Abstract
Varus knee alignment is a risk factor for medial knee osteoarthritis and is associated with high knee adduction moments. Therefore, reducing the knee adduction moment in varus-aligned individuals with otherwise healthy knees may reduce their risk for developing osteoarthritis. A gait modification that improves dynamic knee alignment may reduce the adduction moment, and systematic training may lead to more natural-feeling and less effortful execution of this pattern. To test these hypotheses, eight healthy, varus-aligned individuals underwent a gait modification protocol. Real-time feedback of dynamic knee alignment was provided over eight training sessions, using a fading paradigm. Natural and modified gait were assessed post-training and after 1 month, and compared to pre-training natural gait. The knee adduction moment, as well as hip adduction, hip internal rotation and knee adduction angles were evaluated. At each training session, subjects rated how effortful and natural-feeling the modified pattern was to execute. Post-training, the modified pattern demonstrated an 8° increase in hip internal rotation and 3° increase in hip adduction. Knee adduction decreased 2°, and the knee adduction moment decreased 19%. Natural gait did not differ between the three visits, nor did the modified gait pattern between the post-training and 1 month visits. The modified pattern felt more natural and required less effort after training. Based on these results, gait retraining to improve dynamic knee alignment resulted in significant reductions in the knee adduction moment, primarily though hip internal rotation. Further, systematic training led to more natural-feeling and less effortful execution of the gait pattern.
Keywords: gait retraining, adduction moment, alignment, real-time feedback, varus
Introduction
The lifetime risk of symptomatic knee osteoarthritis (OA) is nearly 50% (Murphy et al., 2008). Therefore, preventative strategies targeting mechanical risk factors are important to develop. As a mechanical factor, varus knee alignment has been linked to incident medial knee OA (Brouwer et al., 2007), likely due to higher-than-normal medial knee joint forces (Andriacchi, 1994). As a surrogate measure for medial knee forces, the knee external adduction moment (KEAM) is often studied. The KEAM has been found to be 40% greater in varus-aligned, healthy knees than normally-aligned knees, values similar to those with established medial OA (Barrios et al., 2009a). The KEAM is also predictive of radiographic disease progression in diseased knees (Miyazaki et al., 2002).
A number of gait modifications are associated with a reduced KEAM. A 33% decrease in walking velocity reduces the KEAM by 10% (Mundermann et al., 2004). Increased foot progression angle reduces the second peak of the KEAM, but not the larger first peak (Andrews et al., 1996; Teichtahl et al., 2006; Lin et al., 2001; Guo et al., 2007; Hurwitz et al., 2002; Rutherford et al., 2008). Ipsilateral trunk lean can reduce the KEAM by 65% (Mundermann et al., 2008). However, this pattern appears abnormal and may increase the risk for back problems. Finally, Fregly et al. (2007, 2008) used a dynamic optimization method in a case study to derive a KEAM-minimizing gait pattern. The alterations involved pelvic obliquity and axial rotation, and flexion at the hip, knee and ankle to produce a ‘medial thrust’ of the knee. Reductions in the KEAM ranged from 39-50% (2007). In a follow-up case study using a force-measuring knee replacement, medial contact forces were reduced by 16% (Fregly et al., 2009).
Hip-driven alterations may be another approach to KEAM reduction. Previously, Davis (2005) described a case study in which a runner with patellofemoral pain was able to reduce her dynamic knee valgus by increasing hip external rotation and abduction. Based on these directional relationships, the opposite changes of increasing hip internal rotation and adduction may reduce knee adduction. As knee adduction angle and moment are correlated (Barrios et al., 2009b), these kinematics might reduce the KEAM.
A notable limitation of the previous gait modification studies is the lack of systematic training. Systematic training should lead to improved retention of the learned pattern, especially if extrinsic feedback mechanisms are initially provided to facilitate learning (Blandin et al., 2008), then later removed to help internalize the task (Winstein, 1991). As a gait pattern is internalized, performance should require less effort and feel more natural.
Therefore, our purpose was to test a KEAM-reducing gait retraining program in varus-aligned, healthy individuals. We expected increases in hip adduction and internal rotation would drive reductions in knee adduction and the KEAM both post-training and after 1 month. We also hypothesized that natural gait patterns would shift over time due to internalization of the learned pattern. Finally, with training, we hypothesized that the gait modification would require less effort and feel more natural.
Methods
Subjects
A sample size calculation for comparing the KEAM between sessions was conducted based on pilot work, using a reduction of 0.08 Nm/(kg*m). The analyses suggested that eight subjects would be sufficient (Cohen, 1988). Subjects were recruited from a university setting. Informed consents in accordance with the University of Delaware's Institutional Review Board were obtained.
All subjects were between 18-35 years of age, fit and healthy. Subjects were excluded if they reported any history of knee pathology. The Sports and Recreational Activities subscale of the Knee Injury and Osteoarthritis Outcome Score Survey (KOOS-SR) was administered (Roos et al., 1998). The KOOS-SR scores difficulty associated with five activities: squatting, running, jumping, twisting/pivoting and kneeling. Responses were based on the previous week, and recorded using a five-point Likert scale. A score of 0 indicated no difficulty, and a score of 4 indicated extreme difficulty. Potential subjects with scores greater than 2/20 were excluded.
Malalignment was clinically determined by measuring the mechanical axis of the tibia with respect to vertical with a caliper-inclinometer device (Acuangle, Isomed, Portland, OR, USA). This method is a valid alternative to the full-limb radiograph (Hinman et al., 2006). For the measurement, individuals stood in tandem stance in full knee extension. The proximal caliper arm was placed at the tibial tuberosity, and the distal arm over the neck of the talus (Figure 1). Tibial mechanical axis was then recorded to the nearest degree. To qualify for the study, the angle had to exceed or equal 11°. This value is 1.5 standard deviations above our normative database mean for this measure (30 healthy individuals, mean age 26.5 ± 6.1 years, mean tibial mechanical axis 8.0 ± 1.9°). The limb with greater malalignment was used for the study. If alignment was symmetrical, the test limb was chosen randomly.
Figure 1.

Clinical measurement of tibial mechanical axis with a caliper-inclinometer device using procedures modified from Hinman and colleagues (2006).
Subject comfort on a treadmill was then rated on a numerical scale, with 0/10 meaning totally uncomfortable and 10/10 meaning totally comfortable. A rating of less than 8/10 would exclude an individual from participating.
Initial Overground Gait Analysis
To establish baseline mechanics, natural walking trials were collected using an eight-camera Vicon (Oxford Metrics, UK) motion analysis system (120 Hz), calibrated over a collection volume measuring approximately 0.9 × 0.9 × 1.3 m. Twenty-nine spherical retroreflective (9 mm) markers were applied to the test limb. Anatomical markers were positioned over the iliac crests, greater trochanters, femoral condyles, tibial plateaus, malleoli, first and fifth metatarsal heads, and distal shoe (Nike Air Pegasus, Beaverton, OR). Individual tracking markers were placed over the anterior superior iliac spines, and the L5-S1 interspinous space. Three individual tracking markers were clustered on the rearfoot. Rigid clusters of four tracking markers were placed on the distal posterior shank and distal posterolateral thigh using an underwrap and an overwrap. A standing calibration trial was then collected. Next, a hip motion trial was collected to establish a functional hip joint center (average error = 1.34 cm) (Hicks & Richards, 2005). These were used to establish the pose for the pelvis, thigh, shank and foot coordinate systems (Grood & Suntay, 1983).
For the dynamic trials, the anatomical markers were removed, leaving fourteen tracking markers. Subjects traversed a floor-embedded force plate (BERTEC Corp., Worthington, OH, USA) (1080 Hz). Walking velocity along the 23 m walkway was monitored with two photoloelectric cells and maintained at 1.46 m/s (± 2.5%). Eight usable trials were collected, reconstructed and exported in C3D format.
Data processing was performed offline using Visual 3D (Version 3.91, C-Motion Inc, Rockville, MD, USA). A fourth-order, phase-corrected, low-pass Butterworth filter with a cut-off frequency of 8 Hz was applied to the marker data. Analog data were low-pass filtered at 50 Hz. Body segments were modeled as frustra of right cones, with inertial properties derived from the literature (Dempster et al., 1959). Joint angle data were derived using an X-Y-Z rotation sequence. Joint moments were expressed as external moments, referenced about the proximal end of the distal segment, and normalized to body mass (kg) and height (m). Custom-written software was used to extract the discrete variables of interest (Labview 8.2, National Instruments, Austin, TX, USA). These variables included the peak KEAM, knee adduction angle, hip adduction angle, and hip internal rotation angles. These variables were averaged over five trials per subject, and then averaged across subjects for each visit. To generate ensemble graphs, data were time-normalized to 100 points and averaged.
Gait Retraining Sessions
Eight gait retraining sessions were conducted. The calibrated volume, measuring approximately 1.3 × 1.8 × 1.5 m, was centered over an instrumented treadmill. An eight-camera VICON (Oxford Metrics, UK) motion analysis system was used (100 Hz). Markers were applied in the same manner as the overground collection. Additional markers were added to the anterior thigh, anterior shank, and over the 2nd metatarsal head. A standing calibration trial was collected to identify markers in the VICON Nexus system, and to establish segmental coordinate systems in Visual 3D Professional. The same anatomical markers were removed, except the ipsilateral iliac crest marker. The additional tracking markers provided segment redundancy to all but eliminate segment loss in real-time.
The subject then began the treadmill protocol. A comfortable walking speed was determined during a two-minute warm-up. This speed was held constant for all subsequent sessions. Subjects walked on a single belt of the side-split instrumented treadmill, as split-belt walking induces a wider base of gait and may thus influence kinematics. No attention was drawn to the split. To identify stance, a kinematic method utilizing the anterior-posterior velocity of the foot segment relative to the pelvis was used (Zeni et al., 2008). The relative positive-to-negative zero crossing of the foot segment velocity identified the start of stance. Similarly, the negative-to-positive zero crossing identified the end of stance.
The subject was then provided visual feedback on a video monitor positioned approximately 1.5 m anterior to the treadmill. As a subject walked, their frontal plane knee angle was displayed and refreshed with each footstrike. Subjects were instructed to lower their stance-phase curve so that it fell within a shaded region that represented one standard deviation of a normative database mean (Figure 2). Each subject was instructed to “bring your thighs inward” and “walk with your knees closer together.” The subjects were also reminded to maintain a normal foot progression angle. Verbal cueing was limited to the first five minutes of each session. A fading feedback design was used across sessions (Figure 3). This type of schedule was devised so as to gradually integrate task acquisition and task transfer to help internalize a learned skill (Winstein, 1991).
Figure 2.
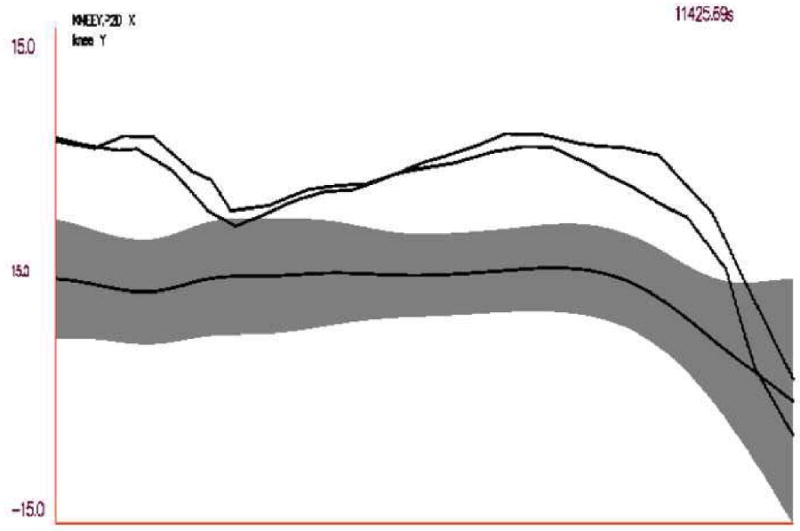
Actual screen image depicting the knee adduction angle data of a varus-aligned subject during training against a shaded region representing ± 1 standard deviation of a normative mean for knee adduction angle. Knee adduction is positive, and the previous two stance-phases are shown. Note the downward deflection in knee adduction angle in early stance, around the same time that peak KEAM occurs.
Figure 3.
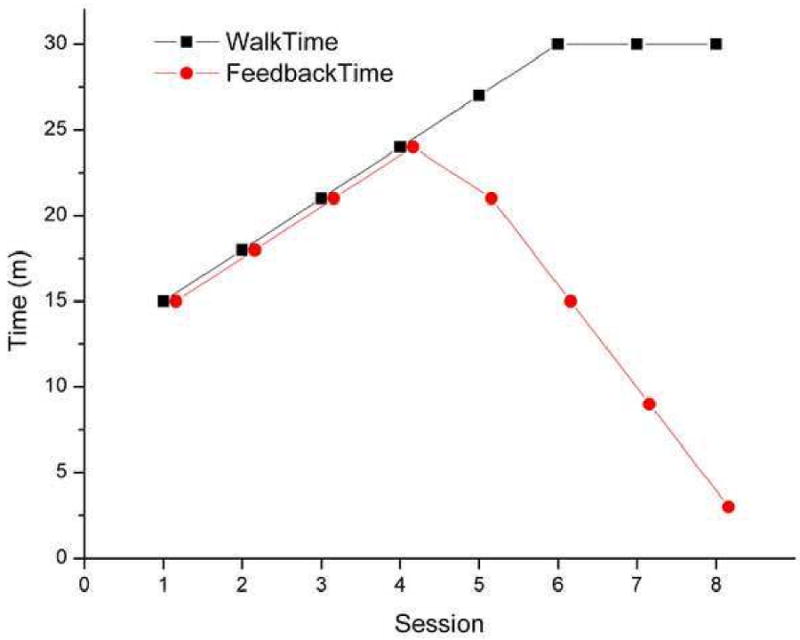
Chart depicting time spent walking on the treadmill during each session, and the respective time with visual feedback for each session. For the first four sessions, subjects received feedback 100% of the session. By visit 8, feedback was provided for 10% the session.
Subjective feedback was recorded at the end of each session. Subjects rated their perception of effort required to execute the modified pattern on a numerical scale. A score of 0/10 meant that the pattern was effortless to execute, and 10/10 meant the gait pattern required maximal effort. Subjects also rated how natural the modified pattern felt, where 10/10 was maximally unnatural and 0/10 was completely natural. Finally, subjects reported the percentage of their walking since the previous session during which they used the modified pattern.
Post-Training and 1 Month Overground Gait Analyses
Overground gait analyses were again performed post-training and at a 1-month follow-up. Subjects were first asked to walk naturally, and then with the modified pattern. The natural pattern was collected to determine whether it had changed from baseline. The how effortful and natural the modified pattern felt was also recorded.
Data Analysis
The post-training and 1-month modified patterns were compared to the baseline mechanics using single-factor repeated measures ANOVAs. Planned pairwise comparisons between the visits were conducted. In addition, subjective data reported for perceived effort and naturalness at training sessions 1 and 8 were compared with paired samples t-tests. Statistical significance was attained at the p≤0.05 level. Statistical trends were identified at the 0.10≥p>0.05 level.
Results
The subject demographics are presented in Table 1. Seven of the eight subjects were male. All subjects were healthy, asymptomatic, and completed the protocol without any adverse events. Soreness over the ipsilateral greater trochanter was reported by two subjects in the beginning of the protocol, which resolved by the third session.
Table 1.
Subject demographics.
| Mean (SD) | |
|---|---|
| Age (years) | 21.4 (1.6) |
| Height (m) | 1.75 (0.07) |
| Weight (kg) | 71.7 (8.8) |
| Tibial Mechanical Axis (°) | 11.5 (0.8) |
| Treadmill Comfort Rating (0-10) | 9.8 (0.5) |
| KOOS-SR Score (0-20) | 0.7 (0.9) |
Comparing the post-training modified gait data to baseline, a 20% average reduction (p=0.027) in peak KEAM was seen (Table 2). The 2° average reduction in knee adduction trended towards significance (p=0.071). All subjects increased their peak hip internal rotation, by nearly 8° on average (p=0.001). A trend towards an increase in hip adduction (3°) was noted (p=0.073).
Table 2.
Natural and modified gait mechanics for the overground visits (mean ± standard deviation. Note the consistency between and within the two patterns.
| Variable | Baseline | Post-training | 1 month | |||
|---|---|---|---|---|---|---|
| Natural | Modified | Natural | Modified | Natural | Modified | |
| Knee adduction moment (Nm/kgm) | 0.426 ± 0.065 | --- | 0.423 ± 0.049 | 0.340 ± 0.066 | 0.441 ± 0.055 | 0.340 ± 0.073 |
| Knee adduction angle (degrees) | 6.8 ± 2.4 | --- | 6.2 ± 2.2 | 5.0 ± 2.1 | 6.6 ± 1.4 | 5.5 ± 2.2 |
| Hip internal rotation (degrees) | 5.3 ± 7.4 | --- | 5.4 ± 6.0 | 13.5 ± 8.5 | 6.0 ± 6.7 | 12.8 ± 9.2 |
| Hip adduction (degrees) | 9.2 ± 2.4 | --- | 8.8 ± 3.1 | 12.3 ± 3.5 | 8.9 ± 3.1 | 11.3 ± 3.0 |
Italics denotes significant reduction from baseline
Comparing the 1 month modified gait data to baseline, subjects again walked with a 20% decreased KEAM (p=0.019). For hip internal rotation, the average increase was 8° (p=0.033). Hip adduction increased by 2° on average, although this was not statistically significant (p=0.210). On average, peak knee adduction decreased only 1° (p=0.276).
Comparing the modified gait between the post-training and 1-month visits, no differences were detected. When comparing baseline natural gait to the natural pattern at both follow-ups, it was clear that natural gait patterns did not change (Table 2).
During the training protocol, how effortful and natural-feeling the pattern felt improved from session 1 to session 8 by greater than 3/10 (Figure 4). This change was significant for effort (p<0.001) and naturalness (p=0.001). The average percentage of walking between sessions during which subjects used the modified pattern was 11% (Figure 6).
Figure 4.
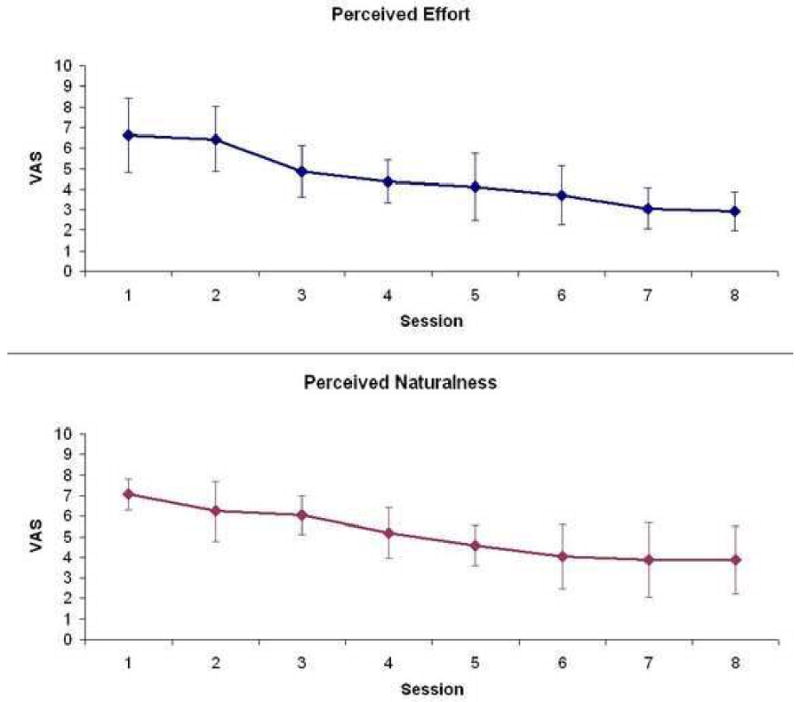
How effortful and natural-feeling the modified gait pattern was perceived across training sessions. Effort: 0 = effortless, 10 = maximal effort. Naturalness: 0 = natural, 10 = maximally unnatural. Error bars depict standard deviations.
Figure 6.
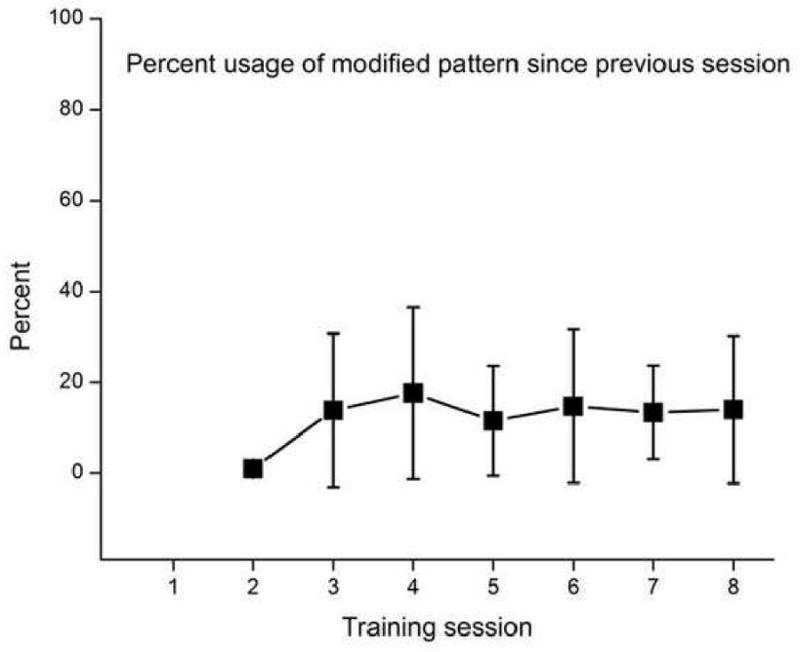
Average percentage of walking between training sessions during which subjects reported using the modified pattern. Error bars depict standard deviations.
Discussion
The primary purpose of this experiment was to examine the effectiveness of a systematic gait retraining program aimed at reducing the KEAM. Young and healthy varus-aligned individuals were targeted as they are predisposed for incident knee OA, but have a greater ability to learn novel locomotor tasks than older individuals (van Hedel et al., 2004). In this study, the male cohort bias was notable and unplanned, but seems to suggest that varus malalignment is more prevalent in males. The training utilized real-time visual feedback on the frontal plane knee angle, with verbal feedback emphasizing the use of hip adduction and internal rotation to reduce knee adduction (Figure 5). Fading feedback over multiple sessions was implemented to help internalize the modifications (Winstein, 1991).
Figure 5.
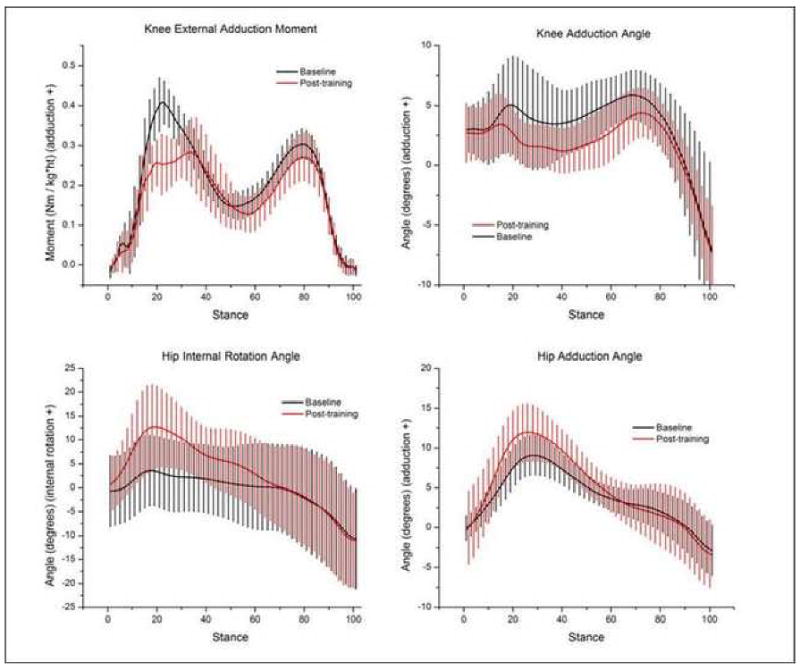
Ensemble averaged curves comparing the modified gait post-training to the baseline visit, depicting decreases in KEAM and knee adduction, and increases in hip adduction and internal rotation. Error bars depict standard deviations.
On average, the retraining produced a 20% reduction in the KEAM. The baseline KEAM magnitudes (0.43 Nm/(kg*m)) were slightly greater than reported for those with established medial knee OA (0.38 Nm/(kg*m)) using nearly identical methods (Butler et al., 2007). These data suggest that the KEAM is aberrantly high in healthy varus knees, and likely contributes to the development of medial knee OA. Therefore, the 20% reduction is meaningful. Subjects were able to reduce their KEAM through hip-driven kinematic modifications, as hypothesized. It was clear that subjects used hip internal rotation, and to a lesser degree, hip adduction to accomplish this. Knee adduction kinematics were less responsive, although some directional shift was noted. This is reasonable, as only a small amount of range of motion is available in the frontal plane of the knee.
Further exploration of the data revealed two other kinematic changes of interest. First, knee flexion at the end of weight acceptance was increased in the modified gait pattern, with a mean increase of 12°. A similar phenomenon was reported using the ‘medial-thrust’ pattern advocated by Fregly et al. (2007, 2008, 2009). This increase in knee flexion appeared to facilitate the reductions in knee adduction during stance, as no subjects produced the desired changes without greater knee flexion. The second alteration was a 9° increase in foot abduction. This finding is attributable to our instruction to maintain a normal foot progression angle. In global, internal rotation of the thigh segment resulted in internal rotation of tibia. In order to maintain a normal foot progression angle, an increased foot abduction angle was used.
The retraining protocol did not alter natural gait. This result differs with the case study by Fregly and colleagues (2007). In their study, the trained individual was unable to revert back to his pre-training gait. However, the trained individual was highly knowledgeable regarding gait mechanics, and practiced the gait alteration for nine months before reassessment. This is a long period, and it is unclear as to when the altered pattern became the more ‘natural’ one. If the goal of the gait retraining intervention is the true alteration of natural walking patterns, a more intensive or lengthy protocol may be required.
While all subjects appeared to execute the modified pattern with ease at the post-training visit, we were interested in whether this ability would be maintained at the 1 month follow-up. Interestingly, all subjects were able to execute the modified pattern. This suggests that the systemic training was effective for both short-term performance and longer-term retention. It should be noted that the subjects were asked to walk with the modified pattern as much as possible during the follow-up period. Despite this, the reported usage was generally poor. However, this did not appear to affect their ability to reproduce the modified pattern.
Subjectively, the systematic training led to easier execution of the pattern. During the training, the modified gait pattern became less effortful to perform. This is a promising finding suggesting that continued reinforcement could eventually make the modified pattern ‘effortless’, a presumed characteristic of natural gait. The modified pattern also became significantly more natural-feeling. Although significant improvements were observed in these factors, we should note that neither approximated zero. However, these data suggest that a longer or more intensive training protocol might result in the modified pattern feeling quite natural, and being effortless to perform.
The observed reductions were greater than those previously reported for lateral wedging and knee bracing. The predominant benefit of gait modification is that it does not require an external device. However, the difficulty in implementation appears to be its internalization, and motivation for subsequent use. These challenges mirror the compliance issues seen in nearly all OA interventions (Carr et al., 2001). The compliance to an intervention tends to improve if patients can perceive a positive change, such as pain reduction. Therefore, individuals with symptomatic medial compartment pathology who experience symptom amelioration may have greater motivation to alter their gait patterns than the healthy individuals in the current study. Another means to increase usage would be to reinforce the pattern on a continual basis. Some form of mobile monitoring or stimulation could lead to improved compliance, and ultimately, towards to the true alteration of natural walking patterns.
In conclusion, the gait modification significantly reduced the KEAM. This reduction was driven by hip internal rotation and adduction. Although natural gait was not altered, execution of the modified pattern required less effort and felt more natural with the training. The modified pattern was easily performed post-training and after 1 month, suggesting some level of internalization. Based on these results, the proposed gait modification and systematic training provide a potentially powerful approach to reducing medial knee joint loads during gait.
Acknowledgments
This study was supported by the American Society of Biomechanics student grant-in-aid award, and National Institutes of Health shared instrumentation grant 1 S10 RR022396-01.
Footnotes
Conflict of Interest Statement: There are no financial or personal relationships with other people or organizations that could inappropriately bias this work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kay M. Crossley, Department of Mechanical Engineering, Melbourne School of Engineering, University of Melbourne, 3010 Australia, k.crossley@unimelb.edu.au.
Irene S. Davis, 305 McKinly Lab, University of Delaware, Newark, DE 19716, 302-831-4263, mcclay@udel.edu.
References
- Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, Dragomir A, Kalsbeek WD, Luta G, Jordan JM. Lifetime risk of symptomatic knee osteoarthritis. Arthritis & Rheumatism. 2008;59:1207–1213. doi: 10.1002/art.24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer GM, van Tol AW, Bergink AP, Belo JN, Bernsen RMD, Reijman M, Pols HAP, Bierma-Zeinstra SMA. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis & Rheumatism. 2007;56:1204–1211. doi: 10.1002/art.22515. [DOI] [PubMed] [Google Scholar]
- Andriacchi TP. Dynamics of knee malalignment. Orthopedic Clinics North America. 1994;25:395–403. [PubMed] [Google Scholar]
- Barrios JA, Davis IS, Higginson JS, Royer TD. Lower extremity walking mechanics of young individuals with asymptomatic varus knee alignment. Journal of Orthopaedic Research. 2009 doi: 10.1002/jor.20904. [DOI] [PubMed] [Google Scholar]
- Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Annals of Rheumatic Disease. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundermann A, Dyrby CO, Hurwitz DE, Sharma L, Andriacchi TP. Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity. Arthritis & Rheumatism. 2004;50:1172–1178. doi: 10.1002/art.20132. [DOI] [PubMed] [Google Scholar]
- Andrews M, Noyes FR, Hewett TE, Andriacchi TP. Lower limb alignment and foot angle are related to stance phase knee adduction in normal subjects: a critical analysis of the reliability of gait analysis data. Journal of Orthopaedic Research. 1996;14:289–295. doi: 10.1002/jor.1100140218. [DOI] [PubMed] [Google Scholar]
- Teichtahl AJ, Morris ME, Wluka AE, Baker R, Wolfe R, Davis SR, Cicuttini FM. Foot rotation—a potential target to modify the knee adduction moment. Journal of Science in Medicine & Sport. 2006;9:67–71. doi: 10.1016/j.jsams.2006.03.011. [DOI] [PubMed] [Google Scholar]
- Lin C, Lai K, Chou Y, Ho C. The effect of changing the foot progression angle on the knee adduction moment in normal teenagers. Gait & Posture. 2001;14:85–91. doi: 10.1016/s0966-6362(01)00126-6. [DOI] [PubMed] [Google Scholar]
- Guo M, Axe MJ, Manal K. The influence of foot progression angle on the knee adduction moment during walking and stair climbing in pain free individuals with knee osteoarthritis. Gait & Posture. 2007;26:436–441. doi: 10.1016/j.gaitpost.2006.10.008. [DOI] [PubMed] [Google Scholar]
- Hurwitz DE, Ryals AB, Case JP, Block JA, Andriacchi TP. The knee adduction moment during gait is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. Journal of Orthopaedic Research. 2002;20:101–107. doi: 10.1016/S0736-0266(01)00081-X. [DOI] [PubMed] [Google Scholar]
- Rutherford DJ, Hubley-Kozey CL, Deluzio KJ, Stanish WD, Dunbar M. Foot progression angle and the knee adduction moment: a cross-sectional investigation in knee osteoarthritis. Osteoarthritis & Cartilage. 2008;16:883–889. doi: 10.1016/j.joca.2007.11.012. [DOI] [PubMed] [Google Scholar]
- Mundermann A, Asay JL, Mundermann L, Andriacchi TP. Implications of increased medio-lateral trunk sway for ambulatory mechanics. Journal of Biomechanics. 2008;41:165–170. doi: 10.1016/j.jbiomech.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Fregly BJ, Reinbolt JA, Rooney KL, Mitchell KH, Chmielewski TL. Design of a patient-specific gait modifications for knee osteoarthritis rehabilitation. IEEE Transactions on Biomedical Engineering. 2007;54:1687–1695. doi: 10.1109/TBME.2007.891934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fregly BJ. Computational assessment of combinations of gait modifications for knee osteoarthritis rehabilitation. IEEE Transactions on Biomedical Engineering. 2008;55:2104–2106. doi: 10.1109/TBME.2008.921171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fregly BJ, D'Lima DD, Coldwell CW. Effective patterns for offloading the medial compartment of the knee. Journal of Orthopaedic Research. 2009 doi: 10.1002/jor.20843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis IS. Gait retraining in runners. Orthopedic Practice. 2005;17:8–13. [Google Scholar]
- Barrios JA, Higginson JS, Royer TD, Davis IS. Static and dynamic correlates of the knee adduction moment in healthy knees ranging from normal to varus-aligned. Clinical Biomechanics. 2009 doi: 10.1016/j.clinbiomech.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blandin Y, Toussaint L, Shea CH. Specificity of practice: interaction between concurrent sensory feedback information and terminal feedback. Journal of Experimental Psychology. 2008;34:994–1000. doi: 10.1037/0278-7393.34.4.994. [DOI] [PubMed] [Google Scholar]
- Winstein CJ. Knowledge of results and motor learning—implications for physical therapy. Physical Therapy. 1991;71:140–149. doi: 10.1093/ptj/71.2.140. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS) -- development of a self-administered outcome measure. Journal of Orthopaedic & Sports Physical Therapy. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- Hinman RS, May RL, Crossley KM. Is there an alternative to the full-length radiograph for determining knee joint alignment in osteoarthritis? Arthritis & Rheumatism. 2006;55:306–313. doi: 10.1002/art.21836. [DOI] [PubMed] [Google Scholar]
- Hicks JL, Richards JG. Clinical applicability of using spherical fitting to find hip joint centers. Gait & Posture. 2005;22:138–145. doi: 10.1016/j.gaitpost.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. Journal of Biomechanical Engineering. 1983;105(2):136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- Dempster WT, Gabel WC, Felts WJ. The anthropometry of the manual work space for the seated subject. American Journal of Physical Anthropology. 1959;17:289–317. doi: 10.1002/ajpa.1330170405. [DOI] [PubMed] [Google Scholar]
- Zeni JA, Ricahrds JG, Higginson JS. Two simple methods to determine gait events during treadmill and overground walking using kinematic data. Gait & Posture. 2008;27:710–714. doi: 10.1016/j.gaitpost.2007.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hedel HJA, Dietz V. The influence of age on learning a locomotor task. Clinical Neurophysiology. 2004;115:2134–2143. doi: 10.1016/j.clinph.2004.03.029. [DOI] [PubMed] [Google Scholar]
- Butler RJ, Marchesi S, Royer T, Davis IS. The effect of a subject-specific amount of lateral wedge on knee mechanics in patients with medial knee osteoarthritis. Journal of Orthopaedic Research. 2007;25:1121–1127. doi: 10.1002/jor.20423. [DOI] [PubMed] [Google Scholar]
- Carr A. Barriers to the effectiveness of any intervention in OA. Best Practice & Research: Clinical Rheumatology. 2001;15:645–656. doi: 10.1053/berh.2001.0179. [DOI] [PubMed] [Google Scholar]


