Abstract
Native Hawaiians have a high cancer burden, but few culturally targeted cancer education brochures exist. The authors followed a participatory four-step protocol, involving more than 200 health providers and clients, to develop and test culturally targeted brochures on skin, oral, cervical, prostate, and testicular cancers. The final products featured Hawaiian faces, scenes, words, and activities. They proved more attractive than existing materials, in particular to younger Hawaiians, and posttests suggested good comprehension of intended messages. This protocol may have application in other communities that want to develop brochures that are attractive, acceptable, readable, and useful to minority clients and their providers.
Keywords: action research, consumer participation, culture, focus groups, Hawai'i, health promotion, indigenous population, information dissemination, neoplasm, Pacific Islander Americans
Native Hawaiians are the indigenous people of Hawai'i. They make up 23% of the state's population; other major ethnic groups in the state include Caucasians (24%), Japanese (22%), and Filipinos (15%) (see http://www3.hawaii.gov/DBEDT/index.cfm). Looking across ethnic groups, the cancer burden is higher among Native Hawaiians (see http://www.cancer.org/docroot/home/index.asp; Hawai'i Department of Health, 2004). For example, for the years 1995 through 2000, male cancer mortality rates were 220 per 100,000 for Native Hawaiians (compared with 199 for Caucasian men), and female cancer mortality rates were 193 per 100,000 for Native Hawaiians (compared with 135 for Caucasian women). Despite high rates of cancer mortality among Native Hawaiians, there were few cancer-related education materials for Native Hawaiians in 2000. Given that brochures are known to play a role in increasing cancer awareness (Doak, Doak, & Root, 1985; Flay, DiTecco, & Schlegel, 1980; National Cancer Institute [NCI], 1998), this article describes a four-step process for developing and testing cancer brochures for this population.
Background
'Imi Hale–Native Hawaiian Cancer Network ('Imi Hale) is one of 25 community network programs funded by the NCI Center to Reduce Cancer Health Disparities to both increase cancer prevention and control among Native Hawaiians and support the development of indigenous researchers. 'Imi Hale's work is guided by principles of community-based participatory research (CBPR), which require that activities follow community-set priorities, build on community strengths, and provide tangible benefits (Matsunaga et al., 1996; Minkler & Wallerstein, 2003). In 'Imi Hale's first year (2000), more than 900 individuals in the state (50+ Native Hawaiian cancer survivors, 500+ Native Hawaiian Health Care System clients, 200+ primary care physicians and oncologists, and 150+ nonphysician providers of health and social services in Hawaiian communities) participated in surveys, interviews, and focus groups to identify program priorities (Braun, Tsark, Santos, Aitaoto, & Chong, 2006). The need for culturally targeted cancer education materials was identified as one of five priorities for the project. Between 2000 and 2003, brochures featuring Native Hawaiian faces and quotes were developed for breast cancer, colorectal cancer, and smoking cessation. In 2004, Hawaiian health partners requested brochures for skin, prostate, testicular, cervical, and oral cancers, which are cancers that can be screened for (unlike ovarian cancer) to supplement their cancer prevention and screening activities in the community (Gellert, Braun, Starkey, & Morris, 2006).
Providing health education is an essential first step in consumer participation in health care, and brochures have a role in changing health knowledge, attitudes, intentions, and behaviors (Kreuter & Wray, 2003; Paul, Redman, & Sanson-Fisher, 2003, 2004). For example, individuals randomly assigned to receive pamphlets about oral cancer significantly increased their knowledge about oral cancer and their intentions to get screened for it over individuals in the control group (Boundouki, Humphris, & Field, 2004). Individuals receiving booklets about skin cancer were more likely to increase their knowledge about skin cancer prevention than individuals who did not receive brochures (Richard et al., 1999). In a study about prostate cancer, men who received an education brochure scored higher on a knowledge test and were more likely to discuss screening with their providers compared with men who did not receive the brochure (Partin et al., 2004). Chinese immigrant women who received culturally appropriate education materials by mail were more likely than those in the control group to subsequently participate in cervical cancer screening (Taylor et al., 2002). Recipients of a booklet on testicular cancer dramatically increased their self-screening practices, and these practices were maintained 2 years after receiving the booklet (Klein, Berry, & Felice, 1991).
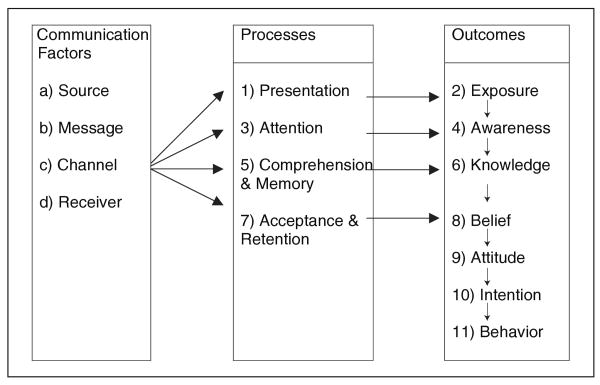
According to the Information Processing Model, to be effective, brochures first must catch the attention of the consumer (Flay et al., 1980). This 11-step model (see Figure 1) suggests that a brochure must be presented in a way that captures the person's attention (Step 1) so that he or she can be exposed to the message (Step 2). When the message is attended to (Step 3), exposure will lead to awareness (Step 4). A consideration in this step is the readability and suitability of materials for the target group. If the message is comprehended (Step 5), then the message can lead to changes in knowledge (Step 6). If the arguments or conclusions of the message are accepted or yielded to (Step 7), this can lead to changes in beliefs (Step 8), which can lead to changes in attitudes (Step 9), changes in intentions (Step 10), and finally, changes in behavior (Step 11).
FIGURE 1. Information Processing Model.
SOURCE: Flay, DiTecco, and Schlegel (1980).
To develop brochures that grasp the reader's attention and transfer knowledge, developers must gather data from the target group on a number of communication factors. The chosen medium must be appropriate for the message and the audience, the information must be seen as coming from a credible source, there must be congruence between the message text and graphics, the look should be culturally appealing, and the message must be clear so that the audience comprehends its learning and behavioral intentions (Brandt, McCree, Lindley, Sharpe, & Hutto, 2005; Doak et al., 1985; Flay et al., 1980; Hunter, 2005; Meade, 2005; NCI, 1998; Solomon et al., 2005; Taylor et al., 2002). Looking specifically at cancer messages, research suggests that individuals want cancer messages that give them hope for preventing cancer and that use neutral terms (e.g., the word risk raises alarm, whereas the word chance minimizes it; NCI, 1998; Richard et al., 1999). Visuals, when used properly, can be effective in transmitting complex information, reinforcing the printed message, and engaging the viewer when the visual is perceived as being culturally relevant and attractive. Visuals that accompany brief text increase attention and understanding over text or visuals alone. It is important also to include information on risk, screening recommendations, and where to get additional information. Formative research strategies, such as focus groups, are helpful in learning audience preferences for credible sources of health information, effective messaging, and the look of the educational materials (Morgan & Krueger, 1998; Solomon et al., 2005). Draft materials must be tested for attractiveness, as well as for readability and message comprehension (Doak et al., 1985; NCI, 1998).
Greater attention is being paid to targeting messages to specific cultures (Guidrey & Walker, 1999; Hunter, 2005; Kreuter & Wray, 2003; Meade, 2005; Solomon et al., 2005; Taylor et al., 2002) and Kreuter and colleagues recommend five strategies: (a) peripheral strategies, using designs and photos that are attractive to the ethnic group; (b) evidential strategies, presenting evidence of the relevance of the problem to the culture; (c) linguistic strategies, using words and phrases from the group's language; (d) constituent-involving strategies, such as drawing directly on the experience of members of the ethnic group; and (e) sociocultural strategies, recognizing and working from the group's cultural values, beliefs, behaviors, and context (Kreuter, Lukwago, Bucholtz, Clark, & Sanders-Thompson, 2003).
Several values, traditions, and experiences should be considered when developing interventions and educational messages for Native Hawaiians. Their worldview is defined by salient cultural concepts, including 'āina (the land), 'ohana (extended family), kōkua (cooperation, helpfulness), and ha'aha'a (humility). As in most cultures, familial affiliations ('ohana) are important. The well-being of the family ('ohana) and the group usually takes precedence over that of the individual, who refrains from calling attention to himself or herself (ha'aha'a). Emphasis is placed on caring for each other (mālama kekahi i kekahi) and contributing (kōkua) in ways that are appropriate to a person's age and skill level (Braun, Mokuau, Hunt, Ka'ano'i, & Gotay, 2002; Pukui, Haertig, & Lee, 1979). Health education interventions that incorporate cultural values have been found to be successful in increasing screening rates among Native Hawaiians. For example, women who received educational materials featuring Hawaiian themes through kōkua groups reported positive changes in cancer screening behaviors, whereas women in the control group did not (Gotay et al., 2000).
Our primary objective was to develop culturally relevant brochures for Native Hawaiians, understanding that increasing awareness and knowledge about cancer through brochures can contribute to behavior change. In this article, we describe the development and testing process. Lessons learned from our endeavor may help other communities develop more effective brochures for their own populations.
Method: The Four-Step Protocol
A four-step protocol was used to develop and test cancer education brochures for five cancer sites: skin, oral, cervical, prostate, and testicular. Brochures on these cancers were requested by community health partners, who earlier had received brochures developed by 'Imi Hale for breast cancer, colorectal cancer, and smoking cessation. The four steps are as follows: (a) draft brochures based on information gained through literature review and focus groups; (b) secure technical review and preliminary endorsement of brochures from health information specialists and physicians; (c) test the brochures with consumers in the community; and (d) obtain final review and endorsement (see Table 1). Each step required a different methodological approach, and brochures were refined several times within each step. A verbal consent process was used at each step, as approved by the Native Hawaiian Health Care System Institutional Review Board.
TABLE 1. Four-Step Protocol for Development and Testing of Culturally Targeted Cancer Brochures.
| Step | Method |
|---|---|
| 1. Draft brochures | |
| Determine source, message, format, and operationalize cultural-targeting strategies | Held focus groups with 45 providers at three community health centers |
| Conduct initial reading level tests | Used Fry test to assess reading level |
| 2. Conduct technical review and obtain preliminary endorsement | |
| Consult with cancer experts | Met with Cancer Information Service–Hawai'i |
| Consult with physicians | Surveyed 10 physician members of 'Ahahui O Nā Kauka (Association of Native Hawaiian Physicians); physicians endorsed refined draft |
| 3. Conduct consumer testing and reinforcement | |
| Consult with providers | Conducted one-on-one structured interviews with 58 providers at seven community health centers |
| Consult with clients | Conducted one-on-one structured interviews with 83 clients at seven community health centers |
| Conduct revision and final readability test | Used Fry test to assess reading level |
| 4. Conduct final review and obtain final endorsement | |
| Consult with health center staff representatives | Staff representatives from five health care centers (one on each island) ranked final product on seven closed-ended items |
| Consult with physician representatives | 'Ahahui O Nā Kauka board members reviewed and endorsed final product |
Step 1: Draft Brochures Through Literature Review and Focus Groups
Drafts of five cancer education brochures were developed, which included factual information on skin, oral, cervical, prostate, and testicular cancers gleaned from Web sites of the NCI (2004), ACS (http://www.cancer.org/docroot/home/index.asp), and the Hawai'i Department of Health (2004). As recommended in health communication literature, information was presented in lay terms, avoiding complicated charts and medical jargon (Doak et al., 1985; Flay et al., 1980; NCI, 1998). Attention was paid to both readability and format, so that the brochure message clearly defined (a) the purpose of the brochure, (b) information about recommended screening tests and recommended frequency of screening tests, and (c) behaviors desired from the reader. Brochures were tested for reading grade level using the Fry Readability Test (Fry, 1968).
Five focus groups were conducted to help target the brochures, engaging 45 health care providers from three O'ahu-based community health centers serving Native Hawaiians. These centers were willing to host focus groups because of similarity in mission and long-time working relationships between them and 'Imi Hale. Eighty percent (n = 36) of focus group participants were Native Hawaiian, and 71% (n = 32) were female. In terms of age, 36% were between 18 and 39 years, 60% were between 40 and 59 years, and only 7% (n = 3) were 60 years or older. Almost one fourth reported having had a cancer diagnosis themselves, and 60% reported having family members with cancer currently or in the past (see Table 2).
TABLE 2. Characteristics of Participants in Focus Group Research and Consumer Testing.
| Participants in Consumer Testing | |||
|---|---|---|---|
| Participants in Focus Groups (n = 45) n (%) |
Providers (n = 58) n (%) |
Clients (n = 90) n (%) |
|
| Age distributiona | |||
| 18-39 | 15 (33.3) | 25 (43.1) | 14 (15.6) |
| 40-59 | 27 (60.0) | 30 (51.7) | 19 (21.1) |
| 60+ | 3 (6.7) | 3 (5.2) | 50 (55.6) |
| Female gender | 32 (71.1) | 43 (74.1) | 61 (67.8) |
| Native Hawaiian | 36 (80.0) | 45 (77.6) | 75 (83.3) |
| Cancer experience | |||
| Self | 11 (24.4) | 12 (20.7) | 16 (17.8) |
| Family | 27 (60.0) | 33 (56.9) | 49 (54.4) |
| Island | |||
| Hawai'i | — | 8 (13.8) | 15 (16.7) |
| Kaua'i | — | 10 (17.2) | 12 (13.3) |
| Maui | — | 8 (13.8) | 18 (20.0) |
| Moloka'i | — | 6 (10.3) | 16 (17.8) |
| O'ahu | 45 (100.0) | 26 (44.8) | 29 (32.2) |
Seven clients did not provide data on age.
Each of the five focus groups convened 6 to 10 individuals. Groups were held at lunch, with food provided by 'Imi Hale, and lasted 90 minutes. Groups were conducted in English and were moderated by the principal investigator (MK), a young Native Hawaiian man, assisted by a young Native Hawaiian female research associate. Both received training in conducting focus groups from the coinvestigators (KB, JT). Using our brochure drafts as something participants could respond to and critique, four questions were asked: (a) What is the best source of the message? For example, what images or faces should appear on the cover? If you don't like this picture, what would be better? What endorsements would be credible? Should brochures stand alone or be part of a series? (b) How should the content, structure, and style of the brochure be arranged? For example, does simple wording with several pictures make the brochure more acceptable? Should people be depicted through illustrations or photographs? Which part of the body do you think this anatomical diagram represents? (c) Should Native Hawaiian values and beliefs be considered in developing the brochure, and if so, which ones? and (d) How and where should brochures be distributed to Native Hawaiians? As each question was discussed, the research associate recorded answers on posted newsprint. After each group, the investigators and research associate discussed and summarized the findings, noting the approximate percentage of the group that spoke to each theme. Similar themes and preferences emerged across groups, and modifications to the brochures were made based on the summary of findings. For example, confusion about diagrams showing the prostate and testes prompted us to show more of the body's torso and add appropriate captions to the diagram.
Step 2: Technical Review and Preliminary Endorsement
The next versions of the brochures were reviewed by the Cancer Information Services (CIS) of Hawai'i for technical accuracy. Corrections and suggestions were incorporated, and new drafts were presented to members of the Association of Native Hawaiian Physicians ('Ahahui O Nā Kauka) for expert review. Involvement of the Native Hawaiian physicians was deliberate, as physicians have a strong influence on patients as an authority to enforce and reinforce health behavior change. At one of their regularly scheduled meetings, 10 Native Hawaiian physicians, including 9 internists and 1 oncologist, reviewed the brochures and provided written responses to questions related to the accuracy and appropriateness of the anatomical diagrams and the information on cause, prevention, and recommended screening. Some wrote comments directly on the brochures. The PI incorporated the recommendations, and subsequent drafts of the brochures were reviewed by the board of the 'Ahahui O Nā Kauka, which voted to provide a preliminary endorsement.
Step 3: Consumer Testing and Reinforcement
The fourth versions of the brochures were reviewed first with 58 health care providers serving Native Hawaiians and, after another revision, with 90 consumers from seven community health centers serving Native Hawaiians. A community outreach worker was identified as a liaison from each agency, and there was high motivation to participate because this initiative was in response to their requests for culturally tailored cancer education materials. In addition, the centers knew they would receive a supply of finished brochures for their clientele. Consumer testing was led by the PI, who conducted 90% of the one-on-one interviews. He was assisted by two Native Hawaiian summer research interns; all three were trained by the coinvestigators in the interview protocol (described below).
As shown in Table 2, providers and clients in the testing phase were similar on gender distribution (about 74% female) and percentage who had had cancer (about 20%) and reported cancer in their families (about 58%). Compared with the health care providers group, the client group had a larger percentage of Native Hawaiians (90% vs. 78%), and there were significantly more clients in the 60+ age group (61% vs. 5%). All interviews were conducted in English, and all participants received a small makana (gift) in appreciation of their time.
Testing with health care providers
Each brochure was reviewed by at least five providers and feedback was solicited through one-on-one interviews. On average, each provider reviewed three of the five brochures, for a minimum of 35 completed reviews per brochure. To test attractiveness and acceptability, our brochures were displayed side-by-side with a selection of brochures on the same topic developed by other agencies. The provider was allowed to choose from the selection and then was queried as to why he or she chose that particular brochure from among the others. Focusing on our brochure, the participant was asked about the title and the cover photograph. Alternative brochure titles and photos were shared and discussed to see if the participant found the alternatives more appealing.
The participant was asked to comment on the anatomical diagrams and pictures, for example, “In your own words, can you tell me what this diagram is? Is this diagram or picture offensive in any way?” Recommendations were solicited with regard to how diagrams could be changed or adapted to increase the clarity and appropriateness of the message. We then asked about the written content of the brochure, focusing on how to improve readability and comprehension. Specific questions were posed about format, including color schemes, print font size, white space (areas with no text), and overall density. Learner verification to assess if the intended message was transmitted to the reader was done by asking questions specific to the facts presented in the brochure, for example, “Who should be screened?” “How is screening done?” and “When should screening occur?” Finally, the participant was asked to rate the usefulness of the brochure and his or her willingness to share it with others. One-on-one interviews lasted 30 minutes, during which time, three to five brochures could be reviewed by a single staff person.
Testing with clients
After another revision, the brochures were then reviewed by seven or eight clients at the same seven health centers. Approximately three brochures were reviewed by each client, for a minimum of 50 responses for each brochure. The assigned center liaison helped arrange the interviews with clients. Participants were approached in the waiting rooms, some of whom were there to participate in one of the agency's health and fitness programs. The same interview procedure used for health care providers (described above) was also used to test clients' perceptions of attractiveness, acceptability appropriateness of photos and diagrams, readability, message comprehension, usefulness, and willingness to share brochures with others.
Revision and retesting of readability
The brochures were revised a final time based on findings, and we again used the Fry readability test to assess the grade level of each brochure.
Step 4: Final Review and Endorsement
Our liaisons at the seven health centers were asked to rate the final drafts of the brochures on attractiveness, acceptability, readability, and usefulness. These representatives attended a health fair on O'ahu at which the PI was staffing an 'Imi Hale display. They were invited to visit the booth to view the final products. A simple scoring sheet was constructed that prompted representatives to rate each brochure along a 10-point continuum, with 1 being not attractive, acceptable, readable, and useful and 10 being very attractive, acceptable, readable, and useful. Finally, the 'Ahahui O Nā Kauka board members who provided preliminary endorsement for the brochures reviewed the final versions.
Findings
Important Message Components and Targeting Strategies
Focus group participants said that the messenger or implied speaker pictured in the brochure needed to be and look Hawaiian. All participants preferred to see a photograph on the cover rather than an illustration and wanted a photo of a Hawaiian who looked healthy active, and engaged in an enjoyable outdoor activity. About 75% agreed that Hawaiian values should be integrated into the brochures, such as recognizing the importance of the family ('ohana), being part of a group ('ohana), caring for each other (mālama kekahi i kekahi), and the natural environment. Thus, selected photographs portrayed Native Hawaiians in outdoor settings, engaged in Hawaiian activities such as canoe paddling and fishing, and together with family and friends caring for each other.
A vocal minority (about 20%) of participants did not want the brochure to include a photo of a physician, relating that “some of my clients are afraid of the doc, you know, and some haven't seen a doc in years.” However, another 20% felt that the credibility of the message would be increased with an endorsement from a medical source, such as the 'Ahahui O Nā Kauka, and that this should be prominently displayed on the front of the brochure. All agreed that presenting the brochures as a series, with a unifying look, also would increase credibility for consumers.
As found by the NCI (1998), all participants said that they preferred messages that were optimistic rather than threatening and scary. This was summarized by a participant who said, “My clients won't respond well to fear messages; many kupuna [elders] still see cancer as a death sentence, so the fear messages will keep them away.” Participants appreciated evidence as to why this cancer was a problem for Native Hawaiians, in particular, and what they could do about it. In fact, about 10% of participants were surprised to learn that Native Hawaiians could get skin cancer.
When asked about format, all participants said that wording should be relatively simple and sparse, with plenty of white space and pictures on each page, including a clear anatomical diagram of the body part (e.g., the prostate, testicles, or cervix) or a photo of the cancer (e.g., skin cancer lesions). About half of participants responded positively to quotes from healthy role models and messages that included Hawaiian values, for example, the final draft of the oral cancer brochure featured a photo of a Native Hawaiian family with the following quote from the father: “I'd rather give up smoking than time with my 'ohana [family].” All participants agreed that brochures should include contact phone numbers and cancer-related Web sites where readers could get additional information. The operationalization of targeting strategies in each brochure is summarized in Table 3 (Kreuter et al., 2003).
TABLE 3. Targeting Strategies for Native Hawaiian Brochures.
| Strategies | Operationalization |
|---|---|
| Peripheral strategies—making materials attractive to the culture | Featured photos of Hawaiian faces |
| Featured photos of scenic places | |
| Incorporated graphics that used Hawaiian patterns and designs | |
| Presented brochures as part of a series, with a unifying look | |
| Evidential strategies—presenting evidence of the relevance of the problem to the ethnic group | Included data on cancer risk factors, with link to activities, for example, paddling (sun exposure), smoking (oral cancer), sexual activity (cervical cancer) |
| Stated that Hawaiians were at risk for this particular cancer | |
| Included 'Ahahui O Nā Kauka endorsement on the cover of the brochures | |
| Linguistic strategies—using words and phrases from the group's language | Revised until brochures were between 5th- and 7th–grade reading levels |
| Used Hawaiian words, for example, 'ohana (family), pulama (cherish), kauka (physician) | |
| Constituent-involving strategies—drawing directly on the experience of members of the ethnic group | Engaged Native Hawaiians in focus groups to design brochures |
| Featured pictures of common activities | |
| Included quotes from Native Hawaiians | |
| Pretested brochures with staff and clients affiliated with community clinics on five islands in both rural and urban sites | |
| Sociocultural strategies—recognizing and working from the group's cultural values, beliefs, behaviors, and context | Featured group activities |
| Stressed importance of self-care for the sake of the 'ohana (family) | |
| Stressed respect for elders and desire to protect keiki (children) |
In terms of distribution, focus group participants felt that the brochures should be attractive and simple enough for use in the waiting room and at health fairs. They said they would welcome and help facilitate brochure testing in their health centers.
Consumer Testing With Health Care Providers and Clients
Attractiveness
As noted, attractiveness was tested by displaying our brochure alongside a selection of brochures on the same topic developed by other agencies and observing which one was selected. As shown in Table 4, 83% or more of health care providers selected our targeted brochures, noting that they were attracted to the cover photo of a local person and the scenery featured. It is surprising that fewer clients chose the targeted brochures. For example, only 36% of clients chose our cervical cancer brochure; instead, many older women chose a brochure by NCI titled,Pap Test for Older Women: A Healthy Habit for You (NCI, 2004), saying that although the young woman on the cover was very attractive and clearly Hawaiian, they felt that the brochure featuring an older woman would be more relevant for them. Other older clients said that they picked up the NCI or ASC brochure first because they noticed that they were endorsed by reliable providers of cancer information, reemphasizing the need for us to clearly display the 'Ahahui O Nā Kauka endorsement and the name of our organization on the cover of our brochures. Client participants who had personal experience with cancer themselves or had a family member with cancer reached for the thicker brochures, which they assumed had more information about cancer treatment, bypassing our one-page brochures that were prevention oriented. Finally, some noted during this testing phase that our brochures did not look very professional. This feedback was expected because our brochures were tested prior to final design by a graphic artist. However, focusing on our brochures, close to 90% of clients and providers agreed that the brochures were attractive to Native Hawaiians. The exception was for the cervical cancer brochure, which only 76% of clients believed was attractive.
TABLE 4.
Findings From Consumer Testing
| Skin Cancer | Prostate Cancer | Testicular Cancer | Oral Cancer | Cervical Cancer | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Staff (n = 35) n (%) |
Client (n= 37) n (%) |
Staff (n= 36) n (%) |
Client (n= 35) n (%) |
Staff (n= 35) n (%) |
Client (n = 35) n (%) |
Staff (n = 35) n (%) |
Client (n= 35) n (%) |
Staff (n= 36) n (%) |
Client (n = 42) n (%) |
|
| Attractiveness | ||||||||||
| Chose brochure | 33 (94.3) | 29 (78.4) | 35 (97.2) | 15 (42.9) | 29 (82.9) | 22 (62.9) | 31 (86.1) | 15 (42.9) | 33 (91.7) | 15 (35.7) |
| Photos attractive to Hawaiians | 33 (91.7) | 37 (100) | 33 (91.7) | 35 (100) | 31 (88.6) | 34 (97.1) | 34 (94.4) | 32 (91.4) | 32 (88.9) | 32 (76.2) |
| Acceptability | ||||||||||
| Anatomical pictures | 31 (88.6) | 33 (89.2) | 35 (97.2) | 33 (91.4) | 33 (94.3) | 32 (76.2) | 32 (88.9) | 30 (85.8) | 32 (88.9) | 36 (85.7) |
| Share with friends | 34 (97.1) | 37 (100) | 31 (86.1) | 34 (97.1) | 28 (80.0) | 32 (91.4) | 34 (94.4) | 32 (91.4) | 34 (94.4) | 41 (97.6) |
| Readability | ||||||||||
| Brochure easy to read | 33 (81.7) | 37 (100) | 33 (91.7) | 34 (97.1) | 32 (95.1) | 34 (97.1) | 34 (94.4) | 32 (91.4) | 30 (83.4) | 40 (95.2) |
| Learner verification: | ||||||||||
| Symptoms | 35 (100) | 34 (91.9) | 36 (100) | 32 (91.4) | 35 (100) | 29 (82.9) | NA | NA | NA | NA |
| Screening | 34 (97.1) | 34 (91.9) | 36 (100) | 32 (91.4) | 35 (100) | 29 (89.2) | 33 (97.1) | 26 (74.3) | 31 (86.1) | 19 (45.2) |
| Prevention | 34 (97.1) | 34 (91.9) | NA | NA | NA | NA | 36 (100) | 27 (77.1) | 33 (83.3) | 15 (35.7) |
| Fry reading level | ||||||||||
| Initial | 5th | 8th | 8th | 10th | 12th | |||||
| Final | 5th | 6th | 6th | 7th | 7th | |||||
| Usefulness | 33 (91.7) | 37 (100) | 33 (91.7) | 34 (97.1) | 33 (94.3) | 34 (97.1) | 33 (91.7) | 32 (91.4) | 35 (97.2) | 41 (97.6) |
Acceptability
We measured acceptability by asking specific questions about the anatomical pictures, with concern that the material might be considered offensive. We found that at least 88% of providers and 76% of clients felt that the anatomical pictures were appropriate. We also asked if reviewers would share the brochures with friends, and 91% or more of clients and 80% or more of providers said that they would share them.
Readability
At the start of Step 3 (consumer testing), the skin cancer brochure tested at a 5th-grade reading level, the prostate and testicular cancer brochures at an 8th-grade reading level, the oral cancer brochure at a 10th-grade reading level, and the cervical cancer brochure at a 12th-grade reading level (Fry, 1968). However, more than 80% of participants felt that the brochures were easy to read. In testing message comprehension, at least 97% of providers and 89% of clients demonstrated understanding of the symptoms, screening, and prevention messages of skin, prostate, and testicular cancer (which were at 5th- to 8th-grade reading levels). At least 97% of staff and 74% of clients grasped the messages in the oral cancer brochure. The cervical cancer brochure was understood by only 83% to 86% of providers and 36% to 45% of clients, suggesting that the messages about screening and prevention were not clearly stated.
Usefulness
During consumer testing, almost all (91% or more) of providers and clients said that the information provided in the brochures was useful.
Final Revisions and Retesting of Reading Level
After consumer testing, the brochures were revised again to reduce the reading level and to incorporate consumer suggestions. When retested, the reading levels of the brochures were between 5th- and 7th-grade reading levels. The cervical cancer brochure underwent the most changes. As recommended by consumers, a new cover photo (featuring four generations of women in one Native Hawaiian family) was secured to give the message that cervical cancer screening is important for all ages. We refocused the brochure's message to “getting screened” (and away from the causes of the disease). This allowed us to remove references to human papilloma virus (HPV) as the major cause of cervical cancer and helped reduce the reading level to 7th grade.
Endorsement
In Step 4, all seven health center liaisons endorsed the brochures, giving them high marks on attractiveness, acceptability, readability, and usefulness. The 'Ahahui O Nā Kauka voted to endorse the brochures, and their endorsement was printed on the front of each brochure.
Discussion
We used a four-step protocol to develop cancer awareness brochures for Native Hawaiians. Although the protocol was based on established research and recommendations related to brochure development, to our knowledge, this is the first time such a protocol has been used to develop cancer brochures with this minority population.
We believe there are multiple advantages to this protocol, given evidence-based targeting strategies and CBPR principles. By incorporating these strategies and principles, we solicited feedback from more than 200 individuals affiliated with Native Hawaiian-serving health centers across the state. Their input, especially on photos and artwork, was invaluable in making the brochures attractive to Native Hawaiians. As noted in the literature, if a brochure is not attractive, it will not be picked up and therefore is of no use (Doak et al., 1985; Flay et al., 1980; NCI, 1998).
The participatory approach also allowed us to demonstrate respect for providers by “playing to their strengths,” for example, asking physicians for advice on content and asking community health center workers for advice on format and distribution. We depended on community health workers to provide access to clients, giving them control over when and where testing took place so disruptions to their work were minimized. We also modeled respect for the participatory process, with its multiple checks and balances, to assure that the brochures were factually correct and professionally endorsed in addition to being attractive, acceptable, readable, and useful. Statewide and early involvement also ensured provider help with dissemination of the final products and created a demand for the final product.
The protocol also helped us forge and reinforce good relationships that would carry through to future projects. The protocol called for face-to-face interactions with providers and clients, essential to good communication among Native Hawaiians (Braun et al., 2002; Pukui et al., 1979). It was structured to solicit information and insights by asking open-ended questions from the people who would ultimately benefit from the brochures. Aside from the protocol's structure, relationship building is dependent on the individuals engaged in building them. Although project staff members were new to research and were meeting many providers and clients for the first time, the PI and assisting research interns were Native Hawaiian themselves and respectful of Hawaiian ways; complimentary reports of their ha'aha'a (humility) were received from the field.
Following this protocol also helped us identify commonalities and differences across sites and to establish for ourselves a bigger picture of the need for and potential use of the brochures. Although there were many similarities, on the island of Kaua'I, we received a request to translate the brochures into Hawaiian because many of the older people there speak Hawaiian. Although this was not requested by any other site, translating brochures would show respect for the Hawaiian language, provide opportunities to partner with native-language resources, and broaden outreach to our native-speaking population.
We learned a number of lessons as well. First, we verified the importance of further segmenting Native Hawaiians by gender and age in the future development and testing of brochures. With regard to gender, we had asked men and women to examine all the brochures because previous research with Native Hawaiians stressed the importance of educating the entire family about cancer screening so that members can support each other in obtaining age- and gender-appropriate screening (Braun et al., 2002). Among clients, however, some men were uncomfortable with being asked to examine the cervical cancer brochure, and some women were uncomfortable reviewing the prostate and testicular cancer brochures. Also, our group of client participants was made up of more women than men. Although we still believe in having both men and women review all brochures, we may consider asking men and women different questions in the review of gender-specific brochures.
We also saw that greater proportions of staff than clients chose our brochures when we tested attractiveness. This may have been due in part to the fact that staff were familiar with existing health materials and were drawn to our product because they were new. In general, staff were happy to have Hawaiian-made and Hawaiian-targeted brochures to distribute. Those clients who did not choose our brochure were more likely to be unfamiliar with existing brochures and thus picked one that addressed their immediate needs. For example, those with cancer or cancer in the family picked thicker brochures that provided more information about the cancer (including treatment), whereas others chose the “most professional looking” or the “most official” brochures. That some of the brochures were better liked by the health care providers than the clients may reflect the fact that we designed brochures based on focus groups with providers (community outreach workers and center staff) who were young and middle-aged adults. However, in consumer testing, 60% of our clients were age 60 or older due to their greater frequency of clinic visits and their availability during the day, when consumer testing was conducted. As the social marketing literature clarifies, it is very important to decide which segment of the target audience you want to deliver your message to and to conduct your formative and summative research with members of this segment (Kreps & Thornton, 1992).
Another lesson learned was that this type of protocol is time intensive, taking about 12 months to carry out. The PI worked full-time on the project, and he was assisted by other 'Imi Hale staff when needed (e.g., in conducting the focus groups and analyzing data to guide revisions). Obtaining permission and coordinating schedules to conduct focus groups and consumer testing in multiple sites took many months, and this was complicated by the expense and time required to fly to neighbor islands. In developing and testing five brochures at once, we demanded a large time commitment from reviewing consumers (e.g., it took about 30 minutes for a health care provider or client to review three to five brochures). It is fortunate that consumers were supportive of the process, and external (nongrant) funding supported staff, travel, and incentives. We also worried that providing an incentive may have led clients to provide us with socially desirable answers; however, variance in the results suggests that they did not, and responses to the incentive (a plastic thermal coffee mug) implied that participants felt appreciative, rather than coerced. Finally, health care providers who participated in the final review and endorsement (Step 4) expressed impatience because they wanted to start distributing the brochures at their health centers. The research team, however, felt that it was important to have the final version reviewed and endorsed by all.
We also realized a need to increase our printing budget to assure an adequate supply in response to the demand that was created during the testing process. Participating health care providers continually asked the researchers if they could duplicate the draft brochures for immediate use at their health centers until the final brochures were available. Although this was discouraged, we know that it occurred, and it verified the need for targeted education materials. Thus, our first printing of 10,000 brochures was distributed to providers and partners as soon as the brochures were finalized. A second printing of 10,000 is now being distributed. Unsolicited requests for these brochures have been received by agencies in the Western Pacific, American Samoa, and Southern California. In response, we share the protocol that we used and emphasize the added benefits of building relationships and creating demand that significantly aids distribution.
As outlined by the Information Processing Model, there are a number of steps between exposure to the message and health behavior change. In this study, we focused on the first few steps to make sure that the brochures captured the attention of Native Hawaiians, the message was read and understood, and knowledge was gained. The brochures still need to be tested for their role in behavior change, and possible future steps could include the testing of brochure effectiveness and dissemination strategies. For example, what types of changes can we expect in screening practices from these brochures? Would screening compliance be enhanced by using these brochures in combination with group or one-on-one educational sessions?
In conclusion, we used a participatory, four-step protocol to develop brochures that were attractive, acceptable, readable, and useful to Native Hawaiians. It is hoped that our successes and challenges will help other communities adapt our protocol to help them develop brochures for their own special populations.
Acknowledgments
Supported by the National Cancer Institute, Center to Reduce Cancer Health Disparities, CA86105, and approved by the Native Hawaiian Health Care Systems Institutional Review Board. Acknowledgments are tendered to the many individuals and groups who assisted with this project, including the Native Hawaiian Health Care Systems' staff and clients; research assistants Kapuaola Gellert, Jordan Lee, and Kara Wong; the 'Ahahui O Nā Kauka; and Audrey Riffenburgh of Riffenburgh & Associates.
Footnotes
Earlier versions of this article were presented at the Pacific Global Health Conference in June 2005 and the Kamehameha Schools Research Conference in October 2005, both in Honolulu, Hawai'i.
Contributor Information
Manny Kulukulualani, Is a research associate with 'Imi Hale–Native Hawaiian Cancer Network, a program of Papa Ola Lōkahi, in Honolulu, Hawai'i.
Kathryn L. Braun, Is a research director with 'Imi Hale–Native Hawaiian Cancer Network. She is also a professor of public health and social work at the University of Hawai'i in Honolulu, Hawai'i.
JoAnn U. Tsark, Is a program director 'Imi Hale–Native Hawaiian Cancer Network in Honolulu, Hawai'i.
References
- Boundouki G, Humphris G, Field A. Knowledge of oral cancer, distress and screening intentions: Longer term effects of a patient information leaflet. Patient Education and Counseling. 2004;53:71–77. doi: 10.1016/S0738-3991(03)00118-6. [DOI] [PubMed] [Google Scholar]
- Brandt HM, McCree DH, Lindley LL, Sharpe PA, Hutto BE. An evaluation of printed HPV educational materials. Cancer Control: Cancer, Culture and Literacy Supplement. 2005:103–106. doi: 10.1177/1073274805012004S17. [DOI] [PubMed] [Google Scholar]
- Braun KL, Mokuau N, Hunt GH, Ka'ano'i M, Gotay CC. Supports and obstacles to cancer survival for Hawaii's native people. Cancer Practice. 2002;10:192–200. doi: 10.1046/j.1523-5394.2002.104001.x. [DOI] [PubMed] [Google Scholar]
- Braun KL, Tsark JU, Santos LA, Aitaoto N, Chong C. Building Native Hawaiian capacity in cancer research and programming: The legacy of 'Imi Hale. Cancer. 2006;107(Suppl 8):2082–2090. doi: 10.1002/cncr.22157. [DOI] [PubMed] [Google Scholar]
- Doak CC, Doak LG, Root JH. Teaching patients with low literacy skills. Philadelphia: Lippincott Company; 1985. [Google Scholar]
- Flay BR, DiTecco D, Schlegel RP. Mass media in health promotion: An analysis using an extended information-processing model. Health Education Quarterly. 1980;7:127–147. doi: 10.1177/109019818000700203. [DOI] [PubMed] [Google Scholar]
- Fry E. A readability formula that saves time. Journal of Reading. 1968;11:513–516. 575–578. [Google Scholar]
- Gellert K, Braun K, Starkey V, Morris W. The 'Ohana (Family) Day Project—a community approach to increase cancer screening. Preventing Chronic Disease [serial online] 2006 Available from http://www.cdc.gov/pcd/issues/2006/jul/pdf/05_0188.pdf. [PMC free article] [PubMed]
- Gotay CC, Banner RO, Matsunaga DS, Hedlund N, Enos R, Issell BF, DeCambra H. Impact of a culturally appropriate intervention on breast and cervical screening among Native Hawaiian women. Preventive Medicine. 2000;31:529–537. doi: 10.1006/pmed.2000.0732. [DOI] [PubMed] [Google Scholar]
- Guidrey JJ, Walker VD. Assessing cultural sensitivity in printer cancer materials. Cancer Practice. 1999;7:291–296. doi: 10.1046/j.1523-5394.1999.76005.x. [DOI] [PubMed] [Google Scholar]
- Hawai'i Department of Health. Hawai'i cancer facts & figures 2003-2004. 2004 Retrieved May 5, 2004, from http://www.hawaii.gov/health/statistics/other-reports/cancer2003-04.pdf.
- Hunter JL. Cervical cancer educational pamphlets: Do they miss the mark for Mexican immigrant women's needs? Cancer Control: Cancer, Culture and Literacy Supplement. 2005:42–50. doi: 10.1177/1073274805012004S07. [DOI] [PubMed] [Google Scholar]
- Klein JF, Berry CC, Felice ME. The development of a testicular self-examination instructional booklet for adolescents. Journal of Adolescent Health Care. 1991;11:235–239. doi: 10.1016/0197-0070(90)90355-6. [DOI] [PubMed] [Google Scholar]
- Kreps GL, Thornton BC. Health communication theory & practice. Prospect Heights, IL: Waveland Press; 1992. [Google Scholar]
- Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: Targeted and tailored approaches. Health Education and Behavior. 2003;30:133–146. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Wray RJ. Tailored and targeted health communication: Strategies for enhancing information relevance. American Journal of Health Behavior. 2003;27(Suppl 3):S227–S232. doi: 10.5993/ajhb.27.1.s3.6. [DOI] [PubMed] [Google Scholar]
- Matsunaga DS, Enos R, Gotay CC, Banner RO, DeCambra H, Hammond OW, Hedlund N, Ilaban EK, Issell BF, Tsark J. Participatory research in a Native Hawaiian community: The Wai'anae Cancer Research Project. Cancer. 1996;78(Suppl 7):1582–1586. [PubMed] [Google Scholar]
- Meade CD. Cancer, culture and literacy: Critical next steps in improving care for diverse populations. Cancer Control: Cancer, Culture and Literacy Supplement. 2005:4–5. doi: 10.1177/1073274805012004S01. [DOI] [PubMed] [Google Scholar]
- Minkler M, Wallerstein N, editors. Community-based participatory research for health. San Francisco: Jossey-Bass; 2003. [Google Scholar]
- Morgan DL, Krueger RA. The focus group kit. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- National Cancer Institute. Making health communication programs work. 1998 Retrieved May 5, 2004, from http://www.cancer.gov/pinkbook.
- National Cancer Institute. Cancer statistics. 2004 Retrieved May 5, 2004, from http://www.cancer.gov/
- Partin MR, Nelson D, Radosevich D, Nugent S, Flood A, Dillon N, Holtzman J, Haas M, Wilt TJ. Randomized trial examining the effect of two prostate cancer screening educational interventions on patient knowledge, preferences, and behaviors. Journal of General Internal Medicine. 2004;19:835–842. doi: 10.1111/j.1525-1497.2004.30047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul CL, Redman S, Sanson-Fisher RW. Print material content and design: Is it relevant to effectiveness? Health Education Research. 2003;18:181–190. doi: 10.1093/her/18.2.181. [DOI] [PubMed] [Google Scholar]
- Paul CL, Redman S, Sanson-Fisher RW. A cost-effective approach to the development of printed materials: A randomized controlled trial of three strategies. Health Education Research. 2004;19:698–706. doi: 10.1093/her/cyg090. [DOI] [PubMed] [Google Scholar]
- Pukui MK, Haertig EW, Lee CA. Nana i ke kumu: Look to the source. Honolulu, HI: Queen Lili'uokalani Children's Center; 1979. [Google Scholar]
- Richard MA, Martin S, Gouvernet J, Folchetti G, Bonerandi JJ, Grob JJ. Humour and alarmism in melanoma prevention: A randomized controlled study of three types of information leaflet. British Journal of Dermatology. 1999;140:909–914. doi: 10.1046/j.1365-2133.1999.02824.x. [DOI] [PubMed] [Google Scholar]
- Solomon FM, Eberl-Lefko AC, Michaels M, Macario E, Tesauro G, Rowland H. Development of a linguistically and culturally appropriate booklet for Latino cancer survivors: Lessons learned. Health Promotion Practice. 2005;6:405–413. doi: 10.1177/1524839905278447. [DOI] [PubMed] [Google Scholar]
- Taylor VM, Hislop TG, Jackson JC, Tu SP, Yasui Y, Schwartz SM, Teh C, Kuniyuki A, Acorda E, Marchand A, Thompson B. A randomized controlled trial of interventions to promote cervical cancer screening among Chinese women in North America. Journal of the National Cancer Institute. 2002;94:670–677. doi: 10.1093/jnci/94.9.670. [DOI] [PMC free article] [PubMed] [Google Scholar]