehan, Armstrong, Suarez, Allmon, & Heard, 1991; Linehan et al., 2006a). Compared to treatment-as-usual (TAU) and treatment by community experts (TBE), DBT participants were significantly less likely to attempt suicide or self-injure, had less medically severe intentional self-injury episodes over the year, lower treatment drop-out, tended to enter psychiatric units less often and had fewer inpatient psychiatric days (Linehan, et al., 1991; Linehan et al., 2006a). McMain and colleagues (2009) also compared DBT with medication tapering to general psychiatric management (psychodynamic therapy, symptom-targeted pharmacotherapy, and suicide risk management) for highly suicidal BPD clients. They found significant reductions following treatment in suicidal behavior, health care utilization, depression, borderline psychopathology and anger, but no difference between the two conditions. Treatment gains were also maintained throughout one year of follow up for both groups. Among less severe patients (i.e., those with suicide risk but not necessarily a recent history of self-inflicted injury), DBT reduces anger (Linehan et al., 2008), suicide ideation, hopelessness, and depression (Koons et al., 2001; Lynch, Morse, Mendelson, & Robins, 2003; Verheul et al., 2003).
Furthermore, DBT skills training alone appears to be an effective intervention. Koons and colleagues (2006) provided only skills training to a group of 12 BPD participants. The eight completers improved significantly from pretreatment to six months follow-up on anger expression, control of anger expression, work role satisfaction, and on number of hours worked weekly (Koons et al., 2006). Miller and colleagues (2000) interviewed suicidal adolescents with BPD features undergoing DBT on the usefulness of skills training. Mean subject ratings for each skill module suggested a high perceived efficacy of DBT skills (Miller, Wyman, Huppert, Glassman, & Rathus, 2000).
In other populations, DBT skills training alone was a feasible treatment for oppositional-defiant adolescents (Nelson-Gray et al., 2006), adult ADHD patients (Hesslinger et al., 2002), treatment resistant major depressive disorder (Harley, Sprich, Safren, Jacobo, & Fava, 2008), women with binge eating disorder (Telch, Agras, & Linehan, 2000), difficult to manage correctional populations (Shelton, Sampl, Kesten, Zhang, & Trestman, 2009) and families of suicidal patients (Rajalin, Wickholm-Pethrus, Hursti, & Jokinen, 2009). DBT-skills-only outperformed standard group therapy in improving drop-out, depression, anger and affect instability among BPD clients (Soller et al., 2009). Lastly, a DBT skills only program, modified for a group of women who were victims of domestic abuse, yielded a reduction in depression, hopelessness and general distress (Iverson, Shenk, & Fruzzetti, 2009).
Despite this growing body of evidence, no study to date has examined whether DBT skills use is indeed one of the mechanisms of change associated with treatment efficacy. Relatedly, two studies have examined the frequency of skills practice in DBT. Lindenboim, Comtois, and Linehan (2007) and Stepp and colleagues (2008) used DBT diary cards, a daily self-monitoring record on which clients were asked to circle the skills that they practiced on any given day, as the measure of frequency of skills used. Use of skills was assessed every week throughout one year of treatment. Both groups reported that participants in DBT practiced increasingly more skills over time (Lindenboim, Comtois, & Linehan, 2007; Stepp, Epler, Jahng, & Trull, 2008). However, neither of these studies examined whether increase in skills use has an effect on treatment outcome.
The present study had two aims. The first aim was to evaluate the effectiveness of DBT versus control treatments in increasing DBT skills use. We hypothesized that DBT would increase behavioral skills use significantly more than control treatments. The second aim was to determine whether DBT skills use mediated primary treatment outcomes of suicide attempts, non-suicidal self-injury, anger, and depression. Based on the DBT skills deficit model, we hypothesized that DBT skills use would fully mediate changes in suicidal behavior (suicide attempts and self inflicted injury) and in indicators of emotional distress (anger and depression).
Method
Participants & Procedure
Participants for the current study were drawn from three larger outcome studies on DBT in which DBT skills use was measured. Participants included 63 recurrently suicidal BPD women (Linehan et al., 2006a) and 45 BPD women with drug dependence (Linehan et al., 1999; Linehan et al., 2002) for a total of 108 women with BPD. Demographic information is provided in Table 1. There were no significant differences in demographic characteristics between the suicidal group and the drug dependent group.
Table 1.
Participant Characteristics Break Down Per Condition.
| Total Sample | DBT sample | Control Treatment sample |
|
|---|---|---|---|
| N | 108 | 54 | 54 |
| Mean Age (SD) | 31.44 (7.39) | 31.54 (6.94) | 31.33 (7.88) |
| % Caucasian | 77.8% | 75.9% | 79.6% |
| % African-American | 10.2% | 11.1% | 9.3% |
| % Asian-American | 2.8% | 1.9% | 3.7% |
| % Latino/Chicano | 1.8% | 1.8% | 0.0% |
| % Other Ethnicity | 7.4% | 11.1% | 7.4% |
| % Less than College Degree | 82.2% | 81.5% | 83% |
| % Single, Divorced or Separated | 89.8% | 87.0% | 93.0% |
| % <$15,000/year | 88.3% | 86.5% | 90.2% |
| # of Suicide Attempts at pre- Treatment (SD; Range) |
0.89 (1.26; 0 -10) |
0.72 (0.90; 0 - 4) |
1.06 (1.52; 0 - 10) |
| #of Self Injury Acts at pre- Treatment (SD) |
19.77 (65.50; 0 - 582) |
11.98 (29.85; 0 -158) |
27.56 (87.45; 0 – 582) |
| Average # of current Axis I (SD) | 3.04 (1.82) | 2.89 (1.75) | 3.19 (1.89) |
| Average # of lifetime Axis I (SD) | 4.02 (1.93) | 3.92 (1.93) | 4.11 (1.95) |
| Mean DBT-WCCL DSS pretreatment score (SD) |
1.50 (0.49) | 1.45 (0.51) | 1.55 (0.46) |
Participants met criteria for BPD on both the International Personality Disorders Examination (Loranger, 1995) and Structured Clinical Interview for DSM-IV Axis II Personality Disorders (First, Spitzer, Gibbons, Williams, & Benjamin, 1996). Exclusion criteria included any psychotic disorder, epilepsy or other severe seizure disorder requiring antiseizure medications, other additional problems requiring immediate attention, or court referral. The most prevalent co-occurring Axis I disorders were major depression (60.2%), substance dependence (55.6%), PTSD (41.7%), panic disorder (26.9%), and social phobia (14.8%). See Table 1 for participant characteristics per treatment condition.
In each of the larger studies, participants provided informed consent and were randomly assigned to a treatment condition. Participants were placed in either a DBT condition (n=52) or one of three control treatments: community treatment by experts (CTBE; n=31) –community-based non-behavioral treatment by therapists nominated as experts in treating difficult clients (see Linehan, et al., 2006a for a more detailed description), treatment as usual (TAU, n=11; see Linehan, et al., 1999 for a more detailed description), or comprehensive validation therapy in conjunction with a 12 step program (CVT+12 Step, n=12; see Linehan et al., 2002 for a detailed description). All participants were assigned to one year of treatment, and completed assessments at pretreatment and then every four months including a four month follow-up (at pretreatment, 4 months, 8 months, 12 months, and four months after treatment ended—at 16 months). Study measures were administered at each assessment point by trained assessors, blind to the study condition.
Measures
DBT Ways of Coping Checklist (DBT-WCCL)
The DBT-WCCL is an adaptation of the Revised Ways of Coping Checklist (RWCCL; Vitaliano, Russo, Carr, Maiuro, & Becker, 1985) that includes additional items intended to represent DBT skills (Neacsiu, Rizvi, Vitaliano, Lynch, & Linehan, 2010). The DBT-WCCL, a self-report questionnaire, has 38 items measuring frequency of DBT skills use over the previous month and 21 items measuring dysfunctional, non-DBT coping strategies. In order to avoid potential response bias, DBT language and terms that would resemble skills training or use are avoided in this scale. Rather, a more general description of skillful behavior is used (e.g., instead of “used GIVE skills”. “Made sure I'm responding in a way that doesn't alienate others”). Further, the title “DBT-WCCL” was not included on the questionnaire nor was there any indication that the questionnaire referred to the skills they learned in DBT, but rather asked about ways in which they have coped with stressful events. In the current study, only the subscale measuring DBT skills use was examined. All items, are rated from 0 to 3 (“never use” to “always use”) and the DBT skills use index was computed by averaging across all items in the scale.
Previous examination of the psychometric properties of the DBT-WCCL in BPD individuals revealed that the DBT Skills Subscale of the DBT-WCCL (DSS) had excellent internal consistency (Cronbach α=0.92 to 0.96; n=316). Test-retest reliability at 4 months for 119 BPD individuals treated without access to skills training was acceptable, (ρI = 0.71, p <0.001). In addition, individuals who received skills training had significantly higher scores after four months of treatment than individuals who did not receive skills training (Neacsiu et al., 2010).
Suicide Attempt and Self Injury Interview (SASII)
The SASII (Linehan, Comtois, Brown, Heard, & Wagner, 2006b) is a semi-structured interview that assesses the factors involved in non-fatal suicide attempts and non-suicidal self-injury. For the present study, two variables were used: number of suicide attempts (including attempts with ambivalent intent) and number of nonsuicidal self injury (NSSI) episodes since the previous assessment. Both variables were highly skewed and clustered; therefore they were transformed into binary variables: attempts (none versus any) and NSSI episodes (none versus any). The SASII has been shown to have very good inter-rater reliability and adequate validity (Linehan et al., 2006b).
Hamilton Rating Scale for Depression (HRSD)
The 17-item HRSD (Hamilton, 1960) is an interviewer-rated scale which has been widely used in clinical research. The interview assesses cognitive and melancholic symptoms, and uses standard prompt questions for each rating. Inter-rater reliability has been found to range from 0.82 and 0.96, with an intraclass r ranging from 0.46 to 0.99. Test-retest reliability ranged from 0.81 to 0.98 (Bagby, Ryder, Schuller, & Marshall, 2004).
State-Trait Anger Expression Inventory (STAXI)
The STAXI (Spielberger, 1988) is a widely used self-report measure for anger. The questionnaire has four subscales which measure the disposition to experience anger (Anger Trait), the frequency with which anger is both suppressed (Anger In) and expressed (Anger Out), and the amount of control over the anger attempted by the participant (Anger Control; Spielberger, 1988). In this study, we used Anger Out, Anger In and Anger Control as indicators of anger throughout the treatment. Anger trait was not used because it is considered a stable personality characteristic of the individual and therefore not as amenable to change as a target of treatment. Internal consistency of the scales is reported to range between 0.73 and 0.93, and construct validity was demonstrated through associations between each scales and responses to anger scenarios (Spielberger, 1988).
Data Analysis
A mixed-effects models approach was used to analyze the repeated measures data (pre-treatment through the 16-month assessment (Longford, 1993). Appropriate covariance structures were analytically determined based on a comparing model fit criteria such as Restricted Maximum likelihood (REML) estimate, Akaike Information criteria (AIC), and the Akaike Information corrected criteria (AICC) in comparing nested models (Verbeke, 1997). As a result, a hierarchical linear modeling approach (HLM; Bryk & Raudenbush, 1992) was chosen. First, we assessed whether the three control conditions had differential effects on skills use. Second, differences in rates of change in DBT skills use (i.e., the slopes of the subject-specific regression lines) were compared for the two treatment groups: DBT and control conditions (TAU+CVS+TBE).
To examine mediation within the context of multi-level models, the procedure outlined by Krull and MacKinnon (2001) was followed. In order to preserve a temporal connection (Kraemer, Wilson, Fairburn, & Agras, 2002), the mediator introduced in equations was DBT skills use at the previous time point. According to Baron and Kenny (1986) and Krull and MacKinnon (2001), three criteria must be met to support full mediation. First, the independent variable needs to be significantly related to the mediator (DBT skills use at time point t-1). Second, the independent variable must significantly predict the outcome variable (e.g., anger at time point t). Third, for full mediation, the relationship between independent variable and outcome must disappear when the mediator is introduced into the equation. If after introducing the mediator into the equation, the coefficient between the independent variable and outcome remains significant but is reduced, there is evidence for partial mediation.
We hypothesized that DBT skills use, as a proxy for skillful behavior, would mediate treatment outcomes in general, and not only in DBT. Doss and Atkins (2006) highlighted that when treatment condition is included in the mediation, what is measured is the effect on outcome of the difference of two treatments, and not necessarily the effect of interventions on outcome. Many of the DBT skills were derived from behavioral assignments and suggested client practices in other treatments (Linehan, 1993b) and therefore, skills use may occur despite explicit skills training. Thus, the hypothesis of the importance of skills use in the change of outcome variables is better examined as a nonspecific predictor of outcome by constructing the mediation model around the significance of the time effect in predicting the mediator and outcome. In our analyses, therefore, the independent variable was time in treatment and not type of treatment. Nevertheless, because the total sample included the participants from three different studies, we added a categorical variable, “study,” as a covariate to our mediation analyses. This addition was made to address the unique sources of variation from each original study that could confound the mediation findings.
The mediation effect was computed by multiplying the path coefficient between the independent variable and the mediator (α) by the path coefficient between the mediator and the outcome variable (β) using the following z-score formula where σβ2 is the square of the standard error of β and σα2 is the square of the standard error of α (Krull & MacKinnon, 2001):
Recent work by Shrout and Bolger (2002) and Preacher and Hayes (2004) has shown that the classical test statistic for mediation has lower power. Therefore, they recommended the use of bootstraps to test mediation. To increase the power of our analysis we therefore used the bootstrap approach by treating the complete mediation data set as if it were a population. From this dataset, 999 bootstrap samples were repeatedly created using replacements from the original data set. Because this technique was applied as part of a longitudinal framework, we followed Chernick's (1999) recommendations and used case resampling through selecting a subject's entire data collection if the participant was selected as part of the bootstrap sample. Within each bootstrap sample we derived its mediation effect. Therefore, the final mediation effect (for the original data set) and its standard error were computed using the bootstrapping approach as the mean and standard deviation of the distribution of the mediation effects over the bootstrap samples. To further assess the statistical significance of the effect, we derived the empirical 95% confidence interval for the mediation effects, which corresponded to the 2.5% and 97.5% observed values. Confidence intervals including 0 indicated a mediation effect that was not statistically significant.
For each of the equations used in the mediation analyses, the mixed-effects models approach (Longford, 1993) was used for normally distributed outcomes (depression and anger) and a generalized estimating equation analysis (GEE; Liang & Zeger, 1986) was used for outcomes that were infrequent and highly skewed (suicide attempts and nonsuicidal self injury). In the latter case, variables were recoded into binary variables (none versus any) and pretreatment values were used as a covariate.
Missing data imputations were not specified in either the HLM or the GEE models. A restricted estimated maximum likelihood (REML) model was used for HLM analyses, which accounts for the missing data. In this approach, time is treated as a continuous variable, and a regression line is modeled for each participant based on the number of available points. The model does not assume each outcome to be measured on the same number of points and therefore any time point sampling is relevant to the regression line the model creates. Thus, subjects with missing data are still modeled using the data points they do have. (Schafer & Graham, 2002; Gibbons, Hedeker, & DuToit, 2010). GEE assumes that if there is missing data, it is missing completely at random (MCAR). The analysis computes the marginal means of the available data, even if it has missing points. Standard errors (SEs) are adjusted as part of the model to accommodate for the amount of independent information that is entered in the model. Therefore, if a subject with missing data is entered, SE may be inflated to account for this difference (Gibbons, Hedeker, & DuToit, 2010).
While the modeling approaches accommodate “missing data”, we implemented pattern-mixture models (Hedeker & Gibbons, 1997) to assess whether important mediations estimates per the HLM and GEE models were dependent on missing data patterns (Hamer & Simpson, 2009). To determine whether mediation effects were driven by informative missing data patterns, we classified two monotonic patterns of patients' available data (treatment completers versus treatment drop outs) and assessed the interaction of pattern with the mediation effect in our analyses.
Results
DBT Skills Use as an Outcome of Treatment
To assess the hypothesis that DBT would increase behavioral skills use significantly more than control treatments, participants who received DBT were compared to participants in the three control conditions. In order to determine whether control conditions had differential effects on skills use, or whether we could combine them into one control group, an HLM analysis was conducted assessing the interaction between time and each control condition in predicting skills use. The analysis revealed a nonsignificant effect for condition (F(2, 217.49)=0.51, p=0.60) and a nonsignificant interaction between time in treatment and control condition (F(2, 76.31)=0.83, p=0.44). All control conditions had similar effects on variations of skills use over time and therefore were combined into one control condition for the rest of the analyses. Thus, in describing the rest of the results, “treatment condition” refers to DBT versus control treatment.
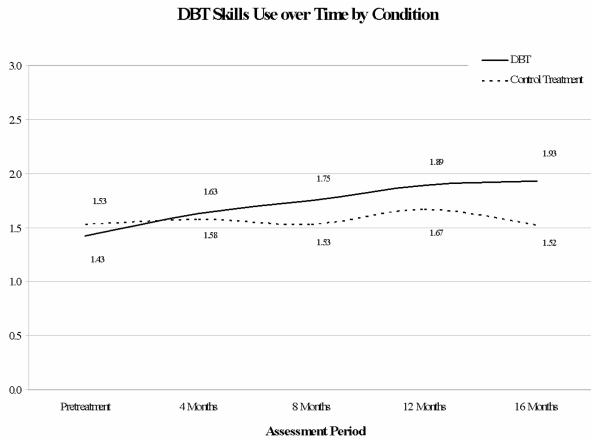
HLM analyses revealed a significant interaction between time and treatment condition in predicting DBT skills use (F (1, 90.85) = 26.41, p<0.001). Specifically, clients in DBT reported higher DBT skills use than clients in the control conditions over time (see Figure 1). Furthermore, participants in the control conditions did not change over time in their DBT skills use. The DBT slope estimate was 0.13 (SD=0.02), which was significant, t(90.61)=7.11, at the 0.001 level; the control treatment slope estimate was −0.004 (SD=0.02), which was not significant, t(91.05)=−0.23.
Figure 1.
Change in DBT Skills Use across Time in DBT and Control Treatment
Note: Treatment ended at 12 months. The 16 month assessment point is a follow up assessment. Skills use was rated on a scale from 0 to 3, 0 denoting no skills use and 3 denoting using all the skills most of the time.
At pretreatment, the mean score for all participants on the DBT-WCCL was 1.48 (SD=0.48; range=0.29 to 2.63). At the end of the treatment year, participants in the DBT condition increased in their mean DBT skills use from 1.43 to 1.89 (a 15.33% increase), while participants in the control conditions increased from 1.53 to 1.67 (a 4.66% increase). Four months after treatment ended, participants in the DBT condition remained at the same level of DBT skills as at the end of their treatment year, while participants in the control condition dropped from 1.67 to 1.52 (a 5.00% decrease).
DBT Skills Use as Mediator of Outcome
To assess the hypothesis that DBT skills use would fully mediate changes in primary outcomes, data from the four treatment conditions were combined. The fact that DBT skills use was seen across treatment conditions at pretreatment strengthened the theoretical decision to examine mediation over time, not by treatment condition. In addition, including all data allowed for sufficient number of data points as well as sufficient variation in the DBT skills use at each time point. Although the participants in the control condition, on average, stayed the same throughout treatment, 24 control participants had higher scores and 16 had lower scores at the end of treatment when compared to pretreatment, suggesting that there was indeed variability in skills use in this group. Mediation analyses were then conducted for each of the following four outcomes: suicidal behavior, nonsuicidal self-injury, anger, and depression. The independent variable used was time in treatment, and the mediator was the DBT-WCCL skills subscale score assessed at the previous time point. Bootstrapping was used to compute a more robust mediation effect as well as confidence intervals and the original study from which the participant was sampled was covaried. Significance for the mediation effect was concluded if the confidence interval computed for the bootstrapped mediation effect did not include 0.
DBT skills use as a mediator of improvements in suicidal behavior and NSSI
Due to the clustering of the data and the binary nature of both outcome variables (suicide attempts and NSSI), a GEE model, covarying study and pretreatment levels of suicidality, was implemented. GEE analyses predicting the likelihood of no suicide attempt/NSSI episode to occur were conducted to assess mediation.
A significant mediation effect indicated that an increase in the DBT skills use fully mediated the relationship between time in treatment and decrease in likelihood for suicide attempts to occur (Table 2). When the mediator was added to the equation, the raw βc coefficient (of the independent variable, time in treatment, predicting the dependent variable, likelihood of no suicide attempt) dropped from 0.36, p<0.05 to 0.27, p=0.16. Significant mediation effect also indicated that an increase in the DBT skills use partially mediated the increase in likelihood of no NSSI episodes to occur over time in treatment (Table 2). In this analysis, when the mediator was added to the equation, the raw βc coefficient (of the independent variable, time in treatment, predicting the dependent variable, likelihood of no NSSI episode) dropped from 0.41, p<0.001 to 0.34, p<0.01. The reverse models for both likelihood of suicide attempts and likelihood of NSSI at the previous time point mediating current use of skills were not significant (p>0.05). Furthermore, the pattern-mixture analyses in which we assessed whether the interaction between the mediator and treatment drop status, were non-significant in both models (p> 0.05).
Table2.
Single level estimates and standard errors of α, β and the mediated effect for different treatment outcomes using the DBT skills use as a mediator and study as covariate
| Outcome | α (SD) | β (SD) | Mediated Effect with Bootstraps method (SE) |
95% confidence interval for mediated effect |
|---|---|---|---|---|
| Suicide Attempts (none vs. any) |
0.09 (0.02)*** | 0.76 (0.34)* | 0.07 (0.04) | [0.003 – 0.15] |
| Nonsuicidal Self Injury (none vs. any) |
0.09 (0.02)*** | .94 (0.28)** | 0.09 (0.04) | [0.03 – 0.18] |
|
| ||||
| Anger Control | 0.09 (0.02)*** | 1.25 (0.48)** | 0.13 (0.05) | [0.04 – 0.25] |
| Anger Out | 0.09 (0.02)*** | −0.62 (0.36) † | −0.06 (0.04) | [−0.14 – 0.01] |
| Anger In | 0.09 (0.02)*** | −0.20 (0.45) | −0.02 (0.04) | [−0.11 – 0.05] |
|
| ||||
| Depression | 0.09 (0.02)*** | −1.55 (.84) † | −0.14 (0.07) | [−0.02 – −0.29] |
p < .10
p < .05
p < .01
p < .001 (2-tailed tests);
α is the coefficient of the independent variable (time in treatment) predicting the mediator (DBT skills use), β is the coefficient of the mediating variable (DBT skills use at the previous time point) predicting the outcome variable when the independent variable (time in treatment) is also included in the equation; Suicide attempts and nonsuicidal self-injury (NSSI) are binary variables, where 0 represents no suicide attempt/NSSI episodes and 1 represents any suicide attempt/NSSI episode since the last assessment; the models for these variables predict the likelihood of no suicide attempt/NSSI episode; confidence intervals are computed on the mediation effect using bootstrapping; confidence intervals containing 0 are not statistically significant mediation effects.
DBT skills use as a mediator of improvements in anger
Anger variables were normally distributed and therefore a single-level HLM model was used for each of the three mediation equations. These analyses indicated that the relationship between time in treatment and increase in Anger Control was fully mediated by DBT skills use (α and β paths in Table 2) when using a bootstrap approach and covarying the original study from which the participant was sampled. The coefficient for time in treatment (βc) predicting Anger Control outcome dropped from 0.57, p<0.001, when the mediator was not part of the model, to 0.35, p>0.05 when the mediator was added to the model. The reverse mediational model (Anger Control at the previous time point mediating current use of skills) and the pattern mixture result (mediator * treatment drop status predicting anger control) were not significant (p>0.05). Single-level mediation analyses indicated that the relationships between time in treatment and Anger In or Anger Out were not mediated by DBT skills use (see Table 2).
DBT skills use as a mediator of improvements in depression
The total score for depression was also normally distributed and therefore a single-level HLM model was used for each of the three mediation equations. As shown in Table 2, the analyses indicated that DBT skills use fully mediated improvements in depression over time (α and β paths in Table 2) when using a bootstrap approach and covarying the original study from which the participant was sampled. Although β was only significant at a trend level, the confidence interval for the mediation effect indicated that the full mediation was significant. The coefficient for time in treatment predicting depression (βc) dropped from −0.91 (p<0.001), when the mediator was not part of the model, to −0.29, (p>0.05) when the mediator was added to the model. The reverse mediational model (depression at the previous time point mediating current use of skills) was not significant (p>0.05). Furthermore, the pattern-mixture result assessing for a significant interaction between the mediator and data missing because of subjects dropping treatment was non-significant (p> 0.05).
Discussion
The present study examined BPD individuals' DBT skills use throughout treatment, and its relationship to primary outcome variables. Four main findings emerged. First, all participants reported using at least some DBT skills about 50% of the time before treatment started. Second, participants treated with DBT reported using skills throughout treatment significantly more than participants in the control condition. Third, DBT skills use fully mediated the likelihood of suicide attempts and partially mediated the likelihood of NSSI to occur. Fourth, skills use fully mediated the change over time of certain indicators of emotional distress (Anger Control and depression). These findings provide further validation for the DBT model by indicating that an increase in DBT skills mediates some of the outcomes reported in DBT RCTs (see Lynch, Trost, Salsman, & Linehan, 2007a).
Although DBT is based on the assumption that remediating skills deficits will drive a decrease in maladaptive behavior, research thus far has at most indicated an association between skills deficit change and maladaptive behavior change. This study is the first to clearly support the skills deficit model for suicidal behavior in BPD by showing that increasing skills use is a mechanism of change for suicide attempts. The partial mediation found for nonsuicidal self injury partially supports the skills deficit model, and suggests that additional factors may play into the change seen in this behavior throughout treatment. For example, research indicates that thought suppression is a partial mediator for the relationship between emotional reactivity and NSSI (Najmi, Wegner, & Nock, 2006) and is also associated with self harm frequency (Chapman, Specht, & Cellucci, 2005). BPD treatments may reduce thought suppression through at least directly assessing problems, which may in turn influence the change seen in NSSI above and beyond skills use.
Skills use also fully mediated the decrease in depression over time. This finding is compatible with the theory proposed by Jacobson, Martell, and Dimidijan (2001) who suggested that the mechanism of change for depression is behavioral activation. DBT conceptualizes the lack of behavioral activation as a skills deficit and therefore teaches principles of behavioral activation within the emotion regulation module (Linehan, 1993b). There have now been a number of studies that indicate DBT's efficacy in treating depression (Harley et al., 2008; Lynch et al., 2003; Lynch et al., 2007b). Furthermore, an increase in emotional processing was found to be related to a reduction in depression only for DBT participants but not for control participants in a treatment resistant group with major depression (Feldman et al., 2009). Thus, while DBT has been shown to be effective in reducing depression in BPD and depression populations, the mechanism of change was to date unclear. Our finding suggest that the use of DBT skills is an active ingredient behind changes in depression.
Skills use also fully mediated the increase in anger control over time. The STAXI Anger Control scale assesses how successful a person is in regulating cues that could trigger anger and is very close to the anger regulation taught in the DBT emotion regulation module (Linehan, 1993b). The full mediation of Anger Control improvement signals that skills training may indeed help clients to better regulate the emotion of anger. Similar to depression, prior studies have shown a positive effect of DBT treatment on anger dysregulation (e.g., Linehan et al., 2008). This finding emphasizes that the mechanism of change behind such findings may be use of DBT skills.
No evidence for mediation was found for changes in Anger In (anger suppression) or Anger Out (anger expression) which may seem puzzling, especially in light of the other findings. However, it is consistent with the DBT skills deficit model because the items in both scales may refer to both functional (“I keep things in”; “I express my anger”) and dysfunctional (“I pout or sulk”, “I do things like slam doors”) behaviors. In DBT skills training, clients learn how to tolerate and problem-solve unjustified anger, how to accept justified anger, how to stand up for themselves if needed, how to be mindful of the current emotion and how to accurately express how they are feeling (Linehan, 1993b). Keeping anger to oneself may be effective behavior (e.g., the individual is mindful of the emotion while aware that expressing it may hurt a relationship) or a target for change (e.g., individual bottles up and explodes periodically in rage attacks). Similarly, expressing anger may be a behavior to increase if emotional numbness or lack of assertiveness is the problem behavior, or to decrease if anger is not justified by the context and appears out of control. DBT skills are aimed at increasing the client's effectiveness in handling inter- and intra- personal situations. The fact that the Anger In and Out scales are not necessarily tied to effectiveness may explain the null findings in this study.
In addition to the mediation findings, results also indicate that DBT is effective in teaching DBT skills, which further supports the studies of Lindenboim and colleagues (2007) and Stepp and colleagues (2008). Besides strengthening their finding that skills use increases with the provision of DBT, this study further indicates that skills use increases more in DBT than in other treatment conditions. Thus, being treated with DBT versus a control treatment results in more skills used in distressing situations, even when DBT-specific language does not confound measurment. Moreover, the fact that the change seen in DBT at the end of treatment was maintained at the four month follow up (unlike in the control conditions) also indicates that DBT is effective in ensuring that generalization of skills use occurs. The important question that remains to be addressed is whether the increase in skills use is particular to the DBT skills taught or whether it represents an increase in DBT skills and self efficacy in general.
It is also interesting to note that when DBT skills were reframed into non-DBT specific language, participants reported using some of the skills even before treatment started. While some people reported using skills only a few times, the majority reported using DBT skills about half the time at pretreatment. Also, skills use and not skills training mediated treatment outcomes. This leads to important questions about whether skills training is the most effective way to increase skills use, whether teaching all the skills is necessary for successful DBT outcomes, or whether the skills training modules could be shortened to incorporate only novel skills.
Although the results are generally supporting of the DBT model, several potential limitations should be noted. Even though there is no reason to believe that there was a systematic over-reporting or under-reporting of skill practice by the entire sample, it is certainly possible that some individuals exhibited either the former or the latter tendency. In a study comparing an assessment of retrospective coping over the past week using the RWCCL and an abbreviated daily coping version, Smith, Leffingwell and Ptacek (1999) reported that only 25% of the variance was shared between the retrospective account and the modified daily version. Since the present analyses used an adapted version of the RWCCL that was assessed over the previous month, retrospective bias may indeed be an important flaw in data accuracy. However, since the statistical model used controls for intra-individual factors, retrospective bias likely had a smaller effect since it can be expected that it did not fluctuate over time within the same individual. A possible future improvement would be to control for retrospective bias by using ambulatory monitoring and assessing DBT skills use on a daily basis. An additional limitation was that the measure used a checklist format that focused on how often a specific skill was practiced in particular distressing situation. The format offered advantages since participants from both DBT and control treatments could offer comparable information about their DBT skills use. Nevertheless, important descriptors of the skills practice such as intensity of use, the appropriateness of the skill used, and the quality of the skill used were not assessed.
It is important to also highlight the statistical approach we took to examine our hypotheses. We considered skills use to be a universal treatment mechanism and assessed its impact on the relationship between time in treatment and various outcomes. The DBT model could have also been assessed using a moderated mediation statistical approach, in which treatment condition (DBT or control) could have been considered the moderator and skills use would have been the mediator (Kraemer et al., 2002). Our decision not to use a moderated mediation approach was based on the fundamental question for the current study being not whether DBT performs better than another treatment, but what processes drive changes in suicidal behavior, depression and anger over time. Moderated mediation investigates the mechanisms through which a treatment performs better than another, not about the mechanism through which change happens over time in treatment in a clinical population (Doss & Atkins, 2006). While DBT may have indeed targeted skills training more explicitly, therapy in general targets engaging in effective behavior that leads to change which is in essence skills use. In this regard using skills or using effective behaviors in difficult situations can be thought as a universal mechanism of change in psychological treatments. Illustrative of this, all clients used some skills before treatment started, and varied in skills use throughout treatment, regardless of the treatment they were receiving.
Nevertheless, our approach has some limitations. First, it may be that skills use is a mechanism of change unique to DBT. In this case, our analysis may underestimate the mediation effect by adding data from treatments where this mechanism was not present. Future analyses should investigate whether skills use is a universal or a unique mechanism of change in treatment. Second, an assumption that is commonly made for standard mediation analysis methods, such as the one used here, is that there is no extraneous variable which influences both the mediator and the outcome (Robins and Rotnitzky, 2005). In the case of our analysis, it is possible to have had unmeasured confounds influencing the results. An interesting avenue for future research would also be to validate the DBT model using a causal inferences approach, which would account for this limitation (MacKinnon et al., 2007). Although there have been some examples of these models used in longitudinal data (e.g., Lin et al., 2008), proper models to accommodate unmeasured confounds coupled with repeated measures are an active area under current research.
An additionally important avenue for future research is therefore to replicate these findings with different samples and statistical techniques. Furthermore, future research should also assess how use of particular skills mediates outcomes that are directly targeted in skills training. Some questions that could be answered from such research include: Does use of emotion regulation skills actually improve emotion regulation? Are distress tolerance skills and/or other skills responsible for the improvement in behavioral self-control seen in DBT? Answers to these questions could lead to the refinement of DBT and other treatments to maximize their effectiveness.
Acknowledgments
This study was supported by the MH34486 and MH01593 grants from the National Institute of Mental Health, as well as by grant DA08674 from the National Institute of Drug Abuse, National Institute of Health, awarded to Marsha M. Linehan, PhD, Principal Investigator. We thank the clients, therapists, assessors, and staff at the Behavioral Research and Therapy Clinics, without whom this research would not have been possible. We also thank Bob Gallop, Ph.D., Melanie Harned, Ph.D. and Tom Lynch, Ph.D. for providing statistical consultation on this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bagby RM, Ryder AG, Schuller DR, Marshall MB. The Hamilton depression rating scale: Has the gold standard become a lead weight? American Journal of Psychiatry. 2004;161:2163–2177. doi: 10.1176/appi.ajp.161.12.2163. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The Moderator Mediator Variable Distinction in Social Psychological-Research - Conceptual, Strategic, and Statistical Considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Brown M, Comtois KA, Linehan MM. Reasons for suicide attempts and nonsuicidal self-injury in women with borderline personality disorder. Journal of Abnormal Psychology. 2002;111:198–202. doi: 10.1037//0021-843x.111.1.198. [DOI] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical linear models: Applications and data analysis methods. Sage; Newbury Park, CA: 1992. [Google Scholar]
- Chapman AL, Specht MW, Cellucci T. Borderline personality disorder and deliberate self-harm: does experiential avoidance play a role? Suicide and Life-Threatening Behavior. 2005;35:388–399. doi: 10.1521/suli.2005.35.4.388. [DOI] [PubMed] [Google Scholar]
- Chernick MR. Bootstrap Methods, A Practitioner's Guide. Wiley; New York, NY: 1999. [Google Scholar]
- Doss BD, Atkins DC. Investigating treatment mediators when simple random assignment to a control group is not possible. Clinical Psychology: Science and Practice. 2006;13:321–336. [Google Scholar]
- Feldman G, Harley R, Kerrigan M, Jacobo M, Fava M. Change in emotional processing during a dialectical behavior therapy based skills group for major depressive disorder. Behaviour Research and Therapy. 2009;47(4):316–321. doi: 10.1016/j.brat.2009.01.005. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbons M, Williams JBW, Benjamin L. User's guide for the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) Biometrics Research Department, New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- Gibbons RD, Hedeker D, DuToit S. Advances in Analysis of Longitudinal Data. Annual Review of Clinical Psychology. 2010;6:79–107. doi: 10.1146/annurev.clinpsy.032408.153550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, Gunderson JG. An experimental investigation of emotion dysregulation in borderline personality disorder. Journal of Abnormal Psychology. 2006;115(6):850–855. doi: 10.1037/0021-843X.115.4.850. [DOI] [PubMed] [Google Scholar]
- Hamer RM, Simpson PM. Last observation carried forward versus mixed models in the analysis of psychiatric clinical trials. American Journal of Psychiatry. 2009;166:639–641. doi: 10.1176/appi.ajp.2009.09040458. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harley R, Sprich S, Safren S, Jacobo M, Fava M. Adaptation of dialectical behavior therapy skills training group for treatment-resistant depression. Journal of Nervous and Mental Disorders. 2008;196(2):136–143. doi: 10.1097/NMD.0b013e318162aa3f. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological Methods. 1997;2:64–78. [Google Scholar]
- Hesslinger B, Tebartz van Elst L, Nyberg E, Dykierek P, Richter H, Berner M, et al. Psychotherapy of attention deficit hyperactivity disorder in adults--a pilot study using a structured skills training program. European Archives of Psychiatry Clinical Neuroscience. 2002;252:177–184. doi: 10.1007/s00406-002-0379-0. [DOI] [PubMed] [Google Scholar]
- Iverson KM, Shenk C, Fruzzetti AE. Dialectical behavior therapy for women victims of domestic abuse: a pilot study. Professional Psychology: Research and Practice. 2009;40(3):242–248. [Google Scholar]
- Jacobson NS, Martell CR, Dimidijan S. Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychology. 2001;8:255–270. [Google Scholar]
- Koons CR, Chapman AL, Betts BB, O'Rourke B, Morse N, Robins CJ. Dialectical behavior therapy adapted for the vocational rehabilitation of significantly disabled mentally ill adults. Cognitive and Behavioral Practice. 2006;13:146–156. [Google Scholar]
- Koons CR, Robins CJ, Tweed JL, Lynch TR, Gonzalez AM, Morse JQ, et al. Efficacy of dialectical behavior therapy in women veterans with borderline personality disorder. Behavior Therapy. 2001;32:371–390. [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Kremers IP, Spinhoven P, Van der Does AJW, Van Dyck R. Social problem solving, autobiographical memory and future specificity in outpatients with borderline personality disorder. Clinical Psychology & Psychotherapy. 2006;13:131–137. [Google Scholar]
- Krull JL, MacKinnon DP. Multilevel modeling of individual and group level mediated effects. Multivariate Behavioral Research. 2001;36:249–277. doi: 10.1207/S15327906MBR3602_06. [DOI] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal Data-Analysis Using Generalized Linear-Models. Biometrika. 1986;73:13–22. [Google Scholar]
- Lin JY, Ten Have TR, Elliott MR. Longitudinal Nested Compliance Class Model in the Presence of Time-Varying Noncompliance. Journal of the American Statistical Association. 2008;103:462–473. [Google Scholar]
- Lindenboim N, Comtois KA, Linehan MM. Skills practice in dialectical behavior therapy for suicidal borderline women. Cognitive and Behavioral Practice. 2007;14:147–156. [Google Scholar]
- Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Archives of General Psychiatry. 1991;48:1060–1064. doi: 10.1001/archpsyc.1991.01810360024003. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. Guilford Press; New York: 1993a. [Google Scholar]
- Linehan MM. Skills training manual for treating borderline personality disorder. Guilford Press; New York, NY: 1993b. [Google Scholar]
- Linehan MM, Schmidt H, III, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. American Journal of Addiction. 1999;8(4):279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welch SS, Heagerty P, et al. Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug and Alcohol Dependence. 2002;67:13–26. doi: 10.1016/s0376-8716(02)00011-x. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs. therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry. 2006a;63:757–766. doi: 10.1001/archpsyc.63.7.757. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Brown MZ, Heard HL, Wagner A. Suicide Attempt Self-Injury Interview (SASII): development, reliability, and validity of a scale to assess suicide attempts and intentional self-injury. Psychological Assessment. 2006b;18:303–312. doi: 10.1037/1040-3590.18.3.303. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Bohus M, Lynch T. Dialectical Behavior Therapy for Pervasive Emotion Dysregulation: Theoretical and Practical Underpinnings. In: Gross J, editor. Handbook of Emotion Regulation. Guilford; New York: 2007. [Google Scholar]
- Linehan MM, McDavid JD, Brown MZ, Sayrs JH, Gallop RJ. Olanzapine plus dialectical behavior therapy for women with high irritability who meet criteria for borderline personality disorder: a double-blind, placebo-controlled pilot study. Journal of Clinical Psychiatry. 2008;69:999–1005. doi: 10.4088/jcp.v69n0617. [DOI] [PubMed] [Google Scholar]
- Longford NT. Random Coefficient Models. Oxford University; New York: 1993. [Google Scholar]
- Loranger AW. International Personality Disorder Examination (IPDE) Manual. Cornell Medical Center; White Plains, NY: 1995. [Google Scholar]
- Lynch TR, Morse JQ, Mendelson T, Robins CJ. Dialectical behavior therapy for depressed older adults: a randomized pilot study. American Journal of Geriatric Psychiatry. 2003;11:33–45. [PubMed] [Google Scholar]
- Lynch TR, Trost WT, Salsman N, Linehan MM. Dialectical behavior therapy for borderline personality disorder. Annual Review of Clinical Psychology. 2007a;3:181–205. doi: 10.1146/annurev.clinpsy.2.022305.095229. [DOI] [PubMed] [Google Scholar]
- Lynch TR, Cheavens JS, Cukrowicz KC, Thorp SR, Bronner L, Beyer J. Treatment of older adults with co-morbid personality disorder and depression: A Dialectical Behavior Therapy approach. International Journal of Geriatric Psychiatry. 2007b;22:131–143. doi: 10.1002/gps.1703. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation Analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L, et al. A randomized trial of Dialectical Behavior Therapy versus general psychiatric management for borderline personality disorder. American Journal of Psychiatry. 2009;166:1365–1374. doi: 10.1176/appi.ajp.2009.09010039. [DOI] [PubMed] [Google Scholar]
- Miller AL, Wyman SE, Huppert JD, Glassman SL, Rathus JH. Analysis of behavioral skills utilized by suicidal adolescents receiving dialectical behavior therapy. Cognitive and Behavioral Practice. 2000;7:183–187. [Google Scholar]
- Najmi S, Wegner DM, Nock M. Thought suppression and self-injurious thoughts and behaviors. Behaviour Research and Therapy. 2007;45(8):1957–1965. doi: 10.1016/j.brat.2006.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neacsiu AD, Rizvi SL, Vitaliano PP, Lynch TR, Linehan MM. The Dialectical Behavior Therapy Ways of Coping Checklist (DBT-WCCL): Development and Psychometric Properties. Journal of Clinical Psychology. 2010;66(6):1–20. doi: 10.1002/jclp.20685. [DOI] [PubMed] [Google Scholar]
- Nelson-Gray RO, Keane SP, Hurst RM, Mitchell JT, Warburton JB, Chok JT, et al. A modified DBT skills training program for oppositional defiant adolescents: promising preliminary findings. Behaviour Research and Therapy. 2006;44:1811–1820. doi: 10.1016/j.brat.2006.01.004. [DOI] [PubMed] [Google Scholar]
- Nixon MK, Cloutier PF, Aggarwal S. Affect regulation and addictive aspects of repetitive self-injury in hospitalized adolescents. Journal of the American Academy for Child and Adolescent Psychiatry. 2002;41:1333–1341. doi: 10.1097/00004583-200211000-00015. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavioral Research Methods, Instruments, and Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Rajalin M, Wickholm-Pethrus L, Hursti T, Jokinen J. Dialectical behavior therapy-based skills training for family members of suicide attempters. Archives of Suicide Research. 2009;13:257–263. doi: 10.1080/13811110903044401. [DOI] [PubMed] [Google Scholar]
- Robins J, Rotnitzky A. Estimation of treatment effects in randomized trials with non-compliance and dichotomous outcome using structural mean models. Biometrika. 2005;91:763–783. [Google Scholar]
- Schafer JL, Graham JW. Missing Data: Our View of the State of the Art. Psychological Methods. 2002;7(2):147–177. [PubMed] [Google Scholar]
- Shelton D, Sampl S, Kesten KL, Zhang WL, Trestman RL. Treatment of impulsive aggression in correctional settings. Behavioral Sciences & the Law. 2009;27:787–800. doi: 10.1002/bsl.889. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Smith RE, Leffingwell TR, Ptacek JT. Can people remember how they coped? Factors associated with discordance between same-day and retrospective reports. Journal of Personality and Social Psychology. 1999;76:1050–1061. [Google Scholar]
- Soler J, Pascual JC, Tiana T, Cebria A, Barrachina J, Campins MJ, et al. Dialectical behaviour therapy skills training compared to standard group therapy in borderline personality disorder: A 3-month randomised controlled clinical trial. Behaviour Research and Therapy. 2009;47:353–358. doi: 10.1016/j.brat.2009.01.013. [DOI] [PubMed] [Google Scholar]
- Spielberger CD. Manual for the State-Trait Anger Expression Inventory(STAXI) Psychological Assessment Resources; Odessa, FL: 1988. [Google Scholar]
- Stepp SD, Epler AJ, Jahng S, Trull TJ. The Effect of Dialectical Behavior Therapy Skills Use on Borderline Personality Disorder Features. Journal of Personality Disorders. 2008;22:549–563. doi: 10.1521/pedi.2008.22.6.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telch CF, Agras WS, Linehan MM. Group dialectical behavior therapy for binge-eating disorder: A preliminary, uncontrolled trial. Behavior Therapy. 2000;31:569–582. [Google Scholar]
- Verbeke G. Linear Mixed Models for Longitudinal Data. In: Verbeke G, Molenberghs G, editors. Linear Mixed Models in Practice. Springer; New York: 1997. [Google Scholar]
- Verheul R, van den Bosch LMC, Koeter MWJ, de Ridder MAJ, Stijnen T, van den BW. Dialectical behaviour therapy for women with borderline personality disorder: 12-month, randomized clinical trial in The Netherlands. British Journal of Psychiatry. 2003;182:135–140. doi: 10.1192/bjp.182.2.135. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP, Russo J, Carr JE, Maiuro RD, Becker J. The Ways of Coping Checklist - Revision and Psychometric Properties. Multivariate Behavioral Research. 1985;20:3–26. doi: 10.1207/s15327906mbr2001_1. [DOI] [PubMed] [Google Scholar]
- Welch SS, Linehan MM, Sylvers P, Chittams J, Rizvi SL. Emotional responses to self-injury imagery among adults with borderline personality disorder. Journal of Consulting and Clinical Psychology. 2008;76:45–51. doi: 10.1037/0022-006X.76.1.45. [DOI] [PubMed] [Google Scholar]