Summary
In a preliminary prospective randomised study, a series of 5 patients submitted to classic Tongue Base Reduction with Hyo-Epiglottoplasty (TBRHE according to Chabolle et al., 1998) is compared to a series of 7 patients submitted to a modified version of Chabolle’s procedure. The changes introduced in the new surgical technique can be summarised as follows: a) lower neck skin incision; b) different neurovascular bundle identification; c) submucosal tongue base muscle resection; d) variation of the caudal hyoid stabilisation, already described by the Authors in 2008 (Tongue Base Reduction with Thyro-Hyoido-Pexy). The objective has been primarily to compare the feasibility, functional effectiveness and overall tolerability of the modified procedure. In this preliminary study Tongue Base Reduction with Thyro-Hyoido-Pexy has proven to be an easy and rapid procedure, with shorter post-operative functional recovery and comparable polysomnographic and neuro-psychological short time results.
Keywords: OSAHS surgery, Tongue base surgery, Prospective randomised study
Riassunto
In uno studio prospettico randomizzato, sono stati preliminarmente confrontati un gruppo di 5 pazienti sottoposti a Resezione della Base Lingua con Ioido-Epiglottoplastica (TBRHE sec. Chabolle et al., 1998) con un secondo gruppo di 7 casi trattati con tecnica di Chabolle modificata sec. l’Autore (CV). Nella nuova tecnica chirurgica, le principali variazioni apportate possono essere riassunte come segue: a) la più bassa sede di incisione cutanea; b) la diversa modalità di reperimento del peduncolo neurovascolare; c) la tecnica di resezione per via sottomucosa del tessuto base-lingua; d) la variazione della sospensione caudale ioidea già descritta dall’Autore (CV) nel 2008 (Resezione della Base Lingua con Tiro-Ioido-Pessia). Il principale obiettivo di questo studio è stato comparare la procedura modificata nella sua fattibilità, efficacia funzionale e tollerabilità complessiva. Nel nostro studio preliminare la Resezione della Base Lingua con Tiro-Ioido-Pessia si è rivelata una procedura facile e veloce, con un più rapido recupero funzionale post-chirurgico, e nel breve tempo, comparabili risultati polisonnografici e neuropsicologici.
Introduction
Tongue Base Surgery for Obstructive Sleep Apnea Hypopnoea Syndrome (OSAHS) has been a classic though uncommon approach for a long time. Tongue Base Reduction with Hyo-Epiglottoplasty (TBRHE) was described for the first time in 1998 by Chabolle et al. 1. One year later, ten cases of severe OSAHS were described in a second report 2. A previous anatomical study was published focusing on the topographic relationship between the neurovascular bundle and the tongue base 3. To our knowledge a single paper was published in the international literature by an Author from a different group 4. Another joint contribution is included in the Official Report of the North Italian ENT Society dealing with Snoring & OSAHS Surgery 5. Unfortunately, far fewer studies, compared to relatively less valid operations (e.g.: genioglossus advancement), were devoted to this highly effective surgical technique. The basic idea of this revisited TBRHE is to improve the fundamental steps of the procedure and to integrate it with an unedited variation of enlarged caudal hyoid stabilisation (Tongue Base Reduction with Thyro-Hyoido-Pexy [TBRTHP]) 6. Additional innovative modifications have been used (Table I).
Table I. Differential features of the two surgical procedures.
| TBRHE | TBRTHP | |
| Skin incision | Supra-hyoid | Infra-hyoid |
| Neuro-vascular identification | Medial | Lateral |
| TB resection | Transmucosal | Submucosal |
| Hyoid suspension | to mandible | to thyroid cartilage |
TBRHE: Tongue Base Reduction with Hyo-Epiglottoplasty; TBRTHP: Tongue Base Reduction with Thyro-Hyoido-Pexy; TB: Tongue Base
Aims of the present study were to assess the feasibility of a modified Tongue Base Reduction (TBR), the TBRTHP, and to compare TBRTHP with TBRHE in short time effectiveness in reducing OSAHS severity and in overall tolerability for the patient. Polysomnographic (PSG), Neuropsychological (NPS) and subjective outcomes together with complication rate have been evaluated in order to demonstrate the equal opportunity offered by this new revisitation of the classic Chabolle procedure.
Surgical procedure: our modifications
An infra-isthmic tracheotomy is usually the first step through a separate low horizontal incision 7. The basic improvements of the revisited TBRHE can be outlined as follows:
The access skin incision is planned in a horizontal natural crease at the level of the thyroid cartilage, with a horizontal curved shape between the two sub-mandible gland areas (Fig. 1).
Following gentle retraction of the mandible gland, the so-called Pirogoff triangle is exposed 8. At that level, through a blunt dissection, the hypoglossal nerve and lingual veins are identified on the surface of the hyoglossus muscle and are followed as far as possible towards the tongue base. In the centre of the triangular area, deep to the hyoglossus muscle, the lingual artery is dissected free further to a blunt division of hyoglossus muscles fibres.
An anterior pharyngotomy is carried out, step by step in a supra-hyoid approach, gaining access to the pharynx at the level of the valleculae. Pharyngeal lateral wall muscle insertion to the superior aspect of hyoid lesser cornu is strictly spared. TBR is carefully performed in a submucosal approach between the vallecular area, lingual-tonsillar folds and circumvallate papillae. Upon completion of the surgical resection, the redundant tongue base lympho-mucosal tissue is trimmed and carefully stitched to the tongue base muscle.
Thyro-Hyoido-Pexy (THP) starts with section of the infra-hyoid muscles at the level of the inferior one third of the thyroid cartilage in order to reveal the internal branch of the superior laryngeal nerve and prevent any surgical injury. After the traditional application of the four stitches between the hyoid bone and thyroid notch, an additional suture is passed around the greater cornu and the posterior area of the thyroid cartilage ala 6 (Fig. 2).
Fig. 1.
Infra-hyoid skin incision.
Fig. 2.
Thyro-Hyoido-Pexy (THP).
Setting
An ENT & Oral Surgery Department in a Tertiary Care Hospital with several years’ experience in Sleep-Disordered Breathing Surgery (since 1995, 1500 patients and overall 2500 procedures).
Material and methods
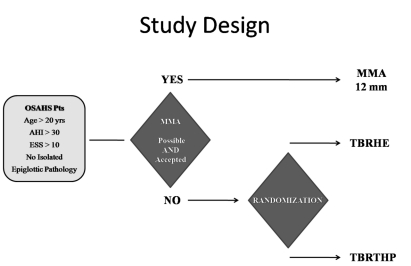
A series of 12 successive cases of severe adult OSAHS (Apnoea-Hypopnoea Index [AHI] > 30, Epworth Sleepiness Scale [ESS] > 10), after refusal of conservative treatment or drop out (nCPAP, oral appliance-MAD, weight loss) and after exclusion for Maxillo-Mandibular Advancement (facial skeleton counter-indication or patient’s specific surgery refusal) have been prospectively randomised into two different branches according to the surgical procedure carried out. Branch one, 5 cases: conventional TBRHE according to Chabolle et al. (1998) 1. Branch two, 7 cases: modified TBR with Thyro-Hyoido-Pexy (TBRTHP) according to the Author (CV) (Fig. 3). The profile of the two recruited groups is outlined in Table II. The standard diagnostic approach included: history, ENT physical examination, digital nose-pharyngo-laryngeal videoendoscopy, imaging (panorex and lateral cephalometric X-rays), polysomnography according to the AIMS-AIPO guidelines 9, NPS evaluation according to our protocol including ESS and verbal numeric scale of subjective percentage satisfaction. Functional recovery times and discharge times, as well as possible complications, were also included in the evaluation. Last but not least, Overall Operating Room (OR) Times (time span between entrance and exit from OR) and Surgical Times (time between the first surgical incision and the last stitch) have been compared. The single step times have been recorded by OR Anaesthesiological Staff Doctors and Nurses with a special monitoring programme: the Managing Programme Log80. The two groups were relatively well balanced in terms of number of randomised cases (7 vs. 5), sex ratio (no females were included in either group), mean age (53.3 vs. 56.2 years), age distribution (46÷65 vs. 47÷63). The randomised TBRTHP group presented a lower mean pre-operative (pre-op) AHI: 54.5 (42÷87) compared with the TBRHE group AHI: 68.4 (54÷76). This is similar for Body Mass Index (BMI) and ESS. All the procedures have been carried out in the same Institution by the same surgeon (CV). If required, patients, in both groups, have also been submitted to associated nose and palate procedures (Table III).
Fig. 3.
Study design. MMA: Maxillo-Mandibular Advancement; TBRHE: Tongue Base Reduction with Hyo-Epiglottoplasty; TBRTHP: Tongue Base Reduction with Thyro-Hyoido-Pexy.
Table II. Pre-operative profile of the two groups of patients.
| TBRHE | TBRTHP | ||
| Cases | 5 | 7 | |
| M/F | 5/0 | 7/0 | |
| Age (yrs) | Mean | 56.2 | 53.3 |
| σ | 6.1 | 6.4 | |
| BMI | Mean | 37.3 | 29.1 |
| σ | 4.1 | 1.9 | |
| AHI pre | Mean | 68.4 | 54.5 |
| σ | 7.9 | 14.2 | |
| LOS pre | Mean | 59.0 | 63.7 |
| σ | 10.6 | 9.4 | |
| ESS pre | Mean | 16.8 | 11.6 |
| σ | 4.5 | 2.9 |
BMI: Body Mass Index; AHI: Apnoea-Hypopnoea Index; LOS: Lowest O2 Sat; ESS: Epworth Sleepiness Scale; σ: Standard Deviation
Table III. Associated procedures and OR times.
| TBRHE | TBRTHP | ||
| + UPPP | 5/5 | 2/7 | |
| + Nose surgery | 3/5 | 0/7 | |
| Overall OR times (min) | |||
| Mean | 242.0 | 225.0 | |
| σ | 60.5 | 48.4 | |
| Surgical times (min) | |||
| Mean | 169.0 | 145.0 | |
| σ | 50.2 | 40.7 | |
Overall OR Times: time span between entrance and exit from operating room; Surgical times: time span between the first surgical incision and the last stitch; σ: Standard Deviation; TBRHE: Tongue Base Reduction with Hyo-Epiglottoplasty; TBRTHP: Tongue Base Reduction with Thyro-Hyoido-Pexy
Results
After an average follow-up of 10 months, PSG and NPS outcomes were evaluated. Results are outlined in Tables III– V. The OR time, general OR occupation, as well as the effective surgical time are almost identical. Swallowing recovery time is shorter for TBRTHP than for TBRHE. The discharge time for TBRTHP is not really shorter. The mean post-operative (post-op) AHI was higher in the TBRHE group (33.6) than in the TBRTHP group (13.1). Post-op Lowest O2 Saturation (LOS) was higher for TBRHTP than for TBRHE. ESS remained about 10 in theTBRHE group and dropped to 6.0 in the TBRTHP patients. Expressed satisfaction degree was 73% in TBRHE, and 89.3% in TBRTHP patients.
Table V. Results.
| TBRHE | TBRTHP | ||
| AHI post | |||
| Mean | 33.6 | 13.1 | |
| σ | 23.0 | 6.2 | |
| LOS post | |||
| Mean | 65.6 | 81.4 | |
| σ | 13.4 | 3.7 | |
| ESS post | |||
| Mean | 10.2 | 6.0 | |
| σ | 3.2 | 2.2 | |
| Satisfaction % | |||
| Mean | 73.0 | 89.3 | |
| σ | 38.9 | 8.6 |
AHI: Apnoea-Hypopnoea Index; LOS: Lowest O2 Sat; ESS: Epworth Sleepiness Scale; σ: Standard Deviation; TBRHE: Tongue Base Reduction with Hyo-Epiglottoplasty; TBRTHP: Tongue Base Reduction with Thyro-Hyoido-Pexy
Complications
Complications are outlined in Table IV. The complication rate is relatively high, however, the complexity of the patient’s status and the severity of the procedure offer a reasonable explanation. Moreover, all the recorded complications have been easily resolved by means of conservative approaches without additional surgical procedures. Infectious problems, related to mandibular sutures, have been recorded only in the TBRHE group. Two temporary small pharyngocutaneous fistulas have been observed in the TBRTHP group, conservatively treated with one week of medical therapy. No permanent neural damage has been recorded.
Table IV. Recovery profile and complications.
| TBRHE | TBRTHP | ||
| Swallowing recovery after (days) | |||
| Mean | 17.3 | 10.0 | |
| σ | 10.3 | 2.7 | |
| Hospital discharge after (days) | |||
| Mean | 22.6 | 18.0 | |
| σ | 10.5 | 4.2 | |
| Complications | |||
| Infection | 2 | 0 | |
| Fistula | 1 | 2 | |
| XII cn paresis (transient) | 1 | 0 | |
| Bleeding | 0 | 0 | |
TBRHE: Tongue Base Reduction with Hyo-Epiglottoplasty; TBRTHP: Tongue Base Reduction with Thyro-Hyoido-Pexy; cn: cranial nerve; σ: Standard Deviation
Discussion
Skin incision, in a natural crease, produces a surgical scar which is far less noticeable than the classical one, which is particularly evident in the anterior sub-mandibular area. Not unlike the classic approach, in oncological neck procedures, this incision is possible since no mandibular dissection in the mental area is required, and no sub-mental extension of the incision has to be planned. Identification of the neurovascular bundle, in the Pirogoff 8 triangle and trigonum linguale, seems to be easier and faster, as well as far less traumatic for the suprahyoid muscles which are completely spared, except for the incision required for pharyngotomy. In no cases in which the modified approach was used, was the hypoglossal nerve inadvertently injured. Following the present comparative study, we strongly believe that sparing the supra-hyoid muscles is of paramount importance for post-op functional recovery. Reduction of the submucosal tongue base muscles by means of bipolar scissors or warm knife allows a final watertight covering of the surgical field, contributing to a less painful post-op period and faster healing. THP with posterior stitches and reabsorbable sutures appear to be particularly effective in lateral wall tending and stabilisation, as theoretically described in the longitudinal forces model of pharynx stabilisation in OSAHS reported by Schwartz et al. 10. Mandible dissection and drilling is not required. The overall surgical time is comparable and functional recovery is significantly faster. It is noteworthy that no infection has been observed in the TBRTHP group, probably due to the absence of a suprahyoid suture. The overall rate of short-term pharyngocutaneous fistulisation in the supra-hyoid area is higher in the TBRTHP group, probably related to the opening forces exerted, in this area, by the thyro-hyoid sutures. The relatively small number of patients in both procedures does not allow further considerations.
Conclusions
In our experience, TBRTHP has proved to be an easy and rapid procedure compared to the classic TBRHE, with better post-op evolution in terms of pain, functional recovery, hospital stay and comparable PSG and NPS outcomes. Further studies, with a larger number of cases and significant statistical evaluations are mandatory in order to confirm these preliminary findings. The present work should be considered a preliminary report: conclusions are supported by simple trend observations and not by strict statistical evaluations. These will be possible only in the next months during which a larger number of cases will be studied.
Acknowledgments
Authors express their gratitude to all medical members of ENT Staff, and Anaesthesiological Staff for assistance in OR time calculations.
References
- 1.Chabolle F, Wagner I, Séquert C, et al. Tongue base reduction with hyoid-epiglottoplasty. A surgical alternative in severe sleep apnea syndromes. Ann Otolaryngol Chir Cervicofac 1998;115:322-31. [PubMed] [Google Scholar]
- 2.Chabolle F, Wagner I, Blumen MB, et al. Tongue base reduction with hyoepiglottoplasty: a treatment for severe obstructive sleep apnea. Laryngoscope 1999;109:1273-80. [DOI] [PubMed] [Google Scholar]
- 3.Séquert C, Lestang P, Baglin AC, et al. Hypoglossal nerve in its intralingual trajectory: anatomy and clinical implications. Ann Otolaryngol Chir Cervicofac 1999;116:207-17. [PubMed] [Google Scholar]
- 4.Sorrenti G, Piccin O, Scaramuzzino G, et al. Tongue base reduction with hyoepiglottoplasty for the treatment of severe OSA. Acta Otorhinolaryngol Ital 2004;24:204-10. [PubMed] [Google Scholar]
- 5.Vicini C, Sorrenti G. Algoritmo decisionale ipofaringeo. In: Vicini C, editor. Strategie di gestione del paziente in roncochirurgia ORL. Official Report of XLVII North Italian ENT Congress. Genova: Giofil 2001, p. 97-106. [Google Scholar]
- 6.Benazzo M, Pagella F, Matti E, et al. Hyoidthyroidpexia as a treatment in multilevel surgery for obstructive sleep apnea. Acta Otolaryngol 2008;128:680-4. [DOI] [PubMed] [Google Scholar]
- 7.Campanini A, De Vito A, Frassineti S, et al. Temporary tracheotomy in the surgical treatment of obstructive sleep apnea syndrome: personal experience. Acta Otorhinolaryngol Ital 2003;23:474-8. [PubMed] [Google Scholar]
- 8.Testut L, Jacob O. Trattato di anatomia topografica. Torino: UTET 1933. [Google Scholar]
- 9.Commissione paritetica AIPO-AIMS. Linee Guida di Procedura Diagnostica nella Sindrome delle Apnee Ostruttive dell’adulto. Rass Patol Appar Respir 2001;16:278-80. [Google Scholar]
- 10.Schwartz AR, Eisele DW, Smith PL. Pharyngeal airway obstruction in obstructive sleep apnea: pathophysiology and clinical implications. Otolaryngol Clin North Am 1998;31:911-8. [DOI] [PubMed] [Google Scholar]