Abstract
Introduction
US disparities in Black:White infant mortality are persistent. National trends, however, may obscure local successes.
Methods
Zero-corrected, negative binomial multivariable modeling was used to predict Black infant mortality (1999–2003) in all US counties with reliable rates. Independent variables included county population size, racial composition, educational attainment, poverty, income and geographic origin. Resilient counties were defined as those whose Black infant mortality rate residual score was <2.0. Mortality data was accessed from the Compressed Mortality File compiled by the National Center for Health Statistics and found on the CDC WONDER website. Demographic information was obtained from the US Census.
Results
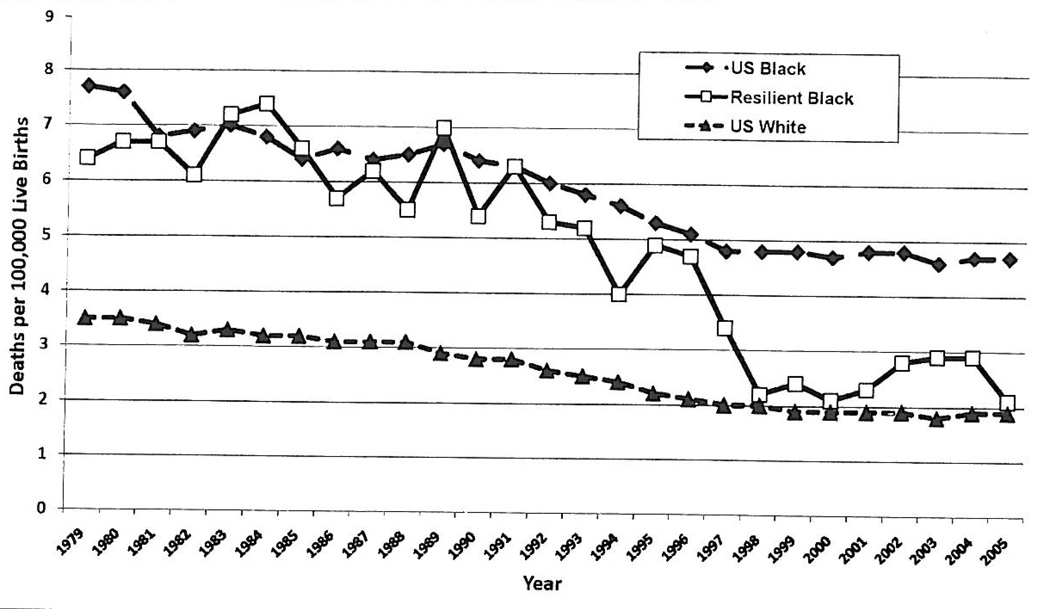
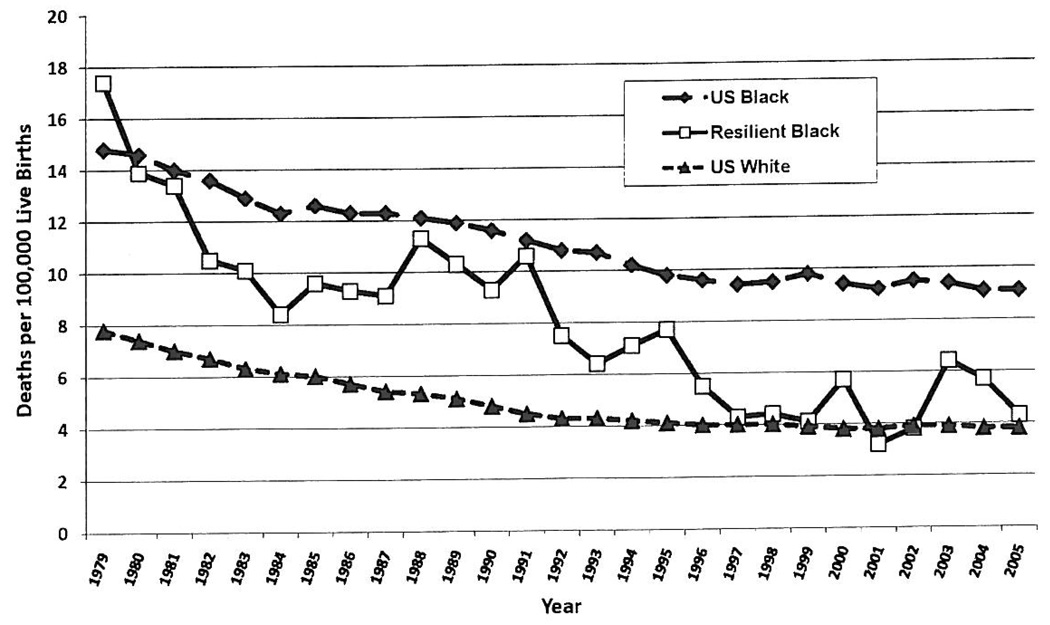
The final model included the percentage of Blacks, age 18 to 64 years, speaking little or no English (P<.008), a socioeconomic index comprising educational attainment, poverty, and per capita income (P<.001), and household income in 1990 (P<.001). After accounting for these factors, a stratum comprising Essex and Plymouth Counties, Mass.; Bronx, N.Y.; and Multnomah, Ore. was identified as unusually resilient. Percentage of Black poverty and educational attainment in Black women in the resilient stratum approximated the average for all 330 counties, In 1979, Black infant mortality in the resilient stratum (23.6 per 1,000 live births) exceeded Black US infant mortality (22.6). By 2001, Black infant mortality in the resilient stratum (5.6) was below the corresponding value for Whites (5.7). Resilient county neonatal mortality declined both early and late in the observation period, while post-neonatal declines were most marked after 1996.
Conclusions
Models for reduction/elimination of racial disparities in US infant mortality, independent from county-level contextual measures of socioeconomic status, may already exist.
Keywords: Infant Mortality, Socioeconomic Status, Resilience, Racial Disparity
INTRODUCTION
Infant mortality rate (IMR) reflects access and quality of pre- and postnatal maternal and infant medical care and is linked to community health status.1 IMR may also be a proxy for overall maternal and infant health, since preterm labor and/or delivery (PTD), and low birthweight or very low birthweight are significant contributors to infant mortality.2
Unfortunately, IMR stands as a marker of continued US health disparity. Black infant mortality is consistently more than twice that of White infants (14.1 vs 5.7 for 1999–2005),3 and nationally, the Black:White infant mortality rate ratio increased from 2.0 in 1979 to 2.4 in 2005. While monitoring of national trends is important, exclusive reliance on national, state or regional data may obscure important successes (or failures) at the local level.4 We used transgeographic analysis5 to learn whether a stratum of communities having greater resilience to disparities in Black:White infant mortality might be found.
METHODS
We used the Compressed Mortality File (CMF) from the National Center for Health Statistics (NCHS), a national mortality and population database in the public domain that contains annual county, age, sex, race, and cause-specific data for the period 1979 to 2005.6 We identified all US counties with stable Black and White infant mortality rates as defined by NCHS (at least 20 deaths) for the period 1999–2003 sufficient to meet standards of confidentiality. This period was selected to provide data that was both current and close to the 2000 Census. We merged the infant mortality data with data from the US Census.7 Independent variables included: a) a socioeconomic index,8 which was calculated by adding county rank for the percent Black women aged ≥25 years, with <high school education to county rank for percent Blacks with annual income below poverty, and 1/county rank for per capita income; the higher the socioeconomic index, the lower the county socioeconomic status; b) percent Blacks with annual income below poverty; c) total population; d) percent Black-alone population; e) percent foreign-born; f) percent population born in another state and born in the south (This variable is found in the 2000 Census survey, and represents a single indicator. For clarification: when surveyed by the Census, these individuals reported that they were not born in their current state of residence, and the state of their birth is documented as Southern. Research has demonstrated that there is increased vulnerability for multiple negative health outcomes for individuals born in the South, including but not limited to cardiovascular disease and cancer); g) household income in 1990 and 2000; h) percent Blacks aged 18 to 64 years speaking little or no English; i) ethnic diversity; j) number of White live births; and k) Black:White infant mortality rate ratio. Strong correlations were found between the socioeconomic index and percent Blacks with annual income below poverty and between White infant mortality and Black:White infant mortality rate ratio. Percent Blacks with annual income below poverty and White infant mortality were therefore not considered in the initial model. The Poisson distribution was rejected for modeling because the value of the ratio between the deviance and the degrees of freedom (40.0) was far in excess of 1.0. Instead, we used the more stable negative binomial model.9,10 This was zero-corrected because county selection was based on having at least 20 Black infant deaths during the observation period. The SAS GEN-MOD (SAS Institute, Cary, N.C., 1999) procedure was used to formulate the final model. Resilient counties were defined as those with standardized residual values of <2.0. Yearly (1979 to 2005) race-specific infant, neonatal and post-neonatal infant mortality was recorded for the stratum of resilient counties and for the United States as a whole.
RESULTS
Of the 3,141 US counties and county equivalents (parishes, independent cities, and the District of Columbia), 330 had 20 or more Black infant deaths in 1999–2003. These counties comprised 84% of all US Black infant deaths and 54% of all White US infant deaths in the observation period. Results for the final multivariable model are shown in Table 1. Statistically significant associations with Black infant mortality for 1999–2003 included percent foreign-born (P<.001), percent Blacks speaking little or no English (P<.001), socioeconomic index (P<.001), and household income in 1990 (P<.018).
Table 1.
Analysis of parameter estimates: Zero-corrected, negative binomial model to predict Black infant mortality for 1999–2003 in 330 US counties
| Parameter | DF | Estimate | Standard Error | Wald 95% | Confidence Limits | Chi-Square | P |
|---|---|---|---|---|---|---|---|
| Intercept | 1 | 6.98 | 0.15 | 6.68 | 7.27 | 2105.37 | <.001 |
| Percent foreign born | 1 | −1.13 | 0.22 | −1.56 | −0.69 | 25.97 | <.001 |
| Percent Blacks ages 18 to 64, speaking little or no English |
1 | −8.29 | 3.12 | −14.42 | −2.17 | 7.04 | .008 |
| Socioeconomic index* | 1 | 0.001 | 0.002 | 0.01 | 0.01 | 15.39 | <.001 |
| Household income (1990) | 1 | 0.05 | 0.004 | −0.001 | −0.000 | 5.58 | .018 |
| Dispersion | 1 | 0.046 | 0.004 | 0.04 | 0.05 |
Equals ranks for (percent Black women aged ≥ 25 years who are not high school graduates + percent of Blacks with annual income below poverty + reciprocal of Black per capita income)/3. The higher value of the index, the lower the socioeconomic status of the county
After accounting for all factors in the final model, Black infant mortality in the following counties were found to have residual values of <2.0 (that is, the county’s Black infant mortality for 1999–2003 was significantly less than that predicted by the model): Essex and Plymouth Counties, Mass.; Bronx County, N.Y.; and Multnomah County, Ore. Notably, these counties were not socioeconomic outliers. On the contrary, the mean ± standard deviation for percentage of Blacks with annual income below poverty was 24.3% ± 0.4 in the resilient stratum and 25.4 ± 0.8 for all 330 counties. Similarly the percentage of Black women aged ≥25 years, without a high school education was 26.1 ± 0.4 in the resilient counties and 27.0 ± 0.8 for all 330 counties. Corresponding values for the nation as a whole according to the 2000 US Census are 30.7 ± 0.2 (percent Blacks with annual income below poverty) and 26.3 ± 0.2 (percent Black women aged ≥25 years who are not high school graduates. According to the 2000 US Census, the percent White individuals aged ≥25 years who were not high school graduates was 16.4% and the percent Whites with annual income below poverty was 8.9%.
Figures 1 through 3 show annual race-specific mortality rates for the United States as a whole and for Blacks in the resilient stratum. Figure 1 details infant mortality, while Figures 2 and 3 show neonatal and post-neonatal infant mortality respectively. Interestingly, these three figures demonstrate a parallel decline in Black and White infant mortality from 1979 through 2005, resulting in consistent disparities of outcomes. However, there are remarkable and dramatic declines in the same indices for the resilient Black communities resulting in rates similar to Whites in 2005.
Fig 1.
Infant mortality. Race-specific US and resilient Black stratum (Essex and Plymouth Counties, MA; Bronx, NY; Multnomah, OR). 1979–2005
Fig 3.
Post-neonatal infant mortality. Race-specific US and resilient Black Stratum (Essex and Plymouth Counties, MA; Bronx, NY; Multnomah, OR). 1979–2005
Fig 2.
Neonatal mortality. Race-specific US and resilient Black stratum (Essex and Plymouth Counties, MA; Bronx, NY; and Multnomah, OR). 1979–2005
DISCUSSION
Contrary to commonly accepted reports based on national or regional samples,11,12 Black:White disparities in infant mortality are not inevitable in the United States. After accounting for socioeconomic and other demographic factors, we identified a stratum of US counties in which racial disparities in overall, neonatal and post-neonatal infant mortality had been reduced and on occasion eliminated or reversed between 1979 and 2005, even though Blacks in these counties had substantially lower educational attainment and higher levels of poverty than White Americans. The data are therefore consistent with the hypothesis that in the resilient counties, poverty was not eliminated, but perhaps was overcome. Our study does not supply sufficient evidence to determine if the improved outcomes are based on medical or sociologic impact, both or neither. But, it does suggest a need to hone in on such counties to identify the contributing factors.
Many theoretical explanations for Black-White differences in IMR are plausible. Low socioeconomic status, low educational status, race, differences in quality of medical care (prenatal care: content, onset, quality in terms of frequency and timeliness),13 subspecialty care and hospital quality have all been suggested.14 In addition, stress, environmental issues such as problems with the water supply (contamination, as in Monsanto and Anniston, Al), toxins, racism, substance abuse, nutrition issues, and bacterial vaginosis or other infectious diseases may be culprits.15,16 Given evidence of multi-factorial influences on birth outcomes, our study may suggest a need for evaluation of the identified successful counties to see how they have addressed the leading health indicators, such as overweight and obesity, environmental quality, immunization, access to health care, responsible sexual behavior, mental health, injury and violence prevention, physical activity, and avoidance of substance abuse and tobacco use.
Methods similar to those used in the present study have also been applied to HIV/AIDS and screening mammography.17 These studies demonstrated that widened US Black:White disparities in HIV mortality occurred among all age groups following the licensure of Highly Active Antiretroviral Treatment (HAART) for HIV/AIDS and after implementation of reimbursement for screening by Medicare, but also demonstrated that these were not inevitable. As in our study, county-level success was not equated with unusually high county-level socioeconomic status. Instead, it is hypothesized that resilience reflected a more equitable racial diffusion of health care innovation. Meis et al 18 have also conducted secondary analyses of a randomized trial of 17α-hydroxyprogesterone in women that raised the questions about unequal diffusion of innovation to economically under-served, and medically under-served communities.
Our study has several limitations. First is its reliance on death certificate data. Death certificates do not provide relevant information concerning the mother and her use of prenatal care or the type and quality of post-natal care. Some information regarding pre-natal care is available through Linked Birth/Infant Death Records (CDC), but a comprehensive understanding of why success came to the resilient counties would require reconstruction of health and illness records in these communities as compared to less successful geographic areas. Second, we used ecological socioeconomic and demographic descriptors. It is not necessarily true that results from ecologic analyses will match those that include information at the individual level. Third, there is debate in the biostatistical literature concerning the best model for use in the multivariate analyses.9,10 The current evidence is that negative binomial models provide the most valid option. Fourth, in selecting the particular communities identified out of the overall reliable sources of communities, we may have eliminated communities of note. Although our analysis accounted for 84% of the Black deaths and 54% of the White deaths, there may be something or significance in communities with very low numbers of infant deaths that represent long-term success rather than “unstable rates.” By eliminating these communities, we have possibly limited the findings of this study. Fifth, social, environmental, community, maternal and/or paternal influences, lifestyle, maternal and/or neonatal interventions (or lack thereof) may all contribute to the occurrence of the identified mortality rates in the anomalous communities. Health care needs to be evaluated not only in terms of availability and affordability, but in actual content and quality of delivery and services. Equity in health care, rather than just enhancing the technological basis of care, may be part of the missing link to solving this conundrum. In addition, we may need to also observe for not only decreases in IMR, but for prevention of increases in these rates. African American women, even if college-educated, have an excess mortality rate that is 90% higher than that of White college-educated women.19
In conclusion, the present data and much of the current literature suggest that continued US infant mortality health disparities go beyond race, socioeconomic status and health care. Murray et al,20 for example, describe this by noting, “The observed disparities in life expectancy cannot be explained by race, income or basic healthcare access and utilization alone.” Similarly, we, in the United States, have observed the “paradoxical” occurrence whereby recent immigrants from Mexico, the Caribbean, Africa and elsewhere, regardless of their financial status on arrival to this country and despite poverty and poor education, have low birthweight, preterm delivery, SIDS, as well as infant mortality rates less than or equivalent to that of Whites. Notably, acculturation of immigrant groups is associated with their subsequent experiences of poorer health outcomes.
IMPLICATIONS FOR IMPROVING HEALTH DISPARITIES
The present data give hope that infant mortality disparities may not be inevitable. Further investigation of resilient counties and/or communities may help guide interventions capable of improving birth outcomes nationally.
ACKNOWLEDGMENTS
This research and publication was made possible by Grant Number 5P20RR011104 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCRR or NIH. Yvonne W. Fry-Johnson, MD, MSCR was funded in part through the MSCR Program: Grant Number 5R25RR17694, from the Clinical Research Education and Career Development (CRECD) in Minority Institutions. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of CRECD, NCRR or NIH.
REFERENCES
- 1.Rowley DL, Fry YW. Handbook of Black American Health: Policies and Issues behind Disparities in Health. 2nd Edition. Santa Barbara, Calif.: Greenwood Publishing Group, Inc.; 2004. Reproductive health disparities among African American women; pp. 451–469. [Google Scholar]
- 2.Centers for Dísease Control and Prevention. Infant mortality and low birch weight among Black and White infants—United States, 1980–2000. MMWR. 2002;51(27):589–592. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Racial and ethnic disparities in infant mortality rates – 60 largest US cities, 1995–1998. MMWR. 2002;51(15):329–332. [PubMed] [Google Scholar]
- 4.Blumenthal DS, DiClemente RJ. Community-Based Health Research: Issues and Methods. New York, New York: Springer Publishing Company; 2004. [Google Scholar]
- 5.Levine RS, Briggs NC, Hollar D, et al. Descriptive and Analytic Epidemiologic Studies to Identify Modifiable Determinants of Disparities in Mortality Rates between Blacks and Whites. Ethn Dis. 2007;17(2):280–283. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Compressed Mortality File 1999–2003. [Last accessed November 20, 2009];Atlanta, Ga.: Centers for Dísease Control; CDC WONDER on-line database, compiled from Compressed Mortality File CMF 1999–2003. 2003 Available at: http://wonder.cdc.gov/cmf-icd9.html.
- 7.US Census Bureau. [Last accessed May 15, 2007];Short Form 3. Available at: http://www.census.gov.
- 8.Steenland K, Halperin W, Hus, et al. Deaths due to injuries among employed adults; the effects of socioeconomic class. Epidemiology. 2003;14(1):74–79. doi: 10.1097/00001648-200301000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Gardner W, Mulvey EP, Shaw EC. Regression analysis of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychol. Bull. 1995;118:393–404. doi: 10.1037/0033-2909.118.3.392. [DOI] [PubMed] [Google Scholar]
- 10.Byers AL, Allore H, Gill TM, Peduzzi PN. Application of negative binomial modeling for discrete outcomes: A case study in aging research. J Clin Epidemiol. 2003;56(6):559–564. doi: 10.1016/s0895-4356(03)00028-3. [DOI] [PubMed] [Google Scholar]
- 11.Gamble VN. Trust, medical care, and racial and ethnic minorities. In: Satcher D, Pamies RJ, editors. Multicultural Medicine and Health Disparities. New York: McGraw-Hill Medical Publishing Division; 2006. pp. 437–448. [Google Scholar]
- 12.Rowland CJ, Hargraves MA. Commentary: Class, Race, and Infant Mortality in the United States. Am J Public Health. 1993;83(1):9–12. doi: 10.2105/ajph.83.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gortmaker SL, Wise PH. The first injustice: socioeconomic disparities, health services technology, and infant mortality. Annu Rev Social. 1997;23:147–170. doi: 10.1146/annurev.soc.23.1.147. [DOI] [PubMed] [Google Scholar]
- 14.Levine RS, Briggs NC, Husaini BA, Hennekens CH. Geographic studies of Black-White mortality”. In: Satcher D, Pamies RJ, editors. Multicultural Medicine and Health Disparities. New York: McGraw-Hill Medical Publishing Division; 2006. pp. 33–104. [Google Scholar]
- 15.Hogue CJR, Bremner JD. Stress model for research into preterm delivery among black women. Am J Obstet Gynecol. 2005;192:S47–S55. doi: 10.1016/j.ajog.2005.01.073. [DOI] [PubMed] [Google Scholar]
- 16.Hogan VK, Ferre CD. The social context of pregnancy for African American women: implications for the study and prevention of adverse perinatal outcomes. Maternal Child Health J. 2001;5(2):67–69. doi: 10.1023/a:1011360813893. [DOI] [PubMed] [Google Scholar]
- 17.Levine RS, Briggs NC, Kilbourne BS, et al. Black-White mortality from HIV-disease before and after introduction of HAART in 1996. Am J Public Health. 2007;97(10):1–9. doi: 10.2105/AJPH.2005.081489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meis PJ, Klebanoffm M, Dombrowski MP, et al. Does progesterone treatment influence risk factors for recurrent preterm delivery? Obstet Gynecol. 2005;106(3):557–561. doi: 10.1097/01.AOG.0000174582.79364.a7. [DOI] [PubMed] [Google Scholar]
- 19.McGrady G, Sung JF, Rowley DL, Hogue CL. Preterm delivery and LBW among first-born infants of Black and White college graduates. Am J of Epidemiol. 1992;136(3):266–276. doi: 10.1093/oxfordjournals.aje.a116492. [DOI] [PubMed] [Google Scholar]
- 20.Murray CJL, Kulkarni SC, Michaud C, et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Medicine. 2006;3(9):1513–1524. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]