Abstract
Background
Native Hawaiians today face a disproportionately high rate of obesity. The Designing Healthy Worksites (DHW) project investigated existing administrative policies and supports for healthy eating and physical activity at eight Native Hawaiian-serving organizations in Hawai‘i, along with employee preferences for worksite wellness programming.
Objectives
We describe the process by which Native Hawaiian researchers and community members worked together to gather formative data to design future worksite wellness programs.
Methods
A Native Hawaiian doctoral student (JHL) and a Native Hawaiian activist (CKH) spearheaded the project, mentored by a Caucasian professor (KLB) who has worked in Hawaii communities for 30 years. Advisors from the worksites supported the use of environmental assessments (n = 36), administrative interviews (n = 33), focus groups (n = 9), and an employee survey (n = 437) to collect data. We used an interactive process of data collection, sharing, and interpretation to assure mutual agreement on conclusions and future directions.
Results
Worksites were at different stages of readiness for worksite wellness programming, suggesting that a toolkit be developed from which agencies could create a program that fit. Activities preferred by large proportions of employees included support groups, experiential nutrition education (e.g., cooking demonstrations and field trips for smart food shopping), food buying clubs, and administrative policies supporting healthy lifestyles. High participation in data collection and interpretation suggest that our methods fostered enthusiasm for worksite wellness programming and for Native Hawaiians as researchers. The team continues to work together to develop and test interventions to promote worksite wellness.
Conclusion
Native-directed research that engages administrators and employees in designing programs heightens program acceptability and applicability.
Keywords: Indigenous, Pacific island, worksite health promotion, nutrition, physical activity, community engagement
Written accounts by Western explorers who arrived in Hawai‘i in 1778 described Native Hawaiians as “perfectly well formed” and “above the middle size, and well made.” These accounts are in sober contrast with today’s picture. In Hawai‘i, Native Hawaiians have the highest age-adjusted death rates for all causes of death, heart disease, cancer, stroke, diabetes, chronic respiratory diseases, other circulatory diseases, and kidney disease,1 and the highest prevalence of obesity among the state’s major ethnic groups.2
Obesity is a risk factor for a variety of chronic illnesses, including hypertension, dyslipidemia, type 2 diabetes, heart disease, stroke, gallbladder disease, osteoarthritis, sleep apnea, asthma, respiratory problems, and some cancers (endometrial, breast, and colon).3 Poor nutrition and insufficient physical activity are major risk factors for chronic diseases and are major contributors to obesity.
Researchers and community members in Hawai’i have worked together to promote obesity reduction and chronic disease control. Best known are interventions to test the effects of the traditional Hawaiian diet (THD)—a high complex carbohydrate, moderate protein, and low-fat diet that Native Hawaiians consumed before their contact with the West.4–6 Results from THD studies demonstrated immediate improvements to serum lipid and glucose profiles, in addition to weight loss.4–7 Unfortunately, improvements are difficult to sustain once the program ends. A follow-up study of diet study participants found that lack of support for healthy eating and exercise at home and work to be a barrier.8 Worksites are ideal settings for health promotion programs, because working adults spend a majority of their waking hours at work, and worksites are characterized by social networks, which can provide significant support for positive behaviors.9
As Native Hawaiian researchers and activists who have implemented and studied THD programs, the first two authors (JHL and CKH) talked to their colleagues in worksites that employed large proportions of Native Hawaiians about designing work-based weight loss programs. This collaboration, the DHW project, explored administrative policies and supports for healthy eating and physical activity, along with employee preferences for worksite wellness programming.
This study was conducted under the auspices of ‘Imi Hale Native Hawaiian Cancer Network (‘Imi Hale), one of 25 Community Network Programs funded by the National Cancer Institute’s Center to Reduce Cancer Health Disparities.10 ‘Imi Hale is initiated and led by Native Hawaiians. It is dedicated to mentoring Native Hawaiian researchers, supporting them to design and test interventions in cancer prevention and control, such as the DHW project. Several of the worksite leaders in the DHW collaborative are advisors to or partners with ‘Imi Hale in its mission to reduce cancer disparities and develop a cadre of indigenous researchers.
In this paper, we describe the community-based research processes used by the DHW collaborative, along with the findings from the worksite assessment and interactive interpretation sessions.
METHODS
As all projects sponsored by ‘Imi Hale, the DHW project was guided by principles of community-based participatory research (CBPR).11,12 This project incorporated indigenous community leadership, respect for Native Hawaiian culture and values, and co-learning and co-ownership of the project.10,13 These principles were honored as the DHW collaborative (comprised of native researchers and worksite leaders) developed the research, collected data, and interpreted findings.
Engaging Indigenous Leaders
Involving indigenous community leaders is a crucial first step in designing and building awareness and support for community-based programs in Native Hawaiian communities. A year before project funding, a DHW project leader (JHL), a young Native Hawaiian nutritionist, asked Hawai‘i’s first Native Hawaiian nutritionist (CKH) to co-lead the project. CKH is well known for a lifetime of activism around Hawaiian health. She served as a community mentor to JHL and her involvement increased the project’s credibility and reach. The third author (KLB) mentored the team throughout the design, grant writing, data analysis, and reporting phases.
Early in the conceptualization stage, 10 Native Hawaiian-serving organizations already partnering with ‘Imi Hale were invited to participate. Meetings were held to discuss the organizations’ participation, with the approach differing based on the researchers’ relationships with the organization’s leadership. Traditionally, Native Hawaiian communities were composed of groups of close-knit families that would recite genealogical relationships between individuals, families, and communities to gain acceptance as they ventured into outside communities. This reliance on relationships and reputations continues to a great degree in Hawaiian communities today.14 Thus, determining the nature of relationships between the researchers and the organizational leaderships was an important first step, and guided how the native researchers approached each organization.
Five of the eight organizations had worked with ‘Imi Hale since 2000 and the native researchers (JHL and CKH) had positive past experiences working with the leadership of these organizations. Soliciting participation of “known” leaders involved spending time catching up on past projects, mutual friends, and personal wellness. Discussion of the DHW project was initiated after this catching-up phase.
The other three organizations also had partnered with ‘Imi Hale, but leaders had not worked specifically with the native researchers spearheading DHW. In these cases, a face-to-face meeting was scheduled with the agencies’ executive directors. Initial meetings involved building rapport between the executives and native researchers by providing personal background information (particularly family names of grandparents, parents, and spouses), island of origin for self and ancestors, high school attended, marital status, and family size. Native Hawaiians traditionally generate knowledge of place and family before a relationship can begin and mutual trust is developed. Impressions generated by the end of these initial meetings would be weighed carefully as agencies decided whether or not to participate in the project.
Agreement to participate in the project, after an invitation to do so, is a public statement of mutual trust between researchers and participating agencies and a commitment to the project. By showing affiliation with each other, both the researchers and agency representatives trust that care will be taken to not exploit or take advantage of the health and welfare of all involved and that the goals of the project are of mutual benefit.
Following these procedures, 8 of the 10 agencies agreed to participate—4 health agencies, 3 social service agencies, and one faith-based organization. The other 2 agencies decided not to participate, citing time constraints. The research team agreed to include all sub-sites (both urban and rural) of each organization in data collection. This commitment demonstrated that no one would be left out, and that ideas, needs, challenges, opinions, and preferences of all employees were valued. All but one agency had multiple offices, and 3 agencies had offices on five or more of Hawai‘i’s seven inhabited islands, for a total of 36 sites (Table 1). Some the sites were very rural, requiring the researcher team to travel by commuter plane and rental car to collect data and share findings.
Table 1.
Participating Organizations and Their Missions
| Name and Type of Agencya | Mission | Sites | Employees |
|---|---|---|---|
| Office of Hawaiian Affairs (OHA) (SS) | Fostering cultural, social, health, intellectual and economic development of Hawaiians, protecting Hawai‘i’s environmental resources and providing an interface with state and federal governments for Native Hawaiians | 1 HQ and 5 other sites | 160 |
| Papa Ola Lōkahi (POL) (H) | Pilots health programs, develop materials, and supports training to improve the health and well-being of Native Hawaiians and provide interface with the federal government programs in health for Native Hawaiians | 1 HQ and 1 other site | 35 |
| ALU LIKE, Inc. (ALI) (SS) | Implements social service and employment programs for Native Hawaiians | 1 HQ and 6 other sites | 155 |
| Queen Lili‘uokalani Children’s Center (QLCC) (SS) | Provides social services to orphaned and destitute children with preference given to Native Hawaiian children | 1 HQ and 9 other sites | 135 |
| Hui Nō Ke Ola Pono (HNKOP) (H) | The Native Hawaiian Health Care System (NHHCS) that provides health services access and health education services to Native Hawaiians on Maui | 1 HQ and 1 other site | 43 |
| Ke Ola Mamo (KOM) (H) | The NHHCS that provides health services access and health education services to Native Hawaiians on O‘ahu | 1 HQ and 5 other sites | 36 |
| Nā Pu‘uwai (NP) (H) | The NHHCS that provides health services access and health education services to Native Hawaiians on Moloka‘i and Lāna‘i | 1 HQ and 1 other site | 23 |
| Kawaiaha‘o Church (KAW) | A Protestant church in Honolulu established in the early 1800s attended by a large Native Hawaiian constituency | 1 HQ and 0 other sites | 21 |
| Total | 36 | 608 |
H, health agency; SS, social service agency.
Collecting the Data
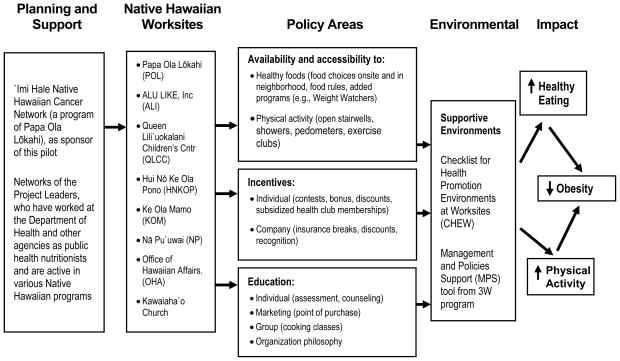
Data collection was informed by a previous study by Sallis et al.15 on policy development and environmental changes to promote physical activity. The study framework use by Sallis et al. was expanded to include healthy eating, as both physical activity and healthy eating are needed for the prevention and reduction of obesity (Figure 1).
Figure 1. Framework for Policy–Environmental Interventions.
From Sallis et al.15
The DHW team agreed to employ different methods to capture data on administrative policy, administrator preferences, and employee preferences. Researchers aimed to ensure broad participation, in each of the four assessment methods utilized (Table 2). As part of the research team, administrators reviewed and approved all tools and consent forms. Decision making was equitable—researchers provided the tools and guidance to help collect information and agencies provided access and insights to the information being identified.
Table 2.
Participants by Island by Type of Data Collection Across 8 Agencies
| O‘ahu | Maui | Kaua‘i | Lana‘i | Moloka‘i | Big Island | Total | |
|---|---|---|---|---|---|---|---|
| CHEW assessments | 15 | 6 | 3 | 3 | 4 | 5 | 36 |
| MPS respondents | 13 | 5 | 3 | 3 | 4 | 5 | 33 |
| Focus group participants | 17 | 14 | 4 | 1 | 9 | 11 | 56 |
| Survey respondents | 296 | 53 | 13 | 3 | 26 | 46 | 437 |
The entire project and all tools and consent forms were approved by the Institutional Review Board (IRB) of the Native Hawaiian Health Care System. This community-based IRB was formed by Native Hawaiians health agencies to ensure that research is respectful of native concerns and builds research capacity in native community, paying added attention to group harm and data ownership and dissemination. About two thirds of the membership are Native Hawaiian.16
Environmental Assessment
To assess the worksite environment, researchers and site supervisors of the 8 main offices and 28 satellite offices worked together to complete a standardized tool called the Checklist of Health Promotion Environments at Worksites (CHEW). The CHEW is a direct observation instrument designed to assess environmental characteristics known to influence health-related behaviors.17 The checklist includes 112 items in three domains: (1) Physical environment (i.e., stairwells, fitness facilities, lunchrooms, on-site healthy food choices); (2) information environment (health information and education signs); and (3) surrounding neighborhood (availability and proximity of fitness and food opportunities).
At each site, the organizational representative and researchers together inspected the buildings, walking every corridor, around the grounds outside, and through the neighborhood just beyond the grounds. Instructions for scoring the CHEW, detailed in Oldenburg’s research17 were followed. For this analysis, scales were developed for physical activity and nutrition-related supports. Some items were omitted from the CHEW, for example, elevator and stair facilitation scales were omitted because there were only three sites with elevators.
Administrative and Managerial Supports
Managers and/or site supervisors (n = 33) associated with the eight worksites were interviewed to assess current resources, worksite policies, and level of management support for establishing and maintaining healthy worksite environments. The Management and Policies Support (MPS) tool, which was developed for the 3W Study by the Kaiser-On-The-Job Program18 was used. This tool has a series of questions in 11 domains, each domain pertaining to a different aspect of worksite health policies. For this study, only 10 areas were measured; the item on stairwell access was eliminated because most worksites were single-story buildings.
Scores were calculated for 10 MPS domains: (1) Wellness committee; (2) physical activity plan; (3) encouragement of active breaks; (4) physical activity facilities; (5) after-hours access to physical activity facilities; (6) nutrition plan; (7) health fair; (8) health education classes; (9) promotion of health programs; and (10) health promotion budget. Each domain was scored as a percentage (ranging from 0% to 100%). For domains with multiple items, the domain score is derived by dividing the number of items to ensure equal weighting of the categories. A composite score is created by summing domain scores. In line with CBPR, data were collected in partnership with the site supervisor using an educational, rather than matter-of-fact, approach. The interaction served to raise awareness about employee wellness and the different areas where wellness could be addressed.
Focus Groups
Researchers conducted focus groups with employers and employees to elicit their opinions and suggestions about desirable components for worksite-sponsored health promotion activities and acceptable ways to measure changes resulting from health programs. Focus group questions were guided by the Sallis framework and touched on three areas: (1) Availability and access; (2) desired education, programs, and incentives; and (3) acceptable measures of determining positive health change.
A total of 56 individuals participated in 9 focus groups conducted on five islands, including O‘ahu, Moloka‘i, Kaua‘i, Maui and Hawai‘i. Each focus group lasted about 90 minutes. The focus group team consisted of the authors and two Native Hawaiian research interns. All participated in a 4-hour training in focus groups designed to build indigenous research capacity.
The first two authors took turns facilitating focus groups on different islands. As with most Native Hawaiian gatherings, focus group sessions started with a pule (prayer) to bless the food and solicit spiritual guidance for a productive and positive discussion. A nutritious lunch was provided for participants as a demonstration of gratitude for their participation and attentiveness to their physical well-being.
Separate focus groups for administrators and staff were held to encourage open discussion. As a result, line staff readily voiced opinions and many ideas. Allowing line staff to share among their peers, without fear of possible reprisals, helped to build support and enthusiasm for the project. The exception was on Kaua‘i, where staff sizes were small and administrators and line staff agreed to participate in a single focus group.
Recorded focus group discussions were transcribed, and each verbatim transcript was read by at least three members of the research team. Readers extracted themes independently, then met with team members to reach consensus on themes and which participants spoke to each theme. Together, team members created a code book, grouping themes into four categories: (1) Supports; (2) barriers; (3) ideas for programs and policies; and (4) acceptable evaluation methods.
Employee Survey
Based on focus group findings, a questionnaire was developed that included 35 multiple choice items and took approximately 10 minutes to complete. Items queried preferences for specific program, policy, and evaluation ideas that had surfaced in the focus groups. Returned surveys were not linked to employee names, and data were analyzed in aggregate.
The survey was sent via the Internet to the directors of the participating agencies, who were partners in the research, and they forwarded it to their employees. This distribution method demonstrated the executive directors’ support of the study and emphasized the importance of participating in the survey.
About 437 out of an estimated 608 individuals total from all eight organizations (72%), completed the survey. Response rates by agency ranged from 66% to 79%. The literature suggests an average response rate of 30% for an on-line survey and 40% for an e-mail survey. Thus, the response rate of 72% demonstrates broad buy-in for the research, and findings represent the views of the majority of employees. Data were analyzed in aggregate to preserve the confidentiality of the respondents and agencies. Not every respondent answered every question, resulting in slight differences in total responses by question.
Data Analysis and Interpretation
After completing the analyses of the four different assessments, findings were shared and interpreted first at a meeting with the executive directors as research partners. It was made clear that no findings would be shared beyond this group without their express permission. Ultimate approval to share the data and guidance on planning the staff presentations also resulted from this meeting. The participatory approach in data sharing and interpretation enhanced the respect that administrators had for the Native Hawaiian researchers, as it was a demonstration of the co-learning and power-sharing principles of CBPR.
After this initial meeting, lunchtime presentations were conducted on each of the major islands, to which administrative and line staff from participating organizations were invited. At each presentation, researchers solicited feedback on the findings and thoughts on the components of an appropriate worksite wellness program (WWP). These meetings provided excellent opportunities for information and idea sharing between all agencies and partners and helped shape the subsequent community presentations as well as the development of the next phase of the project.
Next, findings were presented at ‘Imi Hale’s annual Report to the Community, where Native Hawaiian researchers with ongoing or recently completed projects share project results to more than 80 indigenous outreach workers, community partners, and health professionals. Participating agencies were represented at this community presentation and publicly praised the project’s success. The presentation garnered communities’ praise for the accomplishments of the researchers, the involvement of the participating agencies and encouragement for future work.
RESULTS
Data Findings
Several key findings resulted from the onsite inspections using the CHEW to assess health-enhancing aspects of worksite environments. Higher physical activity environmental supports were seen in rural versus an urban locations, because they generally provide more outdoor opportunities for physical exercise. Having lunchroom appliances, for example, a refrigerator and microwave, was the greatest support for healthy eating behaviors because it allowed employees to store and heat a healthy lunch brought from home.
From the interviews with managers and supervisors using the MPS, it was learned that the number and type of healthy worksite policies and opportunities varied across and within organizations, and no pattern was observed among islands or between rural and urban sites.
As expected, the four participating health agencies, because of their mission and services, had more health activities available to their staff than the other agencies.
The focus groups conducted on each island provided information about the availability of healthy food choices, motivators for engaging in regular exercise, ideas for education programs, incentives for participants, and “acceptable” measures of change. Regarding physical exercise, participants were very supportive of worksite policies that allowed workers time during the work day for exercise. Regarding healthy eating, participants noted that eating behaviors were affected by access to healthy foods, manageable work load, and group support. For those with heavy workloads, eating fast foods or “whatever is around the office” had become habit. The availability of lunchroom appliances, food co-ops, and group support improved access and increased motivation to make healthier choices.
Regarding preferred, hence, acceptable methods of evaluation, focus group participants suggested measuring changes in weight, body fat, and other vital measures. This was also confirmed by the majority of survey respondents. Allowing employees to provide input on evaluation measures will help to ensure that acceptable evaluation methods are used in future worksite wellness programming and research.
Survey results are shown in Table 3. Support groups, group activities, worksite policies, and accessibility to healthy food choices were selected as the most preferred strategies to help employees improve healthy eating and exercise patterns. Observing healthy behaviors practiced by the administrator and other co-workers was also perceived as very motivating, confirming the influence of role models at the worksite.
Table 3.
Participants’ Ideas for Worksite Wellness Programming and Activities
| Supports | N (%) |
|---|---|
| Healthful Food Choices at Work | |
| Healthy local foods sold at the office | 208 (50) |
| Support group | 166 (40) |
| Providing appliances to support healthy home lunch | 165 (40) |
| Water dispenser | 165 (40) |
| Engaging in Regular Exercise | |
| Having worksite policy for time off for exercise | 251 (64) |
| Having worksite policy allowing work week to be adjusted around exercise | 232 (59) |
| Discounts or lower membership rates at nearby fitness centers | 232 (59) |
| Programs | |
| How to cook healthy meals | 239 (61) |
| Healthy meal demonstrations and food tastings | 233 (59) |
| How to shop for healthy foods on a budget | 220 (56) |
| Activities | |
| Annual fitness checks, monitoring weight, blood pressure and other indicators | 262 (67) |
| Paid employee retreats | 246 (63) |
| Employee family exercise classes/opportunities | 192 (49) |
| Evaluation Options | |
| Changes in blood pressure, cholesterol, and blood sugar measures | 205 (53) |
| Employee use of wellness programs and time off for exercise | 187 (49) |
| Changes in weight and body fat | 166 (43) |
| Opinions | |
| I feel that employers can and should promote healthy lifestyles at the worksite | 249 (64) |
| I would feel more appreciated if my agency invested in employee worksite wellness | 155 (40) |
| If my agency organized wellness classes and activities, I would participate in them most of the time. | 157 (40) |
| I would feel more motivated to be healthier at work if my co-workers practiced healthful behaviors. | 89 (23) |
| I would feel more motivated to be healthier at work if my boss practiced healthful behaviors. | 75 (19) |
DISCUSSION
In line with the dual purpose of the paper, to share both our CBPR process and the worksite assessment results, the discussion provides reflections on both the process and the findings.
Reflections on the Process
In CBPR, researchers must learn about the culture of the community and establish trust before the actual research can move forward.19–21 This process requires time, because relationships are built in both a historical and institutional context, while concurrently developing personal trust between the researchers and the community at large.22 Non-minority researchers may have to work harder and longer to establish this trust because, by default, they are “outsiders” in the community. In most cases, non-minority researchers come from privilege, and have had opportunities and advantages not readily accessible to minority Americans.22,23
Our project, however, was led by indigenous researchers (JHL, CKH) and interns, who are from the Native Hawaiian community and are considered “outsider–insiders.” Although they are researchers, they can personally relate to participating community members because they share cultural, historical, and sometimes personal experiences, including historical trauma, racism, and oppression with the Hawaiian community.12,24
Because indigenous researchers led this study, the process of establishing trust was not as time intensive as a first-time partnership might be. Still, protocol was followed in approaching administrators, and protocol differed depending on prior relationships with the agency and administrator partners. Native Hawaiian researchers were more formal in their approach to Native Hawaiian administrators they did not know, meeting face-to-face, sharing ancestry, and so forth. Because researchers were native, common connections were easily identified and new friendships were formed relatively quickly. This gave the researchers more rapid access to “insider” information not typically shared with “outsiders.” It also allowed agency members to be candid and comfortable when sharing personal ideas, goals, and struggles without fear or shame of being misunderstood. The community gained a sense of empowerment by receiving validation of their beliefs and ideas, and through the realization that the information they provided shaped future project design.
Along with the feeling of empowerment resulting from this project, the community participants were co-owners of the project. The high level of trust and accountability of the researchers, the interactive process used in the design and approval of the project, and the interactive nature of data collection and interpretation helped encourage agency espousal of this project. These actions demonstrated commitment to and genuine caring for the community members as part of the research team. Relationships and trust were strengthened by the shared cultural ties and the positive feelings associated with this project.
The willingness of the community and researchers to be co-learners was another strength. This education was largely gained through a “listening-dialogue-action approach” between the researchers and community participants.25 The co-learners willingly identified and reflected on pertinent issues involved, increasing their cognitive understanding and knowledge of real issues and making joint decisions on how to enact positive change. This on-going process will help the community to build capacity and gain independence in developing and maintaining worksite programs. It will also help the researchers to gain knowledge and insights necessary to provide continuing support to the worksites, and to assist in similar initiatives at other worksites.
Reflection on the Findings
All eight agencies guided the development to the DHW project and participated in the assessment even though agencies and subsites were at different stages of readiness to plan and implement formal wellness programs in their worksites. Six of the worksites already had some worksite wellness policies and/or programs in place, and both their administrators and staff were enthusiastic about the DHW project. They expressed willingness to allocate staffing, resources, and time to formalize and expand worksite wellness programs.
Two agencies had no wellness policies or few activities in place. Their administrators seemed to be willing to develop programs, but were less enthusiastic about committing staff or other resources. Although all agencies participated in focus groups and the survey, participation rates were lower in these two agencies. Line staff were found to be more focused on work, rather than worksite health promotion, owing to a combination of being more removed from the decision-making processes by the administrators and less informed about its benefits.26 Thus, these agencies could benefit from information on potential benefits of worksite wellness program, namely, healthier employees, to help encourage enthusiasm for a WWP.
Toolkits were identified by participants as an appropriate tool for their worksites. Generally, toolkits are developed to meet the needs of agencies in various stages of readiness. According to the Centers for Disease Control and Prevention Healthier Worksite Initiative, toolkits are “time saving aids that provide customizable turn-key solutions” and can be selected to meet identified needs and resources of the worksite and its employees.27 They are a compendium of resources and tools that often include step-by-step instructions for getting started, menus of possible activities, and details on how to implement specific activities within a specific subject of interest. Toolkits would provide each worksite the guidance, resources, and flexibility needed to independently plan and tailor their WWP, based on interests, limitations, and parameters. The concept of using toolkits in worksites and for other community programming fits with another CBPR principle—self-determination—because they allow worksites to design and customize their individual WWP and prioritize their activities.28
The Internet contains a plethora of worksite wellness toolkits developed by different states and organizations within the United States. Following this study’s thorough baseline assessment of employee interests and worksite supports, the next step will be to select a toolkit already developed and tested that most closely fits the identified needs and preferences of the participating agencies and tailor it for cultural appropriateness and local usefulness. Different sites and subsites within each organization will be consulted frequently throughout the toolkit adaptation process to ensure appropriateness and acceptability, continuing to build the sense of empowerment and ownership of the project and its chances of success.
CONCLUSION
This project is the first worksite wellness project conducted by Native Hawaiians researchers in collaboration with Native Hawaiian worksites. Although all researchers may be considered as “outsiders” by the community, our Native Hawaiian research team was recognized as belonging to the community, thus helping us to establish trust and acceptance. Findings demonstrated that Native Hawaiians are open to WWP that focus on weight loss, healthy eating, and physical activity. Data collection efforts utilized within a CBPR construct provided opportunities for community engagement at both the administrative and worker levels. This resulted in comprehensive and detailed information on Native Hawaiian employee preferences and employer supports for WWP. Although findings may not be applicable to non-Native Hawaiian serving worksites, our process of engaging indigenous researchers and community members together in research around worksite wellness may have value in other minority communities.
Table 4.
CBPR Principles and Outcomes
| CBPR Principles | Outcomes |
|---|---|
| Use of Indigenous Leaders | Trust established more readily |
| Increased participation | |
| Empowerment | Greater buy-in |
| Increased participation | |
| Co-Ownership | Greater buy-in |
| Increased enthusiasm | |
| Increased participation | |
| Co-Learning | Skills building |
| More detailed information gotten | |
| Respect for Culture and Values | Increased trust |
| Greater buy-in | |
| Increased participation | |
| More detailed information gotten | |
Acknowledgments
The authors thank JoAnn Tsark, MPH, for her endless support and help with this project. We thank our Native Hawaiian interns Kapi‘olani Laronal, MEd and Maile Hirao, MPA, for their help with the project, especially the focus groups.
Supported by the Office of Hawaiian Affairs and the National Cancer Institute (U01 CA114630-03S2 and U01 CA 114630-04S4).
References
- 1.Johnson DB, Oyama N, LeMarchand L, Wilken L. Native Hawaiians mortality, morbidity, and lifestyle: comparing data from 1982, 1990, and 2000. Pacific Health Dialog. 2004;11(2):120–30. [PubMed] [Google Scholar]
- 2.Hawai’i Department of Health [DOH] 2008 State of Hawai’i Behavioral Risk Factor Surveillance System. c2008 [cited April 28, 2009]. Available from: http://hawaii.gov/health/statistics/brfss/brfss2008/demo08.html.
- 3.Centers for Disease Control and Prevention [CDC] Overweight and obesity: Health consequences. c2008 [September 2008]. Available from: http://www.cdc.gov/nccdphp/dnpa/obesity/consequences.htm.
- 4.Aluli NE, et al. 4th National Forum on Minority Health Issues for an Emerging Majority. Washington, DC: National Heart Lung and Blood Institute; 1992. Weight control with the traditional Hawaiian diet and cultural education. [Google Scholar]
- 5.Shintani TT, Beckham S, Tang J, O’Connor HK, Hughes C. Wai‘anae diet program: Long term follow-up. Hawaii Med J. 1999;58:117–22. [PubMed] [Google Scholar]
- 6.Fujita R, Braun KL, Hughes CK. The traditional Hawaiian diet: A review of the literature. Pacific Health Dialog. 2004;11(2):250–9. [PubMed] [Google Scholar]
- 7.Leslie J. Uli‘eo Koa program: Incorporating a traditional Hawaiian dietary component. Pacific Health Dialog. 2001;8(2):401–6. [PubMed] [Google Scholar]
- 8.Hughes C. Traditional Hawaiian diet programs: A culturally competent chronic disease intervention. Pacific Health Dialog. 1998;5(2):328–31. [Google Scholar]
- 9.U.S. Department of Health and Human Services (U.S. DHHS) Healthy people 2010: Understanding and improving health. 2. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- 10.Braun K, Tsark JU, Santos L, Aitaoto N, Chon C. Building Native Hawaiian capacity in cancer research and programming: The Legacy of ‘Imi Hale. Cancer. 2006;107(8 Suppl):2082–90. doi: 10.1002/cncr.22157. [DOI] [PubMed] [Google Scholar]
- 11.Israel BA, Schulz AJ, Parker EA, Becker AB. Community–Campus Partnerships for Health. Community-based participatory research: policy recommendations for promoting a partnership approach in health research. Educ Health (Abingdon) 2001;14(2):182–97. doi: 10.1080/13576280110051055. [DOI] [PubMed] [Google Scholar]
- 12.Minkler M, Wallerstein N, editors. Community-based participatory research for health: From process to outcomes. San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- 13.Tsark J. Cancer in Native Hawaiians. Pacific Health Dialog. 1998;5(2):315–27. [Google Scholar]
- 14.Braun KL, Mokuau N, Hunt GH, Kaanoi M, Gotay CC. Supports and obstacles to cancer survival for Hawaii’s native people. Cancer Practice. 2002;10:192–200. doi: 10.1046/j.1523-5394.2002.104001.x. [DOI] [PubMed] [Google Scholar]
- 15.Sallis JF, Bauman A, Pratt M. Environmental and policy interventions to promote physical activity. Am J Prev Med. 1998;15(4):379–97. doi: 10.1016/s0749-3797(98)00076-2. [DOI] [PubMed] [Google Scholar]
- 16.Braun K, Tsark J. Community-based IRBs: What researchers should know. Nurse Author & Editor. 2008;18(2) [Google Scholar]
- 17.Oldenburg B, Sallis JF, Harris D, Owen N. Checklist of Health Promotion Environments at Worksites (CHEW): Development and measurement characteristics. Am J Health Promot. 2002;16:288–99. doi: 10.4278/0890-1171-16.5.288. [DOI] [PubMed] [Google Scholar]
- 18.Williams AE, Vogt TM, Steven SJ, Albright CJ, Nigg CR, Meenan RT, et al. Work, Weight, and Wellness: The 3W Program: A worksite obesity prevention and intervention trial. Obesity (Silver Spring) 2007;15 (Suppl 1):16S–26S. doi: 10.1038/oby.2007.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Christopher S, Watts V, McCormick AK, Young S. Building and maintaining trust in a community-based participatory research partnership. Am J Public Health. 2008;98(8):1398–406. doi: 10.2105/AJPH.2007.125757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burhansstipanov L, Christopher S, Schumacher SA. Lessons learned from community-based participatory research in Indian country. Cancer Control. 2005;12 (Suppl 2):70–6. doi: 10.1177/1073274805012004s10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strickland CJ. Challenges in community-based participatory research implementation: Experiences in cancer prevention with Pacific Northwest American Indian tribes. Cancer Control. 2006;13(3):230–6. doi: 10.1177/107327480601300312. [DOI] [PubMed] [Google Scholar]
- 22.Minkler M. Ethical challenges for the “outside” researcher in community-based participatory research. Health Educ Behav. 2004;31(6):684–97. doi: 10.1177/1090198104269566. [DOI] [PubMed] [Google Scholar]
- 23.Martin-McDonald K, McCarthy A. ‘Marking’ the white terrain in indigenous health research: literature review. J Adv Nurs. 2008;61(2):126–33. doi: 10.1111/j.1365-2648.2007.04438.x. [DOI] [PubMed] [Google Scholar]
- 24.Noe TD, Manson SM, Cory C, McGough H, Henderson JA, Buchwald DS. The influence of community-based participatory research principles on the likelihood of participation in health research in American Indian communities. Ethn Dis. 2007;17 (Suppl 1):S6–14. [PubMed] [Google Scholar]
- 25.Wallerstein N, Auerbach E, editors. Problem-posing at work: A popular educator’s guide. Edmonton, AB: Grassroots Press; 2004. [Google Scholar]
- 26.Berry TR, Plotnikoff RC, Raine K, Anderson D, Naylor PJ. An examination of the stages of change construct for health promotion within organizations. J Health Organ Manag. 2007;21(2):121–35. doi: 10.1108/14777260710736822. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. Healthier Worksite Initiative. c2007 [cited July 14, 2009]. Available from: http://www.cdc.gov/nccdphp/dnpa/hwi/index.htm.
- 28.Minkler M, Pies C. Improving health through community organization and community participation. In: Minkler IM, editor. Community organizing and community building for health. New Brunswick, NJ: Rutgers University Press; 2005. pp. 26–50. [Google Scholar]