Abstract
The longitudinal course of anxiety disorders in 45 children and adolescents with Williams syndrome was examined. Children were ages 4 to 13 years at the initial assessment. To assess their child’s DSM-IV diagnoses, parents completed a structured diagnostic interview 3 – 9 times at intervals of at least one year. At the first assessment, 60% of the sample presented with at least one anxiety diagnosis; 82.2% received an anxiety diagnosis at some time during the study. Chronic, persistent anxiety within the period 5 years after their initial diagnosis was shown by 62.2% of those with an anxiety diagnosis (51.1% of the entire sample). The most common diagnoses were specific phobias and generalized anxiety disorder. Multilevel logistic regression models were estimated for the presence of any anxiety disorder, specific phobia, and specific phobia of loud noises. Developmental trajectories, expressed as the probability of a positive diagnosis, suggested that the odds of a positive diagnosis did not change with age. IQ was not significantly related to the presence of an anxiety disorder. However, there was a significant relation between executive functioning and anxiety such that the presence of an anxiety diagnosis was associated with increased scores on behavioral regulation, indicative of increased difficulty with inhibitory control of affect and behavior. These findings are discussed in terms of persistence of anxiety over time and the need to develop and test interventions to address the high levels of anxiety experienced by children and adolescents with Williams syndrome.
Keywords: Williams syndrome, anxiety, intellectual disability, developmental trajectory, executive function
INTRODUCTION
Williams syndrome (WS) is a neurodevelopmental disorder caused by deletion of approximately 25 genes on chromosome 7q11.23 [Hillier et al., 2003]. Prevalence is estimated at 1 in 7500 live births [Strømme et al., 2002]. WS has been associated with specific medical, cognitive, and behavioral phenotypes. Medically, the syndrome is associated with mild to moderate intellectual disability, connective tissue abnormalities, characteristic facial features, hypercalcemia, failure to thrive in infancy, cardiovascular disease (particularly supravalvar aortic stenosis), and decreased muscle tone in children [Morris, 2006; Pober & Dykens, 2005]. The cognitive phenotype is characterized by relative strengths in concrete language and verbal short-term memory [Mervis et al., 2000; Mervis and John, 2009] and significant weakness in visuospatial construction [Bellugi et al., 2000; Mervis et al., 2000; Mervis and John, 2009]. Behaviorally, individuals with WS have been described as gregarious, friendly, empathetic, and loquacious [Järvinen-Pasley et al., 2008; Jones et al., 2000; Klein-Tasman and Mervis, 2003; von Arnim and Engel, 1964; Zitzer-Comfort et al., 2007].
Anxiety and fearfulness are also significant aspects of the behavioral phenotype of WS [Dykens, 2003; Einfeld et al., 1997; Einfeld et al., 2001; Einfeld et al., 1999; Leyfer et al., 2006; Leyfer et al., 2009; Porter et al., 2009]. Below, we review the literature to date on the prevalence of anxiety in individuals with WS, cohort studies of anxiety at different ages of individuals with WS, and what is known thus far about the persistence of symptoms over time in individuals with WS. Together, this literature establishes both that anxiety in an important component of the phenotype of WS and that symptoms of anxiety persist over time. We also briefly review the course of anxiety over time in individuals in the general population. The current study extends previous research on anxiety in individuals with WS by examining whether diagnostically significant levels of anxiety are present longitudinally in a sample of children and adolescents with WS. The distinction between the presence of symptoms and the presence of symptoms meeting diagnostic thresholds is important as diagnoses require a constellation of symptoms plus interference and distress, as well as the potential need for intervention. Thus, the current study provides the first longitudinal data on the developmental trajectory of diagnoses of anxiety in WS.
Prevalence of Symptoms of Anxiety in Williams Syndrome
Studies of behavioral characteristics of children with WS consistently find elevations in symptoms of anxiety. For example, Klein-Tasman and Mervis [2003] compared personality features of 8 – 10-year-olds with WS to a CA- and IQ-matched group of children with developmental disabilities of mixed etiologies. Children with WS were significantly more tense than the comparison group. Udwin and Yule [1991] also found that children with WS had higher levels of behavioral and emotional problems, especially anxiety, in comparison to a sample matched on CA, SES, and verbal IQ.
Dykens [2003] presented three studies examining fears and anxiety in individuals aged 6-48 years with WS. In the first two studies, parent- and self-report of fears were examined. Results of both studies supported prior findings of elevated anxiety and fears. Individuals with WS had significantly higher scores on the Fear Survey Schedule for Children-Revised [FSSC-R; Ollendick, 1983] total and all five factor scores in comparison to a matched mixed etiology control group. Examination of the content of fears in both groups suggested some differences by age, with adults and adolescents reporting more fear of criticism and death/danger than did children. There was also an interaction of age and gender, with female adults and adolescents in comparison to female children reporting greater fears of injury and small animals. Although the cohort design precluded examination of the actual course of the fears, it appeared that fears were found across different ages in individuals with WS but that their content may shift somewhat. In the third study, the first to use a DSM-based interview to examine rates of diagnostic levels of phobias and other anxiety disorders, the Diagnostic Interview Schedule for Children-Parent [DICA-P; Reich et al., 1991] was administered to parents/caregivers of 51 individuals with WS, ages 5 – 49 years. Results suggested that many of these fears may reach diagnostically significant levels. Based on DSM-III-R criteria, 35% of the sample met criteria for a specific phobia. In addition, 16% of the sample met diagnostic criteria for overanxious disorder, 4% for separation anxiety disorder, and 2% for obsessive compulsive disorder.
Two research groups have conducted diagnostic studies in which all of the participants were adults. Cherniske and her colleagues [Cherniske et al. 2004] studied a group of adults with WS over the age of 30 years. Nineteen of the 20 participants were described as having clinically significant problems with anxiety. Of the 18 interviewed with a standard diagnostic interview, 13 were diagnosed with moderate to severe anxiety, most often specific phobias or generalized anxiety (frequencies not reported). Stinson et al. [2010] administered the Psychiatric Assessment Schedule for Adults with Developmental Disabilities [PAS-ADD; Moss et al., 1996] to the caregivers of 92 19 – 55-year-olds with WS. The PAS-ADD provides ICD-10 diagnoses of mental health problems, including anxiety disorders. Based on a screening interview, 75 (83%) were identified as having at least one mental health problem. Two of these individuals did not have sufficient linguistic ability to complete the PAS-ADD. The remaining 73 completed this interview, as did caregivers of all 75 individuals. Fifteen people (16.5% of the total sample) met diagnostic criteria for at least one anxiety disorder, with the most common being specific phobia (12% of the total sample). Other anxiety diagnoses included agoraphobia (4 individuals), panic disorder (3 individuals), social phobia (2 individuals), and generalized anxiety disorder (1 individual). Mean IQ was almost identical for individuals who had mental health problems and those who did not. The authors noted that both specific phobias and generalized anxiety disorders may have been under-diagnosed by the PAS-ADD.
Three studies addressing anxiety diagnoses have focused on children and adolescents with WS. Leyfer et al. [2006] examined the prevalence of anxiety disorders in 119 children and adolescents with WS aged 4 – 16 years based on DSM-IV criteria. Use of an interview specifically designed for children and adolescents that is based on current diagnostic criteria allowed careful examination of the rates of diagnostic levels of anxiety. Based on the Anxiety Disorders Interview Schedule for DSM-IV: Parent version [ADIS-P; Silverman and Albano, 1996], Leyfer et al. found that the most prevalent disorder was specific phobia (54% of the sample), followed by generalized anxiety disorder (12%), separation anxiety (7%), and OCD (3%). Kennedy et al. [2006] also used the ADIS to diagnose anxiety disorders in 21 individuals with WS aged 7 – 28 years (mean age 16 years). Ten individuals (48%) received at least one anxiety diagnosis, with the most common being specific phobia (43% of the total sample). Other anxiety diagnoses included generalized anxiety disorder (24%), separation anxiety (5%), panic disorder (5%), agoraphobia (5%), and post-traumatic stress disorder (5%). Leyfer et al. [2009] compared the prevalence of anxiety disorders in 132 4 – 16-year-olds with WS to that reported in epidemiological studies of children from the general population (GP) [Shaffer et al., 2003] and from a population with developmental disabilities [DD; Dekker and Koot, 2003]. Children with WS were found to have significantly higher rates of specific phobias [56.1% (WS); 1.3% (GP); 6.8% (DD)], generalized anxiety [7.6% (WS); 3.1% (GP); 0% (DD)], and separation anxiety [6.1% (WS); 2.3% (GP); 1.9% (DD)].
Course of Symptoms of Anxiety over Time
Together, the literature has established the prevalence of anxiety, both at the symptom and diagnostic levels, in individuals with WS. Several studies have also examined the course of anxiety symptoms over time. Switaj [2000] used parental report measures to examine the course of anxiety behaviors and traits in a cohort design of 190 children, divided into ages 6 – 9, 10 – 13, and 14 – 18 years. On most measures, the oldest group or two older groups scored higher than the youngest group, suggesting that anxiety may increase with age. Leyfer et al. [2006] examined the stability of anxiety diagnoses across time in a cohort design. The sample was divided into three age groups, 4 – 7, 8 – 10, and 11 – 14 years. Prevalence of specific phobias did not differ across the age groups. However, relative to the overall prevalence of generalized anxiety in the WS sample, the prevalence for the youngest group was significantly lower than expected and the prevalence for the oldest group was significantly higher than expected.
Einfeld and colleagues have conducted a series of studies examining the longitudinal course of behavioral and emotional problems in individuals with WS. Einfeld et al. [1997] compared emotional difficulties in 70 children and adolescents with WS to those of an epidemiological control group. After statistically controlling for age, gender, and level of intellectual disability, the WS group was found to score significantly higher on overall levels of emotional and behavioral problems, anxiety, and communication difficulties. The proportion of individuals exceeding the cutoff for probable psychiatric diagnosis was also significantly greater in the WS group [61.4% vs. 40.7%]. In two follow ups to the 1997 study, Einfeld et al. [2002; Time 2] and Tonge and Einfeld [2003; Time 3] examined the persistence of symptoms over time. Five years (Time 2) after the initial assessment, individuals with WS continued to show evidence of emotional and behavioral problems, communication difficulties, and anxiety. Eight years after the initial assessment (Time 3), total behavior problems in the WS group decreased somewhat, although they were still higher than in the comparison sample. The WS group continued to have higher levels of communication difficulties but no longer showed significantly greater levels of anxiety. The WS group also had significantly more behavior problems than a matched epidemiological control group and a matched fragile X syndrome group, but the same level as a matched Prader-Willi syndrome group [Einfeld et al., 1999; Einfeld, 2005]. Together, these studies demonstrate that behavioral and emotional problems are not only prevalent in children with WS but also may persist over time. Einfeld et al.’s results also suggest that these problems may reach the level of diagnostic significance.
Normative Course of Anxiety in Childhood
Anxiety is considered a normative feature of development, with children progressing through what are considered developmentally appropriate stages of anxiety [Beidel and Stanley, 1993; Woodruff-Borden and Leyfer, 2006]. In general, both the content and level of abstraction of anxiety and fears tend to change over time, with a shift from concrete, physical threats to more abstract ones as the capacity for abstract thinking develops [Vasey, 1993]. It is critical to distinguish between transient experiences of childhood and adolescence and those symptoms that are of sufficient significance to cause distress and interference – and thus be diagnostically significant. For the large majority of children, anxiety is a transient experience that does not rise to the level of diagnostically significant anxiety. For those children who are diagnosed with an anxiety disorder, the course of the disorder tends to be relatively unstable over time. For example, Beidel et al. [1996] followed anxious children for 6 months and found that while most remained anxious, their specific diagnosis changed. In a prospective study, Last and colleagues [Last et al., 1996] followed children and adolescents, ages 5 – 18 years, 3 – 4 years after their initial diagnosis of an anxiety disorder. Eighty-two percent of the sample no longer met criteria for their initial diagnosis, with ⅔ of the sample in remission within the first year. Although 31% of the sample met criteria for a specific phobia at the initial assessment, by follow-up only 9.45% met criteria for specific phobia. At follow up, 30% of the full sample had developed a new psychiatric diagnosis, including 16% with a new anxiety diagnosis. These findings suggest that the stability of any specific anxiety diagnosis tends to be rather low in typically developing children, whereas the stability of a diagnosis of any anxiety disorder is somewhat higher. These findings provide a point of comparison to the stability of diagnostic levels of anxiety in children and adolescents with WS.
Current Study
In sum, literature to date has demonstrated that symptoms of anxiety and diagnostic levels of anxiety are highly prevalent in individuals with WS and exceed rates seen in either the general population or epidemiological samples of children with DD. Cohort studies of individuals with WS show that the anxiety is present across age groups, and perhaps even more critically, results from longitudinal studies indicate that symptoms of anxiety in WS persist over time. The question of whether clinically significant diagnostic levels of anxiety similarly persist has not been previously addressed, however. Further, the stability of anxiety diagnoses tends to be relatively low over time in typically developing children. The purpose of the current study was to examine the longitudinal course of clinically significant levels of anxiety over time in children and adolescents with WS. That is, once anxiety is diagnosed in a child with WS, is the course chronic or are there changes over time? Given the cohort findings of age differences in rate of generalized anxiety, we also examined the course of each diagnosis over time. In addition, we addressed the question of whether there was a relation between the presence or absence of an anxiety diagnosis and either IQ or executive functioning, controlling for CA, both at the initial assessment and over time.
METHOD
Participants
Participants were 45 children (24 girls, 21 boys) with genetically-confirmed WS. All of the participants were enrolled in an ongoing longitudinal study of cognitive and language development of individuals with WS conducted at the University of Louisville. The age at first assessment ranged from 4.00 – 13.42 years, with a mean of 6.67 years (SD = 2.89 years). The age at the most recent assessment ranged from 6.02 – 16.95 years with a mean of 10.82 years (SD = 3.04). The median age over all assessments was 8.9 years.
As part of the larger study, the Anxiety Disorders Interview Schedule for DSM-IV: Parent version (ADIS-P) was administered to the parent of every child participant aged 4 years or older each time the child was assessed. Children were included in the current study if their parent had completed the ADIS-P interview at least 3 times. The mean number of assessments per child was 4.91 (range: 3 – 9; SD = 1.74).
Measures
Anxiety Disorders Interview Schedule for DSM-IV: Parent Version (ADIS- P; Silverman and Albano, 1996)
The ADIS-P is a semi-structured interview designed to assess anxiety and related disorders in children and adolescents (through age 16 years). The interview is based on DSM-IV criteria and, in addition to diagnosis, severity ratings from 0 (absent) to 8 (severe) are given for each diagnosis. The ADIS-P has excellent reliability for separation anxiety disorder, social phobia, specific phobia, and generalized anxiety disorder, as well as excellent test-retest reliability of the interview [Silverman et al., 2001]. Although the validity of the ADIS-P has not been reported in samples of children with WS, use of DSM criteria for individuals with mild to moderate intellectual disability is widely accepted [e.g., Brown et al., 2004].
All interviewers were required to meet reliability criteria of three successive matches with training tapes and one final interview reviewed by a licensed clinical psychologist on all diagnoses and severity ratings within one point before conducting interviews. Interviewers were advanced clinical psychology doctoral students or licensed clinical psychologists. All interview protocols were reviewed with the supervising clinical psychologist. Diagnostic disagreements were resolved through discussion. Consistent with DSM criteria, an anxiety disorder was diagnosed only if it caused both interference and distress.
Kaufman Brief Intelligence Test, second edition [KBIT-2; Kaufman and Kaufman, 2004]
The KBIT-2 is an individually administered intellectual ability assessment normed for ages 4 – 89 years, yielding a Verbal standard score, Nonverbal Reasoning standard score, and composite IQ (mean = 100, SD = 15).
Behavior Rating Inventory of Executive Functioning [BRIEF; Gioia et al., 2000]
The BRIEF is an 86-item questionnaire for parents of 6 – 18-year-olds regarding executive functioning behaviors in home and at school. The BRIEF includes 8 scales and yields two summary indices and an overall composite, each reported as a T score (mean = 50, SD = 10, lower scores indicate higher ability). The Behavioral Regulation Index (3 scales) measures the ability to shift cognitive set and to use inhibitory control to monitor both emotions and behavior. The Metacognition Index (5 scales) measures the ability to actively solve problems across a variety of contexts by initiating, planning, organizing, and maintaining future-oriented problem solving in working memory. The Global Executive Composite is a summary measure that incorporates all 8 scales.
Data Analysis Strategy
Our aim was to model within-person change over the study period in the presence of any DSM-IV anxiety diagnosis as measured by the ADIS-P. We also modeled within-person change in the presence of any DSM-IV specific phobia diagnosis (the most common anxiety diagnosis for children with WS; e.g., Leyfer et al., 2006) and in the DSM-IV specific phobia of loud noises diagnosis (the most common specific phobia diagnosis for children with WS; e.g., Leyfer et al., 2006). We also assessed the relations between these diagnoses and measures of executive function (BRIEF BRI and MI) and IQ (KBIT-2 Composite IQ). We used multilevel modeling techniques [Raudenbush et al., 2002; Singer and Willet, 2003] to estimate models that include both estimates of individual change over time and inter-individual variability in change trajectories. Multilevel modeling provides a flexible and powerful method to model developmental change in longitudinal data and has been used extensively with data that tend to be normally distributed (e.g., height, IQ). These techniques can also be applied to binary data (e.g., presence/absence of a disease), although there are considerably more statistical complications (Carlin et al., 2001; Hu et al., 1998; Neuhaus, 2001).
When analyzing longitudinal data, it is important to account for the statistical dependencies or correlations in repeated observations of the same person. Multilevel models accomplish this by specifying models at different hierarchical levels to characterize growth (or decline). For a 2-level model, the Level 1 model describes individual (within-person) change over time. The Level 2 model describes inter-individual (between-person) variability in the change trajectories defined by the parameters of the Level 1 model. In the simplest Level 1 model, individual change over time would be characterized by a linear model which includes only an intercept, typically an indicator of initial status or status at a fixed age, and a slope (change) parameter. The Level 2 model is formulated to account for individual differences in the intercepts and slopes estimated for each individual at the first level. For example, predictors such as gender or socioeconomic status might be introduced at Level 2 to account for individual variability in intercepts and in slopes. (See Singer and Willet, 2003 for detailed conceptual and mathematical accounts of multilevel modeling of longitudinal data).
A major advantage of multilevel modeling is the capacity to handle unbalanced designs. In an unbalanced design, age at the initial measurement and measurement intervals can vary. The data described here constitute an unbalanced design since participants entered the study at different ages. As a first step, models were formulated to determine whether within-person change was independent of the initial age differences [Miyazaki and Raudenbush, 2000; Neuhaus, 2001]. Since there was no evidence of a relation between initial age and within-person change (data not shown), simpler models focusing on within-person change were tested.
One of the first steps in multilevel modeling is to determine the shape of the function defining the within-person change over time (i.e., the Level 1 model). In many cases a linear model is adequate to model change over a limited age range or time period. For example, to model the change in IQ as a function of chronological age (CA) and anxiety diagnosis, the Level 1 model, which estimated an intercept (predicted score at age 9 years) and slope (annual rate of change) for each participant, is specified in the equation below:
| (1) |
In the Level 1 equation, represents the predicted KBIT-2 Composite IQ score for person i at CA t and Xti is person i’s anxiety diagnosis (present or absent) at CA t. The median age of 9 years was subtracted from CA. This procedure, which is referred to as centering age, is recommended because it enables a more meaningful interpretation of the intercept and often increases the stability of the model estimation [Raudenbush et al., 2002; Singer and Willet, 2003]. The parameters π0i and π1i are each individual’s intercept and linear CA slope. The effect of anxiety is indicated by π2i and is a time-varying parameter. The residual error term εti indicates the amount of error in predicting the person’s IQ at a given CA, controlling for the anxiety diagnosis.
In the Level 2 model, the individual parameter estimates from the Level 1 model are the outcome variables and the model is formulated to determine if there is significant inter-individual variability in the developmental trajectories. The Level 2 model typically includes an equation for each Level 1 parameter:
| (2) |
where βk is the average, over individuals, for each of the k parameter estimates. Additionally time-invariant predictors such as gender could be included in the Level 2 models as explanatory variables. The parameter averages are also referred to as fixed effects and each can be evaluated by a significance test. The rki are person-specific (e.g., intercept) residuals and are assumed to be normally distributed about their respective averages with variances, σk2. These variances represent the random effects of the model and are estimates of between-person variability or individual differences.
The multilevel logistic regression can be used to assess developmental change for longitudinal dichotomous data such as the presence or absence of any anxiety diagnosis. This approach is particularly useful when individual differences are considered important as compared to methods which estimate “population-average” effects, treating between-person and within-person effects as indistinguishable (Hu et al., 1998). The Level 1 model is:
| (3) |
where pki is the predicted probability of a positive diagnosis and π0 and π1 are the intercept and slope. In this model the intercepts are allowed to vary among individuals. The Level 2 model for the intercept πki is identical to equation (2). The Level 2 model for slope πki estimates a common slope for all individuals. The intercept fixed effect, β0, represents the log odds of a positive diagnosis for the average individual (i.e., rki = 0) and the slope, β1, estimates the annual rate of change in the log odds.
The software package HLM 6.0 [Raudenbush et al., 2004] was used to fit the multilevel models. The models were fit using restricted maximum likelihood estimation. For the multilevel logistics models, unit-specific estimates of fixed effects with robust errors are reported.
RESULTS
Rate of Anxiety in the Sample
The presence of anxiety at the first ADIS-P administration was examined. Of the 45 children, 27 presented with at least one anxiety diagnosis at their first assessment, translating to a rate of 60%. Next, we examined the rate of anxiety diagnosed at any time during the period the child was assessed. A total of 37 children (82.2% of the sample) met diagnostic criteria for at least one anxiety disorder at some point during the study.
Persistence of Anxiety
To control for the different numbers of assessments across children, we operationally defined persistence as an anxiety diagnosis present in at least 50% of all assessments subsequent to the initial diagnosis. Of the 37 children diagnosed with anxiety at some time during the study, 62.2% (51.1% of total sample) showed chronic, persistent anxiety. Thus, once a child with WS experiences clinically significant anxiety, the normative course is for the anxiety and its associated distress to persist over time.
As shown in Table I, the most common diagnoses were specific phobias and generalized anxiety disorder. For each diagnostic category, we examined the proportion of children continuing to meet diagnostic criteria within the period 5 years after their initial diagnosis. The proportion of children continuing to experience diagnostic levels of anxiety was considerable. As shown in Table I, 74% of those with a phobia of loud noises continued to have that fear during the 5 year period; 63% with other specific phobias also showed chronicity of their fear. Blood-injury-injection phobias also tended to persist over time. Interestingly, there was more variability in animal phobias and generalized anxiety. In part, this appears due to the range of ages for the initial diagnosis.
Table I. Frequency and Persistence of Anxiety Diagnoses.
| Diagnosis | N (out of 45) with diagnosis |
N meeting criteria within 5 years of initial diagnosis |
Percent meeting criteria within 5 years of initial diagnosis (Persistent anxiety) |
|---|---|---|---|
| Specific phobia- loud noises | 27 | 20 | 74.1% |
| Specific phobia-other | 19 | 12 | 63.2% |
| Specific phobia-blood-injury- injection |
18 | 11 | 61.1% |
| Specific phobia-animals | 13 | 5 | 38.5% |
| Specific phobia-natural environment |
7 | 3 | 42.9% |
| Generalized Anxiety Disorder |
7 | 3 | 42.9% |
| Social phobia | 3 | 1 | 33.3% |
| Separation anxiety | 5 | 1 | 20.0% |
Note: Obsessive compulsive disorder was diagnosed in only one case; none of the participants was diagnosed with panic disorder or post traum atic stress disorder.
Table II illustrates the diagnostic profile for each child. Of note is the variability in timing of diagnosis of each disorder. Despite the relatively small sample size, it is clear that anxiety is prevalent, but that the type of anxiety does not appear related to age per se. Rather, it is apparent that once a child with WS is diagnosed with anxiety, the probability of his or her developing additional anxiety disorders is quite significant. Of those children with anxiety, 26 of 36 (72.2%) developed additional anxiety disorders diagnosed at assessments subsequent to the initial diagnosis of anxiety. One participant was excluded from this analysis because anxiety was first diagnosed at the most recent assessment, precluding a test of the subsequent development of anxiety in this case. Thus, using a total sample of 36 anxious children, we calculated the probability of diagnoses of anxiety subsequent to the first diagnosis. Last et al. (1996) reported that 16% of their prospective clinical sample of typically developing children developed at least one additional anxiety diagnosis after the initial assessment. Using 0.16 as the probability that a child will develop an additional anxiety diagnosis beyond that identified in an initial assessment, the identified proportion for the WS sample of 0.72 is significantly greater than the predicted probability, as indicated by a binomial test (p < .00001). The WS probability of 0.72 also significantly exceeds that of a chance 0.50 probability (yes/no additional diagnoses; p < .011). Additionally, the presence of one specific phobia appears to increase the likelihood of diagnosis of additional specific phobias. The frequency of additional diagnoses suggests generalization of anxiety over time.
Table II. Course of Anxiety by Child.
| Age (in years) at first assessment |
Anxiety diagnoses at first assessment |
Number of assessments |
Additional anxiety diagnoses (age first diagnosed) |
Age at most recent assessment |
Anxiety diagnoses at most recent assessment |
|---|---|---|---|---|---|
| 4 | None | 8 | None | 13 | None |
| 4 | Separation Anxiety | 5 | Social phobia (10) SP-Loud noises (10) |
10 | Separation Anxiety Social phobia SP-Loud noises |
| 4 | SP-Loud noises | 9 | SP-Animals (6) SP-B-I-I (9) SP-Natural environ. (11) |
13 | SP-Animals SP-B-I-I |
| 4 | SP-Animals | 9 | SP-Loud noises (11) | 13 | None |
| 4 | None | 6 | SP-Animals (8) SP-Loud noises (9) |
10 | SP-Animals SP-Loud noises |
| 4 | None | 8 | SP-Loud noises (6) SP-Animals (9) |
11 | None |
| 4 | SP-Animals | 5 | SP-B-I-I (7) SP-Loud noises (9) GAD (10) |
10 | GAD SP-Animals |
| 4 | SP-Loud noises SP-Animals |
5 | SP-Natural environ. (6) | 8 | None |
| 4 | SP-Loud noises | 4 | SP-Animals (5) SP-Natural environ. (6) SP-B-I-I (6) |
7 | SP-B-I-I SP-Animals SP-Loud noises |
| 4 | SP-Loud noises | 3 | None | 8 | None |
| 4 | None | 3 | None | 7 | None |
| 4 | SP-Animals SP-Loud noises |
4 | GAD (7) | 7 | GAD |
| 4 | None | 4 | SP-Animals (5) SP-Loud noises (5) SP-B-I-I (6) |
7 | SP-B-I-I SP-Loud noises SP-Animals |
| 4 | None | 4 | SP-Animals (5) SP-Loud noises (5) |
7 | None |
| 4 | SP-Animal SP-B-I-I SP-LN |
5 | SP-Natural environ. (7) | 8 | SP-Animals SP-B-I-I |
| 4 | Separation Anxiety SP-B-I-I SP-Animals |
4 | SP-Loud noises (5) SP-Natural environ. (6) |
9 | SP-B-I-I SP-Animals SP-Loud Noises |
| 4 | None | 4 | SP-Animals (5) SP-Loud noises (5) |
7 | SP-Loud Noises SP-Animals |
| 4 | SP-Loud Noises | 4 | SP-Animals (5) | 7 | SP-Animals SP-Loud Noises |
| 4 | None | 3 | None | 6 | None |
| 4 | None | 3 | SP-Animals (5) | 6 | None |
| 5 | SP-B-I-I SP-Animals |
5 | GAD (10) SP-Loud noises (10) SP-Natural environ. (11) |
14 | SP-Animals SP-B-I-I SP-Loud Noises |
| 5 | SP-Animals | 6 | SP-B-I-I (7) SP-Loud noises (7) GAD (7) |
11 | None |
| 5 | SP-B-I-I SP-Animals |
6 | None | 11 | None |
| 5 | None | 8 | SP-B-I-I (8) | 13 | None |
| 5 | None | 4 | None | 10 | None |
| 5 | None | 6 | SP-Animals (8) SP-Loud noises (8) SP-B-I-I (9) |
10 | None |
| 5 | None | 6 | None | 10 | None |
| 5 | Separation Anxiety SP-Loud noises |
3 | SP-Animals (6) SP-Natural environ. (10) |
10 | SP-Natural environ. |
| 5 | SP-Animals SP-B-I-I SP-Loud noises |
3 | None | 7 | None |
| 6 | None | 6 | SP-Animals (9) SP-Loud noises (10) |
11 | SP-Animals |
| 6 | SP-Loud noises | 4 | SP-Animals (7) GAD (7) SP-B-I-I (8) |
9 | SP-Animals SP-Loud noises GAD |
| 7 | None | 6 | None | 13 | None |
| 7 | None | 3 | None | 9 | None |
| 8 | SP-B-I-I SP-Animal |
8 | SP-Loud noises (11) GAD (14) SP-Natural environ. (15) |
16 | SP-Natural Environ. |
| 8 | SP-Animals | 4 | SP-B-I-I (9) | 13 | SP-B-I-I |
| 9 | SP-B-I-I | 6 | None | 16 | SP-B-I-I |
| 9 | SP-B-I-I | 7 | SP-Animals (13) | 15 | None |
| 10 | SP-B-I-I | 3 | SP-Loud noises (14) | 14 | SP-Loud noises |
| 10 | None | 4 | SP-Natural environ. (14) | 14 | SP-Natural environ. |
| 10 | GAD | 4 | SP-B-I-I (11) | 13 | SP-B-I-I |
| 11 | SP-Natural environ. | 3 | SP-Animals (14) | 14 | SP-Animals |
| 11 | Separation Anxiety SP-B-I-I SP-Animals |
4 | None | 14 | None |
| 12 | GAD | 5 | OCD (13) SP-Loud Noises (14) SP-Animals (15) |
16 | GAD SP-Natural environ. |
| 12 | None | 4 | None | 15 | None |
| 13 | SP-Animals SP-Loud noises |
3 | None | 15 | SP-Loud noises |
Abbreviations: SP: Specific phobia, B-I-I: Blood-Injury-Injection, GAD: Generalized anxiety disorder
We also examined the rate of treatment for anxiety in the sample. Thirteen children were medicated at some point in the study for anxiety (28.9% of the total sample). Of these, 9 (or 69.2% receiving medication) continued to meet the operational definition of chronic anxiety; 3 were not diagnosed during the study as anxious; and 1 was diagnosed as anxious, but not chronically so. A total of 8 children received psychotherapy for anxiety (17.8% of the total sample). Of these, 6 (or 75% of those receiving therapy) continued to meet the operational definition for chronic anxiety whereas 2 were not diagnosed as anxious during the study.
Multilevel Logistic Regression Models
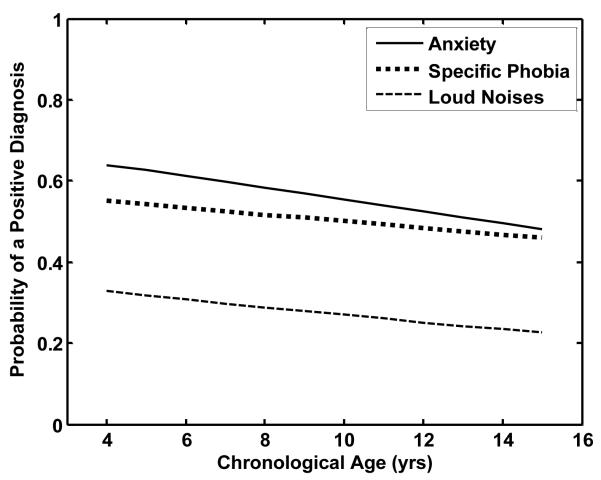
Multilevel logistic regression models were estimated to evaluate the change over time in the presence of any anxiety disorder, specific phobia, and specific phobia of loud noises. As discussed above, models were specified such that the odds of a positive diagnosis could vary across individuals. Table III summarizes the results of these analyses. The developmental trajectories, expressed as the probability of a positive diagnosis, are shown in Figure 1. The predicted logits were converted to probabilities by:
| (4) |
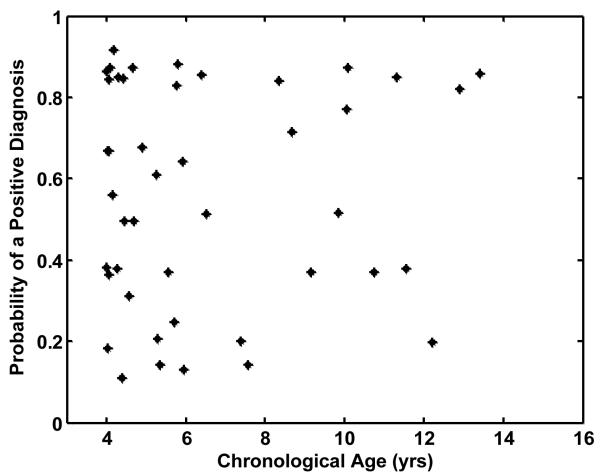
The estimated slopes are not significant in any of the models, suggesting that the odds of a positive diagnosis did not change with age. For the anxiety diagnosis model, the fixed effect for intercept was not significant, suggesting that the odds of a positive diagnosis (e.28 = 1.32) at the median age of 9 years do not differ significantly from 1.0 for the average individual. However the test of intercept variance was significant which implies significant individual variability in the odds or predicted probability. The individual intercepts plotted as predicted probabilities are plotted as a function of each individual’s age at the time he or she entered the study. As can be seen from the figure, this individual variability is not related to differences in participants’ age at the beginning of the study.
Table III.
Multilevel modeling statistics for ADIS developmental trajectories
| Fixed Effects | Coefficient | Standard Error |
T Ratio (df) | p |
|---|---|---|---|---|
| Anxiety Model | ||||
| Intercept (log odds at CA= 9) β0 | 0.28 | 0.29 | 0.95 (44) | 0.348 |
| Slope (annual change) β1 | −0.06 | 0.06 | −0.97 (224) | 0.331 |
| Specific Phobia Model | ||||
| Intercept (log odds at CA= 9) β0 | 0.07 | 0.27 | 0.14 (44) | 0.894 |
| Slope (annual change) β1 | −0.03 | 0.06 | −0.58 (224) | 0.563 |
| Loud Noises Model | ||||
| Intercept (log odds at CA= 9) β0 | −0.95 | 0.26 | −3.69 (44) | 0.001 |
| Slope (annual change) β1 | −0.05 | 0.07 | −0.72 (224) | 0.479 |
| Random Effects | Standard Deviation |
Variance | X2 (df) | p |
|---|---|---|---|---|
| Anxiety Intercept r0 | 1.64 | 2.70 | 131.0 (44) | <.0001 |
| Specific Phobia Intercept r0 | 1.47 | 2.16 | 120.9 (44) | <.0001 |
| Loud Noises Intercept r0 | 1.32 | 1.75 | 105.4 (44) | <.0001 |
Figure 1.
Predicted developmental trajectories for ADIS Anxiety, Specific Phobia and Specific Phobia of Loud Noises. The estimated probability of a positive diagnosis for the average individual is plotted.
The results for the specific phobia diagnosis were very similar. The odds of a positive Specific Phobia diagnosis at age 9 of 1.03 were not significantly different from 1.0. However, the average intercept was significant for the phobia for loud noises. The odds of a positive diagnosis are 0.38 which is significantly less than 1.0. The test of intercept variance is significant, indicating significant variability among individuals in the odds of a positive diagnosis.
Relation of Anxiety to IQ and Executive Functioning
Multilevel modeling was used to test the relation between the presence of an anxiety diagnosis and KBIT-2 Composite IQ. The 40 participants who had 3 or more KBIT-2 assessments were included in the analysis. The Level 1 linear model (i.e., Equation 1) included an intercept which estimated Composite IQ at age 9 years, Composite IQ slope, and anxiety diagnosis. The results of the model are summarized in Table IV. The average Composite IQ at age 9 years for individuals who did not have an anxiety diagnosis was 79.1. The average IQ was 1 point lower for a positive diagnosis (78.2); this difference is not statistically significant. The CA slope of −0.03 also was not significant, which suggests that average Composite IQ remained relatively constant over time. However, the significance tests for IQ intercept and slope variances were significant, reflecting individual differences in developmental trajectories.
Table IV.
Multilevel modeling statistics for KBIT-2 Composite IQ developmental trajectories
| Fixed Effects | Coefficient | Standard Error |
T Ratio (df) | p |
|---|---|---|---|---|
| Intercept (mean at CA= 9) β0 | 79.13 | 2.10 | 36.86 (39) | <.0001 |
| Slope (annual change) β1 | −0.03 | 0.44 | −0.08 (39) | 0.934 |
| Anxiety (positive diagnosis) | −0.95 | 1.18 | −0.89 (157) | 0.376 |
| Random Effects | Standard Deviation |
Variance | X2 (df) | p |
|---|---|---|---|---|
| Intercept r0 | 11.71 | 137.24 | 499.00 (39) | <.0001 |
| Slope r1 | 2.26 | 5.12 | 109.03 (39) | <.0001 |
Although not reported here, similar results were obtained for a model predicting IQ from the specific phobia diagnosis. Because the incidence of specific phobia to loud noises was relatively low, we did not relate this diagnosis to IQ.
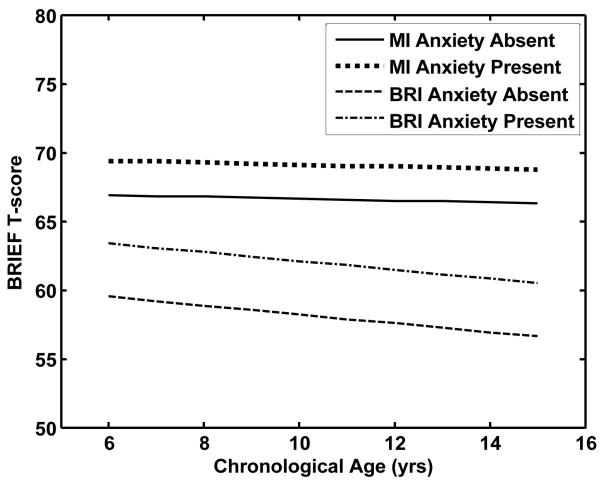
The effect of an anxiety disorder on the developmental trajectories for the BRIEF BRI and MI T-scores was estimated in separate multilevel linear models (e.g., Equations 1 and 2). The parameters estimated in the Level 1 linear model were intercept, CA slope, and presence of an anxiety disorder. This analysis was performed on the 33 participants whose parents had completed the BRIEF at least three times (after the age of 6 years). The multilevel modeling results are summarized in Table V. For the BRIEF BRI the estimated intercept was 58.5, providing an estimate of the average T-score at age 9 years when the anxiety disorder diagnosis was negative. A positive anxiety disorder diagnosis resulted in a significant average increase of 3.9 points (62.4). The test of intercept variance was significant, indicating significant individual differences in overall level. The average slope of −0.32 was not significant, suggesting that the average BRI T-score did not change with age. Nor was the test of variability in individual slopes significant. The average developmental trajectories for the predicted BRIEF BRI T-scores for positive and negative ADIS Anxiety disorder diagnoses are shown in Figure 3.
Table V.
Multilevel modeling statistics for BRIEF BRI and MI developmental trajectories
| Fixed Effects | Coefficient | Standard Error |
T Ratio (df) | p |
|---|---|---|---|---|
| BRI Model | ||||
| Intercept (mean at CA=9)β0 | 58.52 | 1.59 | 36.75(32) | <.0001 |
| Slope (annual change) β1 | −0.32 | 0.33 | −0.97(32) | 0.338 |
| Anxiety(positive diagnosis) β2 | 3.90 | 1.38 | 2.82 (147) | 0.006 |
| MI Model | ||||
| Intercept (mean at CA=9) β0 | 66.69 | 1.31 | 50.95 (32) | <.0001 |
| Slope (annual change) β1 | −0.07 | 0.28 | −0.26 (32) | 0.800 |
| Anxiety (positive diagnosis) β2 | 2.46 | 1.61 | 1.53 (147) | 0.127 |
| Random Effects | Standard Deviation |
Variance | X2 (df) | p |
|---|---|---|---|---|
| BRI Intercept r0 | 7.96 | 63.41 | 148.39 (31) | <.0001 |
| BRI Slope r1 | 0.60 | 0.36 | 40.72 (31) | 0.114 |
| MI Intercept r0 | 5.37 | 28.89 | 83.60 (31) | <.0001 |
| MI Slope r1 | 0.54 | 0.30 | 44.07 (31) | 0.160 |
Figure 3.
Predicted average developmental trajectories for BRIEF Metacognition Index (MI) and Behavioral Regulation Index (BRI) T-scores. Functions are plotted separately for positive and negative ADIS Anxiety diagnoses.
On average the T scores were higher for the BRIEF MI. The average intercept was 66.7 for a negative anxiety diagnosis and 69.2 for a positive Anxiety diagnosis. This difference was not significant. However, the intercept variance was significant indicating individual variability in overall level. The average slope of −0.07 was not significant nor was the slope variance. The average developmental trajectories for the BRIEF MI T-scores are also shown in Figure 3. Models were tested relating the BRIEF BRI and MI T-scores to specific phobia diagnosis. Results were very similar and thus not reported here.
DISCUSSION
The experience of anxiety is highly prevalent in individuals with WS. Diagnostic rates exceed those for both the general population and etiological samples with DD [e.g., Cherniske et al., 2004; Leyfer et al., 2006; Leyfer et al., 2009]. Further, anxiety is present at different ages and the symptoms appear to persist over time [Einfeld et al., 1997; Tonge and Einfeld, 2003]. However, until now little had been known about the stability of diagnoses of anxiety over time. The current study addressed three specific questions regarding diagnostic stability. First, is the course of anxiety chronic in individuals with WS? Second, what is the course for specific anxiety diagnoses? Third, is there a relation between the presence of anxiety and IQ or executive functioning?
Consistent with prior findings [e.g., Dykens, 2003; Leyfer et al., 2006; Leyfer et al., 2009], a significant proportion of the current sample received at least one anxiety diagnosis, with a point prevalence rate of 60% at the time of the initial assessment. The prevalence over the course of the study was 82.2%, meaning that more than ¾ of the sample received an anxiety diagnosis at some point during the study. Unlike children who are developing typically, for whom there is a significant remission within the first year of an anxiety diagnosis [Last et al., 1996], in the current study children and adolescents with WS showed a chronic course of anxiety. The developmental trajectories showed no significant effect of age, demonstrating that the presence of an anxiety diagnosis for children and adolescents with WS is not related to age. That is, the odds of a positive diagnosis for an individual with WS do not change over time. Thus, once diagnosed, anxiety tends to persist at clinically significant levels.
Examination of types of anxiety disorders supports a similar pattern. Although the base rate of some disorders in the current sample was too low to examine, rates of specific phobias and some types of specific phobias could be examined. As with the presence of any anxiety diagnosis, these also tended to remain stable. Unlike prior cross-sectional studies suggesting changes in the content of fears of individuals with WS at different ages [Dykens, 2003], the current sample showed considerable stability in their specific phobias. The differences in study designs likely account for these different findings. Specific phobias were present at each age group assessed in Dykens’ study, allowing aggregation of group data about phobias but no information about the specific phobias of individuals over time. In addition, Dykens included a considerably broader age range in her study, from early school age through middle-adulthood. The longitudinal design of the current study allowed us to assess each participant’s fears over multiple time periods, allowing a precise examination of each individual’s pattern of phobias. When compared over time, the content of phobias shows stability. Phobias of loud noises and of blood-injury-injection show a stability rate in excess of 60% over a five year period. Interestingly, additional phobias develop but the original ones do not resolve, suggesting generalization of anxiety over time as opposed to a shift in the content of the fear. This generalization suggests that the anxiety does not resolve over time nor does it simply shift in content; rather, it becomes associated with additional feared objects and situations.
Overall, the current data suggest that diagnostically significant levels of anxiety persist over time and are not related to age. We were also interested in examining whether the presence of anxiety disorders was related over time to intellectual or executive functioning. There is some indication that the content of fears changes in TD children as they develop cognitively [Vasey, 1993]. That is, as children become more abstract in their thinking, the content of their fears tends to parallel the development of abstract thinking. Thus, a younger child who fears the dark and monsters may become fearful of more abstract concerns such as social rejection as they develop the capacity for less concrete thinking. Consistent with prior studies [Dodd and Porter, 2009; Leyfer et al., 2006, Stinton et al., 2010], the current results showed no relation between IQ and the presence of an anxiety disorder. However, there was a relation between executive functioning and anxiety such that the presence of an anxiety diagnosis was associated with increased (worse) scores on behavioral regulation, suggesting increased difficulty with inhibitory control of affect and behavior. This relation does not change over time as a function of age. As would be expected, a significant proportion of the current sample also presented with attention deficit/hyperactivity disorder (ADHD) which has been associated with impairments in executive functioning in children who are typically developing [Willcutt et al., 2005]. Dodd and Porter [2009] did not find differences in cognitive variables in a sample of individuals with WS with or without a diagnosis of ADHD or with or without a diagnosis of an anxiety disorder. Similarly, Leyfer et al. [2009] found that Differential Ability Scales [DAS; Elliott, 1990] General Conceptual Ability (GCA; similar to IQ) was almost identical for children with and without an anxiety diagnosis. Furthermore, DAS GCA was almost identical for children with and without an ADHD diagnosis.
Treatment Implications
Together with prior research, the present findings suggest that for individuals with WS, anxiety is highly prevalent, does not remit, and generalizes over time. Our longitudinal findings provide compelling rationale for the need to develop prevention and intervention programs. Limited attention has been paid to the mental health needs of individuals with WS. Data from the current study underscore that only a small proportion of our sample was being treated for anxiety, either with medication or therapy, and that even among those who were receiving treatment, most continued to experience chronic anxiety. Despite significant prevalence and chronicity of anxiety in children with WS, treatment of this anxiety remains largely ignored in the literature. To date there have been no controlled studies examining anxiety treatment outcome for individuals with WS. However, a few single case studies have reported success in using cognitive behavioral approaches for various problems. O’Reilly and Lancioni [2001] presented a case of child with acting out and feeding problems. They demonstrated decreased misbehavior and increased positive feeding through the use of behavioral approaches such as time limits and praise. Klein-Tasman and Albano [2007] successfully used exposure and response prevention to decrease obsessive compulsive behaviors in a young adult man with WS. More recently, Phillips and Klein-Tasman [2009] presented two cases of adolescent females with WS, each with multiple anxiety disorders including GAD and specific phobias. The results were mixed, with measures generally showing improvement in worry and symptoms of GAD, but more limited improvement in treatment of specific phobias.
Collectively, these case studies demonstrate that empirically supported approaches can be effectively used in individual cases. Extending this work to larger samples will allow demonstration of efficacy and adaptation of treatment methods to the needs of individuals with WS. The prevalence, chronicity, and apparent generalization of specific phobias make them an ideal target for initial intervention trials. Few empirically supported interventions are geared toward treatment of phobias in children. However, researchers have identified a number of critical components of fear reduction, the most important of which include gradual exposure to feared stimuli and remaining in contact with the stimuli until fear begins to diminish (Barlow, 2002; Craske, 1999; Hazlett-Stevens and Craske, 2008). Gradual exposure provides the basis for fear reduction or habituation. Unlike other methods of anxiety reduction that rely on more cognitively oriented approaches, gradual exposure offers the advantage of being applicable across a range of cognitive ability levels.
Several issues seem particularly critical in testing anxiety reduction treatments for children and adolescents with WS. First, it is crucial to note that all of the case studies relied on parental involvement for interventions. This approach, a common occurrence in treatment of typically developing children as well, seems particularly critical for the successful treatment of anxiety in children and adolescents with WS. Parental support in exposure and consistent parental responses when the child encounters feared stimuli are vital for successful habituation and fear reduction. Second, it also will be critical to examine the impact of treatment of one phobia on the pattern of generalization to other feared stimuli. Third, as treatments are tested, longitudinal follow up will be important to establish reduction in not only the target fear, but the likelihood of developing additional phobias. In addition to exposure as a treatment for phobias, the presence of multiple anxiety disorders and frequent co-morbidity with other diagnoses such as ADHD will require development of empirically supported approaches to manage the complexity of each individual’s clinical presentation.
Limitations of the Current Study
Although this study provides the first longitudinal examination of the course of anxiety diagnoses in children and adolescents with WS, the results need to be considered in light of several limitations. Ideally, age of entry into the study would be standardized so that examination of the progression of diagnoses over time, controlling for age at assessment, would be possible. Additional adolescent time-points would also allow further consideration of the progression of diagnoses over time. The low incidence of several of the anxiety disorders such as panic or social anxiety within WS samples, including the current study, precludes more detailed examination of the course of all of the anxiety disorders. However, studies to date suggest that this is an empirical reality of the anxiety experienced within WS samples; in addition to the present study, all four diagnostic studies that included child and adolescent participants [Dodd and Porter, 2009; Kennedy et al., 2006; Leyfer et al., 2006; Leyfer et al., 2009] reported the highest prevalence for specific phobia and the next highest prevalence for generalized anxiety disorder, with all other anxiety diagnoses at very low levels or not occurring at all in the samples tested. We relied on parental report for the diagnosis of anxiety. As individuals’ experiences of anxiety become more internal and less visible, this method of data collection, while necessary, precludes more thorough assessment of the less overt signs of anxiety such as worry. Finally, we focused on the developmental course of anxiety and did not address diagnostic comorbidity of anxiety disorders with other types of disorders. In the future, comorbidity will be important to consider, especially with regard to the relations among ADHD, anxiety, and behavioral and affect regulation over time.
In sum, the present study demonstrated the persistence of clinically significant levels of anxiety in a longitudinal sample of children and adolescents with WS, demonstrating that the experience of anxiety is highly prevalent, does not remit, and also appears, particularly with regard to specific phobias, to generalize over time. Together, these data present a compelling need to address the experience of anxiety in individuals with WS through the development of empirically supported prevention and intervention approaches.
Figure 2.
Individual differences in the predicted probability of a positive ADIS Anxiety diagnosis at age 9 years (i.e., intercept). The estimates are plotted as a function of the age that the individual entered the study.
Acknowledgements
We very much appreciate the enthusiastic participation of the children with Williams syndrome and their parents in our research. This project was supported by National Institute of Neurological Disorders and Stroke grant R01 NS35201 and by National Institute of Child Health and Human Disorders grant R37 HD29957.
REFERENCES
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd edition Guilford; New York: 2002. [Google Scholar]
- Beidel DC, Stanley MA. Developmental issues in the measurement of anxiety. In: Last CG, editor. Anxiety across the lifespan: A developmental perspective. Springer; New York: 1993. pp. 167–203. [Google Scholar]
- Bellugi U, Klima ES, Wang PP. Cognitive and neural development: Clues from genetically based syndromes. In: Magnussen D, editor. The life-span development of individuals: Behavioral, neuro-biological, and psychosocial perspectives. Cambridge University Press; New York: 1996. pp. 223–243. [Google Scholar]
- Bellugi U, Lichtenberger L, Jones W, Lai Z, St. George M. I. The neurocognitive profile of Williams syndrome: A complex pattern of strengths and weaknesses. J Cogn Neurosci. 2000;12:7–29. doi: 10.1162/089892900561959. [DOI] [PubMed] [Google Scholar]
- Brown EC, Aman MG, Lecavalier L. Empirical Classification of Behavioral and Psychiatric Problems in Children and Adolescents With Mental Retardation. Am J Ment Retard. 2004;109:445–455. doi: 10.1352/0895-8017(2004)109<445:ECOBAP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Carlin JB, Wolfe R, Brown CH, Gelman A. A case study on the choice, interpretation and checking of multilevel models for longitudinal binary outcomes. Biostatistics. 2001;2:397–416. doi: 10.1093/biostatistics/2.4.397. [DOI] [PubMed] [Google Scholar]
- Cherniske EM, Carpenter TO, Klaiman C, Young E, Bregman J, Insogna K, Schultz RT, Pober BR. Multisystem study of 20 older adults with Williams syndrome. Am J Med Genet Part A. 2004;131A:255–264. doi: 10.1002/ajmg.a.30400. [DOI] [PubMed] [Google Scholar]
- Craske MG. Anxiety disorders: Psychological approaches to theory and treatment. Basic Books; New York: 1999. [Google Scholar]
- Dekker MC, Koot HM. DSM-IV Disorders in Children With Borderline to Moderate Intellectual Disability. I: Prevalence and Impact. J Am Acad Child Adolesc Psychiatry. 2003;42:915–922. doi: 10.1097/01.CHI.0000046892.27264.1A. [DOI] [PubMed] [Google Scholar]
- Dodd HF, Porter MA. Psychopathology in Williams syndrome: The effect of individual differences across the life span. J Ment Health Res Intellect Disabil. 2009;2:89–109. [Google Scholar]
- Dykens EM. Anxiety, fears, and phobias in persons with Williams syndrome. Dev Neuropsychol. 2003;23:291–316. doi: 10.1080/87565641.2003.9651896. [DOI] [PubMed] [Google Scholar]
- Einfeld S, Tonge B, Turner G, Parmenter T, Smith A. Longitudinal course of behavioural and emotional problems of young persons with Prader-Willi, Fragile X, Williams and Down syndromes. J Intellect Dev Disabil. 1999;24:349–354. [Google Scholar]
- Einfeld SL. Behavior problems in children with genetic disorders causing intellectual disabililty. Educ Psychol. 2005;25:341–346. [Google Scholar]
- Einfeld SL, Tonge BJ, Florio T. Behavioral and emotional disturbance in individuals with Williams syndrome. Am J Ment Retard. 1997;102:45–53. doi: 10.1352/0895-8017(1997)102<0045:BAEDII>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Einfeld SL, Tonge BJ, Rees VW. Longitudinal course of behavioral and emotional problems in Williams syndrome. Am J Ment Retard. 2001;106:73–81. doi: 10.1352/0895-8017(2001)106<0073:LCOBAE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior Rating Inventory of Executive Function. Child Neuropsychol. 2000;6:235–238. doi: 10.1076/chin.6.3.235.3152. [DOI] [PubMed] [Google Scholar]
- Hazlett-Stevens H, Craske MG. Live (in vivo) exposure. In: O’Donohue WT, Fisher JE, editors. Cognitive behavior therapy: Applying empirically supported techniques in your practice. Wiley; Hoboken, NJ: 2008. pp. 309–316. [Google Scholar]
- Hillier LW, Fulton RS, Fulton LA, Graves TA, Pepin KH, Wagner-McPherson C, et al. The DNA sequence of human chromosome 7. Article. Nature. 2003;424:157. doi: 10.1038/nature01782. [DOI] [PubMed] [Google Scholar]
- Hu FB, Goldberg J, Hedeker D, Flay BR, Pentz MA. Comparison of population-averaged and subject-specific approaches for analyzing repeated binary outcomes. Am J Epidemiol. 1998;147:694–703. doi: 10.1093/oxfordjournals.aje.a009511. [DOI] [PubMed] [Google Scholar]
- Järvinen-Pasley A, Bellugi U, Reilly J, Mills DL, Galaburda A, Reiss AL, et al. Defining the social phenotype in Williams syndrome: A model for linking gene, the brain, and behavior. Dev Psychopathol. 2008;20:1–35. doi: 10.1017/S0954579408000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones W, Bellugi U, Lai Z, Chiles M, Reilly J, Lincoln A, et al. II. Hypersociability in Williams syndrome. J Cogn Neurosci. 2000;12:30–46. doi: 10.1162/089892900561968. [DOI] [PubMed] [Google Scholar]
- Kaufman AS, Kaufman NL. Kaufman Brief Intelligence Test. second edition American Guidance Services; Circle Pines, MN: 2004. [Google Scholar]
- Kennedy JC, Kaye DL, Sadler LS. Psychiatric diagnoses in patients with Williams syndrome and their families. Jefferson J Psychiatry. 2006;20:22–31. [Google Scholar]
- Klein-Tasman BP, Albano AM. Intensive, short-term cognitive behavioral treatment of OCD-like behavior with a young adult with Williams syndrome. Clin Case Stud. 2007:483–492. [Google Scholar]
- Klein-Tasman BP, Mervis CB. Distinctive personality characteristics of 8-, 9-, and 10-year-olds with Williams syndrome. Dev Neuropsychol. 2003;23:269–290. doi: 10.1080/87565641.2003.9651895. [DOI] [PubMed] [Google Scholar]
- Last CG, Perrin S, Hersen M, Kazdin AE. A prospective study of childhood anxiety disorders. J Am Acad Child Adolesc Psychiatry. 1996;35:1502–1510. doi: 10.1097/00004583-199611000-00019. [DOI] [PubMed] [Google Scholar]
- Leyfer OT, Woodruff-Borden J, Klein-Tasman BP, Fricke JS, Mervis CB. Prevalence of psychiatric disorders in 4 to 16-year-olds with Williams syndrome. Am J Med Genet Part B. 2006;141B:615–622. doi: 10.1002/ajmg.b.30344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyfer OT, Woodruff-Borden J, Mervis CB. Anxiety disorders in children with Williams syndrome, their mothers, and their siblings: Implications for the etiology of anxiety disorders. J Neurodev Disord. 2009;1:4–14. doi: 10.1007/s11689-009-9003-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mervis CB, John AE. Williams syndrome: Psychological characteristics. In: Shapiro B, Accardo P, editors. Neurogenetic syndromes: Behavioral issues and their treatment. Brookes; Baltimore, MD: 2009. pp. 81–98. [Google Scholar]
- Mervis CB, Morris CA. Williams syndrome. In: Mazzocco MMM, Ross JL, editors. Neurogenetic developmental disorders: Variation of manifestation in childhood. MIT Press; Cambridge, MA: 2007. pp. 199–262. [Google Scholar]
- Mervis CB, Robinson BF, Bertrand J, Morris CA, Klein-Tasman BP. Armstrong SC. 2000. The Williams Syndrome Cognitive Profile. Brain Cogn. 44:604–628. doi: 10.1006/brcg.2000.1232. [DOI] [PubMed] [Google Scholar]
- Miyazaki Y, Raudenbush SW. Tests for linkage of multiple cohorts in an accelerated longitudinal design. Psychol Methods. 2000;5:44–63. doi: 10.1037/1082-989x.5.1.44. [DOI] [PubMed] [Google Scholar]
- Morris CA. The dysmorphology, genetics, and natural history of Williams-Beuren syndrome. In: Morris CA, Lenhoff HM, Wang PP, editors. Williams-Beuren syndrome: Research, evaluation, and treatment. Johns Hopkins University Press; Baltimore, MD: 2006. pp. 3–17. [Google Scholar]
- Morris CA. Williams syndrome. In: Cassidy SB, Allanson JE, editors. Management of genetic syndromes. 2nd edition Wiley; New York: 2005. pp. 18–58. [Google Scholar]
- Morris CA, Mervis CB. Williams syndrome. In: Goldstein S, Reynolds CR, editors. Handbook of neurodevelopmental and genetic disorders in children. Guilford Press; New York: 1999. pp. 555–590. [Google Scholar]
- Moss S, Goldberg D, Patel P, Prosser H, Ibbotson B, Simpson N, et al. The Psychiatric Assessment Schedule for Adults with Developmental Disabilities. University of Manchester, Hester Adrian Research Centre; Manchester, England: 1996. [Google Scholar]
- Neuhaus JM. Assessing change with longitudinal and clustered binary data. Annu Rev Public Health. 2001;22:115–28. doi: 10.1146/annurev.publhealth.22.1.115. [DOI] [PubMed] [Google Scholar]
- Ollendick TH. Reliability and validity of the Revised Fear Survey Schedule for Children (FSSC-R) Behav Res Ther. 1983;21:685–692. doi: 10.1016/0005-7967(83)90087-6. [DOI] [PubMed] [Google Scholar]
- O’Reilly MF, Lancioni GE. Treating food refusal in a child with Williams syndrome using the parent as therapist in the home setting. J Intellect Disabil Res. 2001;45:41–46. doi: 10.1046/j.1365-2788.2001.00291.x. [DOI] [PubMed] [Google Scholar]
- Phillips KD, Klein-Tasman BP. Mental health concerns in Williams syndrome: Intervention considerations and illustrations from case examples. J Ment Health Res Intellect Disabil. 2009;2:110–133. [Google Scholar]
- Pober BR, Dykens EM. Williams syndrome: An overview of medical, cognitive, and behavioral features. Child Adolesc Psychiatr Clin N Am. 1996;5:929–943. [Google Scholar]
- Porter MA, Dodd H, Cairns D. Psychopathological and behavior impairments in Williams-Beuren syndrome: The influences of gender, chronological age, and cognition. Child Neuropsychol. 2009:1–16. doi: 10.1080/09297040802577881. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YF, Congdon RT. HLM 6: Hiecharchial Linear and Nonlinear Modeling. Scientific Software International; Lincolnwood, IL: 2004. [Google Scholar]
- Reich W, Shayka JJ, Taibelson C. Diagnostic Interview Schedule for Children and Adolescents, parent version. Washington University; St. Louis, MO: 1991. [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV: Parent Interview Schedule. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with anxiety disorders interview schedule for DSM-IV: Child and parent versions. J Am Acad Child Adolesc Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford University Press; New York: 2003. [Google Scholar]
- Stinton C, Elison S, Howlin P. Mental health problems in adults with Williams syndrome. Am J Intellect Dev Disabil. 2010;115:3–18. doi: 10.1352/1944-7558-115.1.3. [DOI] [PubMed] [Google Scholar]
- Strømme P, Bjørnstad PG, Ramstad K. Prevalence estimation of Williams syndrome. J Child Neurol. 2002;17:269–271. doi: 10.1177/088307380201700406. [DOI] [PubMed] [Google Scholar]
- Switaj DM. Identification and measurement of anxiety and obsessive-compulsive tendencies in the Williams Syndrome behavioral phenotype. ProQuest Information & Learning; US: 2000. [Google Scholar]
- Tager-Flusberg H, Plesa-Skwerer D, Faja S, Joseph RM. People with Williams syndrome process faces holistically. Cognition. 2003;89:11–24. doi: 10.1016/s0010-0277(03)00049-0. [DOI] [PubMed] [Google Scholar]
- Tager-Flusberg H, Sullivan K. A componential view of theory of mind: Evidence from Williams syndrome. Cognition. 2000;76:59–89. doi: 10.1016/s0010-0277(00)00069-x. [DOI] [PubMed] [Google Scholar]
- Tonge BJ, Einfeld SL. Psychopathology and intellectual disability: The Australian child to adult longitudinal study. In: Glidden LM, editor. International review of research in mental retardation. Vol. 26. Academic Press; San Diego, CA: 2003. pp. 61–91. [Google Scholar]
- Udwin O, Yule W. A cognitive and behavioral phenotype in Williams syndrome. J Clin Exp Neuropsychol. 1991;13:232–244. doi: 10.1080/01688639108401040. [DOI] [PubMed] [Google Scholar]
- Vasey MW. Development and cognition in childhood anxiety: The example of worry. In: Ollendick TH, Prinz RJ, editors. Advances in clinical child psychology. Vol. 15. Plenum; New York: 1993. pp. 1–39. [Google Scholar]
- von Arnim G, Engle P. Mental retardation related to hypercalcaemia. Dev Med Child Neurol. 1964;6:366–377. doi: 10.1111/j.1469-8749.1964.tb08138.x. [DOI] [PubMed] [Google Scholar]
- Wang S, Robertson GP, Zhu J. A novel human homologue of Drosophila polycomblike gene is up-regulated in multiple cancers. Article. Gene. 2004;343:69–78. doi: 10.1016/j.gene.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JN, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta analytic review. Biol Psychiatry. 2005;57:1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]
- Woodruff-Borden J, Leyfer OT. Anxiety and fear. In: Hersen M, editor. Clinicians’ handbook of child behavioral assessment. Elsevier; Burlington, MA: 2006. pp. 267–289. [Google Scholar]
- Zitzer-Comfort C, Doyle TF, Masataka N, Korenberg JR, Bellugi U. Nature and nurture: Williams syndrome across cultures. Dev Sci. 2007;10:755–762. doi: 10.1111/j.1467-7687.2007.00626.x. [DOI] [PubMed] [Google Scholar]